Preliminary Study of Iron Concentration in the Human Placenta in Twin Pregnancies
Abstract
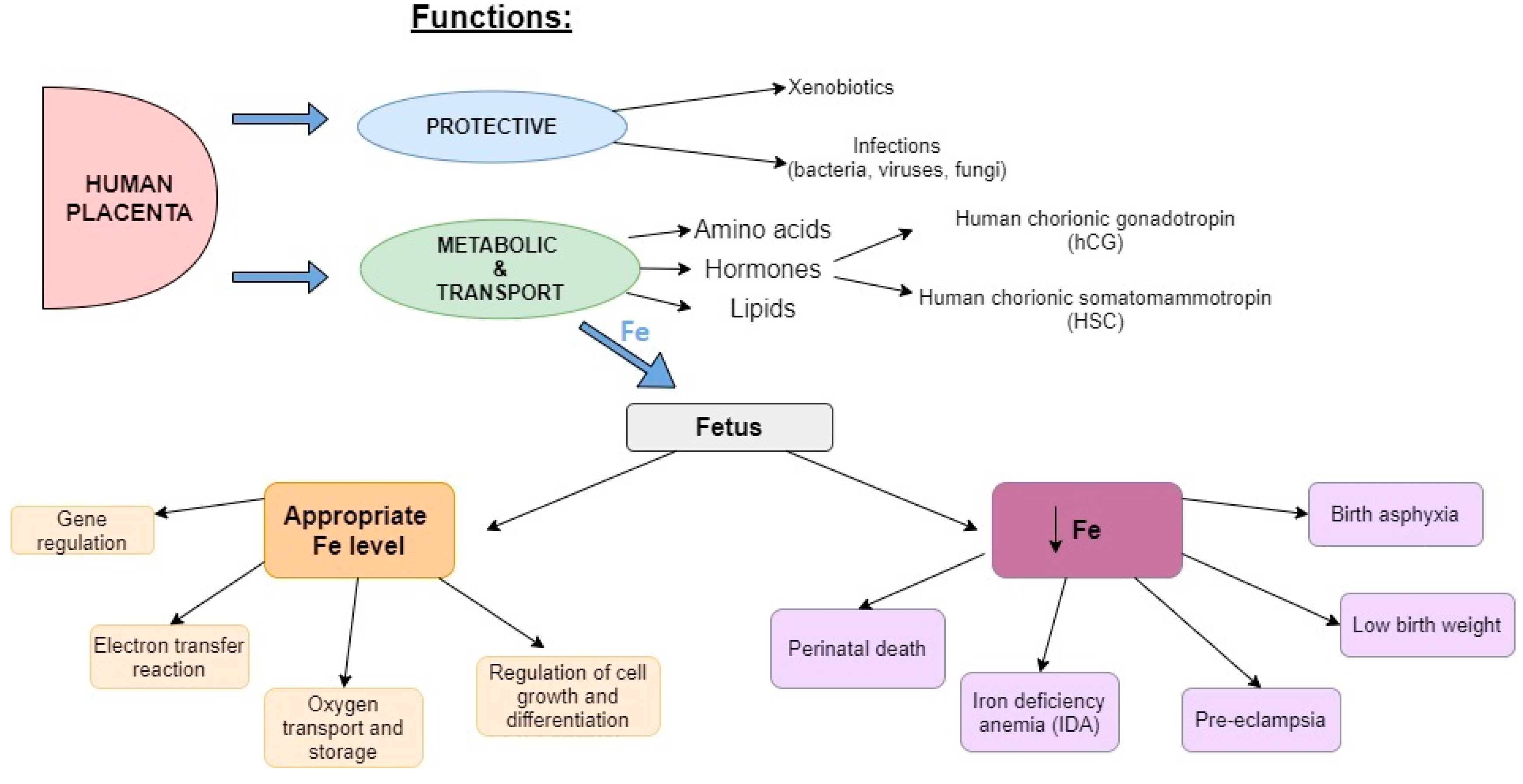
:1. Introduction
2. Materials and Methods
3. Results
4. Limitations and Strengths
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Gude, N.M.; Roberts, C.T.; Kalionis, B.; King, R.G. Growth and function of the normal human placenta. Thromb. Res. 2004, 114, 397–407. [Google Scholar] [CrossRef] [PubMed]
- Iqbal, M.; Audette, M.; Petropoulos, S.; Gibb, W.; Matthews, S. Placental drug transporters and their role in fetal protection. Placenta 2012, 33, 137–142. [Google Scholar] [CrossRef]
- Costa, M. The endocrine function of human placenta: An overview. Reprod. Biomed. Online 2016, 32, 14–43. [Google Scholar] [CrossRef]
- Fisher, A.L.; Nemeth, E. Iron homeostasis during pregnancy. Am. J. Clin. Nutr. 2017, 106 (Suppl. 6), 1567S. [Google Scholar] [CrossRef] [PubMed]
- Sangkhae, V.; Nemeth, E. Placental iron transport: The mechanism and regulatory circuits. Free Radic. Biol. Med. 2019, 133, 254–261. [Google Scholar] [CrossRef] [PubMed]
- Grzeszczak, K.; Kwiatkowski, S.; Kosik-Bogacka, D. The role of Fe, Zn, and Cu in pregnancy. Biomolecules 2020, 10, 1176. [Google Scholar] [CrossRef]
- Beard, J.L. Iron biology in immune function, muscle metabolism and neuronal functioning. J. Nutr. 2001, 131, 568S–579S; discussion 580S. [Google Scholar] [CrossRef]
- Tandon, R.; Jain, A.; Malhotra, P. Management of iron deficiency anemia in pregnancy in India. Indian J. Hematol. Blood Transfus. 2018, 34, 204–215. [Google Scholar] [CrossRef]
- Garzon, S.; Cacciato, P.M.; Certelli, C.; Salvaggio, C.; Magliarditi, M.; Rizzo, G. Iron deficiency anemia in pregnancy: Novel approaches for an old problem. Oman Med. J. 2020, 35, e166. [Google Scholar] [CrossRef]
- Milman, N. Iron in pregnancy: How do we secure an appropriate iron status in the mother and child? Ann. Nutr. Metab. 2011, 59, 50–54. [Google Scholar] [CrossRef]
- Muñoz, M.; Peña-Rosas, J.P.; Robinson, S.; Milman, N.; Holzgreve, W.; Breymann, C.; Goffinet, F.; Nizard, J.; Christory, F.; Samama, C.M.; et al. Patient blood management in obstetrics: Management of anaemia and haematinic deficiencies in pregnancy and in the post-partum period: Nata consensus statement. Transfus. Med. 2018, 28, 22–39. [Google Scholar] [CrossRef] [PubMed]
- Schwartz, A.; Converso-Baran, K.; Michele, D.; Shah, Y. A Genetic mouse model of severe iron deficiency anemia reveals tissue-specific transcriptional stress responses and cardiac remodeling. J. Biol. Chem. 2019, 294, 14991–15002. [Google Scholar] [CrossRef] [PubMed]
- Mazhar, S.B.; Peerzada, A.; Mahmud, G. Maternal and perinatal complications in multiple versus singleton pregnancies: A prospective two years study. J. Pak. Med. Assoc. 2002, 52, 143–147. [Google Scholar] [PubMed]
