Abstract
Lower urinary tract symptoms (LUTS) are common in postmenopausal women. These symptoms are often linked to decreased estrogen levels following menopause. This study investigated the relationship between estrogen levels, alterations in bladder tissue structure, bladder function, and the incidence of urinary frequency. An age-appropriate bilateral ovariectomized mouse model (OVX) was developed to simulate conditions of estrogen deficiency. Mice were divided into three groups: a sham-operated control group, OVX, and an estradiol-treated group. The assessments included estrogen level measurement, urination frequency, cystometry, histological analysis, immunofluorescence staining, and real-time quantitative PCR. Additionally, we quantified the expression of the mechanosensitive channel proteins Piezo1 and TRPV4 in mouse bladder tissues. Lower estrogen levels were linked to increased voiding episodes and structural changes in mouse bladder tissues, notably a significant increase in Collagen III fiber deposition. There was a detectable negative relationship between estrogen levels and the expression of Piezo1 and TRPV4, mechanosensitive proteins in mouse bladder tissues, which may influence voiding frequency and nocturia. Estrogen treatment could improve bladder function, decrease urination frequency, and reduce collagen deposition in the bladder tissues. This study explored the connection between estrogen levels and urinary frequency, potentially setting the stage for novel methods to address frequent urination symptoms in postmenopausal women.
1. Introduction
Lower urinary tract symptoms (LUTS), which include urinary frequency, urgency, nocturia, and overactive bladder, affect approximately 57–72.6% of women [1,2]. These symptoms are closely associated with estrogen deficiency, a critical factor in the progression of LUTS in aging women [3]. A thorough scientific investigation is necessary to explore the mechanisms that influence how varying levels of estrogen impact voiding frequency in this demographic. Recent studies by Christmas and Russo et al. demonstrated that estradiol can improve urodynamic parameters such as maximal bladder capacity, decrease non-voiding contractions of urethral muscles, and potentially alleviate symptoms like frequent urination [4,5]. Although some studies suggest a correlation between estrogen levels and urination frequency, the effectiveness of estrogen replacement therapy in addressing voiding frequency due to postmenopausal estrogen decline remains unclear [6]. This uncertainty emphasizes the importance of continued research into how estrogen levels affect the onset, progression, and potential relief of voiding frequency.
In addition to its role in urinary frequency symptoms, estrogen levels are connected to changes in bladder tissue structure. The lower urinary tract, including both urethral and bladder tissues, contains estrogen receptors [7,8]. Research has shown that estrogen deficiency can damage the bladder tissue structure, whereas estrogen supplementation was shown to increase bladder weight and vascular density within bladder tissues [9]. Moreover, the elasticity of urethral and bladder tissues, which affects various storage phase symptoms, was linked to estrogen levels [7]. Despite these insights, studies examining the link between estrogen levels and structural changes in bladder tissue are still limited.
The mechanosensitive channel Piezo1 is widely distributed throughout the urinary system, primarily found in uroepithelial and mesenchymal cells, as well as in a subset of smooth muscle cells within bladder tissue [10]. As a mechanosensitive ion channel, Piezo1 plays a vital role in detecting bladder stretch, which is crucial for urine storage and release [11]. The activation of Piezo1 by bladder stretching triggers a sequence of events beginning with the flow of intracellular calcium ions, influencing sensations of bladder filling and the subsequent processes of urination [12]. Impaired Piezo1 expression or activity can compromise bladder sensing mechanisms, leading to dysuria. Moreover, the involvement of Piezo1 in urinary frequency is believed to arise from its role in regulating the response of bladder tissue to mechanical stimuli, impacting urine production and release [13,14]. Similarly, the transient receptor potential channel TRPV4, which responds to mechanical, thermal, and certain chemical stimuli, is found in bladder epithelial cells. It plays a role in monitoring bladder filling, thereby managing urine storage and release. The significance of TRPV4 in maintaining normal bladder function is highlighted by the abnormal bladder activity seen in TRPV4-knockout mice [15,16,17,18]. The overactivation of TRPV4 was associated with bladder overactivity and increased urinary frequency. Notably, TRPV4 antagonists have shown effectiveness in alleviating stress-induced bladder issues by improving bladder capacity and reducing urinary frequency, suggesting that TRPV4 is a potential therapeutic target for treating bladder disorders, including overactive bladder [19]. The link between menopausal LUTSs and the expression levels of these channel proteins warrants further investigation.
We hypothesize that the lower urinary tract of the OVX animals will deteriorate alongside estrogen deficiency and that changes in urinary frequency may correlate with collagen deposition and the expression of Piezo1 and TRPV4. In this study, we established an induced surgical menopause model in mice, with and without bilateral ovary removal, to explore the relationship between estrogen levels and changes in urination frequency and bladder tissue structure.
2. Materials and Methods
2.1. Experimental Design of Animal Model
Twenty-four female C57BL/6 mice, weighing between 17.0 and 18.0 g, were sourced from the animal center at GuangXi University. The experimental protocols received approval from the Committee for the Use of Experimental Animals at GuangXi University (approval number: Gxu-2021-1002). The mice were randomly allocated into SHAM, OVX, and E2 groups. For the OVX group, estrogen deficiency was induced through bilateral ovariectomy (OVX) surgery lasting 4 weeks. The procedure involved making a 1 cm incision on both sides of the spine of the female mice, followed by the removal of both ovaries. The OVX surgery was conducted under Tribromoethanol (M2910, Nanjing, China) anesthesia (Figure 1A). In the SHAM group, a similar incision was made, but only the adipose tissue surrounding the ovaries was removed (Figure 1B). The dosage of estrogen for the intervention was determined based on previous studies [20]. In the E2 group, β-estradiol (E8857, Sigma-Aldrich, Saint Louis, MO, USA) was administered at a dosage of 100 μg/kg/day via gavage starting one week after the bilateral OVX surgery (Figure 1C). Serum estrogen levels were measured using an ELISA four weeks post-OVX (Figure 1D). A urine study was conducted across all three groups within the 4-week period. Subsequently, the animals were euthanized, and their bladders were harvested for histological analysis. The experimental protocol adhered to the guidelines depicted in Figure 1E.
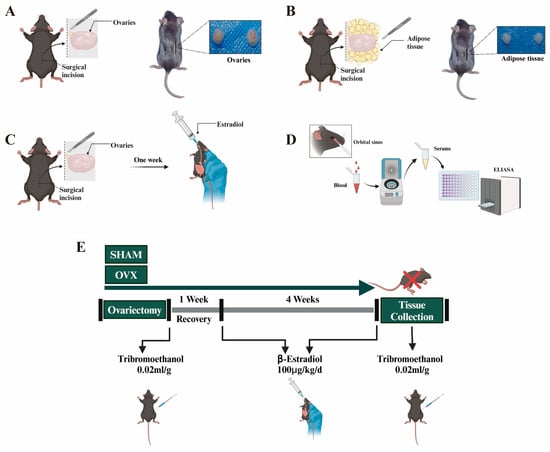
Figure 1.
Development of mice experimental models: (A–C) implementation of experimental protocols in mice, involving bilateral oophorectomy (OVX), sham operation as a control (SHAM), and estrogen intervention; (D) procedures for blood sampling and estrogen level quantification using ELISA technique in mice; (E) details of the estrogen intervention protocol, including dosage and duration.
2.2. Evaluation of Estradiol Level
Serum was collected, and the serum estradiol concentration was determined using an estradiol ELISA kit (Elabscience, Wuhan, China) according to the manufacturer’s instructions [21]. The estradiol concentration was measured at 450 nm using an ELISA reader (Multiskan™ FC, Waltham, MA, USA).
