Development and Implementation of Workshops to Optimize the Delivery of Vaccination Services in Community Pharmacies: Thinking beyond COVID-19
Abstract
1. Introduction
2. Methods
2.1. Participant Recruitment
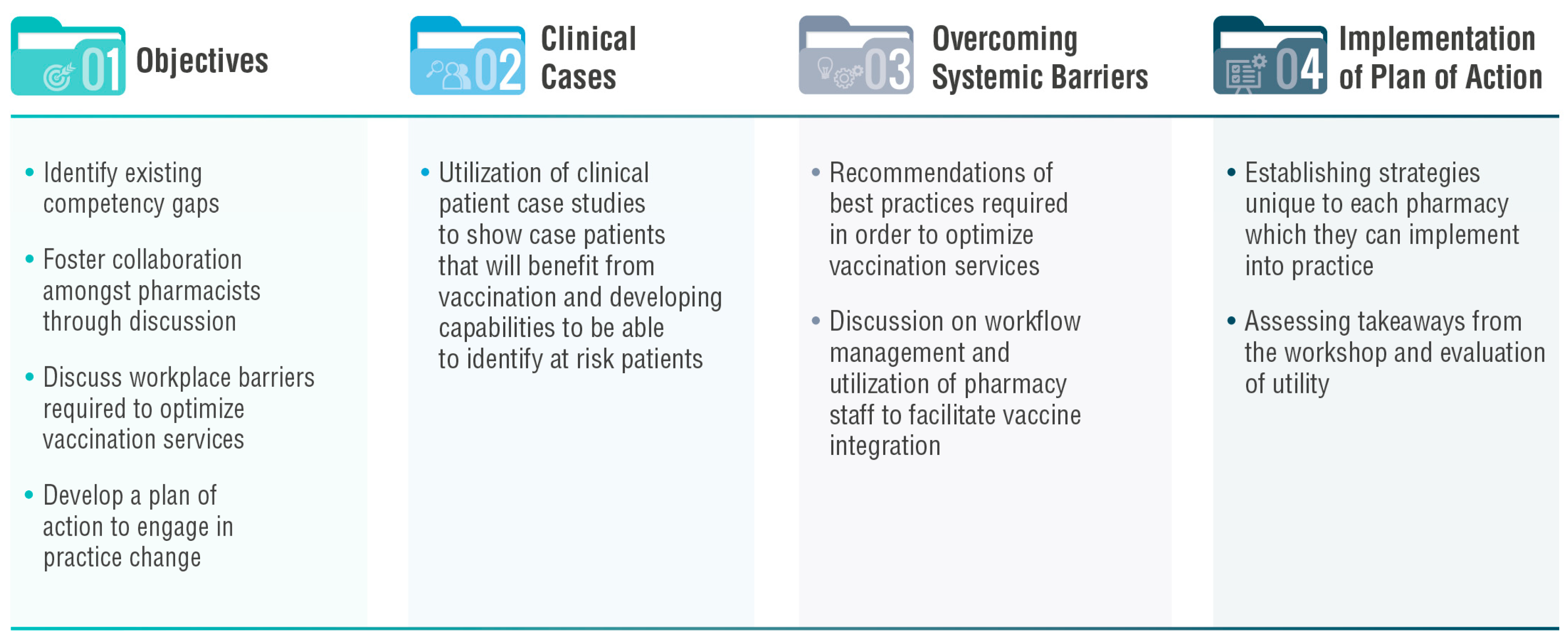
2.2. Workshop Development
2.3. Workshop Evaluation
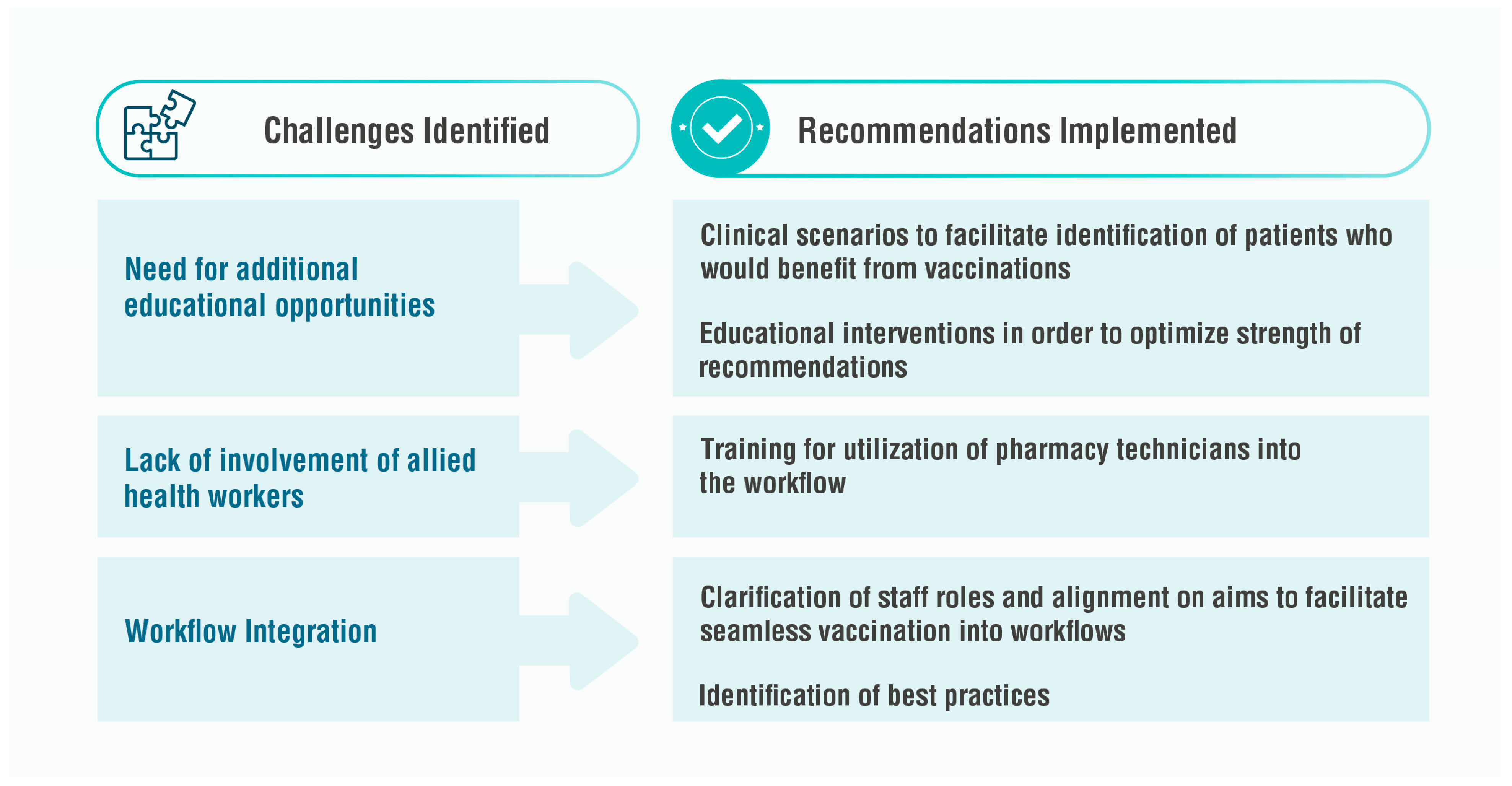
3. Results and Discussion
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Tannenbaum, C.; Tsuyuki, R.T. The Expanding Scope of Pharmacists’ Practice: Implications for Physicians. CMAJ 2013, 185, 1228–1232. [Google Scholar] [CrossRef]
- Zhou, M.; Desborough, J.; Parkinson, A.; Douglas, K.; McDonald, D.; Boom, K. Barriers to Pharmacist Prescribing: A Scoping Review Comparing the UK, New Zealand, Canadian and Australian Experiences. Int. J. Pharm. Pract. 2019, 27, 479–489. [Google Scholar] [CrossRef]
- Bhanbhro, S.; Drennan, V.M.; Grant, R.; Harris, R. Assessing the Contribution of Prescribing in Primary Care by Nurses and Professionals Allied to Medicine: A Systematic Review of Literature. BMC Health Serv. Res. 2011, 11, 330. [Google Scholar] [CrossRef]
- Cooper, R.J.; Anderson, C.; Avery, T.; Bissell, P.; Guillaume, L.; Hutchinson, A.; James, V.; Lymn, J.; McIntosh, A.; Murphy, E.; et al. Nurse and Pharmacist Supplementary Prescribing in the UK—A Thematic Review of the Literature. Health Policy 2008, 85, 277–292. [Google Scholar] [CrossRef]
- Gerard, K.; Tinelli, M.; Latter, S.; Blenkinsopp, A.; Smith, A. Valuing the Extended Role of Prescribing Pharmacist in General Practice: Results from a Discrete Choice Experiment. Value Health 2012, 15, 699–707. [Google Scholar] [CrossRef]
