The Association between Air Temperature and Mortality in Two Brazilian Health Regions
Abstract
1. Introduction
2. Materials and Methods
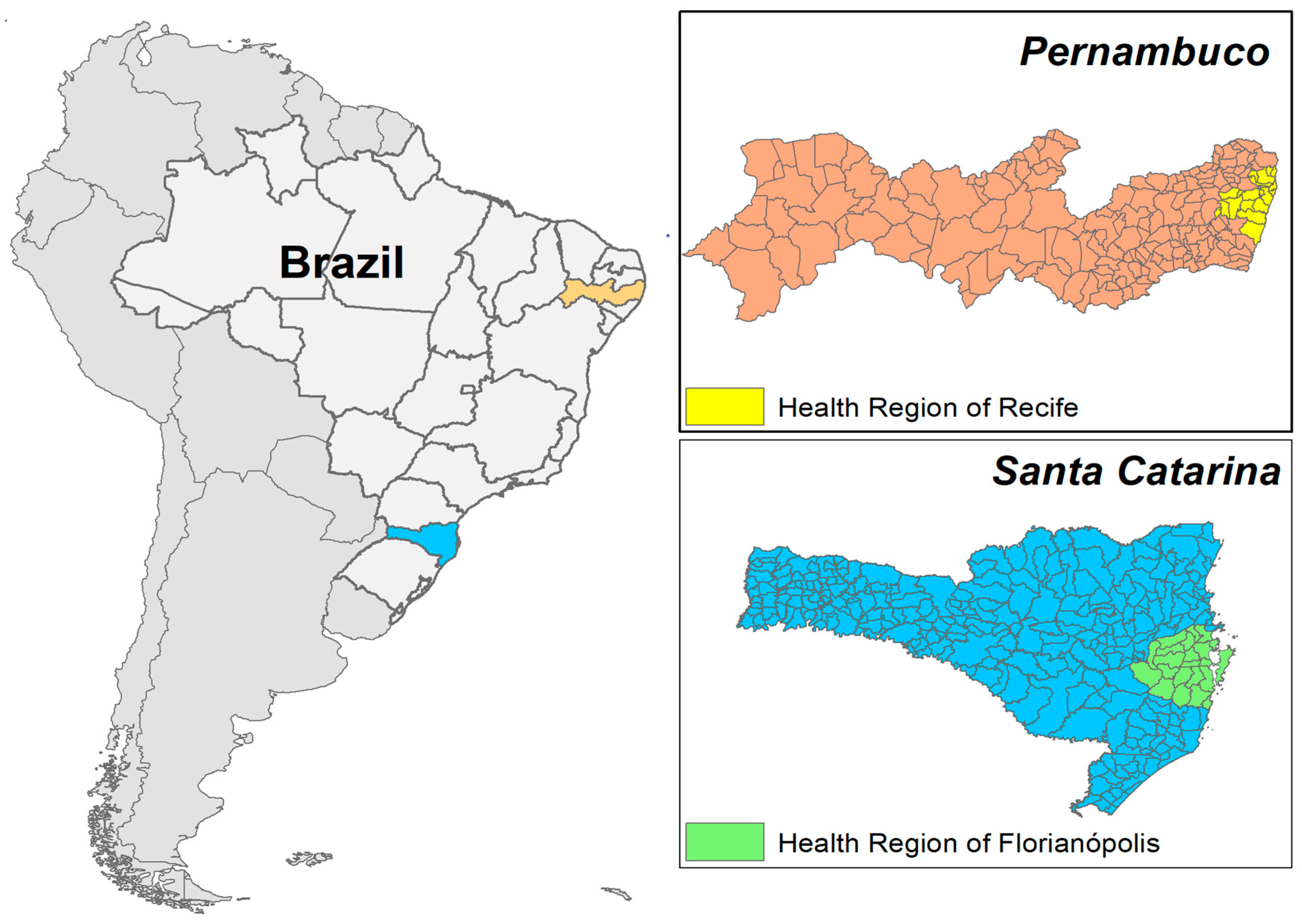
2.1. Case Study
2.2. Temperatures Data
2.3. Mortality Data
2.4. Statistical Analysis
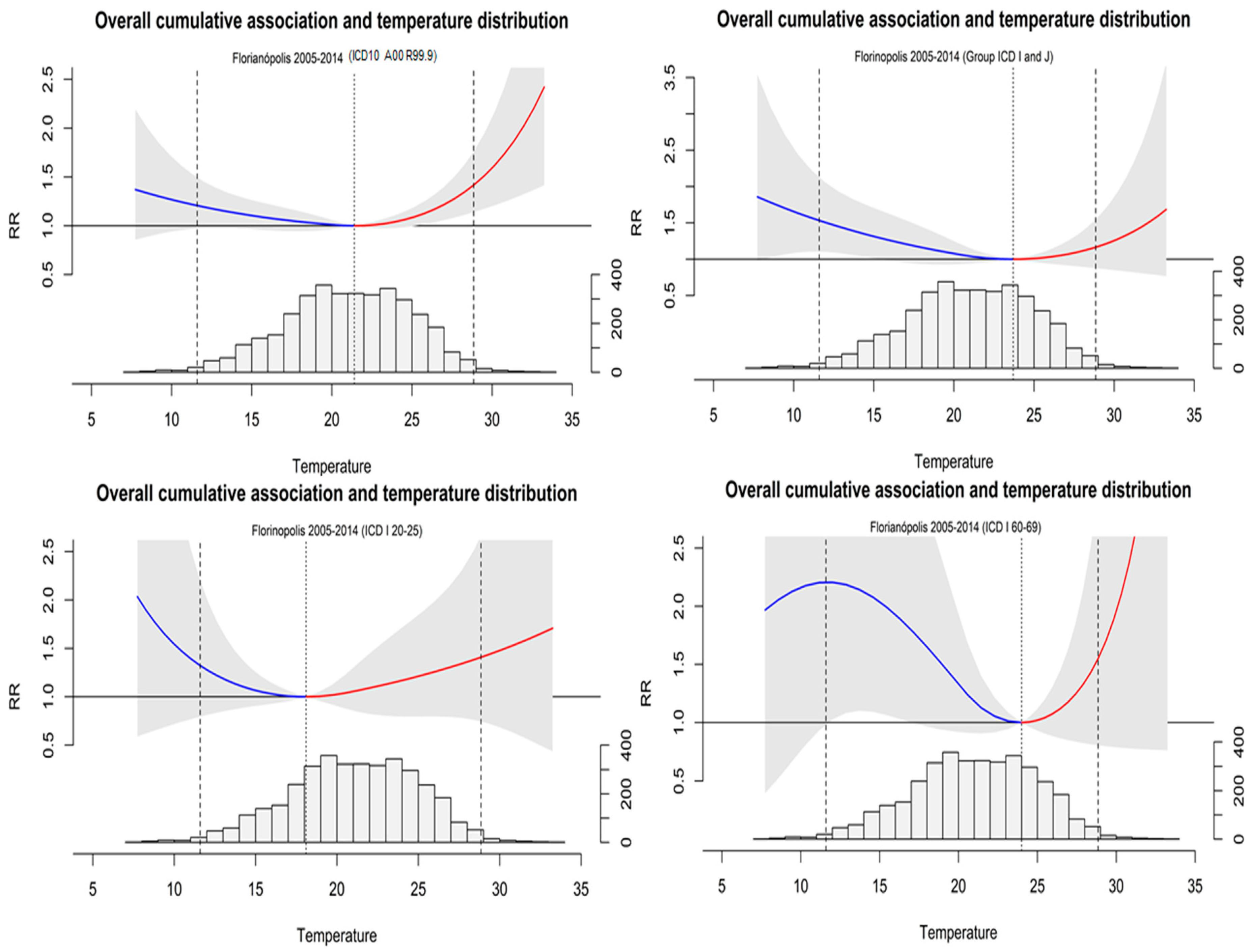
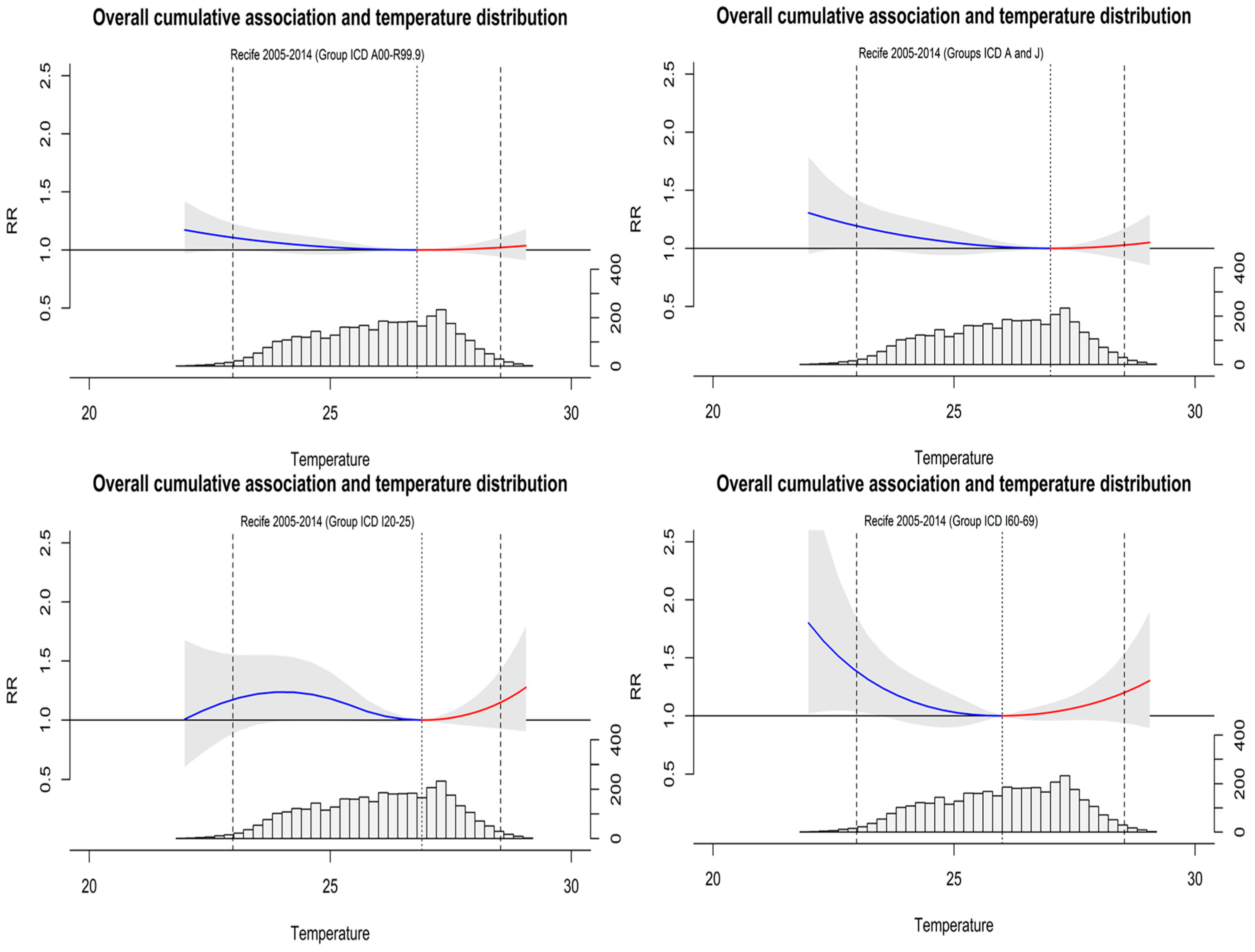
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Guo, Y.; Gasparrini, A.; Armstrong, B.; Li, S.; Tawatsupa, B.; Tobias, A.; Lavigne, E.; de Sousa Zanotti Stagliorio Coelho, M.; Leone, M.; Pan, X.; et al. Global variation in the effects of ambient temperature on mortality: A systematic evaluation. Epidemiology 2014, 25, 781–789. [Google Scholar] [CrossRef] [PubMed]
- Green, D.; Bambrick, H.; Tait, P.; Goldie, J.; Schultz, R.; Webb, L.; Alexander, L.; Pitman, A. Differential effects of temperature extremes on hospital admission rates for respiratory disease between indigenous and non-indigenous Australians in the Northern territory. Int. J. Environ. Res. Public Health 2015, 12, 15352–15365. [Google Scholar] [CrossRef] [PubMed]
- Lowe, R.; García-Díez, M.; Ballester, J.; Creswick, J.; Robine, J.-M.; Herrmann, F.; Rodó, X.; Lowe, R.; García-Díez, M.; Ballester, J.; et al. Evaluation of an early-warning system for heat wave-related mortality in Europe: Implications for sub-seasonal to seasonal forecasting and climate services. Int. J. Environ. Res. Public Health 2016, 13, 206. [Google Scholar] [CrossRef] [PubMed]
- Hales, S.; Kovats, S.; Lloyd, S.; Campbell-Lendrum, D. Quantitative Risk Assessment of the Effects of Climate Change on Selected Causes of Death, 2030s and 2050s; World Health Organization: Geneva, Switzerland, 2014; ISBN 978-9-24-150769-1. [Google Scholar]
- Ye, X.; Wolff, R.; Yu, W.; Vaneckova, P.; Pan, X.; Tong, S. Ambient temperature and morbidity: A review of epidemiological evidence. Environ. Health Perspect. 2012, 120, 19–28. [Google Scholar] [CrossRef]
- Li, M.; Gu, S.; Bi, P.; Yang, J.; Liu, Q. Heat waves and morbidity: Current knowledge and further direction: A comprehensive literature review. Int. J. Environ. Res. Public Health 2015, 12, 5256–5283. [Google Scholar] [CrossRef]
- Basu, R. High ambient temperature and mortality: A review of epidemiologic studies from 2001 to 2008. Environ. Health 2009, 8, 40. [Google Scholar] [CrossRef]
- Ebi, K.L. Resilience to the health risks of extreme weather events in a changing climate in the United States. Int. J. Environ. Res. Public Health 2011, 8, 4582–4595. [Google Scholar] [CrossRef]
- Van Der Linden, S.L.; Leiserowitz, A.A.; Feinberg, G.D.; Maibach, E.W. The scientific consensus on climate change as a gateway belief: Experimental evidence. PLoS ONE 2015, 10, e0118489. [Google Scholar] [CrossRef]
- Coumou, D.; Rahmstorf, S. A decade of weather extremes. Nat. Clim. Chang. 2012, 2, 491–496. [Google Scholar] [CrossRef]
- Bitencourt, D.P.; Fuentes, M.V.; Maia, P.A.; Amorim, F.T. Frequência, duração, abrangência espacial e intensidade das ondas de calor no Brasil. Rev. Bras. Meteorol. 2016, 31, 506–517. [Google Scholar] [CrossRef]
