Antidepressant Drug Sertraline against Human Cancer Cells
Abstract
1. Introduction
2. Review on the Anticancer Effects of Sertraline against Different Human Cancer Cells
2.1. Lung Cancer
2.2. Colorectal Cancer
2.3. Breast Cancer
2.4. Hepatocellular Cancer
2.5. Leukemia
2.6. Brain Cancer
2.7. Melanoma
2.8. Oral Cancer
2.9. Ovarian Cancer
2.10. Prostate Cancer
2.11. Gastric Cancer
2.12. Osteosarcoma
3. Discussion on the Repurposing of Sertraline for Cancer Therapy
4. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Siegel, R.L.; Miller, K.D.; Fuchs, H.E.; Jemal, A. Cancer Statistics, 2022. CA Cancer J. Clin. 2022, 72, 7–33. [Google Scholar] [CrossRef] [PubMed]
- Yabroff, K.R.; Wu, X.-C.; Negoita, S.; Stevens, J.; Coyle, L.; Zhao, J.; Mumphrey, B.J.; Jemal, A.; Ward, K.C. Association of the COVID-19 Pandemic With Patterns of Statewide Cancer Services. J. Natl. Cancer Inst. 2022, 114, 907–909. [Google Scholar] [CrossRef] [PubMed]
- Antoszczak, M.; Markowska, A.; Markowska, J.; Huczyński, A. Old Wine in New Bottles: Drug Repurposing in Oncology. Eur. J. Pharmacol. 2020, 866, 172784. [Google Scholar] [CrossRef] [PubMed]
- Prasad, V.; Mailankody, S. Research and Development Spending to Bring a Single Cancer Drug to Market and Revenues After Approval. JAMA Intern. Med. 2017, 177, 1569–1575. [Google Scholar] [CrossRef]
- Mullard, A. 2015 FDA Drug Approvals. Nat. Rev. Drug Discov. 2016, 15, 73–76. [Google Scholar] [CrossRef]
- Jourdan, J.P.; Bureau, R.; Rochais, C.; Dallemagne, P. Drug Repositioning: A Brief Overview. J. Pharm. Pharmacol. 2020, 72, 1145–1151. [Google Scholar] [CrossRef]
- Pantziarka, P.; Bouche, G.; Meheus, L.; Sukhatme, V.; Sukhatme, V.P.; Vikas, P. The Repurposing Drugs in Oncology (ReDO) Project. Ecancermedicalscience 2014, 8, 442. [Google Scholar] [CrossRef]
- Verbaanderd, C.; Meheus, L.; Huys, I.; Pantziarka, P. Repurposing Drugs in Oncology: Next Steps. Trends Cancer 2017, 3, 543–546. [Google Scholar] [CrossRef]
- Issa, N.T.; Kruger, J.; Byers, S.W.; Dakshanamurthy, S. Drug Repurposing a Reality: From Computers to the Clinic. Expert Rev. Clin. Pharmacol. 2014, 6, 95–97. [Google Scholar] [CrossRef]
- Franks, M.E.; Macpherson, G.R.; Figg, W.D. Thalidomide. Lancet 2004, 363, 1802–1811. [Google Scholar] [CrossRef]
- Morales, D.R.; Morris, A.D. Metformin in Cancer Treatment and Prevention. Annu. Rev. Med. 2015, 66, 17–29. [Google Scholar] [CrossRef] [PubMed]
- Caly, L.; Druce, J.D.; Catton, M.G.; Jans, D.A.; Wagstaff, K.M. The FDA-Approved Drug Ivermectin Inhibits the Replication of SARS-CoV-2 in Vitro. Antivir. Res. 2020, 178, 104787. [Google Scholar] [CrossRef] [PubMed]
- Gao, J.; Tian, Z.; Yang, X. Breakthrough: Chloroquine Phosphate Has Shown Apparent Efficacy in Treatment of COVID-19 Associated Pneumonia in Clinical Studies. Biosci. Trends 2020, 14, 72–73. [Google Scholar] [CrossRef] [PubMed]
- Touret, F.; de Lamballerie, X. Of Chloroquine and COVID-19. Antivir. Res. 2020, 177, 104762. [Google Scholar] [CrossRef]
