Ethnobotanical Survey of Local Flora Used for Medicinal Purposes among Indigenous People in Five Areas in Lagos State, Nigeria
Abstract
:1. Introduction
2. Results and Discussion
2.1. Inventory of Plant Species Used to Treat a Variety of Health Conditions/Diseases
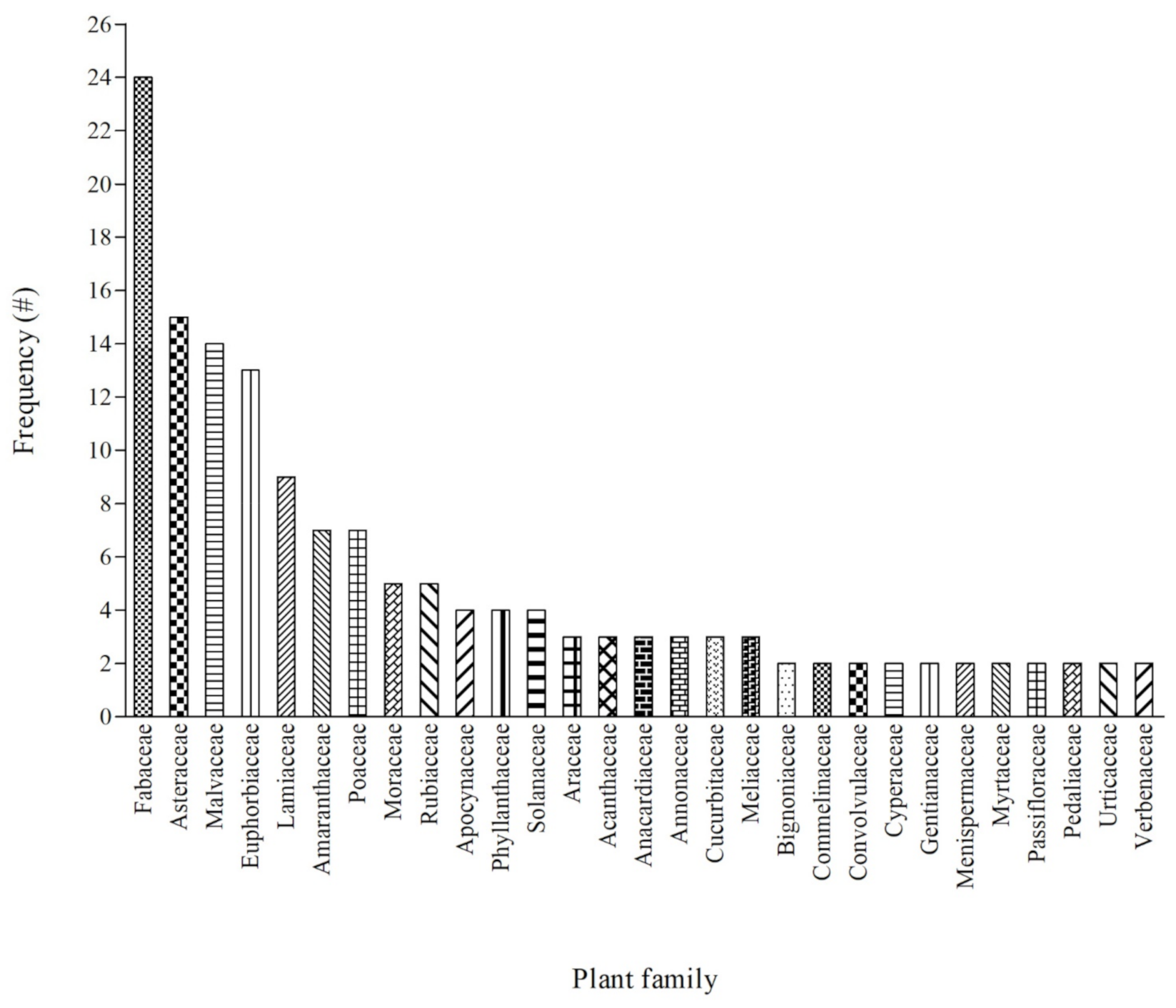
2.2. Plant Families Used for Medicinal Purpose
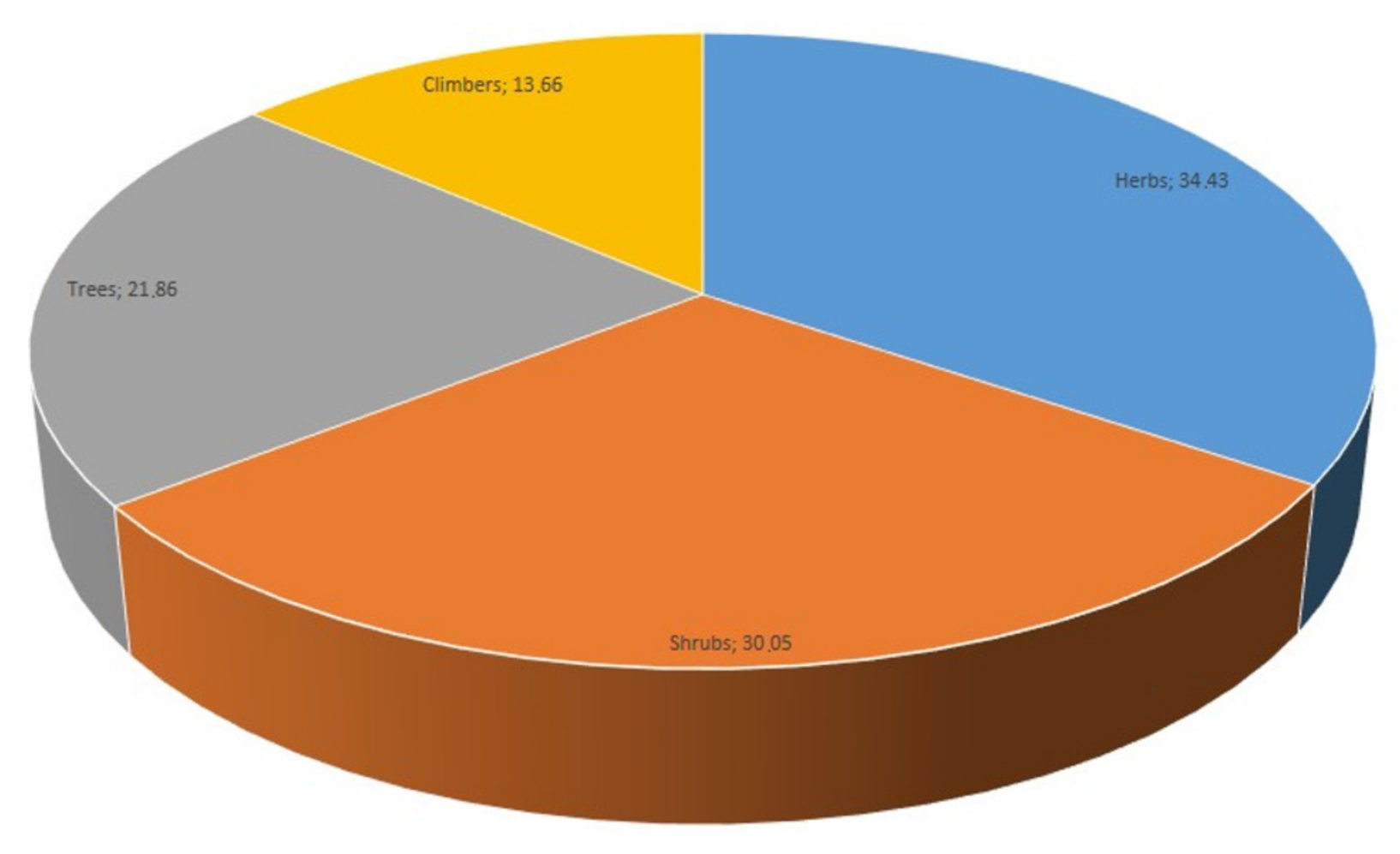
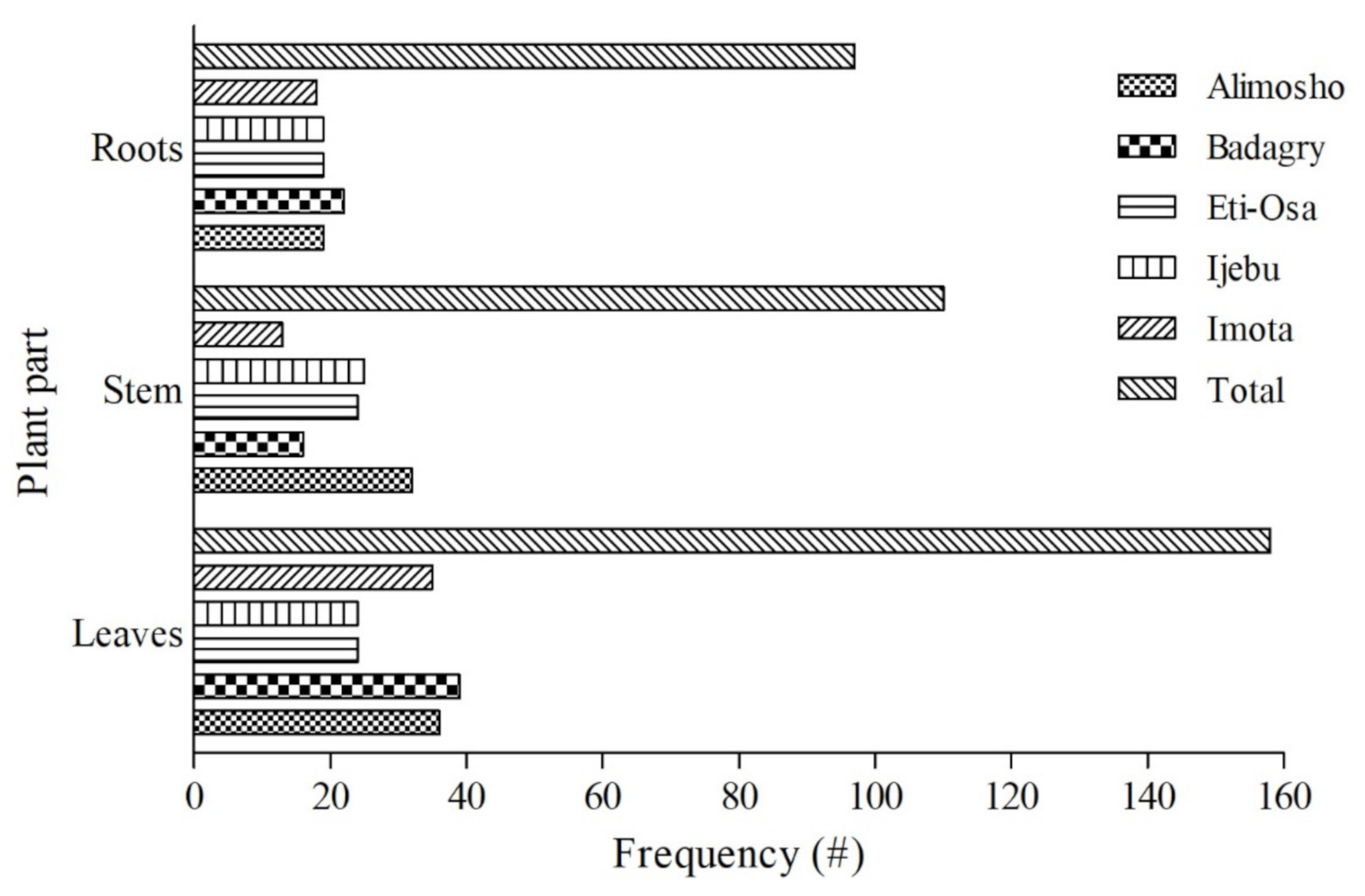
2.3. Life-Forms and Utilised Parts of the Documented Medicinal Plants
2.4. Ethnobotanical Indices of Plant Species Used to Treat a Variety of Health Conditions/Diseases
2.4.1. Frequency of Citation (FC, %) and Relative Frequency of Citation (RFC) for the Documented Plants
2.4.2. Fidelity Level (%) for the Documented Plants
2.4.3. Informant Consensus Factor (ICF) in the Study Area
3. Materials and Methods
3.1. Study Area
3.2. Field Interview
3.3. Plant Collection and Identification
3.4. Quantitative Ethnobotanical Indices
3.4.1. Frequency of Citation (FC) and Relative Frequency of Citation (RFC)
3.4.2. Fidelity Level (FL, %)
3.4.3. Informant Consensus Factor (ICF)
3.5. Ethical Consideration
4. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Ajao, A.A.; Mukaila, Y.O.; Sabiu, S. Wandering through southwestern Nigeria: An inventory of Yoruba useful angiosperm plants. Heliyon 2022, 8, e08668. [Google Scholar] [CrossRef] [PubMed]
- Van Wyk, B.E. A review of ethnobotanical research in southern Africa. S. Afr. J. Bot. 2002, 68, 1–13. [Google Scholar] [CrossRef]
- Seethapathy, G.S.; Ravikumar, K.; Paulsen, B.S.; de Boer, H.J.; Wangensteen, H. Ethnobotany of dioecious species: Traditional knowledge on dioecious plants in India. J. Ethnopharmacol. 2018, 221, 56–64. [Google Scholar] [CrossRef] [Green Version]
- Moyo, M.; Aremu, A.O.; van Staden, J. Ethnopharmacology in Sub-Sahara Africa: Current Trends and Future Perspectives. In Ethnopharmacology; Heinrich, M., Jäger, A.K., Eds.; Wiley Blackwell: Oxford, UK, 2015; pp. 263–278. [Google Scholar]
- Vandebroek, I.; Pieroni, A.; Stepp, J.R.; Hanazaki, N.; Ladio, A.; Alves, R.R.N.; Picking, D.; Delgoda, R.; Maroyi, A.; van Andel, T.; et al. Reshaping the future of ethnobiology research after the COVID-19 pandemic. Nat. Plants 2020, 6, 723–730. [Google Scholar] [CrossRef]
- Cordell, G.A. Ecopharmacognosy and the responsibilities of natural product research to sustainability. Phytochem. Lett. 2015, 11, 332–346. [Google Scholar] [CrossRef]
- Crane, P.R.; Ge, S.; Hong, D.-Y.; Huang, H.-W.; Jiao, G.-L.; Knapp, S.; Kress, W.J.; Mooney, H.; Raven, P.H.; Wen, J.; et al. The Shenzhen declaration on plant sciences—Uniting plant sciences and society to build a green, sustainable Earth. Plants People Planet 2019, 1, 59–61. [Google Scholar] [CrossRef]
- Pachter, L.M. Culture and clinical care: Folk illness beliefs and behaviors and their implications for health care delivery. J. Am. Med. Assoc. 1994, 271, 690–694. [Google Scholar] [CrossRef]
- Staub, P.O.; Geck, M.S.; Weckerle, C.S.; Casu, L.; Leonti, M. Classifying diseases and remedies in ethnomedicine and ethnopharmacology. J. Ethnopharmacol. 2015, 174, 514–519. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Cordell, G.A. Cognate and cognitive ecopharmacognosy—In an anthropogenic era. Phytochem. Lett. 2017, 20, 540–549. [Google Scholar] [CrossRef]
- Heinrich, M.; Edwards, S.; Moerman, D.E.; Leonti, M. Ethnopharmacological field studies: A critical assessment of their conceptual basis and methods. J. Ethnopharmacol. 2009, 124, 1–17. [Google Scholar] [CrossRef]
- Magwede, K.; van Wyk, B.E.; van Wyk, A.E. An inventory of Vhavenḓa useful plants. S. Afr. J. Bot. 2019, 122, 57–89. [Google Scholar] [CrossRef]
- Lawal, I.O.; Olufade, I.I.; Rafiu, B.O.; Aremu, A.O. Ethnobotanical survey of plants used for treating cough associated with respiratory conditions in Ede South Local Government Area of Osun State, Nigeria. Plants 2020, 9, 647. [Google Scholar] [CrossRef] [PubMed]
- Fakchich, J.; Elachouri, M. An overview on ethnobotanico-pharmacological studies carried out in Morocco, from 1991 to 2015: Systematic review (part 1). J. Ethnopharmacol. 2021, 267, 113200. [Google Scholar] [CrossRef] [PubMed]
