A Methodological Perspective on the Function and Assessment of Peripheral Chemoreceptors in Heart Failure: A Review of Data from Clinical Trials
Abstract
1. Introduction
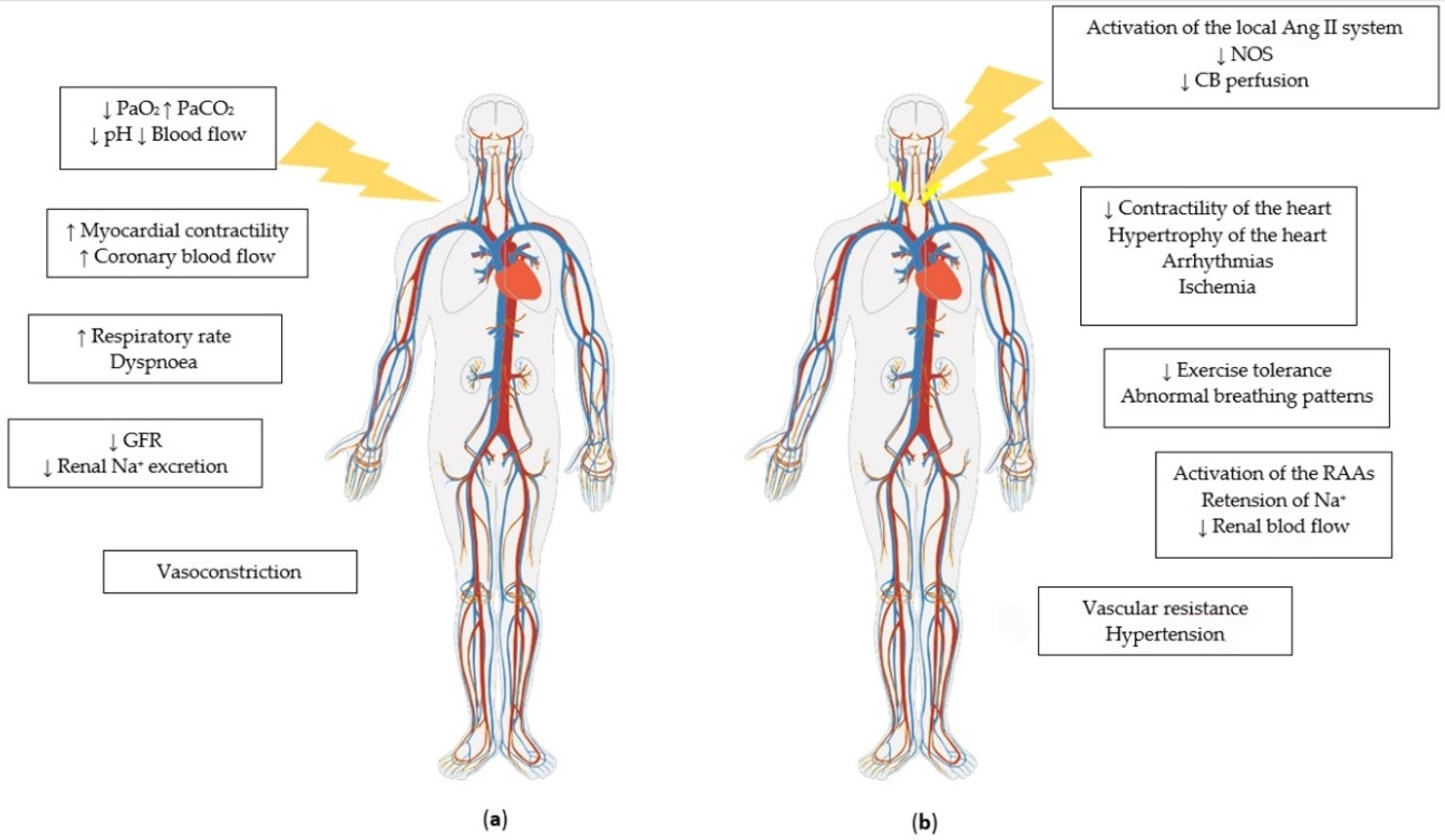
2. Physiology and Pathophysiology of Peripheral Chemoreceptors
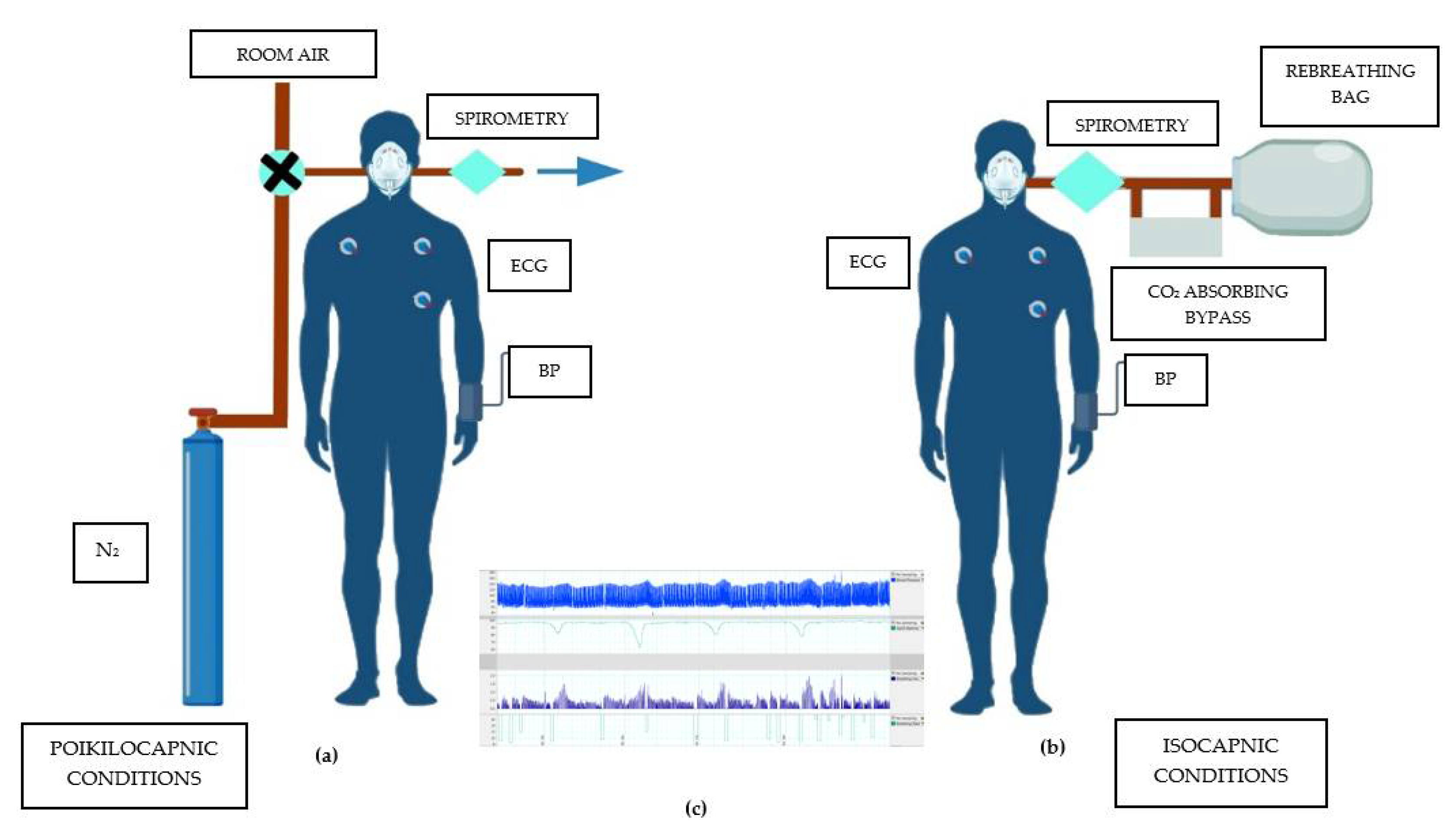
3. Methods of Assessment of PChR Phase Activity
4. Comparison of Studied Populations
5. The Impact of HF Etiology and Management on PChR Function
5.1. Digoxin
5.2. Angiotensin-Converting-Enzyme Inhibitors
5.3. Beta-Blockers
5.4. Mineralocorticoid Receptor Antagonists
5.5. Diuretics
5.6. Antiplatelet Drugs
5.7. Statins
5.8. Devices
5.9. Etiology
6. Methods of Assessment of PChR Tonic Activity
7. Predictors of Increased Chemosensitivity
8. Novel Therapies and Possibilities Research Gaps
9. Limitations
10. Conclusions—Future Directions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Lazovic, B.; Zlatkovic Svenda, M.; Durmic, T.; Stajic, Z.; Duric, V.; Zugic, V. The Regulation Role of Carotid Body Peripheral Chemoreceptors in Physiological and Pathophysiological Conditions. Med. Pregl. 2016, 69, 385–390. [Google Scholar] [CrossRef] [PubMed]
- Marshall, J.M. Peripheral Chemoreceptors and Cardiovascular Regulation. Physiol. Rev. 1994, 74, 543–594. [Google Scholar] [CrossRef] [PubMed]
- O’Regan, R.G.; Majcherczyk, S. Role of Peripheral Chemoreceptors and Central Chemosensitivity in the Regulation of Respiration and Circulation. J. Exp. Biol. 1982, 100, 23–40. [Google Scholar] [CrossRef] [PubMed]
- Iturriaga, R.; Alcayaga, J.; Chapleau, M.W.; Somers, V.K. Carotid Body Chemoreceptors: Physiology, Pathology, and Implications for Health and Disease. Physiol. Rev. 2021, 101, 1177–1235. [Google Scholar] [CrossRef]
- Kara, T.; Narkiewicz, K.; Somers, V.K. Chemoreflexes—Physiology and Clinical Implications. Acta Physiol. Scand. 2003, 177, 377–384. [Google Scholar] [CrossRef] [PubMed]
- Schmidt, H.; Francis, D.P.; Rauchhaus, M.; Werdan, K.; Piepoli, M.F. Chemo- and Ergoreflexes in Health, Disease and Ageing. Int. J. Cardiol. 2005, 98, 369–378. [Google Scholar] [CrossRef] [PubMed]
- Teppema, L.J.; Dahan, A. The Ventilatory Response to Hypoxia in Mammals: Mechanisms, Measurement, and Analysis. Physiol. Rev. 2010, 90, 675–754. [Google Scholar] [CrossRef]
- Nanduri, R. Prabhakar and Ying-Jie Peng Peripheral Chemoreceptors in Health and Disease. J. Appl. Physiol. 2004, 96, 1–2. [Google Scholar] [CrossRef]
- Paton, J.F.R.; Ratcliffe, L.; Hering, D.; Wolf, J.; Sobotka, P.A.; Narkiewicz, K. Revelations about Carotid Body Function through Its Pathological Role in Resistant Hypertension. Curr. Hypertens. Rep. 2013, 15, 273–280. [Google Scholar] [CrossRef]
- Paton, J.F.R.; Sobotka, P.A.; Fudim, M.; Engleman, Z.J.; Hart, E.C.J.; McBryde, F.D.; Abdala, A.P.; Marina, N.; Gourine, A.V.; Lobo, M.; et al. The Carotid Body as a Therapeutic Target for the Treatment of Sympathetically Mediated Diseases. Hypertension 2013, 61, 5–13. [Google Scholar] [CrossRef]
- Toledo, C.; Andrade, D.C.; Lucero, C.; Schultz, H.D.; Marcus, N.; Retamal, M.; Madrid, C.; Del Rio, R. Contribution of Peripheral and Central Chemoreceptors to Sympatho-Excitation in Heart Failure. J. Physiol. 2017, 595, 43–51. [Google Scholar] [CrossRef]
- Niewinski, P.; Janczak, D.; Rucinski, A.; Tubek, S.; Engelman, Z.J.; Piesiak, P.; Jazwiec, P.; Banasiak, W.; Fudim, M.; Sobotka, P.A.; et al. Carotid Body Resection for Sympathetic Modulation in Systolic Heart Failure: Results from First-in-Man Study. Eur. J. Heart Fail. 2017, 19, 391–400. [Google Scholar] [CrossRef] [PubMed]
- Siński, M.; Lewandowski, J.; Przybylski, J.; Bidiuk, J.; Abramczyk, P.; Ciarka, A.; Gaciong, Z. Tonic Activity of Carotid Body Chemoreceptors Contributes to the Increased Sympathetic Drive in Essential Hypertension. Hypertens. Res. 2012, 35, 487–491. [Google Scholar] [CrossRef] [PubMed]
- Schultz, H.D.; Li, Y.L.; Ding, Y. Arterial Chemoreceptors and Sympathetic Nerve Activity: Implications for Hypertension and Heart Failure. Hypertension 2007, 50, 6–13. [Google Scholar] [CrossRef]
- Narkiewicz, K.; van de Borne, P.J.; Montano, N.; Dyken, M.E.; Phillips, B.G.; Somers, V.K. Contribution of Tonic Chemoreflex Activation to Sympathetic Activity and Blood Pressure in Patients with Obstructive Sleep Apnea. Circulation 1998, 97, 943–945. [Google Scholar] [CrossRef] [PubMed]
- Narkiewicz, K.; van de Borne, P.J.; Pesek, C.A.; Dyken, M.E.; Montano, N.; Somers, V.K. Selective Potentiation of Peripheral Chemoreflex Sensitivity in Obstructive Sleep Apnea. Circulation 1999, 99, 1183–1189. [Google Scholar] [CrossRef]
- Mansukhani, M.P.; Wang, S.; Somers, V.K. Chemoreflex Physiology and Implications for Sleep Apnoea: Insights from Studies in Humans. Exp. Physiol. 2015, 100, 130–135. [Google Scholar] [CrossRef] [PubMed]
- Prabhakar, N.R. Carotid Body Chemoreflex: A Driver of Autonomic Abnormalities in Sleep Apnoea. Exp. Physiol. 2016, 101, 975–985. [Google Scholar] [CrossRef]
- Trombetta, I.C.; Maki-Nunes, C.; Toschi-Dias, E.; Alves, M.-J.N.N.; Rondon, M.U.P.B.; Cepeda, F.X.; Drager, L.F.; Braga, A.M.F.W.; Lorenzi-Filho, G.; Negrao, C.E. Obstructive Sleep Apnea Is Associated with Increased Chemoreflex Sensitivity in Patients with Metabolic Syndrome. Sleep 2013, 36, 41–49. [Google Scholar] [CrossRef]
- Conde, S.V.; Ribeiro, M.J.; Melo, B.F.; Guarino, M.P.; Sacramento, J.F. Insulin Resistance: A New Consequence of Altered Carotid Body Chemoreflex? J. Physiol. 2017, 595, 31–41. [Google Scholar] [CrossRef]
