The Relationship of Climate Change and Malaria Incidence in the Gambella Region, Ethiopia
Abstract
1. Introduction
2. Materials and Methods
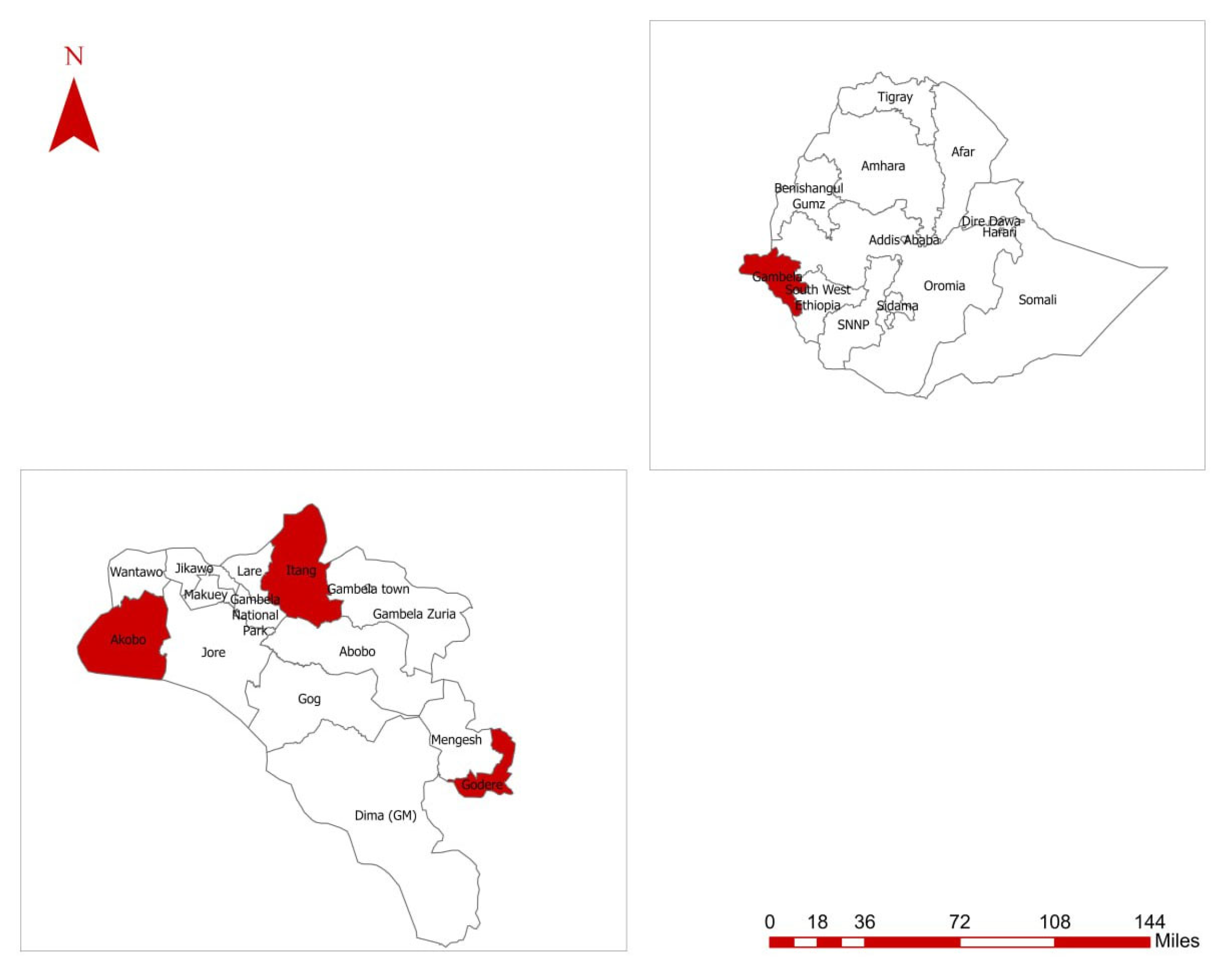
2.1. Setting and Study Design
2.2. Data Sources, Collection Tools, and Procedures
2.3. Data Processing and Analysis
3. Results
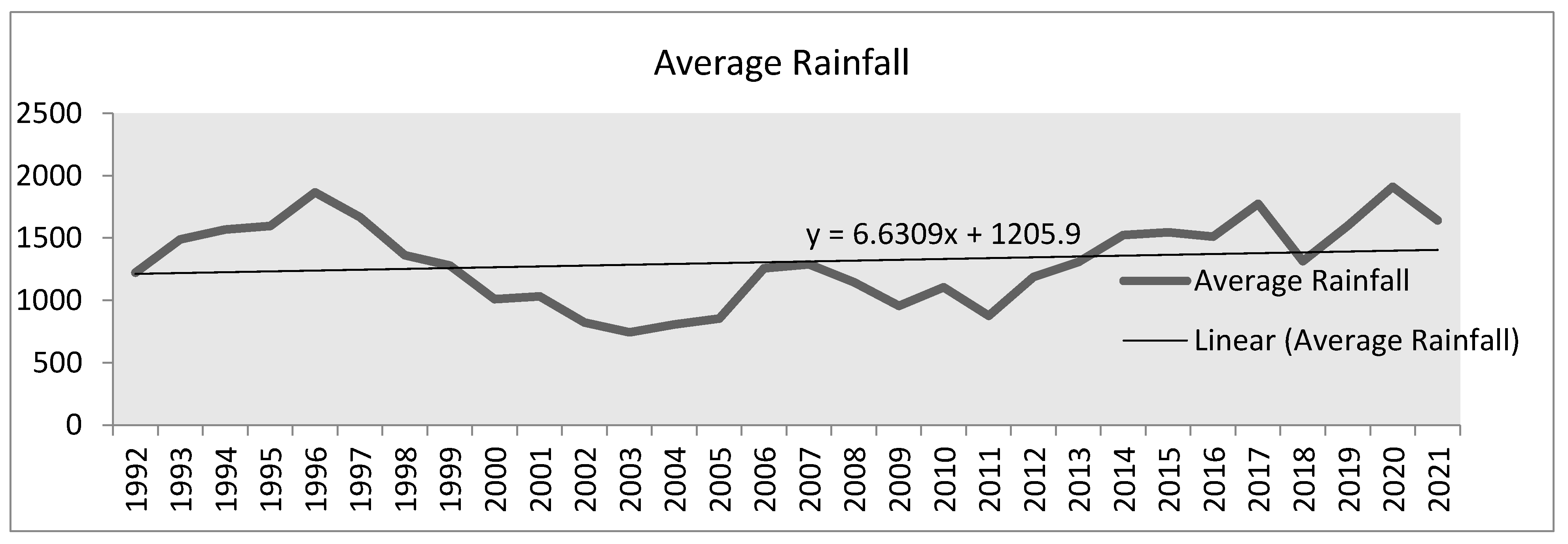
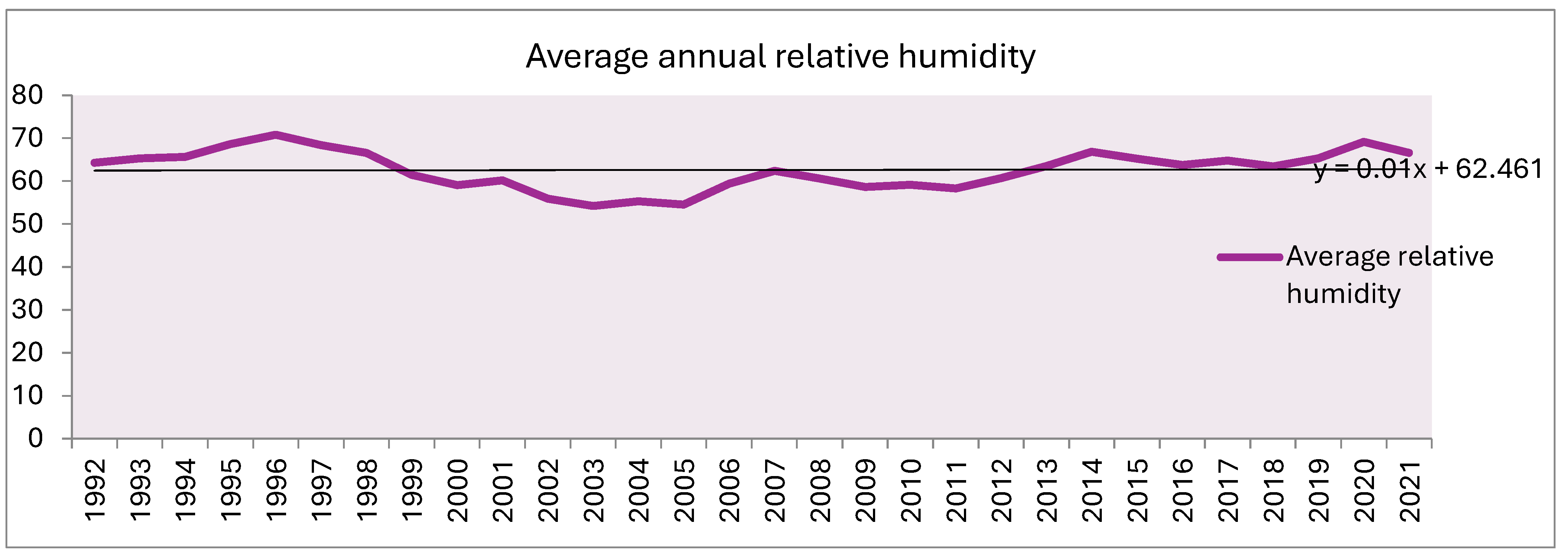
3.1. Trends of Climate Variables Change in Gambella Region