- Vitalini, S.; Iriti, M.; Puricelli, C.; Ciuchi, D.; Segale, A.; Fico, G. Traditional knowledge on medicinal and food plants used in Val San Giacomo (Sondrio, Italy)—An alpine ethnobotanical study. J. Ethnopharmacol. 2013, 145, 517–529. [Google Scholar] [CrossRef]
- Mukaila, Y.O.; Oladipo, O.T.; Ogunlowo, I.; Ajao, A.A.-N.; Sabiu, S. Which plants for what ailments: A quantitative analysis of medicinal ethnobotany of Ile-Ife, Osun State, southwestern Nigeria. Evid.-Based Complementary Altern. Med. 2021, 2021, 5711547. [Google Scholar] [CrossRef]
- Al-Fatimi, M. Ethnobotanical survey of medicinal plants in central Abyan governorate, Yemen. J. Ethnopharmacol. 2019, 241, 111973. [Google Scholar] [CrossRef]
- Ngoua-Meye-Misso, R.-L.; Sima-Obiang, C.; Ndong, J.D.L.C.; Ndong-Atome, G.-R.; Ondo, J.P.; Ovono Abessolo, F.; Obame-Engonga, L.-C. Medicinal plants used in management of cancer and other related diseases in Woleu-Ntem province, Gabon. Eur. J. Integr. Med. 2019, 29, 100924. [Google Scholar] [CrossRef]
- Bekalo, T.H.; Woodmatas, S.D.; Woldemariam, Z.A. An ethnobotanical study of medicinal plants used by local people in the lowlands of Konta Special Woreda, southern nations, nationalities and peoples regional state, Ethiopia. J. Ethnobiol. Ethnomed. 2009, 5, 26. [Google Scholar] [CrossRef] [Green Version]
- Faruque, M.O.; Uddin, S.B.; Barlow, J.W.; Hu, S.; Dong, S.; Cai, Q.; Li, X.; Hu, X. Quantitative ethnobotany of medicinal plants used by indigenous communities in the Bandarban district of Bangladesh. Front. Pharmacol. 2018, 9, 40. [Google Scholar] [CrossRef] [Green Version]
- Nortje, J.M.; van Wyk, B.E. Medicinal plants of the Kamiesberg, Namaqualand, South Africa. J. Ethnopharmacol. 2015, 171, 205–222. [Google Scholar] [CrossRef]
- Erinoso, S.; Aworinde, D. Current outlook and future promise of ethnobotany in Nigeria: A review and personal observation. Afr. J. Plant Sci. 2018, 12, 73–80. [Google Scholar] [CrossRef] [Green Version]
- Sonibare, M.A.; Gbile, Z.O. Ethnobotanical survey of anti-asthmatic plants in South Western Nigeria. Afr. J. Tradit. Complementary Altern. Med. 2008, 5, 340–345. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- El-Ghani, M.M.A. Traditional medicinal plants of Nigeria: An overview. Agric. Biol. J. N. Am. 2016, 7, 220–247. [Google Scholar]
- Adedeji, D.E.; Kayode, J.; Ayeni, M.J. An ethnobotanical study of plant species used for medicine by the Eegun indigenous tribal group of Lagos State, Nigeria. Not. Sci. Biol. 2018, 10, 318–327. [Google Scholar] [CrossRef] [Green Version]
- Gbolade, A.A. Inventory of antidiabetic plants in selected districts of Lagos State, Nigeria. J. Ethnopharmacol. 2009, 121, 135–139. [Google Scholar] [CrossRef] [PubMed]
- Olowokudejo, J.; Kadiri, A.; Travih, V. An ethnobotanical survey of herbal markets and medicinal plants in Lagos State of Nigeria. Ethnobot. Leafl. 2008, 12, 851–865. [Google Scholar]
- Dudney, K.; Warren, S.; Sills, E.; Jacka, J. How study design influences the ranking of medicinal plant importance: A case study from Ghana, West Africa. Econ. Bot. 2015, 69, 306–317. [Google Scholar] [CrossRef]
- Chukwuma, D.M.; Chukwuma, E.C.; Adekola, O.O. An ethnobotanical survey of Malaria-treating plants in Ado-Ekiti Local Government Area, Ekiti State, Nigeria. Ethnobot. Res. Appl. 2019, 18, 1–10. [Google Scholar] [CrossRef]
- Rivera, D.; Allkin, R.; Obón, C.; Alcaraz, F.; Verpoorte, R.; Heinrich, M. What is in a name? The need for accurate scientific nomenclature for plants. J. Ethnopharmacol. 2014, 152, 393–402. [Google Scholar] [CrossRef]
- Boadu, A.A.; Asase, A. Documentation of herbal medicines used for the treatment and management of human diseases by some communities in southern Ghana. Evid.-Based Complementary Altern. Med. 2017, 2017. [Google Scholar] [CrossRef] [Green Version]
- Dauncey, E.A.; Irving, J.; Allkin, R.; Robinson, N. Common mistakes when using plant names and how to avoid them. Eur. J. Integr. Med. 2016, 8, 597–601. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Singh, H. Importance of local names of some useful plants in ethnobotanical study. Indian J. Tradit. Knowl. 2008, 7, 365–370. [Google Scholar]
