SARS-CoV-2 Infection in Unvaccinated High-Risk Pregnant Women in the Bronx, NY, USA Is Associated with Decreased Apgar Scores and Placental Villous Infarcts
Abstract
1. Introduction
2. Methods
2.1. Study Approval
2.2. Patient Population
2.3. Histopathologic Evaluation
2.4. Quantitative Polymerase Chain Reaction (qPCR)
2.4.1. FFPE Tissue Acquisition
2.4.2. FFPE RNA Extraction and Quantification
2.4.3. SARS-CoV-2 Reverse Transcription and qPCR Analyses
2.5. Immunohistochemistry (IHC)
2.6. In Situ Hybridization (ISH)
2.7. Statistical Analysis
3. Results
3.1. Severe Maternal SARS-CoV-2 Infection Affects Birth Weight and Apgar Scores
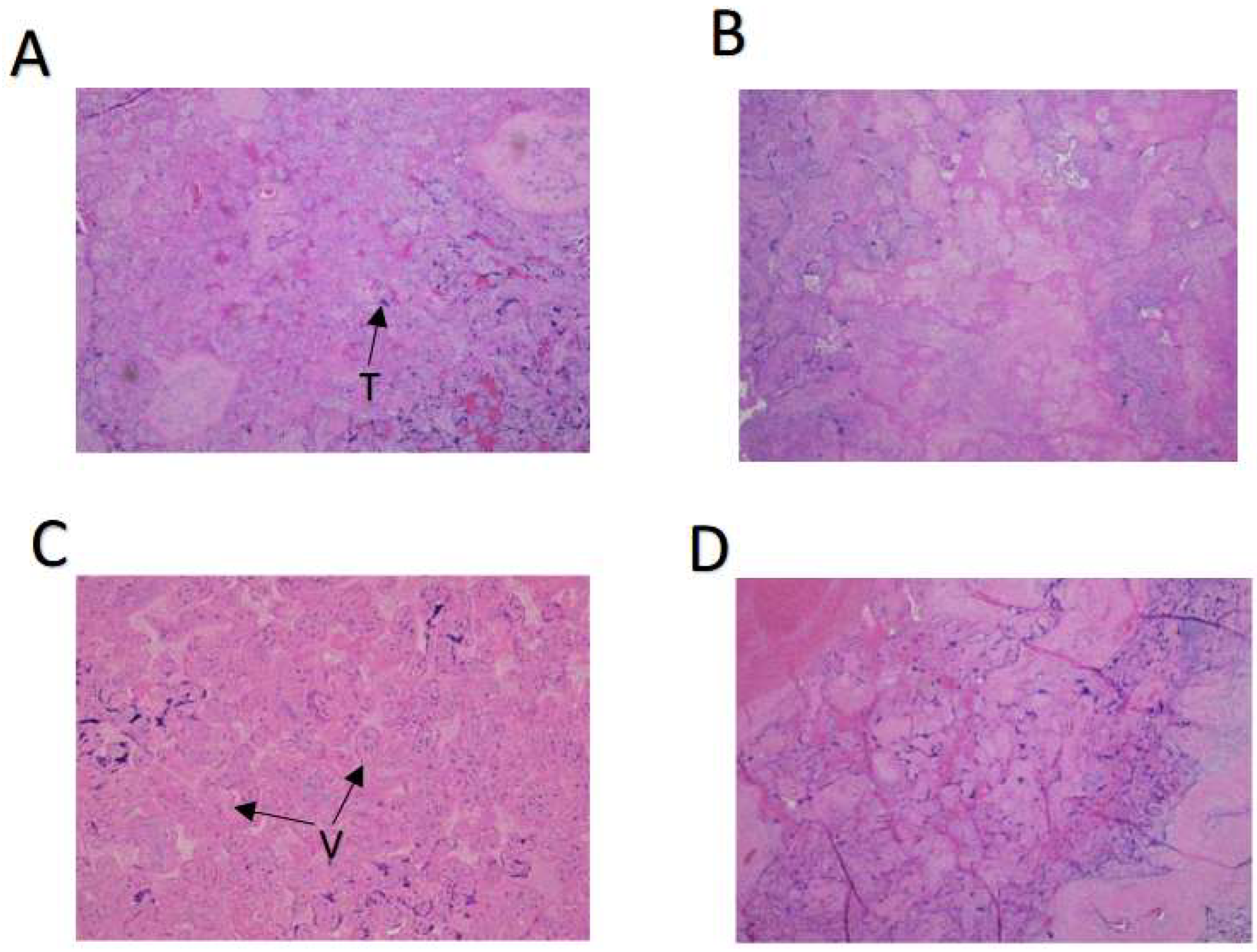
3.2. First-Wave Maternal SARS-CoV-2 Infection Increases Placental Villous Infarcts
3.3. The Placenta Is an Effective Barrier for SARS-CoV-2
4. Discussion
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Bleker, L.S.; De Rooij, S.R.; Roseboom, T.J. Programming Effects of Prenatal Stress on Neural Development—The Pitfall of Introducing a Self-fulfilling Prophecy. Int. J. Environ. Res. Public Health 2019, 16, 2301. [Google Scholar]
- Walsh, K.; McCormack, C.A.; Webster, R.; Pinto, A.; Lee, S.; Feng, T.; Krakovsky, H.S.; O’Grady, S.M.; Tycko, B.; Champagne, F.A.; et al. Maternal Prenatal Stress Phenotypes Associate with Fetal Neurodevelopment and Birth Outcomes. Proc. Natl. Acad. Sci. USA 2019, 116, 23996–24005. [Google Scholar]
- Schwartz, D.A.; Avvad-Portari, E.; Babál, P.; Baldewijns, M.; Blomberg, M.; Bouachba, A.; Camacho, J.; Collardeau-Frachon, S.; Colson, A.; Dehaene, I.; et al. Placental Tissue Destruction and Insufficiency from COVID-19 Causes Stillbirth and Neonatal Death from Hypoxic-Ischemic Injury. Arch. Pathol. Lab. Med. 2022, 146, 660–676. [Google Scholar] [PubMed]