- Analysis of linear trends of rainfall:
- Linear Trends of relative humidity:
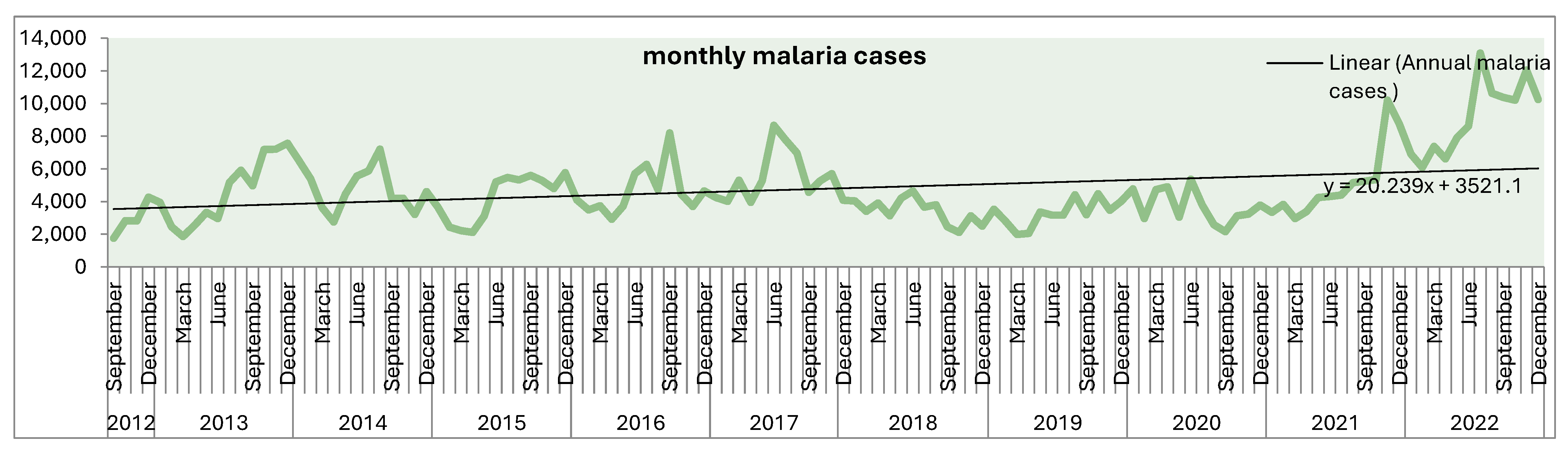
3.2. Malaria Incidence
3.3. Effects of Climate Variables on Malaria Incidence
3.3.1. Temperature
3.3.2. Rainfall
3.3.3. Relative Humidity
3.4. Multivariate Regression Analysis
4. Discussion
Limitations
5. Conclusions
Author Contributions
Funding
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- PAHO. Climate Change and Health. Pan American Health Organization. Available online: https://www.paho.org/en/topics/climate-change-and-health (accessed on 22 July 2023).
- World Health Organization (WHO). WHO Calls for Urgent Action to Protect Health from Climate Change—Sign the Call. 2015. Available online: https://www.who.int/news/item/06-10-2015-who-calls-for-urgent-action-to-protect-health-from-climate-change-sign-the-call (accessed on 22 May 2023).
