Exploring the Spatial Relationship Between Severe Depression, COVID-19 Case Rates, and Vaccination Rates in US Counties: A Spatial Analysis Across Two Time Periods
Abstract
1. Introduction
2. Data and Methods
2.1. Spatial Statistics Models in Public Health Research
2.1.1. Severe Depression Disorder Data
2.1.2. COVID-19 Case Rates and Vaccination Rate Data
2.1.3. Control Variables: Weather, Demographic, and Socioeconomic Data
2.2. Spatial Statistics Models Used for Analysis
2.2.1. Global Model and Local Spatial Autocorrelation
2.2.2. Spatial Regression Models (MGWR)
3. Results
3.1. Descriptive Statistics of the Study Variables
3.2. Summary of Statistic Models
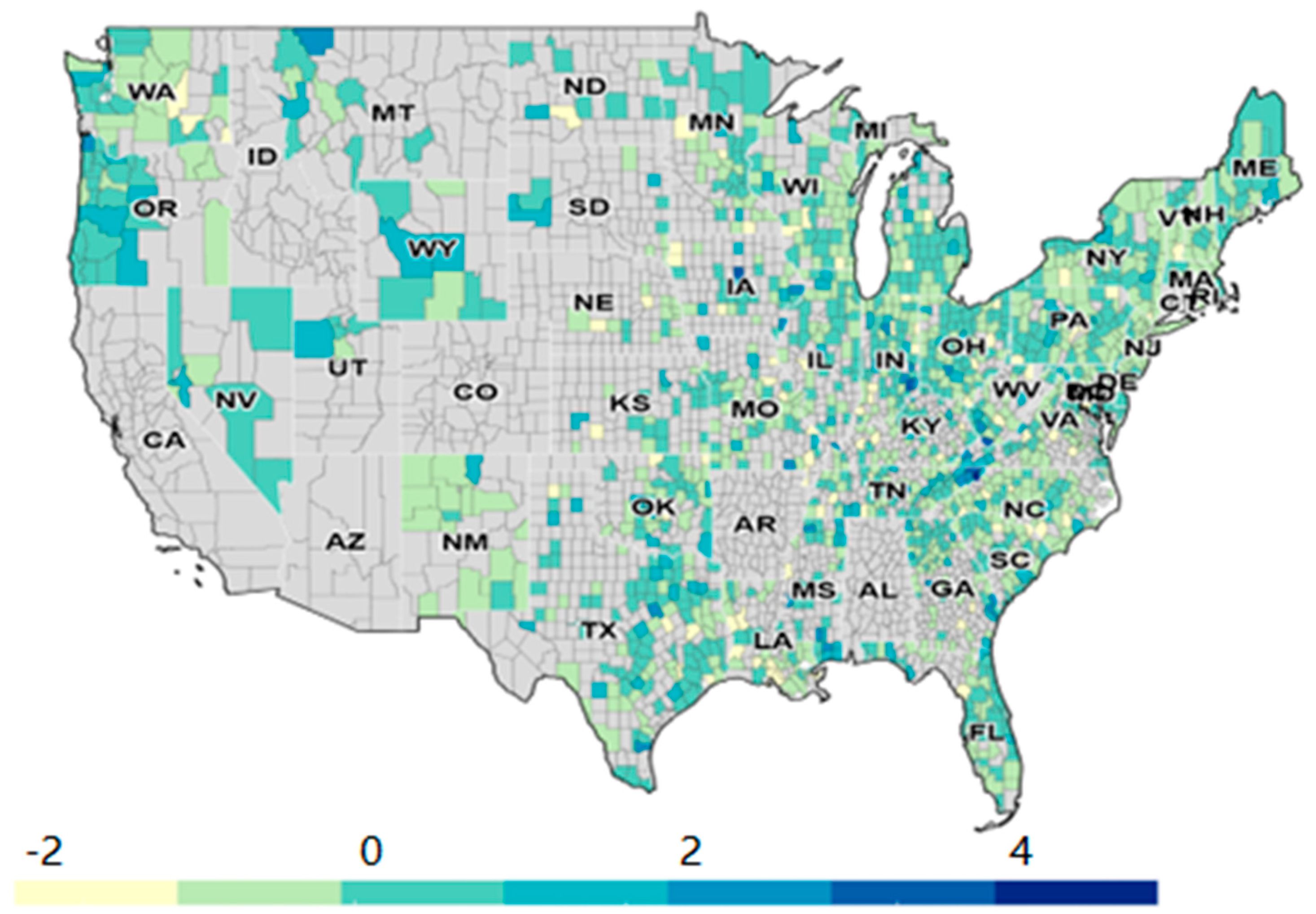
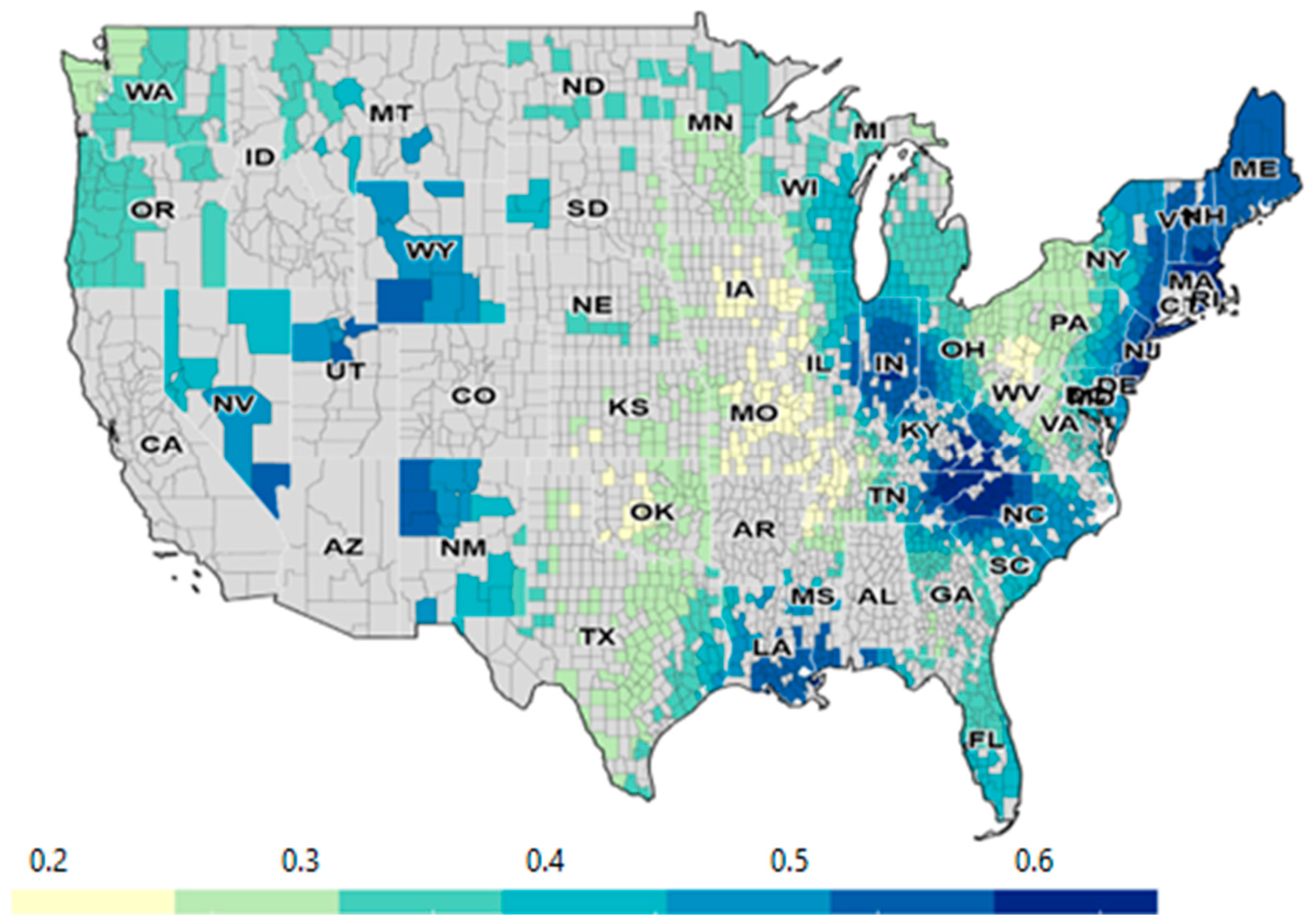
3.3. Spatial Patterns of Severe Depression and Its Relationship with COVID-19 Case Rates and Vaccination Rates
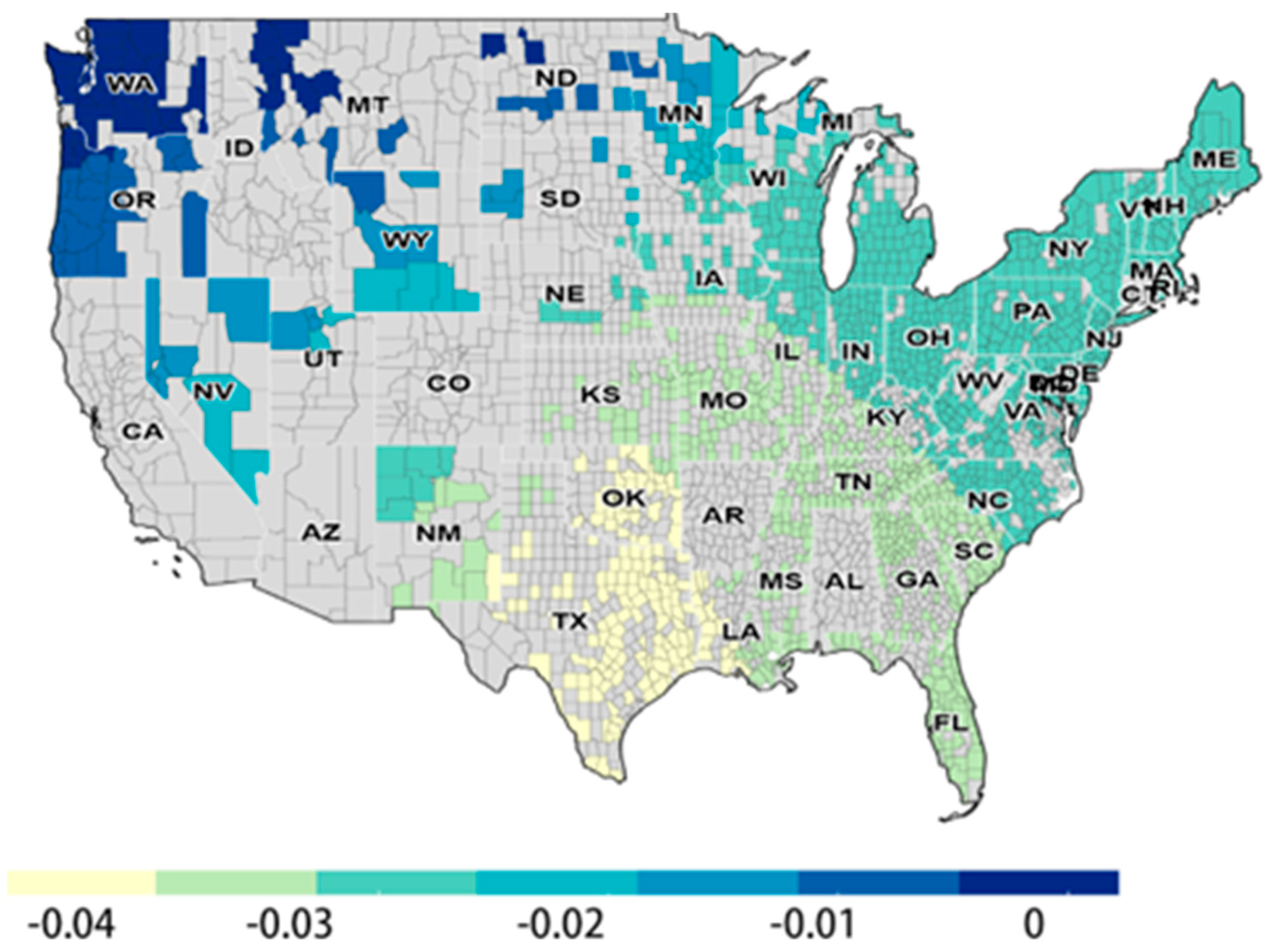
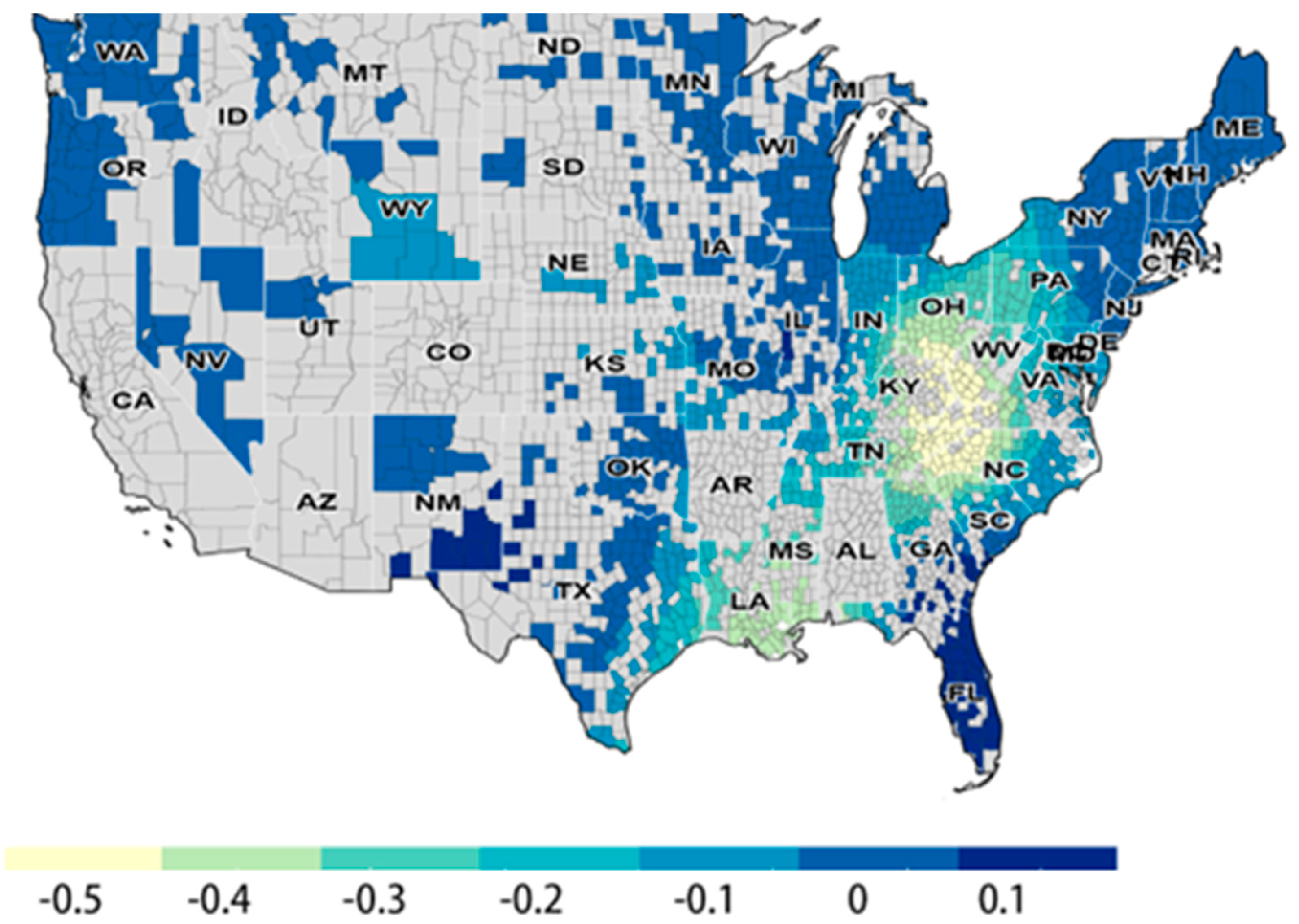
3.4. Influence of Control Variables on the Spatial Relationship
4. Discussion
4.1. COVID-19 Case Rates, Vaccination, and Severe Depression
4.2. Spatial Interpretation
4.3. Other Contributing Factors
4.4. Comparison with Pre-Pandemic Studies
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Data Availability Statement
