Performance of Serum Angiotensin-Converting Enzyme in Diagnosing Sarcoidosis and Predicting the Active Status of Sarcoidosis: A Meta-Analysis
Abstract
:1. Introduction
2. Materials and Methods
2.1. Search Strategy
2.2. Selection of Publications
2.3. Data Extraction and Quality Assessment
2.4. Statistical Analysis
3. Results
3.1. Study Selection
3.2. Clinical Characteristics of the Included Studies
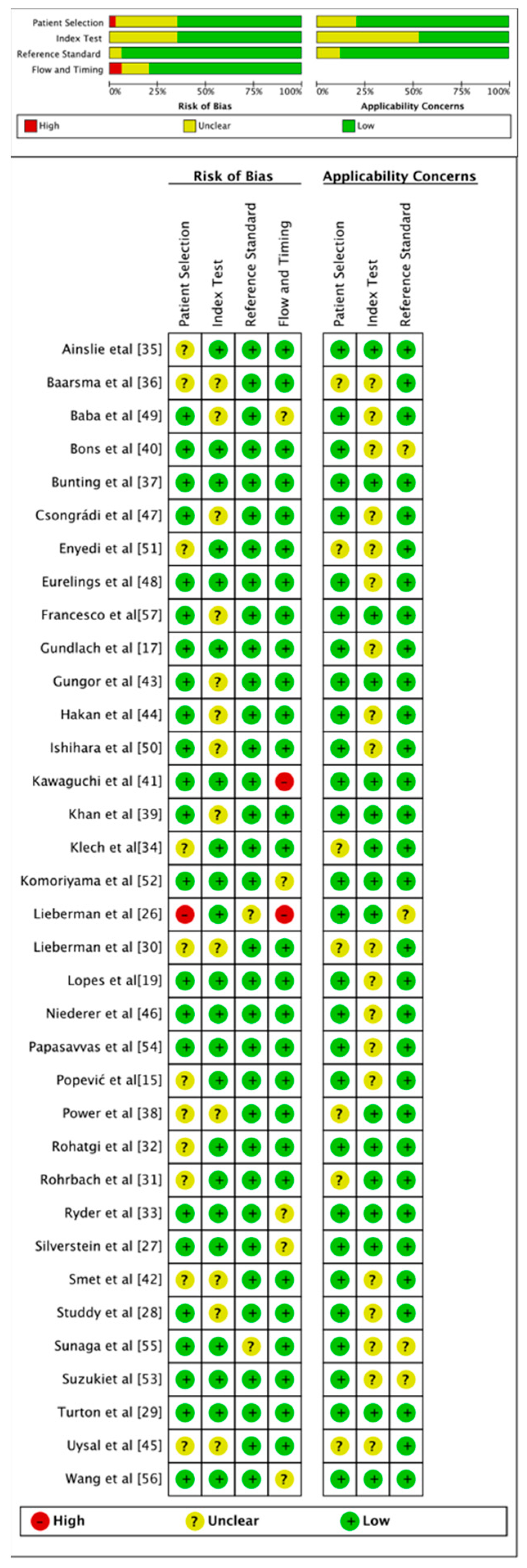
3.3. Risk of Bias Assessment
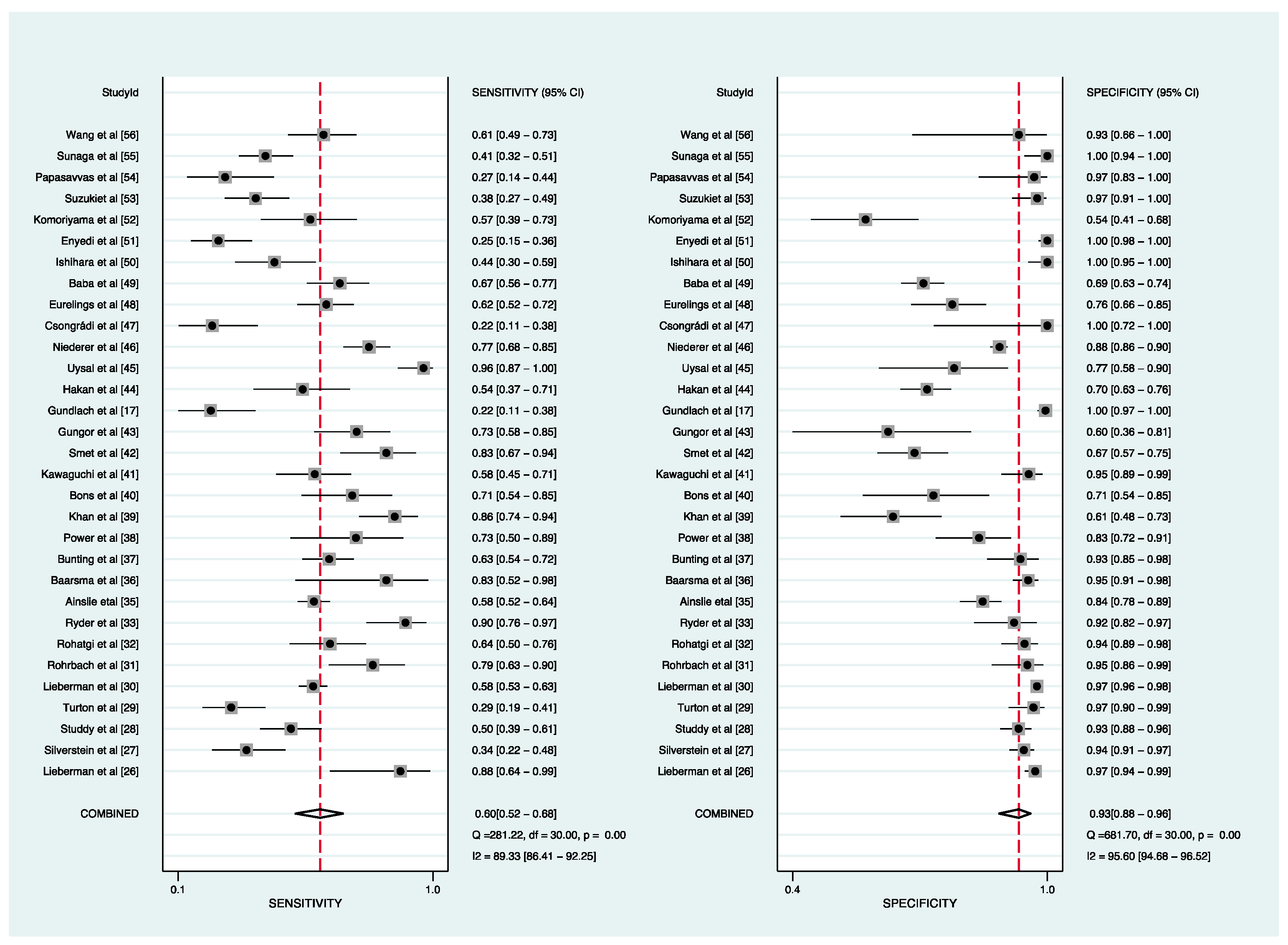
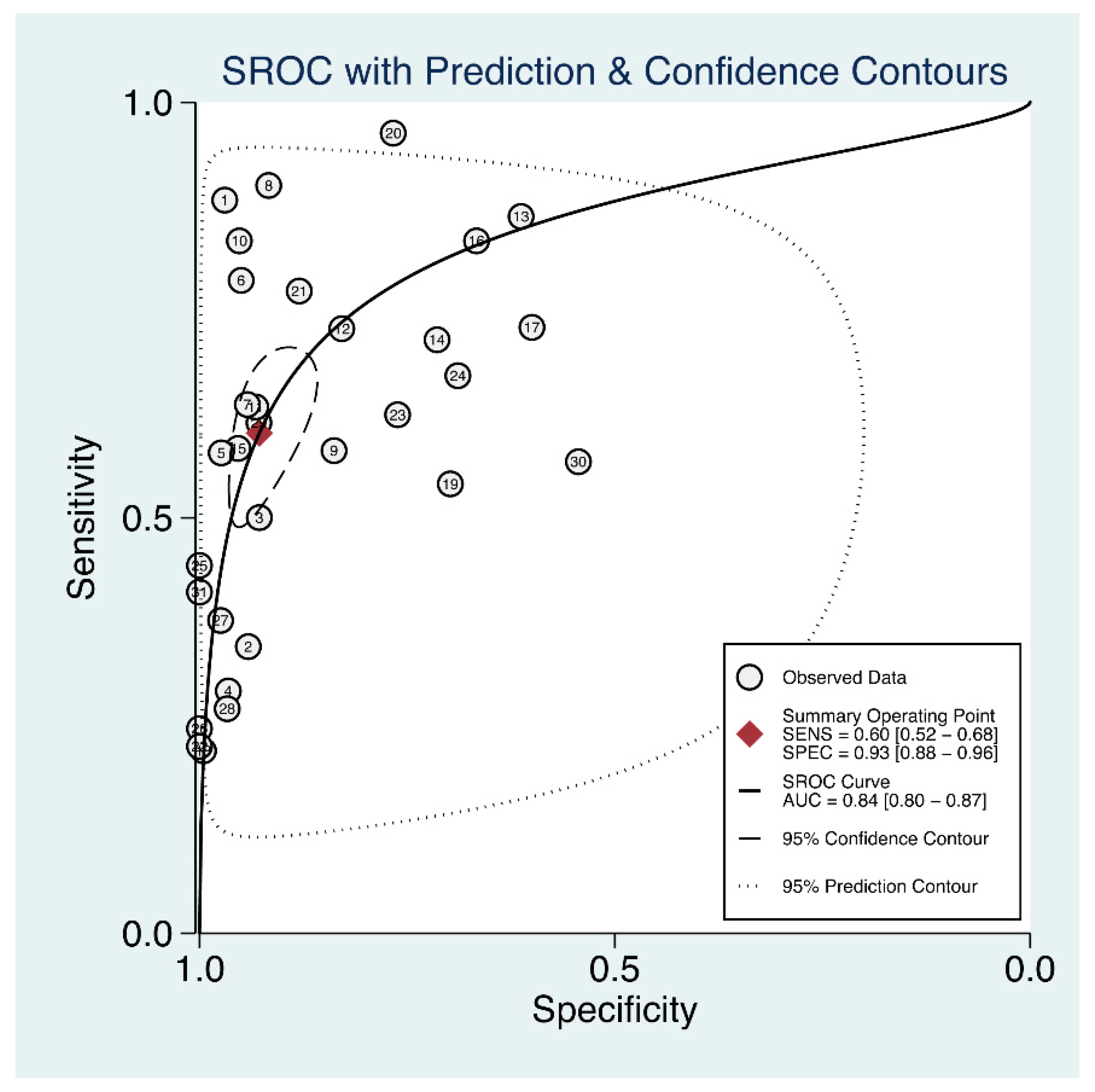
3.4. Diagnosis Utility of sACE for Sarcoidosis
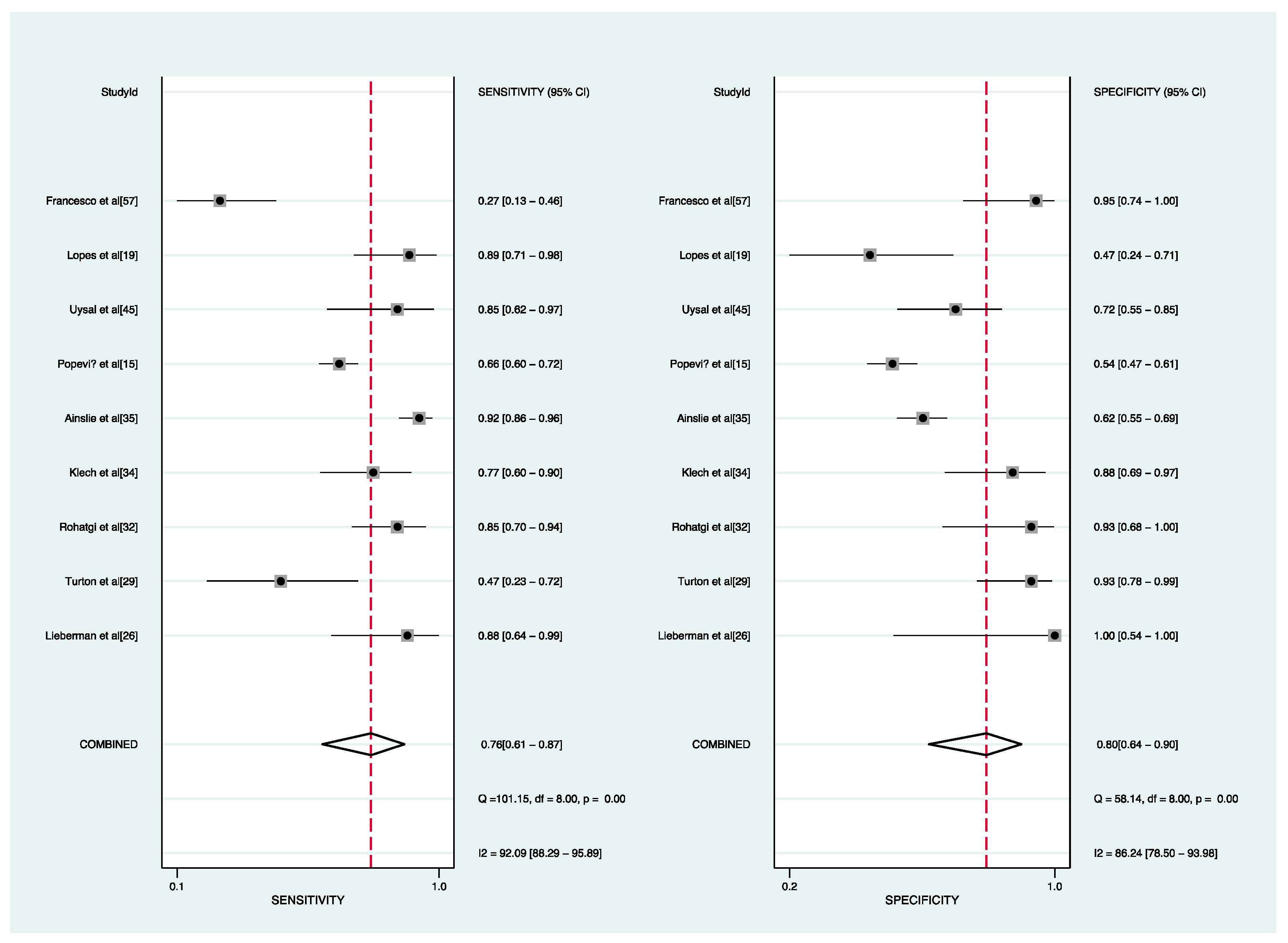
3.5. Predictive Accuracy of sACE for the Active Status of Sarcoidosis
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Llanos, O.; Hamzeh, N. Sarcoidosis. Med. Clin. N. Am. 2019, 103, 527–534. [Google Scholar] [CrossRef] [PubMed]
- Nardi, A.; Brillet, P.-Y.; Letoumelin, P.; Girard, F.; Brauner, M.; Uzunhan, Y.; Naccache, J.-M.; Valeyre, D.; Nunes, H. Stage IV sarcoidosis: Comparison of survival with the general population and causes of death. Eur. Respir. J. 2011, 38, 1368–1373. [Google Scholar] [CrossRef] [PubMed]
- Valeyre, D.; Prasse, A.; Nunes, H.; Uzunhan, Y.; Brillet, P.-Y.; Müller-Quernheim, J. Sarcoidosis. Lancet 2014, 383, 1155–1167. [Google Scholar] [CrossRef]
- Costabel, U.; Ohshimo, S.; Guzman, J. Diagnosis of sarcoidosis. Curr. Opin. Pulm. Med. 2008, 14, 455–461. [Google Scholar] [CrossRef]
- Crouser, E.D.; Maier, L.A.; Wilson, K.C.; Bonham, C.A.; Morgenthau, A.S.; Patterson, K.C.; Abston, E.; Bernstein, R.C.; Blankstein, R.; Chen, E.S.; et al. Diagnosis and Detection of Sarcoidosis. An Official American Thoracic Society Clinical Practice Guideline. Am. J. Respir. Crit. Care Med. 2020, 201, e26–e51. [Google Scholar] [CrossRef]
- Heinle, R.; Chang, C. Diagnostic criteria for sarcoidosis. Autoimmun. Rev. 2014, 13, 383–387. [Google Scholar] [CrossRef]
- Millward, K.; Fiddler, C.A.; Thillai, M. Update on sarcoidosis guidelines. Curr. Opin. Pulm. Med. 2021, 27, 484–489. [Google Scholar] [CrossRef]
- American Thoracic Society. Statement on Sarcoidosis. Joint Statement of the American Thoracic Society (ATS), the European Respiratory Society (ERS) and the World Association of Sarcoidosis and Other Granulomatous Disorders (WASOG) adopted by the ATS Board of Direc-tors and by the ERS Executive Committee, February 1999. Am. J. Respir. Crit. Care Med. 1999, 160, 736–755. [Google Scholar] [CrossRef]
- Soto-Gomez, N.; Peters, J.I.; Nambiar, A. Diagnosis and Management of Sarcoidosis. Am. Fam. Physician 2016, 93, 840–848. [Google Scholar]
- Chopra, A.; Kalkanis, A.; Judson, M.A. Biomarkers in sarcoidosis. Expert Rev. Clin. Immunol. 2016, 12, 1191–1208. [Google Scholar] [CrossRef]
- Ghafouri-Fard, S.; Noroozi, R.; Omrani, M.D.; Branicki, W.; Pośpiech, E.; Sayad, A.; Pyrc, K.; Łabaj, P.; Vafaee, R.; Taheri, M.; et al. Angiotensin converting enzyme: A review on expression profile and its association with human disorders with special focus on SARS-CoV-2 infection. Vasc. Pharmacol. 2020, 130, 106680. [Google Scholar] [CrossRef] [PubMed]
- Liu, M.; Wang, T.; Zhou, Y.; Zhao, Y.; Zhang, Y.; Li, J. Potential role of ACE2 in coronavirus disease 2019 (COVID-19) prevention and management. J. Transl. Intern. Med. 2020, 8, 9–19. [Google Scholar] [CrossRef] [PubMed]
- Yang, H.; Mo, T.; Nie, W.; Li, B. Angiotensin converting enzyme I/D polymorphism and sarcoidosis risk. Sarcoidosis Vasc. Diffus. lung Dis. Off. J. WASOG 2016, 32, 284–288. [Google Scholar]
- Rosen, Y. Pathology of Sarcoidosis. Semin. Respir. Crit. Care Med. 2007, 28, 036–052. [Google Scholar] [CrossRef] [PubMed]
- Popević, S.; Šumarac, Z.; Jovanović, D.; Babić, D.; Stjepanović, M.; Jovičić, S.; Šobić-Šaranović, D.; Filipović, S.; Gvozdenović, B.; Omčikus, M.; et al. Verifying Sarcoidosis Activity: Chitotriosidase Versus ACE in Sarcoidosis—A Case-Control Study. J. Med. Biochem. 2016, 35, 390–400. [Google Scholar] [CrossRef] [PubMed]
