All reagents employed were of American Chemical Society grade or finer and were used without further purification unless otherwise stated. For compound characterization, 1H NMR spectra were recorded at 400 and 500 MHz with chemical shifts reported in parts per million downfield relative to CHCl3 (7.26) or CH3OH (δ 3.31).1H NMR data are reported in the following order: multiplicity (s, singlet; d, doublet; t, triplet; q, quartet; and m, multiplet), coupling constant (J) in hertz (Hz), and the number of protons. Where appropriate, the multiplicity is preceded by br, indicating that the signal was broad. 13C NMR spectra were recorded at 101 or 126 MHz with chemical shifts reported relative to CHCl3 (77.16) or CH3OH (δ 49.00). High-resolution mass spectrometry (HRMS) analysis was performed using a Q-TOF instrument. Purity was confirmed to be ≥95% by LCMS performed on a Shimadzu LC-20AD system (Shimadzu, ’s-Hertogenbosch, The Netherlands) with a Shimadzu Shim-Pack GISS-HP C18 column (3.0 × 150 mm, 3 μm particle size, Shimadzu, ’s-Hertogenbosch, The Netherlands) at 30 °C and equipped with a UV detector monitoring at 214 and 254 nm. The following solvent system, at a flow rate of 0.5 mL/min, was used: solvent A, 0.1% formic acid in water; solvent B, acetonitrile. Gradient elution was as follows: 95:5 (A/B) for 2 min, 95:5 to 0:100 (A/B) over 13 min, 0:100 (A/B) for 2 min, then reversion back to 95:5 (A/B) over 1 min, 95:5 (A/B) for 2 min. This system was connected to a Shimadzu 8040 triple quadrupole mass spectrometer (ESI ionization, Shimadzu, ’s-Hertogenbosch, The Netherlands). The compounds were purified via preparative HPLC performed on a BESTA-Technik system with a Dr. Maisch Reprosil Gold 120 C18 column (25 × 250 mm, 10 μm particle size, Dr.Maisch, Ammerbuch-Entringen, Germany) and equipped with an ECOM Flash UV detector monitoring at 214 nm. The following solvent system, at a flow rate of 12 mL/min, was used: solvent A: 0.1% TFA in water/acetonitrile 95/5; solvent B: 0.1% TFA in water/acetonitrile 5/95. Gradient elution was as follows: 95:5 (A/B) for 5 min, 95:5 to 0:100 (A/B) over 40 min, 0:100 (A/B) for 5 min, then reversion back to 95:5 (A/B) over 2 min, 95:5 (A/B) for 8 min. HRMS analyses were performed on a Shimadzu Nexera X2 UHPLC system (Shimadzu, ’s-Hertogenbosch, The Netherlands) with a Waters Acquity HSS C18 column (2.1 × 100 mm, 1.8 μm particle size, Waters Chromatography, Etten-Leur, The Netherlands) at 30 °C and equipped with a diode array detector. The following solvent system, at a flow rate of 0.5 mL/min, was used: solvent A, 0.1% formic acid in water; solvent B, 0.1% formic acid in acetonitrile. Gradient elution was as follows: 95:5 (A/B) for 1 min, 95:5 to 15:85 (A/B) over 6 min, 15:85 to 0:100 (A/B) over 1 min, 0:100 (A/B) for 3 min, then reversion back to 95:5 (A/B) for 3 min. This system was connected to a Shimadzu 9030 QTOF mass spectrometer (ESI ionization, Shimadzu, ’s-Hertogenbosch, The Netherlands) calibrated internally with Agilent’s API-TOF reference mass solution kit (5.0 mM purine, 100.0 mM ammonium trifluoroacetate and 2.5 mM hexakis(1H,1H,3H-tetrafluoropropoxy)phosphazine) diluted to achieve a mass count of 10,000.