- Ceccherini, G.; Russo, S.; Ameztoy, I.; Romero, C.P.; Carmona-Moreno, C. Magnitude and frequency of heat and cold waves in recent decades: The case of South America. Nat. Hazards Earth Syst. Sci. 2016, 16, 821–831. [Google Scholar] [CrossRef]
- IPCC. Managing the Risks of Extreme Events and Disasters to Advance Climate Change Adaptation: Special Report of the Intergovernmental Panel on Climate Change; Field, C., Barros, V., Stocker, T., Qin, D., Dokken, D., Ebi, K., Mastrandrea, M., Mach, K., Plattner, G.-K., Allen, S., et al., Eds.; Intergovernmental Panel on Climate Change: Cambridge, UK, 2012; ISBN 9781139177245. [Google Scholar]
- Bellard, C.; Bertelsmeier, C.; Leadley, P.; Thuiller, W.; Courchamp, F. Impacts of climate change on the future of biodiversity. Ecol. Lett. 2012, 15, 365–377. [Google Scholar] [CrossRef] [PubMed]
- Klein, R.J.; Huq, S.; Denton, F.; Downing, T.E.; Richels, R.G.; Robinson, J.B.; Toth, F.L. Inter-relationships between adaptation and mitigation. In Climate change 2007: Impacts, Adaptation and Vulnerability: Contribution of Working Group II to the Fourth Assessment Report of the Intergovernmental Panel on Climate Change; Parry, M.L., Canziani, O.F., Palutikof, J.P., van der Linden, P.J., Hanson, C.E., Eds.; IPCC; Cambridge University Press: Cambridge, UK, 2007; pp. 745–777. [Google Scholar]
- Conlon, K.C.; Rajkovich, N.B.; White-Newsome, J.L.; Larsen, L.; O’Neill, M.S. Preventing cold-related morbidity and mortality in a changing climate. Maturitas 2011, 69, 197–202. [Google Scholar] [CrossRef] [PubMed]
- Schwartz, J.; Samet, J.M.; Patz, J.A. Hospital admissions for heart disease. Epidemiology 2004, 15, 755–761. [Google Scholar] [CrossRef] [PubMed]
- Rivero, E.U.; Bolufé, A.; Ortiz, J.; Rodríguez, P.L.; Reyes, Y.; Cristina, M.; Rivero, A.; Bolufé, J.; Ortiz, P.L.; Rodríguez, Y.; et al. Medical education cooperation with Cuba influence of climate variability on acute myocardial infarction mortality in Havana. MEDICC Rev. 2015, 17, 14–19. [Google Scholar]
- Sharovsky, R.; César, L.A.M. Increase in mortality due to myocardial infarction in the Brazilian city of São Paulo during winter. Arq. Bras. Cardiol. 2002, 78, 106–109. [Google Scholar] [CrossRef]
- Vasconcelos, J.; Freire, E.; Almendra, R.; Silva, G.L.; Santana, P. The impact of winter cold weather on acute myocardial infarctions in Portugal. Environ. Pollut. 2013, 183, 14–18. [Google Scholar] [CrossRef]
- Madrigano, J.; Mittleman, M.A.; Baccarelli, A.; Goldberg, R.; Melly, S.; von Klot, S.; Schwartz, J. Temperature, myocardial infarction, and mortality: Effect modification by individual- and area-level characteristics. Epidemiology 2013, 24, 439–446. [Google Scholar] [CrossRef]
- Kwon, B.; Lee, E.; Lee, S.; Heo, S.; Jo, K.; Kim, J.; Park, M. Vulnerabilities to temperature effects on acute myocardial infarction hospital admissions in South Korea. Int. J. Environ. Res. Public Health 2015, 12, 14571–14588. [Google Scholar] [CrossRef]