2.3. Statistics on the Frequency of Urination
The frequency of urination was assessed starting 4 weeks post-OVX surgery. Mice were individually housed in 32 cm × 13.5 cm cages, and after a 48 h acclimation period, urine output was collected over 12 h light/12 h dark cycles using filter paper that covered the entire cage floor. To prevent damage to the filter paper, a plastic mesh with 0.8 cm diameter holes was placed over it. During the 48 h observation period, mice had access to water and food ad libitum. The frequency and intervals of urination were documented using video recording software. The urination events were carefully counted from the recorded videos. To ensure the reliability and accuracy of the data, the video analysis was consistently performed by the same individual. At the end of the 4-week period, the data underwent semi-quantitative analysis.
2.4. Bladder Cystometry (Urodynamics)
The cystometry was measured in accordance with the method previously described [19]. For cystometry, mice were anesthetized with tribromoethanol, which was administered intraperitoneally. Prior to surgery, abdominal hair was removed, and a 1 cm longitudinal incision was made in the lower abdomen to access the bladder. The skin and then the peritoneum were incised. After inspecting and moving aside surrounding fatty tissue, the bladder was exposed and carefully lifted using toothless forceps. A PE-10 catheter was inserted into the bladder wall via a syringe needle, secured with a knot, and routed subcutaneously to emerge at the neck area. The catheter’s end was sealed, and the abdominal incision was closed, layering skin, subcutaneous tissue, and muscle. Cystometry was performed two days post-catheterization using a pressure transducer (YPJ01, Chengdu, China) and flow pump connected to the catheter via a three-way tube. The cystometry assay involved infusing 0.9% saline at room temperature into the bladder at a rate of 0.03 mL/min. Bladder pressure was continuously recorded, analyzing at least five consecutive voiding cycles to assess intravesical pressure-related variables. Bladder capacity was calculated by multiplying the infusion rate by the duration until the onset of micturition, and maximum voiding pressure was defined as the peak pressure exerted by the detrusor muscle during voiding.
2.5. Masson Staining
The entire bladder weight was recorded. Frozen bladder sections, 5 μm thick, were air-dried and fixed in polyformaldehyde. Masson staining was performed using a commercially available Masson staining kit (Solarbio, Beijing, China), which stains collagen blue and smooth muscle red in each image [22]. Sirius Red staining was also conducted according to the Sirius Red staining kit protocol (Solarbio, Beijing, China), using a polarization microscope to distinguish different types of collagen within the samples [23]. Morphometric evaluation was performed on the samples. Using ImageJ/Fiji software version 1.53q (NIH, Bethesda, MD, USA), the total areas occupied by smooth muscle and collagen were quantified, and the ratio of collagen area to smooth muscle area was calculated.
2.6. Immunofluorescence Staining
The immunofluorescence staining procedure followed the methodology used in previous studies [11]. Whole bladder tissues were fixed in cold 4% paraformaldehyde in 0.1 M phosphate-buffered saline (PBS, pH 7.4) overnight. For antigen retrieval, tissue sections were boiled in sodium citrate buffer (pH 6.0) for 15 min. Subsequently, sections were permeabilized with 0.5% Triton X-100 at room temperature for 10 min, followed by three 5 min washes in PBS. The bladder sections were blocked in sheep serum working solution for 30 min. The slides were then incubated overnight at 4 °C with primary antibodies: rabbit polyclonal anti-E-cadherin (AF0131, Affinity, Changzhou, China) at 1:150, rabbit polyclonal anti-Piezo1 (DF12083, Affinity, Changzhou, China) at 1:150, and rabbit polyclonal anti-TRPV4 (DF8624, Affinity, Changzhou, China) at 1:150 in 0.5% BSA solution. After washing in PBS for 15 min, the slides were incubated with Goralite 488 goat anti-rabbit secondary antibodies (SA00013-2, Proteintech, Wuhan, China) diluted 1:400 at room temperature for 2 h. Finally, the slides were sealed with anti-fluorescence attenuation sealing tablets containing DAPI (Solarbio, Beijing, China). Images were captured using a fluorescent microscope (Olympus BX53F2, Tokyo, Japan). All images were taken under the same photography conditions to enable direct comparison between experimental animals and controls. To measure fluorescence signal intensity, the mean gray value was determined using ImageJ/Fiji software version 1.53q (NIH, Bethesda, MD, USA). The procedures were as follows: For a single-channel (monochromatic) fluorescence image, the gray value of each pixel indicated the fluorescence intensity at that point. The formula for calculating fluorescence intensity in a specific region was average fluorescence intensity (mean) = total fluorescence intensity of the region (IntDen)/area of the region (Area) (Mean: mean gray value; IntDen: integrated density).
2.7. Quantitative Real-Time PCR Assay
qRT-PCR was conducted following the manufacturer’s guidelines. Total RNA was extracted using a Trizol reagent (Invitrogen, Carlsbad, CA, USA). The reverse transcription was carried out with a high-capacity cDNA reverse transcription kit (Thermoscientific, Waltham, MA, USA). The cDNA was then amplified via PCR using SYBR-Green dye and the ABI Power SYBR-Green PCR Master Mix kit (Applied Biosystems, Foster City, CA, USA). Mouse primers were designed using Primer 3 software and synthesized by Sangon Biotech Co., Ltd. (Shanghai, China) (Table 1). The relative mRNA expression levels were determined using the 2−∆∆Ct method, with mouse β-actin (Sangon, Shanghai, China) serving as the internal control. Each experiment was independently performed three times, with the averages taken for further analysis.

Table 1.
Primers used for quantitative PCR.
2.8. Statistical Analysis
Data analysis and graphing were performed using GraphPad Prism (Version 9.0, San Diego, CA, USA). Results are presented as means ± standard deviation (SD). Normality tests were conducted for all experimental datasets. Independent data were analyzed using one-way analysis of variance (ANOVA) with Tukey’s post hoc test for multiple comparisons if the data followed a normal distribution. If not, the non-parametric Kruskal–Wallis test with Dunn’s post hoc test was employed; p values < 0.05 were considered statistically significant: * < 0.05, ** < 0.01, *** < 0.001, **** < 0.0001.
3. Results
3.1. Establishment and Validation of Animal Models
Compared to the SHAM group, the mice in the OVX group showed a significant reduction in serum estrogen levels after four weeks of model establishment, as detailed in Table 2 (p < 0.0001). At the same point, estrogen levels in the E2 group matched those of the SHAM group, indicating that OVX effectively reduces estrogen levels. The administration of E2 notably increased circulating estrogen levels in mice. There was also a marked increase in body weight in the OVX group compared to the SHAM group (p < 0.001). Additionally, bladder weight in the E2 group was significantly higher than in the SHAM group (p < 0.01).

Table 2.
Physical indicators for the different experimental groups.
3.2. Urination Frequency in Mice Correlates with Estrogen Levels
Using the behavioral paradigm shown in (Figure 2A), the 48 h urination frequency was monitored and recorded for mice from the three groups four weeks post-establishment of the model. The OVX group displayed a statistically significant increase in 48 h urination frequency compared to the SHAM group (p < 0.01) (Figure 2B). It is important to note that the nocturnal/daytime phases correspond to awake/sleeping phases for mice. Notably, among the three groups, nocturnal urination frequency was highest in the OVX group and was significantly elevated compared to daytime urination frequency (p < 0.001) (Figure 2C). This increase in nocturnal urination frequency was reduced following estrogen treatment, as observed in the E2 group. Moreover, the intervals between urinations were significantly shorter for the OVX group during both daytime and nighttime compared to the SHAM group, a trend that was regressed with estrogen treatment (Figure 2D,E). Figure 2D,E display the number of data points representing the time intervals between adjacent micturition events across three mouse groups. The correlation between the level of estrogen and the urination frequency was analyzed using the Pearson correlation analysis. A negative correlation was found between the frequency of urination in mice and their estrogen levels (p < 0.0001, Figure 2F).
