Abstract
Levonorgestrel emergency contraception and other contraceptive methods are available over-the-counter (OTC); however youth continue to face a number of barriers in accessing healthcare services, including lack of knowledge of the method, fear of loss of privacy, difficulties in finding a provider, and cost. A descriptive, nonexperimental, cross-sectional study of a sample of 112 community pharmacies in San Diego, California was conducted between December 2009 and January 2010 to assess community pharmacy practices related to the availability and accessibility of family planning health pharmacy services and products, particularly to youth. A majority (n = 79/112, 70.5%) of the pharmacies carried a wide selection of male condoms; however, the other OTC nonhormonal contraceptive products were either not available or available with limited selection. A majority of the pharmacies sold emergency contraception (n = 88/111, 78.6%). Most patient counseling areas consisted of either a public or a semi-private area. A majority of the pharmacy sites did not provide materials or services targeting youth. Significant gaps exist in providing family planning products and services in the majority of community pharmacies in San Diego, California. Education and outreach efforts are needed to promote provision of products and services, particularly to the adolescent population.
1. Introduction
Each year, nearly 4% of teenagers in the United States give birth, which accounts for 10% of total births and costs taxpayers over nine billion dollars [1,2]. The teen birth rate in California (3.5%) is slightly lower than the national average and substantially lower than other states with comparable demographics, due to investments in teen pregnancy prevention. However, California experiences the largest number of teen pregnancies due to its large teen population, resulting in 51,704 babies born to teen mothers in California in 2008 [2,3]. For this reason, continued progress remains critical in preventing teen pregnancies, since over 80% are unintended [4]. According to 2002 data, one-third of teens receive no formal instruction about contraception, so the responsibility falls in part on health care providers to educate teens more comprehensively [5]. Pharmacists are visible, accessible professional members of the health care team [6]. Therefore, pharmacists have the opportunity to play an important role in providing health care access for youth. During focus group sessions in 2006, California youth identified flexible hours, confidentiality, and in-store privacy as priorities for pharmacies to serve and retain teens as clients [7].
Pharmacies became an increasingly useful access point of care for older teens when the United States Food and Drug Administration approved levonorgestrel (Plan B—Teva) as an over-the-counter (OTC) emergency contraception (EC) for adults age 18 or older in 2006. Since that time, the age restriction was lowered to consumers age 17 or older in 2009 for all levonorgestrel EC products. Most recently, the age restriction was removed for the brand levonorgestrel 1.5 mg (Plan B One-Step—Teva) in 2013. In addition to consumers accessing EC OTC, pharmacist prescribing of EC remains critical for those women who want to use insurance to help pay for the product or those who do not have acceptable identification. California is one of nine states that allow pharmacists to complete a one-hour continuing education program in order to become EC-certified and provide EC directly to women of any age without an advance prescription [6]. This may present a challenge to many pharmacy professionals since many feel inadequately trained in adolescent-specific issues. According to a survey study of pharmacists in Indiana, only 13% agreed that they had been well trained in adolescent-specific issues, 7% agreed that they had been well trained in adolescent consent issues, and 23% agreed that they had been well trained in adolescent confidentiality issues [6]. Moreover, there is a lack of consumer awareness as to which pharmacies participate in direct pharmacy access to EC [8].
The objective of this study was to assess community pharmacy practices related to the availability and accessibility of family planning pharmacy services and products, particularly to youth, in San Diego, California.
2. Methods
A current list of licensed pharmacies in the County of San Diego was generated on 22 September 2009 via the California Board of Pharmacy public-access website, which had last been updated on 21 September 2009. Pharmacies with canceled or revoked licenses, those located outside of the City of San Diego, and those that were not community or retail pharmacies (e.g., home health, nuclear pharmacy) were excluded, resulting in 172 pharmacies in our target population. The pharmacies were randomized using a random number generator tool to create a convenience sample of 120 community pharmacies in the City of San Diego for inclusion in the study.
These pharmacies were each visited one time between December 2009 and January 2010, on varying days and times, by one of four pharmacy student investigators. The Agency for Healthcare Research and Quality’s (AHRQ) Pharmacy Health Literacy Assessment Tool Part I: Assessment Tour of the Pharmacy was loosely adapted to create the family planning health services pharmacy assessment tool [9]. The elements included in the assessment tool were agreed upon by the investigators upon consultation by family planning experts from the California-based not-for-profit organization Pharmacy Access Partnership. The student pharmacists used this adapted assessment tool to guide their observations of the family planning products available on OTC shelves, pharmacy promotional and educational materials, and pharmacist counseling area. Pharmacists on duty at the time of the visit were asked yes-no questions about their interest in becoming EC-certified and their interest in participating in a one-hour training and continuing education program regarding pharmacy services for adolescents being offered locally through Pharmacy Access Partnership’s Youth-Friendly Pharmacy Initiative. At this time, investigators defined EC-certification, educated pharmacy staff members about direct pharmacy access to EC, and provided pharmacy staff with informational materials.