- Hajat, S.; Kovats, R.S.; Lachowycz, K. Heat-related and cold-related deaths in England and Wales: Who is at risk? Occup. Environ. Med. 2007, 64, 93–100. [Google Scholar] [CrossRef]
- Mazdiyasni, O.; AghaKouchak, A.; Davis, S.J.; Madadgar, S.; Mehran, A.; Ragno, E.; Sadegh, M.; Sengupta, A.; Ghosh, S.; Dhanya, C.T.; et al. Increasing probability of mortality during Indian heat waves. Sci. Adv. 2017, 3, e1700066. [Google Scholar] [CrossRef] [PubMed]
- Pomatto, L.C.D.; Davies, K.J.A. The role of declining adaptive homeostasis in ageing. J. Physiol. 2017, 595, 7275–7309. [Google Scholar] [CrossRef] [PubMed]
- Ma, W.; Zeng, W.; Zhou, M.; Wang, L.; Rutherford, S.; Lin, H.; Liu, T.; Zhang, Y.; Xiao, J.; Zhang, Y.; et al. The short-term effect of heat waves on mortality and its modifiers in China: An analysis from 66 communities. Environ. Int. 2015, 75, 103–109. [Google Scholar] [CrossRef] [PubMed]
- Scovronick, N.; Sera, F.; Acquaotta, F.; Garzena, D.; Fratianni, S.; Wright, C.Y.; Gasparrini, A. The association between ambient temperature and mortality in South Africa: A time-series analysis. Environ. Res. 2018, 161, 229–235. [Google Scholar] [CrossRef]
- Luber, G.; Prudent, N. Climate change and human health. Trans. Am. Clin. Climatol. Assoc. 2009, 120, 113–117. [Google Scholar]
- Curtis, S.; Fair, A.; Wistow, J.; Val, D.V.; Oven, K. Impact of extreme weather events and climate change for health and social care systems. Environ. Health 2017, 16, 128. [Google Scholar] [CrossRef]
- De Castro Martins Ferreira, L.; Nogueira, M.C.; de Britto Pereira, R.V.; de Farias, W.C.M.; de Souza Rodrigues, M.M.; Teixeira, M.T.B.; Carvalho, M.S. Ambient temperature and mortality due to acute myocardial infarction in Brazil: An ecological study of time-series analyses. Sci. Rep. 2019, 9. [Google Scholar] [CrossRef]
- Gronlund, C.J.; Sullivan, K.P.; Kefelegn, Y.; Cameron, L.; O’Neill, M.S. Climate change and temperature extremes: A review of heat- and cold-related morbidity and mortality concerns of municipalities. Maturitas 2018, 114, 54–59. [Google Scholar] [CrossRef]
- Yang, J.; Hu, L.; Wang, C. Population dynamics modify urban residents’ exposure to extreme temperatures across the United States. Sci. Adv. 2019, 5, eaay3452. [Google Scholar] [CrossRef]
- Achebak, H.; Devolder, D.; Ballester, J. Trends in temperature-related age-specific and sex-specific mortality from cardiovascular diseases in Spain: A national time-series analysis. Lancet Planet. Health 2019, 3, e297–e306. [Google Scholar] [CrossRef]
- Mertz, O.; Halsnæs, K.; Olesen, J.E.; Rasmussen, K. Adaptation to Climate Change in Developing Countries. Environ. Manag. 2009, 43, 743–752. [Google Scholar] [CrossRef] [PubMed]
- Campbell-Lendrum, D.; Corvalán, C. Climate change and developing-country cities: Implications for environmental health and equity. J. Urban Health 2007, 84, i109–i117. [Google Scholar] [CrossRef] [PubMed]