- Harvard, T.H.; Chan School of Public Health. Shedding Light on Climate Change’s Threats to Health. 2019. Available online: https://www.hsph.harvard.edu/news/hsph-in-the-news/climate-change-threats-to-health/ (accessed on 24 September 2024).
- Tan, Y.S. 50 Years of Environment: Singapore’s Journey Towards Environmental Sustainability; World Scientific: Singapore, 2016. [Google Scholar]
- Di Napoli, C.; McGushin, A.; Romanello, M.; Ayeb-Karlsson, S.; Cai, W.; Chambers, J.; Dasgupta, S.; Escobar, L.E.; Kelman, I.; Kjellstrom, T.; et al. Tracking the Impacts of Climate Change on Human Health via Indicators: Lessons from the Lancet Countdown. BMC Public Health 2022, 22, 663. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization (WHO). Building Adaptation to Climate Change in Health in Least Developed Countries Through Resilient Water, Sanitation, and Hygiene (WASH). 2012. Available online: https://www.who.int/news/item/01-01-2012-building-adaptation-to-climate-change-in-health-in-least-developed-countries-through-resilient-water-sanitation-and-hygiene-(wash) (accessed on 24 September 2024).
- National Oceanic and Atmospheric Administration (NOAA). Climate Change Impacts. NOAA Education. 2024. Available online: https://www.noaa.gov/education/resource-collections/climate/climate-change-impacts (accessed on 24 September 2024).
- Hassan, M.; Saif, K.; Ijaz, M.S.; Sarfraz, Z.; Sarfraz, A.; Robles-Velasco, K.; Cherrez-Ojeda, I. Mean Temperature and Drought Projections in Central Africa: A Population-Based Study of Food Insecurity, Childhood Malnutrition and Mortality, and Infectious Disease. Int. J. Environ. Res. Public Health 2023, 20, 2697. [Google Scholar] [CrossRef] [PubMed]
- U.S. Global Change Research Program (USGCRP). Fourth National Climate Assessment. 2018. Available online: https://nca2018.globalchange.gov/ (accessed on 24 September 2024).
- Adrien, M. Past and Future Impacts of Climate Change on Swiss River Temperature and Discharge Investigated with Data Analysis and Numerical Modelling; EPFL: Lausanne, Switzerland, 2021; Available online: https://infoscience.epfl.ch/handle/20.500.14299/180729 (accessed on 5 August 2023).
- Silenzi, A.; Marotta, C.; Caredda, E.; Machado, R.S.; Severoni, S.; Rezza, G. Climate Change, Human Migration, and Health Nexus: What Do We Know About Public Health Implications on a Global Scale? Epidemiol. Prev. 2023, 47, 39–43. [Google Scholar] [PubMed]
- Morgan, E.A.; Hallgren, W.; Helfer, F.; Sahin, O.; Nalau, J.; Onyango, E.; Hadwen, W.; Mackey, B. Implications of the Paris Climate Change Agreement for Adaptation Research and Universities. In Climate Change Research at Universities: Addressing the Mitigation and Adaptation Challenges; Leal Filho, W., Ed.; Springer: Cham, Switzerland, 2017; pp. 251–262. [Google Scholar]
- Bandeira, M.; Graham, M.A.; Ebersöhn, L. The Significance of Feeling Safe for Resilience of Adolescents in Sub-Saharan Africa. Front. Psychol. 2023, 14, 1183748. [Google Scholar] [CrossRef]
- Abbott, P.; Shanks, R.; Stanley, I.; D’Ambruoso, L. A Protocol for a Critical Realist Systematic Synthesis of Interventions to Promote Pupils’ Wellbeing by Improving the School Climate in Low- and Middle-Income Countries. PLoS ONE 2024, 19, e0286489. [Google Scholar] [CrossRef]
- Kulkarni, M.A.; Duguay, C.; Ost, K. Charting the Evidence for Climate Change Impacts on the Global Spread of Malaria and Dengue and Adaptive Responses: A Scoping Review of Reviews. Glob. Health 2022, 18, 1. [Google Scholar] [CrossRef]
- Lilay, A.; Asamene, N.; Bekele, A.; Mengesha, M.; Wendabeku, M.; Tareke, I.; Girmay, A.; Wuletaw, Y.; Adossa, A.; Ba, Y.; et al. Reemergence of Yellow Fever in Ethiopia After 50 Years, 2013: Epidemiological and Entomological Investigations. BMC Infect. Dis. 2017, 17, 343. [Google Scholar] [CrossRef]
- Mekuriaw, W.; Kinde, S.; Kindu, B.; Mulualem, Y.; Hailu, G.; Gebresilassie, A.; Sisay, C.; Bekele, F.; Amare, H.; Wossen, M.; et al. Epidemiological, Entomological, and Climatological Investigation of the 2019 Dengue Fever Outbreak in Gewane District, Afar Region, North-East Ethiopia. Insects 2022, 13, 1066. [Google Scholar] [CrossRef]
- World Health Organization (WHO). Africa Faces Rising Climate-Linked Health Emergencies. WHO Regional Office for Africa. 2022. Available online: https://www.afro.who.int/news/africa-faces-rising-climate-linked-health-emergencies (accessed on 5 August 2023).