- Kankara, S.S.; Ibrahim, M.H.; Mustafa, M.; Go, R. Ethnobotanical survey of medicinal plants used for traditional maternal healthcare in Katsina state, Nigeria. S. Afr. J. Bot. 2015, 97, 165–175. [Google Scholar] [CrossRef]
- Van Wyk, B.E. A family-level floristic inventory and analysis of medicinal plants used in Traditional African Medicine. J. Ethnopharmacol. 2020, 249, 112351. [Google Scholar] [CrossRef]
- Daru, B.H.; Berger, D.K.; Wyk, A.E. Opportunities for unlocking the potential of genomics for African trees. New Phytol. 2016, 210, 772–778. [Google Scholar] [CrossRef] [Green Version]
- Muleba, I.; Yessoufou, K.; Rampedi, I.T. Testing the non-random hypothesis of medicinal plant selection using the woody flora of the Mpumalanga Province, South Africa. Environ. Dev. Sustain. 2021, 23, 4162–4173. [Google Scholar] [CrossRef]
- Yaoitcha, A.S.; Houehanou, T.D.; Fandohan, A.B.; Houinato, M.R.B. Prioritization of useful medicinal tree species for conservation in Wari-Maro Forest Reserve in Benin: A multivariate analysis approach. For. Policy Econ. 2015, 61, 135–146. [Google Scholar] [CrossRef]
- Yirgu, A.; Mohammed, K.; Geldenhuys, C.J. Useful medicinal tree species of Ethiopia: Comprehensive review. S. Afr. J. Bot. 2019, 122, 291–300. [Google Scholar] [CrossRef]
- Van Wyk, A.S.; Prinsloo, G. A review of the ethnobotanical uses, pharmacology, toxicology, management and cultivation of selected South African protected multi-purpose tree species. S. Afr. J. Bot. 2019, 124, 258–269. [Google Scholar] [CrossRef]
- Ahoyo, C.C.; Houéhanou, T.D.; Yaoïtcha, A.S.; Prinz, K.; Glèlè Kakaï, R.; Sinsin, B.A.; Houinato, M.R.B. Traditional medicinal knowledge of woody species across climatic zones in Benin (West Africa). J. Ethnopharmacol. 2021, 265, 113417. [Google Scholar] [CrossRef]
- Van Andel, T.; Myren, B.; van Onselen, S. Ghana’s herbal market. J. Ethnopharmacol. 2012, 140, 368–378. [Google Scholar] [CrossRef] [PubMed]
- Selogatwe, K.M.; Asong, J.A.; Struwig, M.; Ndou, R.V.; Aremu, A.O. A review of ethnoveterinary knowledge, biological activities and secondary metabolites of medicinal woody plants used for managing animal health in South Africa. Vet. Sci. 2021, 8, 228. [Google Scholar] [CrossRef] [PubMed]
- De Albuquerque, U.P.; Farias Paiva de Lucena, R. Can apparency affect the use of plants by local people in tropical forests? Interciencia 2005, 30, 506–510. [Google Scholar]
- Moyo, M.; Aremu, A.O.; Van Staden, J. Medicinal plants: An invaluable, dwindling resource in sub-Saharan Africa. J. Ethnopharmacol. 2015, 174, 595–606. [Google Scholar] [CrossRef] [PubMed]
- Leonti, M. The relevance of quantitative ethnobotanical indices for ethnopharmacology and ethnobotany. J. Ethnopharmacol. 2022, 288, 115008. [Google Scholar] [CrossRef]
- Weckerle, C.S.; de Boer, H.J.; Puri, R.K.; van Andel, T.; Bussmann, R.W.; Leonti, M. Recommended standards for conducting and reporting ethnopharmacological field studies. J. Ethnopharmacol. 2018, 210, 125–132. [Google Scholar] [CrossRef]
- Friedman, J.; Yaniv, Z.; Dafni, A.; Palewitch, D. A preliminary classification of the healing potential of medicinal plants, based on a rational analysis of an ethnopharmacological field survey among Bedouins in the Negev Desert, Israel. J. Ethnopharmacol. 1986, 16, 275–287. [Google Scholar] [CrossRef]
- Trotter, R.T.; Logan, M.H. Informant consensus: A new approach for identifying potentially effective medicinal plants. In Plants in Indigenous Medicine & Diet Biobehavioral Approaches; Etkin, N.L., Ed.; Routledge: New York, NY, USA, 1986; pp. 91–112. [Google Scholar]
- Asiimwe, S.; Namutebi, A.; Borg-Karlson, A.-K.; Mugisha, M.K.; Kakudidi, E.K.; Hannington, O.-O. Documentation and consensus of indigenous knowledge on medicinal plants used by the local communities of western Uganda. J. Nat. Prod. Plant Resour. 2014, 4, 34–42. [Google Scholar]
- Balogun, F.O.; Ashafa, A.O.T. A review of plants used in South African traditional medicine for the management and treatment of hypertension. Planta Med. 2019, 85, 312–334. [Google Scholar] [CrossRef] [Green Version]