- Sokolska, J.M.; Sokolski, M.; Zymliński, R.; Biegus, J.; Siwołowski, P.; Nawrocka-Millward, S.; Jankowska, E.A.; Todd, J.; Banasiak, W.; Ponikowski, P. Patterns of Dyspnoea Onset in Patients with Acute Heart Failure: Clinical and Prognostic Implications. ESC Hear. Fail. 2019, 6, 16–26. [Google Scholar] [CrossRef]
- McDonagh, T.A.; Metra, M.; Adamo, M.; Gardner, R.S.; Baumbach, A.; Böhm, M.; Burri, H.; Butler, J.; Celutkiene, J.; Chioncel, O.; et al. 2021 ESC Guidelines for the Diagnosis and Treatment of Acute and Chronic Heart Failure. Eur. Heart J. 2021, 42, 3599–3726. [Google Scholar] [CrossRef]
- Chua, T.P.; Ponikowski, P.; Webb-Peploe, K.; Harrington, D.; Anker, S.D.; Piepoli, M.; Coats, A.J.S. Clinical Characteristics of Chronic Heart Failure Patients with an Augmented Peripheral Chemoreflex. Eur. Heart J. 1997, 18, 480–486. [Google Scholar] [CrossRef]
- Giannoni, A.; Emdin, M.; Poletti, R.; Bramanti, F.; Prontera, C.; Piepoli, M.; Passino, C. Clinical Significance of Chemosensitivity in Chronic Heart Failure: Influence on Neurohormonal Derangement, Cheyne-Stokes Respiration and Arrhythmias. Clin. Sci. 2008, 114, 489–497. [Google Scholar] [CrossRef]
- Ponikowski, P.; Chua, T.P.; Anker, S.D.; Francis, D.P.; Doehner, W.; Banasiak, W.; Poole-Wilson, P.A.; Piepoli, M.F.; Coats, A.J.S. Peripheral Chemoreceptor Hypersensitivity: An Ominous Sign in Patients with Chronic Heart Failure. Circulation 2001, 31, 544–549. [Google Scholar] [CrossRef]
- Cutler, M.J.; Swift, N.M.; Keller, D.M.; Wasmund, W.L.; Burk, J.R.; Smith, M.L. Periods of Intermittent Hypoxic Apnea Can Alter Chemoreflex Control of Sympathetic Nerve Activity in Humans. Am. J. Physiol.—Hear. Circ. Physiol. 2004, 287, 2054–2060. [Google Scholar] [CrossRef][Green Version]
- Edgell, H.; McMurtry, M.S.; Haykowsky, M.J.; Paterson, I.; Ezekowitz, J.A.; Dyck, J.R.B.; Stickland, M.K. Peripheral Chemoreceptor Control of Cardiovascular Function at Rest and during Exercise in Heart Failure Patients. J. Appl. Physiol. 2015, 118, 839–848. [Google Scholar] [CrossRef] [PubMed]
- van de Borne, P.; Oren, R.; Somers, V.K. Dopamine Depresses Minute Ventilation in Patients with Heart Failure. Circulation 1998, 98, 126–131. [Google Scholar] [CrossRef] [PubMed]
- Despas, F.; Lambert, E.; Vaccaro, A.; Labrunee, M.; Franchitto, N.; Lebrin, M.; Galinier, M.; Senard, J.M.; Lambert, G.; Esler, M.; et al. Peripheral Chemoreflex Activation Contributes to Sympathetic Baroreflex Impairment in Chronic Heart Failure. J. Hypertens. 2012, 30, 753–760. [Google Scholar] [CrossRef] [PubMed]
- Ponikowski, P.; Chua, T.P.; Piepoli, M.; Ondusova, D.; Webb-Peploe, K.; Harrington, D.; Anker, S.D.; Volterrani, M.; Colombo, R.; Mazzuero, G.; et al. Augmented Peripheral Chemosensitivity as a Potential Input to Baroreflex Impairment and Autonomic Imbalance in Chronic Heart Failure. Circulation 1997, 96, 2586–2594. [Google Scholar] [CrossRef] [PubMed]
- Niewinski, P.; Engelman, Z.J.; Fudim, M.; Tubek, S.; Paleczny, B.; Jankowska, E.A.; Banasiak, W.; Sobotka, P.A.; Ponikowski, P. Clinical Predictors and Hemodynamic Consequences of Elevated Peripheral Chemosensitivity in Optimally Treated Men with Chronic Systolic Heart Failure. J. Card. Fail. 2013, 19, 408–415. [Google Scholar] [CrossRef]
- Chua, T.P.; Clark, A.L.; Amadi, A.A.; Coats, A.J.S. Relation between Chemosensitivity and the Ventilatory Response to Exercise in Chronic Heart Failure. J. Am. Coll. Cardiol. 1996, 27, 650–657. [Google Scholar] [CrossRef]
- Chua, T.P.; Ponikowski, P.P.; Harrington, D.; Chambers, J.; Coats, A.J.S. Contribution of Peripheral Chemoreceptors to Ventilation and the Effects of Their Suppression on Exercise Tolerance in Chronic Heart Failure. Heart 1996, 76, 483–489. [Google Scholar] [CrossRef]
- Ponikowski, P.; Anker, S.D.; Chua, T.P.; Francis, D.; Banasiak, W.; Poole-Wilson, P.A.; Coats, A.J.S.; Piepoli, M. Oscillatory Breathing Patterns during Wakefulness in Patients with Chronic Heart Failure Clinical Implications and Role of Augmented Peripheral Chemosensitivity. Circulation 1999, 14, 2418–2424. [Google Scholar] [CrossRef]
- Giannoni, A.; Emdin, M.; Bramanti, F.; Iudice, G.; Francis, D.P.; Barsotti, A.; Piepoli, M.; Passino, C. Combined Increased Chemosensitivity to Hypoxia and Hypercapnia as a Prognosticator in Heart Failure. J. Am. Coll. Cardiol. 2009, 53, 1975–1980. [Google Scholar] [CrossRef]
- Giannoni, A.; Gentile, F.; Buoncristiani, F.; Borrelli, C.; Sciarrone, P.; Spiesshoefer, J.; Bramanti, F.; Iudice, G.; Javaheri, S.; Emdin, M.; et al. Chemoreflex and Baroreflex Sensitivity Hold a Strong Prognostic Value in Chronic Heart Failure. JACC Hear. Fail. 2022, 10, 662–676. [Google Scholar] [CrossRef] [PubMed]
- Niewinski, P. Carotid Body Modulation in Systolic Heart Failure from the Clinical Perspective. J. Physiol. 2017, 595, 53–61. [Google Scholar] [CrossRef]
- Keir, D.A.; Duffin, J.; Floras, J.S. Measuring Peripheral Chemoreflex Hypersensitivity in Heart Failure. Front. Physiol. 2020, 11, 595486. [Google Scholar] [CrossRef]
- Niewinski, P. Pathophysiology and Potential Clinical Applications for Testing of Peripheral Chemosensitivity in Heart Failure. Curr. Heart Fail. Rep. 2014, 11, 126–133. [Google Scholar] [CrossRef] [PubMed]
- Langner-Hetmańczuk, A.; Tubek, S.; Niewiński, P.; Ponikowski, P. The Role of Pharmacological Treatment in the Chemoreflex Modulation. Front. Physiol. 2022, 13, 912616. [Google Scholar] [CrossRef] [PubMed]
- Andrade, D.C.; Lucero, C.; Toledo, C.; Madrid, C.; Marcus, N.J.; Schultz, H.D.; Del Rio, R. Relevance of the Carotid Body Chemoreflex in the Progression of Heart Failure. Biomed Res. Int. 2015, 2015. [Google Scholar] [CrossRef] [PubMed]
