Impact of DARC rs12075 Variants on Liver Fibrosis Progression in Patients with Chronic Hepatitis C: A Retrospective Study
Abstract
:1. Introduction
2. Materials and Methods
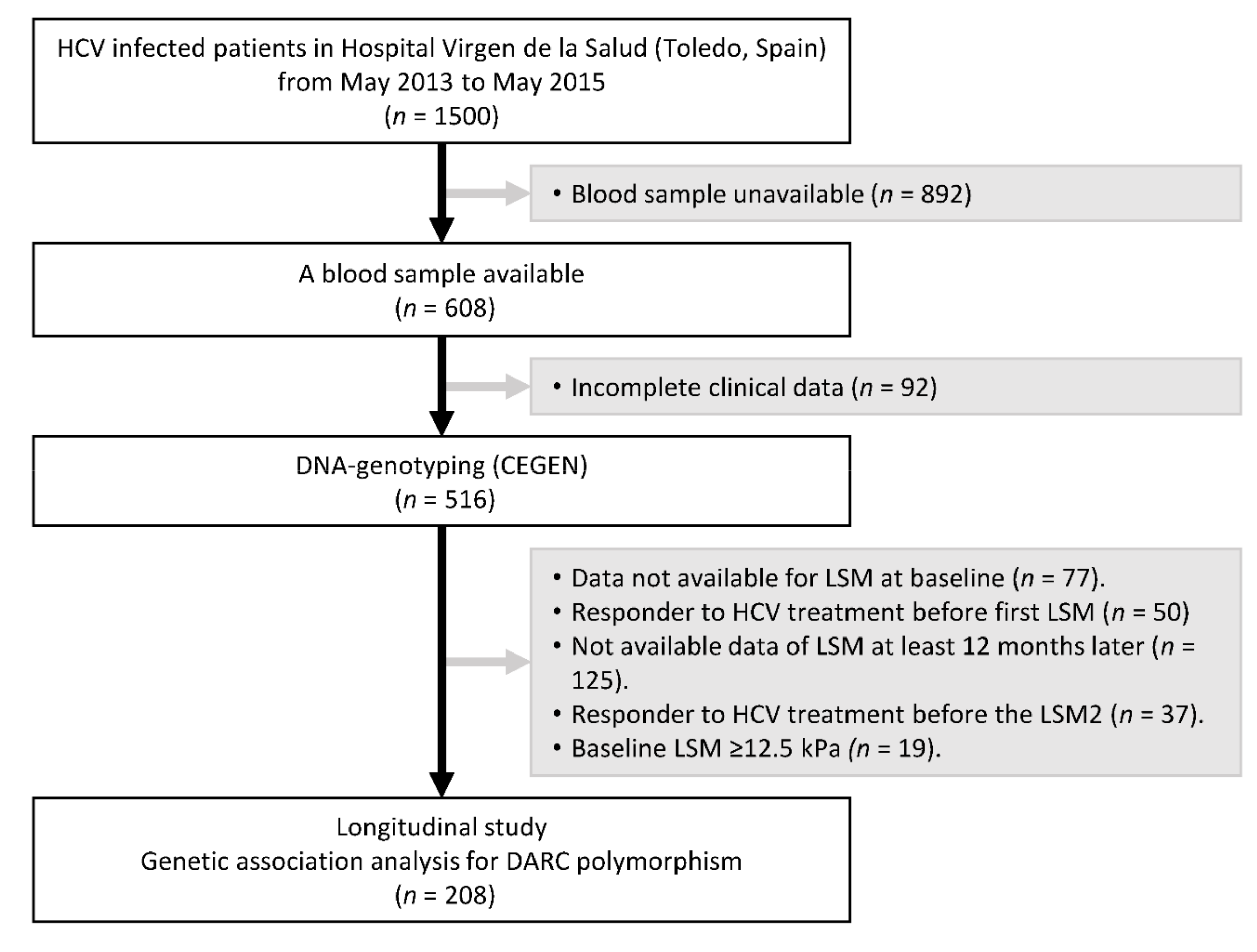
2.1. Study Population
2.2. Clinical Data
2.3. DNA Genotyping
2.4. Liver Stiffness Measurement
2.5. Outcome Variable
2.6. Statistical Analysis
3. Results
3.1. Characteristics of the Study Population
3.2. Characteristics of the DARC rs12075 SNP
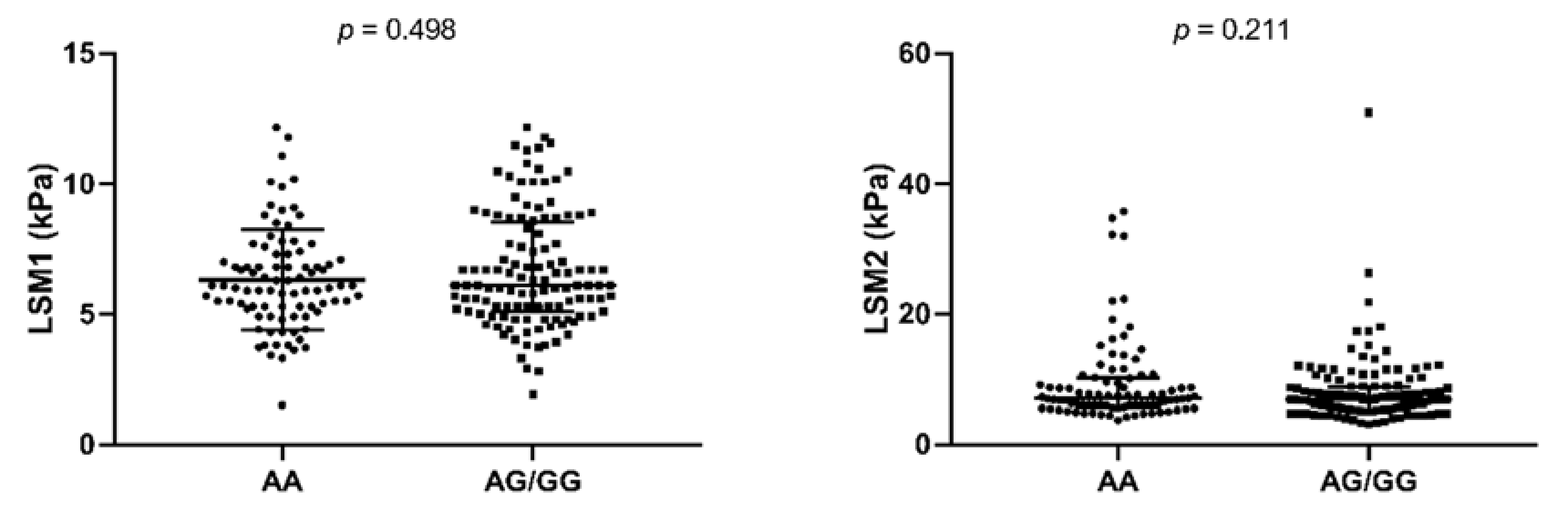
3.3. DARC rs12075 SNP and Fibrosis Progression
4. Discussion
Limitations of the Study
5. Conclusions
Author Contributions
Funding
Acknowledgments
Competing Interests
References
- WHO. Global Hepatitis Report; World Health Organization: Geneva, Switzerland, 2017. [Google Scholar]
- Lagging, L.M.; Westin, J.; Svensson, E.; Aires, N.; Dhillon, A.P.; Lindh, M.; Wejstal, R.; Norkrans, G. Progression of fibrosis in untreated patients with hepatitis C virus infection. Liver 2002, 22, 136–144. [Google Scholar] [CrossRef]
- Hoofnagle, J.H. Course and outcome of hepatitis C. Hepatology 2002, 36, S21–S29. [Google Scholar]
- Conti, F.; Buonfiglioli, F.; Scuteri, A.; Crespi, C.; Bolondi, L.; Caraceni, P.; Foschi, F.G.; Lenzi, M.; Mazzella, G.; Verucchi, G.; et al. Early occurrence and recurrence of hepatocellular carcinoma in HCV-related cirrhosis treated with direct-acting antivirals. J. Hepatol. 2016, 65, 727–733. [Google Scholar] [CrossRef] [PubMed]
- Forner, A.; Reig, M.; Bruix, J. Hepatocellular carcinoma. Lancet 2018, 391, 1301–1314. [Google Scholar] [CrossRef]
- Rueger, S.; Bochud, P.Y.; Dufour, J.F.; Mullhaupt, B.; Semela, D.; Heim, M.H.; Moradpour, D.; Cerny, A.; Malinverni, R.; Booth, D.R.; et al. Impact of common risk factors of fibrosis progression in chronic hepatitis C. Gut 2015, 64, 1605–1615. [Google Scholar] [CrossRef]
- Heim, M.H.; Bochud, P.Y.; George, J. Host—Hepatitis C viral interactions: The role of genetics. J. Hepatol. 2016, 65, S22–S32. [Google Scholar] [CrossRef] [PubMed]
- Pawlotsky, J.M.; Aghemo, A.; Back, D.; Dusheiko, G.; Forns, X.; Puoti, M.; Sarrazin, C. EASL recommendations on treatment of hepatitis C 2015. J. Hepatol. 2015, 63, 199–236. [Google Scholar]