- Nyakudya, T.T.; Tshabalala, T.; Dangarembizi, R.; Erlwanger, K.H.; Ndhlala, A.R. The potential therapeutic value of medicinal plants in the management of metabolic disorders. Molecules 2020, 25, 2669. [Google Scholar] [CrossRef]
- Alebie, G.; Urga, B.; Worku, A. Systematic review on traditional medicinal plants used for the treatment of malaria in Ethiopia: Trends and perspectives. Malar. J. 2017, 16, 307. [Google Scholar] [CrossRef] [PubMed]
- Alamgeer Younis, W.; Asif, H.; Sharif, A.; Riaz, H.; Bukhari, I.A.; Assiri, A.M. Traditional medicinal plants used for respiratory disorders in Pakistan: A review of the ethno-medicinal and pharmacological evidence. Chin. Med. 2018, 13, 48. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Aremu, A.O.; Pendota, S.C. Medicinal plants for mitigating pain and inflammatory-related conditions: An appraisal of ethnobotanical uses and patterns in South Africa. Front. Pharmacol. 2021, 12. [Google Scholar] [CrossRef]
- Frimpong, E.K.; Asong, J.A.; Aremu, A.O. A review on medicinal plants used in the management of headache in Africa. Plants 2021, 10, 2038. [Google Scholar] [CrossRef]
- National Population Commission. Lagos State Nigeria, Census Figures; Nigeria Master Web; National Population Commission (NPC): Abuja, Nigeria, 2006. [Google Scholar]
- Idu, M.; Erhabor, J.O.; Efijuemue, H.M. Documentation on medicinal plants sold in markets in Abeokuta, Nigeria. Trop. J. Pharm. Res. 2010, 9, 110–118. [Google Scholar] [CrossRef] [Green Version]
- Sojobi, A.O.; Balogun, I.I.; Salami, A.W. Climate change in Lagos State, Nigeria: What really changed? Environ. Monit. Assess. 2016, 188, 556. [Google Scholar] [CrossRef] [PubMed]
- Tardío, J.; Pardo-de-Santayana, M. Cultural Importance Indices: A comparative analysis based on the useful wild plants of Southern Cantabria (Northern Spain). Econ. Bot. 2008, 62, 24–39. [Google Scholar] [CrossRef]
- Heinrich, M.; Ankli, A.; Frei, B.; Weimann, C.; Sticher, O. Medicinal plants in Mexico: Healers’ consensus and cultural importance. Soc. Sci. Med. 1998, 47, 1859–1871. [Google Scholar] [CrossRef]

| Plant Species | Heath Condition, FL (%) | RFC | FC (%) |
|---|---|---|---|
| Abrus precatorius L. | Cough, 71.70 Stomachache, 28.30 | 0.53 | 53 |
| Acalypha fimbriata Schumach. & Thonn. | Cough, 38.7 Divinity, 61.29 | 0.31 | 31 |
| Acanthospermum hispidum DC. | Hypertension, 62.96 Divinity, 37.04 | 0.27 | 27 |
| Achyranthes aspera L. | Erection, 28.17 Sight, 47.89 Potency, 23.94 | 0.71 | 71 |
| Adenia lobata (Jacq.) Engl. | Piles, 33.33 Arthritis, 66.67 | 0.48 | 48 |
| Ageratum conyzoides (L.) L. | Infectious disease, 21.25 Malaria, 42.5 Hypertension, 20.00 Sight, 16.25 | 0.80 | 80 |
| Albizia ferruginea (Guill. & Perr.) Benth. | Cough, 46.15 Pregnancy, 53.85 | 0.26 | 26 |
| Albizia lebbeck (L.) Benth. | Fever, 21.05 Arthritis, 45.61 Cough, 33.33 | 0.57 | 57 |
| Albizia zygia (DC.) J.F.Macbr. | Aphrodisiac, 25.97 Arthritis, 53.25 Cough, 33.77 Toothache, 3.90 | 0.77 | 77 |
| Alchornea cordifolia (Schumach. & Thonn.) Müll.Arg. | Arthritis, 18.07 Sight, 39.76 Ulcers, 15.66 Malaria, 7.23 | 0.83 | 83 |
| Alchornea laxiflora (Benth.) Pax & K.Hoffm. | De-worming, 24.56 Infectious diseases, 10.53 Malaria, 35.09 Oral hygiene, 29.82 | 0.57 | 57 |
| Alternanthera sessilis (L.) R.Br. ex DC. | Sight, 64.71 Jaundice, 35.29 | 0.17 | 17 |
| Amaranthus spinosus L. | Sight, 42.86 Cirrhosis, 57.14 | 0.21 | 21 |
| Amaranthus viridis L. | Longevity, 100.00 | 0.13 | 13 |
| Anacardium occidentale L. | Malaria, 100.00 | 0.38 | 38 |
| Anchomanes difformis (Blume) Engl. | Chicken pox, 40.00 Measles, 60.00 | 0.20 | 20 |
| Annona senegalensis Pers. | Malaria, 53.33 Potency, 46.67 | 0.30 | 30 |
| Anthocleista djalonensis A.Chev. | Hypertension, 100.00 | 0.26 | 26 |
| Anthocleista vogelii Planch. | Divinity, 100.00 | 0.07 | 7 |
| Artocarpus communis J.R.Forst. & G.Forst. (Synonym: Artocarpus altilis (Parkinson ex F.A.Zorn) Fosberg) | Malaria, 100.00 | 0.20 | 20 |