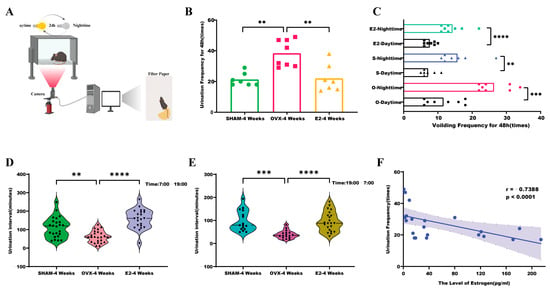
Figure 2.
Association of estrogen fluctuations with altered urinary frequency in mice: (A) methodology for assessing urinary behavior in mice; (B) comparative analysis of voiding frequency over 48 h in OVX, SHAM, and E2 groups; (C) assessment of diurnal variations in 48 h urinary frequency among OVX, SHAM, and E2 groups after 4 weeks of model establishment. The number of data points representing the time intervals between adjacent micturition events across three mouse groups; (D,E) investigation of urination intervals (daytime and nighttime) in OVX, SHAM, and E2 groups; (F) correlation analysis between estrogen levels and voiding frequency. R, Pearson correlation coefficient; p-value, two-tailed p-value of the Pearson correlation. Statistical significance denoted as ** p < 0.01; *** p < 0.001; **** p < 0.0001.
3.3. Bladder Function Is Correlated with Estrogen Levels in Mice
Bladder function assessments, based on urodynamic parameters such as peak pressure, voiding frequency, baseline pressure, and bladder capacity, are depicted in Figure 3. Mice in the SHAM group exhibited regular and steady voiding patterns, as shown in Figure 3A. In contrast, mice in the OVX group demonstrated an increased voiding frequency, which decreased following estrogen intervention (Figure 3B,C). Peak bladder pressure, indicated by arrows, was lower in the OVX group compared to the SHAM and E2 groups (Figure 3E). A comparison between the SHAM and E2 groups with the OVX group showed a significant reduction in bladder capacity in the OVX group (p < 0.05; p < 0.01) (Figure 3D). As depicted in Figure 3F, the interval between micturitions was shorter in the OVX group compared to the SHAM group (p < 0.05). However, after estrogen intervention, the interval between micturitions increased (p < 0.001). Baseline bladder pressure changes showed no significant correlation with estrogen levels across the groups (Figure 3G). Collectively, these findings suggest that bladder capacity and function are compromised in OVX mice but improve with estrogen intervention, indicating a relationship between estrogen levels and bladder function.
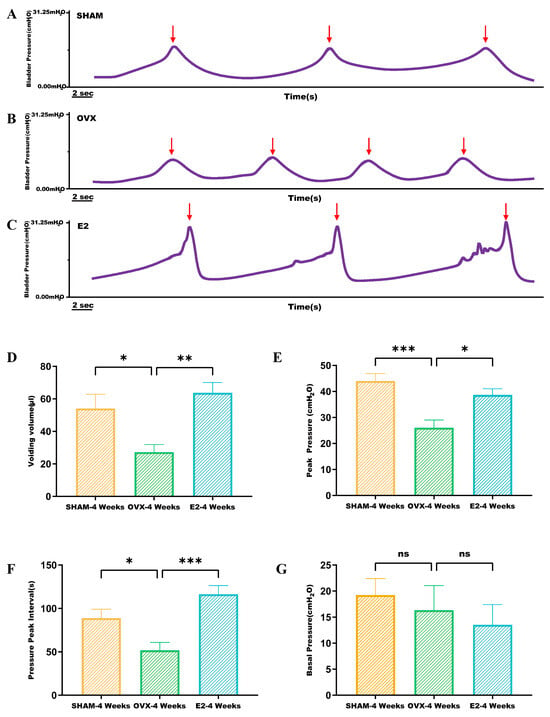
Figure 3.
Urodynamic analysis was conducted to evaluate cystometric parameters in three groups of mice, namely SHAM, OVX, and E2: (A–C) cystometry in SHAM, OVX, and E2 group mice recorded changes in intravesical pressure, voiding time, and bladder contractions (arrows); (D–G) comparison of voiding volume, peak pressure, pressure peak interval, and baseline pressure of mice in SHAM, OVX, and E2 groups. Statistical significance denoted as * p < 0.05; ** p < 0.01; *** p < 0.001; ns indicates non-significant.
3.4. Estrogen Intervention Decreases Collagen Deposition in Bladder Tissue
Masson staining indicated that in the bladder tissue of mice from the SHAM group, smooth muscle fibers were neatly arranged, with scattered collagen fibers distributed sparsely between the uroepithelium and the smooth muscle layer. Conversely, in the OVX group, the arrangement of these fibers differed. The bladder tissue of mice in the OVX group exhibited numerous disorganized collagen fibers between the uroepithelium and the smooth muscle layer. However, in the E2 group, the collagen fibers in the bladder tissue significantly declined following estrogen intervention (Figure 4A).
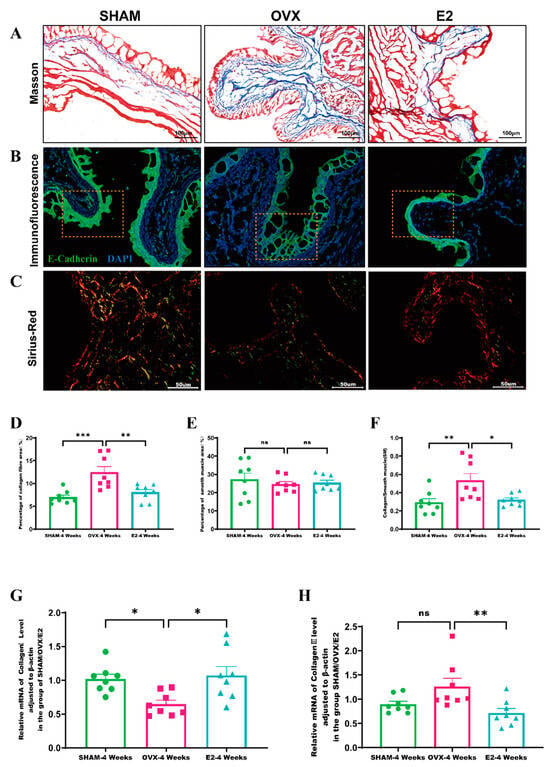
Figure 4.
Alterations in bladder histology attributable to estrogen level variations: (A) Masson’s trichrome staining of bladder tissues from OVX, SHAM, and E2 group mice. This technique demarcates muscle fibers in red, collagen fibers in blue, and uroepithelial tissue in pink; (B) Immunofluorescence staining for E-cadherin in bladder tissues of mice in OVX, SHAM, and E2 groups (yellow dotted box); (C) Sirius Red staining applied to bladder tissues of mice in OVX, SHAM, and E2 groups for collagen detection; (D–F) comparative evaluation of the collagen fiber area, smooth muscle area, and the collagen-to-smooth muscle ratio in bladder tissues of each group; (G,H) quantitative analysis of Collagen I and Collagen III in bladder tissues across all groups. Statistical significance denoted as * p < 0.05; ** p < 0.01; *** p < 0.001; ns indicates non-significant.