- Kabaria, C.W.; Gilbert, M.; Noor, A.M.; Snow, R.W.; Linard, C. The Impact of Urbanization and Population Density on Childhood Plasmodium falciparum Parasite Prevalence Rates in Africa. Malar. J. 2017, 16, 49. [Google Scholar] [CrossRef]
- Taye, G.; Kaba, M.; Woyessa, A.; Deressa, W.; Simane, B.; Kumie, A.; Berhane, G. Modeling Effect of Climate Variability on Malaria in Ethiopia. Ethiop. J. Health Dev. 2015, 29, 183–196. [Google Scholar]
- Food and Agriculture Organization of the United Nations (FAO). Food Security and Nutrition in the Age of Climate Change: Proceedings of the International Symposium Organized by the Government of Québec in Collaboration with FAO; FAO: Rome, Italy, 2018. [Google Scholar]
- Balbus, J.; Crimmins, A.; Gamble, J.L.; Easterling, D.R.; Kunkel, K.E.; Saha, S.; Sarofim, M.C. Ch. 1: Introduction: Climate Change and Human Health. In The Impacts of Climate Change on Human Health in the United States: A Scientific Assessment; U.S. Global Change Research Program: Washington, DC, USA, 2016; pp. 25–42. [Google Scholar]
- Winker, R.; Payton, A.; Brown, E.; McDermott, E.; Freedman, J.H.; Lenhardt, C.; Eaves, L.A.; Fry, R.C.; Rager, J.E. Wildfires and Climate Justice: Future Wildfire Events Predicted to Disproportionally Impact Socioeconomically Vulnerable Communities in North Carolina. Front. Public Health 2024, 12, 1339700. [Google Scholar] [CrossRef] [PubMed]
- Stoian, I.M.; Pârvu, S.; Minca, D.G. Relationship Between Climate Change, Air Pollution, and Allergic Diseases Caused by Ambrosia artemisiifolia (Common Ragweed). Maedica 2024, 19, 94–105. [Google Scholar] [CrossRef] [PubMed]
- United Nations High Commissioner for Refugees (UNHCR). Climate Change and Displacement. Available online: https://www.unhcr.org/what-we-do/build-better-futures/climate-change-and-displacement (accessed on 17 December 2024).
- Ferijal, T.; Batelaan, O.; Shanafield, M.; Alfahmi, F. Determination of Rainy Season Onset and Cessation Based on a Flexible Driest Period. Theor. Appl. Climatol. 2022, 148, 91–104. [Google Scholar] [CrossRef]
- Atiah, W.A.; Muthoni, F.K.; Kotu, B.; Kizito, F.; Amekudzi, L.K. Trends of Rainfall Onset, Cessation, and Length of Growing Season in Northern Ghana: Comparing the Rain Gauge, Satellite, and Farmer’s Perceptions. Atmosphere 2021, 12, 1674. [Google Scholar] [CrossRef]
- Heylen, D.J.A.; Kumsa, B.; Kimbita, E.; Frank, M.N.; Muhanguzi, D.; Jongejan, F.; Adehan, S.B.; Toure, A.; Aboagye-Antwi, F.; Ogo, N.I.; et al. Tick Communities of Cattle in Smallholder Rural Livestock Production Systems in Sub-Saharan Africa. Parasites Vectors 2023, 16, 206. [Google Scholar] [CrossRef]
- Feng, X.; Liu, C.; Xie, F.; Lu, J.; Chiu, L.S.; Tintera, G.; Chen, B. Precipitation Characteristic Changes Due to Global Warming in a High-Resolution (16 km) ECMWF Simulation. Q. J. R. Meteorol. Soc. 2019, 145, 303–317. [Google Scholar] [CrossRef]