- Kalikkot Thekkeveedu, R.; Dankhara, N.; Desai, J.; Klar, A.L.; Patel, J. Outcomes of multiple gestation births compared to singleton: Analysis of multicenter KID database. Matern. Health Neonatol. Perinatol. 2021, 7, 15. [Google Scholar] [CrossRef]
- Hiersch, L.; Attali, E.; Melamed, N. Special considerations regarding antenatal care and pregnancy complications in dichorionic twin pregnancies. Am. J. Obstet. Gynecol. MFM 2022, 4, 100500. [Google Scholar] [CrossRef]
- Stevens, G.; Finucane, M.; De-Regil, L.; Paciorek, C.; Flaxman, S.; Branca, F.; Peña-Rosas, J.; Bhutta, Z.; Ezzati, M. Global, regional, and national trends in haemoglobin concentration and prevalence of total and severe anaemia in children and pregnant and non-pregnant women for 1995–2011: A systematic analysis of population-representative data. Lancet Glob. Health 2013, 1, e16–e25. [Google Scholar] [CrossRef]
- Osungbade, K.; Oladunjoye, A. Anaemiain developing countries: Burden and prospects of prevention and control. In Anemia; Silverberg, D.S., Ed.; IntechOpen: London, UK, 2012; pp. 116–129. [Google Scholar] [CrossRef]
- Kot, K.; Kosik-Bogacka, D.; Łanocha-Arendarczyk, N.; Malinowski, W.; Szymański, S.; Mularczyk, M.; Tomska, N.; Rotter, I. Interactions between 14 elements in the human placenta, fetal membrane and umbilical cord. Int. J. Environ. Res. Public Health 2019, 16, 1615. [Google Scholar] [CrossRef]
- Gonzalez, M.H.; Souza, G.B.; Oliveira, R.V.; Forato, L.A.; Nóbrega, J.A.; Nogueira, A.R. Microwave-assisted digestion procedures for biological samples with diluted nitric acid: Identification of reaction products. Talanta 2009, 79, 396–401. [Google Scholar] [CrossRef]
- Gutowska, I.; Żwierełło, W.; Piorun, K.; Skórka-Majewicz, M.; Maciejewska-Markiewicz, D.; Kupnicka, P.; Baranowska-Bosiacka, I.; Dalewski, B.; Chlubek, D. The extent of burn injury significantly affects serum micro- and macroelement concentrations in patients on the first day of hospitalisation. Nutrients 2022, 14, 4248. [Google Scholar] [CrossRef]
- Janda, K.; Jakubczyk, K.; Kupnicka, P.; Bosiacki, M.; Gutowska, I. Mineral composition and antioxidant potential in the common poppy (Papaver rhoeas L.) petal infusions. Biol. Trace Elem. Res. 2021, 199, 371–381. [Google Scholar] [CrossRef]
- Zachariadis, G.A.; Vogiatzis, C. An overview of the use of yttrium for internal standardization in inductively coupled plasma–atomic emission spectrometry. Appl. Spectrosc. Rev. 2010, 45, 220–239. [Google Scholar] [CrossRef]
- Choi, S.H.; Park, Y.S.; Shim, K.S.; Choi, Y.S.; Chang, J.Y.; Hahn, W.H.; Bae, C.W. Recent trends in the incidence of multiple births and its consequences on perinatal problems in Korea. J. Korean Med. Sci. 2010, 25, 1191–1196. [Google Scholar] [CrossRef] [PubMed]
