Age Trajectories of O2 Saturation and Levels of Serum Bicarbonate or End-Tidal CO2 Across the Life Course of Women and Men: Insights from EHR and PSG Data
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Design
2.2. Electronic Health Record (EHR)
2.3. In-Laboratory Polysomnography Study
2.4. Statistical Analysis
3. Results
3.1. Subject Characteristics
3.1.1. EHR Data
3.1.2. PSG Data
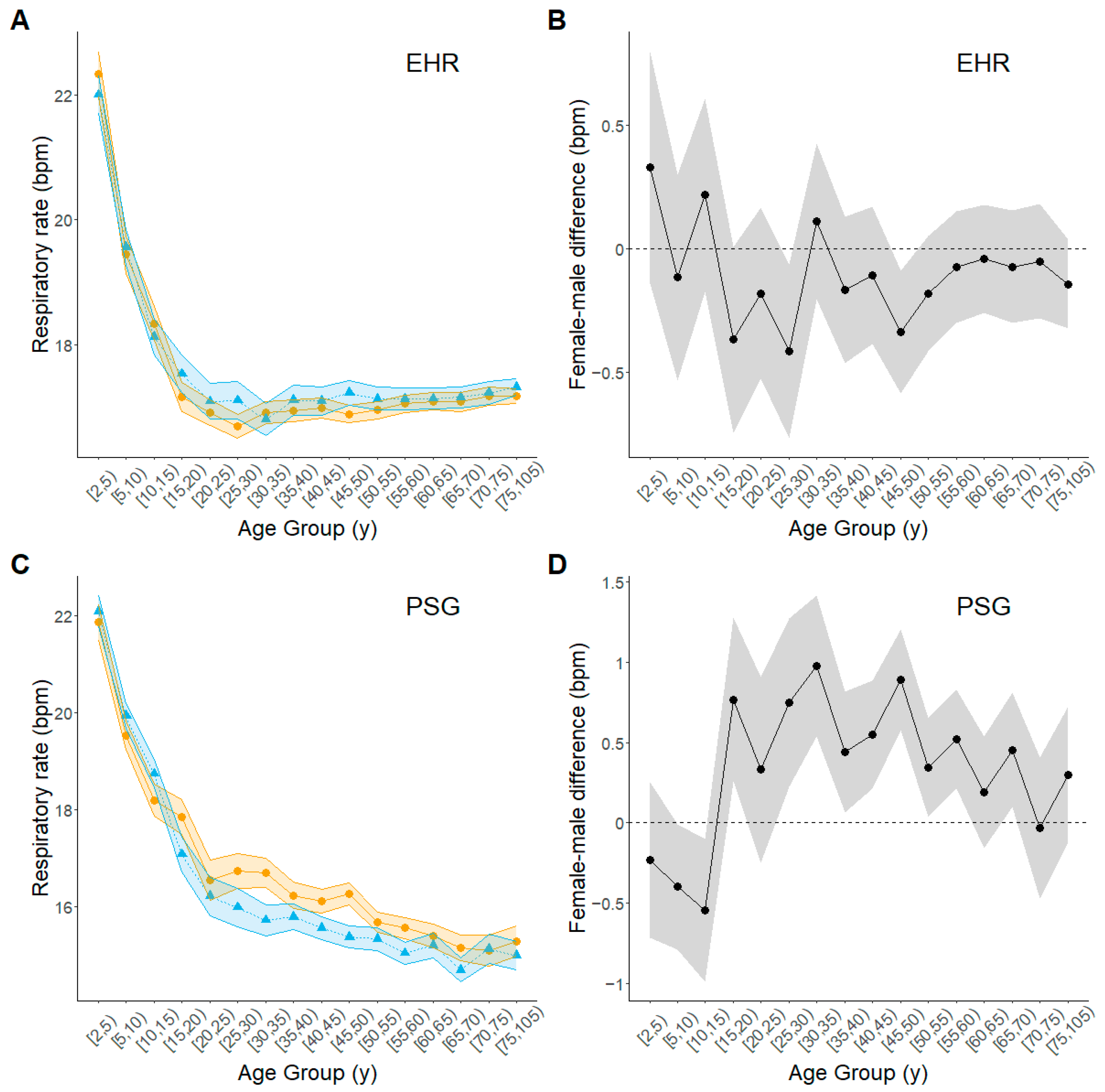
3.2. Age Trajectories of Key Variables
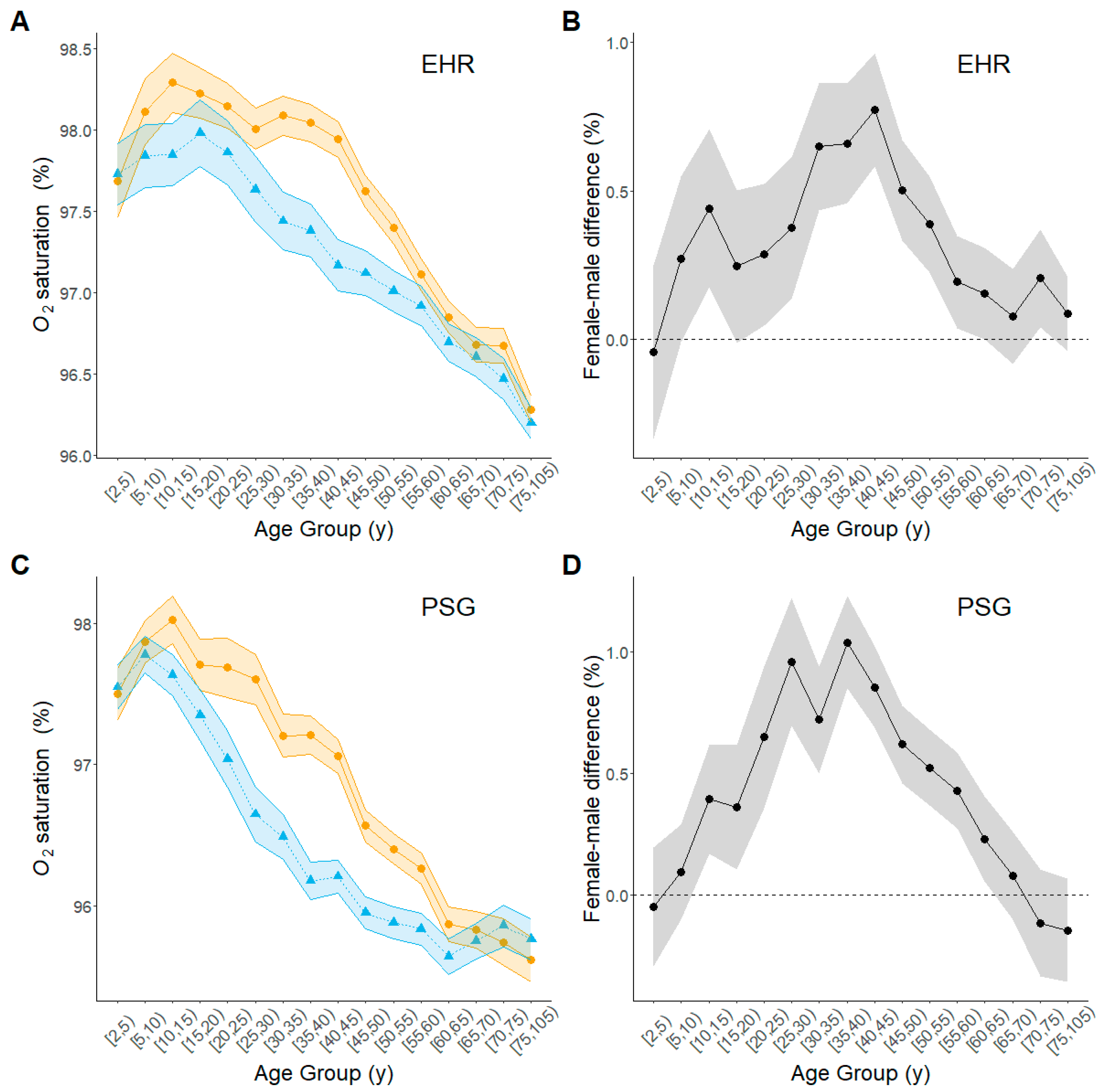
3.2.1. Pulse Oximetry Oxygen Saturation
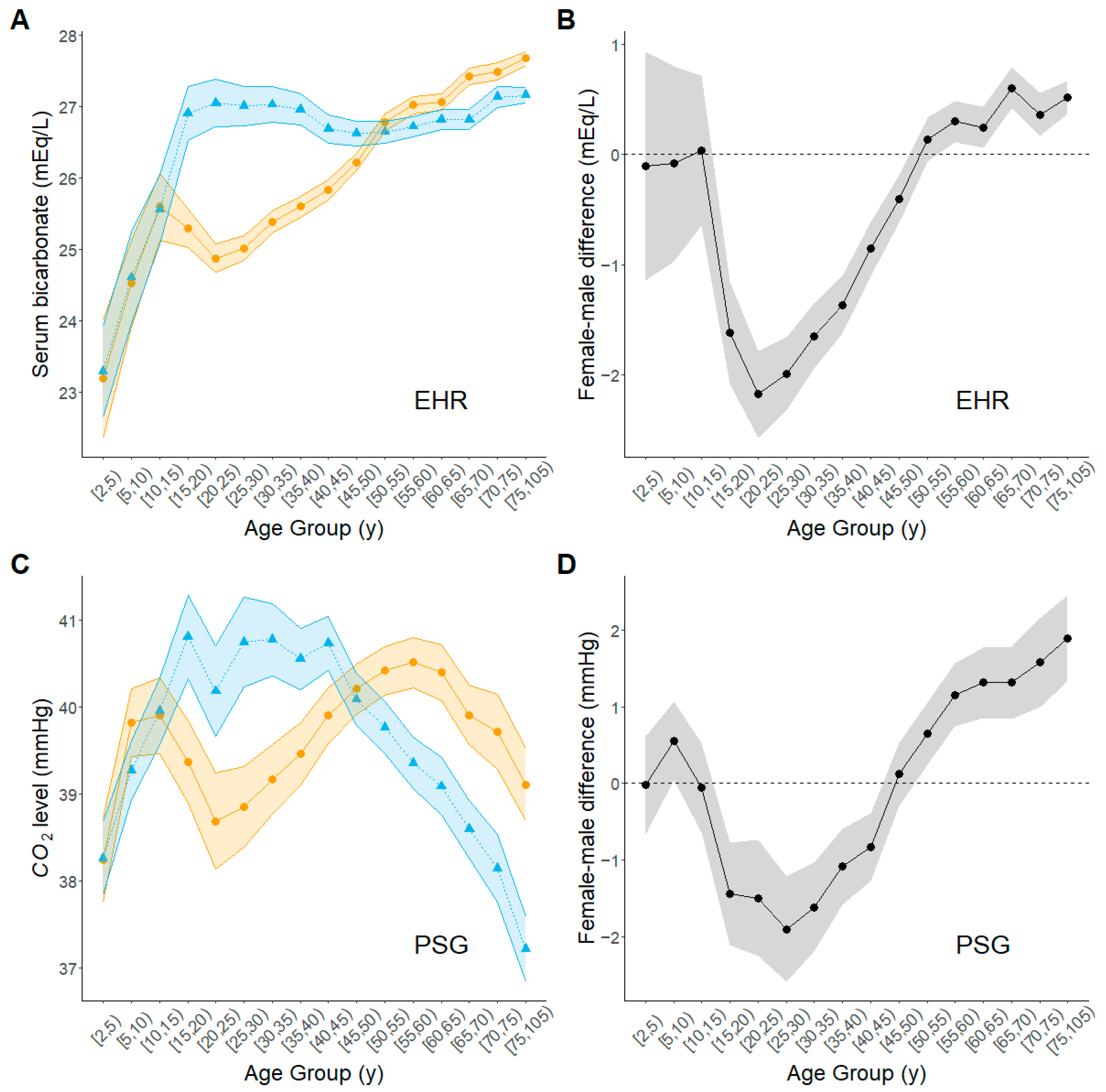
3.2.2. Serum Bicarbonate Level (EHR Data)
3.2.3. End-Tidal CO2 (PSG Data)
3.2.4. Heart Rate
3.2.5. Evidence Supporting the Role of Progesterone in Gas Exchange
4. Discussion
4.1. Limitations and Strengths
4.2. Perspectives and Significance
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Abbreviations
| BMI | Body mass index |
| CHD | Coronary heart disease |
| COPD | Chronic obstructive pulmonary disease |
| EHR | Electronic health record |
| EM | Emphysema |
| HF | Heart failure |
| PE | Pulmonary embolism |
| PSG | Polysomnography |
| RR | Respiratory rate |
References
- Eagly, A.H.; Wood, W. The origins of sex differences in human behavior. Am. Psychol. 1999, 54, 408–423. [Google Scholar] [CrossRef]
- Buss, D.M. Sex differences in human mate preferences: Evolutionary hypotheses tested in 37 cultures. Behav. Brain Sci. 1989, 12, 1–14. [Google Scholar] [CrossRef]
- Ingalhalikar, M.; Smith, A.; Parker, D.; Satterthwaite, T.D.; Elliott, M.A.; Ruparel, K.; Hakonarson, H.; Gur, R.E.; Gur, R.C.; Verma, R. Sex differences in the structural connectome of the human brain. Proc. Natl. Acad. Sci. USA 2014, 111, 823–828. [Google Scholar] [CrossRef]
- Rodriguez-Montes, L.; Ovchinnikova, S.; Yuan, X.; Studer, T.; Sarropoulos, I.; Anders, S.; Kaessmann, H.; Cardoso-Moreira, M. Sex-biased gene expression across mammalian organ development and evolution. Science 2023, 382, eadf1046. [Google Scholar] [CrossRef]
- Regitz-Zagrosek, V. Sex and gender differences in health. Science & Society Series on Sex and Science. EMBO Rep. 2012, 13, 596–603. [Google Scholar] [CrossRef]
- Klein, S.L.; Flanagan, K.L. Sex differences in immune responses. Nat. Rev. Immunol. 2016, 16, 626–638. [Google Scholar] [CrossRef] [PubMed]
