Information and Communication Technologies in Lung Transplantation: Perception of Patients and Medical Teams
Abstract
:1. Introduction
2. Materials and Methods
2.1. Study Design
2.2. Information and Communication Technologies
2.3. Evaluation of Preferences between ICTs
2.4. Statistical Analysis
3. Results
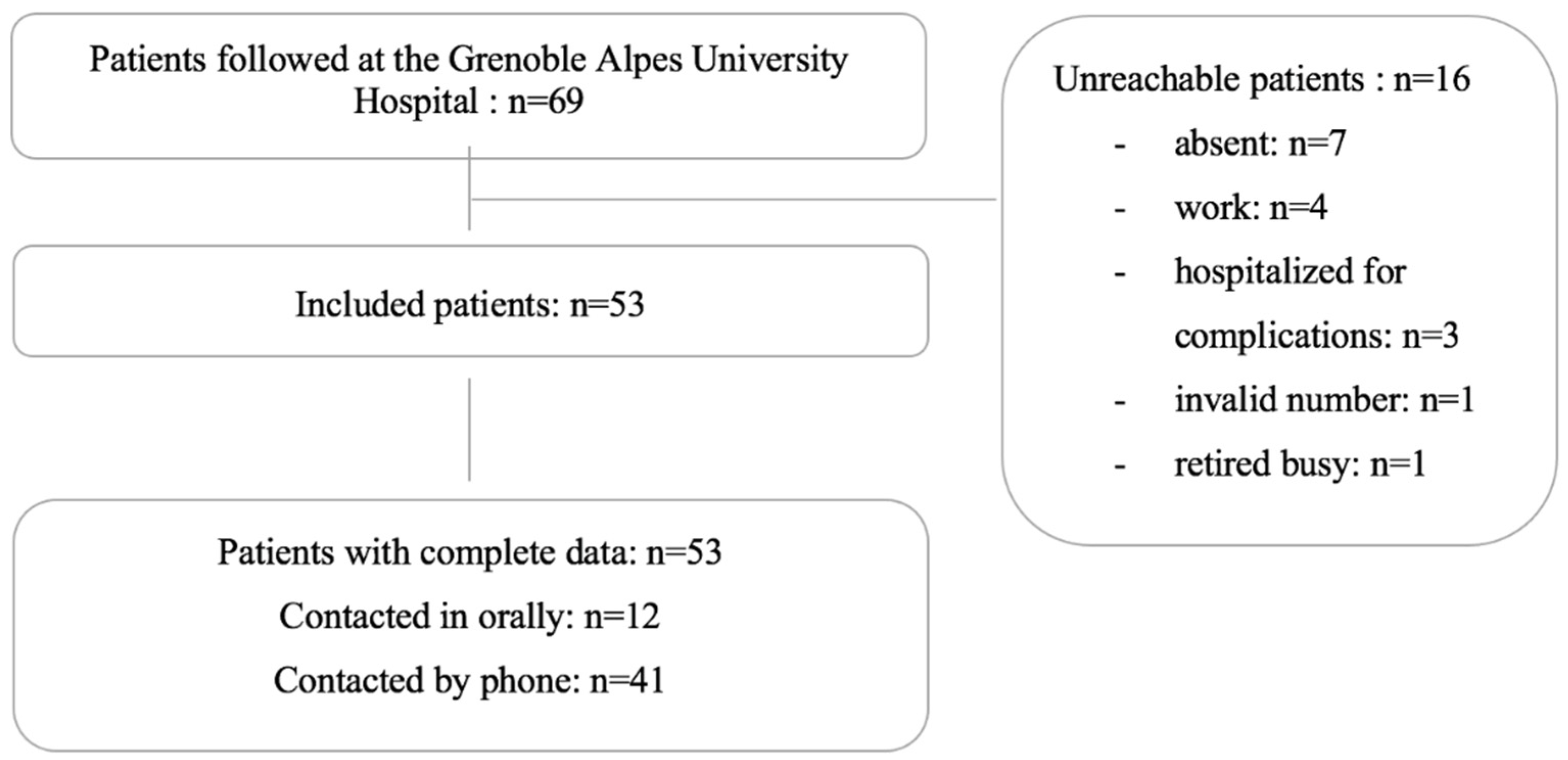
3.1. Patients
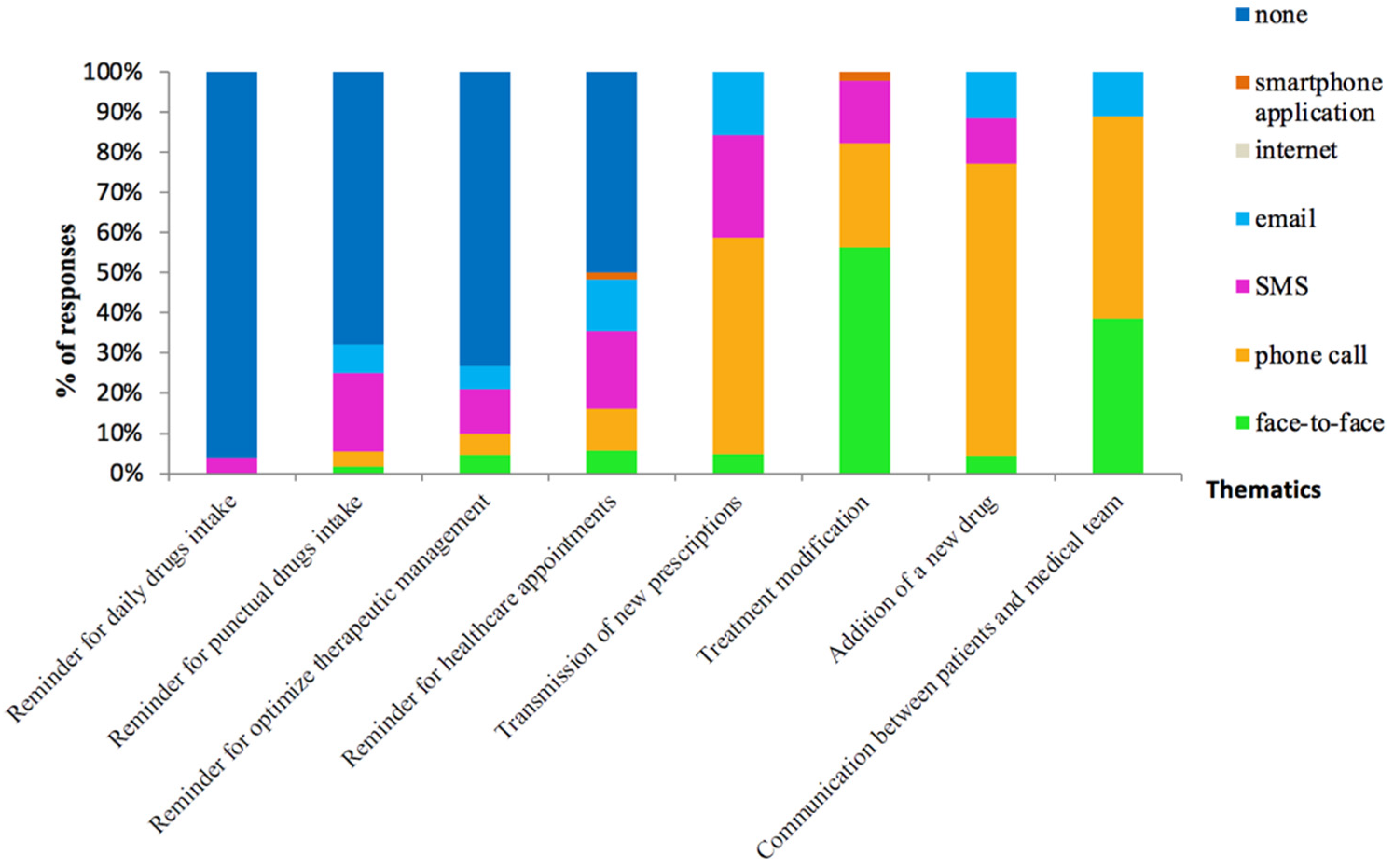
