The Resilience of Final-Year Pharmacy Students and Aspects of the Course They Found to Be Resilience-Building
Abstract
:1. Introduction
2. Materials and Methods
3. Results
3.1. Response Rate and Demographic Information (Section C of the Questionnaire)
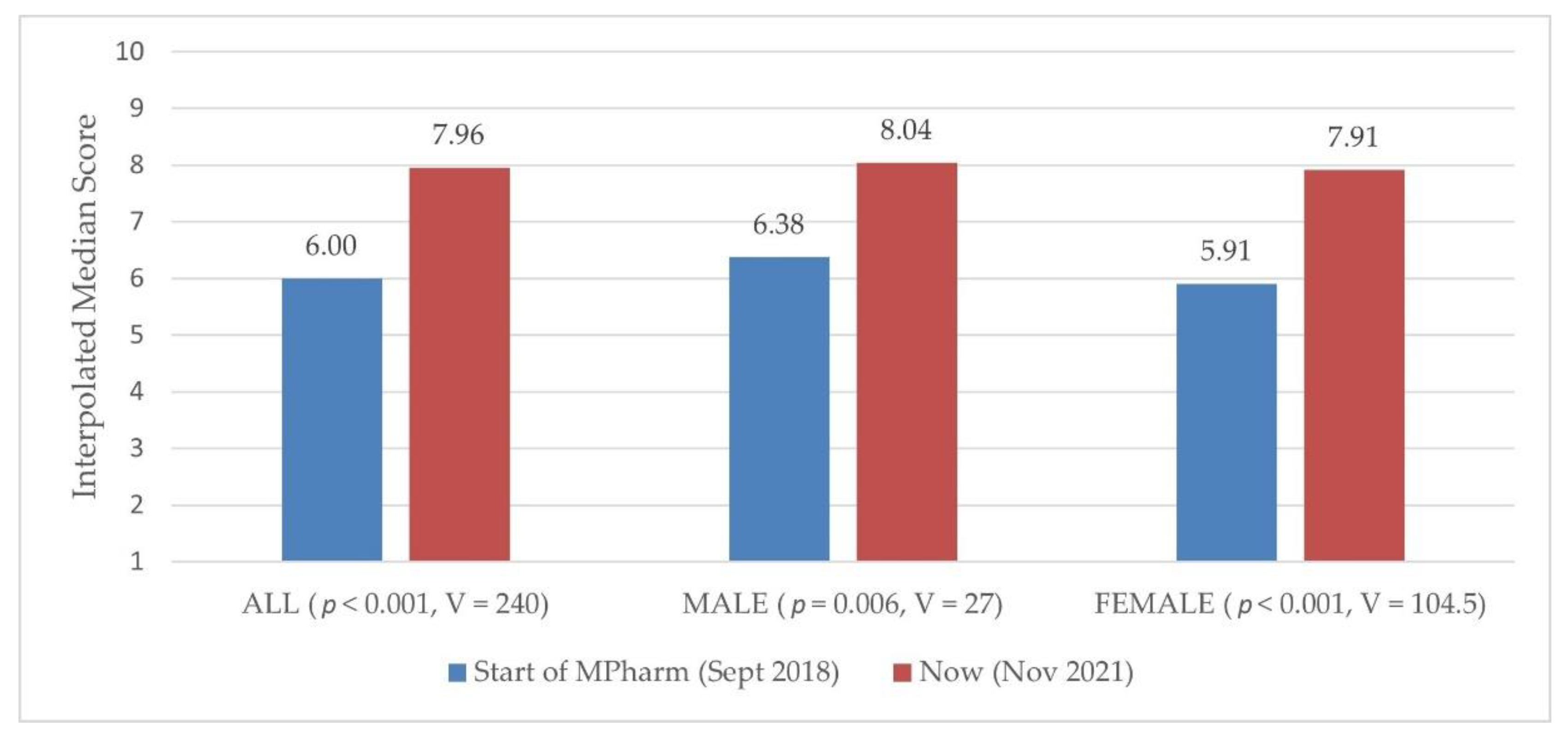
3.2. CD-RISC-25 (Section A of the Questionnaire)
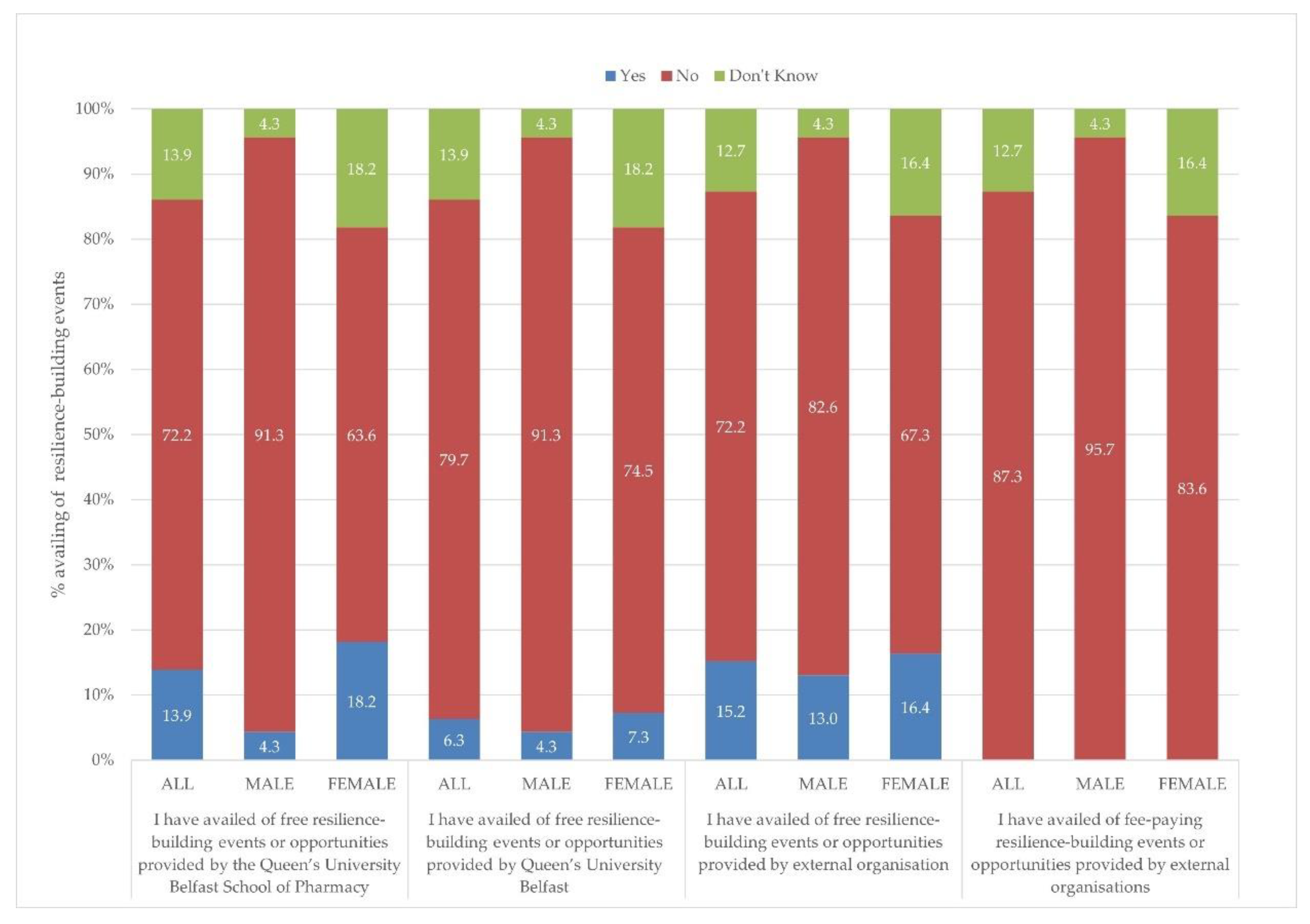
3.3. The Role of the QUB School of Pharmacy in Building Resilience and Whether Certain Aspects Helped Build Resilience (Section B of the Questionnaire)
4. Discussion
Ten Approaches That QUB School of Pharmacy Intend to Implement in Light of Undertaking This Work
- To help students develop skills, we will set expectations and context for the year ahead through a formal induction. We will aim to provide greater scaffolding and support in the earlier years but taper this back as the students progress into third and final year.