- Allinson, M.D.; Black, P.E.; White, S.J. Professional Dilemmas Experienced by Pharmacy Graduates in the United Kingdom When Transitioning to Practice. Am. J. Pharm. Educ. 2022, 86, 8643. [Google Scholar] [CrossRef]
- Atkinson, J. Advances in Pharmacy Practice: A Look towards the Future. Pharmacy 2022, 10, 125. [Google Scholar] [CrossRef]
- Weeks, G.; George, J.; Maclure, K.; Stewart, D. Non-medical prescribing versus medical prescribing for acute and chronic disease management in primary and secondary care. Cochrane Database Syst. Rev. 2016, 11, CD011227. [Google Scholar] [CrossRef]
- Tsuyuki, R.T.; Houle, S.K.; Charrois, T.L.; Kolber, M.R.; Rosenthal, M.M.; Lewanczuk, R.; Campbell, N.R.; Cooney, D.; McAlister, F.A. Randomized trial of the effect of pharmacist prescribing on improving blood pressure in the community: The Alberta clinical trial in optimizing hypertension (RxACTION). Circulation 2015, 132, 93–100. [Google Scholar] [CrossRef]
- Tsuyuki, R.T.; Rosenthal, M.; Pearson, G.J. A randomized trial of a community-based approach to dyslipidemia management: Pharmacist prescribing to achieve cholesterol targets (RxACT Study). Can. Pharm. J. Rev. Des Pharm. Du Can. 2016, 149, 283–292. [Google Scholar]
- Al Hamarneh, Y.N.; Charrois, T.; Lewanczuk, R.; Tsuyuki, R.T. Pharmacist intervention for glycaemic control in the community (the RxING study). BMJ Open 2013, 3, e003154. [Google Scholar] [CrossRef]
- Hedden, L.; Barer, M.L.; McGrail, K.; Law, M.; Bourgeault, I.L. In British Columbia, the supply of primary care physicians grew, but their rate of clinical activity declined. Health Aff. 2017, 36, 1904–1911. [Google Scholar] [CrossRef]