- Mauvais-Jarvis, F.; Bairey Merz, N.; Barnes, P.J.; Brinton, R.D.; Carrero, J.J.; DeMeo, D.L.; De Vries, G.J.; Epperson, C.N.; Govindan, R.; Klein, S.L.; et al. Sex and gender: Modifiers of health, disease, and medicine. Lancet 2020, 396, 565–582. [Google Scholar] [CrossRef]
- Mosca, L.; Barrett-Connor, E.; Wenger, N.K. Sex/gender differences in cardiovascular disease prevention: What a difference a decade makes. Circulation 2011, 124, 2145–2154. [Google Scholar] [CrossRef]
- Lam, C.S.P.; Arnott, C.; Beale, A.L.; Chandramouli, C.; Hilfiker-Kleiner, D.; Kaye, D.M.; Ky, B.; Santema, B.T.; Sliwa, K.; Voors, A.A. Sex differences in heart failure. Eur. Heart J. 2019, 40, 3859–3868c. [Google Scholar] [CrossRef]
- Bots, S.H.; Peters, S.A.E.; Woodward, M. Sex differences in coronary heart disease and stroke mortality: A global assessment of the effect of ageing between 1980 and 2010. BMJ Glob. Health 2017, 2, e000298. [Google Scholar] [CrossRef]
- Regitz-Zagrosek, V.; Gebhard, C. Gender medicine: Effects of sex and gender on cardiovascular disease manifestation and outcomes. Nat. Rev. Cardiol. 2023, 20, 236–247. [Google Scholar] [CrossRef] [PubMed]
- Maas, A.H.; Appelman, Y.E. Gender differences in coronary heart disease. Neth. Heart J. 2010, 18, 598–602. [Google Scholar] [CrossRef]
- Joseph, V.; Behan, M.; Kinkead, R. Sex, hormones, and stress: How they impact development and function of the carotid bodies and related reflexes. Respir. Physiol. Neurobiol. 2013, 185, 75–86. [Google Scholar] [CrossRef]
- Gargaglioni, L.H.; Marques, D.A.; Patrone, L.G.A. Sex differences in breathing. Comp. Biochem. Physiol. A Mol. Integr. Physiol. 2019, 238, 110543. [Google Scholar] [CrossRef]
- LoMauro, A.; Aliverti, A. Sex differences in respiratory function. Breathe 2018, 14, 131–140. [Google Scholar] [CrossRef] [PubMed]
- Massaro, G.D.; Mortola, J.P.; Massaro, D. Sexual dimorphism in the architecture of the lung’s gas-exchange region. Proc. Natl. Acad. Sci. USA 1995, 92, 1105–1107. [Google Scholar] [CrossRef]
- LoMauro, A.; Aliverti, A. Sex and gender in respiratory physiology. Eur. Respir. Rev. 2021, 30, 210038. [Google Scholar] [CrossRef] [PubMed]
