Ribose Intake as Food Integrator: Is It a Really Convenient Practice?
Abstract
:1. Introduction
2. Ribose Metabolism and Nucleotides Synthesis
3. The Claim of Ribose Intake as an Ergogenic Practice
4. Getting Closer to PPP
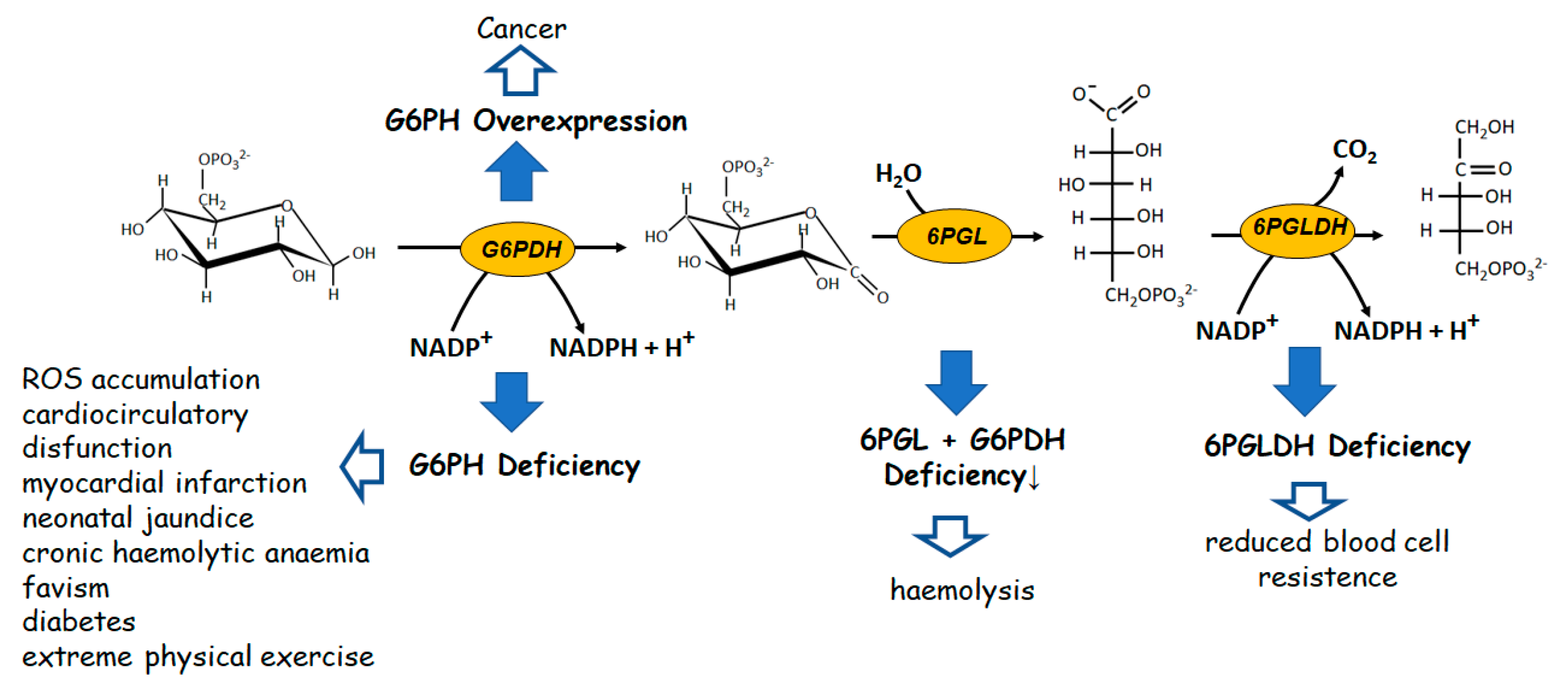
4.1. The Oxidative Branch of PPP
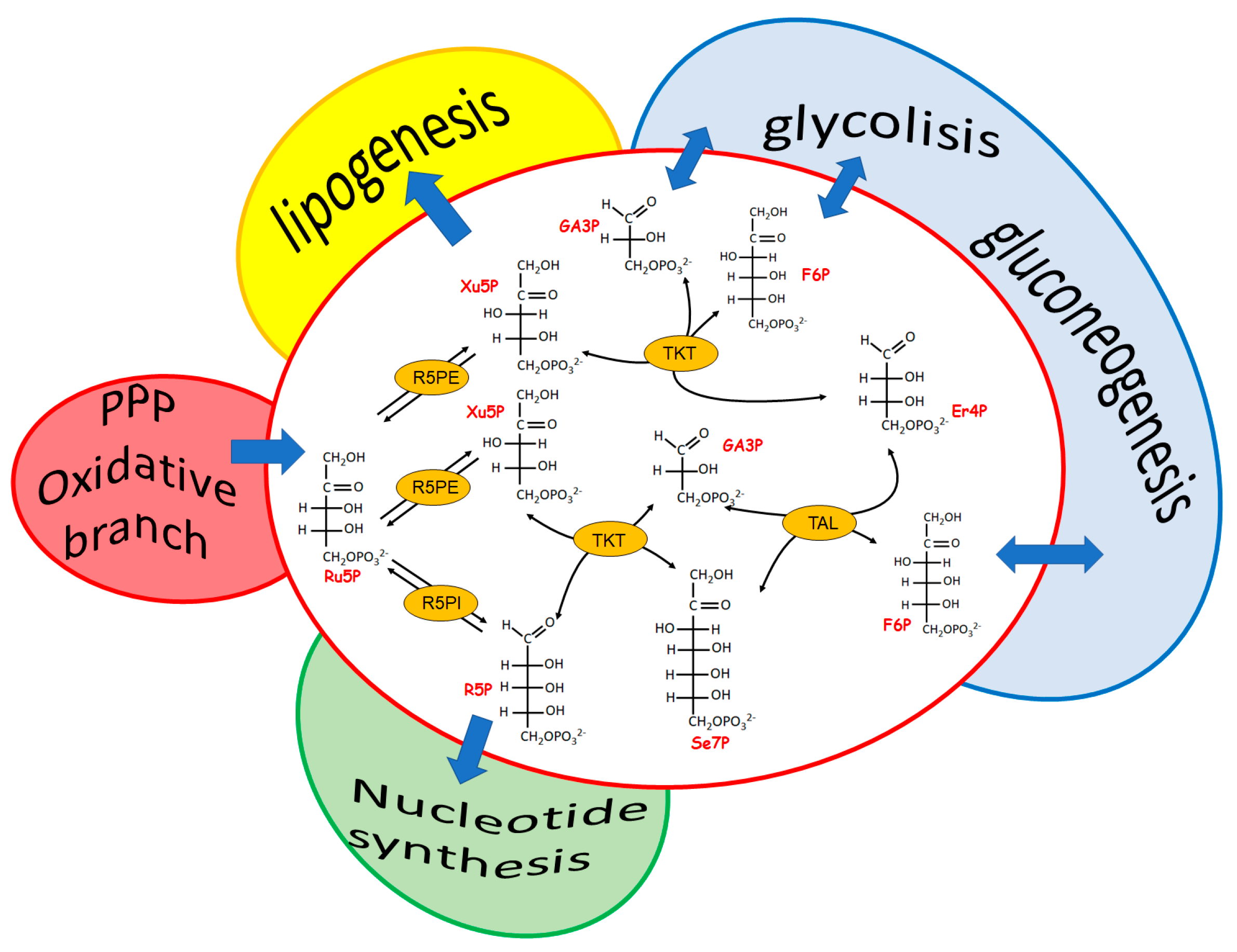
4.2. The Non-Oxidative, Reversible Branch of PPP
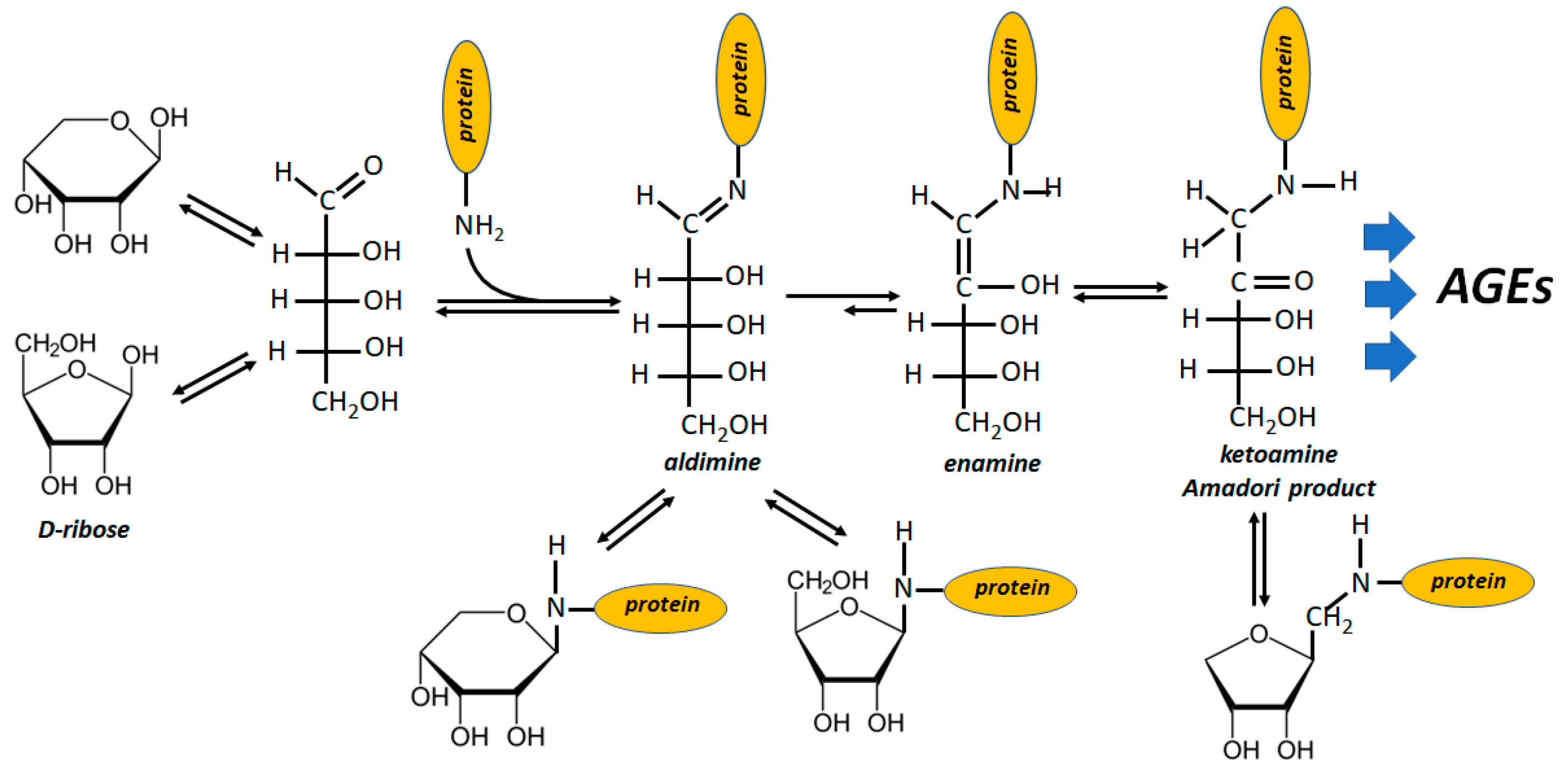
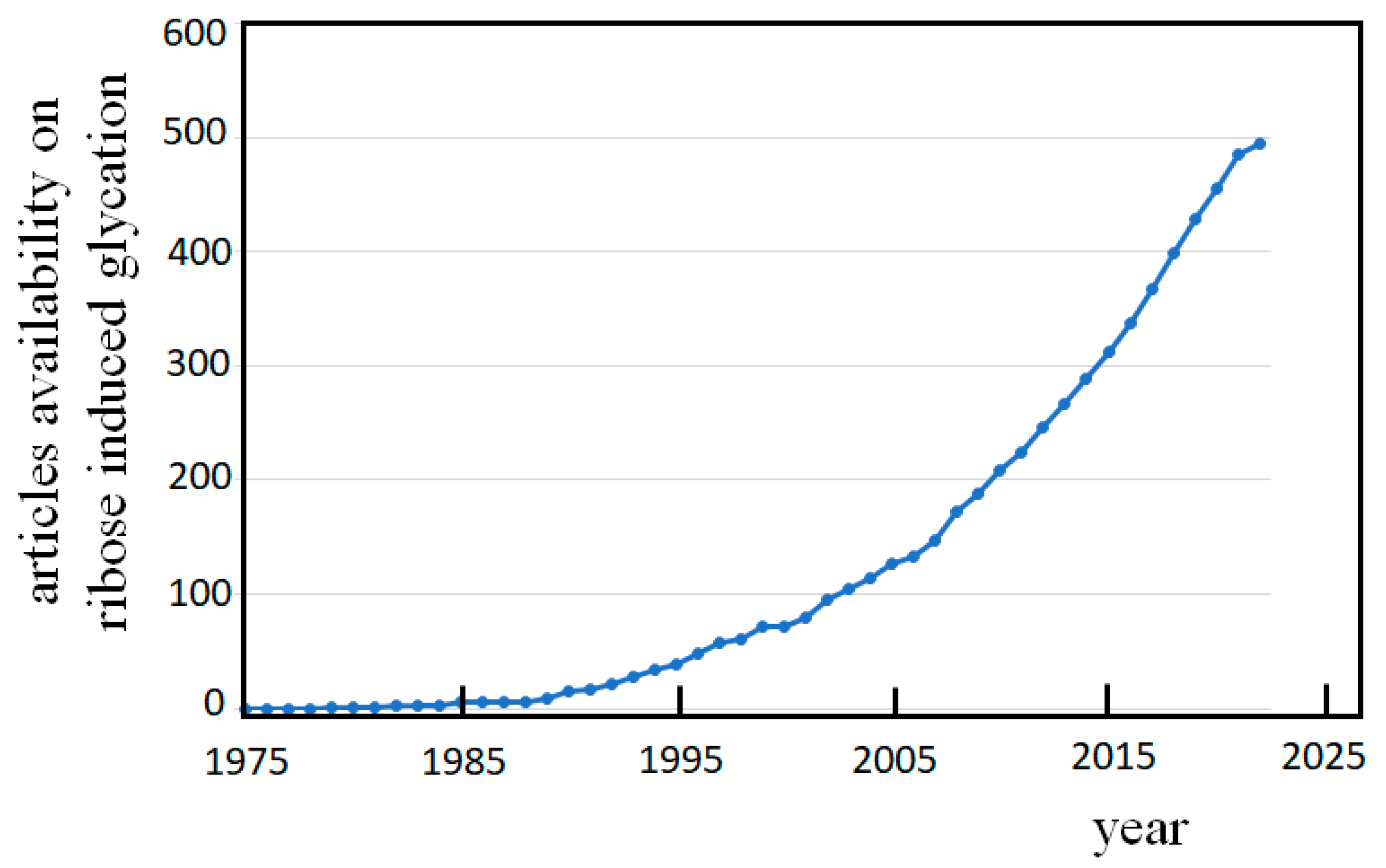
5. The Shady Side of the Ribose Intake
6. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Del-Corso, A.; Cappiello, M.; Moschini, R.; Balestri, F.; Mura, U.; Ipata, P.L. The Furanosidic Scaffold of d-Ribose: A Milestone for Cell Life. Biochem. Soc. Trans. 2019, 47, 1931–1940. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Teitelbaum, J.E.; Johnson, C.; St Cyr, J. The Use of D-Ribose in Chronic Fatigue Syndrome and Fibromyalgia: A Pilot Study. J. Altern. Complement. Med. 2006, 12, 857–862. [Google Scholar] [CrossRef] [PubMed]
- Thompson, J.; Neutel, J.; Homer, K.; Tempero, K.; Shah, A.; Khankari, R. Evaluation of D-Ribose Pharmacokinetics, Dose Proportionality, Food Effect, and Pharmacodynamics after Oral Solution Administration in Healthy Male and Female Subjects. J. Clin. Pharmacol. 2014, 54, 546–554. [Google Scholar] [CrossRef]
- Sinatra, S.T.; Caiazzo, C. (D)-Ribose Supplementation in the Equine: Lack of Effect on Glycated Plasma Proteins Suggesting Safety in Humans. J. Am. Coll. Nutr. 2015, 34, 108–112. [Google Scholar] [CrossRef] [PubMed]
- Mahoney, D.E.; Hiebert, J.B.; Thimmesch, A.; Pierce, J.T.; Vacek, J.L.; Clancy, R.L.; Sauer, A.J.; Pierce, J.D. Understanding D-Ribose and Mitochondrial Function. Adv. Biosci. Clin. Med. 2018, 6, 1–5. [Google Scholar] [CrossRef]
- Alzoubi, K.; Ismail, Z.; Al-Essa, M.; Alshogran, O.; Abutayeh, R.; Abu-Baker, N. Pharmacokinetic Evaluation of D-Ribose after Oral and Intravenous Administration to Healthy Rabbits. CPAA 2018, 10, 73–78. [Google Scholar] [CrossRef] [Green Version]
- EFSA Panel on Dietetic Products, Nutrition and Allergies (NDA); Turck, D.; Bresson, J.; Burlingame, B.; Dean, T.; Fairweather-Tait, S.; Heinonen, M.; Hirsch-Ernst, K.I.; Mangelsdorf, I.; McArdle, H.; et al. Safety of D-ribose as a Novel Food Pursuant to Regulation (EU) 2015/2283. EFSA J. 2018, 16, e05265. [Google Scholar] [CrossRef] [Green Version]
- Del-Corso, A.; Cappiello, M.; Moschini, R.; Balestri, F.; Mura, U. How the Chemical Features of Molecules May Have Addressed the Settlement of Metabolic Steps. Metabolomics 2018, 14, 2. [Google Scholar] [CrossRef] [Green Version]
- Bunn, H.F.; Higgins, P.J. Reaction of Monosaccharides with Proteins: Possible Evolutionary Significance. Science 1981, 213, 222–224. [Google Scholar] [CrossRef]
- Stincone, A.; Prigione, A.; Cramer, T.; Wamelink, M.M.C.; Campbell, K.; Cheung, E.; Olin-Sandoval, V.; Grüning, N.-M.; Krüger, A.; Tauqeer Alam, M.; et al. The Return of Metabolism: Biochemistry and Physiology of the Pentose Phosphate Pathway. Biol. Rev. Camb. Philos. Soc. 2015, 90, 927–963. [Google Scholar] [CrossRef]
- Williams, J.F.; Blackmore, P.F. Non-Oxidative Synthesis of Pentose 5-Phosphate from Hexose 6-Phosphate and Triose Phosphate by the L-Type Pentose Pathway. Int. J. Biochem. 1983, 15, 797–816. [Google Scholar] [CrossRef] [PubMed]
- Bork, P.; Sander, C.; Valencia, A. Convergent Evolution of Similar Enzymatic Function on Different Protein Folds: The Hexokinase, Ribokinase, and Galactokinase Families of Sugar Kinases: Convergent Evolution of Sugar Kinases. Protein Sci. 1993, 2, 31–40. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Park, J.; van Koeverden, P.; Singh, B.; Gupta, R.S. Identification and Characterization of Human Ribokinase and Comparison of Its Properties with E. coli Ribokinase and Human Adenosine Kinase. FEBS Lett. 2007, 581, 3211–3216. [Google Scholar] [CrossRef] [Green Version]
- Quiroga-Roger, D.; Babul, J.; Guixé, V. Role of Monovalent and Divalent Metal Cations in Human Ribokinase Catalysis and Regulation. Biometals 2015, 28, 401–413. [Google Scholar] [CrossRef]
- Chuvikovsky, D.; Esipov, R.; Skoblov, Y.; Chupova, L.; Muravyova, T.; Miroshnikov, A.; Lapinjoki, S.; Mikhailopulo, I. Ribokinase from E. coli: Expression, Purification, and Substrate Specificity. Bioorganic Med. Chem. 2006, 14, 6327–6332. [Google Scholar] [CrossRef] [PubMed]