3.2. Patients’ Preferences about ICTs
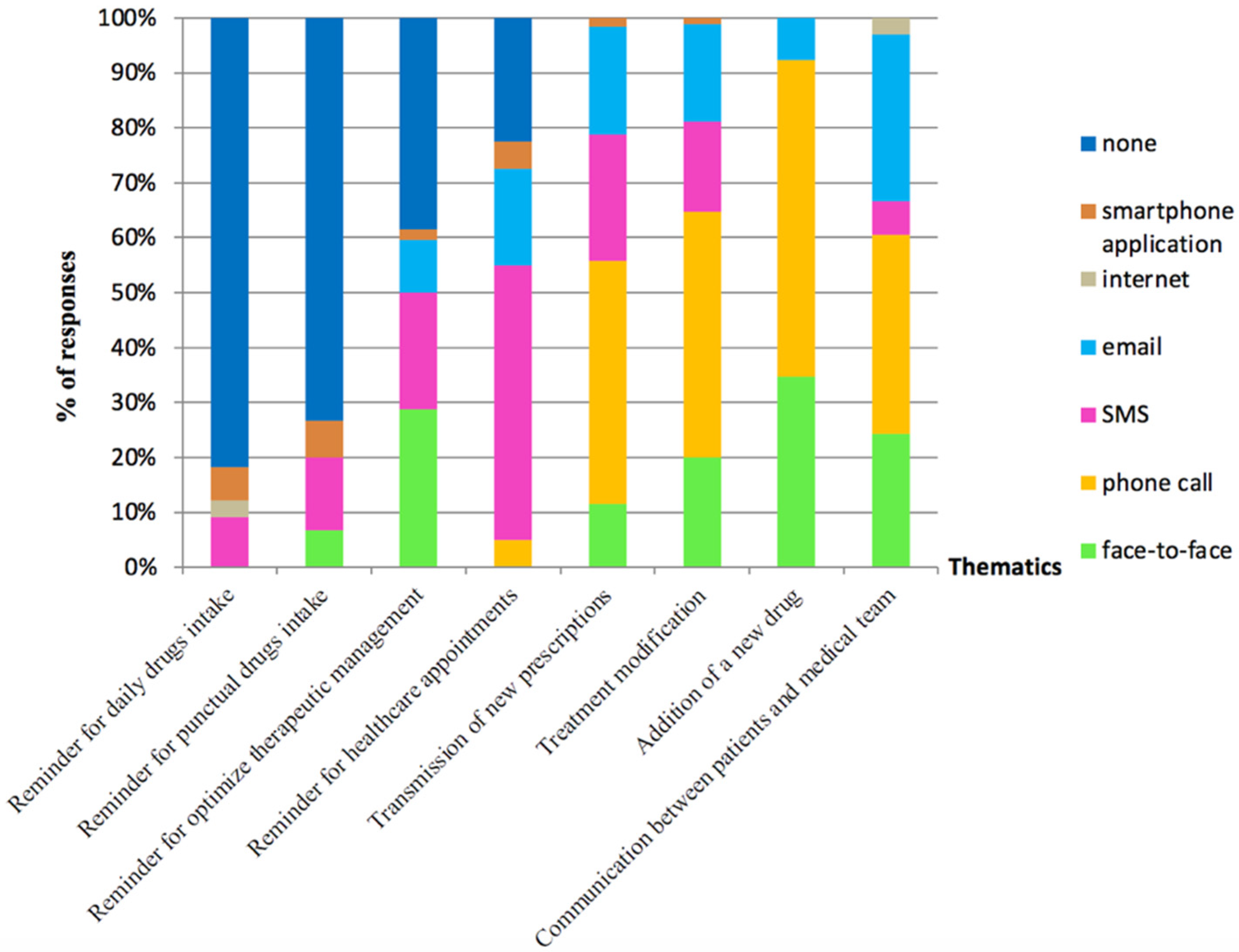
3.3. Healthcare Professionals’ Preferences about ICT in the Management and Monitoring of LT Patients
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Christie, J.D.; Edwards, L.B.; Kucheryavaya, A.Y.; Benden, C.; Dobbels, F.; Kirk, R. The Registry of the International Society for Heart and Lung Transplantation: Twenty-eighth Adult Lung and Heart-Lung Transplant Report. J. Heart Lung Transpl. 2011, 30, 1104–1122. [Google Scholar] [CrossRef] [PubMed]
- Agence de la Biomédecine. Greffe D’organes: Données Générales et Méthodes. 2017. Available online: http://www.agence-biomedecine.fr/annexes/bilan2017/donnees/organes/02-organes/synthese.htm (accessed on 29 June 2022).