- Yang, J.; Yin, P.; Sun, J.; Wang, B.; Zhou, M.; Li, M.; Tong, S.; Meng, B.; Guo, Y.; Liu, Q. Heatwave and mortality in 31 major Chinese cities: Definition, vulnerability and implications. Sci. Total Environ. 2019, 649, 695–702. [Google Scholar] [CrossRef]
- Gouveia, N.; Hajat, S.; Armstrong, B. Socioeconomic differentials in the temperature–mortality relationship in São Paulo, Brazil. Int. J. Epidemiol. 2003, 32, 390–397. [Google Scholar] [CrossRef] [PubMed]
- Bell, M.L.; O’Neill, M.S.; Ranjit, N.; Borja-Aburto, V.H.; Cifuentes, L.A.; Gouveia, N.C. Vulnerability to heat-related mortality in Latin America: A case-crossover study in Sao Paulo, Brazil, Santiago, Chile and Mexico City, Mexico. Int. J. Epidemiol. 2008, 37, 796–804. [Google Scholar] [CrossRef] [PubMed]
- Son, J.-Y.; Gouveia, N.; Bravo, M.A.; de Freitas, C.U.; Bell, M.L. The impact of temperature on mortality in a subtropical city: Effects of cold, heat, and heat waves in São Paulo, Brazil. Int. J. Biometeorol. 2016, 60, 113–121. [Google Scholar] [CrossRef] [PubMed]
- Gasparrini, A.; Guo, Y.; Hashizume, M.; Lavigne, E.; Zanobetti, A.; Schwartz, J.; Tobias, A.; Tong, S.; Rocklöv, J.; Forsberg, B.; et al. Mortality risk attributable to high and low ambient temperature: A multicountry observational study. Lancet 2015, 386, 369–375. [Google Scholar] [CrossRef]
- Santos, L. Healthcare regions and their care networks: An organizational-systemic model for SUS. Cienc. Saude Colet. 2017, 22, 1281–1289. [Google Scholar] [CrossRef]
- Divo, M.J.; Martinez, C.H.; Mannino, D.M. Ageing and the epidemiology of multimorbidity. Eur. Respir. J. 2014, 44, 1055–1068. [Google Scholar] [CrossRef]
- Nunes, B.P.; Batista, S.R.R.; de Andrade, F.B.; de Souza Junior, P.R.B.; Lima-Costa, M.F.; Facchini, L.A.; Facchini, L.A. Multimorbidity: The Brazilian Longitudinal Study of Aging (ELSI-Brazil). Rev. Saude Publica 2018, 52 (Suppl. 2), 10s. [Google Scholar] [CrossRef]
- Frumkin, H.; Hess, J.; Luber, G.; Malilay, J.; McGeehin, M. Climate change: The public health response. Am. J. Public Health 2008, 98, 435–445. [Google Scholar] [CrossRef] [PubMed]
- Madley-Dowd, P.; Hughes, R.; Tilling, K.; Heron, J. The proportion of missing data should not be used to guide decisions on multiple imputation. J. Clin. Epidemiol. 2019, 110, 63–73. [Google Scholar] [CrossRef]
- de Andrade-Barbosa, T.L.; Xavier-Gomes, L.M.; de Andrade Barbosa, V.; Caldeira, A.P. Mortalidade masculina por causas externas em Minas Gerais, Brasil. Cienc. Saude Colet. 2013, 18, 711–719. [Google Scholar] [CrossRef] [PubMed]
- Gasparrini, A.; Leone, M. Attributable risk from distributed lag models. BMC Med. Res. Methodol. 2014, 14, 55. [Google Scholar] [CrossRef] [PubMed]
- Tobias, A.; Armstrong, B.; Zuza, I.; Gasparrini, A.; Linares, C.; Diaz, J. Mortality on extreme heat days using official thresholds in Spain: A multi-city time series analysis. BMC Public Health 2012, 12, 133. [Google Scholar] [CrossRef]
- Lavigne, E.; Gasparrini, A.; Wang, X.; Chen, H.; Yagouti, A.; Fleury, M.D.; Cakmak, S. Extreme ambient temperatures and cardiorespiratory emergency room visits: Assessing risk by comorbid health conditions in a time series study. Environ. Health 2014, 13, 5. [Google Scholar] [CrossRef]