- Kim, J.J.; Tian, A.H.; Pham, L.; Nakhla, N.; Houle, S.K.; Wong, W.W.; Alsabbagh, M.W. Economic evaluation of pharmacists prescribing for minor ailments in Ontario, Canada: A cost-minimization analysis. Int. J. Pharm. Pract. 2021, 29, 228–234. [Google Scholar] [CrossRef]
- Harrington, D.W.; Wilson, K.; Rosenberg, M.W. Waiting for a specialist consultation for a new condition in Ontario: Impacts on patients’ lives. Healthc. Policy 2014, 9, 90. [Google Scholar]
- Majercak, K.R. Advancing pharmacist prescribing privileges: Is it time? J. Am. Pharm. Assoc. 2019, 59, 783–786. [Google Scholar] [CrossRef]
- Raiche, T.; Pammett, R.; Dattani, S.; Dolovich, L.; Hamilton, K.; Kennie-Kaulbach, N.; Mccarthy, L. Community pharmacists’ evolving role in Canadian primary health care: A vision of harmonization in a patchwork system. Pharm. Pract. 2020, 18, 2171. [Google Scholar]
- Gibbard, R. Meeting the Care Needs of Canada’s Aging Population; The Conference Board of Canada: Ottawa, ON, Canada, 2018; pp. 1–12. [Google Scholar]
- Association, Canadian Pharmacists. A Review of Pharmacy Services in Canada and the Health and Economic Evidence; CPA: Ottawa, ON, Canada, 2016. [Google Scholar]
- Dalton, K.; Byrne, S. Role of the pharmacist in reducing healthcare costs: Current insights. Integr. Pharm. Res. Pract. 2017, 6, 37–46. [Google Scholar] [CrossRef]
- Marchildon, G.P. Health Care Cost Drivers: The Facts; Canadian Institute for Health Information: Ottawa, ON, Canada, 2011.