- Duan, J.; Xu, Y.; Zhu, H.; Zhang, H.; Sun, S.; Sun, H.; Wang, W.; Xie, S. Relationship between CT activity score with lung function and the serum angiotensin converting enzyme in pulmonary sarcoidosis on chest HRCT. Medicine 2018, 97, e12205. [Google Scholar] [CrossRef]
- Gundlach, E.; Hoffmann, M.M.; Prasse, A.; Heinzelmann, S.; Ness, T. Interleukin-2 Receptor and Angiotensin-Converting Enzyme as Markers for Ocular Sarcoidosis. PLoS ONE 2016, 11, e0147258. [Google Scholar] [CrossRef]
- Romer, F.K. Angiotensin-converting enzyme activity in sarcoidosis and other disorders. Sarcoidosis 1985, 2, 25–34. [Google Scholar]
- Lopes, M.C.; Amadeu, T.P.; Ribeiro-Alves, M.; da Costa, C.H.; Rodrigues, L.S.; Bessa, E.J.C.; Bruno, L.P.; Lopes, A.J.; Rufino, R. Identification of Active Sarcoidosis Using Chitotriosidase and Angiotensin-Converting Enzyme. Lung 2019, 197, 295–302. [Google Scholar] [CrossRef]
- Leeflang, M. Systematic reviews and meta-analyses of diagnostic test accuracy. Clin. Microbiol. Infect. 2014, 20, 105–113. [Google Scholar] [CrossRef]
- Whiting, P.F.; Rutjes, A.W.S.; Westwood, M.E.; Mallett, S.; Deeks, J.J.; Reitsma, J.B.; Leeflang, M.M.G.; Sterne, J.A.C.; Bossuyt, P.M.M.; QUADAS-2 Group. QUADAS-2: A Revised Tool for the Quality Assessment of Diagnostic Accuracy Studies. Ann. Intern. Med. 2011, 155, 529–536. [Google Scholar] [CrossRef] [PubMed]
- Devillé, W.L.; Buntinx, F.; Bouter, L.M.; Montori, V.M.; de Vet, H.C.W.; van der Windt, D.A.W.M.; Bezemer, P.D. Conducting systematic reviews of diagnostic studies: Didactic guidelines. BMC Med. Res. Methodol. 2002, 2, 9. [Google Scholar] [CrossRef] [PubMed]
- Moses, L.E.; Shapiro, D.; Littenberg, B. Combining independent studies of a diagnostic test into a summary roc curve: Data-analytic approaches and some additional considerations. Stat. Med. 1993, 12, 1293–1316. [Google Scholar] [CrossRef] [PubMed]
- Spineli, L.M.; Pandis, N. Exploring heterogeneity in meta-analysis: Subgroup analysis. Part 1. Am. J. Orthod. Dentofac. Orthop. 2020, 158, 302–304. [Google Scholar] [CrossRef] [PubMed]
- Deeks, J.J.; Macaskill, P.; Irwig, L. The performance of tests of publication bias and other sample size effects in systematic reviews of diagnostic test accuracy was assessed. J. Clin. Epidemiology 2005, 58, 882–893. [Google Scholar] [CrossRef] [PubMed]
- Lieberman, J. Elevation of serum angiotension-converting-enzyme (ACE) level in sarcoidosis. Am. J. Med. 1975, 59, 365–372. [Google Scholar] [CrossRef]
- Silverstein, E.; Friedland, J.; Lyons, H.A.; Gourin, A. Elevation of angiotensin-converting enzyme in granulomatous lymph nodes and serum in sarcoidosis: Clinical and possible pathogenic significance. Ann. N. Y. Acad. Sci. 1976, 278, 498–513. [Google Scholar] [CrossRef]
- Studdy, P.; Bird, R.; James, D.G.; Sherlock, S. Serum angiotensin-converting enzyme (SACE) in sarcoidosis and other granulomatous disorders. Lancet 1978, 312, 1331–1334. [Google Scholar] [CrossRef]
- Turton, C.W.; Grundy, E.; Firth, G.; Mitchell, D.; Rigden, B.G.; Turner-Warwick, M. Value of measuring serum angiotensin I converting enzyme and serum lysozyme in the management of sarcoidosis. Thorax 1979, 34, 57–62. [Google Scholar] [CrossRef]
- Lieberman, J.; Nosal, A.; Schlessner, A.; Sastre-Foken, A. Serum angiotensin-converting enzyme for diagnosis and therapeutic evaluation of sarcoidosis. Am. Rev. Respir. Dis. 1979, 120, 329–335. [Google Scholar] [CrossRef]
- Rohrbach, M.S.; DeRemee, R.A. Serum angiotensin converting enzyme activity in sarcoidosis as measured by a simple radiochemical assay. Am. Rev. Respir. Dis. 1979, 119, 761–767. [Google Scholar] [CrossRef] [PubMed]
- Rohatgi, P.K.; Ryan, J.W. Simple Radioassay for Measuring Serum Activity of Angiotensin-Converting Enzyme in Sarcoidosis. Chest 1980, 78, 69–76. [Google Scholar] [CrossRef] [PubMed]
- Ryder, K.W.; Jay, S.J.; Jackson, S.A.; Hoke, S.R. Characterization of a spectrophotometric assay for angiotensin converting enzyme. Clin. Chem. 1981, 27, 530–534. [Google Scholar] [CrossRef] [PubMed]
- Klech, H.; Kohn, H.; Kummer, F.; Mostbeck, A. Assessment of Activity in Sarcoidosis: Sensitivity and Specificity of 67gallium Scintigraphy, Serum Ace Levels, Chest Roentgenography, and Blood Lymphocyte Subpopulations. Chest 1982, 82, 732–738. [Google Scholar] [CrossRef] [PubMed]