Conflicts of Interest
References
- Dragioti, E.; Li, H.; Tsitsas, G.; Lee, K.H.; Choi, J.; Kim, J.; Choi, Y.J.; Tsamakis, K.; Estradé, A.; Agorastos, A.; et al. A large-scale meta-analytic atlas of mental health problems prevalence during the COVID-19 early pandemic. J. Med. Virol. 2022, 94, 1935–1949. [Google Scholar] [CrossRef]
- Racine, N.; McArthur, B.A.; Cooke, J.E.; Eirich, R.; Zhu, J.; Madigan, S. Global Prevalence of Depressive and Anxiety Symptoms in Children and Adolescents During COVID-19: A Meta-analysis. JAMA Pediatr 2021, 175, 1142–1150. [Google Scholar] [CrossRef] [PubMed]
- Zhang, S.X.; Batra, K.; Xu, W.; Liu, T.; Dong, R.K.; Yin, A.; Delios, A.Y.; Chen, B.Z.; Chen, R.Z.; Miller, S.; et al. Mental disorder symptoms during the COVID-19 pandemic in Latin America—A systematic review and meta-analysis. Epidemiol. Psychiatr Sci. 2022, 31, e23. [Google Scholar] [CrossRef]
- Zhang, S.X.; Miller, S.O.; Xu, W.; Yin, A.; Chen, B.Z.; Delios, A.; Dong, R.K.; Chen, R.Z.; McIntyre, R.S.; Wan, X.; et al. Meta-analytic evidence of depression and anxiety in Eastern Europe during the COVID-19 pandemic. Eur. J. Psychotraumatol. 2022, 13, 2000132. [Google Scholar] [CrossRef]