- Tobías, A.; Armstrong, B.; Gasparrini, A. Investigating uncertainty in the minimum mortality temperature: Methods and application to 52 Spanish cities. Epidemiology 2017, 28, 72–76. [Google Scholar] [CrossRef]
- Gasparrini, A.; Armstrong, B.; Kenward, M.G. Multivariate meta-analysis for non-linear and other multi-parameter associations. Stat. Med. 2012, 31, 3821–3839. [Google Scholar] [CrossRef]
- Gasparrini, A. Distributed lag linear and non-linear models in R: The package DLNM. J. Stat. Softw. 2011, 43, 1–20. [Google Scholar] [CrossRef]
- Lee, W.; Kim, H.; Hwang, S.; Zanobetti, A.; Schwartz, J.D.; Chung, Y. Monte Carlo simulation-based estimation for the minimum mortality temperature in temperature-mortality association study. BMC Med. Res. Methodol. 2017, 17, 137. [Google Scholar] [CrossRef]
- Cox, B.; Gasparrini, A.; Catry, B.; Delcloo, A.; Bijnens, E.; Vangronsveld, J.; Nawrot, T.S. Mortality related to cold and heat. What do we learn from dairy cattle? Environ. Res. 2016, 149, 231–238. [Google Scholar] [CrossRef] [PubMed]
- Gasparrini, A.; Armstrong, B. The impact of heat waves on mortality. Epidemiology 2011, 22, 68–73. [Google Scholar] [CrossRef] [PubMed]
- World Bank. World Development Indicators 2017; World Bank: Washington, DC, USA, 2017. [Google Scholar]
- Silva, I.C.; Restarepo-Mendez, M.C.; Costa, J.C.; Ewerling, F.; Hellwig, F.; Ferreira, L.Z.; Ruas, L.P.; Joseph, G.; Barros, A.J. Mensuração de desigualdades sociais em saúde: Conceitos e abordagens metodológicas no contexto brasileiro. Epidemiol. e Serviços Saúde 2018, 27, e000100017. [Google Scholar] [CrossRef] [PubMed]
- McGregor, G.; Bessemoulin, P.; Ebi, K.; Menne, B. Heatwaves and Health: Guidance on Warning-System Development; World Meteorological Organization, World Health Organization: Geneva, Switzerland, 2013; ISBN 978-0-7695-5111-1. [Google Scholar]
- Lane, K.; Ito, K.; Johnson, S.; Gibson, E.; Tang, A.; Matte, T. Burden and risk factors for cold-related illness and death in New York city. Int. J. Environ. Res. Public Health 2018, 15, 632. [Google Scholar] [CrossRef] [PubMed]
- Lim, J.-S.; Kwon, H.-M.; Kim, S.-E.; Lee, J.; Lee, Y.-S.; Yoon, B.-W. Effects of temperature and pressure on acute stroke incidence assessed using a Korean nationwide insurance database. J. Stroke 2017, 19, 295–303. [Google Scholar] [CrossRef][Green Version]
- Zhang, Y.; Li, S.; Pan, X.; Tong, S.; Jaakkola, J.J.; Gasparrini, A.; Guo, Y.; Wang, S. The effects of ambient temperature on cerebrovascular mortality: An epidemiologic study in four climatic zones in China. Environ. Health 2014, 13, 24. [Google Scholar] [CrossRef]
- Kim, S.-H.; Jo, S.-N.; Myung, H.-N.; Jang, J.-Y. The effect of pre-existing medical conditions on heat stroke during hot weather in South Korea. Environ. Res. 2014, 133, 246–252. [Google Scholar] [CrossRef]