- Zhang, P.; Heyman, T.; Salafia, C.; Lederman, S.; Dygulska, B. Detection of Severe Acute Respiratory Syndrome Coronavirus 2 in Placentas with Pathology and Vertical Transmission. Am. J. Obstet. Gynecol. 2020, 2, 100197. [Google Scholar]
- Thomas, P.; Alexander, P.E.; Ahmed, U.; Elderhorst, E.; El-Khechen, H.; Mammen, M.J.; Debono, V.B.; Aponte Torres, Z.; Aryal, K.; Brocard, E.; et al. Vertical Transmission Risk of SARS-CoV-2 Infection in the Third Trimester: A Systematic Scoping Review. J. Matern. -Fetal Neonatal Med. 2022, 35, 2387–2394. [Google Scholar] [PubMed]
- Simoões e Silva, A.C.; Leal, C.R.V. Is SARS-CoV-2 Vertically Transmitted? Front. Pediatr. 2020, 8, 276. [Google Scholar] [PubMed]
- Komine-Aizawa, S.; Takada, K.; Hayakawa, S. Placental Barrier Against COVID-19. Placenta 2020, 99, 45–49. [Google Scholar] [PubMed]
- Hosier, H.; Farhadian, S.F.; Morotti, R.A.; Deshmukh, U.; Lu-Culligan, A.; Campbell, K.H.; Yasumoto, Y.; Vogels, C.B.; Casanovas-Massana, A.; Vijayakumar, P.; et al. SARS-CoV-2 Infection of the Placenta. J. Clin. Investig. 2020, 130, 4947–4953. [Google Scholar] [PubMed]
- Khoury, R.; Bernstein, P.S.; Debolt, C.; Stone, J.; Sutton, D.M.; Simpson, L.L.; Limaye, M.A.; Roman, A.S.; Fazzari, M.; Penfield, C.A.; et al. Characteristics and Outcomes of 241 Births to Women with Severe Acute Respiratory Syndrome Coronavirus 2 (SARS-CoV-2) Infection at Five New York City Medical Centers. Obstet. Gynecol. 2020, 136, 273–282. [Google Scholar]
- Smith, V.; Seo, D.; Warty, R.; Payne, O.; Salih, M.; Chin, K.L.; Ofori-Asenso, R.; Krishnan, S.; da Silva Costa, F.; Vollenhoven, B.; et al. Maternal and Neonatal Outcomes Associated with COVID-19 Infection: A Systematic Review. PLoS ONE 2020, 15, e0234187. [Google Scholar]