This study was approved by the University of California San Diego Human Research Protections Program institutional review board.
3. Results
Of the 120 pharmacies visited, 112 visits were successful. Unsuccessful visits included pharmacies that were closed for unknown reasons or were not appropriately excluded before randomizing the sample due to lack of information. Pharmacy characteristics varied among hours of operation, pharmacy types, prescription volume, and are summarized in Table 1.
A majority of the pharmacy sites did not carry materials such as pamphlets, magazines, or marketing aimed at youth. Most pharmacies did not carry signs in front of the store (16.1% (n = 18)) or provide health-related pamphlets, or magazines for youth in the pharmacy waiting area (8.9% (n = 10)).
Availability of family planning products is summarized in Figure 1. More than 80% of the pharmacies had OTC family planning products stored in locked cases requiring a staff member to unlock the case for access to the products, contrasted with placing the products on open shelves accessible to the consumer without staff assistance. Of the 88 pharmacies (79.2%) selling EC, it was determined that 47 pharmacies (42.3%) sold only one EC product and 41 pharmacies (36.9%) sold more than one EC product. The average price of EC ranged from approximately $40 for the generic product to $48 for the brand products; levonorgestrel (Next Choice—Watson Pharma, Inc., Corona, CA, USA) $39.83, levonorgestrel (Plan B—Duramed Pharmaceuticals, Inc., Pomona, NY, USA) $47.51, levonorgestrel (Plan B One Step—Duramed Pharmaceuticals, Inc., Pomona, NY, USA) $47.58. Availability of services and products was found to vary by selected pharmacy characteristics, such as pharmacy type and prescription volume, as presented in Table 2.
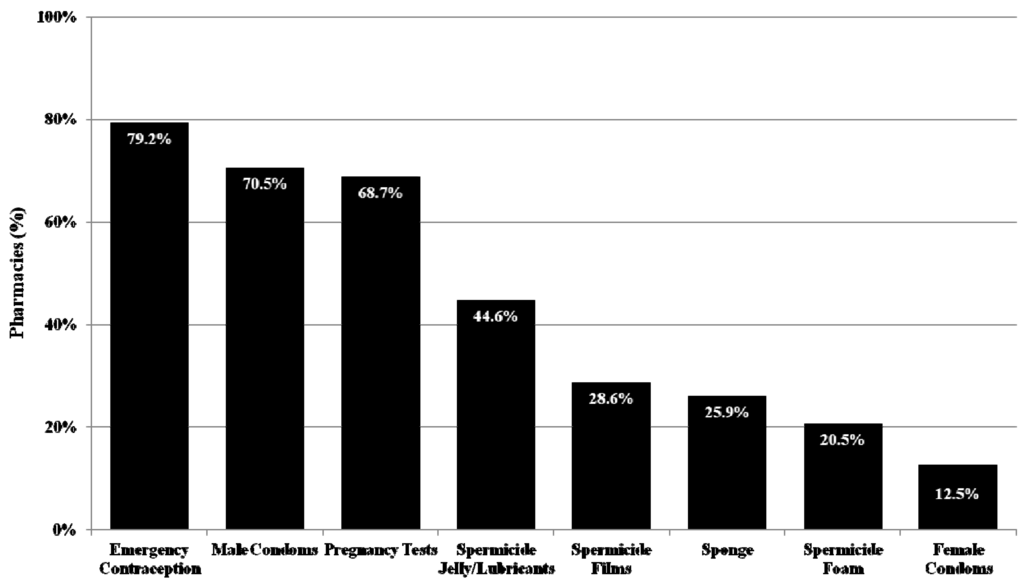
Figure 1.
Availability of family planning products in pharmacies (n = 112).

Table 1.