2.1. Synthetic Procedures
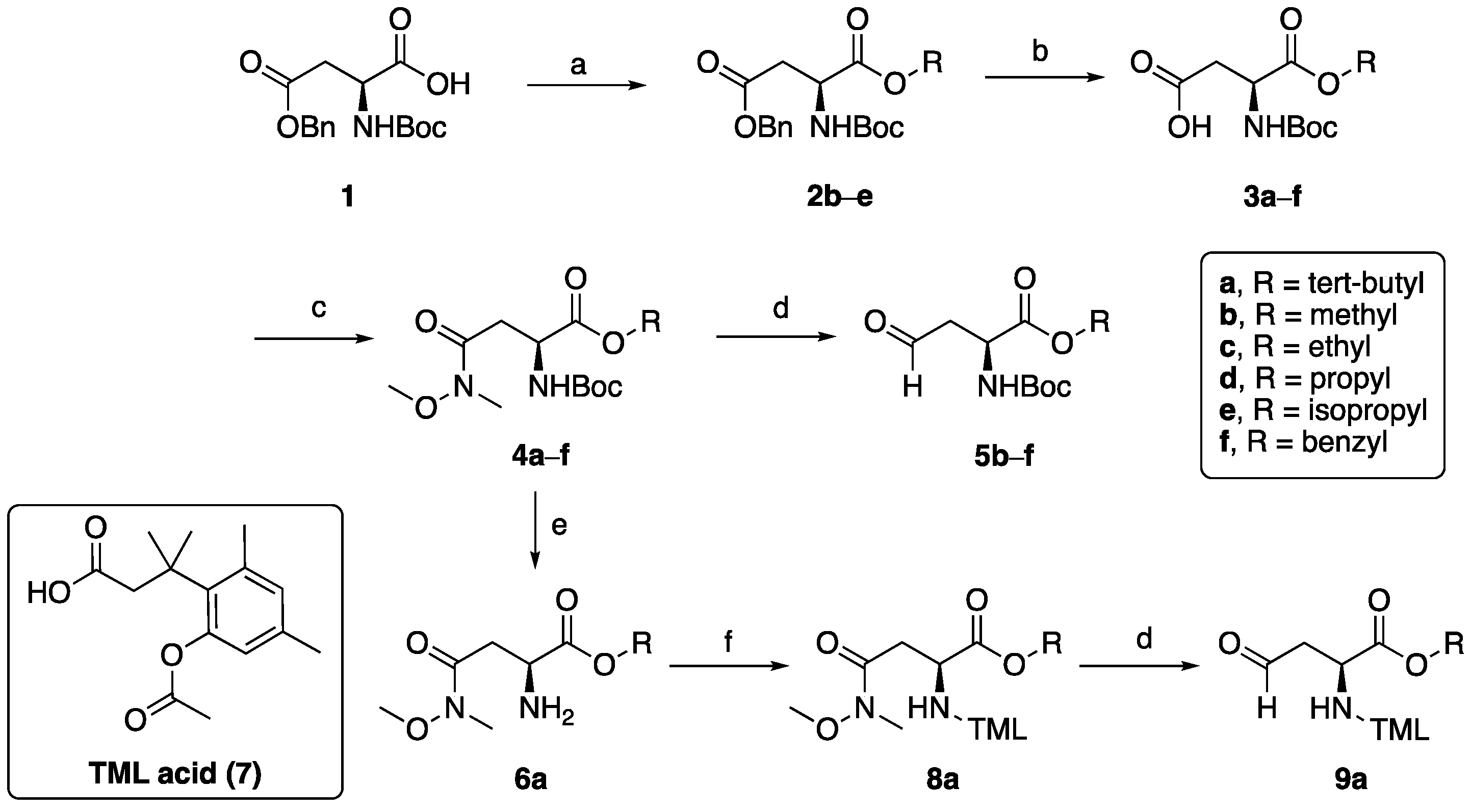
(S)-3-((tert-butoxycarbonyl)amino)-4-isopropoxy-4-oxobutanoic acid (3e). To a stirred suspension of 4-benzyl 1-isopropyl (tert-butoxycarbonyl)-L-aspartate (2e) (1200 mg, 3.3 mmol), 10% Pd-C (120 mg) under H2 atmosphere. After completion of the reaction (TLC), the mixture was filtered through celite, and the filtrate was concentrated under a vacuum to get 3e (900 mg, 99% yield) as a colorless oil. 1H NMR (400 MHz, CDCl3) δ 5.55 (d, J = 8.4 Hz, 1H), 5.11–5.03 (m, 1H), 4.54–4.50 (m, 1H), 3.05 (dd, J = 17.4, 4.5 Hz, 1H), 2.99 (s, 2H), 2.91 (s, 2H), 2.85 (dd, J = 17.3, 4.3 Hz, 1H), 1.46 (s, 9H), 1.25 (dd, J = 10.2, 6.3 Hz, 6H).13C NMR (101 MHz, CDCl3) δ 176.1, 170.5, 155.6, 80.3, 69.7, 50.0, 36.7, 28.3, 21.6. HRMS (ESI): calculated for C12H22NO6 [M + H]+ 276.1447, found 276.1450.