- Stein, D.J.; Phillips, K.A.; Bolton, D.; Fulford, K.W.M.; Sadler, J.Z.; Kendler, K.S. What is a mental/psychiatric disorder? From DSM-IV to DSM-V. Psychol. Med. 2010, 40, 1759–1765. [Google Scholar] [CrossRef]
- Kroenke, K.; Spitzer, R.L.; Williams, J.B. The PHQ-9: Validity of a brief depression severity measure. J. Gen. Intern. Med. 2001, 16, 606–613. [Google Scholar] [CrossRef]
- Vai, B.; Mazza, M.G.; Colli, C.D.; Foiselle, M.; Allen, B.; Benedetti, F.; Borsini, A.; Dias, M.C.; Tamouza, R.; Leboyer, M.; et al. Mental disorders and risk of COVID-19-related mortality, hospitalisation, and intensive care unit admission: A systematic review and meta-analysis. Lancet Psychiatry 2021, 8, 797–812. [Google Scholar] [CrossRef]
- Ceban, F.; Nogo, D.; Carvalho, I.P.; Lee, Y.; Nasri, F.; Xiong, J.; Lui, L.M.W.; Subramaniapillai, M.; Gill, H.; Liu, R.N.; et al. Association Between Mood Disorders and Risk of COVID-19 Infection, Hospitalization, and Death: A Systematic Review and Meta-analysis. JAMA Psychiatry 2021, 78, 1079–1091. [Google Scholar] [CrossRef]
- Dutta, A. COVID-19 waves: Variant dynamics and control. Sci. Rep. 2022, 12, 9332. [Google Scholar] [CrossRef]
- Centers for Disease Control and Prevention. COVID-19 Vaccines. Available online: https://www.cdc.gov/covid/vaccines/index.html (accessed on 1 August 2023).