- Nattie, E. Why Do We Have Both Peripheral and Central Chemoreceptors? J. Appl. Physiol. 2006, 100, 9–10. [Google Scholar] [CrossRef]
- Kumar, P.; Prabhakar, N.R. Peripheral Chemoreceptors: Function and Plasticity of the Carotid Body. Compr. Physiol. 2012, 2, 141–219. [Google Scholar] [CrossRef] [PubMed]
- Grassi, G.; Seravalle, G.; Cattaneo, B.M.; Lanfranchi, A.; Vailati, S.; Giannattasio, C.; Del Bo, A.; Sala, C.; Bolla, G.B.; Pozzi, M. Sympathetic Activation and Loss of Reflex Sympathetic Control in Mild Congestive Heart Failure. Circulation 1995, 92, 3206–3211. [Google Scholar] [CrossRef]
- Tubek, S.; Niewinski, P.; Reczuch, K.; Janczak, D.; Rucinski, A.; Paleczny, B.; Engelman, Z.J.; Banasiak, W.; Paton, J.F.R.; Ponikowski, P. Effects of Selective Carotid Body Stimulation with Adenosine in Conscious Humans. J. Physiol. 2016, 594, 6225–6240. [Google Scholar] [CrossRef] [PubMed]
- De Burgh Daly, M.; Scott, M.J. An Analysis of the Primary Cardiovascular Reflex Effects of Stimulation of the Carotid Body Chemoreceptors in the Dog. J. Physiol. 1962, 162, 555–573. [Google Scholar] [CrossRef]
- Daly, M.D.; Scott, M.J. The Cardiovascular Responses to Stimulation of the Carotid Body Chemoreceptors in the Dog. J. Physiol. 1963, 165, 179–197. [Google Scholar] [CrossRef]
- Paleczny, B.; Seredyński, R.; Tubek, S.; Adamiec, D.; Ponikowski, P.; Ponikowska, B. Hypoxic Tachycardia Is Not a Result of Increased Respiratory Activity in Healthy Subjects. Exp. Physiol. 2019, 104, 476–489. [Google Scholar] [CrossRef]
- Simon, P.M.; Taha, B.H.; Dempsey, J.A.; Skatrud, J.B.; Iber, C. Role of Vagal Feedback from the Lung in Hypoxic-Induced Tachycardia in Humans. J. Appl. Physiol. 1995, 78, 1522–1530. [Google Scholar] [CrossRef]
- Morgan-Hughes, N.J.; Corris, P.A.; Healey, M.D.; Dark, J.H.; McComb, J.M. Cardiovascular and Respiratory Effects of Adenosine in Humans after Pulmonary Denervation. J. Appl. Physiol. 1994, 76, 756–759. [Google Scholar] [CrossRef]
- Eckberg, D.L.; Bastow, H., 3rd; Scruby, A.E. Modulation of Human Sinus Node Function by Systemic Hypoxia. J. Appl. Physiol. 1982, 52, 570–577. [Google Scholar] [CrossRef]
- Karim, F.; Hainsworth, R.; Sofola, O.A.; Wood, L.M. Responses of the Heart to Stimulation of Aortic Body Chemoreceptors in Dogs. Circ. Res. 1980, 46, 77–83. [Google Scholar] [CrossRef]
- Niewinski, P.; Janczak, D.; Rucinski, A.; Tubek, S.; Engelman, Z.J.; Jazwiec, P.; Banasiak, W.; Sobotka, P.A.; Hart, E.C.J.; Paton, J.F.R.; et al. Dissociation between Blood Pressure and Heart Rate Response to Hypoxia after Bilateral Carotid Body Removal in Men with Systolic Heart Failure. Exp. Physiol. 2014, 99, 552–561. [Google Scholar] [CrossRef]
- Watson, A.M.D.; Hood, S.G.; May, C.N. Mechanisms of Sympathetic Activation in Heart Failure. Clin. Exp. Pharmacol. Physiol. 2006, 33, 1269–1274. [Google Scholar] [CrossRef]
- Reiken, S.; Gaburjakova, M.; Gaburjakova, J.; He Kl, K.L.; Prieto, A.; Becker, E.; Yi Gh, G.H.; Wang, J.; Burkhoff, D.; Marks, A.R. Beta-Adrenergic Receptor Blockers Restore Cardiac Calcium Release Channel (Ryanodine Receptor) Structure and Function in Heart Failure. Circulation 2001, 104, 2843–2848. [Google Scholar] [CrossRef]
- Lehnart, S.E.; Wehrens, X.H.T.; Marks, A.R. Calstabin Deficiency, Ryanodine Receptors, and Sudden Cardiac Death. Biochem. Biophys. Res. Commun. 2004, 322, 1267–1279. [Google Scholar] [CrossRef]
- Li, Y.-L.; Schultz, H.D. Enhanced Sensitivity of Kv Channels to Hypoxia in the Rabbit Carotid Body in Heart Failure: Role of Angiotensin II. J. Physiol. 2006, 575, 215–227. [Google Scholar] [CrossRef]
- Schultz, H.D.; Marcus, N.J.; Del Rio, R. Role of the Carotid Body in the Pathophysiology of Heart Failure. Curr. Hypertens. Rep. 2013, 15, 356–362. [Google Scholar] [CrossRef] [PubMed]
- Li, Y.-L.; Zheng, H.; Ding, Y.; Schultz, H.D. Expression of Neuronal Nitric Oxide Synthase in Rabbit Carotid Body Glomus Cells Regulates Large-Conductance Ca2+-Activated Potassium Currents. J. Neurophysiol. 2010, 103, 3027–3033. [Google Scholar] [CrossRef] [PubMed]
- Li, Y.-L.; Sun, S.-Y.; Overholt, J.L.; Prabhakar, N.R.; Rozanski, G.J.; Zucker, I.H.; Schultz, H.D. Attenuated Outward Potassium Currents in Carotid Body Glomus Cells of Heart Failure Rabbit: Involvement of Nitric Oxide. J. Physiol. 2004, 555, 219–229. [Google Scholar] [CrossRef] [PubMed]
- Ding, Y.; Li, Y.-L.; Schultz, H.D. Role of Blood Flow in Carotid Body Chemoreflex Function in Heart Failure. J. Physiol. 2011, 589, 245–258. [Google Scholar] [CrossRef]
- Brognara, F.; Felippe, I.S.A.; Salgado, H.C.; Paton, J.F.R. Autonomic Innervation of the Carotid Body as a Determinant of Its Sensitivity: Implications for Cardiovascular Physiology and Pathology. Cardiovasc. Res. 2021, 117, 1015–1032. [Google Scholar] [CrossRef] [PubMed]
- Felippe, I.S.A.; Zera, T.; da Silva, M.P.; Moraes, D.J.A.; McBryde, F.; Paton, J.F.R. The Sympathetic Nervous System Exacerbates Carotid Body Sensitivity in Hypertension. Cardiovasc. Res. 2022. [Google Scholar] [CrossRef]
- McBryde, F.D.; Abdala, A.P.; Hendy, E.B.; Pijacka, W.; Marvar, P.; Moraes, D.J.A.; Sobotka, P.A.; Paton, J.F.R. The Carotid Body as a Putative Therapeutic Target for the Treatment of Neurogenic Hypertension. Nat. Commun. 2013, 4, 2395. [Google Scholar] [CrossRef] [PubMed]
- Abdala, A.P.; McBryde, F.D.; Marina, N.; Hendy, E.B.; Engelman, Z.J.; Fudim, M.; Sobotka, P.A.; Gourine, A.V.; Paton, J.F.R. Hypertension Is Critically Dependent on the Carotid Body Input in the Spontaneously Hypertensive Rat. J. Physiol. 2012, 590, 4269–4277. [Google Scholar] [CrossRef] [PubMed]
