Self-Assessment of Cultural Competence and Social Determinants of Health within a First-Year Required Pharmacy Course
Abstract
:1. Introduction
2. Materials and Methods
3. Results
3.1. Demographics
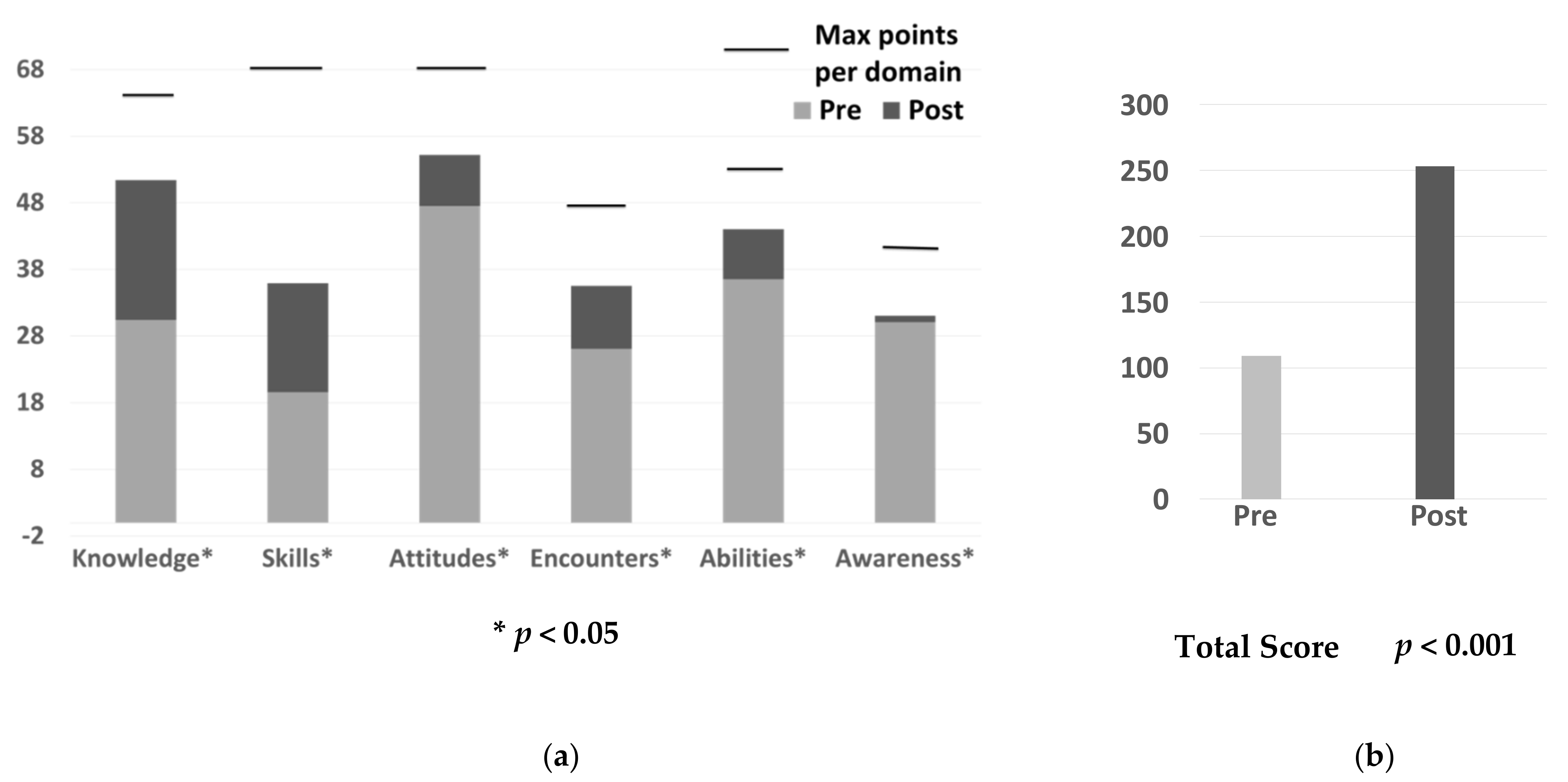
3.2. SAPLCC Domain, Factor, and Total Point Scores
3.3. Factors
3.4. Demographic Differences
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Appendix A. Course Culture and Social Determinants of Health Topics and Homework
| Class Title and Course Hours | Topics | Assessed in SAPLCC | Homework Assignment | Assessed in SAPLCC | Course Percent Points |
| Culture and cultural sensitivity 1.5 h | Culture definitions, race and ethnicity epidemiology, immigration and acculturation, health disparities | Knowledge—F2 Attitudes—F5 Abilities—F11 Aware—F14 | Self-assessment of cultural beliefs related to cause of illness, locus of control, sources of healing, privacy, right to know, family health care decision making, health care delivery, health disparities and culturally incompetent past health care experiences; beliefs from birth to death; and use of complementary health approaches | Awareness—F12, F13 | 3 |
| Culture and communications 1 h | Health literacy, interpreters, and bilingual patient education materials; complete the newest vital sign literacy test | Skills—F3 Attitudes—F6 Encounters—F8 | Either interview an interpreter or find and evaluate a bilingual medication education piece | Skills F3 1 or Encounters 1—F8 | 3 |
| Culture and bioethics 1 h | Documentary about conflict between Native American parents and pediatric surgeon about a transplant for their newborn child family does not wish; small group discussion | Knowledge—F1 Skills—F4 Abilities—F7, F11 Attitudes—F7 Encounters—F8 Awareness—F13 | None | 0 | |
| Culture, biases and models 1 h | Definitions of stereotypes, generalizations, and biases; cultural competence development models; cultural humility; intersectionality; and religion, race and ethnic generalized cultural beliefs about health care, communications and decision making; modified Trading Places exercise, case discussion about health care professionals’ cultural competencies | Abilities—F7, F11 Awareness—F12, F13, F14 | None | 0 | |
| Culture and practice 1 h | Cultural possibilities and encounters; cultural competence continuum model, 4 Cs (call, cause, cope, concerns), seven domains of cultural competent practice | Skills—F3 Encounters—F8 Abilities—F10, F11 Awareness—F13 | None | 0 | |
| Culture and insurance 0.25 h | Income, poverty and insurance by race and ethnic groups | Attitudes—F6 | None | 0 | |