- Mojtabai, R. COVID-19 Vaccination and Mental Health Distress. J. Gen. Intern. Med. 2022, 37, 1020–1021. [Google Scholar] [CrossRef]
- Koltai, J.; Raifman, J.; Bor, J.; McKee, M.; Stuckler, D. COVID-19 Vaccination and Mental Health: A Difference-In-Difference Analysis of the Understanding America Study. Am. J. Prev. Med. 2022, 62, 679–687. [Google Scholar] [CrossRef] [PubMed]
- Chen, S.; Aruldass, A.R.; Cardinal, R.N. Mental health outcomes after SARS-CoV-2 vaccination in the United States: A national cross-sectional study. J. Affect. Disord. 2022, 298, 396–399. [Google Scholar] [CrossRef] [PubMed]
- Ceban, F.; Kulzhabayeva, D.; Rodrigues, N.B.; Di Vincenzo, J.D.; Gill, H.; Subramaniapillai, M.; Lui, L.M.; Cao, B.; Mansur, R.B.; Ho, R.C.; et al. COVID-19 vaccination for the prevention and treatment of long COVID: A systematic review and meta-analysis. Brain Behav. Immun. 2023, 111, 211–229. [Google Scholar] [CrossRef] [PubMed]
- Renaud-Charest, O.; Lui, L.M.; Eskander, S.; Ceban, F.; Ho, R.; Di Vincenzo, J.D.; Rosenblat, J.D.; Lee, Y.; Subramaniapillai, M.; McIntyre, R.S. Onset and frequency of depression in post-COVID-19 syndrome: A systematic review. J. Psychiatr. Res. 2021, 144, 129–137. [Google Scholar] [CrossRef]
- Chou, W.S.; Budenz, A. Considering Emotion in COVID-19 Vaccine Communication: Addressing Vaccine Hesitancy and Fostering Vaccine Confidence. Health Commun. 2020, 35, 1718–1722. [Google Scholar] [CrossRef]
- Wang, S.; Quan, L.; Chavarro, J.E.; Slopen, N.; Kubzansky, L.D.; Koenen, K.C.; Kang, J.H.; Weisskopf, M.G.; Branch-Elliman, W.; Roberts, A.L. Associations of Depression, Anxiety, Worry, Perceived Stress, and Loneliness Prior to Infection With Risk of Post–COVID-19 Conditions. JAMA Psychiatry 2022, 79, 1081–1091. [Google Scholar] [CrossRef]
- Ford, B.N.; Savitz, J. Depression, aging, and immunity: Implications for COVID-19 vaccine immunogenicity. Immun. Ageing 2022, 19, 32. [Google Scholar] [CrossRef]
- Mollalo, A.; Vahedi, B.; Rivera, K.M. GIS-based spatial modeling of COVID-19 incidence rate in the continental United States. Sci. Total Environ. 2020, 728, 138884. [Google Scholar] [CrossRef]
- Mollalo, A.; Tatar, M. Spatial Modeling of COVID-19 Vaccine Hesitancy in the United States. Int. J. Env. Res Public Health 2021, 18, 9488. [Google Scholar] [CrossRef]
- Iyanda, A.E.; Adeleke, R.; Lu, Y.; Osayomi, T.; Adaralegbe, A.; Lasode, M.; Chima-Adaralegbe, N.J.; Osundina, A.M. A retrospective cross-national examination of COVID-19 outbreak in 175 countries: A multiscale geographically weighted regression analysis (11 January–28 June 2020). J. Infect. Public Health 2020, 13, 1438–1445. [Google Scholar] [CrossRef]
- Dong, E.; Du, H.; Gardner, L. An interactive web-based dashboard to track COVID-19 in real time. Lancet Infect. Dis. 2020, 20, 533–534. [Google Scholar] [CrossRef] [PubMed]
- Ali, K.; Partridge, M.D.; Olfert, M.R. Can geographically weighted regressions improve regional analysis and policy making? Int. Reg. Sci. Rev. 2007, 30, 300–329. [Google Scholar] [CrossRef]
- Brunsdon, C.; Fotheringham, S.; Charlton, M. Geographically Weighted Regression. J. R. Stat. Soc. Ser. D 1998, 47, 431–443. [Google Scholar] [CrossRef]
- Waller, L.A.; Zhu, L.; Gotway, C.A.; Gorman, D.M.; Gruenewald, P.J. Quantifying geographic variations in associations between alcohol distribution and violence: A comparison of geographically weighted regression and spatially varying coefficient models. Stoch. Env. Res. Risk Assess. 2007, 21, 573–588. [Google Scholar] [CrossRef]
- Foody, G.M. Spatial nonstationarity and scale-dependency in the relationship between species richness and environmental determinants for the sub-Saharan endemic avifauna. Glob. Ecol. Biogeogr. 2004, 13, 315–320. [Google Scholar] [CrossRef]
- Fotheringham, A.S.; Brunsdon, C.; Charlton, M. Geographically Weighted Regression: The Analysis of Spatially Varying Relationships; John Wiley & Sons: Hoboken, NJ, USA, 2003. [Google Scholar]
- Fotheringham, S.; Charlton, M.; Brunsdon, C. Spatial variations in school performance: A local analysis using geographically weighted regression. Geogr. Environ. Model. 2001, 5, 43–66. [Google Scholar] [CrossRef]