In the SHAM group mice’s bladder tissue, E-cadherin was predominantly located at the uroepithelial cell junctions. In contrast, the OVX group showed lower E-cadherin expression and weaker fluorescence intensity. Estrogen intervention restored E-cadherin fluorescence intensity in the uroepithelium to levels similar to those in the SHAM group (Figure 4B). Meanwhile, semi-quantitative analysis was performed to assess the proportion of collagen fibers and smooth muscle [24] tissue, as well as the ratio of collagen fibers to SM. Four weeks after model establishment, there was a significant increase in the percentage of collagen fibers in the bladder tissue of the OVX group compared to the SHAM group (p < 0.001). The percentage of collagen fibers significantly declined following estrogen intervention (p < 0.01) (Figure 4D). However, no significant changes were observed in SM composition within the bladder tissues of the three groups (Figure 4E). The ratio of collagen fibers to SM in the bladder tissue was significantly higher in the OVX group than in the SHAM group (p < 0.01), and this ratio decreased after estrogen intervention (p < 0.05) (Figure 4F). Sirius Red staining was used to visualize the distribution of Collagen I and Collagen III in the bladder tissues of the three different mouse groups (Figure 4C). Additionally, qRT-PCR was employed to measure the transcript levels of Collagen types I and III in these groups. As shown in Figure 4 and Figure 5, the levels of beta-actin transcripts were stably detected, and the Ct values were 17.04 ± 0.220,17.02 ± 0.294 and 17.01 ± 0.291, respectively.
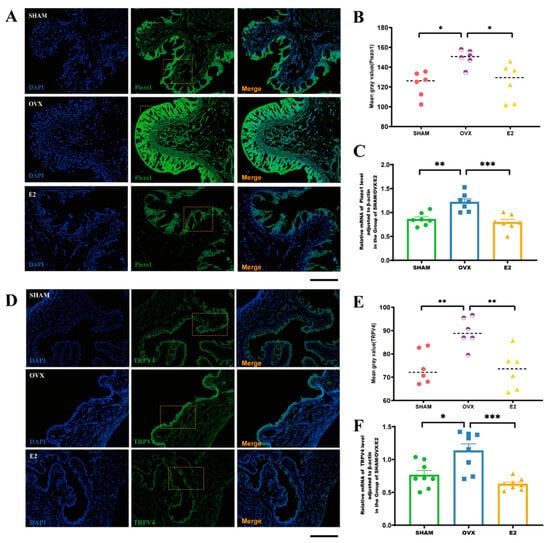
Figure 5.
Correlation between estrogen levels and the expression of Piezo1 and TRPV4 in bladder tissues: (A) immunostaining-based localization of Piezo1 in OVX, SHAM, and E2 groups (yellow dotted box); (B) semi-quantitative analysis of the mean gray value for Piezo1 in OVX, SHAM, and E2 groups; (C) assessment of relative mRNA levels of Piezo1, normalized to β-actin, in OVX, SHAM, and E2 groups; (D) immunostaining-based distribution of TRPV4 in OVX, SHAM, and E2 groups (yellow dotted box); (E) semi-quantitative analysis of the mean gray value for TRPV4 in OVX, SHAM, and E2 groups; (F) evaluation of relative mRNA levels of TRPV4, adjusted to β-actin, in OVX, SHAM, and E2 groups. Statistical significance indicated as * p < 0.05, ** p < 0.01, *** p < 0.001. Scale bar: 50 μm.
Bladder tissues from the SHAM and E2 groups showed lower transcript levels of Collagen I compared to the OVX group, as indicated in Figure 4G. Conversely, transcript levels of Collagen III were higher in the OVX group, as shown in Figure 4H. These findings suggest that decreased estrogen levels may contribute to increased collagen deposition in bladder tissues, predominantly involving Collagen III fibers. Moreover, estrogen seemed to reduce collagen deposition in bladder tissues, potentially slowing the progression of bladder tissue fibrosis.
3.5. Estrogen Intervention Decreases Transcript Levels of Piezo1 and TRPV4 in Mice Bladder Tissue
Previous studies have demonstrated that estrogen levels influence the structural composition of mice bladder tissue [9]. Given the potential association between estrogen levels and urothelial channel, the expression and transcription levels of two mechanosensitive channels, Piezo1 and TRPV4, were compared across the three groups in mice bladder tissue. The results demonstrated that bladder tissues from the OVX group showed higher fluorescence intensity and greater expression of the mechanosensitive channel Piezo1 (Figure 5A,B) and TRPV4 (Figure 5D,E) compared to the SHAM and E2 groups (p < 0.05; p < 0.01). Additionally, the OVX group exhibited increased transcriptional levels of Piezo1 and TRPV4 in bladder tissues relative to the SHAM group (p < 0.01; p < 0.05). Conversely, transcript levels of Piezo1 and TRPV4 decreased following estrogen treatment (p < 0.001; p < 0.001) (Figure 5C,F). These results suggest a significant reversed correlation between estrogen levels and the transcript levels of mechanosensitive channels such as Piezo1 and TRPV4.
4. Discussion
This study developed a bilateral OVX mouse model to simulate reduced estrogen levels in mice, establishing it as a critical tool for investigating the relationship between estrogen levels and various physiological and pathological processes [25,26,27]. Notably, an increase in urination frequency was observed in the bilateral OVX group, demonstrating a negative correlation between estrogen levels and urination frequency. Previous studies, including those by Junya Yoshida et al. and F. Aura Kullmann et al., reported increased urination frequency in rats four weeks post-bilateral ovariectomy and increased nocturnal urination five to six weeks post-procedure, respectively [28,29]. Our findings also highlighted a diurnal variation, with decreased urination frequency during the day and increased frequency at night, a pattern that became more pronounced with lower estrogen levels. Diverging from previous research, our study extended the observation window from 24 to 48 h, allowing for a more comprehensive evaluation of the relationship between estrogen levels and urination frequency.
To address the increased urination frequency in bilateral OVX mice resulting from lowered estrogen levels, estrogenic interventions were implemented. Specifically, β-estradiol was administered orally at a dosage of 100 μg/kg daily for four weeks, starting one week after ovariectomy. Our data suggested that estrogen intervention effectively restored urination frequency to pre-bilateral OVX levels. This finding aligns with the results of Liang and Willmann et al., who showed that β-estradiol administration improved voiding frequency in bilateral ovariectomized rats [30]. Moreover, numerous randomized controlled clinical trials have confirmed the efficacy of estrogen in alleviating symptoms such as nocturia, urgency, and bladder capacity irregularities, highlighting its role in improving frequent urination among postmenopausal women [31,32,33]. This study reinforces the link between estrogen levels and urinary frequency, substantiating the effectiveness of estrogenic intervention in reducing increased urinary frequency in OVX mice. Although the OVX model can simulate a state of declining estrogen levels, aging itself can cause changes in lower urinary tract symptoms, bladder tissue structure, and function. Therefore, our future research will include the study of voiding behavior, bladder tissue structure, and function in aged mice.