- Yang, J.; Yin, P.; Zhou, M.; Ou, C.-Q.; Li, M.; Li, J.; Liu, X.; Gao, J.; Liu, Y.; Qin, R.; et al. The burden of stroke mortality attributable to cold and hot ambient temperatures: Epidemiological evidence from China. Environ. Int. 2016, 92–93, 232–238. [Google Scholar] [CrossRef]
- Díaz, J.; Carmona, R.; Mirón, I.J.; Ortiz, C.; Linares, C. Comparison of the effects of extreme temperatures on daily mortality in Madrid (Spain), by age group: The need for a cold wave prevention plan. Environ. Res. 2015, 143, 186–191. [Google Scholar] [CrossRef]
- Green, H.; Bailey, J.; Schwarz, L.; Vanos, J.; Ebi, K.; Benmarhnia, T. Impact of heat on mortality and morbidity in low and middle income countries: A review of the epidemiological evidence and considerations for future research. Environ. Res. 2019, 171, 80–91. [Google Scholar] [CrossRef]
- Esperón-Rodríguez, M.; Bonifacio-Bautista, M.; Barradas, V.L. Socio-economic vulnerability to climate change in the central mountainous region of eastern Mexico. Ambio 2016, 45, 146–160. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Liu, C.; Yavar, Z.; Sun, Q. Cardiovascular response to thermoregulatory challenges. Am. J. Physiol. Circ. Physiol. 2015, 309, H1793–H1812. [Google Scholar] [CrossRef] [PubMed]
- Huang, C.; Barnett, A.G.; Xu, Z.; Chu, C.; Wang, X.; Turner, L.R.; Tong, S. Managing the health effects of temperature in response to climate change: Challenges ahead. Environ. Health Perspect. 2013, 121, 415–419. [Google Scholar] [CrossRef]
- Gasparrini, A.; Guo, Y.; Sera, F.; Vicedo-Cabrera, A.M.; Huber, V.; Tong, S.; de Sousa Zanotti Stagliorio Coelho, M.; Nascimento Saldiva, P.H.; Lavigne, E.; Matus Correa, P.; et al. Projections of temperature-related excess mortality under climate change scenarios. Lancet Planet. Health 2017, 1, e360–e367. [Google Scholar] [CrossRef]
- Hashim, J.H.; Hashim, Z. Climate change, extreme weather events, and human health implications in the Asia Pacific Region. Asia Pac. J. Public Health 2016, 28, 8S–14S. [Google Scholar] [CrossRef] [PubMed]
- Patz, J.A.; Campbell-Lendrum, D.; Holloway, T.; Foley, J.A. Impact of regional climate change on human health. Nature 2005, 438, 310–317. [Google Scholar] [CrossRef]
- Wang, Y.; Shi, L.; Zanobetti, A.; Schwartz, J.D. Estimating and projecting the effect of cold waves on mortality in 209 US cities. Environ. Int. 2016, 94, 141–149. [Google Scholar] [CrossRef]
- Egondi, T.; Kyobutungi, C.; Rocklöv, J. Temperature variation and heat wave and cold spell impacts on years of life lost among the urban poor population of Nairobi, Kenya. Int. J. Environ. Res. Public Health 2015, 12, 2735–2748. [Google Scholar] [CrossRef]
- Zhang, Y.; Yu, C.; Bao, J.; Li, X. Impact of temperature on mortality in Hubei, China: A multi-county time series analysis. Sci. Rep. 2017, 7, 45093. [Google Scholar] [CrossRef]
- Chan, E.Y.Y.; Goggins, W.B.; Kim, J.J.; Griffiths, S.M. A study of intracity variation of temperature-related mortality and socioeconomic status among the Chinese population in Hong Kong. J. Epidemiol. Community Health 2012, 66, 322–327. [Google Scholar] [CrossRef]