- Reddy, K.D.; Oliver, B.G.G. Sexual dimorphism in chronic respiratory diseases. Cell Biosci. 2023, 13, 47. [Google Scholar] [CrossRef]
- Silveyra, P.; Fuentes, N.; Rodriguez Bauza, D.E. Sex and Gender Differences in Lung Disease. Adv. Exp. Med. Biol. 2021, 1304, 227–258. [Google Scholar] [CrossRef]
- Somayaji, R.; Chalmers, J.D. Just breathe: A review of sex and gender in chronic lung disease. Eur. Respir. Rev. 2022, 31, 210111. [Google Scholar] [CrossRef]
- Saaresranta, T.; Irjala, K.; Polo, O. Effect of medroxyprogesterone on arterial blood gases, leptin and neuropeptide Y in postmenopausal females. Eur. Respir. J. 2002, 20, 1413–1418. [Google Scholar] [CrossRef] [PubMed]
- Pickett, C.K.; Regensteiner, J.G.; Woodard, W.D.; Hagerman, D.D.; Weil, J.V.; Moore, L.G. Progestin and estrogen reduce sleep-disordered breathing in postmenopausal women. J. Appl. Physiol. 1989, 66, 1656–1661. [Google Scholar] [CrossRef] [PubMed]
- Behan, M.; Wenninger, J.M. Sex steroidal hormones and respiratory control. Respir. Physiol. Neurobiol. 2008, 164, 213–221. [Google Scholar] [CrossRef]
- Bayliss, D.A.; Millhorn, D.E.; Gallman, E.A.; Cidlowski, J.A. Progesterone stimulates respiration through a central nervous system steroid receptor-mediated mechanism in cat. Proc. Natl. Acad. Sci. USA 1987, 84, 7788–7792. [Google Scholar] [CrossRef]
- Tyler, J.M. The effect of progesterone on the respiration of patients with emphysema and hypercapnia. J. Clin. Investig. 1960, 39, 34–41. [Google Scholar] [CrossRef] [PubMed]
- Sharma, G.; Goodwin, J. Effect of aging on respiratory system physiology and immunology. Clin. Interv. Aging 2006, 1, 253–260. [Google Scholar] [CrossRef]
- Janssens, J.P.; Pache, J.C.; Nicod, L.P. Physiological changes in respiratory function associated with ageing. Eur. Respir. J. 1999, 13, 197–205. [Google Scholar] [CrossRef]
- Kraut, J.A.; Madias, N.E. Re-Evaluation of the Normal Range of Serum Total CO(2) Concentration. Clin. J. Am. Soc. Nephrol. 2018, 13, 343–347. [Google Scholar] [CrossRef]
- Brinkman, J.E.; Toro, F.; Sharma, S. Physiology, Respiratory Drive. In StatPearls; StatPearls: Treasure Island, FL, USA, 2025. [Google Scholar]
- Cummins, E.P.; Strowitzki, M.J.; Taylor, C.T. Mechanisms and Consequences of Oxygen and Carbon Dioxide Sensing in Mammals. Physiol. Rev. 2020, 100, 463–488. [Google Scholar] [CrossRef]