- Vimercati, A.; De Nola, R.; Trerotoli, P.; Metta, M.E.; Cazzato, G.; Resta, L.; Malvasi, A.; Lepera, A.; Ricci, I.; Capozza, M.; et al. COVID-19 Infection in Pregnancy: Obstetrical Risk Factors and Neonatal Outcomes—A Monocentric, Single Cohort Study. Vaccines 2022, 10, 166. [Google Scholar] [CrossRef] [PubMed]
- Joshi, B.; Chandi, A.; Srinivasan, R.; Saini, S.S.; Prasad, G.; Puri, G.; Bhalla, A.; Suri, V.; Bagga, R. The Placental Pathology in Coronavirus disease 2019 Infected Mothers and its impact on pregnancy outcome. Placenta 2022, 127, 1–7. [Google Scholar] [CrossRef]
- Edlow, A.G.; Castro, V.M.; Shook, L.L.; Kaimal, A.; Perlis, R.H. Neurodevelopmental Outcomes at 1 Year in Infants of Mothers Who Tested Positive for SARS-CoV-2 During Pregnancy. JAMA Netw. 2022, 5, e2215787. [Google Scholar]
- Shanes, E.D.; Mithal, L.B.; Otero, S.; Azad, H.A.; Miller, E.S.; Goldstein, J.A. Placental Pathology in COVID-19. Am. J. Clin. Pathol. 2020, 154, 22–32. [Google Scholar] [CrossRef]
- Patberg, E.T.; Adams, T.; Rekawek, P.; Vahanian, S.A.; Akerman, M.; Hernandez, A.; Rapkiewicz, A.V.; Ragolia, L.; Sicuranza, G.; Chavez, M.R.; et al. Coronavirus Disease 2019 Infection and Placental Histopathology in Women Delivering at Term. Am. J. Obstet. Gynecol. 2021, 224, 382.e1–382.e18. [Google Scholar] [CrossRef]
- Smithgall, M.C.; Liu-Jarin, X.; Hamele-Bena, D.; Cimic, A.; Mourad, M.; Debelenko, L.; Chen, X. Third-Trimester Placentas of Severe Acute Respiratory Syndrome Coronavirus 2 (SARS-CoV-2)-Positive Women: Histomorphology Including Viral Immunohistochemistry and In-situ Hybridization. Histopathology 2020, 77, 994–999. [Google Scholar] [PubMed]
- Bronx County, New York Coronavirus Cases and Deaths. USA Facts. Available online: https://usafacts.org/visualizations/coronavirus-covid-19-spread-map/state/new-york/county/bronx-county (accessed on 25 June 2023).