- Quetant, S.; Rochat, T.; Pison, C. Results of lung transplantation. Rev. Mal. Respir. 2010, 27, 921–938. [Google Scholar] [PubMed]
- Alloway, R.R.; Dupuis, R.; Gabardi, S.; Kaiser, T.E.; Taber, D.J.; Tichy, E.M.; Weimert-Pilch, N.A.; on behalf of the American Society of Transplantation Transplant Pharmacy Community of Practice and the American College of Clinical Pharmacy Immunology/Transplantation Practice and Research Network. Evolution of the Role of the Transplant Pharmacist on the Multidisciplinary Transplant Team. Am. J. Transplant. 2011, 11, 1576–1583. [Google Scholar] [CrossRef] [PubMed]
- Allenet, B.; Baudrant, M.; Lehmann, A.; Gauchet, A.; Roustit, M.; Bedouch, P.; Golay, A. How can we evaluate medication adherence? What are the methods. Ann. Pharm. Fr. 2013, 71, 135–141. [Google Scholar] [CrossRef]
- De Geest, S.; Dobbels, F.; Fluri, C.; Paris, W.; Troosters, T. Adherence to the therapeutic regimen in heart, lung, and heart-lung transplant recipients. J. Cardiovasc. Nurs. 2005, 20, S88–S98. [Google Scholar] [CrossRef]
- Dew, M.A.; DiMartini, A.F.; Dabbs, A.D.V.; Myaskovsky, L.; Steel, J.; Unruh, M.; Switzer, G.E.; Zomak, R.; Kormos, R.L.; Greenhouse, J.B. Rates and Risk Factors for Nonadherence to the Medical Regimen After Adult Solid Organ Transplantation. Transplantation 2007, 83, 858–873. [Google Scholar] [CrossRef]
- Korb-Savoldelli, V.; Sabatier, B.; Gillaizeau, F.; Guillemain, R.; Prognon, P.; Bégué, D.; Durieux, P. Non-adherence with drug treatment after heart or lung transplantation in adults: A systematic review. Patient Educ. Couns. 2010, 81, 148–154. [Google Scholar] [CrossRef]
- Chisholm, M.A. Enhancing transplant patients’ adherence to medication therapy. Clin. Transpl. 2002, 16, 30–38. [Google Scholar] [CrossRef]
- Chisholm, M.A.; Vollenweider, L.J.; Mulloy, L.L.; Jagadeesan, M.; Wynn, J.J.; Rogers, H.E.; Wade, W.E.; DiPiro, J.T. Renal transplant patient compliance with free immunosuppressive medications. Transplantation 2000, 70, 1240–1244. [Google Scholar] [CrossRef]
- Edwards, S.S. The “noncompliant” transplant patient: A persistent ethical dilemma. J. Transpl. Coord. 1999, 9, 202–208. [Google Scholar]
- Greenstein, S.; Siegal, B. Odds probabilities of compliance and noncompliance in patients with a functioning renal transplant: A multicenter study. Transplant. Proc. 1999, 31, 280–281. [Google Scholar] [CrossRef]
- Berben, L.; Dobbels, F.; Kugler, C.; Russell, C.L.; De Geest, S. Interventions used by health care professionals to enhance medication adherence in transplant patients: A survey of current clinical practice. Prog Transpl. 2011, 21, 322–331. [Google Scholar] [CrossRef]
- Hussain, T.; Nassetta, K.; O’Dwyer, L.C.; Wilcox, J.E.; Badawy, S.M. Adherence to immunosuppression in adult heart trans-plant recipients: A systematic review. Transpl. Rev. 2021, 35, 100651. [Google Scholar] [CrossRef] [PubMed]
- De Bleser, L.; Dobbels, F.; Berben, L.; Vanhaecke, J.; Verleden, G.; Nevens, F.; De Geest, S. The spectrum of nonadherence with medication in heart, liver, and lung transplant patients assessed in various ways. Transpl. Int. 2011, 24, 882–891. [Google Scholar] [CrossRef]