- Petersson, J.; Glenny, R.W. Gas exchange and ventilation-perfusion relationships in the lung. Eur. Respir. J. 2014, 44, 1023–1041. [Google Scholar] [CrossRef]
- Jubran, A. Pulse oximetry. Crit. Care 2015, 19, 272. [Google Scholar] [CrossRef] [PubMed]
- Chan, E.D.; Chan, M.M.; Chan, M.M. Pulse oximetry: Understanding its basic principles facilitates appreciation of its limitations. Respir. Med. 2013, 107, 789–799. [Google Scholar] [CrossRef]
- Senewiratne, N.L.; Woodall, A.; Can, A.S. Sodium Bicarbonate. In StatPearls; StatPearls: Treasure Island, FL, USA, 2025. [Google Scholar]
- Nowicki, M.; DeVries, T.; Siegel, D.A. The Influence of Air-Sea CO2 Disequilibrium on Carbon Sequestration by the Ocean’s Biological Pump. Glob. Biogeochem. Cycles 2024, 38, e2023GB007880. [Google Scholar] [CrossRef]
- Centor, R.M. Serum Total Carbon Dioxide. In Clinical Methods: The History, Physical, and Laboratory Examinations, 3rd ed.; Walker, H.K., Hall, W.D., Hurst, J.W., Eds.; Butterworths: Boston, MA, USA, 1990. [Google Scholar]
- Falk, J.L.; Rackow, E.C.; Weil, M.H. End-tidal carbon dioxide concentration during cardiopulmonary resuscitation. N. Engl. J. Med. 1988, 318, 607–611. [Google Scholar] [CrossRef] [PubMed]
- Shapiro, I.; Stein, J.; MacRae, C.; O’Reilly, M. Pulse oximetry values from 33,080 participants in the Apple Heart & Movement Study. NPJ Digit. Med. 2023, 6, 134. [Google Scholar] [CrossRef]
- Duan, D.; Perin, J.; Osman, A.; Sgambati, F.; Kim, L.J.; Pham, L.V.; Polotsky, V.Y.; Jun, J.C. Effects of sex, age, and body mass index on serum bicarbonate. Front. Sleep. 2023, 2, 1195823. [Google Scholar] [CrossRef]
- Amodu, A.; Abramowitz, M.K. Dietary acid, age, and serum bicarbonate levels among adults in the United States. Clin. J. Am. Soc. Nephrol. 2013, 8, 2034–2042. [Google Scholar] [CrossRef]
- Dhokalia, A.; Parsons, D.J.; Anderson, D.E. Resting end-tidal CO2 association with age, gender, and personality. Psychosom. Med. 1998, 60, 33–37. [Google Scholar] [CrossRef]
- Gray, S.H.; Ebe, L.K.; Feldman, H.A.; Emans, S.J.; Osganian, S.K.; Gordon, C.M.; Laufer, M.R. Salivary progesterone levels before menarche: A prospective study of adolescent girls. J. Clin. Endocrinol. Metab. 2010, 95, 3507–3511. [Google Scholar] [CrossRef][Green Version]