| Aspilia africana (Pers.) C.D.Adams | Fibroid, 26.00 Cough, 56.00 Purgative, 18.00 | 0.50 | 50 |
| Asystasia gangetica (L.) T.Anderson | Neck pain, 12.50 Sight, 43.75 Potency, 15.63 Cough, 28.13 | 0.64 | 64 |
| Azadirachta indica A.Juss. | Anti-snake bite, 100.00 | 0.16 | 16 |
| Baphia nitida Lodd. | Divinity, 100.00 | 0.12 | 12 |
| Barleria opaca (Vahl) Nees | Diabetes, 100.00 | 0.17 | 17 |
| Bidens pilosa L. | Cough, 100.00 | 0.19 | 19 |
| Boerhavia diffusa L. | Malaria, 100.00 | 0.18 | 18 |
| Borreria scabra (Schumach. & Thonn.) K.Schum. (Synonym: Spermacoce ruelliae DC.) | Ringworm, 19.18 Diabetes, 35.62 Eczema, 21.92 Birth control, 23.28 | 0.73 | 73 |
| Borreria verticillata (synonym: Spermacoce verticillata L.) | Ringworm, 88.37 Birth control, 11.63 | 0.43 | 43 |
| Bridelia ferruginea Benth. | Diabetes, 66.04 Birth control, 33.96 | 0.53 | 53 |
| Bryophyllum pinnatum (Lam.) Oken | Cough,72.22 Sight, 27.78 | 0.54 | 54 |
| Caladium bicolor (Aiton) Vent. | Pimples, 61.70 Cough, 38.30 | 0.47 | 47 |
| Calophyllum inophyllum L. | Scurvy, 100 | 0.08 | 8 |
| Calopogonium mucunoides Desv. | Cough, 60.94 Scurvy, 17.19 Ulcer, 21.88 | 0.64 | 64 |
| Calotropis procera (Aiton) Dryand. | Malaria, 60.00 Conjunctivitis, 40.00 | 0.25 | 25 |
| Canna indica L. | Cirrhosis, 50.00 Pimples, 50.00 | 0.28 | 28 |
| Canavalia ensiformis (L.) DC. | Pregnancy, 100.00 | 0.10 | 10 |
| Carpolobia lutea G.Don | Easy labour, 100.00 | 0.12 | 12 |
| Celosia argentea L. | Malaria, 100.00 | 0.02 | 2 |
| Centrosema pubescens Benth. | Pimples, 46.15 Purgative, 53.85 | 0.13 | 13 |
| Chassalia kolly (Schumach.) Hepper | Aphrodisiac, 100.00 | 0.18 | 18 |
| Chromolaena odorata (L.) R.M.King & H.Rob. | Malaria, 93.55 Potency, 6.45 | 0.62 | 62 |
| Cissampelos owariensis P.Beauv. ex DC. | Miscarriage, 100.00 | 0.36 | 36 |
| Citrus aurantiifolia (Christm.) Swingle | Malaria, 100.00 | 0.26 | 26 |
| Cleistopholis patens (Benth.) Engl. & Diels | Pimples, 100.00 | 0.23 | 23 |
| Cleome fruticosa L. (Synonym: Cadaba fruticosa (L.) Druce) | Cirrhosis, 61.90 Birth control, 38.10 | 0.21 | 21 |
| Clerodendrum capitatum (Willd.) Schumach. & Thonn | Malaria, 53.85 Diabetes, 46.15 | 0.26 | 26 |
| Clerodendrum paniculatum L. | Cirrhosis, 100.00 | 0.06 | 6 |
| Clerodendrum umbellatum Poir. | Stomachache, 100.00 | 0.16 | 16 |
| Clerodendrum volubile P.Beauv. | Immune booster, 100.00 | 0.02 | 2 |
| Cnestis ferruginea Vahl ex DC. | Immune booster, 100.00 | 0.05 | 5 |
| Cola millenii K.Schum. | Miscarriage, 100.00 | 0.09 | 9 |
| Colocasia esculenta (L.) Schott | Cough, 100.00 | 0.14 | 14 |
| Commelina africana L. | Diabetes, 78.57 Curse, 21.43 | 0.14 | 14 |
| Commelina erecta L. | Potency, 100.00 | 0.15 | 15 |
| Costus afer Ker Gawl. | Cough, 58.44 Ulcer, 41.56 | 0.77 | 77 |
| Croton lobatus L. (Synonym: Astraea lobata (L.) Klotzsch). | Cough, 100.00 | 0.18 | 18 |
| Croton zambesicus Müll.Arg. (Synonym: Croton gratissimus Burch.) | Malaria, 56.52 Hypertension, 43.48 | 0.23 | 23 |
| Cucumeropsis mannii Naudin | Cough, 100.00 | 0.01 | 1 |
| Cyathula prostrata (L.) Blume | Pimples, 100.00 | 0.03 | 3 |
| Cymbopogon citratus (DC.) Stapf | Longevity, 100.00 | 0.09 | 9 |
| Cyperus haspans L. | Arthritis, 100.00 | 0.11 | 11 |
| Dalbergia saxatilis Hook.f. | Longevity, 100.00 | 0.14 | 14 |
| Datura metel L. | Hypertension, 48.27 Immune booster, 37.93 Muscle relaxant, 13.80 | 0.29 | 29 |
| Desmodium velutinum (Willd.) DC. | Erection, 100.00 | 0.01 | 1 |
| Dichrostachys cinerea (L.) Wight & Arn. | Headache, 27.03 Toothache, 32.43 Cough, 40.54 | 0.37 | 37 |
| Dissotis rotundifolia (Sm.) Triana (Synonym Heterotis rotundifolia (Sm.) Jacq.-Fél.) | Easy labour, 20.69 Pregnancy care, 79.31 | 0.29 | 29 |
| Eclipta prostrata (L.) L. | Cough, 100.00 | 0.16 | 16 |
| Elaeis guineensis Jacq. | Blood tonic, 100.00 | 0.03 | 3 |
| Eleusine indica (L.) Gaertn. | Pile, 19.57 Cough, 43.47 Malaria, 36.96 | 0.46 | 46 |
| Eleutheranthera ruderalis (Swartz) Sch.-Bip. | Piles, 61.54 Longevity, 38.46 | 0.26 | 26 |
| Emilia coccinea (Sims) G.Don | Foot pain, 59.46 Birth control, 8.11 Purgative, 32.43 | 0.37 | 37 |
| Entandrophragma angolense (Welw.) C.DC. | Piles, 100.00 | 0.15 | 15 |