| Culture and medicine presentation 1 h outside of class | Attend and write a reflection about a culture and health presentation sponsored by one of two student pharmacist organizations—this year’s topics related to mental health and culture and systemic racism in health care systems | Knowledge 1—F1, F2 Awareness 1—F13 or Knowledge 1—F2 Attitudes 1—F5 Awareness 1—F13 | 3 | ||
| Complementary Health Approaches 2 h | Use by different populations, reasons for use, relationship to culture, complementary provider training, licensure, practice and outcomes, integrated models of care; Small group with three complementary health approaches presentations given by students. | Knowledge—F2 Encounters—F8 | Prepare a 20-min presentation on a complementary health approach with a classmate. | Knowledge—F2 Encounters—F8 | 10 |
| Social determinants of health (SDOH) 1 h | SDOH definition; various models including the social ecological model; SDOH model examples using alcoholism, diabetes, and stroke; Healthy People 2030 SDOH objectives; pharmacy SDOH assessment; small group activity with modified last straw SDOH game | Knowledge—F1, F2 Attitudes—F6 Encounters—F8 | None | 0 | |
| Social determinants of health for women, men, and older adults 1 h | Various SDOH issues for women, men, and older adults; small group activities to create social ecological models for a woman and older adult | Knowledge—F1, F2, F6 Abilities—F7 Awareness—F13 | None | 0 | |
| 1 Factors and domains covered depend on the homework assignment chosen and presentation attended by the student pharmacists. | |||||
Appendix B. Significantly Different SAPLCC Scores by Demographics
| Demographic1R | Gender | Race | Religion | |||
| Categories | Women, Men | White, Asian, Black | Christianity, Islam, Other | |||
| Time Frame | Pre | Post | Pre | Post | Pre | Post |
| pValues ≤ 0.05 | ||||||
| Knowledge domain Factor 2 | ||||||
| 0.050 | ||||||
| Skills domain Factor 3 | ||||||
| 0.033 | ||||||
| Attitudes domain | ||||||
| Factor 6 | 0.025 | |||||
| Encounters domain Factor 8 Factor 9 | ||||||
| 0.033 | ||||||
| 0.046 | ||||||
| Abilities domain Factor 11 | ||||||
| 0.037 | ||||||
| Awareness domain Factor 13 Factor 14 | 0.029 | |||||
| 0.047 | ||||||
| 0.020 | 0.015 | |||||
| 1R No differences pre and post for any scores for age, birth country and education prior to pharmacy school; no differences for knowledge, skills, attitudes, encounters, and abilities domain; no differences for factors 1, 4, 5, 7, 10, and 12 across any demographics. | ||||||