- Dew, M.A.; DiMartini, A.F.; Dabbs, A.D.V.; Zomak, R.; De Geest, S.; Dobbels, F.; Myaskovsky, L.; Switzer, G.E.; Unruh, M.; Steel, J.L.; et al. Adherence to the Medical Regimen During the First Two Years After Lung Transplantation. Transplantation 2008, 85, 193–202. [Google Scholar] [CrossRef] [Green Version]
- Gordon, E.; Prohaska, T.; Gallant, M.; Siminoff, L. Adherence to Immunosuppression: A Prospective Diary Study. Transplant. Proc. 2007, 39, 3081–3085. [Google Scholar] [CrossRef] [Green Version]
- Russell, C.; Conn, V.; Ashbaugh, C.; Madsen, R.; Wakefield, M.; Webb, A.; Coffey, D.; Peace, L. Taking immunosuppressive medications effectively (TIMELink): A pilot randomized controlled trial in adult kidney transplant recipients. Clin. Transplant. 2010, 25, 864–870. [Google Scholar] [CrossRef] [Green Version]
- Vlaminck, H.; Maes, B.; Evers, G.; Verbeke, G.; Lerut, E.; Van Damme, B.; Vanrenterghem, Y. Prospective Study on Late Consequences of Subclinical Non-Compliance with Immunosuppressive Therapy in Renal Transplant Patients. Am. J. Transpl. 2004, 4, 1509–1513. [Google Scholar] [CrossRef]
- Murray, E.; Burns, J.; Tai, S.S.; Lai, R.; Nazareth, I. Interactive Health Communication Applications for people with chronic disease. Cochrane Database Syst. Rev. 2005, 4, CD004274. [Google Scholar] [CrossRef]
- Frøisland, D.H.; Årsand, E.; Skårderud, F.; Istepanian, R.; Cox, D.; Diehl, L. Improving Diabetes Care for Young People with Type 1 Diabetes Through Visual Learning on Mobile Phones: Mixed-Methods Study. J. Med. Internet Res. 2012, 14, e111. [Google Scholar] [CrossRef] [Green Version]
- Atherton, H.; Sawmynaden, P.; Meyer, B.; Car, J. Email for the coordination of healthcare appointments and attendance reminders. Cochrane Database Syst. Rev. 2012, 8, CD007981. [Google Scholar] [CrossRef] [PubMed]
- Gurol-Urganci, I.; De Jongh, T.; Vodopivec-Jamsek, V.; Atun, R.; Car, J. Mobile phone messaging reminders for attendance at healthcare appointments. Cochrane Database Syst. Rev. 2013, 12, CD007458. [Google Scholar] [CrossRef] [PubMed]
- Gomis-Pastor, M.; Perez, S.M.; Minguell, E.R.; Loidi, V.B.; Lopez, L.L.; Abarca, S.R.; Tugas, E.G.; Mas-Malagarriga, N.; Bafalluy, M.M. Mobile Health to Improve Adherence and Patient Experience in Heart Transplantation Recipients: The mHeart Trial. Healthcare 2021, 9, 463. [Google Scholar] [CrossRef] [PubMed]
- De Jongh, T.; Gurol-Urganci, I.; Vodopivec-Jamsek, V.; Car, J.; Atun, R. Mobile phone messaging for facilitating self-management of long-term illnesses. Cochrane Database Syst. Rev. 2012, 12, CD007459. [Google Scholar] [CrossRef]
- Gurol-Urganci, I.; De Jongh, T.; Vodopivec-Jamsek, V.; Car, J.; Atun, R. Mobile phone messaging for communicating results of medical investigations. Cochrane Database Syst. Rev. 2012, 6, CD007456. [Google Scholar] [CrossRef]