- Thiele, M.; Kjaergaard, M.; Thielsen, P.; Krag, A. Contemporary use of elastography in liver fibrosis and portal hypertension. Clin. Physiol. Funct. Imaging 2017, 37, 235–242. [Google Scholar] [CrossRef] [PubMed]
- Tsochatzis, E.A.; Bosch, J.; Burroughs, A.K. Liver cirrhosis. Lancet 2014, 383, 1749–1761. [Google Scholar] [CrossRef]
- Resino, S.; Sanchez-Conde, M.; Berenguer, J. Coinfection by human immunodeficiency virus and hepatitis C virus: Noninvasive assessment and staging of fibrosis. Curr. Opin. Infect. Dis. 2012, 25, 564–569. [Google Scholar] [CrossRef] [PubMed]
- Castera, L. Noninvasive assessment of liver fibrosis. Dig. Dis. 2015, 33, 498–503. [Google Scholar] [CrossRef] [PubMed]
- Zeremski, M.; Dimova, R.; Brown, Q.; Jacobson, I.M.; Markatou, M.; Talal, A.H. Peripheral CXCR3-associated chemokines as biomarkers of fibrosis in chronic hepatitis C virus infection. J. Infect. Dis. 2009, 200, 1774–1780. [Google Scholar] [CrossRef]
- Fallahi, P.; Ferrari, S.M.; Giuggioli, D.; Sebastiani, M.; Colaci, M.; Ferri, C.; Antonelli, A. Chemokines in the pathogenesis and as therapeutical markers and targets of HCV chronic infection and HCV extrahepatic manifestations. Curr. Drug Targets 2017, 18, 786–793. [Google Scholar] [CrossRef]
- Promrat, K.; McDermott, D.H.; Gonzalez, C.M.; Kleiner, D.E.; Koziol, D.E.; Lessie, M.; Merrell, M.; Soza, A.; Heller, T.; Ghany, M.; et al. Associations of chemokine system polymorphisms with clinical outcomes and treatment responses of chronic hepatitis C. Gastroenterology 2003, 124, 352–360. [Google Scholar] [CrossRef] [PubMed]
- Hellier, S.; Frodsham, A.J.; Hennig, B.J.; Klenerman, P.; Knapp, S.; Ramaley, P.; Satsangi, J.; Wright, M.; Zhang, L.; Thomas, H.C.; et al. Association of genetic variants of the chemokine receptor CCR5 and its ligands, rantes and MCP-2, with outcome of HCV infection. Hepatology 2003, 38, 1468–1476. [Google Scholar] [CrossRef] [PubMed]
- Mantovani, A.; Locati, M.; Vecchi, A.; Sozzani, S.; Allavena, P. Decoy receptors: A strategy to regulate inflammatory cytokines and chemokines. Trends Immunol. 2001, 22, 328–336. [Google Scholar] [CrossRef]
- Marsh, W.L. Present status of the duffy blood group system. CRC Crit. Rev. Clin. Lab. Sci. 1975, 5, 387–412. [Google Scholar] [CrossRef] [PubMed]