- Winter, J.S.; Faiman, C. Pituitary-gonadal relations in female children and adolescents. Pediatr. Res. 1973, 7, 948–953. [Google Scholar] [CrossRef]
- Lee, P.A.; Migeon, C.J. Puberty in boys: Correlation of plasma levels of gonadotropins (LH, FSH), androgens (testosterone, androstenedione, dehydroepiandrosterone and its sulfate), estrogens (estrone and estradiol) and progestins (progesterone and 17-hydroxyprogesterone). J. Clin. Endocrinol. Metab. 1975, 41, 556–562. [Google Scholar] [CrossRef] [PubMed]
- Henderson, V.W. Gonadal hormones and cognitive aging: A midlife perspective. Womens Health 2011, 7, 81–93. [Google Scholar] [CrossRef]
- Thomas, P.; Pang, Y. Protective actions of progesterone in the cardiovascular system: Potential role of membrane progesterone receptors (mPRs) in mediating rapid effects. Steroids 2013, 78, 583–588. [Google Scholar] [CrossRef]
- Hermsmeyer, R.K.; Thompson, T.L.; Pohost, G.M.; Kaski, J.C. Cardiovascular effects of medroxyprogesterone acetate and progesterone: A case of mistaken identity? Nat. Clin. Pract. Cardiovasc. Med. 2008, 5, 387–395. [Google Scholar] [CrossRef]
- Kannel, W.B.; Hjortland, M.C.; McNamara, P.M.; Gordon, T. Menopause and risk of cardiovascular disease: The Framingham study. Ann. Intern. Med. 1976, 85, 447–452. [Google Scholar] [CrossRef]
- Lin, C.M.; Davidson, T.M.; Ancoli-Israel, S. Gender differences in obstructive sleep apnea and treatment implications. Sleep Med. Rev. 2008, 12, 481–496. [Google Scholar] [CrossRef]
- Jordan, A.S.; White, D.P.; Lo, Y.L.; Wellman, A.; Eckert, D.J.; Yim-Yeh, S.; Eikermann, M.; Smith, S.A.; Stevenson, K.E.; Malhotra, A. Airway dilator muscle activity and lung volume during stable breathing in obstructive sleep apnea. Sleep 2009, 32, 361–368. [Google Scholar] [CrossRef] [PubMed]
- Whittle, A.T.; Marshall, I.; Mortimore, I.L.; Wraith, P.K.; Sellar, R.J.; Douglas, N.J. Neck soft tissue and fat distribution: Comparison between normal men and women by magnetic resonance imaging. Thorax 1999, 54, 323–328. [Google Scholar] [CrossRef] [PubMed]
- Kellum, J.A. Determinants of blood pH in health and disease. Crit. Care 2000, 4, 6–14. [Google Scholar] [CrossRef][Green Version]