- While we have a role to play in building students’ resilience, there is still a lack of evidence outlining the best way to do this. Any training sessions or multicomponent interventions about resilience that we add into the course should be evaluated to determine their short- and longer-term success.
- Encourage and facilitate students to reflect, including suggesting that they may want to keep a journal.
- Introduce productive meetings for students with their personal tutors about ways to build resilience and confidence. Help personal tutors to appreciate where support is available for students’ mental health and well-being, and help them with professional and personal development.
- Develop guidance about assessments (including how to prepare, perfectionism, and dealing with stress, pressure, failure and setbacks) and produce an assessment and feedback calendar for students.
- Increase the amount of peer support and encouragement available through the formation of communities of practice and networks.
- Expand the School of Pharmacy Mental Health and Well-Being team’s scope to include resilience ambassadors (alongside the student mental health first-aiders).
- Review the learning and teaching strategy to ensure that our approaches enable students to become competent and confident through active learning opportunities. Investigate the balance between instructor-led teaching and peer- or self-directed learning and discovery. Review the interprofessional learning material to ensure that it encompasses real-world issues.
- Review the assessment strategy to ensure there is adequate formative assessment to allow students to make mistakes in a safe environment and learn from them. Consider the justification for using a range of pass marks and think more holistically about the assessment burden
- Ensure that resilience-building events have explicit links to resilience and are promoted adequately. Recommend relevant resources, such as the podcast series ‘The Resilient Pharmacist’ [37].
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Kokou-Kpolou, C.K.; Jumageldinov, A.; Park, S.; Nieuviarts, N.; Noorishad, P.-G.; Cénat, J.M. Prevalence of Depressive Symptoms and Associated Psychosocial Risk Factors among French University Students: The Moderating and Mediating Effects of Resilience. Psychiatr. Q. 2021, 92, 443–457. [Google Scholar] [CrossRef]
- Mladen, S.; Loughan, A.; Kinser, P.; Crawford, M.; Jones, A.; Edwards, S.; Rybarczyk, B.; Braun, S.E. An analysis of psychological distress profiles and their correlates in interdisciplinary health-care professional students. Glob. Adv. Health Med. 2019, 8, 2164956119879872. [Google Scholar] [CrossRef] [PubMed]
- Jiménez-Ortiz, J.L.; Islas-Valle, R.M.; Jiménez-Ortiz, J.D.; Pérez-Lizárraga, E.; Hernández-García, M.E.; González-Salazar, F. Emotional exhaustion, burnout, and perceived stress in dental students. J. Int. Med. Res. 2019, 47, 4251–4259. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Frajerman, A.; Morvan, Y.; Krebs, M.O.; Gorwood, P.; Chaumette, B. Burnout in medical students before residency: A systematic review and meta-analysis. Eur. Psychiatry 2019, 55, 36–42. [Google Scholar] [CrossRef] [PubMed]
- Farrell, S.M.; Kadhum, M.; Lewis, T.; Singh, G.; Penzenstadler, L.; Molodynski, A. Wellbeing and burnout amongst medical students in England. Int. Rev. Psychiatry 2019, 31, 579–583. [Google Scholar] [CrossRef] [PubMed]
- Chisholm-Burns, M.A.; Berg-Poppe, P.; Spivey, C.A.; Karges-Brown, J.; Pithan, A. Systematic review of noncognitive factors influence on health professions students’ academic performance. Adv. Health Sci. Educ. Theory Pract. 2021, 26, 1373–1445. [Google Scholar] [CrossRef]
- McCann, L.; Hughes, C.M.; Adair, C.G.; Cardwell, C. Assessing job satisfaction and stress among pharmacists in Northern Ireland. Pharm. World Sci. 2009, 31, 188–194. [Google Scholar] [CrossRef]
- Kushal, A.; Gupta, S.; Metha, M.; Singh, M.M. Study of stress among health care professionals: A systemic review. Int. J. Res. Found. Hosp. Healthc. Adm. 2018, 6, 6–11. [Google Scholar] [CrossRef]
- Robertson, H.D.; Elliott, A.M.; Burton, C.; Iversen, L.; Murchie, P.; Porteous, T.; Matheson, C. Resilience of primary healthcare professionals: A systematic review. Br. J. Gen. Pract. 2016, 66, e423–e433. [Google Scholar] [CrossRef] [Green Version]
- Whitfield, K.; Arya, V.; Austin, Z.; Bajis, D.; Bradley, C.; Clark, B.; Exintaris, B.; Galbraith, K.; El Hajj, M.S.; Hall, K.; et al. Developing a Global Community of Practice for Pharmacy Workforce Resilience—Meet GRiT. Pharmacy 2021, 9, 110. [Google Scholar] [CrossRef]
- Windle, G.; Bennett, K.M.; Noyes, J. A methodological review of resilience measurement scales. Health Qual. Life Outcomes 2011, 9, 8. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Davidson, J.R.T. Connor-Davidson Resilience Scale (CD-RISC) Manual. 23 June 2021. Unpublished. Available online: www.cd-risc.com (accessed on 5 September 2021).