- Ainslie, G.M.; Benatar, S.R. Serum Angiotensin Converting Enzyme in Sarcoidosis: Sensitivity and Specificity in Diagnosis: Correlations with Disease Activity, Duration, Extra-thoracic Involvement, Radiographic Type and Therapy. QJM Int. J. Med. 1985, 55, 253–270. [Google Scholar] [CrossRef]
- Baarsma, G.; La Hey, E.; Glasius, E.; de Vries, J.; Kijlstra, A. The Predictive Value of Serum Angiotensin Converting Enzyme and Lysozyme Levels in the Diagnosis of Ocular Sarcoidosis. Am. J. Ophthalmol. 1987, 104, 211–217. [Google Scholar] [CrossRef]
- Bunting, P.S.; Szalai, J.P.; Katic, M. Diagnostic aspects of angiotensin converting enzyme in pulmonary sarcoidosis. Clin. Biochem. 1987, 20, 213–219. [Google Scholar] [CrossRef]
- Power, W.J.; Neves, R.A.; Rodriguez, A.; Pedroza-Seres, M.; Foster, C.S. The Value of Combined Serum Angiotensin-converting Enzyme and Gallium Scan in Diagnosing Ocular Sarcoidosis. Ophthalmology 1995, 102, 2007–2011. [Google Scholar] [CrossRef]
- Khan, A.H.; Ghani, F.; Khan, M.A.; Khurshid, M. Role of serum angiotensin converting enzyme in sarcoidosis. J. Pak. Med. Assoc. 1998, 48, 131. [Google Scholar]
- Kawaguchi, T.; Hanada, A.; Horie, S.; Sugamoto, Y.; Sugita, S.; Mochizuki, M. Evaluation of Characteristic Ocular Signs and Systemic Investigations in Ocular Sarcoidosis Patients. Jpn. J. Ophthalmol. 2007, 51, 121–126. [Google Scholar] [CrossRef]
- Bons, J.A.; Drent, M.; Bouwman, F.G.; Mariman, E.C.; van Dieijen-Visser, M.P.; Wodzig, W.K. Potential biomarkers for diagnosis of sarcoidosis using proteomics in serum. Respir. Med. 2007, 101, 1687–1695. [Google Scholar] [CrossRef] [PubMed]
- De Smet, D.; Martens, G.A.; Berghe, B.V.; Meysman, M.; Heylen, O.; Gorus, F.K.; De Waele, M. Use of Likelihood Ratios Improves Interpretation of Laboratory Testing for Pulmonary Sarcoidosis. Am. J. Clin. Pathol. 2010, 134, 939–947. [Google Scholar] [CrossRef] [PubMed]
- Gungor, S.; Ozseker, F.; Yalcinsoy, M.; Akkaya, E.; Can, G.; Eroglu, H.; Genc, N.S. Conventional markers in determination of activity of sarcoidosis. Int. Immunopharmacol. 2015, 25, 174–179. [Google Scholar] [CrossRef] [PubMed]
- Groen-Hakan, F.; Eurelings, L.; Berge, J.C.T.; Van Laar, J.; Ramakers, C.R.B.; Dik, W.A.; Rothova, A. Diagnostic Value of Serum-Soluble Interleukin 2 Receptor Levels vs Angiotensin-Converting Enzyme in Patients with Sarcoidosis-Associated Uveitis. JAMA Ophthalmol. 2017, 135, 1352–1358. [Google Scholar] [CrossRef] [PubMed]
- Uysal, P.; Durmus, S.; Sozer, V.; Gelisgen, R.; Seyhan, E.C.; Erdenen, F.; Simsek, G.; Uzun, H. YKL-40, Soluble IL-2 Receptor, Angiotensin Converting Enzyme and C-Reactive Protein: Comparison of Markers of Sarcoidosis Activity. Biomolecules 2018, 8, 84. [Google Scholar] [CrossRef] [PubMed]
- Niederer, R.; Al-Janabi, A.; Lightman, S.L.; Tomkins-Netzer, O. Serum Angiotensin-Converting Enzyme Has a High Negative Predictive Value in the Investigation for Systemic Sarcoidosis. Am. J. Ophthalmol. 2018, 194, 82–87. [Google Scholar] [CrossRef] [PubMed]
- Csongrádi, A.; Enyedi, A.; Takács, I.; Végh, T.; Mányiné, I.S.; Pólik, Z.; Altorjay, I.T.; Balla, J.; Balla, G.; Édes, I.; et al. Optimized angiotensin-converting enzyme activity assay for the accurate diagnosis of sarcoidosis. Clin. Chem. Lab. Med. (CCLM) 2018, 56, 1117–1125. [Google Scholar] [CrossRef]
- Eurelings, L.E.M.; Miedema, J.R.; Dalm, V.A.S.H.; Van Daele, P.L.A.; Van Hagen, P.M.; Van Laar, J.A.M.; Dik, W.A. Sensitivity and specificity of serum soluble interleukin-2 receptor for diagnosing sarcoidosis in a population of patients suspected of sarcoidosis. PLoS ONE 2019, 14, e0223897. [Google Scholar] [CrossRef]
- Baba, Y.; Kubo, T.; Yamanaka, S.; Ochi, Y.; Hirota, T.; Yamasaki, N.; Ohnishi, H.; Kubota, T.; Yokoyama, A.; Kitaoka, H. Reconsideration of the cut-off value of angiotensin-converting enzyme for screening of sarcoidosis in Japanese patients. J. Cardiol. 2019, 74, 507–511. [Google Scholar] [CrossRef]