Characteristics of pharmacies (n = 112).
| Pharmacy Characteristic | n (%) |
|---|---|
| Hours of operation | |
| Open 24 h | 9 (8.0%) |
| Open weekend and evening | 65 (58.0%) |
| Pharmacy type | |
| Chain | 68 (60.7%) |
| Independent | 29 (26.0%) |
| Clinic-/Hospital-based | 15 (13.4%) |
| Weekly prescription volume | |
| <500 | 11 (10.9%) |
| 500–1,000 | 30 (29.7%) |
| 1,001–1,500 | 24 (23.7%) |
| 1,501–2,000 | 13 (12.9%) |
| >2,000 | 23 (22.8%) |
| Patient counseling area | |
| Public area | 54 (48.2%) |
| Semi-private area | 52 (46.4%) |
| Private area | 6 (5.4%) |
| Availability of materials targeting youth | |
| Front of the store | 18 (16.1%) |
| Pharmacy waiting area | 10 (8.9%) |
| Ability to flag minor’s prescription for confidentiality | |
| Flags prescription | 11 (10.2%) |

Table 2.
Availability of family planning services and products by pharmacy characteristics.
| Product or Service | Chain (n = 68) | Independent, Clinic-/Hospital-Based (n = 44) | High Weekly Prescription Volume (≥1,250, n = 50) | Low Weekly Prescription Volume (<1,250, n = 51) |
|---|---|---|---|---|
| Male condoms | 67 (98.5%) | 12 (27.3%) | 45 (90.0%) | 27 (52.9%) |
| Emergency contraception | 65 (95.6%) | 23 (52.3%) | 44 (88.0%) | 23 (45.1%) |
| Semi-/private counseling area | 40 (58.8%) | 18 (40.9%) | 28 (56.0%) | 14 (27.5%) |
Only 9 pharmacies (8.1%) employed at least one EC-certified pharmacist and these pharmacies were more likely to sell EC (89.0% of pharmacies with an EC-certified pharmacist vs. 77.7% of pharmacies without an EC-certified pharmacist). Pharmacists from a total of 8 (7.1%) pharmacy sites showed an interest in becoming EC-certified. Pharmacists or ancillary pharmacy staff (i.e., technicians) from 10 (8.9%) pharmacy sites showed an interest in participating in a one-hour training program to learn about providing pharmacy services to youth.
4. Discussion
This study is the first to assess community pharmacy practices related to the availability and accessibility of family planning pharmacy services and products, particularly for youth. Despite OTC availability of levonorgestrel EC and other contraceptive methods, youth continue to face a number of barriers in accessing healthcare services, including lack of knowledge of the method, fear of loss of privacy, difficulties in finding a provider, and cost [8,10]. Pharmacies are well positioned with our communities to address these barriers and facilitate timely access to family planning products and services for youth.
A 2004 California study revealed that teens younger than 16 took 27 h longer to seek EC at pharmacies with EC-certified pharmacists than women aged 30 or older [8]. This disparity may be reduced with pharmacies promoting availability of EC and other family products, as well as ensuring accessibility with extended hours of operation and storing these products on open shelves versus keeping them in locked cases. Additionally, younger teens may particularly benefit from EC-certified pharmacists prescribing EC so that the prescription can be processed under insurance to minimize out-of-pocket costs to the patient. Only a small fraction of pharmacies assessed in this study had an EC-certified pharmacist whereas 42% of pharmacists in California responding to a 2007 survey indicated they are EC-certified [11]. In the literature, interest in prescribing EC is high, but may not translate to practice due to barriers cited, such as time and lack of incentive to participate [11,12]. On the other hand, most pharmacies assessed in this study did sell EC (79.2%) compared to lower rates in a 2007 study in North Carolina (60.7%) [13]. It is unknown whether this increase is a result of changes in the OTC age restriction for the EC products, increasing demand over time, or a regional variation.
This study did have limitations. As the first study of its kind, there was no existing tool to employ for the study and no data to compare our findings against. The other parts of the AHRQ tool were not adapted for use in this study, thus we were unable to assess the perspectives of both patients and staff. Further, the tool did not assess language services available at pharmacies, which has been found to be a barrier for Spanish-speaking adolescents in California [14]. Each pharmacy was visited only one time by a single investigator, which is a deviation from the AHRQ’s recommendation since it does not allow for comparison of assessments. In addition, a majority of the interviews were performed in chain pharmacies and some of the pharmacists working in these pharmacies felt strongly about not sharing information that they felt was proprietary or confidential (e.g., weekly prescription volume). Corporate rules could have also affected the ability of their pharmacists to provide direct pharmacy access to EC or to market and advertise beyond corporate standards, but this was not assessed. Finally, the pharmacist questioned may not have been fully aware of whether or not her/his pharmacist colleagues are EC-certified.