- Chisholm-Burns, M.A.; Spivey, C.A.; Sherwin, E.; Williams, J.; Phelps, S. Development of an instrument to measure academic resilience among pharmacy students. Am. J. Pharm. Educ. 2019, 83, 6896. [Google Scholar] [CrossRef] [PubMed]
- Cassidy, S.; Mawdsley, A.; Langran, K.; Hughes, L.; Willis, S.C. A Large-Scale Multicentre Study of Academic Resilience and Wellbeing in Pharmacy Education. Am. J. Pharm. Educ. 2022, 86, 8998. [Google Scholar] [CrossRef] [PubMed]
- Chisholm-Burns, M.A. Building resilience to combat stress, burnout, and suicidal ideation among pharmacists. Am. J. Health Syst. Pharm. 2019, 76, 1364–1367. [Google Scholar] [CrossRef] [PubMed]
- Dresser, J.D.; Whitfield, K.M.; Kremer, L.J.; Wilby, K.J. Exploring how postmillennial pharmacy students balance life priorities and avoid situations known to deplete resilience. Am. J. Pharm. Educ. 2021, 85, 8369. [Google Scholar] [CrossRef] [PubMed]
- Schlesselman, L.S.; Cain, J.; DiVall, M. Improving and Restoring the Well-being and Resilience of Pharmacy Students during a Pandemic. Am. J. Pharm. Educ. 2020, 84, ajpe8144. [Google Scholar] [CrossRef]
- Hanna, L.-A.; Wilson, M.; Hall, M.; Hanna, A. A questionnaire study to investigate stress among future pharmacists by gender and year group. Pharmacy 2018, 6, 75. [Google Scholar] [CrossRef] [Green Version]
- Dillman, D.A.; Smyth, J.D.; Christian, L.M. Internet, Phone, Mail, and Mixed-Mode Surveys: The Tailored Design Method, 4th ed.; John Wiley & Sons: Hoboken, NJ, USA, 2014; p. 21. [Google Scholar]
- Nowell, L.S.; Norris, J.M.; White, D.E.; Moules, N.J. Thematic analysis: Striving to meet the trustworthiness criteria. Int. J. Qual. Methods 2017, 16, 1609406917733847. [Google Scholar] [CrossRef]
- Enrique Roig, A.; Mooney, O.; Salamanca-Sanabria, A.; Lee, C.T.; Farrell, S.; Richards, D. Assessing the Efficacy and Acceptability of a Web-Based Intervention for Resilience among College Students: Pilot Randomized Controlled Trial. JMIR Form. Res. 2020, 4, e20167. [Google Scholar] [CrossRef]
- Peng, L.; Zhang, J.; Li, M.; Li, P.; Zhang, Y.; Zuo, X.; Miao, Y.; Xu, Y. Negative life events and mental health of Chinese medical students: The effect of resilience, personality and social support. Psychiatry Res. 2012, 196, 138–141. [Google Scholar] [CrossRef]
- Cheng, J.; Zhao, Y.Y.; Wang, J.; Sun, Y.H. Academic burnout and depression of Chinese medical students in the pre-clinical years: The buffering hypothesis of resilience and social support. Psychol. Health Med. 2020, 25, 1094–1105. [Google Scholar] [CrossRef]
- Liu, Y.; Pan, H.; Yang, R.; Wang, X.; Rao, J.; Zhang, X.; Pan, C. The relationship between test anxiety and emotion regulation: The mediating effect of psychological resilience. Ann. Gen. Psychiatry 2021, 20, 40. [Google Scholar] [CrossRef] [PubMed]