- Ostro, B.; Lipsett, M.; Reynolds, P.; Goldberg, D.; Hertz, A.; Garcia, C.; Henderson, K.D.; Bernstein, L. Long-term exposure to constituents of fine particulate air pollution and mortality: Results from the California Teachers Study. Environ. Health Perspect. 2010, 118, 363–369. [Google Scholar] [CrossRef] [PubMed]
- Bobb, J.F.; Peng, R.D.; Bell, M.L.; Dominici, F. Heat-related mortality and adaptation to heat in the United States. Environ. Health Perspect. 2014, 122, 811–816. [Google Scholar] [CrossRef] [PubMed]
- Michelozzi, P. Temperature and summer mortality: Geographical and temporal variations in four Italian cities. J. Epidemiol. Community Health 2006, 60, 417–423. [Google Scholar] [CrossRef] [PubMed]
- Morabito, M.; Crisci, A.; Moriondo, M.; Profili, F.; Francesconi, P.; Trombi, G.; Bindi, M.; Gensini, G.F.; Orlandini, S. Air temperature-related human health outcomes: Current impact and estimations of future risks in Central Italy. Sci. Total Environ. 2012, 441, 28–40. [Google Scholar] [CrossRef] [PubMed]
- Jiménez-Candil, J.; Díaz-Castro, Ó.; Barrabés, J.A.; García de la Villa, B.; Bodí Peris, V.; López Palop, R.; Fernández-Ortiz, A.; Martínez-Sellés, M. Actualización en cardiopatía isquémica y cuidados críticos cardiológicos. Rev. Española Cardiol. 2013, 66, 198–204. [Google Scholar] [CrossRef]
- Arós, F.; Heras, M.; Vila, J.; Sanz, H.; Ferreira-González, I.; Permanyer-Miralda, G.; Cuñat, J.; López-Bescós, L.; Cabadés, A.; Loma-Osorio, A.; et al. Reducción de la mortalidad precoz y a 6 meses en pacientes con IAM en el periodo 1995-2005. Datos de los registros PRIAMHO I, II y MASCARA. Rev. Española Cardiol. 2011, 64, 972–980. [Google Scholar] [CrossRef]
- Puymirat, E. Association of changes in clinical characteristics and management with improvement in survival among patients with ST-elevation myocardial infarction. Jama 2012, 308, 998. [Google Scholar] [CrossRef]
- Ebi, K.L.; Bowen, K. Extreme events as sources of health vulnerability: Drought as an example. Weather Clim. Extrem. 2016, 11, 95–102. [Google Scholar] [CrossRef]
- Medina-Ramón, M.; Zanobetti, A.; Cavanagh, D.P.; Schwartz, J. Extreme temperatures and mortality: Assessing effect modification by personal characteristics and specific cause of death in a multi-city case-only analysis. Environ. Health Perspect. 2006, 114, 1331–1336. [Google Scholar] [CrossRef]
- Wang, X.; Li, G.; Liu, L.; Westerdahl, D.; Jin, X.; Pan, X. Effects of extreme temperatures on cause-specific cardiovascular mortality in China. Int. J. Environ. Res. Public Health 2015, 12, 16136–16156. [Google Scholar] [CrossRef]
- Zhao, Q.; Li, S.; Coelho, M.S.Z.S.; Saldiva, P.H.N.; Hu, K.; Huxley, R.R.; Abramson, M.J.; Guo, Y. The association between heatwaves and risk of hospitalization in Brazil: A nationwide time series study between 2000 and 2015. PLoS Med. 2019, 16. [Google Scholar] [CrossRef] [PubMed]