References
- Napier, D.; Depledge, M.H.; Knipper, M.; Lovell, R.; Ponarin, E.; Sanabria, E.; Thomas, F. Policy Brief No. 1. Culture Matters: Using a Cultural Contexts of Health Approach to Enhance Policy-Making. 2017, pp. 1–54. Available online: https://www.euro.who.int/__data/assets/pdf_file/0009/334269/14780_World-Health-Organisation_Context-of-Health_TEXT-AW-WEB.pdf (accessed on 8 November 2021).
- Healthy People 2030. Social Determinants of Health. Available online: https://health.gov/healthypeople/search?query=social+determinants+of+health (accessed on 8 November 2021).
- Gómez, C.A.; Kleinman, D.V.; Pronk, N.; Gordon, G.L.W.; Ochiai, E.; Blakey, C.; Johnson, A.; Brewer, K.H. Addressing Health Equity and Social Determinants of Health Through Healthy People 2030. J. Public Health Manag. Pract. 2021, 27 (Suppl. 6), S249–S257. [Google Scholar] [CrossRef] [PubMed]
- National Center of Cultural Competence, Georgetown University Center for Child and Human Development. Definitions of Cultural Competency. Available online: https://nccc.georgetown.edu/curricula/culturalcompetence.html (accessed on 8 November 2021).
- Rockich-Winston, N.; Wyatt, T.R. The case for culturally responsive teaching in pharmacy curriculums. Am. J. Pharm. Educ. 2019, 83, 7425. [Google Scholar] [CrossRef]
- World Health Organization. Social Determinants of Health. Available online: https://www.who.int/health-topics/social-determinants-of-health#tab=tab_1 (accessed on 8 November 2021).
- University of Wisconsin Population Health Institute. County Health Rankings Model. Available online: https://www.countyhealthrankings.org/explore-health-rankings/measures-data-sources/county-health-rankings-model (accessed on 8 November 2021).
- Accreditation Council for Pharmacy Education (ACPE). Accreditation Standards and Key Elements for the Professional Program in Pharmacy Leading to the Doctor of Pharmacy Degree, Chicago, Illinois: 2016. Available online: https://www.acpe-accredit.org/pdf/Standards2016FINAL.pdf (accessed on 8 November 2021).
- Medina, M.S.; Plaza, C.M.; Stowe, C.D.; Robinson, E.T.; DeLander, G.; Beck, D.E.; Melchert, R.; Supernaw, R.B.; Roche, V.F.; Gleason, B.L.; et al. Center for the Advancement of Pharmacy Education 2013 Educational Outcomes. Am. J. Pharm. Educ. 2013, 77, 162. [Google Scholar] [CrossRef] [Green Version]
- Pharmacy Council of New Zealand. Competence Standards for the Pharmacy Profession. Available online: https://pharmacycouncil.org.nz/wp-content/uploads/2021/04/CompStds2015Web.pdf (accessed on 6 December 2021).