- Li, L.; Shi, M.; Umbach, D.M.; Bricker, K.; Fan, Z. Sex- and age-differences in supine positional obstructive sleep apnea in children and adults. Sleep. Breath. 2025, 29, 106. [Google Scholar] [CrossRef]
- Yaffe, K.; Laffan, A.M.; Harrison, S.L.; Redline, S.; Spira, A.P.; Ensrud, K.E.; Ancoli-Israel, S.; Stone, K.L. Sleep-disordered breathing, hypoxia, and risk of mild cognitive impairment and dementia in older women. JAMA 2011, 306, 613–619. [Google Scholar] [CrossRef] [PubMed]
- Sjoding, M.W.; Dickson, R.P.; Iwashyna, T.J.; Gay, S.E.; Valley, T.S. Racial Bias in Pulse Oximetry Measurement. N. Engl. J. Med. 2020, 383, 2477–2478. [Google Scholar] [CrossRef] [PubMed]

| Age Group (y) | EHR Data Set (N = 53,252) | PSG Data Set (N = 21,477) | ||||||
|---|---|---|---|---|---|---|---|---|
| Female (N = 32,760) | Male (N = 20,492) | Female (N = 10,568) | Male (N = 10,909) | |||||
| N | % | N | % | N | % | N | % | |
| [2,5) | 276 | 0.8 | 396 | 1.9 | 376 | 3.6 | 510 | 4.7 |
| [5,10) | 361 | 1.1 | 387 | 1.9 | 583 | 5.5 | 771 | 7.1 |
| [10,15) | 460 | 1.4 | 427 | 2.1 | 456 | 4.3 | 586 | 5.4 |
| [15,20) | 852 | 2.6 | 491 | 2.4 | 393 | 3.7 | 386 | 3.5 |
| [20,25) | 1310 | 4.0 | 541 | 2.6 | 285 | 2.7 | 323 | 3.0 |
| [25,30) | 1603 | 4.9 | 657 | 3.2 | 411 | 3.9 | 335 | 3.1 |
| [30,35) | 1951 | 6.0 | 830 | 4.1 | 556 | 5.3 | 507 | 4.6 |
| [35,40) | 2062 | 6.3 | 1002 | 4.9 | 694 | 6.6 | 730 | 6.7 |
| [40,45) | 2338 | 7.1 | 1166 | 5.7 | 886 | 8.4 | 923 | 8.5 |
| [45,50) | 2775 | 8.5 | 1473 | 7.2 | 1070 | 10.1 | 986 | 9.0 |
| [50,55) | 2884 | 8.8 | 1761 | 8.6 | 1151 | 10.9 | 982 | 9.0 |
| [55,60) | 3063 | 9.3 | 2047 | 10.0 | 1090 | 10.3 | 1032 | 9.5 |
| [60,65) | 3062 | 9.3 | 2137 | 10.4 | 859 | 8.1 | 808 | 7.4 |
| [65,70) | 2842 | 8.7 | 2117 | 10.3 | 758 | 7.2 | 821 | 7.5 |
| [70,75) | 2595 | 7.9 | 1828 | 8.9 | 485 | 4.6 | 583 | 5.3 |
| [75,105) | 4326 | 13.2 | 3232 | 15.8 | 515 | 4.9 | 626 | 5.7 |
| EHR Data Set a | PSG Data Set b | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Female–Male Difference c | Female–Male Difference c | |||||||||
| Outcome | Sex | Total Patients | Mean | SD | Test Statistic | p Value | Mean | SD | Test Statistic | p Value |