- Wheeler, D.; Tiefelsdorf, M. Multicollinearity and correlation among local regression coefficients in geographically weighted regression. J. Geogr. Syst. 2005, 7, 161–187. [Google Scholar] [CrossRef]
- Fotheringham, A.S.; Yang, W.; Kang, W. Multiscale geographically weighted regression (MGWR). Ann. Am. Assoc. Geogr. 2017, 107, 1247–1265. [Google Scholar] [CrossRef]
- Oshan, T.M.; Li, Z.; Kang, W.; Wolf, L.J.; Fotheringham, A.S. mgwr: A Python implementation of multiscale geographically weighted regression for investigating process spatial heterogeneity and scale. ISPRS Int. J. Geo-Inf. 2019, 8, 269. [Google Scholar] [CrossRef]
- Kim, S.Y.; Bang, M.; Wee, J.H.; Min, C.; Yoo, D.M.; Han, S.-M.; Kim, S.; Choi, H.G. Short-and long-term exposure to air pollution and lack of sunlight are associated with an increased risk of depression: A nested case-control study using meteorological data and national sample cohort data. Sci. Total Environ. 2021, 757, 143960. [Google Scholar] [CrossRef]
- Wang, J.; Wei, Z.; Yao, N.; Li, C.; Sun, L. Association Between Sunlight Exposure and Mental Health: Evidence from a Special Population Without Sunlight in Work. Risk Manag. Healthc. Policy 2023, 16, 1049–1057. [Google Scholar] [CrossRef]
- Sun, Y.; Wu, Y.; Fan, S.; Santo, T.D.; Li, L.; Jiang, X.; Li, K.; Wang, Y.; Tasleem, A.; Krishnan, A.; et al. Comparison of mental health symptoms before and during the COVID-19 pandemic: Evidence from a systematic review and meta-analysis of 134 cohorts. BMJ 2023, 380, e074224. [Google Scholar] [CrossRef] [PubMed]
- Cummings, J.R.; Wen, H.; Ko, M.; Druss, B.G. Race/ethnicity and geographic access to Medicaid substance use disorder treatment facilities in the United States. JAMA Psychiatry 2014, 71, 190–196. [Google Scholar] [CrossRef]
- Choi, E.P.H.; Hui, B.P.H.; Wan, E.Y.F. Depression and Anxiety in Hong Kong during COVID-19. Int. J. Environ. Res. Public Health 2020, 17, 3740. [Google Scholar] [CrossRef] [PubMed]
- Ettman, C.K.; Abdalla, S.M.; Cohen, G.H.; Sampson, L.; Vivier, P.M.; Galea, S. Prevalence of Depression Symptoms in US Adults Before and During the COVID-19 Pandemic. JAMA Netw. Open 2020, 3, e2019686. [Google Scholar] [CrossRef] [PubMed]
- Hyland, P.; Shevlin, M.; McBride, O.; Murphy, J.; Karatzias, T.; Bentall, R.P.; Martinez, A.; Vallières, F. Anxiety and depression in the Republic of Ireland during the COVID-19 pandemic. Acta Psychiatr. Scand. 2020, 142, 249–256. [Google Scholar] [CrossRef]
- Tsampasian, V.; Elghazaly, H.; Chattopadhyay, R.; Debski, M.; Naing, T.K.P.; Garg, P.; Clark, A.; Ntatsaki, E.; Vassiliou, V.S. Risk Factors Associated With Post-COVID-19 Condition: A Systematic Review and Meta-analysis. JAMA Intern. Med. 2023, 183, 566–580. [Google Scholar] [CrossRef]
- Davis, H.E.; McCorkell, L.; Vogel, J.M.; Topol, E.J. Long COVID: Major findings, mechanisms and recommendations. Nat. Rev. Microbiol. 2023, 21, 133–146. [Google Scholar] [CrossRef]
- Sun, Y.; Kong, Z.; Song, Y.; Liu, J.; Wang, X. The validity and reliability of the PHQ-9 on screening of depression in neurology: A cross sectional study. BMC Psychiatry 2022, 22, 98. [Google Scholar] [CrossRef]
- Vallée, A. Heterogeneity of the COVID-19 Pandemic in the United States of America: A Geo-Epidemiological Perspective. Front. Public Health 2022, 10, 818989. [Google Scholar] [CrossRef]
- Igoe, M.; Das, P.; Lenhart, S.; Lloyd, A.L.; Luong, L.; Tian, D.; Lanzas, C.; Odoi, A. Geographic disparities and predictors of COVID-19 hospitalization risks in the St. Louis Area, Missouri (USA). BMC Public Health 2022, 22, 321. [Google Scholar] [CrossRef]
- Hsiang, S.; Allen, D.; Annan-Phan, S.; Bell, K.; Bolliger, I.; Chong, T.; Druckenmiller, H.; Huang, L.Y.; Hultgren, A.; Krasovich, E.; et al. The effect of large-scale anti-contagion policies on the COVID-19 pandemic. Nature 2020, 584, 262–267. [Google Scholar] [CrossRef]
- Health Workforce Shortage Areas. Available online: https://data.hrsa.gov/topics/health-workforce/shortage-areas (accessed on 1 August 2023).