- Despas, F.; Detis, N.; Dumonteil, N.; Labrunee, M.; Bellon, B.; Franchitto, N.; Galinier, M.; Senard, J.-M.; Pathak, A. Excessive Sympathetic Activation in Heart Failure with Chronic Renal Failure: Role of Chemoreflex Activation. J. Hypertens. 2009, 27, 1849–1854. [Google Scholar] [CrossRef]
- Ponikowski, P.; Chua, T.P.; Piepoli, M.; Amadi, A.A.; Harrington, D.; Webb-Peploe, K.; Volterrani, M.; Colombo, R.; Mazzuero, G.; Giordano, A.; et al. Chemoreceptor Dependence of Very Low Frequency Rhythms in Advanced Chronic Heart Failure. Am. J. Physiol.—Hear. Circ. Physiol. 1997, 272, 438–447. [Google Scholar] [CrossRef]
- Chua, T.P.; Harrington, D.; Ponikowski, P.; Webb-Peploe, K.; Poole-Wilson, P.A.; Coats, A.J.S. Effects of Dihydrocodeine on Chemosensitivity and Exercise Tolerance in Patients with Chronic Heart Failure. J. Am. Coll. Cardiol. 1997, 29, 147–152. [Google Scholar] [CrossRef]
- Ponikowski, P.; Piepoli, M.; Chua, T.P.; Banasiak, W.; Francis, D.; Anker, S.D.; Coats, A.J.S. The Impact of Cachexia on Cardiorespiratory Reflex Control in Chronic Heart Failure. Eur. Heart J. 1999, 20, 1667–1675. [Google Scholar] [CrossRef]
- Ponikowski, P.P.; Chua, T.P.; Francis, D.P.; Capucci, A.; Coats, A.J.S.; Piepoli, M.F. Muscle Ergoreceptor Overactivity Reflects Deterioration in Clinical Status and Cardiorespiratory Reflex Control in Chronic Heart Failure. Circulation 2001, 104, 2324–2330. [Google Scholar] [CrossRef]
- Mirizzi, G.; Giannoni, A.; Ripoli, A.; Iudice, G.; Bramanti, F.; Emdin, M.; Passino, C. Prediction of the Chemoreflex Gain by Common Clinical Variables in Heart Failure. PLoS ONE 2016, 11, e0153510. [Google Scholar] [CrossRef]
- Tubek, S.; Niewinski, P.; Paleczny, B.; Langner-Hetmanczuk, A.; Banasiak, W.; Ponikowski, P. Acute Hyperoxia Reveals Tonic Influence of Peripheral Chemoreceptors on Systemic Vascular Resistance in Heart Failure Patients. Sci. Rep. 2021, 11, 20823. [Google Scholar] [CrossRef]
- Collins, S.; Phillips, D.B.; McMurtry, M.S.; Bryan, T.L.; Paterson, D.I.; Wong, E.; Ezekowitz, J.A.; Forhan, M.A.; Stickland, M.K. The Effect of Carotid Chemoreceptor Inhibition on Exercise Tolerance in Chronic Heart Failure. Front. Physiol. 2020, 11, 195. [Google Scholar] [CrossRef]
- Hennersdorf, M.G.; Hillebrand, S.; Perings, C.; Strauer, B.E. Chemoreflexsensitivity in Chronic Heart Failure Patients. Eur. J. Heart Fail. 2001, 3, 679–684. [Google Scholar] [CrossRef] [PubMed]
- Franchitto, N.; Despas, F.; Labrunée, M.; Roncalli, J.; Boveda, S.; Galinier, M.; Senard, J.M.; Pathak, A. Tonic Chemoreflex Activation Contributes to Increased Sympathetic Nerve Activity in Heart Failure-Related Anemia. Hypertension 2010, 55, 1012–1017. [Google Scholar] [CrossRef] [PubMed]
- Rebuck, A.S.; Campbell, E.J. A Clinical Method for Assessing the Ventilatory Response to Hypoxia. Am. Rev. Respir. Dis. 1974, 109, 345–350. [Google Scholar] [CrossRef]
- Guyenet, P.G.; Bayliss, D.A.; Stornetta, R.L.; Kanbar, R.; Shi, Y.; Holloway, B.B.; Souza, G.M.P.R.; Basting, T.M.; Abbott, S.B.G.; Wenker, I.C. Interdependent Feedback Regulation of Breathing by the Carotid Bodies and the Retrotrapezoid Nucleus. J. Physiol. 2018, 596, 3029–3042. [Google Scholar] [CrossRef] [PubMed]
- Keir, D.A.; Duffin, J.; Millar, P.J.; Floras, J.S. Simultaneous Assessment of Central and Peripheral Chemoreflex Regulation of Muscle Sympathetic Nerve Activity and Ventilation in Healthy Young Men. J. Physiol. 2019, 597, 3281–3296. [Google Scholar] [CrossRef] [PubMed]
- Prasad, B.; Morgan, B.J.; Gupta, A.; Pegelow, D.F.; Teodorescu, M.; Dopp, J.M.; Dempsey, J.A. The Need for Specificity in Quantifying Neurocirculatory vs. Respiratory Effects of Eucapnic Hypoxia and Transient Hyperoxia. J. Physiol. 2020, 598, 4803–4819. [Google Scholar] [CrossRef]
- Gheorghiade, M.; Ferguson, D. Digoxin. A Neurohormonal Modulator in Heart Failure? Circulation 1991, 84, 2181–2186. [Google Scholar] [CrossRef]
- Janssen, C.; Lheureux, O.; Beloka, S.; Deboeck, G.; Adamopoulos, D.; Naeije, R.; van de Borne, P. Digoxin Increases Peripheral Chemosensitivity and the Ventilatory Response to Exercise in Normal Subjects. Clin. Exp. Pharmacol. Physiol. 2010, 37, 303–308. [Google Scholar] [CrossRef]
- Schobel, H.P.; Ferguson, D.W.; Clary, M.P.; Somers, V.K. Differential Effects of Digitalis on Chemoreflex Responses in Humans. Hypertension 1994, 23, 302–307. [Google Scholar] [CrossRef]
- Paganelli, F.; Maixent, J.M.; Gélisse, R.; Barnay, P.; Dodero, F.; Francheschi, F.; Lévy, S.; Saadjian, A. Effects of Digoxin on Chemoreflex in Patients with Chronic Heart Failure. Cell. Mol. Biol. 2001, 47, 335–340. [Google Scholar]
- Li, Y.-L.; Gao, L.; Zucker, I.H.; Schultz, H.D. NADPH Oxidase-Derived Superoxide Anion Mediates Angiotensin II-Enhanced Carotid Body Chemoreceptor Sensitivity in Heart Failure Rabbits. Cardiovasc. Res. 2007, 75, 546–554. [Google Scholar] [CrossRef][Green Version]
- Li, Y.-L.; Xia, X.-H.; Zheng, H.; Gao, L.; Li, Y.-F.; Liu, D.; Patel, K.P.; Wang, W.; Schultz, H.D. Angiotensin II Enhances Carotid Body Chemoreflex Control of Sympathetic Outflow in Chronic Heart Failure Rabbits. Cardiovasc. Res. 2006, 71, 129–138. [Google Scholar] [CrossRef]
- Allen, A.M. Angiotensin AT1 Receptor-Mediated Excitation of Rat Carotid Body Chemoreceptor Afferent Activity. J. Physiol. 1998, 510 Pt 3, 773–781. [Google Scholar] [CrossRef]