| Eragrostis namaquennsis Nees ex Schrad. (Synonym: Eragrostis japonica (Thunb.) Trin.) | Stomachache, 100.00 | 0.10 | 10 |
| Erigeron floribundus (Kunth) Sch.Bip. | Scurvy, 100.00 | 0.09 | 9 |
| Erythrina senegalensis DC. | Diabetes, 100.00 | 0.13 | 13 |
| Euphorbia glaucophylla Poir. (Synonym: Euphorbia trinervia Schumach. & Thonn.) | Longevity, 46.94 Malaria, 22.45 Cough, 30.61 | 0.49 | 49 |
| Euphorbia heterophylla L. | Longevity, 100.00 | 0.01 | 1 |
| Ficus benjamina L. | Scurvy, 30.30 Cough, 69.70 | 0.33 | 33 |
| Ficus capensis Thunb. (Synonym: Ficus sur Forssk.) | Hypertension, 26.67 Cough, 73.33 | 0.45 | 45 |
| Ficus exasperata Vahl | Scurvy, 50.00 Cough, 27.27 Hypertension, 22.73 | 0.44 | 44 |
| Ficus polita Vahl | Pimples, 100.00 | 0.06 | 6 |
| Fleurya aestuans (L.) Chew | Cough, 100.00 | 0.18 | 18 |
| Gliricidia sepium (Jacq.) Walp. | Arthritis, 46.15 Hypertension, 53.85 | 0.26 | 26 |
| Glyphaea brevis (Spreng.) Monach. | Ulcer, 100.00 | 0.13 | 13 |
| Gomphrena celosioides Mart. | Pimples, 62.16 Potency, 37.84 | 0.37 | 37 |
| Grewia pubescens P.Beauv. | Hypertension, 100.00 | 0.16 | 16 |
| Harungana madagascariensis Lam. ex Poir. | Anti-snake bite, 100.00 | 0.18 | 18 |
| Heliotropium indicum L. | Erection, 33.33 Piles, 66.67 | 0.27 | 27 |
| Hibiscus rosa-sinensis L. | Cough, 100.00 | 0.10 | 10 |
| Hibiscus surattensis L. | Diabetes, 65.71 Potency, 34.29 | 0.35 | 35 |
| Hippocratea pallens Planch. ex Oliv. (Synonym: Apodostigma pallens (Planch. ex Oliv.) R.Wilczek) | Malaria, 100.00 | 0.17 | 17 |
| Hoslundia opposita Vahl | Ulcer, 100.00 | 0.19 | 19 |
| Hyptis suaveolens (L.) Poit. | Anti-snake bite, 100.00 | 0.22 | 22 |
| Icacina trichantha Oliv. | Curse, 20.90 Potency, 79.10 | 0.67 | 67 |
| Indigofera arrecta A.Rich. | Piles, 61.11 Pregnancy, 38.89 | 0.18 | 18 |
| Indigofera hirsuta L. | Sight, 22.95 Stomachache, 45.90 Purgative, 31.15 | 0.61 | 61 |
| Ipomoea involucrata P.Beauv. (Synonym: Ipomoea pileata Roxb.) | Anti-snake bite, 19.75 Malaria, 19.76 Cough, 60.49 | 0.81 | 81 |
| Jatropha curcas L. | Piles, 83.64 Sight, 16.36 | 0.55 | 55 |
| Jatropha gossypiifolia L. | Piles, 100.00 | 0.40 | 40 |
| Kigelia africana (Lam.) Benth. | Cough, 46.43 Piles, 53.57 | 0.28 | 28 |
| Lantana camara L. | Purgative, 50.00 Nervousness, 7.14 Potency, 42.86 | 0.14 | 14 |
| Lawsonia inermis L. | Malaria, 77.27 Gonorrhoea, 22.73 | 0.44 | 44 |
| Leucaena leucocephala (Lam.) de Wit | Purgative, 100.00 | 0.06 | 6 |
| Luffa cylindrica (L.) M.Roem. | Cramps, 14.00 Fever, 30.00 Purgative, 38.00 Convulsion, 18.00 | 0.50 | 50 |
| Macaranga barteri Müll.Arg. | Easy labour, 42.42 Anti-snake bite, 57.58 | 0.33 | 33 |
| Microdesmis puberula Hook.f. ex Planch. | Easy labour, 100.00 | 0.11 | 11 |
| Mallotus oppositifolius (Geiseler) Müll.Arg. | Stomach problems, 51.61 Malaria, 32.26 Sight, 16.13 | 0.31 | 31 |
| Malvastrum coromandelianum (L.) Garcke | Anti-snake bite, 100.00 | 0.02 | 2 |
| Mangifera indica L. | Malaria, 76.84 Fever, 23.16 | 0.95 | 95 |
| Margaritaria discoidea (Baill.) G.L.Webster | Malaria, 100.00 | 0.23 | 23 |
| Mariscus alternifolius Vahl (Synonym: Cyperus cyperoides (L.) Kuntze) | Jaundice, 33.33 Arthritis, 66.67 | 0.09 | 9 |
| Melanthera scandens (Schumach. & Thonn.) Roberty | Curse, 37.50 Malaria, 62.50 | 0.24 | 24 |
| Merremia pterygocaulos (Choisy) Hallier f. | Foot pain, 80.00 Sight, 20.00 | 0.20 | 20 |
| Mezoneuron benthamianum (Synonym: Caesalpinia benthamiana (Baill.) Herend. & Zarucchi) | Piles, 100.00 | 0.25 | 25 |
| Mimosa pudica L. | Erection, 84.00 Anti-snake bite, 16.00 | 0.25 | 25 |
| Morinda lucida Benth. | Malaria, 62.86 Fever, 24.29 Jaundice, 12.85 | 0.70 | 70 |
| Moringa oleifera Lam. | Cough, 100.00 | 0.27 | 27 |
| Myrianthus arboreus P.Beauv. | Neck pain, 70.59 Cough, 29.41 | 0.17 | 17 |
| Nauclea latifolia Sm. (Synonym: Sarcocephalus latifolius (Sm.) E.A.Bruce) | Malaria, 50.00 Pimples, 27.27 Diabetes, 22.73 | 0.66 | 66 |
| Newbouldia laevis (P.Beauv.) Seem. | Diabetes, 40.30 Measles, 25.37 Worm-expellant, 10.45 Jaundice, 23.88 | 0.67 | 67 |
| Ocimum gratissimum L. | Piles, 38.46 Purgative, 46.15 Cough, 15.39 | 0.78 | 78 |