- Gardner, L.; Patterson, A.M.; Ashton, B.A.; Stone, M.A.; Middleton, J. The human duffy antigen binds selected inflammatory but not homeostatic chemokines. Biochem. Biophys. Res. Commun. 2004, 321, 306–312. [Google Scholar] [CrossRef]
- Chaudhuri, A.; Nielsen, S.; Elkjaer, M.L.; Zbrzezna, V.; Fang, F.; Pogo, A.O. Detection of Duffy antigen in the plasma membranes and caveolae of vascular endothelial and epithelial cells of nonerythroid organs. Blood 1997, 89, 701–712. [Google Scholar] [PubMed]
- Pruenster, M.; Mudde, L.; Bombosi, P.; Dimitrova, S.; Zsak, M.; Middleton, J.; Richmond, A.; Graham, G.J.; Segerer, S.; Nibbs, R.J.; et al. The Duffy antigen receptor for chemokines transports chemokines and supports their promigratory activity. Nat. Immunol. 2009, 10, 101–108. [Google Scholar] [CrossRef]
- Lee, J.S.; Frevert, C.W.; Wurfel, M.M.; Peiper, S.C.; Wong, V.A.; Ballman, K.K.; Ruzinski, J.T.; Rhim, J.S.; Martin, T.R.; Goodman, R.B. Duffy antigen facilitates movement of chemokine across the endothelium in vitro and promotes neutrophil transmigration in vitro and in vivo. J. Immunol. 2003, 170, 5244–5251. [Google Scholar] [CrossRef] [PubMed]
- Darbonne, W.C.; Rice, G.C.; Mohler, M.A.; Apple, T.; Hebert, C.A.; Valente, A.J.; Baker, J.B. Red blood cells are a sink for interleukin 8, a leukocyte chemotaxin. J. Clin. Investig. 1991, 88, 1362–1369. [Google Scholar] [CrossRef] [PubMed]
- Yamamoto, A.; Saito, N.; Ogasawara, S.; Shiratori, T.; Kondo, J.; Itoga, M.; Kayaba, H. Intracellular storage of duffy antigen-binding chemokines by duffy-positive red blood cells. Clin. Lab. 2017, 63, 717–723. [Google Scholar] [CrossRef]
- Fukuma, N.; Akimitsu, N.; Hamamoto, H.; Kusuhara, H.; Sugiyama, Y.; Sekimizu, K. A role of the duffy antigen for the maintenance of plasma chemokine concentrations. Biochem. Biophys. Res. Commun. 2003, 303, 137–139. [Google Scholar] [CrossRef]
- Schnabel, R.B.; Baumert, J.; Barbalic, M.; Dupuis, J.; Ellinor, P.T.; Durda, P.; Dehghan, A.; Bis, J.C.; Illig, T.; Morrison, A.C.; et al. Duffy antigen receptor for chemokines (DARC) polymorphism regulates circulating concentrations of monocyte chemoattractant protein-1 and other inflammatory mediators. Blood 2010, 115, 5289–5299. [Google Scholar] [CrossRef]