- Padmanabhan, V.; Cardoso, R.C.; Puttabyatappa, M. Developmental Programming a Pathway to Disease. Endocrinology 2016, 157, 1328–1340. [Google Scholar] [CrossRef]
- Loudig, O.; Milova, E.; Brandwein-Gensler, M.; Massimi, A.; Belbin, T.J.; Childs, G.; Singer, R.H.; Rohan, T.; Prystowsky, M.B. Molecular Restoration of Archived Transcriptional Profiles by Complementary-Template Reverse-Transcription (CT-RT). Nucleic Acids Res. 2007, 35, e94. [Google Scholar]
- Kotorashvili, A.; Ramnauth, A.; Liu, C.; Lin, J.; Ye, K.; Kim, R.; Hazan, R.; Rohan, T.; Fineberg, S.; Loudig, O. Effective DNA/RNA Co-extraction for Analysis of MicroRNAs, mRNAs, and Genomic DNA from Formalin-Fixed Paraffin-Embedded Specimens. PLoS ONE 2012, 7, e34683. [Google Scholar]
- Sekulic, M.; Harper, H.; Nezami, B.G.; Shen, D.L.; Sekulic, S.P.; Koeth, A.T.; Harding, C.V.; Gilmore, H.; Sadri, N. Molecular Detection of SARS-CoV-2 Infection in FFPE Samples and Histopathologic Findings in Fatal SARS-CoV-2 Cases. Am. J. Clin. Path. 2020, 154, 190–200. [Google Scholar]
- Ko, C.J.; Harigopal, M.; Damsky, W.; Gehlhausen, J.R.; Bosenberg, M.; Patrignelli, R.; McNiff, J.M. Perniosis During the COVID-19 Pandemic: Negative Anti-SARS-CoV-2 Immunohistochemistry in Six Patients and Comparison to Perniosis Before the Emergence of SARS-CoV-2. J. Cutan. Pathol. 2020, 47, 997–1002. [Google Scholar] [CrossRef]
- Pique-Regi, R. Does the Human Placenta Express the Canonical Cell Entry Mediators for SARS-CoV-2? eLife 2020, 9, e58716. [Google Scholar] [CrossRef] [PubMed]
- Vimercati, A.; De Nola, R.; Battaglia, S.; Di Mussi, R.; Cazzato, G.; Resta, L.; Chironna, M.; Loconsole, D.; Vinci, L.; Chiarello, G.; et al. Adverse Maternal Outcomes in Pregnant Women Affected by Severe-Critical COVID-19 Illness: Correlation with Vaccination Status in the Time of Different Viral Strains’ Dominancy. Vaccines 2022, 10, 2061. [Google Scholar] [PubMed]
- Schwartz, D.A.; Mulkey, S.B.; Roberts, D.J. SARS-CoV-2 Placentitis, Stillbirth, and Maternal COVID-19 Vaccination: Clinical-pathologic Correlations. Am. J. Obstet. Gynecol. 2023, 228, 261–269. [Google Scholar] [PubMed]
- Goldfarb, I.T.; Diouf, K.; Barth, W.H.; Robinson, J.N.; Katz, D.; Gregory, K.E.; Ciaranello, A.; Yawetz, S.; Shenoy, E.S.; Klompas, M. Universal SARS-CoV-2 Testing on Admission to the Labor and Delivery Unit: Low Prevalence Among Asymptomatic Obstetric Patients. Infect. Control. Hosp. Epidemiol. 2020, 41, 1095–1096. [Google Scholar] [CrossRef] [PubMed]
- Sutton, D.; Fuchs, K.; D’Alton, M.; Goffman, D. Universal Screening for SARS-CoV-2 Women Aadmitted for Delivery. N. Engl. J. Med. 2020, 382, 2164–2165. [Google Scholar] [CrossRef]
- Vintzileos, W.S.; Muscat, J.; Hoffmann, E.; John, N.S.; Vertichio, R.; Vintzileos, A.M.; Vo, D. Screening All Pregnant Women Admitted to Labor and Delivery for the Virus Responsible for Coronavirus Disease 2019. Am. J. Obstet. Gynecol. 2020, 223, 284–286. [Google Scholar] [CrossRef]
- Razaz, N.; Cnattingius, S.; Joseph, K.S. Association Between Apgar Scores of 7 to 9 and Neonatal Morbidity and Mortality: Population Based Cohort Study of Term Infants in Sweden. BMJ 2019, 365, l1656. [Google Scholar]