- Grossman, E.R.; Benjamin-Neelon, S.E.; Sonnenschein, S. Alcohol consumption during the COVID-19 pandemic: A cross-sectional survey of US adults. Int. J. Environ. Res. Public Health 2020, 17, 9189. [Google Scholar] [CrossRef]
- Barbosa, C.; Cowell, A.J.; Dowd, W.N. Alcohol consumption in response to the COVID-19 pandemic in the United States. J. Addict. Med. 2021, 15, 341–344. [Google Scholar] [CrossRef]
- Snell-Rood, C.; Hauenstein, E.; Leukefeld, C.; Feltner, F.; Marcum, A.; Schoenberg, N. Mental health treatment seeking patterns and preferences of Appalachian women with depression. Am. J. Orthopsychiatry 2017, 87, 233. [Google Scholar] [CrossRef]
- Dotson, T.; Derringer, J.; Rose, L.H.; Vanderford, N.L.; Hinkle, A.; Cormier, L.E. An investigation into the prevalence and perceptions of mental health disorders in Appalachian West Virginia. Discov. Ment. Health 2025, 5, 80. [Google Scholar] [CrossRef] [PubMed]
- Shadrina, M.; Bondarenko, E.A.; Slominsky, P.A. Genetics factors in major depression disease. Front. Psychiatry 2018, 9, 334. [Google Scholar] [CrossRef] [PubMed]
- Gonçalves, L.C.; Endrass, J.; Rossegger, A.; Dirkzwager, A.J. A longitudinal study of mental health symptoms in young prisoners: Exploring the influence of personal factors and the correctional climate. BMC Psychiatry 2016, 16, 91. [Google Scholar] [CrossRef] [PubMed]
- Velten, J.; Lavallee, K.L.; Scholten, S.; Meyer, A.H.; Zhang, X.C.; Schneider, S.; Margraf, J. Lifestyle choices and mental health: A representative population survey. BMC psychology 2014, 2, 58. [Google Scholar] [CrossRef]
- Bourmistrova, N.W.; Solomon, T.; Braude, P.; Strawbridge, R.; Carter, B. Long-term effects of COVID-19 on mental health: A systematic review. J. Affect. Disord. 2022, 299, 118–125. [Google Scholar] [CrossRef]
- Bains, N.; Abdijadid, S. Major depressive disorder. In StatPearls; StatPearls Publishing: Treasure Island, FL, USA, 2020. [Google Scholar]
- Levis, B.; Benedetti, A.; Ioannidis, J.P.; Sun, Y.; Negeri, Z.; He, C.; Thombs, B.D. Patient Health Questionnaire-9 scores do not accurately estimate depression prevalence: Individual participant data meta-analysis. J. Clin. Epidemiol. 2020, 122, 115–128. [Google Scholar] [CrossRef]
- Sundaram-Stukel, R.; Davidson, R.J. Associational and plausible causal effects of COVID-19 public health policies on economic and mental distress. arXiv 2021, arXiv:2112.11564. [Google Scholar] [CrossRef]