- Ishihara, M.; Meguro, A.; Ishido, M.; Takeuchi, M.; Shibuya, E.; Mizuki, N. Usefulness of Combined Measurement of Serum Soluble IL-2R and Angiotensin-Converting Enzyme in the Detection of Uveitis Associated with Japanese Sarcoidosis. Clin. Ophthalmol. 2020, 14, 2311–2317. [Google Scholar] [CrossRef]
- Enyedi, A.; Csongrádi, A.; Altorjay, I.T.; Beke, G.L.; Váradi, C.; Enyedi, E.E.; Kiss, D.R.; Bányai, E.; Kalina, E.; Kappelmayer, J.; et al. Combined application of angiotensin converting enzyme and chitotriosidase analysis improves the laboratory diagnosis of sarcoidosis. Clin. Chim. Acta 2019, 500, 155–162. [Google Scholar] [CrossRef] [PubMed]
- Komoriyama, H.; Omote, K.; Nagai, T.; Kato, Y.; Nagano, N.; Koyanagawa, K.; Kamiya, K.; Konishi, T.; Sato, T.; Kobayashi, Y.; et al. Lower left ventricular ejection fraction and higher serum angiotensin-converting enzyme activity are associated with histopathological diagnosis by endomyocardial biopsy in patients with cardiac sarcoidosis. Int. J. Cardiol. 2020, 321, 113–117. [Google Scholar] [CrossRef] [PubMed]
- Suzuki, K.; Namba, K.; Mizuuchi, K.; Iwata, D.; Ito, T.; Hase, K.; Kitaichi, N.; Ishida, S. Validation of systemic parameters for the diagnosis of ocular sarcoidosis. Jpn. J. Ophthalmol. 2021, 65, 191–198. [Google Scholar] [CrossRef] [PubMed]
- Papasavvas, I.; Gehrig, B.; Herbort, C.P., Jr. The Comparative Value of Serum Angiotensin Converting Enzyme (ACE) and Lysozyme and the Use of Polyclonal Antibody Activation in the Work-up of Ocular Sarcoidosis. Diagnostics 2021, 11, 608. [Google Scholar] [CrossRef] [PubMed]
- Sunaga, N.; Koga, Y.; Hachisu, Y.; Yamaguchi, K.; Aikawa, M.; Kasahara, N.; Miura, Y.; Tsurumaki, H.; Yatomi, M.; Sakurai, R.; et al. Role of Neuron-Specific Enolase in the Diagnosis and Disease Monitoring of Sarcoidosis. Can. Respir. J. 2022, 2022, 3726395. [Google Scholar] [CrossRef]
- Wang, W.; Ma, Y.; Zhang, Y.; Lin, J.; He, J.; Nong, Y.; Zhang, X.; Jia, Y. Diagnostic and Staging Value of Serum Angiotensin-Converting Enzyme in Sarcoidosis. Comput. Math. Methods Med. 2022, 2022, 4657502. [Google Scholar] [CrossRef]
- Di Francesco, A.M.; Verrecchia, E.; Sicignano, L.L.; Massaro, M.G.; Antuzzi, D.; Covino, M.; Pasciuto, G.; Richeldi, L.; Manna, R. The Use of Chitotriosidase as a Marker of Active Sarcoidosis and in the Diagnosis of Fever of Unknown Origin (FUO). J. Clin. Med. 2021, 10, 5283. [Google Scholar] [CrossRef]
- El Jammal, T.; Jamilloux, Y.; Gerfaud-Valentin, M.; Richard-Colmant, G.; Weber, E.; Bert, A.; Androdias, G.; Sève, P. Challenging Mimickers in the Diagnosis of Sarcoidosis: A Case Study. Diagnostics 2021, 11, 1240. [Google Scholar] [CrossRef]
- Baughman, R.P.; Teirstein, A.S.; Judson, M.A.; Rossman, M.D.; Yeager, H., Jr.; Bresnitz, E.A.; DePalo, L.; Hunninghake, G.; Iannuzzi, M.C.; Johns, C.J.; et al. Clinical Characteristics of Patients in a Case Control Study of Sarcoidosis. Am. J. Respir. Crit. Care Med. 2001, 164, 1885–1889. [Google Scholar] [CrossRef]
- Deeks, J.J.; Altman, D.G. Diagnostic tests 4: Likelihood ratios. BMJ 2004, 329, 168–169. [Google Scholar] [CrossRef]
- Springer-Wanner, C.; Brauns, T. Okuläre Sarkoidose. Zeitschrift Für Rheumatol. 2017, 76, 391–397. [Google Scholar] [CrossRef] [PubMed]
- Febvay, C.; Kodjikian, L.; Maucort-Boulch, D.; Perard, L.; Iwaz, J.; Jamilloux, Y.; Broussolle, C.; Burillon, C.; Seve, P. Clinical features and diagnostic evaluation of 83 biopsy-proven sarcoid uveitis cases. Br. J. Ophthalmol. 2015, 99, 1372–1376. [Google Scholar] [CrossRef] [PubMed]
- Studdy, P.R.; Bird, R. Serum Angiotensin Converting Enzyme in Sarcoidosis—Its Value in Present Clinical Practice. Ann. Clin. Biochem. Int. J. Lab. Med. 1989, 26, 13–18. [Google Scholar] [CrossRef] [PubMed]
- Ma, J.; Yin, H.; Hao, X.; Sha, W.; Cui, H. Development of a random forest model to classify sarcoidosis and tuberculosis. Am. J. Transl. Res. 2021, 13, 6166–6174. [Google Scholar]
- Alhenc-Gelas, F.; Richard, J.; Courbon, D.; Warnet, J.M.; Corvol, P. Distribution of plasma angiotensin I-converting enzyme levels in healthy men: Relationship to environmental and hormonal parameters. J. Lab. Clin. Med. 1991, 117, 33–39. [Google Scholar]