- Resta, L.; Vimercati, A.; Cazzato, G.; Fanelli, M.; Scarcella, S.V.; Ingravallo, G.; Colagrande, A.; Sablone, S.; Stolfa, M.; Arezzo, F.; et al. SARS-CoV-2, Placental Histopathology, Gravity of Infection and Immunopathology: Is There an Association? Viruses 2022, 14, 1330. [Google Scholar] [CrossRef] [PubMed]
- Barker, D.J.; Martyn, C.N. The Maternal and Fetal Origins of Cardiovascular Disease. J. Epidemiol. Community Health 1992, 46, 8–11. [Google Scholar] [CrossRef]
- Todros, T.; Masturzo, B.; De Francia, S. COVID-19 Infection: ACE2, Pregnancy and Preeclampsia. Eur. J. Obstet. Gynecol. Reprod. Biol. 2020, 253, 330. [Google Scholar]
- Levy, A.; Yagil, Y.; Bursztyn, M.; Barkalifa, R.; Scharf, S.; Yagil, C. ACE2 Expression and Activity are Enhanced During Pregnancy. Am. J. Physiool. Regul. Integr. Comp. Physiol. 2008, 295, R1953–R1961. [Google Scholar] [CrossRef]
- Tamanna, S.; Clifton, V.L.; Rae, K.; van Helden, D.F.; Lumbers, E.R.; Pringle, K.G. Angiotensin Converting Enzyme 2 (ACE2) in Pregnancy: Preeclampsia and Small for Gestational Age. Front. Physiol. 2020, 11, 590787. [Google Scholar]
- Delforce, S.J.; Lumbers, E.R.; Ellery, S.J.; Murthi, P.; Pringle, K.G. Dysregulation of the Placental Renin-Angiotensin System in Human Fetal Growth Restriction. Reproduction 2019, 158, 237–245. [Google Scholar] [CrossRef]
- Merrill, D.C.; Karoy, M.; Chen, K.; Ferrario, C.M.; Brosnihan, B. Angiotensin-(1-7) in Normal and Preeclamptic Pregnancy. Endocrine 2002, 18, 239–245. [Google Scholar] [CrossRef]

| SARS-CoV-2-Negative (n = 61) | SARS-CoV-2-Positive, First Wave (n = 56) | SARS-CoV-2-Positive, Second Wave (n = 48) | p, First Wave vs. Negative | p, Second Wave vs. Negative | p, First Wave vs. Second Wave | |
|---|---|---|---|---|---|---|
| Severity of Infection (%) | ||||||
| --Asymptomatic | N/A | 63.2 | 47.8 | N/A | N/A | NS |
| --Mild | N/A | 19.3 | 39.1 ** | N/A | N/A | p < 0.01 |
| --Severe | N/A | 17.5 | 13.1 | N/A | N/A | NS |
| Mean age ± SEM (Years) | 30.92 ± 1.20 | 29.42 ± 1.08 | 30.03 ± 1.57 | NS | NS | NS |
| Mean BMI ± SEM (kg m−2) | 32.76 ± 1.76 | 32.00 ± 1.46 | 31.61 ± 1.78 | NS | NS | NS |
| Race (%) | ||||||
| --Black | 52 | 47 | 43 | NS | NS | NS |
| --Latina | 40 | 42 | 0 ***** | NS | p < 0.00001 | p < 0.00001 |
| --Non-Latina white | 4.0 | 5.3 | 35 * | NS | p < 0.05 | p < 0.0001 |
| --Asian | 4.0 | 5.3 | 11 | NS | NS | NS |
| Cigarette smoking (%) | 12 | 0 | 4.3 | NS | NS | NS |
| Mean Gravidity ± SEM | 2.9 ± 0.2 | 3.0 ± 0.2 | 3.3 ± 0.5 | NS | NS | NS |
| Mean Parity ± SEM | 1.2 ± 0.2 | 1.8 ± 0.2 | 1.4 ± 0.4 | NS | NS | NS |
| Mode of delivery (%) | ||||||
| --Cesarean | 39.3 | 38.6 | 39.2 | NS | NS | NS |
| --Vaginal | 60.7 | 61.4 | 60.8 | NS | NS | NS |
| Mean Apgar scores ± SEM | ||||||
| --Apgar score at 1 min | 8.21 ± 0.23 | 7.56 ± 0.37 | 7.42 ± 0.73 | NS | NS | NS |
| --Apgar score at 5 min | 8.63 ± 0.21 | 7.94 ± 0.36 | 7.95 ± 0.65 | NS | NS | NS |
| Mean gestational age ± SEM (weeks) | 37.5 ± 0.7 | 37.2 ± 0.7 | 38.2 ± 0.5 | NS | NS | NS |