- Monden, C.; Pison, G.; Smits, J. Twin peaks: More twinning in humans than ever before. Hum. Reprod. 2021, 36, 1666–1673. [Google Scholar] [CrossRef] [PubMed]
- Abbaspour, N.; Hurrell, R.; Kelishadi, R. Review on iron and its importance for human health. J. Res. Med. Sci. 2014, 19, 164–174. [Google Scholar] [PubMed]
- De Angelis, P.; Miller, R.K.; Darrah, T.H.; Katzman, P.J.; Pressman, E.K.; Kent, T.R.; O’Brien, K.O. Elemental content of the placenta: A comparison between two high-risk obstetrical populations, adult women carrying multiples and adolescents carrying singletons. Environ. Res. 2017, 158, 553–565. [Google Scholar] [CrossRef]
- Mbofung, C.M.F.; Subbarau, V.V. Trace element (zinc, copper, iron and magnesium) concentrations in human placenta and their relationship to birth weight of babies. Nutr. Res. 1990, 10, 359–366. [Google Scholar] [CrossRef]
- Reddy, Y.S.; Aparna, Y.; Ramalaksmi, B.A.; Dinesh Kumar, B. Lead and trace element levels in placenta, maternal and cord blood: A cross-sectional pilot study. J. Obstet. Gynaecol. Res. 2014, 40, 2184–2190. [Google Scholar] [CrossRef]
- Singh, L.; Agarwal, P.; Anand, M.; Taneja, A. Toxic and essential metals in placenta and its relation with lipid peroxides/glutathione status in pre-term and full-term deliveries. Asian J. Med. Sci. 2015, 7, 34–39. [Google Scholar] [CrossRef]
- Irwinda, R.; Wibowo, N.; Putri, A.S. The concentration of micronutrients and heavy metals in maternal serum, placenta, and cord blood: A cross-sectional study in preterm birth. J. Pregnancy 2019, 2019, 5062365. [Google Scholar] [CrossRef]
- Mikelson, C.K.; Troisi, J.; LaLonde, A.; Symes, S.J.K.; Thurston, S.W.; Di Re, L.M.; Adair, C.D.; Miller, R.K.; Richards, S.M. Placental concentrations of essential, toxic, and understudied metals and relationships with birth outcomes in Chattanooga, TN. Environ. Res. 2019, 168, 118–129. [Google Scholar] [CrossRef]
- Georgieff, M.K.; Berry, S.A.; Wobken, J.D.; Leibold, E.A. Increased placental iron regulatory protein-1 expression in diabetic pregnancies complicated by fetal iron deficiency. Placenta 1999, 20, 87–93. [Google Scholar] [CrossRef] [PubMed]
- Jensen, P.H.; Moestrup, S.K.; Gliemann, J. Purification of the human placental alpha 2- macroglobulin receptor. FEBS Lett. 1989, 255, 275–280. [Google Scholar] [CrossRef] [PubMed]
- Hvidberg, V.; Maniecki, M.B.; Jacobsen, C.; Hojrup, P.; Moller, H.J.; Moestrup, S.K. Identification of the receptor scavenging hemopexin-heme complexes. Blood 2005, 106, 2572–2579. [Google Scholar] [CrossRef] [PubMed]
- Bastin, J.; Drakesmith, H.; Rees, M.; Sargent, I.; Townsend, A. Localisation of proteins of iron metabolism in the human placenta and liver. Br. J. Haematol. 2006, 134, 532–543. [Google Scholar] [CrossRef]