- Samokhodskaya, L.M.; Jain, M.S.; Kurilova, O.V.; Bobkov, A.P.; Kamalov, A.A.; Dudek, S.M.; Danilov, S.M. Phenotyping Angiotensin-Converting Enzyme in Blood: A Necessary Approach for Precision Medicine. J. Appl. Lab. Med. 2021, 6, 1179–1191. [Google Scholar] [CrossRef]
- Rigat, B.; Hubert, C.; Alhenc-Gelas, F.; Cambien, F.; Corvol, P.; Soubrier, F. An insertion/deletion polymorphism in the angiotensin I-converting enzyme gene accounting for half the variance of serum enzyme levels. J. Clin. Investig. 1990, 86, 1343–1346. [Google Scholar] [CrossRef]
- Danser, A.J.; Batenburg, W.W.; Meiracker, A.H.V.D.; Danilov, S.M. ACE phenotyping as a first step toward personalized medicine for ACE inhibitors. Why does ACE genotyping not predict the therapeutic efficacy of ACE inhibition? Pharmacol. Ther. 2007, 113, 607–618. [Google Scholar] [CrossRef]
- Song, G.G.; Kim, J.-H.; Lee, Y.H. Associations between the angiotensin-converting enzyme insertion/deletion polymorphism and susceptibility to sarcoidosis: A meta-analysis. J. Renin-Angiotensin-Aldosterone Syst. 2013, 16, 219–226. [Google Scholar] [CrossRef]
- Fløe, A.; Hoffmann, H.J.; Nissen, P.H.; Møller, H.J.; Hilberg, O. Genotyping increases the yield of angiotensin-converting enzyme in sarcoidosis—A systematic review. Dan. Med, J. 2014, 61, A4815. [Google Scholar]
- Biller, H.; Zissel, G.; Ruprecht, B.; Nauck, M.; Grawitz, A.B.; Muller-Quernheim, J. Genotype-corrected reference values for serum angiotensin-converting enzyme. Eur. Respir. J. 2006, 28, 1085–1091. [Google Scholar] [CrossRef] [PubMed]
- Stokes, G.S.; Monaghan, J.C.; Schrader, A.P.; Glenn, C.L.; Ryan, M.; Morris, B.J. Influence of angiotensin converting enzyme (ACE) genotype on interpretation of diagnostic tests for serum ACE activity. Aust. N. Z. J. Med. 1999, 29, 315–318. [Google Scholar] [CrossRef] [PubMed]
- Kruit, A.; Grutters, J.C.; Gerritsen, W.B.; Kos, S.; Wodzig, W.K.; Bosch, J.M.V.D.; Ruven, H.J. ACE I/D-corrected Z-scores to identify normal and elevated ACE activity in sarcoidosis. Respir. Med. 2007, 101, 510–515. [Google Scholar] [CrossRef] [PubMed]
- Danilov, S.M.; Kurilova, O.V.; Sinitsyn, V.E.; Kamalov, A.A.; Garcia, J.G.N.; Dudek, S.M. Predictive potential of ACE phenotyping in extrapulmonary sarcoidosis. Respir. Res. 2022, 23, 211. [Google Scholar] [CrossRef]
- Alia, P.; Mañá, J.; Capdevila, O.; Alvarez, A.; Navarro, M.A. Association between ACE gene I/D polymorphism and clinical presentation and prognosis of sarcoidosis. Scand. J. Clin. Lab. Investig. 2005, 65, 691–698. [Google Scholar] [CrossRef]
- Rømer, F.K. Clinical and biochemical aspects of sarcoidosis. With special reference to angiotensin-converting enzyme (ACE). Acta Med. Scand. Suppl. 1984, 690, 3–96. [Google Scholar]
- Brice, E.A.; Friedlander, W.; Bateman, E.D.; Kirsch, B.E. Serum Angiotensin-Converting Enzyme Activity, Concentration, and Specific Activity in Granulomatous Interstitial Lung Disease, Tuberculosis, and COPD. Chest 1995, 107, 706–710. [Google Scholar] [CrossRef]
- Maier, L.A.; Raynolds, M.V.; Young, D.A.; Barker, E.A.; Newman, L.S. Angiotensin-1 Converting Enzyme Polymorphisms in Chronic Beryllium Disease. Am. J. Respir. Crit. Care Med. 1999, 159, 1342–1350. [Google Scholar] [CrossRef]
- Ryder, K.W.; Jay, S.J.; Kiblawi, S.O.; Hull, M.T. Serum angiotensin converting enzyme activity in patients with histoplasmosis. JAMA 1983, 249, 1888–1889. [Google Scholar] [CrossRef]
- Khurana, V.; Goswami, B. Angiotensin converting enzyme (ACE). Clin. Chim. Acta 2021, 524, 113–122. [Google Scholar] [CrossRef]
- Kocak, N.D.; Gungor, S.; Akturk, U.A.; Yalcinsoy, M.; Kavas, M.; Oztas, S.; Akkaya, M.E.; Aksoy, E.; Agca, M.C.; Duman, D.; et al. Analysis of Age Distribution and Disease Presentation of 1269 Patients with Sarcoidosis. Eurasian J. Med. 2017, 49, 161–166. [Google Scholar] [CrossRef] [PubMed]
- Birnbaum, A.D.; Rifkin, L.M. Sarcoidosis: Sex-Dependent Variations in Presentation and Management. J. Ophthalmol. 2014, 2014, 236905. [Google Scholar] [CrossRef] [PubMed]