- Schindel, T.J.; Yuksel, N.; Breault, R.; Daniels, J.; Varnhagen, S.; Hughes, C.A. Perceptions of pharmacists’ roles in the era of expanding scopes of practice. Res. Soc. Adm. Pharm. 2017, 13, 148–161. [Google Scholar] [CrossRef]
- Schindel, T.J.; Yuksel, N.; Hughes, C.A. Prescribing by Pharmacists. In Encyclopedia of Evidence in Pharmaceutical Public Health and Health Services Research in Pharmacy; Springer: Berlin/Heidelberg, Germany, 2022; pp. 1–22. [Google Scholar]
- Adams, T.L.; Wannamaker, K. Professional regulation, profession-state relations and the pandemic response: Australia, Canada, and the UK compared. Soc. Sci. Med. 2022, 296, 114808. [Google Scholar] [CrossRef]
- Kellar, J.; Austin, Z. The only Way Round Is through: Professional Identity in Pharmacy Education and Practice; SAGE Publications Sage CA: Los Angeles, CA, USA, 2022; pp. 238–240. [Google Scholar]
- Draaisma, M. Pharmacies Ready to Help Administer COVID-19 Vaccines across Canada, Association Says. Available online: https://www.cbc.ca/news/canada/toronto/neighbourhood-pharmacy-association-of-canada-local-pharmacies-role-covid-19-vaccine-rollout-1.5913587 (accessed on 8 February 2023).
- Waite, N.M.; McCarthy, L.; Milne, E.; Hillier, C.; Houle, S.K.; Dolovich, L. Perceived preparedness for full-scope pharmacist services among recent Doctor of Pharmacy graduates from Ontario schools of pharmacy. J. Am. Pharm. Assoc. 2018, 58, 630–637. [Google Scholar] [CrossRef]
- The Canadian Pharmacists Association Pharmacists’ Vaccination Authority Across Canada. Available online: http://www.pharmacists.ca/cpha-ca/assets/File/cpha-on-the-issues/Scope_of_Practice_Immunization_Dec2020.pdf (accessed on 8 February 2023).