Estrogen levels can not only influence the frequency of urination in mice but also affect the structural integrity of bladder tissue, particularly in terms of collagen deposition. Postmenopausal alterations in bladder structure were partially attributed to changes in estrogen levels [9]. In this study, we observed collagen deposition in the bladder tissue of OVX mice. This finding is consistent with the observations of Nicole et al., who noted collagen deposition in bladder tissues of the OVX model, linked to bladder instability [34]. Similarly, a previous study has investigated the collagen to SM tissue ratios in bilaterally ovariectomized and normal bladders, finding a significantly higher ratio in the OVX model [35]. These results align with our current findings, indicating that estrogen levels predominantly influence bladder tissue structure by altering collagen amounts. Additionally, previous studies have shown that abnormal bladder tissue increases connective tissue deposition, which in turn may improve the formation of bladder trabeculae and reduce bladder tissue compliance [36,37,38]. In this study, the collagen fibers between the uroepithelium and bladder smooth muscle in the bladder tissues of mice in the OVX group were significantly increased compared to the SHAM and E2 groups. It was observed that estrogen intervention resulted in increased bladder capacity and maximum bladder pressure. Estrogen may reduce collagen deposition in bladder tissues and bladder function in mice. However, further research is needed to confirm the relationship between collagen deposition in bladder tissue and bladder function. The detrusor muscles and their innervation are particularly susceptible to long-term deficiencies in ovarian hormones, resulting in impaired contractility of the bladder’s urethral muscles [39]. Notably, declining estrogen levels lead to various changes in the genitourinary system, including hypoxia, reduced blood flow to the bladder mucosa, and increased permeability, all contributing to decreased bladder compliance and potential urinary frequency [40,41,42,43,44]. Previous studies have established a link between the mechanical properties of the bladder wall and its elastic and connective tissue content, particularly in the force-generating muscles of the bladder. These properties are believed to depend on collagen distribution [45,46]. Collagen types I and III are crucial for tissue tensile strength [47]. Our study explored the relationship between these collagen types and estrogen levels, specifically examining how estrogen correlates with the collagen fiber content in bladder tissue. We observed that estrogen levels were associated with both Collagen I and Collagen III fibers in the bladder but exhibited distinct behaviors. Specifically, in the OVX group, characterized by low estrogen levels, Collagen I fiber content and transcript levels were reduced, while Collagen III fiber content and transcript levels were elevated. These findings suggest that the decrease in estrogen levels predominantly led to the deposition of Collagen III fibers in the bladder tissues of mice. Research on the impact of altered estrogen levels on the content of and Collagen I and III fibers in bladder tissue is limited. A study by Trabucco et al. observed a significant decrease in Collagen I content in the periurethral tissues of postmenopausal patients, highlighting potential impacts on connective tissue tensile strength [48].
The present study aimed to investigate the relationship between collagen deposition and estrogen levels in mouse bladder tissues. The results suggest that ovariectomy (OVX)-induced decreases in estrogen levels are followed by increases in collagen deposition in mouse bladder tissues. This pathological change can be improved after estrogen intervention. Estrogen plays a vital role in maintaining the elasticity of the bladder and periurethral tissues, potentially inducing the hypertrophy of the bladder detrusor muscle and increasing myosin levels in bladder tissue, thereby improving bladder contractility [49,50,51]. Estrogen intervention also improved bladder vascular density and distribution, which in turn improved contractility and bladder compliance. However, the specific mechanism by which estrogen inhibits bladder collagen formation remains unclear. Existing studies have suggested that estrogen may exert a cardioprotective effect in cardiac vessels by inhibiting fibroblast proliferation and collagen deposition, potentially mediated by the release of nitric oxide from endothelial cells [52]. The primary collagen types in bladder tissue are collagen I and collagen III. Collagen I is an essential component of the extracellular matrix in bladder tissue, providing a fundamental structural element. It is closely associated with the mechanical strength of the bladder wall and plays a role in maintaining the shape and function of the bladder wall. Its synthesis and accumulation in bladder smooth muscle are critical for maintaining normal bladder function [53]. Recent studies have shown that in conditions such as chronic cystitis, excessive accumulation of collagen I may lead to fibrosis of the bladder wall, which in turn affects bladder compliance and results in dysfunction in urine storage and voiding. Collagen III is a component of the extracellular matrix in the bladder and plays a crucial role in maintaining the structural stability of the bladder wall by forming a fibrous network. This network helps preserve the structural integrity of bladder tissue under mechanical stress, thereby preventing long-term damage to the bladder wall; In pathological states, such as bladder fibrosis, the expression of collagen III increases, typically resulting in sclerosis and a decline in the functional capacity of the bladder wall. In such cases, collagen III contributes to pathological remodeling of the tissue, potentially worsening urinary storage function [54,55,56]. Our study’s findings suggest that a reduction in estrogen levels is associated with an increase in collagen III deposits in bladder tissue. Therefore, it can be hypothesized that estrogen deficiency may affect the structural integrity of the bladder, potentially leading to the development of bladder fibrosis. This may impair the bladder’s ability to store urine, resulting in symptoms such as frequent urination. In conclusion, estrogen levels are linked to collagen deposition in mouse bladder tissue, particularly affecting the expression and transcript levels of Collagen III.
This study illustrated a link between estrogen levels and changes in bladder tissue structure. It further explored how estrogen levels influence the expression of mechanosensitive channels. Various channels are present in the urothelium of bladder tissue, including the transient receptor potential channel (TRPV1, TRPV4, etc.) and the mechanosensitive channel. The mRNA levels of TRPV4 and Piezo1 are higher than those of TRPV1 in both bladder uroepithelial cells with sensory signaling and bladder lamina propria mesenchymal cells [57,58]. Piezo1 and TRPV4 in the uroepithelium are critical for sensing bladder fullness [59]. As shown in the graphical abstract presentation, previous research has revealed that Piezo1 and TRPV4 increase uroepithelial Ca2+ entry, subsequently increasing ATP release and stimulating bladder sensory nerve fiber afferents [12,60]. Recent studies have indicated that the functions of Piezo1 and TRPV4 are regulated by clock genes, which are active during waking hours and dormant during sleep, aligning with circadian rhythms [61]. Therefore, the increased expression and elevated transcript levels of Piezo1 and TRPV4 in bladder tissues, induced by decreased estrogen levels, may be linked to increased voiding frequency and nocturia. Piezo1 and TRPV4 are both expressed in bladder smooth muscle tissue and in the uroepithelial cells of mouse bladder tissue. Piezo1 is expressed in various cell types within the bladder wall, including smooth muscle and mesenchymal cells. In a mouse model, Piezo1 activation was shown to closely relate to the regulation of voiding frequency and bladder function. Intervention targeting Piezo1 can alter bladder responsiveness and, consequently, influence voiding behaviour [13]. In addition to its role in sensing bladder filling, TRPV4 was demonstrated to directly affect the contraction of bladder smooth muscle. By regulating the muscle’s mechanical sensitivity, TRPV4 plays a dual role in bladder storage and voiding. Its activation was shown to increase smooth muscle contractility by triggering the Ca²⁺ signalling pathway, thereby facilitating efficient bladder emptying [60]. Consequently, we included these two channel proteins in our study. In conjunction with our findings, suggesting that reduced estrogen levels could impair urinary epithelial barrier function, the expression and transcript levels of Piezo1 and TRPV4 channels in bladder tissue were evaluated. This assessment revealed a strong negative correlation between estrogen levels and the expression and transcript levels of Piezo1 and TRPV4. Further research is needed to understand the impact of reduced estrogen on Piezo1 and TRPV4 expression and its association with urinary frequency and nocturia.
5. Conclusions
Our findings revealed a significant negative correlation between decreased estrogen levels and urinary frequency in mice. Decreased estrogen levels are associated with Collagen III deposition in mouse bladder tissue. Estrogen supplementation improved bladder function and tissue structure and reduced collagen deposition. Given that the Piezo1 and TRPV4 levels in bladder tissue increased significantly after OVX, these proteins may be associated with frequent urination and nocturia caused by estrogen deficiency.