- Khoury, F.; Teasdale, P.R.; Smith, L.; Jones, O.G.; Carter, J.R. Angiotensin-converting enzyme in sarcoidosis: A British study. Br. J. Dis. Chest 1979, 73, 382–388. [Google Scholar] [CrossRef]
- Yeager, H.; Williams, M.C.; Beekman, J.F.; Bayly, T.C.; Beaman, B.L. Sarcoidosis: Analysis of cells obtained by bronchial lavage. Am. Rev. Respir. Dis. 1977, 116, 951–955. [Google Scholar] [CrossRef]
- Valeyre, D.; Soler, P.; Clerici, C.; Pre, J.; Battesti, J.P.; Georges, R.; Hance, A.J. Smoking and pulmonary sarcoidosis: Effect of cigarette smoking on prevalence, clinical manifestations, alveolitis, and evolution of the disease. Thorax 1988, 43, 516–524. [Google Scholar] [CrossRef]
- Mordelet-Dambrine, M.S.; Stanislas-Leguern, G.M.; Huchon, G.J.; Baumann, F.C.; Marsac, J.H.; Chrétien, J. Elevation of the bronchoalveolar concentration of angiotensin I converting enzyme in sarcoidosis. Am. Rev. Respir. Dis. 1982, 126, 472–475. [Google Scholar] [CrossRef]
- Sugiyama, Y.; Yotsumoto, H.; Okabe, T.; Takaku, F. Measurement of Angiotensin-Converting Enzyme Activity in Intact Human Alveolar Macrophages and Effect of Smoking. Respiration 1988, 53, 153–157. [Google Scholar] [CrossRef]
- Hinman, L.M.; Stevens, C.; Matthay, R.A.; Gee, J.B.L. Angiotensin Convertase Activities in Human Alveolar Macrophages: Effects of Cigarette Smoking and Sarcoidosis. Science 1979, 205, 202–203. [Google Scholar] [CrossRef]
- Krasowski, M.D.; Savage, J.; Ehlers, A.; Maakestad, J.; Schmidt, G.A.; La’Ulu, S.L.; Rasmussen, N.N.; Strathmann, F.G.; Genzen, J.R. Ordering of the Serum Angiotensin-Converting Enzyme Test in Patients Receiving Angiotensin-Converting Enzyme Inhibitor Therapy: An Avoidable but Common Error. Chest 2015, 148, 1447–1453. [Google Scholar] [CrossRef]
- Selroos, O.B. Value of biochemical markers in serum for determination of disease activity in sarcoidosis. Sarcoidosis 1984, 1, 45–49. [Google Scholar]
- Grosso, S.; Margollicci, M.A.; Bargagli, E.; Buccoliero, Q.R.; Perrone, A.; Galimberti, D.; Morgese, G.; Balestri, P.; Rottoli, P. Serum levels of chitotriosidase as a marker of disease activity and clinical stage in sarcoidosis. Scand. J. Clin. Lab. Investig. 2004, 64, 57–62. [Google Scholar] [CrossRef] [PubMed]
- Judson, M.A. Corticosteroids in Sarcoidosis. Rheum. Dis. Clin. North Am. 2016, 42, 119–135. [Google Scholar] [CrossRef] [PubMed]
- Grutters, J.C.; Bosch, J.M.M.V.D. Corticosteroid treatment in sarcoidosis. Eur. Respir. J. 2006, 28, 627–636. [Google Scholar] [CrossRef] [PubMed]
- Lieberman, J. The specificity and nature of serum-angiotensin-converting enzyme (serum ACE) elevations in sarcoidosis. Ann. N. Y. Acad. Sci. 1976, 278, 488–497. [Google Scholar] [CrossRef] [PubMed]
- Yotsumoto, H. Longitudinal Observations of Serum Angiotensin-converting Enzyme Activity in Sarcoidosis with and Without Treatment. Chest 1982, 82, 556–559. [Google Scholar] [CrossRef] [PubMed]

| Author | Year | Country | Criterial | Diseased Region | Method | Sarcoidosis | Control | Design | Cut-Off | TP | FP | FN | TN | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Case | Age | Gender (M/F) | sACE | Unit | Control | Age | Gender (M/F) | sACE | Unit | ||||||||||||
| Lieberman et al. [26] | 1975 | US | Histology | NA | Spectrophotometry | 17 | NA | NA | 13.65 ± 2.26 | U/mL | 296 | NA | NA | NA | U/mL | NA | 11.6 | 15 | 9 | 2 | 287 |
| Silverstein et al. [27] | 1976 | US | NA | NA | Spectrophotometry | 58 | 48.3 ± 4.8 | NA | 48.3 + 4.8 | nmol/min/mL | 256 | NA | NA | NA | nmol/min/mL | NA | 30.48 | 20 | 15 | 38 | 241 |
| Studdy et al. [28] | 1978 | UK | Histology | NA | Spectrophotometry | 90 | NA | NA | 58 ± 24 | nmol/min/mL | 194 | NA | NA | NA | nmol/min/mL | NA | 52 | 45 | 14 | 45 | 180 |
| Turton et al. [29] | 1979 | UK | Histology | NA | Spectrophotometry | 72 | 37(19–67) | 31/41 | 35.6 ± 14.4 | U/mL | 87 | NA | NA | NA | U/mL | NA | 41 | 21 | 3 | 51 | 84 |
| Lieberman et al. [30] | 1979 | US | NA | NA | Spectrophotometry | 391 | 39.6 ± 10 | NA | NA | U/mL | 1150 | NA | NA | NA | U/mL | NA | 35 | 226 | 30 | 165 | 1120 |