- Maj, M.C.; Gupta, R.S. The Effect of Inorganic Phosphate on the Activity of Bacterial Ribokinase. J. Protein Chem. 2001, 20, 139–144. [Google Scholar] [CrossRef]
- Yamada, Y.; Goto, H.; Ogasawara, N. Adenosine Kinase from Human Liver. Biochim. Biophys. Acta 1981, 660, 36–43. [Google Scholar] [CrossRef]
- Schnebli, H.P.; Hill, D.L.; Bennett, L.L. Purification and Properties of Adenosine Kinase from Human Tumor Cells of Type H. Ep. No. 2. J. Biol. Chem. 1967, 242, 1997–2004. [Google Scholar] [CrossRef] [PubMed]
- Palella, T.D.; Andres, C.M.; Fox, I.H. Human Placental Adenosine Kinase: Kinetic Mechanism and Inhibition. J. Biol. Chem. 1980, 255, 5264–5269. [Google Scholar] [CrossRef]
- Angyal, S.; Bethell, G.; Cowley, D.; Pickles, V. Equilibria between Pyranoses and Furanoses. IV. 1-Deoxyhexuloses and 3-Hexuloses. Aust. J. Chem. 1976, 29, 1239. [Google Scholar] [CrossRef]
- Angyal, S.; Bethell, G. Conformational Analysis in Carbohydrate Chemistry: III. The 13C N.M.R. Spectra of the Hexuloses. Aust. J. Chem. 1976, 29, 1249. [Google Scholar] [CrossRef]
- Mahoney, J.R.; Sako, E.Y.; Seymour, K.M.; Marquardt, C.A.; Foker, J.E. A Comparison of Different Carbohydrates as Substrates for the Isolated Working Heart. J. Surg. Res. 1989, 47, 530–534. [Google Scholar] [CrossRef]
- Chang, R.S. Genetic study of human cells in vitro. J. Exp. Med. 1960, 111, 235–254. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Reitzer, L.J.; Wice, B.M.; Kennell, D. The Pentose Cycle. Control and Essential Function in HeLa Cell Nucleic Acid Synthesis. J. Biol. Chem. 1980, 255, 5616–5626. [Google Scholar] [CrossRef]
- Zimmer, H.G.; Ibel, H. Ribose Accelerates the Repletion of the ATP Pool during Recovery from Reversible Ischemia of the Rat Myocardium. J. Mol. Cell. Cardiol. 1984, 16, 863–866. [Google Scholar] [CrossRef] [PubMed]
- St Cyr, J.A.; Bianco, R.W.; Schneider, J.R.; Mahoney, J.R.; Tveter, K.; Einzig, S.; Foker, J.E. Enhanced High Energy Phosphate Recovery with Ribose Infusion after Global Myocardial Ischemia in a Canine Model. J. Surg. Res. 1989, 46, 157–162. [Google Scholar] [CrossRef]
- Pliml, W.; von Arnim, T.; Stäblein, A.; Hofmann, H.; Zimmer, H.G.; Erdmann, E. Effects of Ribose on Exercise-Induced Ischaemia in Stable Coronary Artery Disease. Lancet 1992, 340, 507–510. [Google Scholar] [CrossRef]
- Bayram, M.; St. Cyr, J.A.; Abraham, W.T. d-Ribose Aids Heart Failure Patients with Preserved Ejection Fraction and Diastolic Dysfunction: A Pilot Study. Ther. Adv. Cardiovasc. Dis. 2015, 9, 56–65. [Google Scholar] [CrossRef] [Green Version]
- Shecterle, L.M.; Terry, K.R.; St Cyr, J.A. Potential Clinical Benefits of D-Ribose in Ischemic Cardiovascular Disease. Cureus 2018, 10, e2291. [Google Scholar] [CrossRef] [Green Version]
- Bengtsson, A.; Henriksson, K.G.; Larsson, J. Reduced High-Energy Phosphate Levels in the Painful Muscles of Patients with Primary Fibromyalgia. Arthritis Rheum. 1986, 29, 817–821. [Google Scholar] [CrossRef]
- Patten, B.M. Beneficial Effect of D-Ribose in Patient with Myoadenylate Deaminase Deficiency. Lancet 1982, 1, 1071. [Google Scholar] [CrossRef] [PubMed]
- Lecky, B.R.F. Failure of D-Ribose in Myoadenylate Deaminase Deficiency. Lancet 1983, 321, 193. [Google Scholar] [CrossRef] [PubMed]
- Pauly, D.F.; Pepine, C.J. D-Ribose as a Supplement for Cardiac Energy Metabolism. J. Cardiovasc. Pharmacol. Ther. 2000, 5, 249–258. [Google Scholar] [CrossRef] [PubMed]
- Li, S.; Wang, J.; Xiao, Y.; Zhang, L.; Fang, J.; Yang, N.; Zhang, Z.; Nasser, M.I.; Qin, H. D-ribose: Potential Clinical Applications in Congestive Heart Failure and Diabetes, and Its Complications (Review). Exp. Ther. Med. 2021, 21, 496. [Google Scholar] [CrossRef]
- Kreider, R.B.; Melton, C.; Greenwood, M.; Rasmussen, C.; Lundberg, J.; Earnest, C.; Almada, A. Effects of Oral D-Ribose Supplementation on Anaerobic Capacity and Selected Metabolic Markers in Healthy Males. Int. J. Sport. Nutr. Exerc. Metab. 2003, 13, 76–86. [Google Scholar] [CrossRef]
- Berardi, J.M.; Ziegenfuss, T.N. Effects of Ribose Supplementation on Repeated Sprint Performance in Men. J. Strength Cond. Res. 2003, 17, 47–52. [Google Scholar] [CrossRef]
- Hellsten, Y.; Skadhauge, L.; Bangsbo, J. Effect of Ribose Supplementation on Resynthesis of Adenine Nucleotides after Intense Intermittent Training in Humans. Am. J. Physiol. Regul. Integr. Comp. Physiol. 2004, 286, R182–R188. [Google Scholar] [CrossRef]