- Adams, A.J. Regulating pharmacist services: Achieving a full scope of practice. Can. Pharm. J. Rev. Des Pharm. Du Can. 2023, 20, 1–10. [Google Scholar] [CrossRef]
- Isenor, J.; Edwards, N.; Alia, T.; Slayter, K.; MacDougall, D.; McNeil, S.; Bowles, S. Impact of pharmacists as immunizers on vaccination rates: A systematic review and meta-analysis. Vaccine 2016, 34, 5708–5723. [Google Scholar] [CrossRef]
- Fonseca, J.; Pearson Sharpe, J.; Houle, S.K.; Waite, N.M. Time for harmonization: Pharmacists as immunizers across Canadian jurisdictions. Can. Pharm. J. Rev. Des Pharm. Du Can. 2019, 152, 395–400. [Google Scholar] [CrossRef]
- Srirangan, K.; Lavenue, A. Helping québec pharmacists seize the vaccination service opportunity: The pharmacy best practice workshops. Pharmacy 2021, 9, 51. [Google Scholar] [CrossRef]
- Rampin, R.; Rampin, V. Taguette: Open-source qualitative data analysis. J. Open Source Softw. 2021, 6, 3522. [Google Scholar] [CrossRef]
- Gobis, B.; Zed, P.J. The journey begins: BC roadmap for pharmacist integration into team-based primary care. Can. Pharm. J. Rev. Des Pharm. Du Can. 2020, 153, 141–143. [Google Scholar]
- Violette, R.R.; Houle, S.K.; Nissen, L.M.; Waite, N.M. The International Pharmacists-as-Immunizers Partnership (IPIP)—Advancing Research on Pharmacist-Administered Immunizations Worldwide. Pharmacy 2019, 7, 53. [Google Scholar] [CrossRef]
- Skoy, E.T.; Kelsch, M.; Hall, K.; Choi, B.-J.; Carson, P. Increasing adult immunization rates in a rural state through targeted pharmacist education. J. Am. Pharm. Assoc. 2020, 60, e301–e306. [Google Scholar] [CrossRef]
- Caffrey, A.R.; DeAngelis, J.M.; Ward, K.E.; Orr, K.K.; Morrill, H.J.; Gosciminski, M.; LaPlante, K.L.; Bratberg, J.P.; Caetano, M.L.; Feret, B. A pharmacist-driven academic detailing program to increase adult pneumococcal vaccination. J. Am. Pharm. Assoc. 2018, 58, 303–310. [Google Scholar] [CrossRef]
- Pullagura, G.R.; Violette, R.; Houle, S.K.; Waite, N.M. Exploring influenza vaccine hesitancy in community pharmacies: Knowledge, attitudes and practices of community pharmacists in Ontario, Canada. Can. Pharm. J. Rev. Pharm. Can. 2020, 153, 361–370. [Google Scholar]
- Tolentino, V.; Unni, E.; Montuoro, J.; Bezzant-Ogborn, D.; Kepka, D. Utah pharmacists’ knowledge, attitudes, and barriers regarding human papillomavirus vaccine recommendation. J. Am. Pharm. Assoc. 2018, 58, S16–S23. [Google Scholar] [CrossRef]
- Peteet, B.; Belliard, J.; Abdul-Mutakabbir, J.; Casey, S.; Simmons, K. Community-academic partnerships to reduce COVID-19 vaccine hesitancy in minoritized communities. EClinicalMedicine 2021, 34, 100834. [Google Scholar] [CrossRef]
- Rhodes, L.A.; Branham, A.R.; Dalton, E.E.; Moose, J.S.; Marciniak, M.W. Implementation of a vaccine screening program at an independent community pharmacy. J. Am. Pharm. Assoc. 2017, 57, 222–228. [Google Scholar] [CrossRef]
- Percy, J.N.; Crain, J.; Rein, L.; Hohmeier, K.C. The impact of a pharmacist-extender training program to improve pneumococcal vaccination rates within a community chain pharmacy. J. Am. Pharm. Assoc. 2020, 60, 39–46. [Google Scholar] [CrossRef]
- McKeirnan, K.C.; Frazier, K.R.; Nguyen, M.; MacLean, L.G. Training pharmacy technicians to administer immunizations. J. Am. Pharm. Assoc. 2018, 58, 174–178.e1. [Google Scholar] [CrossRef]
- Bertsch, T.G.; McKeirnan, K.C.; Frazier, K.; VanVoorhis, L.; Shin, S.; Le, K. Supervising pharmacists’ opinions about pharmacy technicians as immunizers. J. Am. Pharm. Assoc. 2019, 59, 527–532. [Google Scholar] [CrossRef]
- Administration of COVID-19 Vaccine by Pharmacy Professionals. Ontario College of Pharmacists. Available online: https://www.ocpinfo.com/regulations-standards/practice-policies-guidelines/administration-of-covid-19-vaccine-by-pharmacy-professionals/ (accessed on 8 February 2023).