- Marra, F.; Tacke, F. Roles for chemokines in liver disease. Gastroenterology 2014, 147, 577–594. [Google Scholar] [CrossRef] [PubMed]
- Jimenez-Sousa, M.A.; Gomez-Moreno, A.Z.; Pineda-Tenor, D.; Medrano, L.M.; Sanchez-Ruano, J.J.; Fernandez-Rodriguez, A.; Artaza-Varasa, T.; Saura-Montalban, J.; Vazquez-Moron, S.; Ryan, P.; et al. The IL7RA rs6897932 polymorphism is associated with progression of liver fibrosis in patients with chronic hepatitis C: Repeated measurements design. PLoS ONE 2018, 13, e0197115. [Google Scholar] [CrossRef] [PubMed]
- Calvaruso, V.; Craxì, A. 2011 european association of the study of the liver hepatitis C virus clinical practice guidelines. Liver Int. 2012, 32, 2–8. [Google Scholar] [CrossRef]
- European Association for Study of Liver. EASL clinical practice guidelines: Management of hepatitis C virus infection. In J. Hepatol.; 2014; Volume 60, pp. 392–420. [Google Scholar]
- Gabriel, S.; Ziaugra, L.; Tabbaa, D. SNP genotyping using the sequenom MassARRAY iPLEX platform. In Current Protocols in Human Genetics; Haines, J.L., Ed.; John Wiley & Sons, Inc.: Weinheim, Germany, 2009; Volume 60, pp. 2–12. [Google Scholar]
- Jimenez-Sousa, M.A.; Gomez-Moreno, A.Z.; Pineda-Tenor, D.; Sanchez-Ruano, J.J.; Fernandez-Rodriguez, A.; Artaza-Varasa, T.; Gomez-Sanz, A.; Martin-Vicente, M.; Vazquez-Moron, S.; Resino, S. PNPLA3 rs738409 polymorphism is associated with liver fibrosis progression in patients with chronic hepatitis C: A repeated measures study. J. Clin. Virol. 2018, 103, 71–74. [Google Scholar] [CrossRef]
- Jimenez-Sousa, M.A.; Gomez-Moreno, A.Z.; Pineda-Tenor, D.; Brochado-Kith, O.; Sanchez-Ruano, J.J.; Artaza-Varasa, T.; Gomez-Sanz, A.; Fernandez-Rodriguez, A.; Resino, S. The myeloid-epithelial-reproductive tyrosine kinase (MERKT) rs4374383 polymorphism predicts progression of liver fibrosis in hepatitis C virus-infected patients: A longitudinal study. J. Clin. Med. 2018, 7, 473. [Google Scholar] [CrossRef]
- Castera, L.; Vergniol, J.; Foucher, J.; Le Bail, B.; Chanteloup, E.; Haaser, M.; Darriet, M.; Couzigou, P.; De Ledinghen, V. Prospective comparison of transient elastography, fibrotest, APRI, and liver biopsy for the assessment of fibrosis in chronic hepatitis C. Gastroenterology 2005, 128, 343–350. [Google Scholar] [CrossRef]