- General Pharmaceutical Council. Standards for the Initial Education and Training of Pharmacists. Available online: https://www.pharmacyregulation.org/sites/default/files/document/standards-for-the-initial-education-and-training-of-pharmacists-january-2021_0.pdf (accessed on 6 December 2021).
- Arya, V.; Butler, L.; Leal, S.; Maine, L.; Alvarez, N.; Jackson, N.; Varkey, A.C. Systemic racism: Pharmacists’ role and responsibility. J. Am. Pharm. Assoc. 2020, 60, E43–E46. [Google Scholar] [CrossRef]
- Accreditation Council for Pharmacy Education. International Services Program. Available online: https://www.acpe-accredit.org/international-services-program/ (accessed on 6 December 2021).
- Chun, M.B.J.; Jackson, D.S. Scoping Review of Economical, Efficient, and Effective Cultural Competency Measures. Eval. Health Prof. 2020, 44, 279–292. [Google Scholar] [CrossRef] [PubMed]
- Lin, C.-J.; Lee, C.-K.; Huang, M.-C. Cultural Competence of Healthcare Providers: A Systematic Review of Assessment Instruments. J. Nurs. Res. 2017, 25, 174–186. [Google Scholar] [CrossRef] [PubMed]
- Echeverri, M.; Brookover, C.; Kennedy, K. Assessing pharmacy students’ self-perception of cultural competence. J. Health Care Poor Underserved 2013, 24, 64–92. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Echeverri, M.; Dise, T. Racial Dynamics and Cultural Competence Training in Medical and Pharmacy Education. J. Health Care Poor Underserved 2017, 28, 266–278. [Google Scholar] [CrossRef] [PubMed]
- Echeverri, M.; Unni, E.; Harpe, S.E.; Kavookjian, J.; Alkhateeb, F.; Ekong, G.; Law, A. A Multi-School Validation of a Revised Scale for Assessing Cultural Competence in Pharmacy Students. Am. J. Pharm. Educ. 2019, 83, 6602. [Google Scholar] [CrossRef] [PubMed]
- Echeverri, M.; Unni, E.; Harpe, S.E.; Kavookjian, J.; Alkhateeb, F.; Ekong, G.; Law, A. Identifying areas of improvement for cultural competence in pharmacy curricula: A multi-school study using the self-assessment of perceived level of cultural competence (SAPLCC) questionnaire. Curr. Pharm. Teach. Learn. 2021, 13, 1278–1287. [Google Scholar] [CrossRef] [PubMed]
- Carter, M.M.; Lewis, E.L.; Sbrocco, T.; Tanenbaum, R.; Oswald, J.C.; Sykora, W.; Williams, P.; Hill, L.D. Cultural competency training for third-year clerkship students: Effects of an interactive workshop on student attitudes. J. Natl. Med. Assoc. 2006, 98, 1772–1778. [Google Scholar] [PubMed]
- Doroudgar, S.; Dang, B.; Nguyen, H.; Matsumoto, R.R. Assessment of Cultural Competence in Pharmacy Students Prior to Advanced Pharmacy Practice Experiences. Am. J. Pharm. Educ. 2021, 85, 7928. [Google Scholar] [CrossRef] [PubMed]