| Panicum scandens (Schrad. ex Schult.) Trin. (Synonym: Setaria scandens Schrad.) | Malaria, 100.00 | 0.21 | 21 |
| Passiflora foetida L. | Foot pain, 80.65 Sight, 19.35 | 0.31 | 31 |
| Paullinia pinnata L. | Aphrodisiac, 52.17 Piles, 47.83 | 0.23 | 23 |
| Perotis indica (L.) Kuntze | Blood tonic,100.00 | 0.03 | 3 |
| Persea americana Mill. | Longevity, 100.00 | 0.14 | 14 |
| Phaulopsis falcisepala C.B.Clarke (Synonym: Phaulopsis ciliata (Willd.) Hepper) | Malaria, 100.00 | 0.15 | 15 |
| Phyllanthus amarus Schumach. & Thonn. | Fever, 23.40 Pregnancy, 36.18 Immune booster, 17.02 Cough, 23.40 | 0.47 | 47 |
| Phyllanthus niruri L. | Foot pain, 57.89 Sight, 42.11 | 0.19 | 19 |
| Physalis angulata L. | Skin rashes, 76.00 Piles, 24.00 | 0.50 | 50 |
| Piliostigma thonningii (Schum.) Milne-Redh. (Synonym: Bauhinia thonningii Schum.) | Potency, 100.00 | 0.06 | 6 |
| Pinus caribaea Morelet | Cough, 100.00 | 0.05 | 5 |
| Pleioceras barteri Baill. | Neck pain, 38.89 Stomachache, 61.11 | 0.18 | 18 |
| Polyalthia suaveolens Engl. & Diels (Synonym: Greenwayodendron suaveolens (Engl. & Diels) Verdc.) | Cough, 100.00 | 0.02 | 2 |
| Portulaca oleracea L. | Cough, 55.56 Anti-snake bite, 44.44 | 0.18 | 18 |
| Psidium guajava L. | Fever, 22.50 Stomachache, 77.50 | 0.40 | 40 |
| Rauvolfia vomitoria Afzel. | Malaria, 16.13 Insanity, 29.03 Hypertension, 22.58 Muscle relaxant, 16.13 Cough, 16.13 | 0.62 | 62 |
| Ricinus communis L. | Divinity, 44.83 Sight, 55.17 | 0.29 | 29 |
| Scoparia dulcis L. | Black coated tongue, 30.77 Birth control, 69.23 | 0.13 | 13 |
| Secamone afzelii (Roem. & Schult.) K.Schum. | Immune booster, 100.00 | 0.26 | 26 |
| Securinega virosa (Roxb. ex Willd.) Baill. (Synonym: Flueggea virosa (Roxb. ex Willd.) Royle) | Typhoid, 47.83 Pregnancy, 28.26 Immune booster, 23.91 | 0.46 | 46 |
| Senna hirsuta (L.) H.S.Irwin & Barneby | Cough, 37.04 Purgative, 62.96 | 0.27 | 27 |
| Senna obtusifolia (L.) H.S.Irwin & Barneby | Scurvy, 39.02 Cough, 60.98 | 0.41 | 41 |
| Senna podocarpa (Guill. & Perrottet) Lock | Stomach problem, 100.00 | 0.16 | 16 |
| Senna siamea (Lamarck) H.S.Irwin & Barneby | Immune booster, 100.00 | 0.11 | 11 |
| Senna tora (L.) Roxb. | Potency, 33.33 Sight, 19.44 Malaria, 36.12 Divinity, 11.11 | 0.36 | 36 |
| Sesamum indicum L. | Potency, 100.00 | 0.03 | 3 |
| Sesamum radiatum Schumach. & Thonn. | Potency, 100.00 | 0.06 | 6 |
| Sida acuta Burm.f. | Fibroids, 38.89 Sight, 61.11 | 0.18 | 18 |
| Sida cordifolia L. | Cough, 100.00 | 0.12 | 12 |
| Sida linifolia Juss. ex Cav. | Scurvy, 58.82 Pimples, 41.18 | 0.17 | 17 |
| Smilax kraussiana Meisn. (Synonym: Smilax anceps Willd.) | Erection, 100.00 | 0.12 | 12 |
| Solanum nigrum L. (Synonym: Solanum americanum Mill.) | Diabetes, 46.87 Cough, 53.13 | 0.32 | 32 |
| Solanum torvum Sw. | Pimples, 22.22 Potency, 41.67 Hypertension, 36.11 | 0.36 | 36 |
| Solenostemon monostachyus (P.Beauv.) Briq. (Synonym: Plectranthus monostachyus (P.Beauv.) B.J.Pollard) | Piles, 26.92 Malaria, 34.62 Purgative, 17.31 Potency, 21.15 | 0.52 | 52 |
| Sorghum bicolor (L.) Moench | Malaria, 100.00 | 0.07 | 7 |
| Sphenocentrum jollyanum Pierre | Deworming, 45.16 Malaria, 19.36 Fever, 35.48 | 0.31 | 31 |
| Spigellia anthelmia L. | Diabetes, 38.46 Piles, 61.54 | 0.26 | 26 |
| Spondias mombin L. | Penile erection, 40.00 Diabetes, 28.57 Anti-snake bite, 14.29 Insomnia, 17.14 | 0.35 | 35 |
| Sporobolus indicus (L.) R.Br. | Diabetes, 60.87 Purgative, 39.13 | 0.23 | 23 |
| Stachytarpheta indica (L.) Vahl | Erection, 20.00 Hypertension, 80.00 | 0.20 | 20 |
| Sterculia tragacantha Lindl. | Diabetes, 100.00 | 0.13 | 13 |
| Synedrella nodiflora (L.) Gaertn. | Potency, 55.55 Sight, 5.56 Longevity, 27.78 Malaria, 11.11 | 0.18 | 18 |
| Syzygium guineense (Willd.) DC. | Diabetes, 100.00 | 0.12 | 12 |
| Talinum triangulare (Jacq.) Willd. (Synonym: Talinum fruticosum (L.) Juss.) | Blood tonic, 86.36 Malaria, 13.64 | 0.44 | 44 |
| Tapinanthus globiferous (A.Rich.) Tiegh. | Fibroid, 100.00 | 0.11 | 11 |
| Telfairia occidentalis Hook.f. | Blood tonic, 79.55 Hypertension, 20.45 | 0.44 | 44 |