| Rohrbach et al. [31] | 1979 | US | Histology | NA | Radiochemistry | 42 | 44.8 | 22/20 | 71.9 ± 19.2 | U/mL | 60 | NA | NA | 40.2 ± 8.6 | U/mL | R | 57 | 33 | 3 | 9 | 57 |
| Rohatgi et al. [32] | 1980 | US | Histology | NA | Radiochemistry | 55 | 17–69 | NA | NA | mU/mL | 122 | NA | NA | NA | mU/mL | NA | 137.5 | 35 | 7 | 20 | 115 |
| Ryder et al. [33] | 1981 | US | Clinical findings and/or histology | NA | Spectrophotometry | 40 | NA | NA | 44 ± 8 | kU/L | 60 | NA | NA | NA | kU/L | P | 35 | 36 | 5 | 4 | 55 |
| Ainslie et al. [35] | 1985 | South Africa | Histology | NA | Spectrophotometry | 303 | NA | NA | NA | nmol/min/mL | 210 | NA | NA | NA | nmol/min/mL | R | 54 | 176 | 34 | 127 | 176 |
| Baarsma et al. [36] | 1987 | Netherlands | Clinical and biochemical findings | Ocular sarcoidosis | Spectrophotometry | 12 | NA | NA | NA | U/L | 209 | NA | NA | NA | U/L | NA | 50 | 10 | 10 | 2 | 199 |
| Bunting et al. [37] | 1987 | Canada | Clinical findings or histology | NA | Fluorimetry | 120 | NA | NA | NA | U/L | 74 | NA | NA | NA | U/L | NA | 50 | 76 | 5 | 44 | 69 |
| Power et al. [38] | 1995 | US | Histology | Ocular sarcoidosis | Spectrophotometry | 22 | 35 (22–64) | 10/12 | NA | U/L | 70 | 39 (17–58) | 29/41 | NA | U/L | R | 52 | 16 | 12 | 6 | 58 |
| Khan et al. [39] | 1998 | Pakistan | Clinical findings and/or histology | NA | Spectrophotometry | 51 | NA | NA | 104.44 | IU/L | 62 | NA | NA | NA | IU/L | R | 52 | 44 | 24 | 7 | 38 |
| Bons et al. [40] | 2007 | Netherlands | WASOG | NA | Spectrophotometry | 35 | 45.67 ± 8.8 | 18/17 | 22.0 (16.0–24.0) | U/L | 35 | 47.37 ± 9.8 | 16/19 | 13.5 (12.0–17.8) | U/L | p | 16.5 | 25 | 10 | 10 | 25 |
| Kawaguchi et al. [41] | 2007 | Japan | Histology | Ocular sarcoidosis | NA | 60 | NA | NA | NA | NA | 86 | NA | NA | NA | NA | R | NA | 35 | 4 | 25 | 82 |
| Smet et al. [42] | 2010 | Belgium | Histology | NA | Spectrophotometry | 36 | NA | 21/15 | 48 (39–80) | U/L | 117 | NA | 65/52 | 27 (19–40) | U/L | R | 34 | 30 | 39 | 6 | 78 |
| Gungor et al. [43] | 2015 | Turkey | Histology | NA | Spectrophotometry | 48 | 44.29 ± 10.90 | 9/39 | 49.50 ± 41.04 | U/L | 20 | 38.05 ± 8.36 | 10/10 | 25.44 ± 13.38 | U/L | P | NA | 35 | 8 | 13 | 12 |
| Gundlach et al. [17] | 2016 | Germany | IWOS | Ocular sarcoidosis | Spectrophotometry | 41 | NA | NA | NA | U/mL | 220 | NA | NA | NA | U/mL | R | 82 | 9 | 1 | 32 | 219 |
| Hakan et al. [44] | 2017 | Netherlands | IWOS | Ocular sarcoidosis | Spectrophotometry | 37 | NA | NA | NA | U/L | 212 | NA | NA | NA | U/L | R | 51 | 20 | 64 | 17 | 148 |
| Uysal et al. [45] | 2018 | Turkey | WASOG | NA | ELISA | 59 | NA | NA | NA | mg/mL | 25 | 46.1 ± 8.4 | 12/13 | NA | mg/mL | NA | 5.37 | 52 | 7 | 2 | 23 |
| Niederer et al. [46] | 2018 | UK | IWOS | NA | NA | 110 | NA | NA | 32 (21–47) | NA | 925 | NA | NA | NA | NA | P | 52 | 85 | 111 | 25 | 814 |
| Csongrádi et al. [47] | 2018 | Hungary | Histology | NA | Fluorimetry | 40 | 39.0 ± 11.0 | 22/18 | NA | U/L | 11 | 54.0 ± 15.2 | 8/3 | 9.12 ± 2.07 | U/L | P | 21.4 | 9 | 0 | 31 | 11 |
| Eurelings et al. [48] | 2019 | Netherlands | ATS/ERS/WASOG | NA | Spectrophotometry | 101 | 43 (35–52) | 50/51 | 77 (44–109) | U/mL | 88 | 44 (31–57) | 36/52 | 51(31–69) | U/mL | R | 68 | 63 | 21 | 38 | 67 |
| Baba et al. [49] | 2019 | Japan | JSSOG 2015 | NA | Spectrophotometry | 79 | 65.0 (55.0–71.0) | 27/52 | 20.3 (16.0–24.4) | IU/L | 299 | NA | NA | 15.4 (12.8–18.5) | IU/L | R | 17.7 | 53 | 93 | 26 | 206 |
| Ishihara et al. [50] | 2020 | Japan | Clinical findings and/or histology | Ocular sarcoidosis | Spectrophotometry | 52 | 58.8 ± 15.2 | 13/39 | 26.4 ± 9.18 | U/L | 74 | 49.6 ± 16.5 | 40/34 | 13.5 ± 3.83 | U/L | R | NA | 23 | 0 | 29 | 74 |
| Enyedi et al. [51] | 2020 | Hungary | Histology | NA | Fluorimetry | 69 | 40.9 (±12.3) | 30/39 | 11.89 (10.5–13.7) | U/L | 168 | NA | NA | NA | U/L | P | NA | 17 | 0 | 52 | 168 |
| Komoriyama et al. [52] | 2020 | Japan | Histology | NA | Spectrophotometry | 37 | 57 ± 12 | 7/30 | 15.5 ± 7.9 | IU/L | 57 | 61 ± 9 | 12/45 | 12.4 ± 6.9 | IU/L | R | 13.5 | 21 | 26 | 16 | 31 |