- Colson, P.; Rolain, J.M.; Lagier, J.C.; Brouqui, P.; Raoult, D. Chloroquine and Hydroxychloroquine as Available Weapons to Fight COVID-19. Int. J. Antimicrob. Agents 2020, 55, 105932. [Google Scholar] [CrossRef]
- Li, M.; Fitzgerald, P.; Rodin, G. Evidence-Based Treatment of Depression in Patients with Cancer. J. Clin. Oncol. 2012, 30, 1187–1196. [Google Scholar] [CrossRef]
- Rodin, G.; Katz, M.; Lloyd, N.; Green, E.; Mackay, J.A.; Wong, R.K.S. Treatment of Depression in Cancer Patients. Curr. Oncol. 2007, 14, 180–188. [Google Scholar] [CrossRef][Green Version]
- Grassi, L.; Nanni, M.G.; Rodin, G.; Li, M.; Caruso, R. The Use of Antidepressants in Oncology: A Review and Practical Tips for Oncologists. Ann. Oncol. 2018, 29, 101–111. [Google Scholar] [CrossRef]
- Roney, M.S.I.; Park, S.-K. Antipsychotic Dopamine Receptor Antagonists, Cancer, and Cancer Stem Cells. Arch. Pharm. Res. 2018, 41, 384–408. [Google Scholar] [CrossRef]
- Fond, G.; Macgregor, A.; Attal, J.; Larue, A.; Brittner, M.; Ducasse, D.; Capdevielle, D. Antipsychotic Drugs: Pro-Cancer or Anti-Cancer? A Systematic Review. Med. Hypotheses 2012, 79, 38–42. [Google Scholar] [CrossRef]
- Zong, D.; Zielinska-Chomej, K.; Juntti, T.; Mörk, B.; Lewensohn, R.; Hååg, P.; Viktorsson, K. Harnessing the Lysosome-Dependent Antitumor Activity of Phenothiazines in Human Small Cell Lung Cancer. Cell Death Dis. 2014, 5, e1111. [Google Scholar] [CrossRef]
- Munson, J.M.; Fried, L.; Rowson, S.A.; Bonner, M.Y.; Karumbaiah, L.; Diaz, B.; Courtneidge, S.A.; Knaus, U.G.; Brat, D.J.; Arbiser, J.L.; et al. Anti-Invasive Adjuvant Therapy with Imipramine Blue Enhances Chemotherapeutic Efficacy Against Glioma. Sci. Transl. Med. 2012, 4, 127ra36. [Google Scholar] [CrossRef]
- Abdelaleem, M.; Ezzat, H.; Osama, M.; Megahed, A.; Alaa, W.; Gaber, A.; Shafei, A.; Refaat, A. Prospects for Repurposing CNS Drugs for Cancer Treatment. Oncol. Rev. 2019, 13, 37–42. [Google Scholar] [CrossRef]
- Costa, P.; McCrae, R.; Cloninger, C.; Svrakic, D.; Sadock, B.; Sadock, V.; Adams, R.; Cultbertson, J. Kaplan and Sadock’s Comprehensive Textbook of Psychiatry; Wolters Kluwer: Alphen aan den Rijn, The Netherlands, 2000; Volume 1. [Google Scholar]
- Antoszczak, M.; Markowska, A.; Markowska, J.; Huczyński, A. Antidepressants and Antipsychotic Agents as Repurposable Oncological Drug Candidates. Curr. Med. Chem. 2021, 28, 2137–2174. [Google Scholar] [CrossRef]
- Booth, R.; Kim, H. Permeability Analysis of Neuroactive Drugs through a Dynamic Microfluidic in Vitro Blood-Brain Barrier Model. Ann. Biomed. Eng. 2014, 42, 2379–2391. [Google Scholar] [CrossRef]
- Wang, J.S.; Zhu, H.J.; Gibson, B.B.; Markowitz, J.S.; Donovan, J.L.; DeVane, C.L. Sertraline and Its Metabolite Desmethylsertraline, but Not Bupropion or Its Three Major Metabolites, Have High Affinity for P-Glycoprotein. Biol. Pharm. Bull. 2008, 31, 231–234. [Google Scholar] [CrossRef][Green Version]
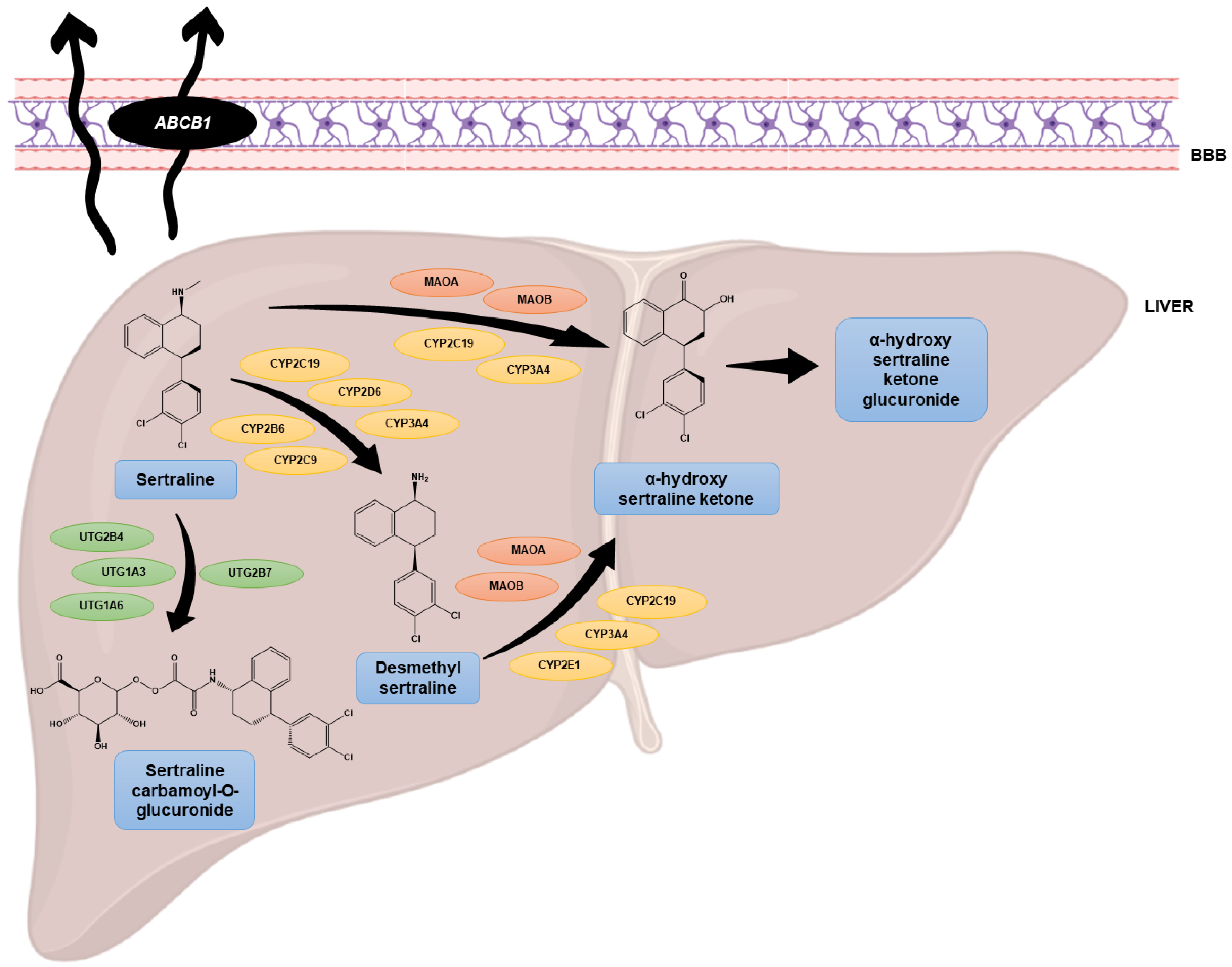