| Age (y) | F | 32,760 | 52 | 20 | 45 | 21 | ||||
| M | 20,492 | 54 | 21 | −9.92 | <0.0001 | 44 | 22 | 3.52 | 0.01 | |
| BMI (kg/m2) | F | 32,760 | 31 | 8 | 33 | 11 | ||||
| M | 20,492 | 29 | 7 | 17.91 | <0.0001 | 51 | 9 | 20 | <0.0001 | |
| O2 saturation (%) | F | 14,132 | 97.37 | 1.84 | 96.73 | 2.04 | ||||
| M | 9204 | 96.98 | 1.9 | 15.64 | <0.0001 | 96.33 | 2.01 | 14.36 | <0.0001 | |
| CO2 d | F | 27,294 | 26.6 | 3.2 | 40 | 5 | ||||
| M | 16,628 | 26.8 | 3.2 | −6.76 | <0.0001 | 39.7 | 4.9 | 3.89 | <0.0001 | |
| HR (bpm) | F | 13,724 | 82 | 13 | 76 | 14 | ||||
| M | 8871 | 80 | 14 | 11.09 | <0.0001 | 74 | 15 | 12.81 | <0.0001 | |
| RR (bpm) | F | 11,217 | 17.18 | 2.34 | 16.4 | 3.9 | ||||
| M | 7279 | 17.44 | 2.51 | −6.37 | <0.0001 | 16.2 | 4.1 | 3.82 | <0.0001 | |
| Disease | Sex | Total Patients | N | % | Test Statistic | p Value | N | % | Test Statistic | p Value |
| Coronary Heart Disease | F | 32,760 | 1120 | 3.4 | 374 | 3.5 | <0.0001 | |||
| M | 20,492 | 1792 | 8.7 | 691.8 | <0.0001 | 665 | 6.1 | 76.23 | ||
| Pulmonary Embolism | F | 32,760 | 73 | 0.2 | 99 | 0.9 | 0.30 | |||
| M | 20,492 | 76 | 0.4 | 9.9 | 0.002 | 88 | 0.8 | 1.05 | ||
| Emphysema | F | 32,760 | 1145 | 3.5 | 248 | 2.3 | 0.40 | |||
| M | 20,492 | 1139 | 5.6 | 130.7 | <0.0001 | 236 | 2.2 | 0.82 | ||
| Heart Failure | F | 32,760 | 247 | 0.8 | 35 | 0.3 | 0.70 | |||
| M | 20,492 | 191 | 0.9 | 4.9 | 0.027 | 40 | 0.4 | 0.19 | ||
| COPD | F | 32,760 | 926 | 2.8 | 468 | 4.4 | 0.002 | |||
| M | 20,492 | 722 | 3.5 | 20.4 | <0.0001 | 391 | 3.6 | 9.96 | ||
| Female | Male | Female−Male | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Outcome | Pre–Post Boundary | Estimate a | Confidence Limits | Estimate | Confidence Limits | Estimate | Confidence Limits | p Value | |||
| Lower | Upper | Lower | Upper | Lower | Upper | ||||||
| EHR | |||||||||||
| O2 | Puberty | 0.37 | 0.18 | 0.56 | 0.17 | −0.02 | 0.37 | 0.20 | −0.07 | 0.47 | 0.15 |
| Menopause | −1.31 | −1.38 | −1.24 | −0.94 | −1.03 | −0.85 | −0.37 | −0.48 | −0.25 | <0.0001 | |
| HCO3− | Puberty | 1.65 | 1.07 | 2.23 | 2.22 | 1.67 | 2.76 | −0.57 | −1.37 | 0.22 | 0.16 |
| Menopause | 1.98 | 1.88 | 2.07 | 0.05 | −0.09 | 0.18 | 1.93 | 1.77 | 2.09 | <0.0001 | |
| HR | Puberty | −8.42 | −10.19 | −6.65 | −9.16 | −10.82 | −7.50 | 0.74 | −1.69 | 3.16 | 0.61 |