- Albert, P.S. Longitudinal data analysis (repeated measures) in clinical trials. Stat. Med. 1999, 18, 1707–1732. [Google Scholar] [CrossRef]
- Senn, S.; Stevens, L.; Chaturvedi, N. Repeated measures in clinical trials: Simple strategies for analysis using summary measures. Stat. Med. 2000, 19, 861–877. [Google Scholar] [CrossRef]
- Mangalmurti, N.S.; Xiong, Z.; Hulver, M.; Ranganathan, M.; Liu, X.H.; Oriss, T.; Fitzpatrick, M.; Rubin, M.; Triulzi, D.; Choi, A.; et al. Loss of red cell chemokine scavenging promotes transfusion-related lung inflammation. Blood 2009, 113, 1158–1166. [Google Scholar] [CrossRef] [PubMed]
- Akalin, E.; Neylan, J.F. The influence of duffy blood group on renal allograft outcome in African Americans. Transplantation 2003, 75, 1496–1500. [Google Scholar] [CrossRef] [PubMed]
- Aragones, G.; Ercilla, A.; Barreda, M.; Rull, A.; Beltran-Debon, R.; Rodriguez-Gallego, E.; Alonso-Villaverde, C.; Camps, J.; Joven, J. Human duffy blood group alloantigen system influences the measurement of monocyte chemoattractant protein-1 (MCP-1) in serum but not in plasma. Clin. Lab. 2012, 58, 185–188. [Google Scholar] [PubMed]
- Naitza, S.; Porcu, E.; Steri, M.; Taub, D.D.; Mulas, A.; Xiao, X.; Strait, J.; Dei, M.; Lai, S.; Busonero, F.; et al. A genome-wide association scan on the levels of markers of inflammation in Sardinians reveals associations that underpin its complex regulation. PLoS Genet. 2012, 8, e1002480. [Google Scholar] [CrossRef]
- Moreno Velasquez, I.; Kumar, J.; Bjorkbacka, H.; Nilsson, J.; Silveira, A.; Leander, K.; Berglund, A.; Strawbridge, R.J.; Arnlov, J.; Melander, O.; et al. Duffy antigen receptor genetic variant and the association with interleukin 8 levels. Cytokine 2015, 72, 178–184. [Google Scholar] [CrossRef] [PubMed]
- Rull, A.; Hernandez-Aguilera, A.; Fibla, M.; Sepulveda, J.; Rodriguez-Gallego, E.; Riera-Borrull, M.; Sirvent, J.J.; Martin-Paredero, V.; Menendez, J.A.; Camps, J.; et al. Understanding the role of circulating chemokine (C-C motif) ligand 2 in patients with chronic ischemia threatening the lower extremities. Vasc. Med. 2014, 19, 442–451. [Google Scholar] [CrossRef]