Ethyl-N2-(tert-butoxycarbonyl)-N4-methoxy-N4-methyl-L-asparaginate (4c). To a stirred suspension of 3c (100 mg, 0.4 mmol) in 10 mL CH2Cl2, benzotriazol-1-yloxytris(dimethylamino)phosphonium hexafluorophosphate (BOP) (194 mg, 0.44 mmol) and 0.1 mL Et3N were added and after 10 min N,O-dimethylhydroxylamine hydrogen chloride (43 mg, 0.44) was added followed by another 0.1 mL Et3N. The resulting mixture was stirred at room temperature for 2 h, 10 mL water was added to quench the reaction, the product extracted with CH2Cl2 (10 mL × 3), the organic layer washed with water, brine, dried over NaSO4. The solvent was removed and the crude compound purified by column chromatography to get compound 4c as a colorless oil (960 mg, 80% yield). 1H NMR (400 MHz, CDCl3) δ 5.73 (d, J = 8.8 Hz, 1H), 4.59–4.55 (m, 1H), 4.24–4.19 (m, 2H), 3.70 (s, 3H), 3.18 (s, 3H), 2.97–2.91 (m, 1H), 1.46 (s, 9H), 1.28 (t, J = 7.1 Hz, 3H). LRMS (ESI): calculated for C13H25N2O6 [M + H]+ 305.17, found 305.19.
Propyl-N2-(tert-butoxycarbonyl)-N4-methoxy-N4-methyl-L-asparaginate (4d). Following the procedure described for compound 4c, coupling compound 3d (730 mg, 2.6 mmol) with N,O-dimethylhydroxylamine hydrogen chloride (284 mg, 2.9 mmol) yielded compound 4d as a colourless oil (708 mg, 84% yield).1H NMR (400 MHz, CDCl3) δ 5.70 (d, J = 8.9 Hz, 1H), 4.53 (dt, J = 9.3, 4.4 Hz, 1H), 4.08–4.01 (m, 2H), 3.66 (s, 3H), 3.21–3.15 (m, 1H), 3.12 (s, 3H), 2.91–2.86 (br m, 1H), 1.67–1.56 (m, 2H), 1.41 (s, 9H), 0.90 (t, J = 7.4 Hz, 3H).13C NMR (101 MHz, CDCl3) δ 171.8, 155.8, 80.6, 67.1, 62.1, 49.1, 34.7, 32.4, 21.9, 4.8. HRMS (ESI): calculated for C14H27N2O6 [M + H]+ 319.1869, found 318.1873.