- Miller, J.L. Iron deficiency anemia: A common and curable disease. Cold Spring Harb. Perspect. Med. 2013, 3, a011866. [Google Scholar] [CrossRef]
- Tan, J.; Qi, Y.N.; He, G.L.; Yang, H.M.; Zhang, G.T.; Zou, K.; Luo, W.; Sun, X.; Liu, X.H. Association between maternal weight indicators and iron deficiency anemia during pregnancy: A cohort study. Chin. Med. J. 2018, 131, 2566–2574. [Google Scholar] [CrossRef]
- Jones, A.D.; Zhao, G.; Jiang, Y.P.; Zhou, M.; Xu, G.; Kaciroti, N.; Zhang, Z.; Lozoff, B. Maternal Obesity during pregnancy is negatively associated with maternal and neonatal iron status. Eur. J. Clin. Nutr. 2016, 70, 918. [Google Scholar] [CrossRef]
- Phillips, A.K.; Roy, S.C.; Lundberg, R.; Guilbert, T.W.; Auger, A.P.; Blohowiak, S.E.; Coe, C.L.; Kling, P.J. Neonatal iron status is impaired by maternal obesity and excessive weight gain during pregnancy. J. Perinatol. 2014, 34, 513–518. [Google Scholar] [CrossRef]
- Tussing-Humphreys, L.; Labomascus, B.; Obrien, K.; Nemeth, E.; Sangkhae, V.; Steffen, A.D.; Castellanos, K.; Demartelly, V.; Ruchob, R.; Welke, L.; et al. Pregnancyobesity does not impact placental iron trafficking. J. Nutr. 2021, 151, 2646–2654. [Google Scholar] [CrossRef]
- Ludwig, D.S.; Currie, J. The relationship between pregnancy weight gain and birth weight: A within family comparison. Lancet 2010, 376, 984–990. [Google Scholar] [CrossRef]
- Brown, B.; Wright, C. Safety and efficacy of supplements in pregnancy. Nutr. Rev. 2020, 78, 813–826. [Google Scholar] [CrossRef] [PubMed]
- Ru, Y.; Pressman, E.K.; Cooper, E.M.; Guillet, R.; Katzman, P.J.; Kent, T.R.; Bacak, S.J.; O’Brien, K.O. Iron deficiency and anemia are prevalent in women with multiple gestations. Am. J. Clin. Nutr. 2016, 104, 1052–1060. [Google Scholar] [CrossRef] [PubMed]
- Shinar, S.; Skornick-Rapaport, A.; Maslovitz, S. Iron supplementation in twin pregnancy—The benefit of doubling the iron dose in iron deficient pregnant women: A randomized controlled trial. Twin Res. Hum. Genet. 2017, 20, 419–424. [Google Scholar] [CrossRef]
- Ali, M.K.; Abbas, A.M.; Abdelmagied, A.M.; Mohammed, G.E.; Abdalmageed, O.S. A randomized clinical trial of the efficacy of single versus double-daily dose of oral iron for prevention of iron deficiency anemia in women with twin gestations. J. Matern. Fetal Neonatal Med. 2017, 30, 2884–2889. [Google Scholar] [CrossRef] [PubMed]
- Abbas, A.M.; Elhalwagy, M.M.; Afifi, K.; Ibrahim, K.; Sweed, M.S.; Abbas, A.M.; Elhalwagy, M.M.; Afifi, K.; Ibrahim, K.; Sweed, M.S. Single vs. double dose iron supplementation for prevention of iron deficiency anemia in twin pregnancy: A randomized controlled clinical trial. Open J. Obstet. Gynecol. 2020, 10, 1788–1802. [Google Scholar] [CrossRef]
- Gambling, L.; Dunford, S.; Wallace, D.I.; Zuur, G.; Solanky, N.; Srai, S.K.S.; McArdle, H.J. Iron deficiency during pregnancy affects postnatal blood pressure in the rat. J. Physiol. 2003, 552 Pt 2, 603. [Google Scholar] [CrossRef] [PubMed]