- Voruganti, V.S.; Laston, S.; Haack, K.; Mehta, N.R.; Smith, C.W.; Cole, S.A.; Butte, N.F.; Comuzzie, A.G. Genome-wide association replicates the association of duffy antigen receptor for chemokines (DARC) polymorphisms with serum monocyte chemoattractant protein-1 (MCP-1) levels in Hispanic children. Cytokine 2012, 60, 634–638. [Google Scholar] [CrossRef]
- Crosslin, D.R.; McDavid, A.; Weston, N.; Nelson, S.C.; Zheng, X.; Hart, E.; de Andrade, M.; Kullo, I.J.; McCarty, C.A.; Doheny, K.F.; et al. Genetic variants associated with the white blood cell count in 13,923 subjects in the emerge network. Hum. Genet. 2012, 131, 639–652. [Google Scholar] [CrossRef]
- Marra, F.; DeFranco, R.; Grappone, C.; Milani, S.; Pastacaldi, S.; Pinzani, M.; Romanelli, R.G.; Laffi, G.; Gentilini, P. Increased expression of monocyte chemotactic protein-1 during active hepatic fibrogenesis: Correlation with monocyte infiltration. Am. J. Pathol. 1998, 152, 423–430. [Google Scholar] [PubMed]
- Gonzalez-Reimers, E.; Quintero-Platt, G.; Martin-Gonzalez, C.; Perez-Hernandez, O.; Romero-Acevedo, L.; Santolaria-Fernandez, F. Thrombin activation and liver inflammation in advanced hepatitis C virus infection. World J. Gastroenterol. 2016, 22, 4427–4437. [Google Scholar] [CrossRef] [PubMed]
- Lettow, I.; Berres, M.L.; Schmitz, P.; Muller, T.; Berg, T.; Neumann, U.P.; Trautwein, C.; Wasmuth, H.E. A duffy antigen receptor for chemokines (DARC) polymorphism that determines pro-fibrotic chemokine serum concentrations is not directly associated with severity of hepatitis C infection. Hum. Immunol. 2011, 72, 273–277. [Google Scholar] [CrossRef] [PubMed]
- Carmona, I.; Cordero, P.; Ampuero, J.; Rojas, A.; Romero-Gomez, M. Role of assessing liver fibrosis in management of chronic hepatitis C virus infection. Clin. Microbiol. Infect. 2016, 22, 839–845. [Google Scholar] [CrossRef]
| DARC rs12075 Polymorphism | |||||
|---|---|---|---|---|---|
| Characteristic | All Patients | AA | AG | GG | p-Value |
| No. | 208 | 88 | 92 | 28 | |
| Male | 112 (53.8%) | 44 (50%) | 56 (60.9%) | 12 (4.9%) | 0.156 |
| Age (years) | 47.1(41.5; 57.6) | 49.2 (40.7; 56.1) | 46.5 (42.8; 55.2) | 48.8 (42.4; 59.6) | 0.830 |
| Time of HCV infection (years) | 8.2 (3.2; 13.2) | 9.3 (3.4; 13.6) | 8.05 (3.6; 12.9) | 4.22 (1.1; 11.0) | 0.694 |