- Huddart, R.; Hicks, J.K.; Ramsey, L.B.; Strawn, J.R.; Smith, D.M.; Bobonis Babilonia, M.; Altman, R.B.; Klein, T.E. PharmGKB Summary: Sertraline Pathway, Pharmacokinetics. Pharmacogenet. Genom. 2020, 30, 26–33. [Google Scholar] [CrossRef]
- Chiles, C. Handbook of Psychiatric Drug Therapy, 5th Ed. J. Clin. Psychiatry 2007, 68, 339. [Google Scholar] [CrossRef]
- Abdul, M.; Logothetis, C.J.; Hoosein, N.M. Growth-Inhibitory Effects of Serotonin Uptake Inhibitors on Human Prostate Carcinoma Cell Lines. J. Urol. 1995, 154, 247–250. [Google Scholar] [CrossRef]
- Španová, A.; Kovářů, H.; Lisá, V.; Lukášová, E.; Rittich, B. Estimation of Apoptosis in C6 Glioma Cells Treated with Antidepressants. Physiol. Res. 1997, 46, 161–164. [Google Scholar]
- Levkovitz, Y.; Gil-Ad, I.; Zeldich, E.; Dayag, M.; Weizman, A. Differential Induction of Apoptosis by Antidepressants in Glioma and Neuroblastoma Cell Lines: Evidence for p-c-Jun, Cytochrome c, and Caspase-3 Involvement. J. Mol. Neurosci. 2005, 27, 029–042. [Google Scholar] [CrossRef]
- Koch, J.M.; Kell, S.; Aldenhoff, J.B. Differential Effects of Fluoxetine and Imipramine on the Phosphorylation of the Transcription Factor CREB and Cell-Viability. J. Psychiatr. Res. 2003, 37, 53–59. [Google Scholar] [CrossRef]
- Schuster, C.; Fernbach, N.; Rix, U.; Superti-Furga, G.; Holy, M.; Freissmuth, M.; Sitte, H.H.; Sexl, V. Selective Serotonin Reuptake Inhibitors-A New Modality for the Treatment of Lymphoma/Leukaemia? Biochem. Pharmacol. 2007, 74, 1424–1435. [Google Scholar] [CrossRef]
- Peer, D.; Dekel, Y.; Melikhov, D.; Margalit, R. Fluoxetine Inhibits Multidrug Resistance Extrusion Pumps and Enhances Responses to Chemotherapy in Syngeneic and in Human Xenograft Mouse Tumor Models. Cancer Res. 2004, 64, 7562–7569. [Google Scholar] [CrossRef]
- Telerman, A.; Tuynder, M.; Dupressoir, T.; Robaye, B.; Sigaux, F.; Shaulian, E.; Oren, M.; Rommelaere, J.; Amson, R. A Model for Tumor Suppression Using H-1 Parvovirus. Proc. Natl. Acad. Sci. USA 1993, 90, 8702–8706. [Google Scholar] [CrossRef]
- Tuynder, M.; Fiucci, G.; Prieur, S.; Lespagnol, A.; Géant, A.; Beaucourt, S.; Duflaut, D.; Besse, S.; Susini, L.; Cavarelli, J.; et al. Translationally Controlled Tumor Protein Is a Target of Tumor Reversion. Proc. Natl. Acad. Sci. USA 2004, 101, 15364–15369. [Google Scholar] [CrossRef]
- Nautiyal, K.; Li, R.; Yellapragada, S.; Thiagarajan, P.; Mims, M.; Rivero, G. Progressive Transfusion and Growth Factor Independence with Adjuvant Sertraline in Low Risk Myelodysplastic Syndrome Treated with an Erythropoiesis Stimulating Agent and Granulocyte-Colony Stimulating Factor. Leuk. Res. Rep. 2015, 4, 1–3. [Google Scholar] [CrossRef]
- Salacz, M.; Halatsch, M.; Neuro-oncology, G.K.-M.; Kast, R. RARE-09. Minimally Toxic Multimodal and Polypharmacological Therapy In Treatment of Diffuse Midline Glioma. Neuro-oncology 2017, 19, vi213. [Google Scholar] [CrossRef]