- MacLeod, D. Seasonal Predictability of Onset and Cessation of the East African Rains. Weather Clim. Extrem. 2018, 21, 27–35. [Google Scholar] [CrossRef]
- Zaitchik, B.F.; Rodell, M.; Olivera, F. Evaluation of the Global Land Data Assimilation System Using Global River Discharge Data and a Source-to-Sink Routing Scheme. Water Resour. Res. 2010, 46, W06507. [Google Scholar] [CrossRef]
- Alemu, A.; Abebe, G.; Tsegaye, W.; Golassa, L. Climatic Variables and Malaria Transmission Dynamics in Jimma Town, South West Ethiopia. Parasites Vectors 2011, 4, 30. [Google Scholar] [CrossRef]
- Klepac, P.; Hsieh, J.L.; Ducker, C.L.; Assoum, M.; Booth, M.; Byrne, I.; Dodson, S.; Martin, D.L.; Turner, C.M.R.; van Daalen, K.R.; et al. Climate Change, Malaria, and Neglected Tropical Diseases: A Scoping Review. Trans. R. Soc. Trop. Med. Hyg. 2024, 118, 561–579. [Google Scholar] [CrossRef]
- Beck-Johnson, L.M.; Nelson, W.A.; Paaijmans, K.P.; Read, A.F.; Thomas, M.B.; Bjørnstad, O.N. The Importance of Temperature Fluctuations in Understanding Mosquito Population Dynamics and Malaria Risk. R. Soc. Open Sci. 2017, 4, 160969. [Google Scholar] [CrossRef] [PubMed]
- Haileselassie, W.; Ejigu, A.; Alemu, T.; Workneh, S.; Habtemichael, M.; David, R.E.; Lelisa, K.; Deressa, W.; Yan, G.; Parker, D.M.; et al. International Border Malaria Transmission in the Ethiopian District of Lare, Gambella Region: Implications for Malaria Spread into South Sudan. Malar. J. 2023, 22, 64. [Google Scholar] [CrossRef]
- Chanyalew, T.; Natea, G.; Amenu, D.; Yewhalaw, D.; Simma, E.A. Composition of Mosquito Fauna and Insecticide Resistance Status of Anopheles gambiae Sensu Lato in Itang Special District, Gambella, Southwestern Ethiopia. Malar. J. 2022, 21, 125. [Google Scholar] [CrossRef]
- Samset, B.H.; Lund, M.T.; Fuglestvedt, J.S.; Wilcox, L.J. 2023 Temperatures Reflect Steady Global Warming and Internal Sea Surface Temperature Variability. Commun. Earth Environ. 2024, 5, 460. [Google Scholar] [CrossRef]
- Ma, J.; Guo, Y.; Gao, J.; Tang, H.; Xu, K.; Liu, Q.; Xu, L. Climate Change Drives the Transmission and Spread of Vector-Borne Diseases: An Ecological Perspective. Biology 2022, 11, 1628. [Google Scholar] [CrossRef]
- Caminade, C.; Kovats, S.; Rocklov, J.; Tompkins, A.M.; Morse, A.P.; Colón-González, F.J.; Stenlund, H.; Martens, P.; Lloyd, S.J. Impact of Climate Change on Global Malaria Distribution. Proc. Natl. Acad. Sci. USA 2014, 111, 3286–3291. [Google Scholar] [CrossRef]
- Chou, W.C.; Wu, J.L.; Wang, Y.C.; Huang, H.; Sung, F.C.; Chuang, C.Y. Modeling the Impact of Climate Variability on Diarrhea-Associated Diseases in Taiwan (1996–2007). Sci. Total Environ. 2010, 409, 43–51. [Google Scholar] [CrossRef]
- Tigu, F.; Gebremaryam, T.; Desalegn, A. Seasonal Profile and Five-Year Trend Analysis of Malaria Prevalence in Maygaba Health Center, Welkait District, Northwest Ethiopia. J. Parasitol. Res. 2021, 2021, 6727843. [Google Scholar] [CrossRef]