- Xiao, J.; Spicer, T.; Jian, L.; Yun, G.Y.; Shao, C.; Nairn, J.; Fawcett, R.J.B.; Robertson, A.; Weeramanthri, T.S. Variation in population vulnerability to heat wave in Western Australia. Front. Public Health 2017, 5, 64. [Google Scholar] [CrossRef] [PubMed]
- Bi, P.; Williams, S.; Loughnan, M.; Lloyd, G.; Hansen, A.; Kjellstrom, T.; Dear, K.; Saniotis, A. The effects of extreme heat on human mortality and morbidity in Australia: Implications for public health. Asia Pac. J. Public Health 2011, 23, 27S–36S. [Google Scholar] [CrossRef] [PubMed]
- Arbuthnott, K.; Hajat, S.; Heaviside, C.; Vardoulakis, S. Changes in population susceptibility to heat and cold over time: Assessing adaptation to climate change. Environ. Health 2016, 15, S33. [Google Scholar] [CrossRef] [PubMed]
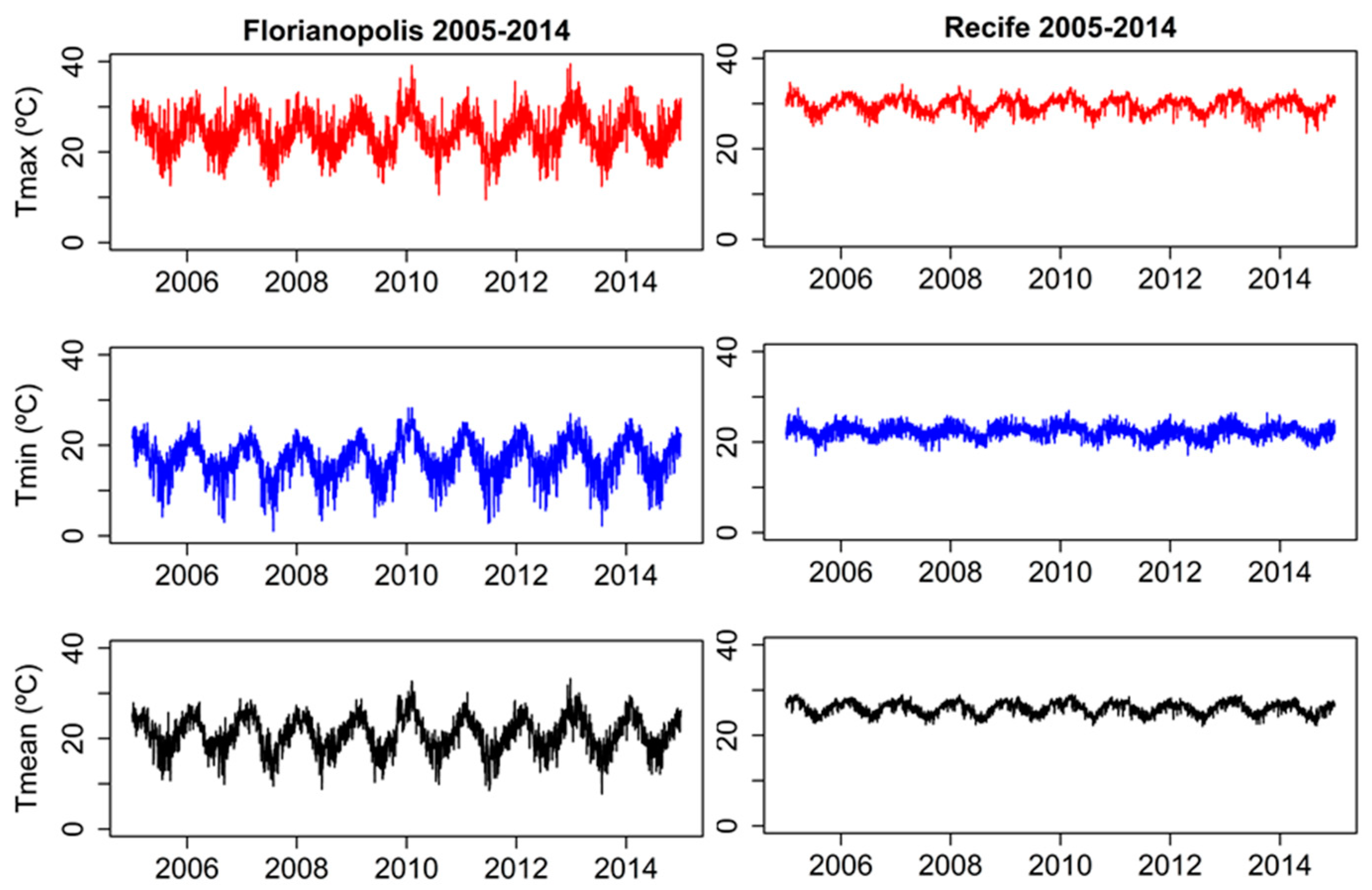
| Health Regions | Temp. (°C) | STATISTIC | |||
|---|---|---|---|---|---|
| TMean (°C) | TMin. (°C) | TMax (°C) | SD | ||
| Florianopolis | TMax. | 24.28 | 9.49 | 39.5 | 4.23 |
| TMin. | 17.06 | 1.05 | 28.28 | 4.30 | |
| TMean. | 21.01 | 7.74 | 33.25 | 3.87 | |
| Recife | TMax. | 29.76 | 23.5 | 34.7 | 1.56 |
| TMin. | 22.35 | 17 | 27.5 | 1.45 | |
| TMean. | 26.00 | 21.98 | 29.06 | 1.36 | |
| TIPO/CAUSE GROUP | DEATHS A | DEATHS B | RELATIVE RISK (95% CI) | |||||
|---|---|---|---|---|---|---|---|---|
| Total | % | MMT C (°C) | % Cold | % Heat | 1st Perc. | 99th Perc. | ||
| FLORIANÓPOLIS | NON-ACCIDENTAL MORTALITY | 2.490 | 5.80 | 21.4 | 2.40 | 3.40 | 1.20 (0.97–1.49) | 1.41 (1.14–1.76) |
| RESPIRATORY AND CIRCULATORY | 1853 | 8.90 | 23.7 | 8.03 | 0.91 | 1.53 (1.11–2.20) | 1.16 (0.87–1.54) | |
| CEREBROVASCULAR | 780 | 23.30 | 24 | 20.94 | 2.37 | 2.20 (0.98–4.95) | 1.55 (0.80–2.99) | |
| CARDIOVASCULAR | 602 | 8.70 | 18.1 | 1.20 | 7.50 | 1.32 (0.79–2.20) | 1.41 (0.74–2.66) | |
| RECIFE | NON-ACCIDENTAL MORTALITY | 3773 | 1.8 | 26.8 | 1.53 | 0.16 | 1.10 (1.00–1.22) | 1.02 (0.94–1.10) |
| RESPIRATORY AND CIRCULATORY | 2470 | 3.30 | 27 | 2.95 | 0.18 | 1.19 (1.01–1.41) | 1.02 (0.91–1.17) | |
| CEREBROVASCULAR | 1289 | 5.57 | 26 | 2.96 | 2.42 | 1.38 (1.03–1.84) | 1.20 (0.93–1.54) | |
| CARDIOVASCULAR | 2319 | 8.08 | 26.9 | 7.15 | 0.97 | 1.17 (0.89–1.55) | 1.14 (0.92–1.42) | |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Péres, W.E.; Ribeiro, A.F.S.; Russo, A.; Nunes, B. The Association between Air Temperature and Mortality in Two Brazilian Health Regions. Climate 2020, 8, 16. https://doi.org/10.3390/cli8010016
Péres WE, Ribeiro AFS, Russo A, Nunes B. The Association between Air Temperature and Mortality in Two Brazilian Health Regions. Climate. 2020; 8(1):16. https://doi.org/10.3390/cli8010016
Chicago/Turabian StylePéres, Wolmir Ercides, Andreia F. S. Ribeiro, Ana Russo, and Baltazar Nunes. 2020. "The Association between Air Temperature and Mortality in Two Brazilian Health Regions" Climate 8, no. 1: 16. https://doi.org/10.3390/cli8010016
APA StylePéres, W. E., Ribeiro, A. F. S., Russo, A., & Nunes, B. (2020). The Association between Air Temperature and Mortality in Two Brazilian Health Regions. Climate, 8(1), 16. https://doi.org/10.3390/cli8010016