- Gambling, L.; Andersen, H.S.; Czopek, A.; Wojciak, R.; Krejpcio, Z.; McArdle, H.J. Effect of timing of iron supplementation on maternal and neonatal growth and iron status of iron-deficient pregnant rats. J. Physiol. 2004, 561 Pt 1, 195. [Google Scholar] [CrossRef]
- Cogswell, M.E.; Parvanta, I.; Ickes, L.; Yip, R.; Brittenham, G.M. Iron supplementation during pregnancy, anemia, and birth weight: A randomized controlled trial. Am. J. Clin. Nutr. 2003, 78, 773–781. [Google Scholar] [CrossRef]
- Alwan, N.A.; Greenwood, D.C.; Simpson, N.A.B.; McArdle, H.J.; Godfrey, K.M.; Cade, J.E. Dietary iron intake during early pregnancy and birth outcomes in a cohort of british women. Hum. Reprod. 2011, 26, 911. [Google Scholar] [CrossRef]
- Peña-Rosas, J.P.; De-Regil, L.M.; Garcia-Casal, M.N.; Dowswell, T. Daily oral iron supplementation during pregnancy. Cochrane Database Syst. Rev. 2015, 2015, CD004736. [Google Scholar] [CrossRef]
- Figueiredo, A.C.M.G.; Gomes-Filho, I.S.; Silva, R.B.; Pereira, P.P.S.; Da Mata, F.A.F.; Lyrio, A.O.; Souza, E.S.; Cruz, S.S.; Pereira, M.G. Maternal anemia and low birth weight: A systematic review and meta-analysis. Nutrients 2018, 10, 601. [Google Scholar] [CrossRef] [PubMed]
- Cnattingius, S. The epidemiology of smoking during pregnancy: Smoking prevalence, maternal characteristics, and pregnancy outcomes. Nicotine Tob. Res. 2004, 6 (Suppl. 2), S125–S140. [Google Scholar] [CrossRef] [PubMed]
- Aldosari, K.H.; Ahmad, G.; Al-Ghamdi, S.; Alsharif, M.H.K.; Elamin, A.Y.; Musthafa, M.; Abbas, M.Y.; Alqarni, A.A.; Alqudeebi, S.K.; Binsaqer, A.A.; et al. The influence and impact of smoking on red blood cell morphology and buccal microflora: A case-control study. J. Clin. Lab. Anal. 2020, 34, e23212. [Google Scholar] [CrossRef] [PubMed]
- Van Tiel, E.D.; Peeters, P.H.M.; Smit, H.A.; Nagelkerke, N.J.D.; Van Loon, A.J.M.; Grobbee, D.E.; Bueno-De-Mesquita, H.B. Quitting smoking may restore hematological characteristics within five years. Ann. Epidemiol. 2002, 12, 378–388. [Google Scholar] [CrossRef]
- McDonald, E.A.; Gundogan, F.; Olveda, R.M.; Bartnikas, T.B.; Kurtis, J.D.; Friedman, J.F. Iron transport across the human placenta is regulated by hepcidin. Pediatr. Res. 2022, 92, 396–402. [Google Scholar] [CrossRef]
| Parameter | AM ± SD | −95% CL | +95% CL | Med | Range | |
|---|---|---|---|---|---|---|
| Maternal Characteristics | ||||||
| age (years) | 31.0 ± 4.2 | 3.55 | 5.02 | 30 | 21–41 | |
| BMI before pregnancy | 23.5 ± 3.6 | 2.92 | 4.48 | 22.9 | 18.4–34.2 | |
| weight (kg) before pregnancy | 65.5 ± 11.4 | 9.34 | 14.19 | 65 | 50–100 | |
| weight (kg) before delivery | 83.9 ± 4.2 | 13.27 | 18.77 | 81.7 | 63–138 | |