- Ezeruigbo, C.F.; Ezeoha, A. Climate Change and the Burden of Healthcare Financing in African Households. Afr. J. Prim. Health Care Fam. Med. 2023, 15, e1–e3. [Google Scholar] [CrossRef]
- Williams, J.; Chin-Yee, S.; Maslin, M.; Barnsley, J.; Costello, A.; Lang, J.; McGlade, J.; Mulugetta, Y.; Taylor, R.; Winning, M.; et al. Africa and Climate Justice at COP27 and Beyond: Impacts and Solutions Through an Interdisciplinary Lens. UCL Open Environ. 2023, 5, e062. [Google Scholar] [CrossRef]
- Barber, B.; Rainham, D.G.; Tyedmers, P.; Vandertuin, T.; Ritcey, G.; Christie, S.D. Taking Action Towards Climate-Resilient, Low-Carbon, Health Systems: Perspectives from Canadian Health Leaders and Healthcare Professionals. Healthc. Manag. Forum 2024, 37, 395–400. [Google Scholar] [CrossRef] [PubMed]
- Wang, C.; Thakuri, B.; Roy, A.K.; Mondal, N.; Qi, Y.; Chakraborty, A. Changes in the Associations Between Malaria Incidence and Climatic Factors Across Malaria Endemic Countries in Africa and Asia-Pacific Region. J. Environ. Manag. 2023, 331, 117264. [Google Scholar] [CrossRef] [PubMed]
- Huang, F.; Zhou, S.; Zhang, S.; Wang, H.; Tang, L. Temporal Correlation Analysis Between Malaria and Meteorological Factors in Motuo County, Tibet. Malar. J. 2011, 10, 54. [Google Scholar] [CrossRef] [PubMed]
- Thomson, M.C.; Muñoz, Á.G.; Cousin, R.; Shumake-Guillemot, J. Climate Drivers of Vector-Borne Diseases in Africa and Their Relevance to Control Programmes. Infect. Dis. Poverty 2018, 7, 81. [Google Scholar] [CrossRef]
- World Health Organization (WHO). Regional Initiative to Tackle Health Impacts of Climate Change in Africa Launched. WHO Regional Office for Africa. 2023. Available online: https://www.afro.who.int/news/regional-initiative-tackle-health-impacts-climate-change-africa-launched (accessed on 24 September 2024).
- Deglon, M.; Dalvie, M.A.; Abrams, A. The Impact of Extreme Weather Events on Mental Health in Africa: A Scoping Review of the Evidence. Sci. Total Environ. 2023, 881, 163420. [Google Scholar] [CrossRef]
- Simane, B.; Beyene, H.; Deressa, W.; Kumie, A.; Berhane, K.; Samet, J. Review of Climate Change and Health in Ethiopia: Status and Gap Analysis. Ethiop. J. Health Dev. 2016, 30, 28–41. [Google Scholar]
- Gangwisch, M.; Matzarakis, A. Composition of Factors for Local Heat Adaptation Measures at the Local Level in Cities of the Mid-Latitude—An Approach for the South-West of Germany. Environ. Int. 2024, 187, 108718. [Google Scholar] [CrossRef]
- Azage, M.; Kumie, A.; Worku, A.; Bagtzoglou, A.C.; Anagnostou, E. Effect of Climatic Variability on Childhood Diarrhea and Its High Risk Periods in Northwestern Parts of Ethiopia. PLoS ONE 2017, 12, e0186933. [Google Scholar] [CrossRef]
- Sinore, T.; Wang, F. Impact of Climate Change on Agriculture and Adaptation Strategies in Ethiopia: A Meta-Analysis. Heliyon 2024, 10, e26103. [Google Scholar] [CrossRef]
- Concern Worldwide. Climate Change in Ethiopia. 2023. Available online: https://www.concern.net/news/climate-change-in-ethiopia (accessed on 24 September 2024).