- Op’t Eijnde, B.; Van Leemputte, M.; Brouns, F.; Van Der Vusse, G.J.; Labarque, V.; Ramaekers, M.; Van Schuylenberg, R.; Verbessem, P.; Wijnen, H.; Hespel, P. No Effects of Oral Ribose Supplementation on Repeated Maximal Exercise and de Novo ATP Resynthesis. J. Appl. Physiol. 2001, 91, 2275–2281. [Google Scholar] [CrossRef]
- Raue, U.; Gallagher, P.M.; Williamson, D.L.; Godard, M.P.; Trappe, S.W. Effects of Ribose Supplementation on Performance During Repeated High-Intensity Cycle Sprints. Med. Sci. Sports Exerc. 2001, 33, S44. [Google Scholar] [CrossRef]
- Van Gammeren, D.; Falk, D.; Antonio, J. The Effects of Four Weeks of Ribose Supplementation on Body Composition and Exercise Performance in Healthy, Young, Male Recreational Bodybuilders: A Double-Blind, Placebo-Controlled Trial. Curr. Ther. Res. 2002, 63, 486–495. [Google Scholar] [CrossRef]
- Seifert, J.G.; Brumet, A.; St Cyr, J.A. The Influence of D-Ribose Ingestion and Fitness Level on Performance and Recovery. J. Int. Soc. Sports Nutr. 2017, 14, 47. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Cao, W.; Qiu, J.; Cai, T.; Yi, L.; Benardot, D.; Zou, M. Effect of D-Ribose Supplementation on Delayed Onset Muscle Soreness Induced by Plyometric Exercise in College Students. J. Int. Soc. Sports Nutr. 2020, 17, 42. [Google Scholar] [CrossRef] [PubMed]
- Patra, K.C.; Hay, N. The Pentose Phosphate Pathway and Cancer. Trends Biochem. Sci. 2014, 39, 347–354. [Google Scholar] [CrossRef] [Green Version]
- Ho, H.; Cheng, M.; Chiu, D.T. Glucose-6-Phosphate Dehydrogenase—From Oxidative Stress to Cellular Functions and Degenerative Diseases. Redox Rep. 2007, 12, 109–118. [Google Scholar] [CrossRef] [PubMed]
- Vulliamy, T.J.; D’Urso, M.; Battistuzzi, G.; Estrada, M.; Foulkes, N.S.; Martini, G.; Calabro, V.; Poggi, V.; Giordano, R.; Town, M. Diverse Point Mutations in the Human Glucose-6-Phosphate Dehydrogenase Gene Cause Enzyme Deficiency and Mild or Severe Hemolytic Anemia. Proc. Natl. Acad. Sci. USA 1988, 85, 5171–5175. [Google Scholar] [CrossRef] [Green Version]
- Gómez-Manzo, S.; Marcial-Quino, J.; Vanoye-Carlo, A.; Serrano-Posada, H.; Ortega-Cuellar, D.; González-Valdez, A.; Castillo-Rodríguez, R.; Hernández-Ochoa, B.; Sierra-Palacios, E.; Rodríguez-Bustamante, E.; et al. Glucose-6-Phosphate Dehydrogenase: Update and Analysis of New Mutations around the World. Int. J. Mol. Sci. 2016, 17, 2069. [Google Scholar] [CrossRef] [Green Version]
- Johnson, L.H.; Bhutani, V.K.; Brown, A.K. System-Based Approach to Management of Neonatal Jaundice and Prevention of Kernicterus. J. Pediatr. 2002, 140, 396–403. [Google Scholar] [CrossRef]
- Filosa, S.; Cai, W.; Galanello, R.; Cao, A.; De Mattia, D.; Schettini, F.; Martini, G. A Novel Single-Base Mutation in the Glucose 6-Phosphate Dehydrogenase Gene Is Associated with Chronic Non-Spherocytic Haemolytic Anaemia. Hum. Genet. 1994, 94, 560–562. [Google Scholar] [CrossRef]
- Luzzatto, L.; Poggi, V. Chapter 17: Glucose-6-Phosphate Dehydrogenase Deficiency. In Nathan and Oski’s Hematology of Infancy and Childhood; Orkin, S., Ed.; Elsevier: Philadelphia, PA, USA, 2009. [Google Scholar]
- Manganelli, G.; Fico, A.; Martini, G.; Filosa, S. Discussion on Pharmacogenetic Interaction in G6PD Deficiency and Methods to Identify Potential Hemolytic Drugs. Cardiovasc. Hematol. Disord. Drug Targets 2010, 10, 143–150. [Google Scholar] [CrossRef]
- Liu, W.-L.; Li, F.; He, Z.-X.; Jiang, H.-Y.; Ai, R. Glucose-6-Phosphate Dehydrogenase Qingzhen: Identification of a Novel Splice Mutation (IVS5-1 G>A). Pediatr. Blood Cancer 2012, 58, 825–826. [Google Scholar] [CrossRef]
- Luzzatto, L.; Arese, P. Favism and Glucose-6-Phosphate Dehydrogenase Deficiency. N. Engl. J. Med. 2018, 378, 60–71. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Beutler, E. Glucose-6-Phosphate Dehydrogenase Deficiency: A Historical Perspective. Blood 2008, 111, 16–24. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Maisels, M.J. Neonatal Jaundice. Pediatr. Rev. 2006, 27, 443–454. [Google Scholar] [CrossRef]
- Carette, C.; Dubois-Laforgue, D.; Gautier, J.-F.; Timsit, J. Diabetes Mellitus and Glucose-6-Phosphate Dehydrogenase Deficiency: From One Crisis to Another. Diabetes Metab. 2011, 37, 79–82. [Google Scholar] [CrossRef]