- Okoro, O.; Odedina, F.; Smith, T. Determining the sufficiency of cultural competency instruction in pharmacy school curriculum. Am. J. Pharm. Educ. 2015, 79, 50. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Drame, I. The association between students’ emotional intelligence, cultural competency, and cultural awareness. Curr. Pharm. Teach. Learn. 2021, 13, 1146–1152. [Google Scholar] [CrossRef] [PubMed]
- Butler, L.; Chen, A.M.H.; Borja-Hart, N.; Arif, S.; Armbruster, A.L.; Petry, N.; Riley, A.C. Assessment of a multi-institutional integration of cultural competency activities. Curr. Pharm. Teach. Learn. 2020, 12, 517–523. [Google Scholar] [CrossRef] [PubMed]
- Chen, A.M.H.; Cailor, S.M.; Wicker, E.; Harper, N.G.; Franz, T.T.; Pahl, B. Integrating Health Literacy and Cultural Competency Concepts Across the Doctor of Pharmacy Curriculum. Am. J. Pharm. Educ. 2020, 84, ajpe7764. [Google Scholar] [CrossRef] [PubMed]
- Chen, A.M.H.; Armbruster, A.L.; Buckley, B.; Campbell, J.A.; Dang, D.K.; Devraj, R.; Drame, I.; Edwards, A.; Haack, S.L.; Ma, Q.; et al. Inclusion of Health Disparities, Cultural Competence, and Health Literacy Content in US and Canadian Pharmacy Curriculums. Am. J. Pharm. Educ. 2021, 85, 8200. [Google Scholar] [CrossRef] [PubMed]
- Robinson, K.; Drame, I.; Turner, M.R.; Brown, C. Antiracism teaching in pharmacy education: Developing the “upstreamist. ” Am. J. Pharm. Educ. 2021, 85, 8585. [Google Scholar] [CrossRef] [PubMed]
- Kiles, T.M.; Garey, K.W.; Wanat, M.A.; Pitman, P. A survey to assess experiences and social support of underrepresented minority doctor of pharmacy students. Curr. Pharm. Teach. Learn. 2021, 13, 245–254. [Google Scholar] [CrossRef] [PubMed]
| Category | Number, (%) |
|---|---|
| Gender Female Male | 58 (66.7) 29 (33.3) |
| Race White Asian Black/African American | 66 (75.9) 18 (20.7) 3 (3.4) |
| Ethnicity Arab American Hispanic/Latinx Neither | 32 (36.8) 1 (1.1) 54 (62.1) |
| Age (years) ≤24 25–29 ≥30 | 70 (83.3) 8 (9.5) 6 (7.1) |
| Education prior to pharmacy school High school diploma Associate degree Bachelor’s degree Master’s degree | 38 (43.7) 14 (16.1) 33 (37.9) 2 (2.3) |
| Religion/spirituality Christianity Islam Agnosticism Atheism Buddhism Hinduism Sikhism Spiritual | 46 (53.5) 29 (33.7) 4 (4.7) 3 (3.5) 1 (1.2) 1 (1.2) 1 (1.1) 1 (1.1) |
| Birth country and current residence Born United States, live in Michigan Born Canada, live in Michigan Born Canada, live in Canada Born another country, live in Michigan Born another country, live in Canada | 57 (65.1) 2 (2.3) 3 (3.5) 24 (27.9) 1 (1.2) |
| Domains and Factors | Number of Survey Items | Maximum Points | Factor Titles | Pre Point Score Mean ± SD | Percent of Maximum Points at Baseline | Points Change 1 After Course Mean ± SD |