- Vodopivec-Jamsek, V.; de Jongh, T.; Gurol-Urganci, I.; Atun, R.; Car, J. Mobile phone messaging for preventive health care. Cochrane Database Syst. Rev. 2012, 12, CD007457. [Google Scholar] [CrossRef]
- Han, A.; Min, S. Ahn. Mobile medication manager application to improve adherence with immunosuppressive therapy in renal transplant recipients: A randomized controlled trial. PLoS ONE 2019, 14, e0224595. [Google Scholar] [CrossRef] [Green Version]
- Guldager, T.B.; Hyldgaard, C.; Hilberg, O.; Bendstrup, E. An E-Learning Program Improves Patients’ Knowledge After Lung Transplantation. Telemed. E.Health 2021, 27, 800–806. [Google Scholar] [CrossRef]
- Nieuwlaat, R.; Wilczynski, N.; Navarro, T.; Hobson, N.; Jeffery, R.; Keepanasseril, A. Interventions for enhancing medication adherence. Cochrane Database Syst. Rev. 2014, 11, CD000011. [Google Scholar] [CrossRef]
- Serper, M.; Ladner, D.P.; Curtis, L.M.; Nair, S.S.; Hur, S.I.; Kwasny, M.J.; Ho, B.; Friedewald, J.; Reese, P.P.; Abecassis, M.M.; et al. Transplant regimen adherence for kidney recipients by engaging information technologies (TAKE IT): Rationale and methods for a randomized controlled trial of a strategy to promote medication adherence among transplant recipients. Contemp. Clin. Trials 2021, 103, 106294. [Google Scholar] [CrossRef]
- Charpentier, G.; Benhamou, P.Y.; Dardari, D.; Clergeot, A.; Franc, S.; Schaepelynck-Belicar, P. The Diabeo software enabling individualized insulin dose adjustments combined with telemedicine support improves HbA1c in poorly controlled type 1 diabetic patients: A 6-month, randomized, open-label, parallel-group, multicenter trial (TeleDiab 1 Study). Diabetes Care 2011, 34, 533–539. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Lester, R.T.; Ritvo, P.; Mills, E.J.; Kariri, A.; Karanja, S.; Chung, M.H. Effects of a mobile phone short message service on an-tiretroviral treatment adherence in Kenya (WelTel Kenya1): A randomised trial. Lancet 2010, 376, 1838–1845. [Google Scholar] [CrossRef]
- Petrie, K.J.; Perry, K.; Broadbent, E.; Weinman, J.A. A text message programme designed to modify patients’ illness and treatment beliefs improves self-reported adherence to asthma preventer medication. Br. J. Health Psychol. 2011, 17, 74–84. [Google Scholar] [CrossRef] [PubMed]
- Sereika, S.M.; Dabbs, A.D.; Handler, S.M.; Schlenk, E.A.; Jiang, Y. Acceptance and Use of Mobile Technology for Health Self-Monitoring in Lung Transplant Recipients during the First Year Post-Transplantation. Appl. Clin. Inform. 2016, 7, 430–445. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Allenet, B.; Bedouch, P.; Bourget, S.; Baudrant, M.; Foroni, L.; Calop, J.; Bosson, J.-L. Physicians’ perception of CPOE implementation. Int. J. Clin. Pharm. 2011, 33, 656–664. [Google Scholar] [CrossRef] [PubMed]
- Blake, H. Innovation in practice: Mobile phone technology in patient care. Br. J. Community Nurs. 2008, 13, 160–165. [Google Scholar] [CrossRef]
- Miloh, T.; Annunziato, R.; Arnon, R.; Warshaw, J.; Parkar, S.; Suchy, F.J.; Iyer, K.; Kerkar, N. Improved Adherence and Outcomes for Pediatric Liver Transplant Recipients by Using Text Messaging. Pediatrics 2009, 124, e844–e850. [Google Scholar] [CrossRef] [Green Version]