- Wisnivesky, J.P.; Lorenzo, J.; Lyn-Cook, R.; Newman, T.; Aponte, A.; Kiefer, E.; Halm, E.A. Barriers to adherence to asthma management guidelines among inner-city primary care providers. Ann. Allergy Asthma Immunol. 2008, 101, 264–270. [Google Scholar] [CrossRef]
- Galvao, T.F.; Silva, M.T.; Neiva, C.S.; Ribeiro, L.M.; Pereira, M.G. Problem-based learning in pharmaceutical education: A systematic review and meta-analysis. Sci. World J. 2014, 2014, 578382. [Google Scholar] [CrossRef]
- Zhou, J.; Zhou, S.; Huang, C.; Xu, R.; Zhang, Z.; Zeng, S.; Qian, G. Effectiveness of problem-based learning in Chinese pharmacy education: A meta-analysis. BMC Med. Educ. 2016, 16, 23. [Google Scholar] [CrossRef]
- Firkus, D.; McCoy, R.G.; Matulis III, J.; Kessler, M.; Mara, K.; Herges, J. Evaluation of pharmacist consults within a collaborative enhanced primary care team model to improve diabetes care. PLoS ONE 2023, 18, e0280654. [Google Scholar] [CrossRef]
- Scott, S. Unveiling the Latest Deprescribing Research: A New Themed Collection; Oxford University Press UK: Oxford, UK, 2023; pp. 267–268. [Google Scholar]
- Fathima, M.; Naik-Panvelkar, P.; Saini, B.; Armour, C.L. The role of community pharmacists in screening and subsequent management of chronic respiratory diseases: A systematic review. Pharm. Pract. 2013, 11, 228. [Google Scholar] [CrossRef]
- Bridgeman, M.B.; Wilken, L.A. Essential role of pharmacists in asthma care and management. J. Pharm. Pract. 2021, 34, 149–162. [Google Scholar] [CrossRef]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Lavenue, A.; Simoneau, I.; Mahajan, N.; Srirangan, K. Development and Implementation of Workshops to Optimize the Delivery of Vaccination Services in Community Pharmacies: Thinking beyond COVID-19. Pharmacy 2023, 11, 129. https://doi.org/10.3390/pharmacy11040129
Lavenue A, Simoneau I, Mahajan N, Srirangan K. Development and Implementation of Workshops to Optimize the Delivery of Vaccination Services in Community Pharmacies: Thinking beyond COVID-19. Pharmacy. 2023; 11(4):129. https://doi.org/10.3390/pharmacy11040129
Chicago/Turabian StyleLavenue, Arnaud, Isabelle Simoneau, Nikita Mahajan, and Kajan Srirangan. 2023. "Development and Implementation of Workshops to Optimize the Delivery of Vaccination Services in Community Pharmacies: Thinking beyond COVID-19" Pharmacy 11, no. 4: 129. https://doi.org/10.3390/pharmacy11040129
APA StyleLavenue, A., Simoneau, I., Mahajan, N., & Srirangan, K. (2023). Development and Implementation of Workshops to Optimize the Delivery of Vaccination Services in Community Pharmacies: Thinking beyond COVID-19. Pharmacy, 11(4), 129. https://doi.org/10.3390/pharmacy11040129