| Weight gain during pregnancy | 19.4 ± 8.6 | 7.08 | 10.76 | 16.0 | 8–38 | |
| red blood cell indices | HgB (mmol/L) | 7.7 ± 0.9 | 0.76 | 1.08 | 7.5 | 5.7–9.7 |
| HCT (L/L) | 0.361 ± 0.004 | 0.03 | 0.04 | 0.362 | 0.266–0.436 | |
| MCV (fl) | 87.7 ± 5.7 | 4.81 | 6.79 | 89.0 | 73.4–100.3 | |
| MCH (fmol) | 1.87 ± 0.16 | 0.14 | 0.19 | 1.86 | 1.46–2.28 | |
| MCHC (mmol/L) | 21.3 ± 0.7 | 0.59 | 0.84 | 21.3 | 19.9–22.7 | |
| Neonatal characteristics | ||||||
| gestational age—weeks | 35 ± 2 | 1.81 | 2.56 | 36 | 27–38 | |
| birth weight (g) | 2376.6 ± 467.3 | 397.32 | 561.80 | 2485 | 690–3350 | |
| length (cm) | 49.0 ± 4.0 | 3.37 | 4.77 | 50 | 29–55 | |
| head circumference (cm) | 32.4 ± 2.1 | 1.76 | 2.49 | 33 | 25–37 | |
| shoulder width (cm) | 29.8 ± 2.9 | 2.47 | 3.49 | 30 | 18–36 | |
| placenta weight (g) | 519.7 ± 102.5 | 87.13 | 123.20 | 500 | 330–800 | |
| length of the umbilical cord (cm) | 53.8 ± 8.2 | 6.92 | 9.79 | 54 | 28–75 | |
| Centiles for Length (cm) | Boys | Girls | Total | Centiles for Birth Weight (kg) | Boys | Girls | Total |
|---|---|---|---|---|---|---|---|
| <3 | 2 | 0 | 2 | <3 | 1 | 1 | 2 |
| 3–10 | 1 | 0 | 1 | 3 | 0 | 2 | 2 |
| 10–50 | 1 | 1 | 2 | 3–10 | 0 | 1 | 1 |
| 50 | 5 | 1 | 6 | 10 | 6 | 5 | 11 |
| 50–90 | 3 | 3 | 6 | 10–50 | 13 | 9 | 22 |
| 90 | 6 | 16 | 22 | 50 | 8 | 10 | 18 |
| 90–97 | 5 | 0 | 5 | 50–90 | 5 | 2 | 7 |
| 97 | 6 | 7 | 13 | 90 | 1 | 0 | 1 |
| >97 | 6 | 3 | 9 | 97 | 0 | 1 | 1 |
| >97 | 1 | 0 | 1 |
| Supplementation | Med | Smoked Cigarettes before Pregnancy | Med | Centiles for Length | Med | Centiles for Birth Weight | Med | |||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Supplementation | Non-Take Supplementation | Cigarette no Smoking # | Cigarette Smoking # | NormalCentiles for Length | AbnormalCentiles for Length | NormalCentiles for Birth Weight | AbnormalCentiles for Birth Weight | |||||
| Gestational age | 2.41 * | 36 | 34 | 2.58 ** | 36 | 34 | ||||||
| Placenta weight | −3.59 *** | 520 | 435 | 2.32 * | 510 | 430 | 2.07 * | 500 | 430 | |||
| Infant’s shoulder width | −3.24 *** | 31 | 28 | 2.45 ** | 30 | 25 | ||||||
| Infant’s weight | −2.62 ** | 2540 | 2055 | |||||||||
| Circumference of the infant’s head | −2.31 * | 33 | 31.5 | |||||||||
| MCV maternal | 2.95 *** | 89.3 | 83.5 | |||||||||
| MCH maternal | 3.02 *** | 1.920 | 1.745 | |||||||||
| MCHC maternal | 2.46 ** | 21.4 | 20.5 | |||||||||
| AM ± SD | −95% CL | +95% CL | Med | Min | Max | |
|---|---|---|---|---|---|---|
| pairs of monozygotic twins | ||||||
| T1 (n = 23) | 465.87 ± 106.21 | 82.14 | 150.32 | 484.24 | 206.28 | 665.82 |
| T2 (n = 23) | 435.45 ± 143.58 | 110.47 | 205.19 | 429.14 | 189.19 | 747.67 |
| T1 + T2 (n = 46) | 451.00 ± 125.36 | 103.78 | 158.36 | 480.31 | 189.19 | 747.67 |
| pairs of mixed-sex twins | ||||||