- Leopold, J.A.; Cap, A.; Scribner, A.W.; Stanton, R.C.; Loscalzo, J. Glucose-6-phosphate Dehydrogenase Deficiency Promotes Endothelial Oxidant Stress and Decreases Endothelial Nitric Oxide Bioavailability. FASEB J. 2001, 15, 1771–1773. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Jain, M.; Brenner, D.A.; Cui, L.; Lim, C.C.; Wang, B.; Pimentel, D.R.; Koh, S.; Sawyer, D.B.; Leopold, J.A.; Handy, D.E.; et al. Glucose-6-Phosphate Dehydrogenase Modulates Cytosolic Redox Status and Contractile Phenotype in Adult Cardiomyocytes. Circ. Res. 2003, 93, e9–e16. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Jain, M.; Cui, L.; Brenner, D.A.; Wang, B.; Handy, D.E.; Leopold, J.A.; Loscalzo, J.; Apstein, C.S.; Liao, R. Increased Myocardial Dysfunction After Ischemia-Reperfusion in Mice Lacking Glucose-6-Phosphate Dehydrogenase. Circulation 2004, 109, 898–903. [Google Scholar] [CrossRef] [Green Version]
- Caprari, P.; Caforio, M.P.; Cianciulli, P.; Maffi, D.; Pasquino, M.T.; Tarzia, A.; Amadori, S.; Salvati, A.M. 6-Phosphogluconate Dehydrogenase Deficiency in an Italian Family. Ann. Hematol. 2001, 80, 41–44. [Google Scholar] [CrossRef]
- Vives Corrons, J.L.; Colomer, D.; Pujades, A.; Rovira, A.; Aymerich, M.; Merino, A.; Aguilar i Bascompte, J.L. Congenital 6-Phosphogluconate Dehydrogenase (6PGD) Deficiency Associated with Chronic Hemolytic Anemia in a Spanish Family. Am. J. Hematol. 1996, 53, 221–227. [Google Scholar] [CrossRef]
- Beutler, E.; Kuhl, W.; Gelbart, T. 6-Phosphogluconolactonase Deficiency, a Hereditary Erythrocyte Enzyme Deficiency: Possible Interaction with Glucose-6-Phosphate Dehydrogenase Deficiency. Proc. Natl. Acad. Sci. USA 1985, 82, 3876–3878. [Google Scholar] [CrossRef]
- Kowalik, M.A.; Columbano, A.; Perra, A. Emerging Role of the Pentose Phosphate Pathway in Hepatocellular Carcinoma. Front. Oncol. 2017, 7, 87. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Song, J.; Sun, H.; Zhang, S.; Shan, C. The Multiple Roles of Glucose-6-Phosphate Dehydrogenase in Tumorigenesis and Cancer Chemoresistance. Life 2022, 12, 271. [Google Scholar] [CrossRef] [PubMed]
- Heinrich, P.C.; Morris, H.P.; Weber, G. Behavior of Transaldolase (EC 2.2. 1.2) and Transketolase (EC 2.2. 1.1) Activities in Normal, Neoplastic, Differentiating, and Regenerating Liver. Cancer Res. 1976, 36, 3189–3197. [Google Scholar] [PubMed]
- Samland, A.K.; Sprenger, G.A. Transaldolase: From Biochemistry to Human Disease. Int. J. Biochem. Cell. Biol. 2009, 41, 1482–1494. [Google Scholar] [CrossRef]
- Ahopelto, K.; Böckelman, C.; Hagström, J.; Koskensalo, S.; Haglund, C. Transketolase-like Protein 1 Expression Predicts Poor Prognosis in Colorectal Cancer. Cancer Biol. Ther. 2016, 17, 163–168. [Google Scholar] [CrossRef] [Green Version]
- Zhang, S.; Yang, J.-H.; Guo, C.-K.; Cai, P. Gene Silencing of TKTL1 by RNAi Inhibits Cell Proliferation in Human Hepatoma Cells. Cancer Lett. 2007, 253, 108–114. [Google Scholar] [CrossRef]
- Krockenberger, M.; Engel, J.B.; Schmidt, M.; Kohrenhagen, N.; Häusler, S.F.M.; Dombrowski, Y.; Kapp, M.; Dietl, J.; Honig, A. Expression of Transketolase-like 1 Protein (TKTL1) in Human Endometrial Cancer. Anticancer Res. 2010, 30, 1653–1659. [Google Scholar]
- Langbein, S.; Frederiks, W.M.; zur Hausen, A.; Popa, J.; Lehmann, J.; Weiss, C.; Alken, P.; Coy, J.F. Metastasis Is Promoted by a Bioenergetic Switch: New Targets for Progressive Renal Cell Cancer. Int. J. Cancer 2008, 122, 2422–2428. [Google Scholar] [CrossRef]
- Zerilli, M.; Amato, M.C.; Martorana, A.; Cabibi, D.; Coy, J.F.; Cappello, F.; Pompei, G.; Russo, A.; Giordano, C.; Rodolico, V. Increased Expression of Transketolase-like-1 in Papillary Thyroid Carcinomas Smaller than 1.5 Cm in Diameter Is Associated with Lymph-Node Metastases. Cancer 2008, 113, 936–944. [Google Scholar] [CrossRef]
- Chen, H.; Yue, J.-X.; Yang, S.-H.; Ding, H.; Zhao, R.-W.; Zhang, S. Overexpression of Transketolase-like Gene 1 Is Associated with Cell Proliferation in Uterine Cervix Cancer. J. Exp. Clin. Cancer Res. 2009, 28, 43. [Google Scholar] [CrossRef] [Green Version]
- Ahopelto, K.; Laitinen, A.; Hagström, J.; Böckelman, C.; Haglund, C. Transketolase-Like Protein 1 and Glucose Transporter 1 in Gastric Cancer. Oncology 2020, 98, 643–652. [Google Scholar] [CrossRef] [PubMed]
- Huang, J.-B.; Espinoza, J.; Romero, R.; Petty, H.R. Transaldolase Is Part of a Supramolecular Complex Containing Glucose-6-Phosphate Dehydrogenase in Human Neutrophils That Undergoes Retrograde Trafficking during Pregnancy. Metabolism 2005, 54, 1027–1033. [Google Scholar] [CrossRef] [PubMed]