Isopropyl-N2-(tert-butoxycarbonyl)-N4-methoxy-N4-methyl-L-asparaginate (4e). Following the procedure described for compound 4c, coupling compound 3e (800 mg, 2.9 mmol) with N,O-dimethylhydroxylamine hydrogen chloride (312 mg, 3.2 mmol) yielded compound 4e as a colourless oil (760 mg, 82% yield). 1H NMR (400 MHz, CDCl3) δ 5.71 (d, J = 8.8 Hz, 1H), 5.11–5.01 (m, 1H), 4.55–4.50 (m, 1H), 3.70 (s, 3H), 3.25–3.18 (m, 1H), 3.17 (s, 3H), 2.95 –2.89 (br m, 1H), 1.46 (s, 10H), 1.25 (dd, J = 13.5, 6.3 Hz, 6H). 13C NMR (101 MHz, CDCl3) δ 171.1, 155.8, 69.1, 61.3, 50.0, 34.7, 32.0, 28.4, 21.7. HRMS (ESI): calculated for C14H27N2O6 [M + H]+ 319.1869, found 318.1872.
Methyl-(S)-2-((tert-butoxycarbonyl)amino)-4-oxobutanoate (5b). To a solution of methyl N2-(tert-butoxycarbonyl)-N4-methoxy-N4-methyl-L-asparaginate 4b (1000 mg, 4.1 mmol) in CH2Cl2 (20 mL) at −78 °C was added DIBAL-H (1M in hexane, 6.0 mL) and the resulting mixture was stirred at −78 °C for 2 h. An amount of 10 mL water was added to quench the reaction, 10 mL 1M HCl (aq) was added to the solution, and the product was extracted with Et2O. Organic layer wash was combined with H2O, brine, and dried over Na2SO4. The solvent was removed to yield compound 5b as a colorless oil used in the next step without further purification.
Ethyl-(S)-2-((tert-butoxycarbonyl)amino)-4-oxobutanoate (5c). Following the procedure described for compound 5a, compound ethyl N2-(tert-butoxycarbonyl)-N4-methoxy-N4-methyl-L-asparaginate 4c (560 mg, 1.84 mmol) was reduced using DIBAL-H (1M in hexane, 3 mL) to yield compound 5c, which was used in the next step without further purification.
Propyl-(S)-2-((tert-butoxycarbonyl)amino)-4-oxobutanoate (5d). Following the procedure described for compound 5a, compound propyl N2-(tert-butoxycarbonyl)-N4-methoxy-N4-methyl-L-asparaginate 4d (400 mg, 1.3 mmol) was reduced by DIBAL-H (1M in hexane, 2 mL) to yield compound 5d which was used in the next step without further purification.
Isopropyl-(S)-2-((tert-butoxycarbonyl)amino)-4-oxobutanoate (5e). Following the procedure described for compound 5a, compound isopropyl N2-(tert-butoxycarbonyl)-N4-methoxy-N4-methyl-L-asparaginate 4e (450 mg, 1.4 mmol) was reduced by DIBAL-H (1M in hexane, 2 mL) to yield compound 5e which was used in the next step without further purification.
Benzyl-(S)-2-((tert-butoxycarbonyl)amino)-4-oxobutanoate (5f). Following the procedure described for compound 5a, compound benzyl N2-(tert-butoxycarbonyl)-N4-methoxy-N4-methyl-L-asparaginate 4f (370 mg, 1.0mmol) was reduced by DIBAL-H (1M in hexane, 1.2 mL) to yield compound 5f which was used in the next step without further purification.