| Mean Birthweight ± SEM (g) | 3079 ± 88 | 3046 ± 91 | 2951 ± 190 | NS | NS | NS |
| Fetal death (%) | 12 | 0 | 5 | NS | NS | NS |
| SARS CoV-2-Negative (n = 61) | SARS-CoV-2-Positive, First Wave (n = 56) | SARS-CoV-2-Positive, Second Wave (n = 48) | p, First Wave vs. Negative | p, Second Wave vs. Negative | p, First Wave vs. Second Wave | |
|---|---|---|---|---|---|---|
| Maternal vascular malperfusion (%) | ||||||
| --Small for gestational age placenta | 23.0 | 12.5 | 37.5 | NS | NS | NS |
| --Distal villous hypoplasia | 8.2 | 7.1 | 6.3 | NS | NS | NS |
| --Villous congestion | 8.2 | 5.4 | 12.5 | NS | NS | NS |
| --Villous infarct | 6.6 | 19.6 | 10.4 | p < 0.05 | NS | NS |
| --Intervillous thrombus | 11.5 | 10.7 | 10.4 | NS | NS | NS |
| --Decidual vasculopathy | 1.7 | 1.8 | 0 | NS | NS | NS |
| Inflammatory responses (%) | ||||||
| ----Chorioamnionitis | 34.4 | 28.6 | 39.6 | NS | NS | NS |
| ----Funisitis | 16.7 | 10.7 | 14.6 | NS | NS | NS |
| SARS-CoV-2-Negative (n = 61) | SARS-CoV-2-Positive Asymptomatic (n = 57) | SARS-CoV-2-Positive Mild Symptoms (n = 28) | SARS-CoV-2-Positive Severe Symptoms (n = 10) | p | |
|---|---|---|---|---|---|
| Mean birth weight ± SEM (g) | 3079 ± 88 | 3000 ± 92 | 3210 ± 135 | 2595 ± 191 | p = 0.06 |
| Mean Apgar scores ± SEM | |||||
| --Apgar score at 1 min | 8.21 ± 0.31 | 7.78 ± 0.32 | 7.85 ± 0.47 | 6.06 ± 0.63 | p < 0.05 |
| --Apgar score at 5 min | 8.63 ± 0.29 | 7.85 ± 0.46 | 8.07 ± 0.43 | 6.66 ± 0.59 | p < 0.05 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Reznik, S.E.; Vuguin, P.M.; Cohen, A.; Khoury, R.; Loudig, O.; Balakrishnan, R.; Fineberg, S.A.; Hughes, F.; Harigopal, M.; Charron, M.J. SARS-CoV-2 Infection in Unvaccinated High-Risk Pregnant Women in the Bronx, NY, USA Is Associated with Decreased Apgar Scores and Placental Villous Infarcts. Biomolecules 2023, 13, 1224. https://doi.org/10.3390/biom13081224
Reznik SE, Vuguin PM, Cohen A, Khoury R, Loudig O, Balakrishnan R, Fineberg SA, Hughes F, Harigopal M, Charron MJ. SARS-CoV-2 Infection in Unvaccinated High-Risk Pregnant Women in the Bronx, NY, USA Is Associated with Decreased Apgar Scores and Placental Villous Infarcts. Biomolecules. 2023; 13(8):1224. https://doi.org/10.3390/biom13081224
Chicago/Turabian StyleReznik, Sandra E., Patricia M. Vuguin, Alexa Cohen, Rasha Khoury, Olivier Loudig, Ridin Balakrishnan, Susan A. Fineberg, Francine Hughes, Malini Harigopal, and Maureen J. Charron. 2023. "SARS-CoV-2 Infection in Unvaccinated High-Risk Pregnant Women in the Bronx, NY, USA Is Associated with Decreased Apgar Scores and Placental Villous Infarcts" Biomolecules 13, no. 8: 1224. https://doi.org/10.3390/biom13081224
APA StyleReznik, S. E., Vuguin, P. M., Cohen, A., Khoury, R., Loudig, O., Balakrishnan, R., Fineberg, S. A., Hughes, F., Harigopal, M., & Charron, M. J. (2023). SARS-CoV-2 Infection in Unvaccinated High-Risk Pregnant Women in the Bronx, NY, USA Is Associated with Decreased Apgar Scores and Placental Villous Infarcts. Biomolecules, 13(8), 1224. https://doi.org/10.3390/biom13081224