|---|---|---|---|---|---|---|
| Knowledge domain | 16 | 64 | 30.4 ± 8.2 | 47.5 | 21.0 ± 9.5 | |
| Factor 1 | 7 | 28 | Addressing Population Health Issues | 13.7 ± 3.9 | 48.9 | 8.6 ± 4.7 |
| Factor 2 | 9 | 36 | Understanding the Context of Care | 16.7 ± 4.8 | 46.4 | 12.4 ±6.0 |
| Skills domain | 11 | 44 | 19.6 ± 7.1 | 44.5 | 16.3 ± 8.6 | |
| Factor 3 | 7 | 28 | Providing Culturally Competent Services | 12.3 ± 4.5 | 43.9 | 10.3 ± 5.6 |
| Factor 4 | 4 | 16 | Dealing with Cross-Cultural Conflicts | 7.2 ± 2.8 | 45.0 | 6.0 ± 3.4 |
| Abilities domain | 15 | 60 | 47.5 ± 7.2 | 79.2 | 7.7 ± 7.1 | |
| Factor 5 | 6 | 24 | Recognizing Disparities-Related Discrimination | 18.6 ± 4.4 | 77.5 | 3.1 ± 4.2 |
| Factor 6 | 5 | 20 | Recognizing Social Determinants of Health Improving | 16.8 ± 2.7 | 84.0 | 1.9 ± 2.9 |
| Factor 7 | 4 | 16 | Interpersonal/Intercultural Interactions | 14.0 ± 2.7 | 87.5 | 0.9 ± 2.4 |
| Encounters domain | 11 | 44 | 26.1 ± 7.6 | 59.3 | 9.4 ± 8.3 | |
| Factor 8 | 3 | 12 | Increasing Comfort During Cross-Cultural Encounters | 8.5 ± 2.3 | 70.8 | 1.6 ± 2.3 |
| Factor 9 | 8 | 32 | Managing Cross-Cultural Communication Challenges | 17.5 ± 5.9 | 54.7 | 7.8 ± 6.7 |
| Abilities domain | 13 | 52 | 36.5 ± 7.9 | 70.2 | 7.5 ± 7.4 | |
| Factor 10 | 8 | 32 | Assessing Population Health Needs | 22.4 ± 5.5 | 70.0 | 4.3 ± 5.1 |
| Factor 11 | 5 | 20 | Applying Multicultural Knowledge | 14.1 ± 3.1 | 70.5 | 3.3 ± 3.3 |
| Awareness domain | 9 | 36 | 30.1 ± 4.3 | 83.6 | 0.9 ± 4.5 | |
| Factor 12 | 3 | 12 | Engaging in Self-Reflection | 10.6 ± 1.6 | 88.3 | −0.6 ± 2.4 |
| Factor 13 | 4 | 16 | Understanding Barriers to Health Care | 12.8 ± 2.3 | 80.0 | 0.0 ± 2.6 |
| Factor 14 | 2 | 8 | Confronting Racial Dynamics | 6.8 ± 1.4 | 85.0 | 0.4 ± 1.4 |
| Total score | 75 | 300 | 190.2 ± 29.3 | 63.4 | 62.9 ± 32.9 |
| Domains and Factors (Number of Items) | Normalized Score 1 Mean ± SD | Mean Change Scores 1 Mean ± SD | Median Score 2 | Percent Students 3 | Percent Students 3 | ||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Low Score <2 | Mod Score 2–3 | High Score >3 | Low Score <2 | Mod Score 2–3 | High Score >3 | ||||||
| Pre | Post | Pre | Post | Pre | Post | ||||||
| Knowledge domain Factor 1 (7) Factor 2 (9) | 1.9 ± 0.51 | 3.2 ± 0.47 | 1.3 ± 0.6 | 1.9 | 3.2 * | 63% | 34% | 3% | 1% | 42% | 57% |
| 2.0 ± 0.56 | 3.2 ± 0.58 | 1.2 ± 0.7 | 2.0 | 3.0 * | 39% | 58% | 3% | 1% | 54% | 45% | |
| 1.9 ± 0.54 | 3.2 ± 0.48 | 1.4 ± 0.7 | 1.8 | 3.2 * | 63% | 34% | 3% | 1% | 40% | 59% | |
| Skills domain Factor 3 (7) Factor 4 (4) | 1.8 ± 0.64 | 3.6 ± 0.59 | 1.5 ± 0.8 | 1.7 | 3.3 * | 63% | 32% | 5% | 1% | 43% | 56% |