- Jiang, X.; Lu, W.; Shen, X.; Wang, Q.; Lv, J.; Liu, M.; Cheng, F.; Zhao, Z.; Pang, X. Repurposing Sertraline Sensitizes Non-Small Cell Lung Cancer Cells to Erlotinib by Inducing Autophagy. JCI Insight 2018, 3, e98921. [Google Scholar] [CrossRef]
- Zinnah, K.M.A.; Seol, J.-W.; Park, S.-Y. Inhibition of Autophagy Flux by Sertraline Attenuates TRAIL Resistance in Lung Cancer via Death Receptor 5 Upregulation. Int. J. Mol. Med. 2020, 46, 795–805. [Google Scholar] [CrossRef]
- Amson, R.; Karp, J.E.; Telerman, A. Lessons from Tumor Reversion for Cancer Treatment. Curr. Opin. Oncol. 2013, 25, 59–65. [Google Scholar] [CrossRef] [PubMed]
- Amson, R.; Pece, S.; Lespagnol, A.; Vyas, R.; Mazzarol, G.; Tosoni, D.; Colaluca, I.; Viale, G.; Rodrigues-Ferreira, S.; Wynendaele, J.; et al. Reciprocal Repression between P53 and TCTP. Nat. Med. 2011, 18, 91–99. [Google Scholar] [CrossRef] [PubMed]
- MacDonald, S.M.; Rafnar, T.; Langdon, J.; Lichtenstein, L.M. Molecular Identification of an IgE-Dependent Histamine-Releasing Factor. Science 1995, 269, 688–690. [Google Scholar] [CrossRef] [PubMed]
- Telerman, A.; Amson, R. Introduction: How We Encountered TCTP and Our Purpose in Studying It. Results Probl. Cell Differ. 2017, 64, 1–8. [Google Scholar] [CrossRef]
- Gil-Ad, I.; Zolokov, A.; Lomnitski, L.; Taler, M.; Bar, M.; Luria, D.; Ram, E.; Weizman, A. Evaluation of the Potential Anti-Cancer Activity of the Antidepressant Sertraline in Human Colon Cancer Cell Lines and in Colorectal Cancer-Xenografted Mice. Int. J. Oncol. 2008, 33, 277–286. [Google Scholar] [CrossRef]
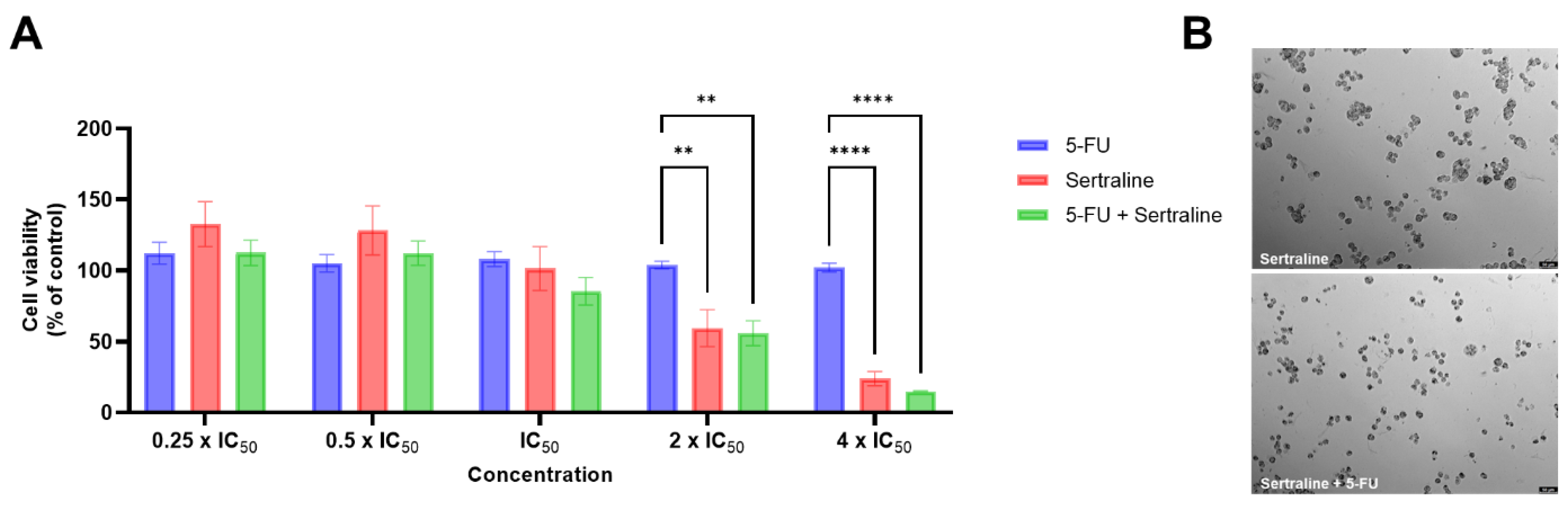
- Duarte, D.; Cardoso, A.; Vale, N. Synergistic Growth Inhibition of HT-29 Colon and MCF-7 Breast Cancer Cells with Simultaneous and Sequential Combinations of Antineoplastics and CNS Drugs. Int. J. Mol. Sci. 2021, 22, 7408. [Google Scholar] [CrossRef]
- Chou, T.-C.T.C. Theoretical Basis, Experimental Design, and Computerized Simulation of Synergism and Antagonism in Drug Combination Studies. Pharmacol. Rev. 2006, 58, 621–681. [Google Scholar] [CrossRef]
- Chou, T.C. Drug Combination Studies and Their Synergy Quantification Using the Chou-Talalay Method. Cancer Res. 2010, 70, 440–446. [Google Scholar] [CrossRef]
- Duarte, D.; Rêma, A.; Amorim, I.; Vale, N. Drug Combinations: A New Strategy to Extend Drug Repurposing and Epithelial-Mesenchymal Transition in Breast and Colon Cancer Cells. Biomolecules 2022, 12, 190. [Google Scholar] [CrossRef]
- Duarte, D.; Falcão, S.I.; El Mehdi, I.; Vilas-Boas, M.; Vale, N.; El Mehdi, I.; Vilas-Boas, M.; Vale, N. Honeybee Venom Synergistically Enhances the Cytotoxic Effect of CNS Drugs in HT-29 Colon and MCF-7 Breast Cancer Cell Lines. Pharmaceutics 2022, 14, 511. [Google Scholar] [CrossRef]
- Ye, D.; Xu, H.; Xia, H.; Zhang, C.; Tang, Q.; Bi, F. Targeting SERT Promotes Tryptophan Metabolism: Mechanisms and Implications in Colon Cancer Treatment. J. Exp. Clin. Cancer Res. 2021, 40, 173. [Google Scholar] [CrossRef]