- Brown, C.V.; Boulet, L.M.; Vermeulen, T.D.; Sands, S.A.; Wilson, R.J.A.; Ayas, N.T.; Floras, J.S.; Foster, G.E. Angiotensin II-Type I Receptor Antagonism Does Not Influence the Chemoreceptor Reflex or Hypoxia-Induced Central Sleep Apnea in Men. Front. Neurosci. 2020, 14, 382. [Google Scholar] [CrossRef] [PubMed]
- Chua, T.P.; Coats, A.J.S. The Reproducibility and Comparability of Tests of the Peripheral Chemoreflex: Comparing the Transient Hypoxic Ventilatory Drive Test and the Single-breath Carbon Dioxide Response Test in Healthy Subjects. Eur. J. Clin. Investig. 1995, 25, 887–892. [Google Scholar] [CrossRef]
- Agostoni, P.; Contini, M.; Magini, A.; Apostolo, A.; Cattadori, G.; Bussotti, M.; Veglia, F.; Andreini, D.; Palermo, P. Carvedilol Reduces Exercise-Induced Hyperventilation: A Benefit in Normoxia and a Problem with Hypoxia. Eur. J. Heart Fail. 2006, 8, 729–735. [Google Scholar] [CrossRef] [PubMed]
- Contini, M.; Apostolo, A.; Cattadori, G.; Paolillo, S.; Iorio, A.; Bertella, E.; Salvioni, E.; Alimento, M.; Farina, S.; Palermo, P.; et al. Multiparametric Comparison of CARvedilol, vs. NEbivolol, vs. BIsoprolol in Moderate Heart Failure: The CARNEBI Trial. Int. J. Cardiol. 2013, 168, 2134–2140. [Google Scholar] [CrossRef] [PubMed]
- Alzahrani, A.A.; Cao, L.L.; Aldossary, H.S.; Nathanael, D.; Fu, J.; Ray, C.J.; Brain, K.L.; Kumar, P.; Coney, A.M.; Holmes, A.P. β-Adrenoceptor Blockade Prevents Carotid Body Hyperactivity and Elevated Vascular Sympathetic Nerve Density Induced by Chronic Intermittent Hypoxia. Pflugers Arch. Eur. J. Physiol. 2021, 473, 37–51. [Google Scholar] [CrossRef]
- Prabhakar, N.R.; Kumar, G.K.; Chang, C.H.; Agani, F.H.; Haxhiu, M.A. Nitric Oxide in the Sensory Function of the Carotid Body. Brain Res. 1993, 625, 16–22. [Google Scholar] [CrossRef]
- Wang, Z.Z.; Bredt, D.S.; Fidone, S.J.; Stensaas, L.J. Neurons Synthesizing Nitric Oxide Innervate the Mammalian Carotid Body. J. Comp. Neurol. 1993, 336, 419–432. [Google Scholar] [CrossRef]
- Ding, Y.; Li, Y.L.; Schultz, H.D. Downregulation of Carbon Monoxide as Well as Nitric Oxide Contributes to Peripheral Chemoreflex Hypersensitivity in Heart Failure Rabbits. J. Appl. Physiol. 2008, 105, 14–23. [Google Scholar] [CrossRef][Green Version]
- Airaksinen, K.E.; Niemelä, M.J.; Huikuri, H.V. Effect of Beta-Blockade on Baroreflex Sensitivity and Cardiovascular Autonomic Function Tests in Patients with Coronary Artery Disease. Eur. Heart J. 1994, 15, 1482–1485. [Google Scholar] [CrossRef]
- Floras, J.S.; Jones, J.V.; Hassan, M.O.; Sleight, P. Effects of Acute and Chronic Beta-Adrenoceptor Blockade on Baroreflex Sensitivity in Humans. J. Auton. Nerv. Syst. 1988, 25, 87–94. [Google Scholar] [CrossRef] [PubMed]
- La Rovere, M.T.; Pinna, G.D.; Maestri, R.; Robbi, E.; Caporotondi, A.; Guazzotti, G.; Sleight, P.; Febo, O. Prognostic Implications of Baroreflex Sensitivity in Heart Failure Patients in the Beta-Blocking Era. J. Am. Coll. Cardiol. 2009, 53, 193–199. [Google Scholar] [CrossRef]
- Yee, K.M.; Struthers, A.D. Aldosterone Blunts the Baroreflex Response in Man. Clin. Sci. 1998, 95, 687–692. [Google Scholar] [CrossRef] [PubMed]
- Fletcher, J.; Buch, A.N.; Routledge, H.C.; Chowdhary, S.; Coote, J.H.; Townend, J.N. Acute Aldosterone Antagonism Improves Cardiac Vagal Control in Humans. J. Am. Coll. Cardiol. 2004, 43, 1270–1275. [Google Scholar] [CrossRef]
- Wray, D.W.; Supiano, M.A. Impact of Aldosterone Receptor Blockade Compared with Thiazide Therapy on Sympathetic Nervous System Function in Geriatric Hypertension. Hypertension 2010, 55, 1217–1223. [Google Scholar] [CrossRef] [PubMed]
- Cattaneo, M.; Faioni, E.M. Why Does Ticagrelor Induce Dyspnea? Thromb. Haemost. 2012, 108, 1031–1036. [Google Scholar] [CrossRef]
- McQueen, D.S.; Ribeiro, J.A. Effects of Ouabain on Carotid Body Chemoreceptor Activity in the Cat. J. Physiol. 1983, 335, 221–235. [Google Scholar] [CrossRef]
- Giannoni, A.; Borrelli, C.; Gentile, F.; Mirizzi, G.; Coceani, M.; Paradossi, U.; Vergaro, G.; Bramanti, F.; Iudice, G.; Emdin, M.; et al. Central Apnoeas and Ticagrelor-Related Dyspnoea in Patients with Acute Coronary Syndrome. Eur. Hear. journal. Cardiovasc. Pharmacother. 2021, 7, 180–188. [Google Scholar] [CrossRef]
- Dekker, R.J.; van Thienen, J.V.; Rohlena, J.; de Jager, S.C.; Elderkamp, Y.W.; Seppen, J.; de Vries, C.J.M.; Biessen, E.A.L.; van Berkel, T.J.C.; Pannekoek, H.; et al. Endothelial KLF2 Links Local Arterial Shear Stress Levels to the Expression of Vascular Tone-Regulating Genes. Am. J. Pathol. 2005, 167, 609–618. [Google Scholar] [CrossRef]
- Haack, K.K.V.; Marcus, N.J.; Del Rio, R.; Zucker, I.H.; Schultz, H.D. Simvastatin Treatment Attenuates Increased Respiratory Variability and Apnea/Hypopnea Index in Rats with Chronic Heart Failure. Hypertension 2014, 63, 1041–1049. [Google Scholar] [CrossRef] [PubMed]
- Marcus, N.J.; Del Rio, R.; Ding, Y.; Schultz, H.D. KLF2 Mediates Enhanced Chemoreflex Sensitivity, Disordered Breathing and Autonomic Dysregulation in Heart Failure. J. Physiol. 2018, 596, 3171–3185. [Google Scholar] [CrossRef]
- Sen-Banerjee, S.; Mir, S.; Lin, Z.; Hamik, A.; Atkins, G.B.; Das, H.; Banerjee, P.; Kumar, A.; Jain, M.K. Kruppel-like Factor 2 as a Novel Mediator of Statin Effects in Endothelial Cells. Circulation 2005, 112, 720–726. [Google Scholar] [CrossRef] [PubMed]
- Laufs, U.; Liao, J.K. Post-Transcriptional Regulation of Endothelial Nitric Oxide Synthase MRNA Stability by Rho GTPase. J. Biol. Chem. 1998, 273, 24266–24271. [Google Scholar] [CrossRef]