Author Contributions
Conceptualization, C.Z., Y.C. and Y.Z.; Methodology, C.Z., Y.Z. and J.Y.; Validation, C.Z. and L.Y.; Investigation, C.Z., G.D., X.X., X.T. and L.Y.; Data Curation, C.Z., G.D. and L.Y.; Writing—Original Draft Preparation, C.Z.; Writing—Review and Editing, Y.C., Y.Z. and J.Y.; Visualization, C.Z.; Supervision, Y.Z. and J.Y.; Funding Acquisition, J.Y. All authors have read and agreed to the published version of the manuscript.
Funding
This work was supported by the National Nature Science Foundation of China (31970946).
Institutional Review Board Statement
This study was conducted according to the guidelines of the Declaration of Helsinki and approved by the Committee for the Use of Experimental Animals at GuangXi University (approval number: Gxu-2021-1002, 4 May 2021).
Informed Consent Statement
Not applicable.
Data Availability Statement
Data are available upon request.
Acknowledgments
We would like to thank all members of the Guangxi Key Laboratory of Special Biomedicine and Advanced Institute for Brain and Intelligence and the Department of Urology of the PLA Naval Medical Center for stimulating discussions. We acknowledge Biorender (©BioRender—biorender.com accessed on 10 June 2024 ) since the graphical abstract of this manuscript was made using this software.
Conflicts of Interest
The authors declare no conflicts of interest.
References
- Przydacz, M.; Golabek, T.; Dudek, P.; Lipinski, M.; Chlosta, P. Prevalence and bother of lower urinary tract symptoms and overactive bladder in Poland, an Eastern European Study. Sci. Rep. 2020, 10, 12. [Google Scholar] [CrossRef]
- Liu, S.P.; Chuang, Y.C.; Sumarsono, B.; Chang, H.C. The prevalence and bother of lower urinary tract symptoms in men and women aged 40 years or over in Taiwan. J. Formos. Med. Assoc. 2019, 118, 170–178. [Google Scholar] [CrossRef]
- Stenberg, A.; Heimer, G.; Ulmsten, U. The prevalence of urogenital symptoms in postmenopausal women. Maturitas 1995, 22, S17–S20. [Google Scholar] [CrossRef]
- Christmas, M.M.; Iyer, S.; Daisy, C.; Maristany, S.; Letko, J.; Hickey, M. Menopause hormone therapy and urinary symptoms: A systematic review. Menopause-J. N. Am. Menopause Soc. 2023, 30, 672–685. [Google Scholar] [CrossRef]
- Russo, E.; Misasi, G.; Montt-Guevara, M.M.; Giannini, A.; Simoncini, T. Effects of ospemifene on overactive bladder in postmenopausal women with vulvovaginal atrophy. Climacteric 2023, 26, 284–288. [Google Scholar] [CrossRef]
- Pauwaert, K.; Goessaert, A.-S.; Ghijselings, L.; Bower, W.; Mariman, A.; Vogelaers, D.; Depypere, H.; Everaert, K. Hormone therapy as a possible solution for postmenopausal women with nocturia: Results of a pilot trial. Menopause-J. N. Am. Menopause Soc. 2021, 28, 502–510. [Google Scholar] [CrossRef]
- Robinson, D.; Cardozo, T.H.L. The effect of hormones on the lower urinary tract. Menopause Int. 2013, 19, 155–162. [Google Scholar] [CrossRef]
- Robinson, D.; Cardozo, L. Estrogens and the Lower Urinary Tract. Neurourol. Urodyn. 2011, 30, 754–757. [Google Scholar] [CrossRef]
- Palmieri, K.; Mannikarottu, A.S.; Chichester, P.; Kogan, B.; Leggett, R.E.; Whitbeck, C.; Levin, R.M. The effects of cyclical oestrogen on bladder and urethral structure and function. BJU Int. 2007, 99, 171–176. [Google Scholar] [CrossRef] [PubMed]
- Dalghi, M.G.; Clayton, D.R.; Ruiz, W.G.; Al-Bataineh, M.M.; Satlin, L.M.; Kleyman, T.R.; Ricke, W.A.; Carattino, M.D.; Apodaca, G. Expression and distribution of PIEZO1 in the mouse urinary tract. Am. J. Physiol.-Renal Physiol. 2019, 317, F303–F321. [Google Scholar] [CrossRef]
- Dalghi, M.G.; Ruiz, W.G.; Clayton, D.R.; Montalbetti, N.; Daugherty, S.L.; Beckel, J.M.; Carattino, M.D.; Apodaca, G. Functional roles for PIEZO1 and PIEZO2 in urothelial mechanotransduction and lower urinary tract interoception. JCI Insight. 2021, 6, 19. [Google Scholar] [CrossRef]
- Miyamoto, T.; Mochizuki, T.; Nakagomi, H.; Kira, S.; Watanabe, M.; Takayama, Y.; Suzuki, Y.; Koizumi, S.; Takeda, M.; Tominaga, M. Functional Role for Piezo1 in Stretch-evoked Ca2+ Influx and ATP Release in Urothelial Cell Cultures. J. Biol. Chem. 2014, 289, 16565–16575. [Google Scholar] [CrossRef]
- Beča, K.I.K.; Girard, B.M.; Heppner, T.J.; Hennig, G.W.; Herrera, G.M.; Nelson, M.T.; Vizzard, M.A. The Role of PIEZO1 in Urinary Bladder Function and Dysfunction in a Rodent Model of Cyclophosphamide-Induced Cystitis. Front. Pain Res. 2021, 2, 748385. [Google Scholar] [CrossRef] [PubMed]
- Lai, A.; Cox, C.D.; Sekar, N.C.; Thurgood, P.; Jaworowski, A.; Peter, K.; Baratchi, S. Mechanosensing by Piezo1 and its implications for physiology and various pathologies. Biol. Rev. 2022, 97, 604–614. [Google Scholar] [CrossRef] [PubMed]
- Wu, Y.Y.; Qi, J.; Wu, C.H.; Rong, W.F. Emerging roles of the TRPV4 channel in bladder physiology and dysfunction. J. Physiol.-Lond. 2021, 599, 39–47. [Google Scholar] [CrossRef]
- Janssen, D.A.W.; Hoenderop, J.G.; Jansen, K.; Kemp, A.W.; Heesakkers, J.; Schalken, J.A. The Mechanoreceptor TRPV4 is Localized in Adherence Junctions of the Human Bladder Urothelium: A Morphological Study. J. Urol. 2011, 186, 1121–1127. [Google Scholar] [CrossRef]
- Gevaert, T.; Vriens, J.; Segal, A.; Everaerts, W.; Roskams, T.; Talavera, K.; Owsianik, G.; Liedtke, W.; Daelemans, D.; Dewachter, I.; et al. Deletion of the transient receptor potential cation channel TRPV4 impairs murine bladder voiding. J. Clin. Investig. 2007, 117, 3453–3462. [Google Scholar] [CrossRef] [PubMed]
- Deruyver, Y.; Weyne, E.; Dewulf, K.; Rietjens, R.; Pinto, S.; Van Ranst, N.; Franken, J.; Vanneste, M.; Albersen, M.; Gevaert, T.; et al. Intravesical Activation of the Cation Channel TRPV4 Improves Bladder Function in a Rat Model for Detrusor Underactivity. Eur. Urol. 2018, 74, 336–345. [Google Scholar] [CrossRef]