tert-Butyl-N2-(3-(2-acetoxy-4,6-dimethylphenyl)-3-methylbutanoyl)-N4-methoxy-N4-methyl-L-asparaginate (8a). tert-butyl N2-(tert-butoxycarbonyl)-N4-methoxy- N4-methyl-L-asparaginate 4a (300 mg, 0.9 mmol) in dioxane (5 mL) was selectively deprotected using 4N HCl in dioxanes (10 mL) while stirring for 1 h at 0 °C and 75 min at room temperature. The mixture was concentrated and added to a mixture of TML acid 7 (220 mg, 0.83 mmol, 0.9 eq), Et3N (330 µL, 2.4 mmol, 2.8 eq), and BOP (450 mg, 1 mmol, 1.1 eq) in CH2Cl2 (10 mL). The mixture was stirred overnight, diluted with CH2Cl2 to 100 mL, washed with saturated NaHCO3, water, and brine, dried over sodium sulfate, and concentrated. The crude product was purified by column chromatography (30% EtOAc in petroleum ether, followed by flushing with 20% MeOH in EtOAc) yielding compound 8a (350 mg, 88%) of an off-white powder. 1H NMR (300 MHz, CDCl3) δ 6.77 (d, J = 2.0 Hz, 1H), 6.56 (d, J = 2.1 Hz, 1H), 6.51 (d, J = 8.4 Hz, 1H), 4.66 (dt, J = 8.4, 4.2 Hz, 1H), 3.62 (s, 3H), 3.11 (s, 3H), 2.98 (dd, J = 17.3, 4.2 Hz, 1H), 2.78 (d, J = 13.8 Hz, 1H), 2.64–2.41 (m, 5H), 2.30 (s, 3H), 2.19 (s, 3H), 1.61 (s, 3H), 1.54 (s, 3H), 1.40 (s, 9H). 13C NMR (75 MHz, CDCl3) δ 170.66, 170.19, 170.08, 149.60, 138.14, 136.15, 133.61, 132.47, 123.21, 81.76, 61.15, 49.28, 48.51, 39.54, 34.32, 31.97, 31.64, 27.88, 25.45, 21.92, 20.24. LRMS (ESI): calculated for C25H39N2O7 [M + H]+ 479.28, found 479.35.
tert-Butyl-(S)-2-(3-(2-acetoxy-4,6-dimethylphenyl)-3-methylbutanamido)-4-oxobutanoate (9a). Following the procedure described for compound 5a, compound 8a (110 mg, 0.23 mmol) was reduced by DIBAL-H (1M in hexane, 0.4 mL) to yield compound 9a, which was used in the next step without further purification.