- Laufs, U.; La Fata, V.; Plutzky, J.; Liao, J.K. Upregulation of Endothelial Nitric Oxide Synthase by HMG CoA Reductase Inhibitors. Circulation 1998, 97, 1129–1135. [Google Scholar] [CrossRef]
- Najem, B.; Unger, P.; Preumont, N.; Jansens, J.L.; Houssière, A.; Pathak, A.; Xhaet, O.; Gabriel, L.; Friart, A.; De Roy, L.; et al. Sympathetic Control after Cardiac Resynchronization Therapy: Responders versus Nonresponders. Am. J. Physiol.—Hear. Circ. Physiol. 2006, 291, H2647–H2652. [Google Scholar] [CrossRef]
- Gademan, M.G.J.; Van Bommel, R.J.; Ypenburg, C.; Haest, J.C.W.; Schalij, M.J.; Van Der Wall, E.E.; Bax, J.J.; Swenne, C.A. Biventricular Pacing in Chronic Heart Failure Acutely Facilitates the Arterial Baroreflex. Am. J. Physiol.—Hear. Circ. Physiol. 2008, 295, 755–760. [Google Scholar] [CrossRef][Green Version]
- Notarius, C.F.; Spaak, J.; Morris, B.L.; Floras, J.S. Comparison of Muscle Sympathetic Activity in Ischemic and Nonischemic Heart Failure. J. Card. Fail. 2007, 13, 470–475. [Google Scholar] [CrossRef] [PubMed]
- Deng, M.C.; Brisse, B.; Erren, M.; Khurana, C.; Breithardt, G.; Scheld, H.H. Ischemic versus Idiopathic Cardiomyopathy: Differing Neurohumoral Profiles despite Comparable Peak Oxygen Uptake. Int. J. Cardiol. 1997, 61, 261–268. [Google Scholar] [CrossRef]
- Minisi, A.J.; Thames, M.D. Distribution of Left Ventricular Sympathetic Afferents Demonstrated by Reflex Responses to Transmural Myocardial Ischemia and to Intracoronary and Epicardial Bradykinin. Circulation 1993, 87, 240–246. [Google Scholar] [CrossRef] [PubMed]
- Malliani, A.; Montano, N. Sympathetic Overactivity in Ischaemic Heart Disease. Clin. Sci. 2004, 106, 567–568. [Google Scholar] [CrossRef]
- Zipes, D.P. Influence of Myocardial Ischemia and Infarction on Autonomic Innervation of Heart. Circulation 1990, 82, 1095–1105. [Google Scholar] [CrossRef]
- Pardridge, W.M. The Blood-Brain Barrier: Bottleneck in Brain Drug Development. NeuroRx 2005, 2, 3–14. [Google Scholar] [CrossRef] [PubMed]
- Welsh, M.J.; Heistad, D.D.; Abboud, F.M. Depression of Ventilation by Dopamine in Man. Evidence for an Effect on the Chemoreceptor Reflex. J. Clin. Investig. 1978, 61, 708–713. [Google Scholar] [CrossRef]
- Smit, B.; Smulders, Y.M.; van der Wouden, J.C.; Oudemans-van Straaten, H.M.; Spoelstra-de Man, A.M.E. Hemodynamic Effects of Acute Hyperoxia: Systematic Review and Meta-Analysis. Crit. Care 2018, 22, 45. [Google Scholar] [CrossRef]
- Cornet, A.D.; Kooter, A.J.; Peters, M.J.L.; Smulders, Y.M. The Potential Harm of Oxygen Therapy in Medical Emergencies. Crit. Care 2013, 17, 313. [Google Scholar] [CrossRef]
- Mouren, S.; Souktani, R.; Beaussier, M.; Abdenour, L.; Arthaud, M.; Duvelleroy, M.; Vicaut, E. Mechanisms of Coronary Vasoconstriction Induced by High Arterial Oxygen Tension. Am. J. Physiol. 1997, 272, H67–H75. [Google Scholar] [CrossRef]
- McNulty, P.H.; King, N.; Scott, S.; Hartman, G.; McCann, J.; Kozak, M.; Chambers, C.E.; Demers, L.M.; Sinoway, L.I. Effects of Supplemental Oxygen Administration on Coronary Blood Flow in Patients Undergoing Cardiac Catheterization. Am. J. Physiol. Heart Circ. Physiol. 2005, 288, H1057–H1062. [Google Scholar] [CrossRef]
- Messina, E.J.; Sun, D.; Koller, A.; Wolin, M.S.; Kaley, G. Increases in Oxygen Tension Evoke Arteriolar Constriction by Inhibiting Endothelial Prostaglandin Synthesis. Microvasc. Res. 1994, 48, 151–160. [Google Scholar] [CrossRef] [PubMed]
- Niewinski, P.; Tubek, S.; Banasiak, W.; Paton, J.F.R.; Ponikowski, P. Consequences of Peripheral Chemoreflex Inhibition with Low-Dose Dopamine in Humans. J. Physiol. 2014, 592, 1295–1308. [Google Scholar] [CrossRef] [PubMed]
- Polakowski, J.S.; Segreti, J.A.; Cox, B.F.; Hsieh, G.C.; Kolasa, T.; Moreland, R.B.; Brioni, J.D. Effects of Selective Dopamine Receptor Subtype Agonists on Cardiac Contractility and Regional Haemodynamics in Rats. Clin. Exp. Pharmacol. Physiol. 2004, 31, 837–841. [Google Scholar] [CrossRef]
- Armando, I.; Villar, V.A.M.; Jose, P.A. Dopamine and Renal Function and Blood Pressure Regulation. Compr. Physiol. 2011, 1, 1075–1117. [Google Scholar] [CrossRef]
- Endoh, M. Effects of Dopamine on Sinus Rate and Ventricular Contractile Force of the Dog Heart In Vitro and In Vivo. Br. J. Pharmacol. 1975, 55, 475–486. [Google Scholar] [CrossRef] [PubMed]
- Limberg, J.K.; Johnson, B.D.; Holbein, W.W.; Ranadive, S.M.; Mozer, M.T.; Joyner, M.J. Interindividual Variability in the Dose-Specific Effect of Dopamine on Carotid Chemoreceptor Sensitivity to Hypoxia. J. Appl. Physiol. 2016, 120, 138–147. [Google Scholar] [CrossRef] [PubMed]
- Hennersdorf, M.G.; Perings, C.; Niebch, V.; Hillebrand, S.; Vester, E.G.; Strauer, B.E. Chemoreflexsensitivity in Patients with Survived Sudden Cardiac Arrest and Prior Myocardial Infarction. PACE—Pacing Clin. Electrophysiol. 2000, 23, 457–462. [Google Scholar] [CrossRef]
- Anderson, E.A.; Sinkey, C.A.; Lawton, W.J.; Mark, A.L. Elevated Sympathetic Nerve Activity in Borderline Hypertensive Humans. Evidence from Direct Intraneural Recordings. Hypertens. 1989, 14, 177–183. [Google Scholar] [CrossRef]
- Grassi, G. Counteracting the Sympathetic Nervous System in Essential Hypertension. Curr. Opin. Nephrol. Hypertens. 2004, 13, 513–519. [Google Scholar] [CrossRef]
- Smith, P.A.; Graham, L.N.; Mackintosh, A.F.; Stoker, J.B.; Mary, D.A.S.G. Relationship between Central Sympathetic Activity and Stages of Human Hypertension. Am. J. Hypertens. 2004, 17, 217–222. [Google Scholar] [CrossRef]
- Brunner-La Rocca, H.P.; Esler, M.D.; Jennings, G.L.; Kaye, D.M. Effect of Cardiac Sympathetic Nervous Activity on Mode of Death in Congestive Heart Failure. Eur. Heart J. 2001, 22, 1136–1143. [Google Scholar] [CrossRef]