| High alcohol intake | 28 (13.5%) | 11 (12.5%) | 14 (15.2%) | 3 (10.7%) | 0.781 |
| Prior injection drug use | 21 (10.1%) | 9 (10.2%) | 11 (12%) | 1 (3.6%) | 0.517 |
| HCV genotype (n = 204) | |||||
| 1 | 174 (85.3%) | 75 (88.2%) | 78 (84.8%) | 21 (77.8%) | 0.402 |
| 3 | 14 (6.9%) | 6 (7.1%) | 5 (5.4%) | 3 (11.1%) | 0.588 |
| 4 | 15 (7.4%) | 4 (4.7%) | 8 (8.7%) | 3 (11.1%) | 0.432 |
| 5 | 1 (0.5%) | 0 (0%) | 1 (1.1%) | - | - |
| Prior failed HCV therapy | 47 (22.6%) | 20 (22.7%) | 22 (23.9%) | 5 (17.9%) | 0.798 |
| IFN-α | 22 (10.6%) | 10 (11.4%) | 9 (9.8%) | 3 (10.7%) | 0.942 |
| IFN-α/RBV | 1 (0.5%) | - | 1 (1.1%) | - | - |
| peg-IFN-α/RBV | 22 (10.6%) | 10 (11.4%) | 10 (10.9%) | 2 (7.1%) | 0.812 |
| DAAs + peg-IFN-α/RBV | 2 (1%) | - | 2 (2.2%) | - | - |
| Baseline LSM (kPa) | 6.1 (5.2; 7.7) | 6.1 (5.3; 7.2) | 6.1 (5.3; 8.7) | 5.6 (4.9; 7.4) | 0.280 |
| F0–F1 (<7.1 kPa) | 149 (71.6%) | 66 (75%) | 62 (67.4%) | 21 (75.0%) | 0.481 |
| F2 (7.1–9.4 kPa) | 38 (18.3%) | 16 (18.2%) | 19 (20.7%) | 3 (10.7%) | 0.432 |
| F3 (9.5–12.4 kPa) | 21 (10.1%) | 6 (6.8%) | 11 (12.0%) | 4 (14.3%) | 0.315 |
| HCV Cohort | IBS Group | p-Value | ||
|---|---|---|---|---|
| No. | 208 | 107 | ||
| Alleles | A | 64.4% | 70.1% | 0.312 |
| G | 35.6% | 29.9% | ||
| Genotype | AA | 42.3% | 49.5% | 0.160 |
| AG | 44.2% | 41.1% | ||
| GG | 13.5% | 9.3% | ||
| HWE (p-value) | 0.718 | 0.856 |
| All Patients | rs12075 AA Genotype | rs12075 AG/GG Genotype | |||||||
|---|---|---|---|---|---|---|---|---|---|
| Characteristic | Baseline | End | p-Value | Baseline | End | p -Value | Baseline | End | p -Value |
| Follow-up (months) | 46.6 (28.7; 61.5) | 50.6 (29.1; 64.2) | 43.8 (28.2; 60.2) | ||||||
| LSM (kPa) | 6.1 (5.2; 7.7) | 6.8 (5.5; 9.4) | <0.001 | 6.1 (5.3; 7.2) | 7.1 (5.8; 10.1) | <0.001 | 6.1 (5.1; 8.5) | 6.8 (5.3; 8.8) | <0.001 |
| F0–F1 (<7.1 kPa) | 149 (71.6%) | 110 (52.9%) | <0.001 | 66 (75%) | 44 (50%) | <0.001 | 83 (69.2%) | 66 (55%) | 0.004 |
| F2 (7.1–9.4 kPa) | 38 (18.3%) | 47 (22.6%) | 0.382 | 16 (18.2%) | 21 (23.9%) | 0.584 | 22 (18.3%) | 26 (21.7%) | 0.607 |
| F3 (9.5–12.4 kPa) | 21 (10.1%) | 25 (12%) | 0.055 | 6 (6.8%) | 8 (9.1%) | 0.077 | 15 (12.5%) | 17 (14.2%) | 0.361 |
| F4 (≥12.5 kPa) | 0 (0%) | 26 (12.5%) | <0.001 | 0 (0%) | 15 (17%) | <0.001 | 0 (0%) | 11 (9.2%) | 0.001 |