- American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorderss, 5th ed.; Text Rev.; American Psychiatric Association: Washington, DC, USA, 2022. [Google Scholar]

| Variable Name | Detail | Timestamps | Spatial Resolution | Source |
|---|---|---|---|---|
| severe_depression_per_100K * | Incidence of severe depression disorder per 100k population | 2022 | County | Mental Health America (MHA) |
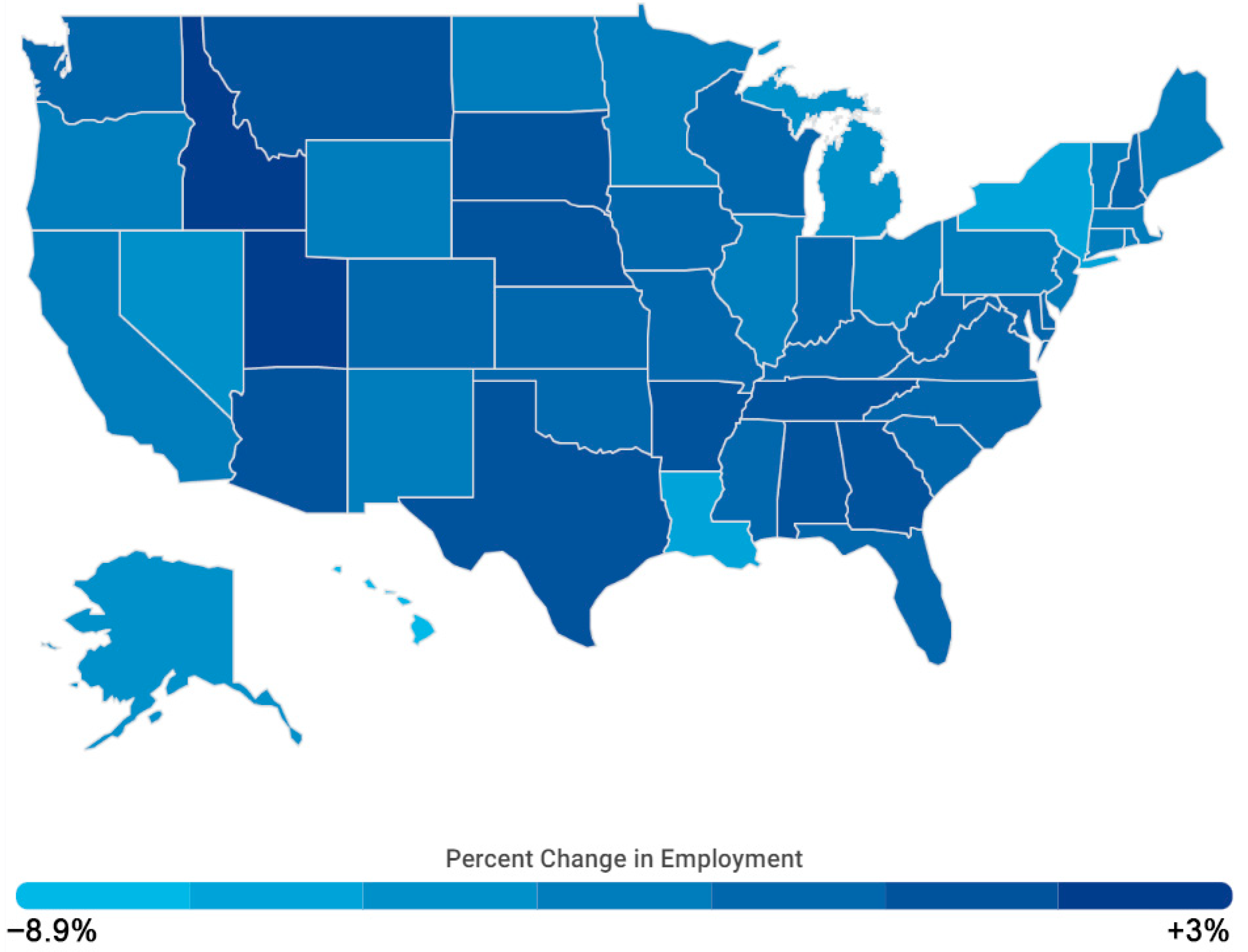
| 2dose_Vac_Complete_5PlusPop_Pct (%) ** | Change in the percentage of population over age 5 that received two doses of COVID-19 vaccine from last year | 2021, 2022 | County | Centers for Disease Control and Prevention (CDC) |
| covid_case_per100k ** | Number of COVID-19 cases per 100k population | 2021,2022 | County | Johns Hopkins University |
| Age_524_pct (%) | Percentage of population age between 5 and 24 | 2021 | County | US Census |
| Avg Daily Sunlight (KJ/m2) | Average daily sunlight power | - | County | North America Land Data Assimilation System (NLDAS) |
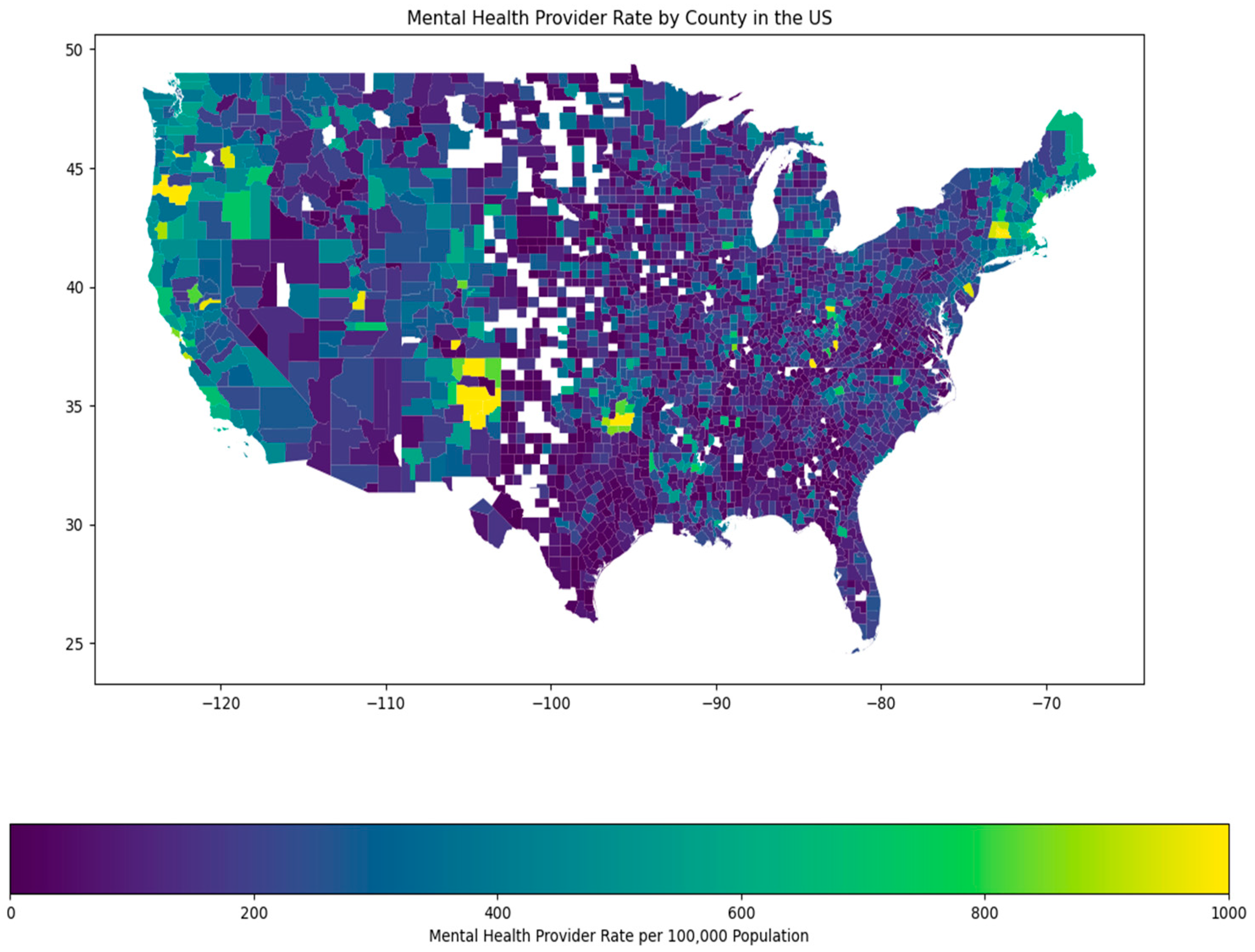
| Mental Health Provider Rate_log | Mental health providers per 100k population (logged) | 2021 | County | Centers for Medicare and Medicaid Services (CMS) |
| pctExcessiveDrinking_log | Percentage of adults reporting binge or heavy drinking (age-adjusted, logged) | 2019 | County | Behavioral Risk Factor Surveillance System |
| Unemployment_rate (%) | The number of unemployed divided by the labor force | 2021 | County | U.S. Bureau of Labor Statistics |
| Variable Name | Time | Mean | Min | Median | Max | Std. |
|---|---|---|---|---|---|---|
| severe_depression_per_100K | 2022 | 40.97 | 12.38 | 39.71 | 118.54 | 12.08 |
| 2dose_Vac_Complete_5PlusPop_Pct | 2021 | 53.53 | 14.10 | 53.30 | 94.20 | 12.46 |
| 2022 | 6.04 | −39.00 | 5.00 | 32.50 | 4.45 | |
| covid_case_per100k | 2021 | 11,051.54 | 2833.33 | 11,131.09 | 21,032.36 | 2165.84 |
| 2022 | 12,669.73 | 1749.78 | 12,309.26 | 30,513.09 | 3290.59 | |
| Age_524_pct | 2021 | 0.25 | 0.08 | 0.25 | 0.45 | 0.04 |
| Avg Daily Sunlight | - | 16,317.22 | 12,306.63 | 15,798.31 | 21,701.97 | 1904.41 |
| Mental Health Provider Rate | 2021 | 196.02 | 4.00 | 155.50 | 2408.00 | 166.67 |
| pctExcessiveDrinking | 2019 | 19.26 | 7.00 | 19.00 | 30.00 | 3.16 |
| Unemployment_rate | 2021 | 4.77 | 1.80 | 4.50 | 16.20 | 1.49 |