- Hasking, G.J.; Esler, M.D.; Jennings, G.L.; Burton, D.; Johns, J.A.; Korner, P.I. Norepinephrine Spillover to Plasma in Patients with Congestive Heart Failure: Evidence of Increased Overall and Cardiorenal Sympathetic Nervous Activity. Circulation 1986, 73, 615–621. [Google Scholar] [CrossRef]
- Floras, J.S.; Ponikowski, P. The Sympathetic/Parasympathetic Imbalance in Heart Failure with Reduced Ejection Fraction. Eur. Heart J. 2015, 36, 1974–1982. [Google Scholar] [CrossRef]
- Del Rio, R.; Marcus, N.J.; Schultz, H.D. Carotid Chemoreceptor Ablation Improves Survival in Heart Failure. J. Am. Coll. Cardiol. 2013, 62, 2422–2430. [Google Scholar] [CrossRef]
- Narkiewicz, K.; Ratcliffe, L.E.K.; Hart, E.C.; Briant, L.J.B.; Chrostowska, M.; Wolf, J.; Szyndler, A.; Hering, D.; Abdala, A.P.; Manghat, N.; et al. Unilateral Carotid Body Resection in Resistant Hypertension: A Safety and Feasibility Trial. JACC. Basic to Transl. Sci. 2016, 1, 313–324. [Google Scholar] [CrossRef]
- Niewinski, P.; Tubek, S.; Paton, J.F.R.; Banasiak, W.; Ponikowski, P. Oxygenation Pattern and Compensatory Responses to Hypoxia and Hypercapnia Following Bilateral Carotid Body Resection in Humans. J. Physiol. 2021, 599, 2323–2340. [Google Scholar] [CrossRef]
- Victor, R.G. Carotid Baroreflex Activation Therapy for Resistant Hypertension. Nat. Rev. Cardiol. 2015, 12, 451–463. [Google Scholar] [CrossRef]
- Zile, M.R.; Lindenfeld, J.; Weaver, F.A.; Zannad, F.; Galle, E.; Rogers, T.; Abraham, W.T. Baroreflex Activation Therapy in Patients With Heart Failure with Reduced Ejection Fraction. J. Am. Coll. Cardiol. 2020, 76. [Google Scholar] [CrossRef]
- Dell’Oro, R.; Gronda, E.; Seravalle, G.; Costantino, G.; Alberti, L.; Baronio, B.; Staine, T.; Vanoli, E.; Mancia, G.; Grassi, G. Restoration of Normal Sympathetic Neural Function in Heart Failure Following Baroreflex Activation Therapy: Final 43-Month Study Report. J. Hypertens. 2017, 35, 2532–2536. [Google Scholar] [CrossRef] [PubMed]
- Pardini, B.J.; Lund, D.D.; Schmid, P.G. Organization of the Sympathetic Postganglionic Innervation of the Rat Heart. J. Auton. Nerv. Syst. 1989, 28, 193–201. [Google Scholar] [CrossRef] [PubMed]
- Garus, M.; Zdanowicz, A.; Fudim, M.; Zymliński, R.; Niewiński, P.; Paleczny, B.; Rosiek-Biegus, M.; Iwanek, G.; Ponikowski, P.; Biegus, J. Clinical Determinants and Prognostic Significance of Hypocapnia in Acute Heart Failure. Sci. Rep. 2022, 12, 16889. [Google Scholar] [CrossRef] [PubMed]
| Study | Method | Number of Participants | Age of Patients [Years] | LVEF [%] | Etiology of HF [%] | Treatment [%] | Peripheral Chemosensitivity to Hypoxia [L · min−1 · %SpO2−1] | Prevalence of Increased PChS [%] |
|---|---|---|---|---|---|---|---|---|
| Chua et al. (1996) [32] | Transient hypoxia; | 38 HF patients 15 healthy controls | 60.2 ± 8 | 25.7 ± 14.17 | IHD 57.9 DCM 31.6 VHD 5.2 Alcoholic-CM 2.6 HTN-CM 2.6 | Diuretics 100 ACE-I 92.1 Digoxin 26.3 | HF: 0.707 ± 0.47 Controls: 0.293 ± 0.22 | NR |
| Chua et al. (1996) [33] | Transient hypoxia | 13 HF patients 8 healthy controls | 60.5 ± 7.56 | 25.5 ± 15.48 | IHD 53.8 DCM 46.2 | Diuretics 100 ACE-I 92.3 | HF: 0.572 ± 0.295 Controls: 0.232 ± 0.062 | NR |
| Chua et al. (1997) [23] | Transient hypoxia | 50 HF patients 12 healthy controls | 58.7 ± 12.1 | 26.5 ± 13 | IHD 58 DCM 34 VHD 2 Alcoholic-CM 4 HTN-CM 2 | Diuretics 100 ACE-I 100 Digoxin 24 | HF: 0.673 ± 0.41 Controls: 0.272 ± 0.201 | 40 |
| Ponikowski et al. (1997) [30] | Transient hypoxia | 26 HF patients | 60 ± 8 | 25.6 ± 8.6 | IHD 80.8 DCM 19.2 | Diuretics 100 ACE-I 100 Digoxin 100 Nitrates 100 | HF: 0.72 ± 0.36 | 42 |
| Ponikowski et al. (1997) [67] | Transient hypoxia | 14 HF patients | 60 ± 1.1 | 26.6 ± 11.1 | IHD 78.6 DCM 21.4 | BB 0 | HF: 0.6 ± 0.28 (mean of 9 subjects with higher PChS) | 64 |
| Chua et al. (1997) [68] | Transient hypoxia | 12 HF patients | 65.5 ± 5.19 | 21.3 ± 10.38 | IHD 66.7 DCM 33.3 | Diuretics 100 ACE-I 100 | HF: 0.746 ± 0.36 | NR |
| Ponikowski et al. (1999) [34] | Transient hypoxia | 74 HF patients | 57 ± 10 | 25 ± 10 | IHD 77 DCM 23 | ACE-I 93 Diuretics 97 Digoxin 29 | HF with CSR: 0.80 ± 0.48 HF with PB: 0.75 ± 0.68 HF with NB 0.34 ± 0.16 | NR |
| Ponikowski et al. (1999) [69] | Transient hypoxia | 39 HF patients (13 with cachexia) 11 healthy controls | 60 ± 9 | 24 ± 9 | IHD 87.2 DCM 25.6 | Diuretics 94.8 ACE-I 87.2 Digoxin 48.7 | HF: 0.62 ± 0.34 (cachectic: 0.91 ± 0.37 non-cachectic: 0.47 ± 0.2) Controls: 0.29 ± 0.21 | NR |
| Ponikowski et al. (2001) [70] | Transient hypoxia | 38 HF patients 12 healthy controls | 57.8 ± 8 | 26.2 ± 11.7 | IHD 74 DCM 26 | Diuretics 100 ACE-I 95 Digoxin 39 | HF: 0.6 ± 2.46 Controls: 0.2 ± 0.35 | NR |
| Ponikowski et al. (2001) [25] | Transient hypoxia | 80 HF patients | 58 ± 9 | 24 ± 12 | IHD 69 DCM 31 | ACE-I 93 Diuretics 98 Digoxin 31 | HF: 0.69 ± 0.50 | 34 |
| Giannoni et al. (2008) [24] | Hypoxic isocapnic rebreathing technique; | 60 HF patients 12 healthy controls | 66 ± 7.75 | 31 ± 6.98 | IHD 38 Idiopathic 50 Secondary 12 | Diuretics 90 BB 92 ACE-I 62 ARB 22 MRA 62 | HF: 0.74 ± 0.47 Controls: 0.35 ± 0.2 | 40 |
| Giannoni et al. (2009) [35] | Hypoxic isocapnic rebreathing technique | 110 HF patients | 62 ± 15 | 31.1 ± 7.1 | IHD 47 Idiopathic 40 Secondary 13 | Diuretics 80 BB 86 ACE-I/ARB 78 MRA 42 CRT 27 ICD 17 | HF: 0.67 ± 0.45 | 40 |