| Suzukiet al. [53] | 2021 | Japan | Histology | Ocular sarcoidosis | ELISA | 77 | 54.6 ± 14.8 | NA | NA | U/L | 79 | 43.2 ± 17.8 | NA | NA | U/L | R | 12.7 | 29 | 2 | 48 | 77 |
| Papasavvas et al. [54] | 2021 | Switzerland | IWOS | Ocular sarcoidosis | Spectrophotometry | 37 | 54.52 ± 23.74 | NA | 49.17 ± 29 | U/L | 30 | 41 ± 11.3 | NA | 27.4 ± 15.34 | U/L | R | NA | 10 | 1 | 27 | 29 |
| Sunaga et al. [55] | 2022 | Japan | Histology | NA | Spectrophotometry | 112 | 61(14–86) | 36/78 | 20.2 (0–56.4) | IU/L | 62 | NA | NA | NA | IU/L | R | 21.4 | 46 | 0 | 66 | 62 |
| Wang et al. [56] | 2022 | China | Histology | NA | Spectrophotometry | 70 | 55.94 ± 11:83 | 14/56 | 56:61 ± 30.80 | U/L | 14 | 55.25 ± 16:70 | 8/6 | 28:07 ± 14.11 | U/L | P | 44 | 43 | 1 | 27 | 13 |
| Author | Year | Country | Criterial | Method | Sarcoidosis | Control | Design | Cut-Off | TP | FP | FN | TN | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Number | Age | Gender (M/F) | sACE | Unit | Number | Age | Gender (M/F) | sACE | Unit | |||||||||||
| Lieberman et al. [26] | 1975 | US | Histology | Spectrophotometry | 17 | NA | NA | 13.65 ± 2.26 | U/mL | 6 | NA | NA | NA | U/mL | NA | 11.6 | 15 | 0 | 2 | 6 |
| Turton et al. [29] | 1979 | UK | Histology | Spectrophotometry | 17 | NA | NA | NA | U/mL | 30 | NA | NA | NA | U/mL | NA | 41 | 8 | 2 | 9 | 28 |
| Rohatgi et al. [32] | 1980 | UK | Histology | Radiochemistry | 40 | NA | NA | 177.7 ± 59.7 | U/mL | 15 | NA | NA | NA | U/mL | NA | 137.5 | 34 | 1 | 6 | 14 |
| Klech et al. [34] | 1982 | Austria | Histology | Spectrophotometry | 35 | NA | NA | NA | U/mL | 25 | NA | NA | NA | U/mL | NA | 24 | 27 | 3 | 8 | 22 |
| Ainslie et al. [35] | 1985 | South Africa | Histology | Spectrophotometry | 114 | NA | NA | 100.4 ± 45.7 | nmol/min/mL | 189 | NA | NA | 51.9 ± 19.9 | nmol/min/mL | R | 54 | 105 | 71 | 9 | 118 |
| Popević et al. [15] | 2016 | Serbia | Histology | Spectrophotometry | 230 | NA | NA | 43 (26–62) | U/L | 199 | NA | NA | 30 (20–44) | U/L | NA | 32 | 152 | 92 | 78 | 107 |
| Uysal et al. [45] | 2018 | Turkey | WASOG | ELISA | 20 | 45.15 ± 11.55 | 4/16 | NA | U/L | 39 | 42.4 ± 10.4 | 15/24 | NA | U/L | NA | 26.23 | 17 | 11 | 3 | 28 |
| Lopes et al. [19] | 2019 | Brazil | WASOG | ELISA | 27 | 46 (13.5) | 8/19 | 470.96 (407.81–534.09) | ng/mL | 19 | 56 (18.5) | 7/12 | 337.866 (262.47–413.26) | ng/mL | NA | 270 | 24 | 10 | 3 | 9 |
| Francesco et al. [57] | 2021 | Italy | Histology | ELISA | 33 | 63(56.5–74.5) | 5/28 | 34.0 (26.0–62.0) | UI/L | 19 | 65.0 (56.0–71.0) | NA | NA | UI/L | NA | 65 | 9 | 1 | 24 | 18 |
| Sensitivity | Specificity | PLR | NLR | DOR | Area under the Curve (95% CI) | |
|---|---|---|---|---|---|---|
| Sarcoidosis | 60% | 93% | 8.4 | 0.43 | 19 | 0.84 (0.80–0.87) |
| Ocular sarcoidosis | 48% | 96% | 13.3 | 0.54 | 25 | 0.77 (0.73–0.80) |
| Active sarcoidosis | 76% | 80% | 3.9 | 0.29 | 13 | 0.85 (0.82–0.88) |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Hu, X.; Zou, L.; Wang, S.; Zeng, T.; Li, P.; Shen, Y.; Chen, L. Performance of Serum Angiotensin-Converting Enzyme in Diagnosing Sarcoidosis and Predicting the Active Status of Sarcoidosis: A Meta-Analysis. Biomolecules 2022, 12, 1400. https://doi.org/10.3390/biom12101400
Hu X, Zou L, Wang S, Zeng T, Li P, Shen Y, Chen L. Performance of Serum Angiotensin-Converting Enzyme in Diagnosing Sarcoidosis and Predicting the Active Status of Sarcoidosis: A Meta-Analysis. Biomolecules. 2022; 12(10):1400. https://doi.org/10.3390/biom12101400
Chicago/Turabian StyleHu, Xueru, Li Zou, Shuyan Wang, Tingting Zeng, Ping Li, Yongchun Shen, and Lei Chen. 2022. "Performance of Serum Angiotensin-Converting Enzyme in Diagnosing Sarcoidosis and Predicting the Active Status of Sarcoidosis: A Meta-Analysis" Biomolecules 12, no. 10: 1400. https://doi.org/10.3390/biom12101400
APA StyleHu, X., Zou, L., Wang, S., Zeng, T., Li, P., Shen, Y., & Chen, L. (2022). Performance of Serum Angiotensin-Converting Enzyme in Diagnosing Sarcoidosis and Predicting the Active Status of Sarcoidosis: A Meta-Analysis. Biomolecules, 12(10), 1400. https://doi.org/10.3390/biom12101400