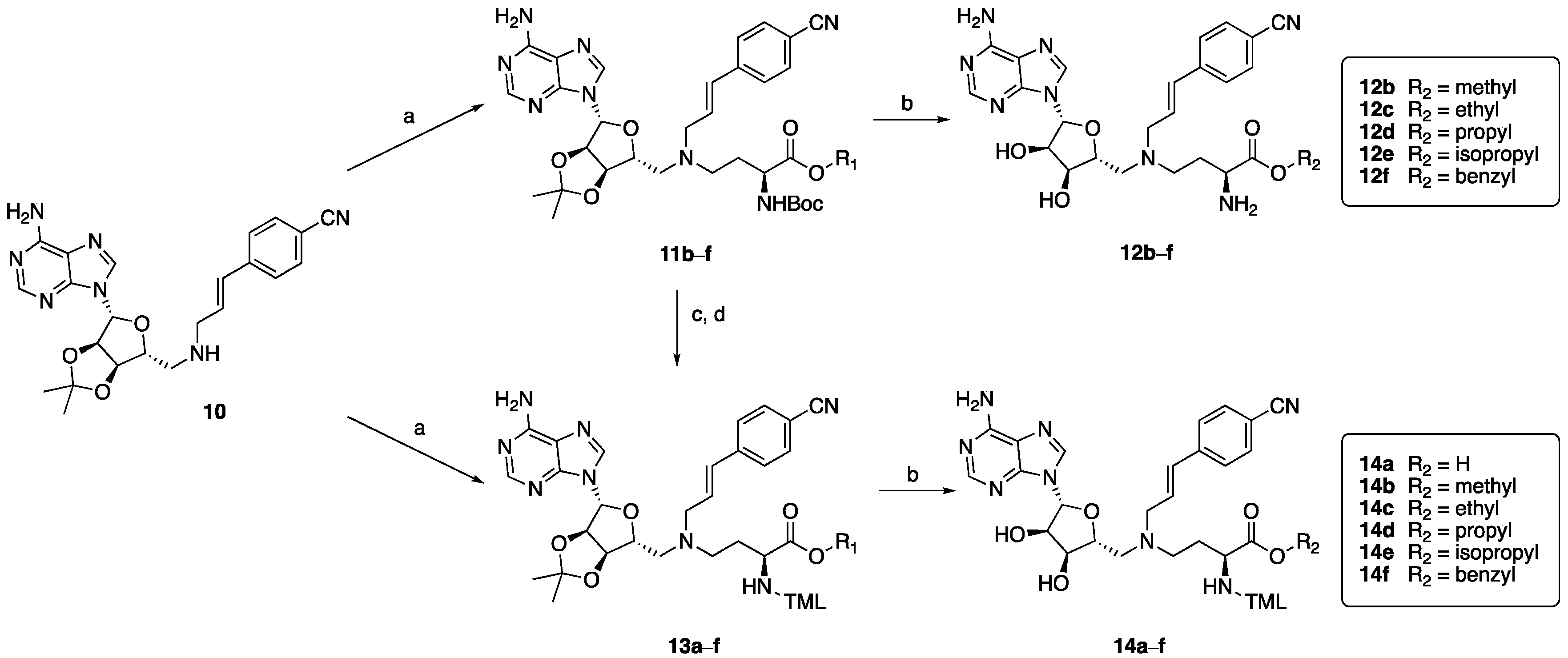
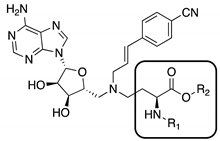
Methyl-(S)-4-((((3aR,4R,6R,6aR)-6-(6-amino-9H-purin-9-yl)-2,2-dimethyl-tetra-ydrofuro[3,4-d][1,3]dioxol-4-yl)methyl)((E)-3-(4-cyanophenyl)allyl)amino)-2-((tert-butoxycarbonyl)amino)butanoate (11b). 4-((E)-3-((((3aR,4R,6R,6aR)-6- (6-amino-9H-purin-9-yl)-2,2-dimethyltetrahydrofuro[3,4-d][1,3]dioxol-4-yl)methyl)amino)prop-1-en-1-yl)benzonitrile 10 (50 mg, 0.11 mmol), 5b (30, 0.13 mmol), NaBH(OAc)3 (36 mg, 0.17 mmol) and AcOH (one drop) were dissolved in 1,2- dichloroethane (DCE, 10 mL) and stirred at room temperature under a N2 atmosphere overnight. The reaction was quenched by adding 1 N NaOH (10 mL), and the product was extracted with CH2Cl2. The combined organic layers were washed with brine and dried over Na2SO4. The solvent was evaporated, and the crude product was purified by column chromatography (5% MeOH in CH2Cl2) to give compound 11b as a white powder (47 mg, 65% yield). 1H NMR (400 MHz, CDCl3) δ 8.21 (s, 1H), 7.94 (s, 1H), 7.49 (d, J = 8.3 Hz, 2H), 7.27 (d, J = 8.3 Hz, 2H), 6.60 (s, 2H), 6.35 (d, J = 16.0 Hz, 1H), 6.27–6.22 (m, 1H), 6.06 (s, 1H), 5.94 (d, J = 8.1 Hz, 1H), 5.45 (d, J = 6.2 Hz, 1H), 5.03–4.95 (m, 1H), 4.41–4.30 (m, 2H), 3.64 (s, 3H), 3.23 (d, J = 6.0 Hz, 2H), 2.79–2.69 (m, 2H), 2.58–2.54 (m, 2H), 2.00–1.89 (m, 1H), 1.82-1.77 (br m, 1H), 1.58 (s, 3H), 1.38 (br s, 12H). 13C NMR (101 MHz, CDCl3) δ 173.3, 155.9, 155.6, 153.0, 149.0, 141.3, 140.1, 132.3, 131.0, 126.7, 120.2, 119.0, 114.4, 110.5, 90.7, 85.7, 83.9, 83.3, 56.6, 56.1, 53.6, 52.2, 50.6, 44.8, 29.2, 28.4, 27.2, 25.4. HRMS (ESI): calculated for C33H43N8O7 [M + H]+ 663.3255, found 663.3262.