- Ni, T.-C.; Savageau, M.A. Application of Biochemical Systems Theory to Metabolism in Human Red Blood Cells. J. Biol. Chem. 1996, 271, 7927–7941. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Banki, K.; Hutter, E.; Colombo, E.; Gonchoroff, N.J.; Perl, A. Glutathione Levels and Sensitivity to Apoptosis Are Regulated by Changes in Transaldolase Expression. J. Biol. Chem. 1996, 271, 32994–33001. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Lachaise, F.; Martin, G.; Drougard, C.; Perl, A.; Vuillaume, M.; Wegnez, M.; Sarasin, A.; Daya-Grosjean, L. Relationship between Posttranslational Modification of Transaldolase and Catalase Deficiency in UV-Sensitive Repair-Deficient Xeroderma Pigmentosum Fibroblasts and SV40-Transformed Human Cells. Free Radic. Biol. Med. 2001, 30, 1365–1373. [Google Scholar] [CrossRef]
- Coy, J.F.; Dressler, D.; Wilde, J.; Schubert, P. Mutations in the Transketolase-like Gene TKTL1: Clinical Implications for Neurodegenerative Diseases, Diabetes and Cancer. Clin. Lab. 2005, 51, 257–273. [Google Scholar]
- Zhao, J.; Zhong, C.-J. A Review on Research Progress of Transketolase. Neurosci. Bull. 2009, 25, 94–99. [Google Scholar] [CrossRef] [Green Version]
- Perl, A. The Pathogenesis of Transaldolase Deficiency. IUBMB Life 2007, 59, 365–373. [Google Scholar] [CrossRef]
- Perl, A.; Hanczko, R.; Telarico, T.; Oaks, Z.; Landas, S. Oxidative Stress, Inflammation and Carcinogenesis Are Controlled through the Pentose Phosphate Pathway by Transaldolase. Trends Mol. Med. 2011, 17, 395–403. [Google Scholar] [CrossRef] [Green Version]
- Balestri, F.; Cappiello, M.; Moschini, R.; Rotondo, R.; Abate, M.; Del-Corso, A.; Mura, U. Modulation of Aldose Reductase Activity by Aldose Hemiacetals. Biochim. Biophys. Acta (BBA) Gen. Subj. 2015, 1850, 2329–2339. [Google Scholar] [CrossRef] [Green Version]
- Tozzi, M.G.; Camici, M.; Mascia, L.; Sgarrella, F.; Ipata, P.L. Pentose Phosphates in Nucleoside Interconversion and Catabolism. FEBS J. 2006, 273, 1089–1101. [Google Scholar] [CrossRef] [PubMed]
- Maliekal, P.; Sokolova, T.; Vertommen, D.; Veiga-da-Cunha, M.; Van Schaftingen, E. Molecular Identification of Mammalian Phosphopentomutase and Glucose-1,6-Bisphosphate Synthase, Two Members of the Alpha-D-Phosphohexomutase Family. J. Biol. Chem. 2007, 282, 31844–31851. [Google Scholar] [CrossRef] [PubMed]
- Kabashima, T.; Kawaguchi, T.; Wadzinski, B.E.; Uyeda, K. Xylulose 5-Phosphate Mediates Glucose-Induced Lipogenesis by Xylulose 5-Phosphate-Activated Protein Phosphatase in Rat Liver. Proc. Natl. Acad. Sci. USA 2003, 100, 5107–5112. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Iizuka, K.; Wu, W.; Horikawa, Y.; Takeda, J. Role of Glucose-6-Phosphate and Xylulose-5-Phosphate in the Regulation of Glucose-Stimulated Gene Expression in the Pancreatic β Cell Line, INS-1E. Endocr. J. 2013, 60, 473–482. [Google Scholar] [CrossRef] [Green Version]
- Iizuka, K. The Roles of Carbohydrate Response Element Binding Protein in the Relationship between Carbohydrate Intake and Diseases. Int. J. Mol. Sci. 2021, 22, 12058. [Google Scholar] [CrossRef]
- Chou, Y.-T.; Chen, L.-Y.; Tsai, S.-L.; Tu, H.-C.; Lu, J.-W.; Ciou, S.-C.; Wang, H.-D.; Yuh, C.-H. Ribose-5-Phosphate Isomerase A Overexpression Promotes Liver Cancer Development in Transgenic Zebrafish via Activation of ERK and β-Catenin Pathways. Carcinogenesis 2019, 40, 461–473. [Google Scholar] [CrossRef]
- Ciou, S.; Chou, Y.; Liu, Y.; Nieh, Y.; Lu, J.; Huang, S.; Chou, Y.; Cheng, L.; Lo, J.; Chen, M.; et al. Ribose-5-phosphate Isomerase A Regulates Hepatocarcinogenesis via PP2A and ERK Signaling. Int. J. Cancer 2015, 137, 104–115. [Google Scholar] [CrossRef]
- Jin, L.; Zhou, Y. Crucial Role of the Pentose Phosphate Pathway in Malignant Tumors (Review). Oncol. Lett. 2019, 17, 4213–4221. [Google Scholar] [CrossRef] [Green Version]
- Ge, T.; Yang, J.; Zhou, S.; Wang, Y.; Li, Y.; Tong, X. The Role of the Pentose Phosphate Pathway in Diabetes and Cancer. Front. Endocrinol. 2020, 11, 365. [Google Scholar] [CrossRef]
- Wei, Y.; Han, C.S.; Zhou, J.; Liu, Y.; Chen, L.; He, R.Q. D-Ribose in Glycation and Protein Aggregation. Biochim. Biophys. Acta 2012, 1820, 488–494. [Google Scholar] [CrossRef]
- Siddiqui, Z.; Ishtikhar, M.; Moinuddin, N.; Ahmad, S. D-Ribose Induced Glycoxidative Insult to Hemoglobin Protein: An Approach to Spot Its Structural Perturbations. Int. J. Biol. Macromol. 2018, 112, 134–147. [Google Scholar] [CrossRef] [PubMed]