- Pangarakis, S.J.; Harrington, K.; Lindquist, R.; Peden-McAlpine, C.; Finkelstein, S. Electronic feedback messages for home spirometry lung transplant recipients. Heart Lung 2008, 37, 299–307. [Google Scholar] [CrossRef] [Green Version]
| Characteristic | n | (%) | |
|---|---|---|---|
| Sex | Male | 33 | −62 |
| Age (years) | <40 | 15 | −28 |
| 40 ≤ Age ≤ 60 | 15 | −28 | |
| >60 | 23 | −43 | |
| Marital Status | Married | 26 | −49 |
| Single | 18 | −34 | |
| Divorced | 9 | −17 | |
| Occupational | Unemployed | 19 | −36 |
| Employed/Student | 16 | −30 | |
| Retired | 18 | −34 | |
| ICT accessibility | Possession of a mobile phone | 50 | −94 |
| Package to send free SMS | 37 | −70 | |
| Comfortable with SMS | 41 | −77 | |
| Internet access at home | 46 | −87 | |
| Comfortable with email | 35 | −66 | |
| Comfortable with internet | 39 | −74 | |
| Indication of LT | COPD/Emphysema/bronchiectasis | 28 | −53 |
| Cystic fibrosis | 14 | −26 | |
| Pulmonary fibrosis/PH | 11 | −21 | |
| Post-transplantation time | <1 year | 12 | −23 |
| ≥1 year | 41 | −77 | |
| Immunosuppressive therapy regimen | tacrolimus + MMF + corticosteroids | 26 | −49 |
| tacrolimus + MMF + everolimus + corticosteroids | 18 | −34 | |
| tacrolimus + AZA + corticosteroids | 3 | −6 | |
| tacrolimus + everolimus + corticosteroids | 3 | −6 | |
| tacrolimus + AZA + everolimus + corticosteroids | 1 | −2 | |
| tacrolimus + MMF + everolimus | 1 | −2 | |
| everolimus + corticosteroids | 1 | −2 | |
| Therapeutic Drug Monitoring | For 1 immunosuppressive drug | 30 | −57 |
| For 2 immunosuppressive drugs | 23 | −43 | |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Chanoine, S.; Roch, C.; Liaigre, L.; Roustit, M.; Genty, C.; Vitale, E.; Bosson, J.-L.; Pison, C.; Allenet, B.; Bedouch, P. Information and Communication Technologies in Lung Transplantation: Perception of Patients and Medical Teams. Pharmacy 2022, 10, 75. https://doi.org/10.3390/pharmacy10040075
Chanoine S, Roch C, Liaigre L, Roustit M, Genty C, Vitale E, Bosson J-L, Pison C, Allenet B, Bedouch P. Information and Communication Technologies in Lung Transplantation: Perception of Patients and Medical Teams. Pharmacy. 2022; 10(4):75. https://doi.org/10.3390/pharmacy10040075
Chicago/Turabian StyleChanoine, Sébastien, Christelle Roch, Léa Liaigre, Matthieu Roustit, Céline Genty, Elisa Vitale, Jean-Luc Bosson, Christophe Pison, Benoît Allenet, and Pierrick Bedouch. 2022. "Information and Communication Technologies in Lung Transplantation: Perception of Patients and Medical Teams" Pharmacy 10, no. 4: 75. https://doi.org/10.3390/pharmacy10040075
APA StyleChanoine, S., Roch, C., Liaigre, L., Roustit, M., Genty, C., Vitale, E., Bosson, J.-L., Pison, C., Allenet, B., & Bedouch, P. (2022). Information and Communication Technologies in Lung Transplantation: Perception of Patients and Medical Teams. Pharmacy, 10(4), 75. https://doi.org/10.3390/pharmacy10040075