- Juurlink, D. Revisiting the Drug Interaction between Tamoxifen and SSRI Antidepressants. BMJ 2016, 354, i5309. [Google Scholar] [CrossRef]
- Lin, C.-J.; Robert, F.; Sukarieh, R.; Michnick, S.; Pelletier, J. The Antidepressant Sertraline Inhibits Translation Initiation by Curtailing Mammalian Target of Rapamycin Signaling. Cancer Res. 2010, 70, 3199–3208. [Google Scholar] [CrossRef]
- Bavadekar, S.; Panchal, P.; Hanbashi, A.; Vansal, S. Cytotoxic Effects of Selective Serotonin- and Serotonin-Norepinephrine Reuptake Inhibitors on Human Metastatic Breast Cancer Cell Line, MCF-7 (842.3). FASEB J. 2014, 28, 842.3. [Google Scholar] [CrossRef]
- Gwynne, W.D.; Hallett, R.M.; Girgis-Gabardo, A.; Bojovic, B.; Dvorkin-Gheva, A.; Aarts, C.; Dias, K.; Bane, A.; Hassell, J.A. Serotonergic System Antagonists Target Breast Tumor Initiating Cells and Synergize with Chemotherapy to Shrink Human Breast Tumor Xenografts. Oncotarget 2017, 8, 32101–32116. [Google Scholar] [CrossRef]
- Hallett, R.M.; Girgis-Gabardo, A.; Gwynne, W.D.; Giacomelli, A.O.; Bisson, J.N.P.; Jensen, J.E.; Dvorkin-Gheva, A.; Hassell, J.A. Serotonin Transporter Antagonists Target Tumor-Initiating Cells in a Transgenic Mouse Model of Breast Cancer. Oncotarget 2016, 7, 53137–53152. [Google Scholar] [CrossRef]
- Geeraerts, S.L.; Kampen, K.R.; Rinaldi, G.; Gupta, P.; Planque, M.; Louros, N.; Heylen, E.; de Cremer, K.; de Brucker, K.; Vereecke, S.; et al. Repurposing the Antidepressant Sertraline as SHMT Inhibitor to Suppress Serine/Glycine Synthesis–Addicted Breast Tumor Growth. Mol. Cancer Ther. 2021, 20, 50–63. [Google Scholar] [CrossRef]
- Chen, S.; Xuan, J.; Wan, L.; Lin, H.; Couch, L.; Mei, N.; Dobrovolsky, V.N.; Guo, L. Sertraline, an Antidepressant, Induces Apoptosis in Hepatic Cells Through the Mitogen-Activated Protein Kinase Pathway. Toxicol. Sci. 2014, 137, 404–415. [Google Scholar] [CrossRef]
- Kuwahara, J.; Yamada, T.; Egashira, N.; Ueda, M.; Zukeyama, N.; Ushio, S.; Masuda, S. Comparison of the Anti-Tumor Effects of Selective Serotonin Reuptake Inhibitors as Well as Serotonin and Norepinephrine Reuptake Inhibitors in Human Hepatocellular Carcinoma Cells. Biol. Pharm. Bull. 2015, 38, 1410–1414. [Google Scholar] [CrossRef]
- Amit, B.H.; Gil-Ad, I.; Taler, M.; Bar, M.; Zolokov, A.; Weizman, A. Proapoptotic and Chemosensitizing Effects of Selective Serotonin Reuptake Inhibitors on T Cell Lymphoma/Leukemia (Jurkat) in Vitro. Eur. Neuropsychopharmacol. J. Eur. Coll. Neuropsychopharmacol. 2009, 19, 726–734. [Google Scholar] [CrossRef]
- Xia, D.; Zhang, Y.-T.; Xu, G.-P.; Yan, W.-W.; Pan, X.-R.; Tong, J.-H. Sertraline Exerts Its Antitumor Functions through Both Apoptosis and Autophagy Pathways in Acute Myeloid Leukemia Cells. Leuk. Lymphoma 2017, 58, 2208–2217. [Google Scholar] [CrossRef] [PubMed]
- Tzadok, S.; Beery, E.; Israeli, M.; Uziel, O.; Lahav, M.; Fenig, E.; Gil-Ad, I.; Weizman, A.; Nordenberg, J. In Vitro Novel Combinations of Psychotropics and Anti-Cancer Modalities in U87 Human Glioblastoma Cells. Int. J. Oncol. 2010, 37, 1043–1051. [Google Scholar] [CrossRef] [PubMed]