- Chen, Y.; Yu, L.; Wang, Y.; Wei, Y.; Xu, Y.; He, T.; He, R. D-Ribose Contributes to the Glycation of Serum Protein. Biochim. Et Biophys. Acta (BBA) Mol. Basis Dis. 2019, 1865, 2285–2292. [Google Scholar] [CrossRef] [PubMed]
- Feroz, A.; Khaki, P.S.S.; Khan, M.S.; Bano, B. Protein Aggregation as a Consequence of Non-Enzymatic Glycation: Therapeutic Intervention Using Aspartic Acid and Arginine. Int. J. Biol. Macromol. 2020, 163, 1844–1858. [Google Scholar] [CrossRef] [PubMed]
- Mou, L.; Hu, P.; Cao, X.; Chen, Y.; Xu, Y.; He, T.; Wei, Y.; He, R. Comparison of Bovine Serum Albumin Glycation by Ribose and Fructose in Vitro and in Vivo. Biochim. Biophys. Acta (BBA) Mol. Basis Dis. 2022, 1868, 166283. [Google Scholar] [CrossRef] [PubMed]
- Ahmad, S.; Al-Shaghdali, K.; Rehman, S.; Khan, M.Y.; Rafi, Z.; Faisal, M.; Alatar, A.A.; Tahir, I.K.; Khan, S.; Ahmad, S.; et al. Nonenzymatic Glycosylation of Isolated Human Immunoglobulin-G by D-ribose. Cell Biochem. Funct. 2022, 40, 526–534. [Google Scholar] [CrossRef] [PubMed]
- Willett, T.L.; Kandel, R.; De Croos, J.N.A.; Avery, N.C.; Grynpas, M.D. Enhanced Levels of Non-Enzymatic Glycation and Pentosidine Crosslinking in Spontaneous Osteoarthritis Progression. Osteoarthr. Cartil. 2012, 20, 736–744. [Google Scholar] [CrossRef] [Green Version]
- Sell, D.R.; Monnier, V.M. End-Stage Renal Disease and Diabetes Catalyze the Formation of a Pentose-Derived Crosslink from Aging Human Collagen. J. Clin. Investig. 1990, 85, 380–384. [Google Scholar] [CrossRef]
- Dyer, D.G.; Blackledge, J.A.; Thorpe, S.R.; Baynes, J.W. Formation of Pentosidine during Nonenzymatic Browning of Proteins by Glucose. Identification of Glucose and Other Carbohydrates as Possible Precursors of Pentosidine in Vivo. J. Biol. Chem. 1991, 266, 11654–11660. [Google Scholar] [CrossRef]
- Sell, D.R.; Monnier, V.M. Structure Elucidation of a Senescence Cross-Link from Human Extracellular Matrix. J. Biol. Chem. 1989, 264, 21597–21602. [Google Scholar] [CrossRef]
- Dworkin, J.P.; Miller, S.L. A Kinetic Estimate of the Free Aldehyde Content of Aldoses. Carbohydr. Res. 2000, 329, 359–365. [Google Scholar] [CrossRef]
- Pierce, J.; Serianni, A.S.; Barker, R. Anomerization of Furanose Sugars and Sugar Phosphates. J. Am. Chem. Soc. 1985, 107, 2448–2456. [Google Scholar] [CrossRef]
- Munanairi, A.; O’Banion, S.K.; Gamble, R.; Breuer, E.; Harris, A.W.; Sandwick, R.K. The Multiple Maillard Reactions of Ribose and Deoxyribose Sugars and Sugar Phosphates. Carbohydr. Res. 2007, 342, 2575–2592. [Google Scholar] [CrossRef]
- Sandwick, R.; Johanson, M.; Breuer, E. Maillard Reactions of Ribose 5-Phosphate and Amino Acids. Ann. N. Y. Acad. Sci. 2005, 1043, 85–96. [Google Scholar] [CrossRef] [PubMed]
- Gersten, R.A.; Gretebeck, L.M.; Hildick-Smith, G.; Sandwick, R.K. Maillard Reaction of Ribose 5-Phosphate Generates Superoxide and Glycation Products for Bovine Heart Cytochrome c Reduction. Carbohydr. Res. 2010, 345, 2499–2506. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Fica-Contreras, S.M.; Shuster, S.O.; Durfee, N.D.; Bowe, G.J.K.; Henning, N.J.; Hill, S.A.; Vrla, G.D.; Stillman, D.R.; Suralik, K.M.; Sandwick, R.K.; et al. Glycation of Lys-16 and Arg-5 in Amyloid-β and the Presence of Cu2+ Play a Major Role in the Oxidative Stress Mechanism of Alzheimer’s Disease. J. Biol. Inorg. Chem. 2017, 22, 1211–1222. [Google Scholar] [CrossRef]
- Chen, X.; Su, T.; Chen, Y.; He, Y.; Liu, Y.; Xu, Y.; Wei, Y.; Li, J.; He, R. D -Ribose as a Contributor to Glycated Haemoglobin. EBioMedicine 2017, 25, 143–153. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Bokiej, M.; Livermore, A.T.; Harris, A.W.; Onishi, A.C.; Sandwick, R.K. Ribose Sugars Generate Internal Glycation Cross-Links in Horse Heart Myoglobin. Biochem. Biophys. Res. Commun. 2011, 407, 191–196. [Google Scholar] [CrossRef] [Green Version]
- Liu, J.-J.; You, Y.; Gao, S.-Q.; Tang, S.; Chen, L.; Wen, G.-B.; Lin, Y.-W. Identification of the Protein Glycation Sites in Human Myoglobin as Rapidly Induced by D-Ribose. Molecules 2021, 26, 5829. [Google Scholar] [CrossRef]
- Viviani, G.L.; Puddu, A.; Sacchi, G.; Garuti, A.; Storace, D.; Durante, A.; Monacelli, F.; Odetti, P. Glycated Fetal Calf Serum Affects the Viability of an Insulin-Secreting Cell Line in Vitro. Metabolism 2008, 57, 163–169. [Google Scholar] [CrossRef]