| Variable Name | Model 1 | Model 2 | Model 3 | |||
|---|---|---|---|---|---|---|
| Coef. | Coef. | Med. Coef. | Min. Coef. | Max. Coef. | Bandwidth | |
| 2dose_Vac_Complete_5PlusPop_Pct | −0.0684 ** | −0.0246 | −0.032 | −0.047 | 0.002 | 1444 |
| covid_case_per100k | 0.0887 *** | 0.0174 | 0.088 | −0.141 | 0.501 | 191 |
| Age_524_pct | 0.1228 *** | 0.1192 *** | 0.177 | 0.165 | 0.181 | 1481 |
| Avg Daily Sunlight | −0.1298 *** | −0.1287 *** | −0.192 | −0.202 | −0.191 | 1481 |
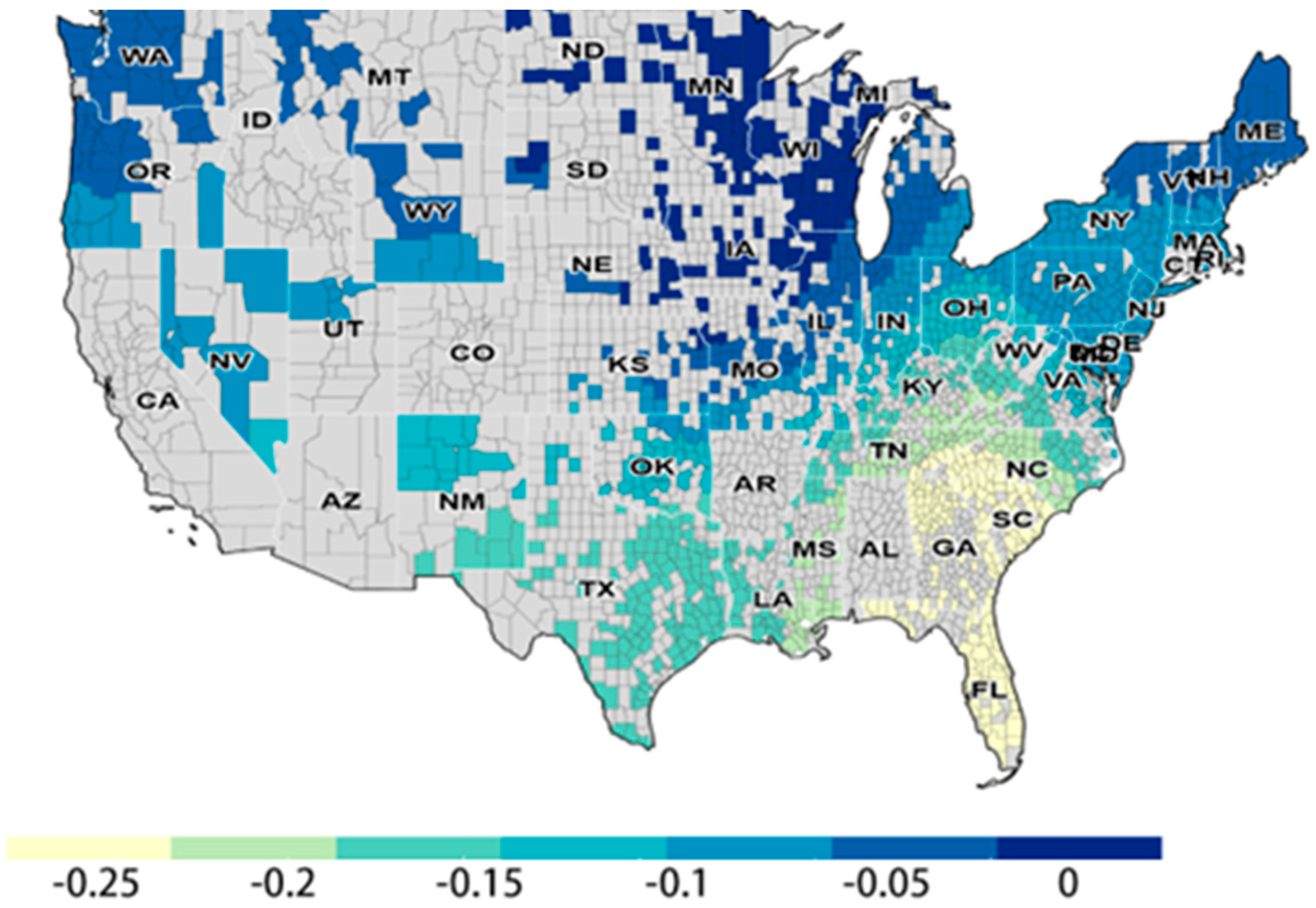
| Mental Health Provider Rate_log | −0.0806 *** | −0.1189 *** | −0.038 | −0.294 | 0.326 | 216 |
| pctExcessiveDrinking_log | −0.2008 *** | −0.2323 *** | −0.075 | −0.545 | 0.126 | 229 |
| Unemployment_rate | −0.1430 *** | −0.1517 *** | −0.097 | −0.280 | 0.049 | 720 |
| Diagnostic Results | ||||||
| Adjusted R-squared | 0.117 | 0.105 | 0.306 | |||
| AICc | 4031 | 4050 | 3835.58 | |||
| Value | |
|---|---|
| Moran’s Index | 0.075 |
| Z-score | 10.664 |
| p-value | 0.000 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Published by MDPI on behalf of the International Society for Photogrammetry and Remote Sensing. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Wang, Y.; Cui, W. Exploring the Spatial Relationship Between Severe Depression, COVID-19 Case Rates, and Vaccination Rates in US Counties: A Spatial Analysis Across Two Time Periods. ISPRS Int. J. Geo-Inf. 2025, 14, 376. https://doi.org/10.3390/ijgi14100376
Wang Y, Cui W. Exploring the Spatial Relationship Between Severe Depression, COVID-19 Case Rates, and Vaccination Rates in US Counties: A Spatial Analysis Across Two Time Periods. ISPRS International Journal of Geo-Information. 2025; 14(10):376. https://doi.org/10.3390/ijgi14100376
Chicago/Turabian StyleWang, Yuqing, and Wencong Cui. 2025. "Exploring the Spatial Relationship Between Severe Depression, COVID-19 Case Rates, and Vaccination Rates in US Counties: A Spatial Analysis Across Two Time Periods" ISPRS International Journal of Geo-Information 14, no. 10: 376. https://doi.org/10.3390/ijgi14100376
APA StyleWang, Y., & Cui, W. (2025). Exploring the Spatial Relationship Between Severe Depression, COVID-19 Case Rates, and Vaccination Rates in US Counties: A Spatial Analysis Across Two Time Periods. ISPRS International Journal of Geo-Information, 14(10), 376. https://doi.org/10.3390/ijgi14100376