- Reddy, K.K.; Lefkove, B.; Chen, L.B.; Govindarajan, B.; Carracedo, A.; Velasco, G.; Carrillo, C.O.; Bhandarkar, S.S.; Owens, M.J.; Mechta-Grigoriou, F.; et al. The Antidepressant Sertraline Downregulates Akt and Has Activity against Melanoma Cells. Pigment Cell Melanoma Res. 2008, 21, 451–456. [Google Scholar] [CrossRef]
- Boia-Ferreira, M.; Basílio, A.B.; Hamasaki, A.E.; Matsubara, F.H.; Appel, M.H.; Da Costa, C.R.V.; Amson, R.; Telerman, A.; Chaim, O.M.; Veiga, S.S.; et al. TCTP as a Therapeutic Target in Melanoma Treatment. Br. J. Cancer 2017, 117, 656–665. [Google Scholar] [CrossRef]
- Chien, J.-M.; Chou, C.-T.; Pan, C.-C.; Kuo, C.-C.; Tsai, J.-Y.; Liao, W.-C.; Kuo, D.-H.; Shieh, P.; Ho, C.-M.; Chu, S.-T.; et al. The Mechanism of Sertraline-Induced [Ca2+]i Rise in Human OC2 Oral Cancer Cells. Hum. Exp. Toxicol. 2011, 30, 1635–1643. [Google Scholar] [CrossRef] [PubMed]
- Drinberg, V.; Bitcover, R.; Rajchenbach, W.; Peer, D. Modulating Cancer Multidrug Resistance by Sertraline in Combination with a Nanomedicine. Cancer Lett. 2014, 354, 290–298. [Google Scholar] [CrossRef] [PubMed]
- Huang, J.-K.; Chang, H.-T.; Chou, C.-T.; Shu, S.-S.; Kuo, C.-C.; Tsai, J.-Y.; Liao, W.-C.; Wang, J.-L.; Lin, K.-L.; Lu, Y.-C.; et al. The Mechanism of Sertraline-Induced [Ca(2+) ](i) Rise in Human PC3 Prostate Cancer Cells. Basic Clin. Pharmacol. Toxicol. 2011, 109, 103–110. [Google Scholar] [CrossRef] [PubMed]
- Chinnapaka, S.; Bakthavachalam, V.; Munirathinam, G. Repurposing Antidepressant Sertraline as a Pharmacological Drug to Target Prostate Cancer Stem Cells: Dual Activation of Apoptosis and Autophagy Signaling by Deregulating Redox Balance. Am. J. Cancer Res. 2020, 10, 2043–2065. [Google Scholar]
- Mu, C.; Peng, R.-K.; Guo, C.-L.; Li, A.; Yang, X.-M.; Zeng, R.; Li, Y.-L.; Gu, J.; Ouyang, Q. Discovery of Sertraline and Its Derivatives Able to Combat Drug-Resistant Gastric Cancer Cell via Inducing Apoptosis. Bioorg. Med. Chem. Lett. 2021, 41, 127997. [Google Scholar] [CrossRef]
- Lin, K.-L.; Chi, C.-C.; Lu, T.; Tseng, L.-L.; Wang, J.-L.; Lu, Y.-C.; Jan, C.-R. Effect of Sertraline on [Ca2+](i) and Viability of Human MG63 Osteosarcoma Cells. Drug Chem. Toxicol. 2013, 36, 231–240. [Google Scholar] [CrossRef]
- Cipriani, A.; La Ferla, T.; Furukawa, T.A.; Signoretti, A.; Nakagawa, A.; Churchill, R.; McGuire, H.; Barbui, C. Sertraline versus Other Antidepressive Agents for Depression. Cochrane Database Syst. Rev. 2010, 4, CD006117. [Google Scholar] [CrossRef]
- Rot, M.A.H.; Mathew, S.J.; Charney, D.S. Neurobiological Mechanisms in Major Depressive Disorder. CMAJ 2009, 180, 305–313. [Google Scholar] [CrossRef]
- Sangkuhl, K.; Klein, T.E.; Altman, R.B. Selective Serotonin Reuptake Inhibitors Pathway. Pharmacogenet. Genom. 2009, 19, 907–909. [Google Scholar] [CrossRef]