- Lekan, D.A.; Ward, T.D.; Elliott, A.A. Resilience in Baccalaureate Nursing Students: An Exploration. J. Psychosoc. Nurs. Ment. Health Serv. 2018, 56, 46–55. [Google Scholar] [CrossRef] [PubMed]
- Rahimi, B.; Baetz, M.; Bowen, R.; Balbuena, L. Resilience, stress, and coping among Canadian medical students. Can. Med. Educ. J. 2014, 5, e5–e12. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Aloba, O.; Olabisi, O.; Aloba, T. The 10-Item Connor-Davidson Resilience Scale: Factorial Structure, Reliability, Validity, and Correlates Among Student Nurses in Southwestern Nigeria. J. Am. Psychiatr. Nurses Assoc. 2016, 22, 43–51. [Google Scholar] [CrossRef]
- Ang, W.H.D.; Shorey, S.; Hoo, M.X.Y.; Chew, H.S.J.; Lau, Y. The role of resilience in higher education: A meta-ethnographic analysis of students’ experiences. J. Prof. Nurs. 2021, 37, 1092–1109. [Google Scholar] [CrossRef]
- Kunzler, A.M.; Helmreich, I.; König, J.; Chmitorz, A.; Wessa, M.; Binder, H.; Lieb, K. Psychological interventions to foster resilience in healthcare students. Cochrane Database Syst. Rev. 2020, 7, CD013684. [Google Scholar] [CrossRef]
- Seo, C.; Corrado, M.; Fournier, K.; Bailey, T.; Haykal, K.A. Addressing the physician burnout epidemic with resilience curricula in medical education: A systematic review. BMC Med. Educ. 2021, 21, 80. [Google Scholar] [CrossRef]
- Dunn, L.; Iglewicz, A.; Moutier, C. A Conceptual Model of Medical Student Well-Being: Promoting Resilience and Preventing Burnout. Acad. Psychiatry 2008, 32, 44–53. [Google Scholar] [CrossRef]
- Baumgartner, P.J.N.; Schneider, P.T.R. A randomized controlled trial of mindfulness-based stress reduction on academic resilience and performance in college students. J. Am. Coll. Health 2021, 1–10. [Google Scholar] [CrossRef]
- Danaher, P.J.; Mullarkey, G.W. Factors Affecting Online Advertising Recall: A Study of Students. J. Advert. Res. 2003, 43, 252–267. [Google Scholar] [CrossRef]
- Boardman, L. Building resilience in nursing students: Implementing techniques to foster success. Int. J. Emerg. Ment. Health 2016, 18, 1–5. [Google Scholar] [CrossRef] [Green Version]
- General Pharmaceutical Council. Standards for the Initial Education and Training of Pharmacists 2021. Available online: https://www.pharmacyregulation.org/sites/default/files/document/standards-for-the-initial-education-and-training-of-pharmacists-january-2021_1.pdf (accessed on 28 May 2022).
- Kannangara, C.S.; Allen, R.E.; Carson, J.F.; Khan, S.Z.N.; Waugh, G.; Kandadi, K.R. Onwards and upwards: The development, piloting and validation of a new measure of academic tenacity- The Bolton Uni-Stride Scale (BUSS). PLoS ONE 2020, 15, e0235157. [Google Scholar] [CrossRef] [PubMed]
- Irish Institute of Pharmacy. The Resilient Pharmacist Podcast. Available online: https://iiop.ie/content/resilient-pharmacist-podcast (accessed on 28 May 2022).