| T1 (n = 10) | 442.10 ± 83.46 | 57.41 | 152.37 | 423.96 | 331.33 | 589.42 |
| T2 (n = 10) | 420.31 ± 106.76 | 73.43 | 194.90 | 415.27 | 297.88 | 653.27 |
| T1 + T2 (n = 20) | 431.21 ± 93.93 | 71.44 | 137.20 | 423.96 | 297.88 | 653.27 |
| Total | ||||||
| T1 (n = 33) | 458.67 ± 99.18 | 79.76 | 131.19 | 468.34 | 206.28 | 665.82 |
| T2 (n = 33) | 430.72 ± 131.63 | 105.53 | 175.00 | 423.94 | 189.19 | 747.67 |
| T1 + T2 (n = 66) | 444.91 ± 116.23 | 99.12 | 140.54 | 445.85 | 189.19 | 747.67 |
| Fe Concentration of Placenta | Gestational Age | Infant’s Weight | Infant’s Length | Placenta Weight | Circumference of the Infant’s Head | Maternal Age | Weight before Delivery | Weight before Pregnancy | HgB | HCT | MCV | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Neonatal characteristics | ||||||||||||
| Infant’s weight | −0.30 ** | 0.63 *** | ||||||||||
| Infant’s length | 0.64 *** | 0.63 *** | ||||||||||
| Placenta weight | 0.43 *** | 0.41 *** | 0.33 ** | |||||||||
| Circumference of the infant’s head | −0.30 ** | 0.44 *** | 0.79 *** | 0.45 *** | 0.39 *** | |||||||
| Infant’s shoulder width | 0.69 *** | 0.78 *** | 0.55 *** | 0.52 *** | 0.65 *** | |||||||
| Maternal characteristics | ||||||||||||
| Maternal age | −0.28 *** | |||||||||||
| Weight before delivery | 0.40 ** | 0.81 *** | ||||||||||
| Weight gain during pregnancy | 0.36 ** | 0.54 *** | ||||||||||
| BMI | 0.66 *** | 0.90 *** | ||||||||||
| Weight before pregnancy | ||||||||||||
| Maternal morphology | ||||||||||||
| HgB | 0.26 * | |||||||||||
| HCT | 0.26 * | 0.94 *** | ||||||||||
| MCV | 0.26 * | |||||||||||
| MCH | 0.36 *** | 0.91 *** | ||||||||||
| MCHC | 0.56 *** | 0.29 *** | ||||||||||
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Grzeszczak, K.; Kapczuk, P.; Kupnicka, P.; Mularczyk, M.; Kwiatkowski, S.; Chlubek, D.; Kosik-Bogacka, D. Preliminary Study of Iron Concentration in the Human Placenta in Twin Pregnancies. Biomolecules 2023, 13, 749. https://doi.org/10.3390/biom13050749
Grzeszczak K, Kapczuk P, Kupnicka P, Mularczyk M, Kwiatkowski S, Chlubek D, Kosik-Bogacka D. Preliminary Study of Iron Concentration in the Human Placenta in Twin Pregnancies. Biomolecules. 2023; 13(5):749. https://doi.org/10.3390/biom13050749
Chicago/Turabian StyleGrzeszczak, Konrad, Patrycja Kapczuk, Patrycja Kupnicka, Maciej Mularczyk, Sebastian Kwiatkowski, Dariusz Chlubek, and Danuta Kosik-Bogacka. 2023. "Preliminary Study of Iron Concentration in the Human Placenta in Twin Pregnancies" Biomolecules 13, no. 5: 749. https://doi.org/10.3390/biom13050749
APA StyleGrzeszczak, K., Kapczuk, P., Kupnicka, P., Mularczyk, M., Kwiatkowski, S., Chlubek, D., & Kosik-Bogacka, D. (2023). Preliminary Study of Iron Concentration in the Human Placenta in Twin Pregnancies. Biomolecules, 13(5), 749. https://doi.org/10.3390/biom13050749