- Romero, L.; Bel, N.; Artigas, F.; De Montigny, C.; Blier, P. Effect of Pindolol on the Function of Pre- and Postsynaptic 5-HT1A Receptors: In Vivo Microdialysis and Electrophysiological Studies in the Rat Brain. Neuropsychopharmacology 1996, 15, 349–360. [Google Scholar] [CrossRef]
- Artigas, F.; Romero, L.; De Montigny, C.; Blier, P. Acceleration of the Effect of Selected Antidepressant Drugs in Major Depression by 5-HT1A Antagonists. Trends Neurosci. 1996, 19, 378–383. [Google Scholar] [CrossRef]
- El Mansari, M.; Sánchez, C.; Chouvet, G.; Renaud, B.; Haddjeri, N. Effects of Acute and Long-Term Administration of Escitalopram and Citalopram on Serotonin Neurotransmission: An in Vivo Electrophysiological Study in Rat Brain. Neuropsychopharmacology 2005, 30, 1269–1277. [Google Scholar] [CrossRef]
- Hervás, I.; Vilaró, M.T.; Romero, L.; Scorza, M.C.; Mengod, G.; Artigas, F. Desensitization of 5-HT1A Autoreceptors by a Low Chronic Fluoxetine Dose Effect of the Concurrent Administration of WAY-100635. Neuropsychopharmacology 2001, 24, 11–20. [Google Scholar] [CrossRef]
- Boldrini, M.; Underwood, M.D.; Mann, J.J.; Arango, V. Serotonin-1A Autoreceptor Binding in the Dorsal Raphe Nucleus of Depressed Suicides. J. Psychiatr. Res. 2008, 42, 433–442. [Google Scholar] [CrossRef]
- Parsey, R.V.; Olvet, D.M.; Oquendo, M.A.; Huang, Y.Y.; Ogden, R.T.; Mann, J.J. Higher 5-HT1A Receptor Binding Potential during a Major Depressive Episode Predicts Poor Treatment Response: Preliminary Data from a Naturalistic Study. Neuropsychopharmacology 2006, 31, 1745–1749. [Google Scholar] [CrossRef]
- Kitaichi, Y.; Inoue, T.; Nakagawa, S.; Boku, S.; Kakuta, A.; Izumi, T.; Koyama, T. Sertraline Increases Extracellular Levels Not Only of Serotonin, but Also of Dopamine in the Nucleus Accumbens and Striatum of Rats. Eur. J. Pharmacol. 2010, 647, 90–96. [Google Scholar] [CrossRef]
- Busby, J.; Murray, L.; Mills, K.; Zhang, S.-D.; Liberante, F.; Cardwell, C.R. A Combined Connectivity Mapping and Pharmacoepidemiology Approach to Identify Existing Medications with Breast Cancer Causing or Preventing Properties. Pharmacoepidemiol. Drug Saf. 2018, 27, 78–86. [Google Scholar] [CrossRef] [PubMed]
- Chan, H.-L.; Chiu, W.-C.; Chen, V.C.-H.; Huang, K.-Y.; Wang, T.-N.; Lee, Y.; McIntyre, R.S.; Hsu, T.-C.; Lee, C.T.-C.; Tzang, B.-S. SSRIs Associated with Decreased Risk of Hepatocellular Carcinoma: A Population-Based Case-Control Study. Psychooncology 2018, 27, 187–192. [Google Scholar] [CrossRef] [PubMed]
- Christensen, D.K.; Armaiz-Pena, G.N.; Ramirez, E.; Matsuo, K.; Zimmerman, B.; Zand, B.; Shinn, E.; Goodheart, M.J.; Bender, D.; Thaker, P.H.; et al. SSRI Use and Clinical Outcomes in Epithelial Ovarian Cancer. Oncotarget 2016, 7, 33179–33191. [Google Scholar] [CrossRef] [PubMed]
- Mørch, L.S.; Dehlendorff, C.; Baandrup, L.; Friis, S.; Kjaer, S.K. Use of Antidepressants and Risk of Epithelial Ovarian Cancer. Int. J. Cancer 2017, 141, 2197–2203. [Google Scholar] [CrossRef] [PubMed]
- Ferguson, J.M. SSRI Antidepressant Medications: Adverse Effects and Tolerability. Prim. Care Companion J. Clin. Psychiatry 2001, 3, 22–27. [Google Scholar] [CrossRef] [PubMed]