| Niewinski et al. (2013) [31] | Transient hypoxia | 34 HF patients 16 healthy controls | 62 ± 11 | 27 [20,21,22,23,24,25,26,27,28,29,30] | IHD 71 | BB 100 ACE-I 91 MRA 88 Diuretics 74 ICD 50 CRT 29 | HF: 0.58 [0.32–0.95] Controls: 0.17 [0.06–0.29] | 44 |
| Mirizzi et al. (2016) [71] | Hypoxic isocapnic rebreathing technique | 191 HF patients | 62 ± 14 | 30 ± 8 | IHD 48 | BB 84 ACE-I/ARB 77 MRA 56 Diuretics 79 | HF: 0.5 [0.2–1.2] | 34 |
| Collins et al. (2020) [73] | Transient hypoxia | 12 HF patients 12 healthy controls | 53.6 ± 12.8 | 43.0 ± 8.7 | NR | BB 83 ACE-I/ARB 100 MRA 83 Diuretics 50 | HF: 0.81 ± 0.59 Controls: 0.39 ± 0.17 | NR |
| Tubek et al. (2021) [72] | Transient hypoxia | 30 HF patients 30 healthy controls | 62 ± 10 | 27.4 ± 7 | NR | BB 100 ACE-I/ARB 100 MRA 90 Diuretics 70 | HF: 0.6 ± 0.4 Controls: 0.3 ± 0.2 | 40 |
| Giannoni et al. (2022) [36] | Hypoxic isocapnic rebreathing technique | 369 HF patients | 65 ± 12 | 31 [25,26,27,28,29,30,31,32,33,34,35,36,37,38] | IHD 43 | BB 95 ACE-I/ARB 89 ARNI 4 MRA 77 Diuretics 71 ICD 21 CRT 19 | HF: 0.5 [0.3–0.9] (267 subjects) | 29 |
| Study | Time of O2 Inhalation | Rest/Exercise | Number of Participants | Age of Patients | LVEF [%] | Etiology of HF [%] | Treatment [%] | Effects of Hyperoxia |
|---|---|---|---|---|---|---|---|---|
| Chua et al. (1996) [33] | 3 breaths | rest; exercise | 13 HF patients 8 healthy controls | 60.5 ± 7.6 | 25.5 ± 15.5 | IHD 53.8 DCM 46.2 | Diuretics 100 ACE-I 92.3 | ↓ Ventilation (HF and Controls, p = NS) |
| Chua et al. (1996) [33] | NR | exercise | 12 HF patients | 65.5 ± 5.2 | 21.3 ± 10.4 | IHD 66.7 DCM 33.3 | Diuretics 100 ACE-I 100 | ↑ exercise time ↓ ventilatory response to exercise |
| Ponikowski et al. (1997) [30] | 20 min | rest | 12 HF patients | NR | NR | NR | NR | ↑ LFr and HFr power of HRV ↑ α index |
| Hennersdorf et al. (2001) [74] | 5 min | rest | 23 HF patients 26 healthy controls | 62.9 ± 7.9 | 29.9 ± 9.6 | IHD 91 DCM 9 | ACE-I 100 Digoxin 100 Diuretics 100 | ↓ HR (HF < Controls) |
| Franchitto et al. (2010) [75] | 15 min | rest | 18 HF + anemia patients 18 HF controls | 63.4 ± 11 | 29.9 ± 8.9 | IHD 77 | BB 89 ACE-I/ARB 66 Diuretics 72 | ↓ MSNA (HF + anemia) |
| Despas et al. (2012) [29] | 15 min | rest | 18 HF patients with augmented chemosensitivity 20 HF controls | 63.7 ± 16.1 | 29.5 ± 10.6 | IHD 67 DCM 28 VHD 6 | BB 78 ACE-I 72 Diuretics 83 | ↑ arterial baroreflex gain (HF with augmented PChS) ↓ MSNA (HF with augmented PChS) |
| Edgell et al. (2015) [27] | 2 min | rest | 11 HF patients 10 healthy controls | 60.3 ± 10 | 38.7 ± 15.3 | NR | BB 100 ACE-I 90.9 Diuretics 81.8 | ↓ HR (HF and Controls) ↓Ventilation (HF) |
| Tubek et al. (2021) [72] | 1 min | rest | 30 HF patients 30 healthy controls | 62 ± 10 | 27.4 ± 7 | no data | BB 100 ACE-I/ARB 100 MRA 90 Diuretics 70 | ↑ SVR, MAP (Controls) ↔ HR, MAP (HF) ↓ CO (HF and Controls) ↓ HR (Controls) ↓ Ventilation (HF) |
| Study | Dose of Dopamine [µg·kg−1·min−1] | Rest/Exercise | Number of Participants | Age of Patients | LVEF [%] | Etiology of HF [%] | Treatment [%] | Effects of Dopamine |
|---|---|---|---|---|---|---|---|---|
| Van der Borne et al. (1998) [28] | 5 | rest | 8 HF patients 8 healthy controls | 57 ± 12 | NR | IHD 62.5 Idiopathic 37.5 | NR | ↔ MAP, HR ↓ MV, HVR |
| Collins et al. (2020) [73] | 2 | exercise | 12 HF patients 12 healthy controls | 53.6 ± 12.8 | 43.0 ± 8.7 | NR | BB 83 ACE-I/ARB 100 MRA 83 Diuretics 50 | ↑ PETCO2, CO, SV, CO/MAP ↔ exercise time, MAP, HR |
| Edgell et al. (2015) [27] | 2 | rest | 11 HF patients 10 healthy controls | 60.3 ± 10 | 38.7 ± 15.3 | NR | BB 100 ACE-I 90.9 Diuretics 81.8 | ↑ CO, SV ↔ HR, MAP ↓ MV |
| Group of Predictors | Characteristics of Patients with High Chemosensitivity |
|---|---|
| Biochemical | ↓Hb [75] ↑GGT [71] ↑NA [24,36,71] ↑NT-proBNP [24,31,36,71] ↑BNP [24] |
| Clinical | Cardiac cachexia [69] ↑NYHA class [23,24,35,70,74] ↑Age [71] ↑MSNA [29] ↓Arterial baroreflex sensitivity [29] ↓Renal function [36] |
| Haemodynamic | ↓LVEF [23,25,31,70,71,74] ↑nsVT [23,35,74] ↑AF [35] ↓HRV [31] ↑RV dimensions [71] ↑SBP [31] ↑Systolic pulmonary pressure [36] |
| Respiratory | ↓Peak VO2 [31,35,70] ↑VE/VCO2 slope [23,35,36,70,71] |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Jura, M.; Garus, M.; Krakowska, K.; Urban, S.; Błaziak, M.; Iwanek, G.; Zymliński, R.; Biegus, J.; Paleczny, B. A Methodological Perspective on the Function and Assessment of Peripheral Chemoreceptors in Heart Failure: A Review of Data from Clinical Trials. Biomolecules 2022, 12, 1758. https://doi.org/10.3390/biom12121758
Jura M, Garus M, Krakowska K, Urban S, Błaziak M, Iwanek G, Zymliński R, Biegus J, Paleczny B. A Methodological Perspective on the Function and Assessment of Peripheral Chemoreceptors in Heart Failure: A Review of Data from Clinical Trials. Biomolecules. 2022; 12(12):1758. https://doi.org/10.3390/biom12121758
Chicago/Turabian StyleJura, Maksym, Mateusz Garus, Kornelia Krakowska, Szymon Urban, Mikołaj Błaziak, Gracjan Iwanek, Robert Zymliński, Jan Biegus, and Bartłomiej Paleczny. 2022. "A Methodological Perspective on the Function and Assessment of Peripheral Chemoreceptors in Heart Failure: A Review of Data from Clinical Trials" Biomolecules 12, no. 12: 1758. https://doi.org/10.3390/biom12121758
APA StyleJura, M., Garus, M., Krakowska, K., Urban, S., Błaziak, M., Iwanek, G., Zymliński, R., Biegus, J., & Paleczny, B. (2022). A Methodological Perspective on the Function and Assessment of Peripheral Chemoreceptors in Heart Failure: A Review of Data from Clinical Trials. Biomolecules, 12(12), 1758. https://doi.org/10.3390/biom12121758