| Terminalia ivorensis A.Chev. | Divinity, 100.00 | 0.09 | 9 |
| Tetracera alnifolia Willd. | Fibroid, 100.00 | 0.05 | 5 |
| Thaumatococcus daniellii (Benn.) Benth. | Ulcer, 75.38 Food sweetener, 24.62 | 0.65 | 65 |
| Thevetia peruviana (Pers.) K.Schum. | Purgative, 61.54 Pimples, 17.95 Cough, 20.51 | 0.39 | 39 |
| Tithonia diversifolia (Hemsl.) A.Gray | Malaria, 86.15 Piles, 13.85 | 0.65 | 65 |
| Trichilia monadelpha (Thonn.) J.J.de Wilde | Insomnia, 100.00 | 0.02 | 2 |
| Tridax procumbens (L.) L. | Ulcer, 22.22 Foot pain, 33.33 Malaria, 19.44 Hypertension, 25.01 | 0.36 | 36 |
| Triumfetta cordifolia A.Rich. | Easy labour, 64.29 Birth control, 35.71 | 0.14 | 14 |
| Urena lobata L. var. var. glauca (Blume) Borss. Waalk. | Potency, 100.00 | 0.15 | 15 |
| Urena lobata L. | Birth control, 18.64 Rheumatism, 16.95 Wound, 28.81 Diarrhoea, 22.03 Stomachache, 13.57 | 0.59 | 59 |
| Vernonia amygdalina Delile | Diabetes, 18.99 Malaria, 39.24 Oral hygiene, 21.52 Diarrhoea, 20.25 | 0.79 | 79 |
| Vernonia cinerea (L.) Less. (Synonym: Cyanthillium cinereum (L.) H.Rob. | Asthma, 28.57 Bronchitis, 22.45 Cold, 26.53 Stomachache, 22.45 | 0.49 | 49 |
| Vitex doniana Sweet | Dysentery, 36.20 Diarrhoea, 24.14 Hypertension, 24.14 Indigestion, 15.52 | 0.58 | 58 |
| Waltheria indica L. | Wound, 13.98 Blood tonic, 33.33 Ulcer, 17.21 Cold, 10.75 Cough, 24.73 | 0.93 | 93 |
| Zingiber officinale Roscoe | Ulcer, 24.14 Indigestion, 27.59 Cough, 36.78 Flu, 11.49 | 0.87 | 87 |
| S/n | Disease Category | Number of Species | Use Citation | ICF |
|---|---|---|---|---|
| 1 | Respiratory-related ailments | 46 | 842 | 0.95 |
| 2 | Stomach-related ailments | 50 | 917 | 0.95 |
| 3 | Infectious diseases | 21 | 320 | 0.94 |
| 4 | Malaria and other fevers | 49 | 944 | 0.95 |
| 5 | Cardiovascular-related diseases | 31 | 496 | 0.94 |
| 6 | Male reproductive-related issues | 27 | 304 | 0.91 |
| 7 | Female reproductive-related issues | 25 | 293 | 0.92 |
| 8 | Vision-related issues | 18 | 224 | 0.92 |
| 9 | Foot pain, neck pain, rheumatism, arthritis | 16 | 266 | 0.94 |
| 10 | Oral hygiene, black coated tongue, toothache | 5 | 53 | 0.92 |
| 11 | Divinity, curse (spiritual-related) | 10 | 100 | 0.91 |
| 12 | Anti-snake bite, de-wormer, worm-expellant | 10 | 118 | 0.92 |
| 13 | Cirrhosis, scurvy, blood tonic, longevity, immune booster | 31 | 404 | 0.93 |
| 14 | Insomnia, insanity, convulsion, nervousness, muscle relaxant | 7 | 50 | 0.88 |
| Feature | Frequency (n) |
|---|---|
| Age group | |
| 30–39 | 2 |
| 40–49 | 28 |
| 50–59 | 34 |
| 60–69 | 18 |
| 70–79 | 12 |
| 80 and above | 6 |
| Gender | |
| Male | 89 |
| Female | 11 |
| Marital status | |
| Widower/widow | 7 |
| Single | 2 |
| Married | 91 |
| Religion status | |
| African traditionalist | 60 |
| Christianity | 12 |
| Islam | 28 |
| Formal education level | |
| None | 7 |
| Primary | 79 |
| Secondary | 12 |
| Tertiary | 2 |
| Occupation-type | |
| Farmer | 29 |
| Herbalist | 52 |
| Trader | 19 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Lawal, I.O.; Rafiu, B.O.; Ale, J.E.; Majebi, O.E.; Aremu, A.O. Ethnobotanical Survey of Local Flora Used for Medicinal Purposes among Indigenous People in Five Areas in Lagos State, Nigeria. Plants 2022, 11, 633. https://doi.org/10.3390/plants11050633
Lawal IO, Rafiu BO, Ale JE, Majebi OE, Aremu AO. Ethnobotanical Survey of Local Flora Used for Medicinal Purposes among Indigenous People in Five Areas in Lagos State, Nigeria. Plants. 2022; 11(5):633. https://doi.org/10.3390/plants11050633
Chicago/Turabian StyleLawal, Ibraheem Oduola, Basirat Olabisi Rafiu, Joy Enitan Ale, Onuyi Emmanuel Majebi, and Adeyemi Oladapo Aremu. 2022. "Ethnobotanical Survey of Local Flora Used for Medicinal Purposes among Indigenous People in Five Areas in Lagos State, Nigeria" Plants 11, no. 5: 633. https://doi.org/10.3390/plants11050633
APA StyleLawal, I. O., Rafiu, B. O., Ale, J. E., Majebi, O. E., & Aremu, A. O. (2022). Ethnobotanical Survey of Local Flora Used for Medicinal Purposes among Indigenous People in Five Areas in Lagos State, Nigeria. Plants, 11(5), 633. https://doi.org/10.3390/plants11050633