| 1.8 ± 0.64 | 3.2 ± 0.59 | 1.5 ± 0.8 | 1.6 | 3.3 * | 66% | 29% | 5% | 1% | 45% | 54% | |
| 1.8 ± 0.71 | 3.3 ± 0.65 | 1.5 ± 0.9 | 1.8 | 3.3 * | 51% | 46% | 3% | 1% | 47% | 52% | |
| Attitudes domain Factor 5 (6) Factor 6 (5) Factor 7 (4) | 3.2 ± 0.48 | 3.7 ± 0.39 | 0.5 ± 0.5 | 3.1 | 3.9 * | 1% | 39% | 60% | 1% | 11% | 88% |
| 3.1 ± 0.74 | 3.6 ± 0.48 | 0.5 ± 0.7 | 3.0 | 3.8 * | 6% | 50% | 44% | 1% | 23% | 76% | |
| 3.4 ± 0.55 | 3.7 ± 0.39 | 0.4 ± 0.6 | 3.4 | 4.0 * | 3% | 34% | 63% | 1% | 15% | 84% | |
| 3.5 ± 0.67 | 3.7 ± 0.49 | 0.2 ± 0.6 | 4.0 | 4.0 * | 1% | 34% | 65% | 1% | 16% | 83% | |
| Encounters domain Factor 8 (3) Factor 9 (8) | 2.4 ± 0.69 | 3.2 ± 0.59 | 0.9 ± 0.8 | 2.2 | 3.2 * | 29% | 55% | 16% | 1% | 43% | 56% |
| 2.8 ± 0.76 | 3.4 ± 0.56 | 0.5 ± 0.8 | 3.0 | 3.3 * | 13% | 57% | 30% | 2% | 43% | 55% | |
| 2.2 ± 0.74 | 3.2 ± 0.64 | 1.0 ± 0.8 | 2.0 | 3.1 * | 40% | 49% | 11% | 3% | 46% | 51% | |
| Abilities domain Factor 10 (8) Factor 11 (5) | 2.8 ± 0.61 | 3.4 ± 0.43 | 0.6 ± 0.6 | 2.8 | 3.3 * | 6% | 68% | 26% | 1% | 35% | 64% |
| 2.8 ± 0.68 | 3.3 ± 0.47 | 0.5 ± 0.6 | 2.9 | 3.1 * | 5% | 73% | 22% | 1% | 47% | 52% | |
| 2.8 ± 0.61 | 3.5 ± 0.47 | 0.7 ± 0.7 | 2.8 | 3.4 * | 5% | 74% | 21% | 1% | 40% | 59% | |
| Awareness domain Factor 12 (3) Factor 13 (4) Factor 14 (2) | 3.3 ± 0.47 | 3.5 ± 0.37 | 0.1 ± 0.5 | 3.3 | 3.6 * | 1% | 25% | 74% | 1% | 16% | 83% |
| 3.5 ± 0.54 | 3.3 ± 0.56 | -0.2 ± 0.8 | 3.7 | 3.3 * | 2% | 35% | 63% | 3% | 36% | 61% | |
| 3.2 ± 0.58 | 3.2 ± 0.39 | 0.7 ± 0.7 | 3.0 | 3.5 | 1% | 55% | 44% | 1% | 36% | 63% | |
| 3.4 ± 0.71 | 3.6 ± 0.56 | 0.2 ± 0.7 | 3.5 | 4.0 * | 2% | 37% | 61% | 1% | 27% | 72% | |
| Total score (75) | 2.5 ± 0.39 | 3.4 ± 0.36 | 0.8 ± 0.4 | .2.5 | 3.4 * | 5% | 87% | 8% | 1% | 17% | 82% |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kucherepa, U.; O’Connell, M.B. Self-Assessment of Cultural Competence and Social Determinants of Health within a First-Year Required Pharmacy Course. Pharmacy 2022, 10, 6. https://doi.org/10.3390/pharmacy10010006
Kucherepa U, O’Connell MB. Self-Assessment of Cultural Competence and Social Determinants of Health within a First-Year Required Pharmacy Course. Pharmacy. 2022; 10(1):6. https://doi.org/10.3390/pharmacy10010006
Chicago/Turabian StyleKucherepa, Ulyana, and Mary Beth O’Connell. 2022. "Self-Assessment of Cultural Competence and Social Determinants of Health within a First-Year Required Pharmacy Course" Pharmacy 10, no. 1: 6. https://doi.org/10.3390/pharmacy10010006
APA StyleKucherepa, U., & O’Connell, M. B. (2022). Self-Assessment of Cultural Competence and Social Determinants of Health within a First-Year Required Pharmacy Course. Pharmacy, 10(1), 6. https://doi.org/10.3390/pharmacy10010006