- Kesim, M.; Tiryaki, A.; Kadioglu, M.; Muci, E.; Kalyoncu, N.I.; Yaris, E. The Effects of Sertraline on Blood Lipids, Glucose, Insulin and HBA1C Levels: A Prospective Clinical Trial on Depressive Patients. J. Res. Med. Sci. 2011, 16, 1525–1531. [Google Scholar] [PubMed]
- Sertraline: MedlinePlus Drug Information. Available online: https://medlineplus.gov/druginfo/meds/a697048.html (accessed on 26 September 2022).
- A Proof-of-Concept Clinical Trial Assessing the Safety of the Coordinated Undermining of Survival Paths by 9 Repurposed Drugs Combined With Metronomic Temozolomide (CUSP9v3 Treatment Protocol) for Recurrent Glioblastoma—No Study Results Posted—ClinicalTrials.Gov. Available online: https://clinicaltrials.gov/ct2/show/results/NCT02770378?term=NCT02770378&draw=2&rank=1 (accessed on 21 September 2022).
- Sertraline and Cytosine Arabinoside in Adults With Relapsed and Refractory AML—Full Text View—ClinicalTrials.Gov. Available online: https://clinicaltrials.gov/ct2/show/study/NCT02891278?term=NCT02891278&draw=2&rank=1 (accessed on 21 September 2022).


| Condition | Cell Lines | In Vivo Results? | Main Findings | References |
|---|---|---|---|---|
| Lung cancer | A549, H522, PC9/R, and H1975 | + |
| [40] |
| A549, HCC-15, and Calu-3 | - |
| [41] | |
| Colorectal cancer | HCT116 | + |
| [43] |
| HT-29 and LS1034 | + |
| [46] | |
| HT-29 | - |
| [47] | |
| HT-29 | - |
| [50] | |
| HT-29 | - |
| [51] | |
| SW480 and HCT116 | + |
| [52] | |
| Breast cancer | MCF-7 | + |
| [54] |
| MCF-7 | - |
| [55] | |
| BTIC | + |
| [56,57] | |
| MDA-MB-231, MDA-MB-468, MCF-7 and HCC70 | + |
| [58] | |
| MCF-7 | - |
| [47,50] | |
| MCF-7 | - |
| [51] | |
| Hepatocellular cancer | HepG2 | - |
| [59] |
| HepG2 | - |
| [60] | |
| Leukemia | Jurkat T cell | - |
| [61] |
| NB4, NB4-R1 and NB4-R2 | + |
| [62] | |
| Brain cancer | U87 | - |
| [63] |
| Melanoma | A375 | + |
| [64] |
| MeWo, A2058, and B16-F10 | + |
| [65] | |
| Oral cancer | OC2 | - |
| [66] |
| Ovarian cancer | OVCAR-8 and NCI/ADR-Res (NAR) | + |
| [67] |
| Prostate cancer | PC-3 | - |
| [68] |
| PCSC | - |
| [69] | |
| Gastric cancer | SGC-7901/DDP | - |
| [70] |
| Osteosarcoma | MG63 | - |
| [71] |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Duarte, D.; Vale, N. Antidepressant Drug Sertraline against Human Cancer Cells. Biomolecules 2022, 12, 1513. https://doi.org/10.3390/biom12101513
Duarte D, Vale N. Antidepressant Drug Sertraline against Human Cancer Cells. Biomolecules. 2022; 12(10):1513. https://doi.org/10.3390/biom12101513
Chicago/Turabian StyleDuarte, Diana, and Nuno Vale. 2022. "Antidepressant Drug Sertraline against Human Cancer Cells" Biomolecules 12, no. 10: 1513. https://doi.org/10.3390/biom12101513
APA StyleDuarte, D., & Vale, N. (2022). Antidepressant Drug Sertraline against Human Cancer Cells. Biomolecules, 12(10), 1513. https://doi.org/10.3390/biom12101513