- Wei, Y.; Chen, L.; Chen, J.; Ge, L.; He, R.Q. Rapid Glycation with D-Ribose Induces Globular Amyloid-like Aggregations of BSA with High Cytotoxicity to SH-SY5Y Cells. BMC Cell. Biol. 2009, 10, 10. [Google Scholar] [CrossRef] [Green Version]
- Das, A.; Basak, P.; Pramanik, A.; Majumder, R.; Ghosh, A.; Hazra, S.; Guria, M.; Bhattacharyya, M.; Banik, S.P. Ribosylation Induced Structural Changes in Bovine Serum Albumin: Understanding High Dietary Sugar Induced Protein Aggregation and Amyloid Formation. Heliyon 2020, 6, e05053. [Google Scholar] [CrossRef] [PubMed]
- Khanam, A.; Alouffi, S.; Rehman, S.; Ansari, I.A.; Shahab, U.; Ahmad, S. An in Vitro Approach to Unveil the Structural Alterations in d-Ribose Induced Glycated Fibrinogen. J. Biomol. Struct. Dyn. 2021, 39, 5209–5223. [Google Scholar] [CrossRef] [PubMed]
- Ahmad, S.; Akhter, F.; Moinuddin; Shahab, U.; Khan, M.S. Studies on Glycation of Human Low Density Lipoprotein: A Functional Insight into Physico-Chemical Analysis. Int. J. Biol. Macromol. 2013, 62, 167–171. [Google Scholar] [CrossRef] [PubMed]
- Akhter, F.; Salman Khan, M.; Faisal, M.; Alatar, A.A.; Ahmad, S. Detection of Circulating Auto-Antibodies Against Ribosylated-LDL in Diabetes Patients. J. Clin. Lab. Anal. 2017, 31, e22039. [Google Scholar] [CrossRef]
- Akhter, F.; Khan, M.S.; Ahmad, S. Acquired Immunogenicity of Calf Thymus DNA and LDL Modified by D-Ribose: A Comparative Study. Int. J. Biol. Macromol. 2015, 72, 1222–1227. [Google Scholar] [CrossRef]
- Iannuzzi, C.; Irace, G.; Sirangelo, I. Role of Glycation in Amyloid: Effect on the Aggregation Process and Cytotoxicity. In Exploring New Findings on Amyloidosis; Fernandez-Escamilla, A.M., Ed.; IntechOpen: London, UK, 2016; ISBN 978-953-51-2618-8. [Google Scholar]
- Javed, M.; Ahmad, M.I.; Javed, H.; Naseem, S. D-Ribose and Pathogenesis of Alzheimer’s Disease. Mol. Biol. Rep. 2020, 47, 2289–2299. [Google Scholar] [CrossRef]
- Chen, L.; Wei, Y.; Wang, X.; He, R. D-Ribosylated Tau Forms Globular Aggregates with High Cytotoxicity. Cell. Mol. Life Sci. 2009, 66, 2559–2571. [Google Scholar] [CrossRef]
- Kong, F.-L.; Cheng, W.; Chen, J.; Liang, Y. D-Ribose Glycates Β2-Microglobulin to Form Aggregates with High Cytotoxicity through a ROS-Mediated Pathway. Chem. Biol. Interact. 2011, 194, 69–78. [Google Scholar] [CrossRef]
- Wei, Y.; Han, C.; Wang, Y.; Wu, B.; Su, T.; Liu, Y.; He, R. Ribosylation Triggering Alzheimer’s Disease-like Tau Hyperphosphorylation via Activation of CaMKII. Aging Cell 2015, 14, 754–763. [Google Scholar] [CrossRef]
- Wu, B.; Wang, Y.; Shi, C.; Chen, Y.; Yu, L.; Li, J.; Li, W.; Wei, Y.; He, R. Ribosylation-Derived Advanced Glycation End Products Induce Tau Hyperphosphorylation Through Brain-Derived Neurotrophic Factor Reduction. J. Alzheimer Dis. 2019, 71, 291–305. [Google Scholar] [CrossRef]
- Farzadfard, A.; König, A.; Petersen, S.V.; Nielsen, J.; Vasili, E.; Dominguez-Meijide, A.; Buell, A.K.; Outeiro, T.F.; Otzen, D.E. Glycation Modulates Alpha-Synuclein Fibrillization Kinetics: A Sweet Spot for Inhibition. J. Biol. Chem. 2022, 298, 101848. [Google Scholar] [CrossRef] [PubMed]
- Chen, L.; Wei, Y.; Wang, X.; He, R. Ribosylation Rapidly Induces α-Synuclein to Form Highly Cytotoxic Molten Globules of Advanced Glycation End Products. PLoS ONE 2010, 5, e9052. [Google Scholar] [CrossRef] [PubMed]
- Han, C.; Lu, Y.; Wei, Y.; Wu, B.; Liu, Y.; He, R. D-Ribosylation Induces Cognitive Impairment through RAGE-Dependent Astrocytic Inflammation. Cell Death Dis. 2014, 5, e1117. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Han, C.; Lu, Y.; Wei, Y.; Liu, Y.; He, R. D-Ribose Induces Cellular Protein Glycation and Impairs Mouse Spatial Cognition. PLoS ONE 2011, 6, e24623. [Google Scholar] [CrossRef] [Green Version]
- Yu, L.; Chen, Y.; Xu, Y.; He, T.; Wei, Y.; He, R. D-Ribose Is Elevated in T1DM Patients and Can Be Involved in the Onset of Encephalopathy. Aging 2019, 11, 4943–4969. [Google Scholar] [CrossRef]
- Lu, Y.; Jiang, H.; Zhang, H.; Li, R.; Zhang, Q.; Luo, D.; Cai, X.; Li, M. Serum Oxidized Low Density Lipoprotein Serves as a Mediator for the Inverse Relationship between Serum D-Ribose and Cognitive Performance in Type 2 Diabetic Patients. Free Radic. Biol. Med. 2021, 171, 91–98. [Google Scholar] [CrossRef]
- Xu, K.; Wang, M.; Zhou, W.; Pu, J.; Wang, H.; Xie, P. Chronic D-Ribose and D-Mannose Overload Induce Depressive/Anxiety-like Behavior and Spatial Memory Impairment in Mice. Transl. Psychiatry 2021, 11, 90. [Google Scholar] [CrossRef]