- Merrill, L.; Vizzard, M.A. Intravesical TRPV4 blockade reduces repeated variate stress-induced bladder dysfunction by increasing bladder capacity and decreasing voiding frequency in male rats. Am. J. Physiol.-Regul. Integr. Comp. Physiol. 2014, 307, R471–R480. [Google Scholar] [CrossRef]
- Zhang, K.; Yang, Q.; Yang, L.; Li, Y.-J.; Wang, X.-S.; Dang, R.-L.; Guan, S.-Y.; Guo, Y.-Y.; Sun, T.; Wu, Y.-M.; et al. CB1 agonism prolongs therapeutic window for hormone replacement in ovariectomized mice. J. Clin. Invest. 2019, 129, 2333–2350. [Google Scholar] [CrossRef]
- Li, C.; Wang, B.; Lu, X.; Huang, Y.; Wang, H.; Xu, D.; Zhang, J. Maternal exposure to cadmium from puberty through lactation induces abnormal reproductive development in female offspring. Ecotox. Environ. Safe 2022, 242, 10. [Google Scholar] [CrossRef]
- Hong, Y.; Xu, W.-Q.; Feng, J.; Lou, H.; Liu, H.; Wang, L.; Cui, H.; Jiang, L.-T.; Xu, R.-C.; Xu, H.-H.; et al. Nitidine chloride induces cardiac hypertrophy in mice by targeting autophagy-related 4B cysteine peptidase. Acta Pharmacol. Sin. 2023, 44, 561–572. [Google Scholar] [CrossRef] [PubMed]
- Gan, D.; Zhang, W.; Huang, C.; Chen, J.; He, W.; Wang, A.; Li, B.; Zhu, X. Ursolic acid ameliorates CCl4-induced liver fibrosis through the NOXs/ROS pathway. J. Cell Physiol. 2018, 233, 6799–6813. [Google Scholar] [CrossRef] [PubMed]
- Munoz, A.; Somogyi, G.T.; Boone, T.B.; Ford, A.P.; Smith, C.P. Modulation of bladder afferent signals in normal and spinal cord-injured rats by purinergic P2X3 and P2X2/3 receptors. BJU Int. 2012, 110, E409–E414. [Google Scholar] [CrossRef]
- Deer, R.R.; Stallone, J.N. Effects of estrogen on cerebrovascular function: Age-dependent shifts from beneficial to detrimental in small cerebral arteries of the rat. Am. J. Physiol.-Heart Circul. Physiol. 2016, 310, H1285–H1294. [Google Scholar] [CrossRef]
- Deer, R.R.; Stallone, J.N.; Pabbidi, M.R.; Kuppusamy, M.; Didion, S.P.; Sanapureddy, P.; Reed, J.T.; Sontakke, S.P.; Toth, P.; Tarantini, S.; et al. Hormonal gain control of a medial preoptic area social reward circuit. Nat. Neurosci. 2017, 20, 449–458. [Google Scholar]
- Piotrowska, K.; Tarnowski, M.; Zgutka, K.; Pawlik, A. Gender Differences in Response to Prolonged Every-Other-Day Feeding on the Proliferation and Apoptosis of Hepatocytes in Mice. Nutrients 2016, 8, 13. [Google Scholar] [CrossRef]
- Yoshida, J.; Aikawa, K.; Yoshimura, Y.; Shishido, K.; Yanagida, T.; Yamaguchi, O. The effects of ovariectomy and estrogen replacement on acetylcholine release from nerve fibres and passive stretch-induced acetylcholine release in female rat bladder. Neurourol. Urodyn. 2007, 26, 1050–1055. [Google Scholar] [CrossRef]
- Kullmann, F.A.; Limberg, B.J.; Artim, D.E.; Shah, M.; Downs, T.R.; Contract, D.; Wos, J.; Rosenbaum, J.S.; de Groat, W.C. Effects of β3-Adrenergic Receptor Activation on Rat Urinary Bladder Hyperactivity Induced by Ovariectomy. J. Pharmacol. Exp. Ther. 2009, 330, 704–717. [Google Scholar] [CrossRef]
- Liang, W.; Afshar, K.; Stothers, L.; Laher, I. The influence of ovariectomy and estrogen replacement on voiding patterns and detrusor muscarinic receptor affinity in the rat. Life Sci. 2002, 71, 351–362. [Google Scholar] [CrossRef]
- Diep, N.; Constantinou, C.E. Age dependent response to exogenous estrogen on micturition, contractility and cholinergic receptors of the rat bladder. Life Sci. 1999, 64, PL279–PL289. [Google Scholar] [CrossRef]
- Hextall, A. The Effect of Oestrogen and the Menopause on the Female Lower Urinary Tract. PhD Thesis, University of London, London, UK, 2002. [Google Scholar]
- Long, C.Y.; Liu, C.M.; Hsu, S.C.; Wu, C.H.; Wang, C.L.; Tsai, E.M. A randomized comparative study of the effects of oral and topical estrogen therapy on the vaginal vascularization and sexual function in hysterectomized postmenopausal women. Menopause-J. N. Am. Menopause Soc. 2006, 13, 737–743. [Google Scholar] [CrossRef] [PubMed]
- Fleischmann, N.; Christ, G.; Sclafani, T.; Melman, A. The effect of ovariectomy and long-term estrogen replacement on bladder structure and function in the rat. J. Urol. 2002, 168, 1265–1268. [Google Scholar] [CrossRef] [PubMed]
- Rodrìguez, L.V.; Wang, B.Y.; Shortliffe, L.M.D. Structural changes in the bladder walls of pregnant and hormone-treated rats: Correlation with bladder dynamics. BJU Int. 2004, 94, 1366–1372. [Google Scholar] [CrossRef] [PubMed]
- Zhang, F.; Liao, L.M. Long-term follow-up of neurogenic bladder patients after bladder augmentation with small intestinal submucosa. World J. Urol. 2020, 38, 2279–2288. [Google Scholar] [CrossRef] [PubMed]
- Collado, A.; Batista, E.; Gelabert-Más, A.; Corominas, J.M.; Arañó, P.; Villavicencio, H. Detrusor quantitative morphometry in obstructed males and controls. J. Urol. 2006, 176, 2722–2728. [Google Scholar] [CrossRef]
- Anumanthan, G.; Tanaka, S.T.; Adams, C.M.; Thomas, J.C.; Wills, M.L.; Adams, M.C.; Hayward, S.W.; Matusik, R.J.; Bhowmick, N.A.; Brock, J.W.; et al. Bladder Stromal Loss of Transforming Growth Factor Receptor II Decreases Fibrosis After Bladder Obstruction. J. Urol. 2009, 182, 1775–1780. [Google Scholar] [CrossRef]
- Zhu, Q.; Ritchie, J.; Marouf, N.; Dion, S.B.; Resnick, N.M.; Elbadawi, A.; Elbadawi, A.; Kuchel, G.A. Role of ovarian hormones in the pathogenesis of impaired detrusor contractility: Evidence in ovariectomized rodents. J. Urol. 2001, 166, 1136–1141. [Google Scholar] [CrossRef]
- Dobberfuhl, A.D.; Schuler, C.; Leggett, R.E.; De, E.J.B.; Levin, R.M. Estrogen replacement is protective to the effect of in vitro hypoxia on female rabbit bladder and pelvic floor contractile response. Investig. Clin. Urol. 2020, 61, 432–440. [Google Scholar] [CrossRef]
- Lin, A.D.-Y.; Mannikarottu, A.; A Kogan, B.; Whitbeck, C.; Chichester, P.; E Leggett, R.; Levin, R.M. Estrogen induces angiogenesis of the female rabbit bladder. J. Endocrinol. 2006, 190, 241–246. [Google Scholar] [CrossRef]