- Weiss, D.J.; Bhatt, S.; Mappin, B.; Van Boeckel, T.P.; Smith, D.L.; Hay, S.I.; Gething, P.W. Air Temperature Suitability for Plasmodium falciparum Malaria Transmission in Africa 2000–2012: A High-Resolution Spatiotemporal Prediction. Malar. J. 2014, 13, 171. [Google Scholar] [CrossRef]
- Etana, D.; Snelder, D.J.R.M.; van Wesenbeeck, C.F.A.; de Cock Buning, T. Trends of Climate Change and Variability in Three Agro-Ecological Settings in Central Ethiopia: Contrasts of Meteorological Data and Farmers’ Perceptions. Climate 2020, 8, 123. [Google Scholar] [CrossRef]
- Zinsstag, J.; Ruiz De Castañeda, R.; Comte, É.; Tschopp, R.; Bonfoh, B.; Nkwescheu, A.S.; Wanda, F.; Bolon, I. Evolution and Impact of the One Health Approach in Switzerland and Worldwide. Rev. Med. Suisse 2023, 19, 1407–1411. [Google Scholar] [PubMed]
- Kelly-Hope, L.A.; Harding-Esch, E.M.; Willems, J.; Ahmed, F.; Sanders, A.M. Conflict-Climate-Displacement: A Cross-Sectional Ecological Study Determining the Burden, Risk, and Need for Strategies for Neglected Tropical Disease Programmes in Africa. BMJ Open 2023, 13, e071557. [Google Scholar] [CrossRef]
- Mahmud, A.S.; Martinez, P.P.; Baker, R.E. The Impact of Current and Future Climates on Spatiotemporal Dynamics of Influenza in a Tropical Setting. PNAS Nexus 2023, 2, pgad307. [Google Scholar] [CrossRef]
- Bayoh, M.N.; Lindsay, S.W. Effect of Temperature on the Development of the Aquatic Stages of Anopheles gambiae Sensu Stricto (Diptera: Culicidae). Bull. Entomol. Res. 2003, 93, 375–381. [Google Scholar] [CrossRef]
- National Aeronautics and Space Administration (NASA). Climate Data. NASA Science. Available online: https://science.nasa.gov/earth/data/climate-data (accessed on 7 May 2023).
- Hamed, K.H.; Rao, A.R. A Modified Mann-Kendall Trend Test for Autocorrelated Data. J. Hydrol. 1998, 204, 182–196. [Google Scholar] [CrossRef]

| Monthly Mean Climate Variable | Lag Months | Spearman’s r | p Value |
|---|---|---|---|
| Temperature in °C | 0 months | −0.0482 | 0.432 |
| 1 months | −0.0518 | 0.657 | |
| 2 months | 0.0408 | 0.121 | |
| Rainfall in mm | 0 months | 0.2276 | 0.003 |
| 1 months | 0.4262 | 0.001 | |
| 2 months | 0.3861 | 0.005 | |
| Relative humidity | 0 months | 0.5158 | 0.027 |
| 1 months | 0.3567 | 0.011 | |
| 2 months | 0.4262 | 0.001 |
| Climate Variables | Lag | Crude IRR (95% CI) | Adjusted IRR (95% CI) |
|---|---|---|---|
| Monthly mean Temperature | 0 months | 1.000 (0.997, 1.002) * | 1.000 (1.000, 1.001) * |
| 1 months | 0.999 (0.997, 1.002) | 0.998 (0.996,1.000) | |
| 2 months | 0.999(0.996,1.001) | 0.998(0.996,1.000) | |
| Monthly mean Relative humidity | 0 months | 1.002 (1.001, 1.003) * | 1.002 (1.001, 1.003) * |
| 1 months | 1.001(1.000,1.002) * | 1.002(1.001,1.003) * | |
| 2 months | 1.001(1.000,1.002) * | 1.001(1.000, 1.002) * | |
| Monthly mean Rainfall | 0 months | 1.001 (1.000, 1.002) * | 1.001(1.000, 1.002) * |
| 1 months | 1.002(1.001,1.003) * | 1.001 (1.0001,1.003) * | |
| 2 months | 1.002 (1.001, 1.003) * | 1.002(1.001,1.003) * |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Assefa, G.M.; Muluneh, M.D.; Alemu, Z.A. The Relationship of Climate Change and Malaria Incidence in the Gambella Region, Ethiopia. Climate 2025, 13, 104. https://doi.org/10.3390/cli13050104
Assefa GM, Muluneh MD, Alemu ZA. The Relationship of Climate Change and Malaria Incidence in the Gambella Region, Ethiopia. Climate. 2025; 13(5):104. https://doi.org/10.3390/cli13050104
Chicago/Turabian StyleAssefa, Geteneh Moges, Muluken Desalegn Muluneh, and Zewdie Aderaw Alemu. 2025. "The Relationship of Climate Change and Malaria Incidence in the Gambella Region, Ethiopia" Climate 13, no. 5: 104. https://doi.org/10.3390/cli13050104
APA StyleAssefa, G. M., Muluneh, M. D., & Alemu, Z. A. (2025). The Relationship of Climate Change and Malaria Incidence in the Gambella Region, Ethiopia. Climate, 13(5), 104. https://doi.org/10.3390/cli13050104