| All | Male | Female | |
|---|---|---|---|
| Mean score | 68.01 | 70.39 | 67.18 |
| Standard deviation | 10.82 | 10.69 | 10.86 |
| Median score | 67 | 71 | 66 |
| Verbatim Questionnaire Statements from Section B, and in the Exact Order They Were Asked | SA * n (%) | A * n (%) | NAD * n (%) | D * n (%) | SD * n (%) | Interpolated Median |
|---|---|---|---|---|---|---|
| 49 (62.03) | 30 (37.97) | 0 (0.00) | 0 (0.00) | 0 (0.00) | 4.69 |
| 36 (45.57) | 38 (48.10) | 3 (3.80) | 1 (1.27) | 1 (1.27) | 4.41 |
| 33 (41.77) | 34 (43.04) | 7 (8.86) | 5 (6.33) | 0 (0.00) | 4.31 |
| 25 (31.65) | 38 (48.10) | 14 (17.72) | 2 (2.53) | 0 (0.00) | 4.12 |
| 22 (27.85) | 36 (45.57) | 14 (17.72) | 5 (6.33) | 2 (2.53) | 4.01 |
| 17 (21.52) | 40 (50.63) | 17 (21.52) | 3 (3.80) | 2 (2.5) | 3.94 |
| 29 (37.18) | 37 (47.44) | 10 (12.82) | 2 (2.56 | 0 (0.00) | 4.23 |
| 22 (27.85) | 33 (41.77) | 12 (15.20) | 10 (12.66) | 2 (2.53) | 3.97 |
| 18 (23.08) | 38 (48.72) | 13 (16.67) | 6 (7.70) | 3 (3.85) | 3.95 |
| 9 (11.39) | 22 (27.85) | 23 (29.11) | 9 (11.39) | 16 (20.25) | 3.13 |
| 23 (29.11) | 24 (30.38) | 23 (29.11) | 7 (8.86) | 2 (2.53) | 3.81 |
| 19 (24.05) | 46 (58.23) | 10 (12.66) | 4 (5.06) | 0 (0.00) | 4.05 |
| Theme | Respondent Quote (R = Respondent Number) |
|---|---|
| Goal setting and reflection | “One of the ways of establishing resilience was by establishing goals and keeping a diary for reflection.” (R66) |
| Having to take personal responsibility for developing resilience | “Not 100% sure the university prepares us for the stress/workload associated with being pharmacists. Speaking to pharmacists in work they say they’ve had to learn this themselves…” (R27) |
| Having a safe environment to learn/ the importance of formative assessments) | “I feel I would like to build resilience in an environment that isn’t assessed. This just adds pressure and I beat myself up afterwards, but if unassessed I commend myself on going and taking part.” (R3) |
| Realistic link to practice within teaching | “More IPL [interprofessional learning] realistic scenarios with other students would help build resilience.” (R14) |
| Health and well-being and the impact on resilience | “A health condition has reduced my level of resilience at times, both within and outside the MPharm degree. However, I still feel I am a hard worker and determined to keep going.” (R49) “COVID pandemic has definitely increased the need for the development of my resilience.”(R62) |
| Personal issues | “Issues at home and the amount of pressure I put on myself etc. provided me with more resilience than anything related to university.” (R25) |
| Other resilience-building aspects of the MPharm degree program | “I think extemporaneous dispensing in Level 2 of the MPharm degree really helped me to build resilience.” (R54) “Building resilience in MPharm started in Level 2 with extemporaneous dispensing.” (R69) |
| What resilience means | “In terms of resilience in pharmacy students, I feel like it is mostly about being able to balance everything you have on in uni, as well as other aspects of your life.” (R48) |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Hanna, L.-A.; Clerkin, S.; Hall, M.; Craig, R.; Hanna, A. The Resilience of Final-Year Pharmacy Students and Aspects of the Course They Found to Be Resilience-Building. Pharmacy 2022, 10, 84. https://doi.org/10.3390/pharmacy10040084
Hanna L-A, Clerkin S, Hall M, Craig R, Hanna A. The Resilience of Final-Year Pharmacy Students and Aspects of the Course They Found to Be Resilience-Building. Pharmacy. 2022; 10(4):84. https://doi.org/10.3390/pharmacy10040084
Chicago/Turabian StyleHanna, Lezley-Anne, Simone Clerkin, Maurice Hall, Rebecca Craig, and Alan Hanna. 2022. "The Resilience of Final-Year Pharmacy Students and Aspects of the Course They Found to Be Resilience-Building" Pharmacy 10, no. 4: 84. https://doi.org/10.3390/pharmacy10040084
APA StyleHanna, L.-A., Clerkin, S., Hall, M., Craig, R., & Hanna, A. (2022). The Resilience of Final-Year Pharmacy Students and Aspects of the Course They Found to Be Resilience-Building. Pharmacy, 10(4), 84. https://doi.org/10.3390/pharmacy10040084