- Parekh, M.H.; Chichester, P.; Lobel, R.W.; Aikawa, K.; Levin, R.M. Effects of castration on female rabbit bladder physiology and morphology. Urology 2004, 64, 1048–1051. [Google Scholar] [CrossRef] [PubMed]
- Hass, M.A.; Nichol, P.; Lee, L.; Levin, R.M. Estrogen modulates permeability and prostaglandin levels in the rabbit urinary bladder. Prostaglandins Leukot Essent Fat. Acids. 2009, 80, 125–129. [Google Scholar] [CrossRef]
- Lin, W.Y.; Radu, F.; Schuler, C.; Leggett, R.E.; Mannikarottu, A.; Levin, R.M. The effect of ovariectomy and oestrogen therapy on the free fatty acid content, endogenous lipase activity, and phospholipid content of the rabbit urinary bladder. BJU Int. 2008, 102, 885–889. [Google Scholar] [CrossRef] [PubMed]
- Landau, E.H.; Jayanthi, V.R.; Churchill, B.M.; Shapiro, E.; Gilmour, R.F.; Khoury, A.E.; Macarak, E.J.; Mclorie, G.A.; Steckler, R.E.; Kogan, B.A. Loss of elasticity in dysfunctional bladders—Urodynamic and histochemical correlation. J. Urol. 1994, 152, 702–705. [Google Scholar] [CrossRef]
- Inaba, M.; Fushiki, S.; Yaoi, T.; Iwata, T.; Kamoi, K.; Okihara, K.; Ukimura, O.; Kawauchi, A.; Miyashita, H.; Kojima, M.; et al. Changes in extracellular matrix components of bladder detrusor in relation to bladder hypertrophy and compliance in patients with benign prostatic hyperplasia. Acta Histochem. Cytochem. 2000, 33, 131–139. [Google Scholar] [CrossRef]
- Zhang, W.; Li, Y.; Xi, X.; Zhu, G.; Wang, S.; Liu, Y.; Song, M. MicroRNA-15a-5p induces pulmonary artery smooth muscle cell apoptosis in a pulmonary arterial hypertension model via the VEGF/p38/MMP-2 signaling pathway. Int. J. Mol. Med. 2020, 45, 461–474. [Google Scholar] [CrossRef]
- Trabucco, E.; Soderberg, M.; Cobellis, L.; Torella, M.; Bystrom, B.; Ekman-Ordeberg, G.; Petraglia, F.; Colacurci, N. Role of proteoglycans in the organization of periurethral connective tissue in women with stress urinary incontinence. Maturitas 2007, 58, 395–405. [Google Scholar] [CrossRef]
- Kobata, S.; Girão, M.; Baracat, E.; Kajikawa, M.; Di Bella, V.; Sartori, M.; Bella, Z.J.-D. Estrogen therapy influence on periurethral vessels in postmenopausal incontinent women using Dopplervelocimetry analysis. Maturitas 2008, 61, 243–247. [Google Scholar] [CrossRef]
- Aikawa, K.; Sugino, T.; Matsumoto, S.; Chichester, P.; Whitbeck, C.; Levin, R.M. The effect of ovariectomy and estradiol on rabbit bladder smooth muscle contraction and morphology. J. Urol. 2003, 170, 634–637. [Google Scholar] [CrossRef]
- Sánchez-Ortiz, R.F.; Wang, Z.; Menon, C.; DiSanto, M.E.; Wein, A.J.; Chacko, S. Estrogen modulates the expression of myosin heavy chain in detrusor smooth muscle. Am. J. Physiol.-Cell Physiol. 2001, 280, C433–C440. [Google Scholar] [CrossRef]
- Blacher, J.; Dabire, H.; Pomies, J.P.; Safar, M.E.; Stimpel, M. Long-term cardiovascular effects of high “osteoprotective” dose levels of 17β-estradiol in spontaneously hypertensive rats. Cardiovasc. Drugs Ther. 2000, 14, 303–307. [Google Scholar] [CrossRef]
- Naomi, R.; Ridzuan, P.M.; Bahari, H. Current Insights into Collagen Type I. Polymers 2021, 13, 19. [Google Scholar] [CrossRef] [PubMed]
- Lai, J.; Ge, M.; Shen, S.; Yang, L.; Jin, T.; Cao, D.; Xu, H.; Zheng, X.; Qiu, S.; Wang, K.; et al. Activation of NFKB-JMJD3 signaling promotes bladder fibrosis via boosting bladder smooth muscle cell proliferation and collagen accumulation. Biochim. Biophys. Acta-Mol. Basis. Dis. 2019, 1865, 2403–2410. [Google Scholar] [CrossRef]
- He, Q.; Lin, Y.; Liao, B.; Zhou, L.; Ai, J.; Jin, X.; Li, H.; Wang, K. The role of interleukin-6/interleukin-6 receptor signaling in the mechanical stress-induced extracellular matrix remodeling of bladder smooth muscle. Arch. Biochem. Biophys. 2021, 702, 8. [Google Scholar] [CrossRef] [PubMed]
- Fakhrieh, M.; Darvish, M.; Ardeshirylajimi, A.; Taheri, M.; Omrani, M.D. Improved bladder smooth muscle cell differentiation of the mesenchymal stem cells when grown on electrospun polyacrylonitrile/polyethylene oxide nanofibrous scaffold. J. Cell Biochem. 2019, 120, 15814–15822. [Google Scholar] [CrossRef]
- Everaerts, W.; Vriens, J.; Owsianik, G.; Appendino, G.; Voets, T.; De Ridder, D.; Nilius, B. Functional characterization of transient receptor potential channels in mouse urothelial cells. Am. J. Physiol.-Renal. Physiol. 2010, 298, F692–F701. [Google Scholar] [CrossRef]
- Zhao, M.; Chen, Z.; Liu, L.; Ding, N.; Wen, J.; Liu, J.; Wang, W.; Ge, N.; Zu, S.; Song, W.; et al. Functional Expression of Transient Receptor Potential and Piezo1 Channels in Cultured Interstitial Cells of Human-Bladder Lamina Propria. Front. Physiol. 2022, 12, 11. [Google Scholar] [CrossRef] [PubMed]
- Ihara, T.; Mitsui, T.; Nakamura, Y.; Kanda, M.; Tsuchiya, S.; Kira, S.; Nakagomi, H.; Sawada, N.; Kamiyama, M.; Shigetomi, E.; et al. The time-dependent variation of ATP release in mouse primary-cultured urothelial cells is regulated by the clock gene. Neurourol. Urodyn. 2018, 37, 2535–2543. [Google Scholar] [CrossRef]
- Roberts, M.W.; Sui, G.; Wu, R.; Rong, W.; Wildman, S.; Montgomery, B.; Ali, A.; Langley, S.; Ruggieri Sr, M.R.; Wu, C. TRPV4 receptor as a functional sensory molecule in bladder urothelium: Stretch-independent, tissue-specific actions and pathological implications. Faseb. J. 2020, 34, 263–286. [Google Scholar] [CrossRef]
- Ihara, T.; Mitsui, T.; Nakamura, Y.; Kanda, M.; Tsuchiya, S.; Kira, S.; Nakagomi, H.; Sawada, N.; Kamiyama, M.; Hirayama, Y.; et al. The oscillation of intracellular Ca2+ influx associated with the circadian expression of Piezo1 and TRPV4 in the bladder urothelium. Sci. Rep. 2018, 8, 9. [Google Scholar] [CrossRef]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).