| Menopause | −6.12 | −6.64 | −5.59 | −6.58 | −7.29 | −5.87 | 0.46 | −0.42 | 1.34 | 0.61 | |
| RR | Puberty | −3.10 | −3.39 | −2.80 | −3.07 | −3.37 | −2.78 | −0.02 | −0.44 | 0.39 | 0.91 |
| Menopause | 0.27 | 0.17 | 0.37 | 0.17 | 0.04 | 0.31 | 0.10 | −0.08 | 0.27 | 0.55 | |
| PSG | |||||||||||
| O2 | Puberty | 0.18 | 0.01 | 0.35 | −0.17 | −0.33 | −0.02 | 0.35 | 0.12 | 0.59 | 0.0027 |
| Menopause | −1.49 | −1.59 | −1.40 | −0.74 | −0.84 | −0.65 | −0.75 | −0.88 | −0.61 | <0.0001 | |
| ETCO2 | Puberty | 0.60 | 0.16 | 1.05 | 1.61 | 1.21 | 2.02 | −1.01 | −1.61 | −0.40 | 0.0011 |
| Menopause | 0.71 | 0.46 | 0.96 | −2.12 | −2.36 | −1.87 | 2.83 | 2.48 | 3.18 | <0.0001 | |
| HR | Puberty | −15.35 | −16.47 | −14.23 | −14.73 | −15.75 | −13.71 | −0.62 | −2.14 | 0.89 | 0.42 |
| Menopause | −6.50 | −7.12 | −5.87 | −5.55 | −6.16 | −4.93 | −0.95 | −1.83 | −0.07 | 0.07 | |
| RR | Puberty | −2.68 | −3.02 | −2.34 | −3.1 | −3.41 | −2.79 | 0.42 | −0.03 | 0.88 | 0.07 |
| Menopause | −1.16 | −1.35 | −0.97 | −0.84 | −1.03 | −0.65 | −0.32 | −0.59 | −0.06 | 0.04 | |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Li, L.; Shi, M.; Umbach, D.M.; Fan, Z. Age Trajectories of O2 Saturation and Levels of Serum Bicarbonate or End-Tidal CO2 Across the Life Course of Women and Men: Insights from EHR and PSG Data. Biomolecules 2025, 15, 884. https://doi.org/10.3390/biom15060884
Li L, Shi M, Umbach DM, Fan Z. Age Trajectories of O2 Saturation and Levels of Serum Bicarbonate or End-Tidal CO2 Across the Life Course of Women and Men: Insights from EHR and PSG Data. Biomolecules. 2025; 15(6):884. https://doi.org/10.3390/biom15060884
Chicago/Turabian StyleLi, Leping, Min Shi, David M. Umbach, and Zheng Fan. 2025. "Age Trajectories of O2 Saturation and Levels of Serum Bicarbonate or End-Tidal CO2 Across the Life Course of Women and Men: Insights from EHR and PSG Data" Biomolecules 15, no. 6: 884. https://doi.org/10.3390/biom15060884
APA StyleLi, L., Shi, M., Umbach, D. M., & Fan, Z. (2025). Age Trajectories of O2 Saturation and Levels of Serum Bicarbonate or End-Tidal CO2 Across the Life Course of Women and Men: Insights from EHR and PSG Data. Biomolecules, 15(6), 884. https://doi.org/10.3390/biom15060884