| DARC rs12075 Genotypes | Unadjusted | Adjusted | ||||
|---|---|---|---|---|---|---|
| Outcome | AA | AG/GG | Exp(B) (95% CI) | p Value a | Exp(B) (95% CI) | p Value b |
| LSM2/LSM1 | 1.26 (0.98; 1.51) | 1.10 (0.94; 1.31) | 0.79 (0.71; 0.87) | <0.001 | 0.83 (0.75; 0.93) | 0.001 |
| ΔLSM ≥ 5 kPa | 16 (18.2%) | 9 (7.5%) | 0.36 (1.53; 0.87) | 0.023 | 0.28 (0.10; 0.73) | 0.009 |
| ΔLSM ≥ 7 kPa | 10 (11.4%) | 4 (3.3%) | 0.27 (0.08; 0.88) | 0.031 | 0.31 (0.07; 1.27) | 0.104 |
| ΔLSM ≥ 10 kPa | 7 (8%) | 4 (3.3%) | 0.39 (0.11; 1.41) | 0.153 | 0.47 (0.11; 2.06) | 0.322 |
| Progression to F4 | 15 (17%) | 11 (9.2%) | 0.49 (0.21; 1.13) | 0.094 | 0.24 (0.08; 0.70) | 0.009 |
© 2019 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Jiménez-Sousa, M.Á.; Gómez-Moreno, A.Z.; Pineda-Tenor, D.; Sánchez-Ruano, J.J.; Artaza-Varasa, T.; Martin-Vicente, M.; Fernández-Rodríguez, A.; Martínez, I.; Resino, S. Impact of DARC rs12075 Variants on Liver Fibrosis Progression in Patients with Chronic Hepatitis C: A Retrospective Study. Biomolecules 2019, 9, 143. https://doi.org/10.3390/biom9040143
Jiménez-Sousa MÁ, Gómez-Moreno AZ, Pineda-Tenor D, Sánchez-Ruano JJ, Artaza-Varasa T, Martin-Vicente M, Fernández-Rodríguez A, Martínez I, Resino S. Impact of DARC rs12075 Variants on Liver Fibrosis Progression in Patients with Chronic Hepatitis C: A Retrospective Study. Biomolecules. 2019; 9(4):143. https://doi.org/10.3390/biom9040143
Chicago/Turabian StyleJiménez-Sousa, María Ángeles, Ana Zaida Gómez-Moreno, Daniel Pineda-Tenor, Juan José Sánchez-Ruano, Tomas Artaza-Varasa, María Martin-Vicente, Amanda Fernández-Rodríguez, Isidoro Martínez, and Salvador Resino. 2019. "Impact of DARC rs12075 Variants on Liver Fibrosis Progression in Patients with Chronic Hepatitis C: A Retrospective Study" Biomolecules 9, no. 4: 143. https://doi.org/10.3390/biom9040143
APA StyleJiménez-Sousa, M. Á., Gómez-Moreno, A. Z., Pineda-Tenor, D., Sánchez-Ruano, J. J., Artaza-Varasa, T., Martin-Vicente, M., Fernández-Rodríguez, A., Martínez, I., & Resino, S. (2019). Impact of DARC rs12075 Variants on Liver Fibrosis Progression in Patients with Chronic Hepatitis C: A Retrospective Study. Biomolecules, 9(4), 143. https://doi.org/10.3390/biom9040143