- Wu, B.; Wei, Y.; Wang, Y.; Su, T.; Zhou, L.; Liu, Y.; He, R. Gavage of D-Ribose Induces Aβ-like Deposits, Tau Hyperphosphorylation as Well as Memory Loss and Anxiety-like Behavior in Mice. Oncotarget 2015, 6, 34128–34142. [Google Scholar] [CrossRef] [Green Version]
- Hong, J.; Li, G.; Zhang, Q.; Ritter, J.; Li, W.; Li, P.-L. D-Ribose Induces Podocyte NLRP3 Inflammasome Activation and Glomerular Injury via AGEs/RAGE Pathway. Front. Cell Dev. Biol. 2019, 7, 259. [Google Scholar] [CrossRef] [Green Version]
- Hong, J.; Wang, X.; Zhang, N.; Fu, H.; Li, W. D-Ribose Induces Nephropathy through RAGE-Dependent NF-ΚB Inflammation. Arch. Pharm. Res. 2018, 41, 838–847. [Google Scholar] [CrossRef] [Green Version]
- Zhang, N.; Zhao, S.; Hong, J.; Li, W.; Wang, X. Protective Effects of Kaempferol on D-Ribose-Induced Mesangial Cell Injury. Oxidative Med. Cell. Longev. 2019, 2019, 7564207. [Google Scholar] [CrossRef] [PubMed]
- Vashishth, D.; Gibson, G.J.; Khoury, J.I.; Schaffler, M.B.; Kimura, J.; Fyhrie, D.P. Influence of Nonenzymatic Glycation on Biomechanical Properties of Cortical Bone. Bone 2001, 28, 195–201. [Google Scholar] [CrossRef] [PubMed]
- Jia, S.; Gong, H.; Cen, H.; Shi, P.; Zhang, R.; Li, Z.; Bi, X. Influence of Non-Enzymatic Glycation on the Mechanical Properties of Cortical Bone. J. Mech. Behav. Biomed. Mater. 2021, 119, 104553. [Google Scholar] [CrossRef]
- Lee, J.M.; Veres, S.P. Advanced Glycation End-Product Cross-Linking Inhibits Biomechanical Plasticity and Characteristic Failure Morphology of Native Tendon. J. Appl. Physiol. 2019, 126, 832–841. [Google Scholar] [CrossRef]
- De Caro, L.; Terzi, A.; Fusaro, L.; Altamura, D.; Boccafoschi, F.; Bunk, O.; Giannini, C. Time Scale of Glycation in Collagen of Bovine Pericardium-Derived Bio-Tissues. IUCrJ 2021, 8, 1024–1034. [Google Scholar] [CrossRef]
- Kajimoto, Y.; Matsuoka, T.; Kaneto, H.; Watada, H.; Fujitani, Y.; Kishimoto, M.; Sakamoto, K.; Matsuhisa, M.; Kawamori, R.; Yamasaki, Y.; et al. Induction of Glycation Suppresses Glucokinase Gene Expression in HIT-T15 Cells. Diabetologia 1999, 42, 1417–1424. [Google Scholar] [CrossRef] [Green Version]
- Waris, S.; Pischetsrieder, M.; Saleemuddin, M. DNA Damage by Ribose: Inhibition at High Ribose Concentrations. Indian J. Biochem. Biophys. 2010, 47, 148–156. [Google Scholar]
- Akhter, F.; Salman Khan, M.; Shahab, U.; Moinuddin; Ahmad, S. Bio-Physical Characterization of Ribose Induced Glycation: A Mechanistic Study on DNA Perturbations. Int. J. Biol. Macromol. 2013, 58, 206–210. [Google Scholar] [CrossRef] [PubMed]
- Chandra, G.K.; Eklouh-Molinier, C.; Fere, M.; Angiboust, J.-F.; Gobinet, C.; Van-Gulick, L.; Jeannesson, P.; Piot, O. Probing in Vitro Ribose Induced DNA-Glycation Using Raman Microspectroscopy. Anal. Chem. 2015, 87, 2655–2664. [Google Scholar] [CrossRef]
- Dinda, A.K.; Tripathy, D.R.; Dasgupta, S. Glycation of Ribonuclease A Affects Its Enzymatic Activity and DNA Binding Ability. Biochimie 2015, 118, 162–172. [Google Scholar] [CrossRef]
- Su, T.; Xin, L.; He, Y.-G.; Wei, Y.; Song, Y.-X.; Li, W.-W.; Wang, X.-M.; He, R.-Q. The Abnormally High Level of Uric D-Ribose for Type-2 Diabetics. Acta Agron. Sin. 2013, 40, 816. [Google Scholar] [CrossRef]
- Siddiqui, Z.; Faisal, M.; Alatar, A.R.; Ahmad, S. Prevalence of Auto-Antibodies against D-Ribose-Glycated-Hemoglobin in Diabetes Mellitus. Glycobiology 2019, 29, 409–418. [Google Scholar] [CrossRef] [PubMed]
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Moschini, R.; Balestri, F.; Cappiello, M.; Signore, G.; Mura, U.; Del-Corso, A. Ribose Intake as Food Integrator: Is It a Really Convenient Practice? Biomolecules 2022, 12, 1775. https://doi.org/10.3390/biom12121775
Moschini R, Balestri F, Cappiello M, Signore G, Mura U, Del-Corso A. Ribose Intake as Food Integrator: Is It a Really Convenient Practice? Biomolecules. 2022; 12(12):1775. https://doi.org/10.3390/biom12121775
Chicago/Turabian StyleMoschini, Roberta, Francesco Balestri, Mario Cappiello, Giovanni Signore, Umberto Mura, and Antonella Del-Corso. 2022. "Ribose Intake as Food Integrator: Is It a Really Convenient Practice?" Biomolecules 12, no. 12: 1775. https://doi.org/10.3390/biom12121775
APA StyleMoschini, R., Balestri, F., Cappiello, M., Signore, G., Mura, U., & Del-Corso, A. (2022). Ribose Intake as Food Integrator: Is It a Really Convenient Practice? Biomolecules, 12(12), 1775. https://doi.org/10.3390/biom12121775