Recommendations that can be made to community pharmacies based on these preliminary findings include implementing policies and procedures to maintain minors’ confidentiality, encouraging and supporting EC-certification for pharmacist employees, and raising community awareness of the pharmacy location, hours, and services. Future studies are warranted and should involve youth to better understand their attitudes toward healthcare services and providers, as well as pharmacists to determine widely acceptable improvements in providing services to youth in pharmacies.
5. Conclusions
While pharmacies often serve as a point of access for family planning products and services, this study demonstrates gaps in pharmacy practices. Pharmacies must respond to the identified opportunities to improve their practices, related to availability and accessibility of family planning products and services, particularly to youth.
Acknowledgments
These findings were previously presented as a poster abstract at the Reproductive Health Annual Clinical Meeting, Las Vegas, NV, 16–17 September 2011. There was no funding support for this work. The authors would like to acknowledge the contributions of staff from Pharmacy Access Partnership, which closed in February 2010.
Conflicts of Interest
The authors declare no conflict of interest.
References
- Centers for Disease Control and Prevention. CDC Vital Signs April 2011: Preventing Teen Pregnancy in the U.S. Available online: http://www.cdc.gov/vitalsigns/TeenPregnancy/?s_cid=vitalsigns_058/ (accessed on 18 June 2013).
- California Department of Public Health. Available online: http://www.cdph.ca.gov/Pages/NR10-014.aspx/ (accessed on 18 June 2013).
- Kost, K.; Henshaw, S. U.S. Teenage Pregnancies, Births and Abortions, 2008: State Trends by Age, Race and Ethnicity. Available online: http://www.guttmacher.org/pubs/USTPtrendsState08.pdf (accessed on 18 June 2013).
- Finer, L.B.; Zolna, M.R. Unintended pregnancy in the United States: Incidence and disparities, 2006. Contraception 2011, 84, 478–485. [Google Scholar] [CrossRef]
- Lindberg, L.D.; Santelli, J.S.; Singh, S. Changes in formal sex education: 1995–2002. Perspect. Sex. Reprod. Health 2006, 38, 182–189. [Google Scholar] [CrossRef]
- Conard, L.E.; Fortenberry, J.D.; Blythe, M.J.; Orr, D.P. Pharmacists’ attitudes toward and practices with adolescents. Arch. Pediatr. Adolesc. Med. 2003, 157, 361–365. [Google Scholar] [CrossRef]
- Nicole Monastersky Maderas. Personal communication, 1 March 2009.
- Foster, D.G.; Landau, S.C.; Monastersky, N.; Chung, F.; Kim, N.; Melton, M.; McGhee, B.T.; Stewart, F. Pharmacy access to emergency contraception in California. Perspect. Sex. Reprod. Health 2006, 38, 46–52. [Google Scholar] [CrossRef]
- Is our pharmacy meeting patients’ needs? A pharmacy health literacy assessment tool user’s guide. Available online: http://www.ahrq.gov/legacy/qual/pharmlit/pharmlit.pdf (accessed on 18 June 2013).
- Lindberg, C.E. Emergency contraception for prevention of adolescent pregnancy. MCN Am. J. Matern. Child Nurs. 2003, 28, 199–204. [Google Scholar] [CrossRef]
- Landau, S.; Besinque, K.; Chung, F.; Dries-Daffner, I.; Maderas, N.M.; McGhee, B.T.; Foster, D.G. Pharmacist interest in and attitudes toward direct pharmacy access to hormonal contraception in the United States. J. Am. Pharm. Assoc. 2009, 49, 43–50. [Google Scholar]
- Rafie, S.; El-Ibiary, S.Y. Student pharmacist perspectives on providing pharmacy-access hormonal contraception services. J. Am. Pharm. Assoc. 2011, 51, 762–765. [Google Scholar]
- McKoy, J.N. Access to Emergency Contraception in North Carolina Pharmacies. Available online: http://www.prochoicenc.org/assets/bin/pdfs/ecaccessfinal.pdf (accessed on 18 June 2013).
- Sampson, O.; Navarro, S.K.; Khan, A.; Hearst, N.; Raine, T.R.; Gold, M.; Miller, S.; de Bocanegra, H.T. Barriers to adolescents’ getting emergency contraception through pharmacy access in California: Differences by language and region. Perspect. Sex. Reprod. Health 2009, 41, 110–118. [Google Scholar] [CrossRef]
© 2013 by the authors; licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution license (http://creativecommons.org/licenses/by/3.0/).