Ethyl-(S)-4-((((3aR,4R,6R,6aR)-6-(6-amino-9H-purin-9-yl)-2,2-dimethyltetrahydrofuro[3,4-d][1,3]dioxol-4-yl)methyl)((E)-3-(4-cyanophenyl)allyl)amino)-2-((tert-butoxycarbonyl)amino)butanoate (11c). Following the procedure described for compound 11b, coupling compound 10 (50 mg, 0.11 mmol) with 5c (32 mg, 0.13 mmol) afforded compound 11c as a white powder (53 mg, 72% yield). 1H NMR (400 MHz, CDCl3) δ 8.15 (s, 1H), 7.91 (s, 1H), 7.46 (d, J = 8.3 Hz, 2H), 7.24 (d, J = 8.3 Hz, 2H), 6.58 (s, 2H), 6.32 (d, J = 16.0 Hz, 1H), 6.26–6.16 (br, 1H), 6.01 (s, 1H), 5.85 (d, J = 8.0 Hz, 1H), 5.39 (t, J = 8.2 Hz, 2H), 4.95-4.89 (m, 2H), 4.36–4.17 (m, 2H), 3.74–3.51 (m, 6H), 3.43 (s, 4H), 3.29–3.03 (m, 4H), 2.80–2.52 (m, 6H), 2.49 (s, 5H), 1.83-1.64 (m, 3H), 1.53 (s, 3H), 1.34 (br d, J = 7.8 Hz, 15H). 13C NMR (101 MHz, CDCl3) δ 172.2, 156.1, 155.8, 153.0, 148.9, 141.3, 132.3, 126.7, 120.2, 114.4, 110.4, 90.6, 85.6, 83.9, 83.2, 68.8, 65.0, 59.7, 56.8, 56.0, 52.4, 51.0, 44.8, 29.3, 28.3, 25.4, 21.7. HRMS (ESI): calculated for C33H43N8O7 [M + H]+677.3411, found 677.3420.
Propyl-(S)-4-((((3aR,4R,6R,6aR)-6-(6-amino-9H-purin-9-yl)-2,2-dimethyl-tetrahydrofuro[3,4-d][1,3]dioxol-4-yl)methyl)((E)-3-(4-cyanophenyl)allyl)amino)-2-((tert-butoxycarbonyl)amino)butanoate (11d). Following the procedure described for compound 11b, coupling compound 10 (50 mg, 0.11 mmol) with 5d (34 mg, 0.13 mmol) afforded compound 11d as a white powder (46 mg, 60% yield). 1H NMR (400 MHz, CDCl3) δ 8.18 (s, 1H), 7.93 (s, 1H), 7.48 (d, J = 8.3 Hz, 2H), 7.26 (d, J = 8.3 Hz, 2H), 6.55 (s, 2H), 6.34 (d, J = 15.9 Hz, 1H), 6.27–6.17 (m, 1H), 6.03 (s, 1H), 5.88 (d, J = 8.1 Hz, 1H), 5.41 (d, J = 5.6 Hz, 2H), 4.96 (dd, J = 6.3, 3.7 Hz, 1H), 4.33 (t, J = 8.1 Hz, 2H), 3.98 (t, J = 6.7 Hz, 2H), 3.64 (d, J = 2.7 Hz, 1H), 3.59 (d, J = 3.1 Hz, 1H), 3.26–3.19 (m, 2H), 3.11 (d, J = 6.8 Hz, 1H), 2.79–2.50 (m, 8H), 2.02–1.65 (m, 4H), 1.62-1.52 (m, 6H), 1.39–1.34 (m, 19H). 13C NMR (101 MHz, CDCl3) δ 172.8, 155.9, 153.0, 149.0, 141.3, 132.3, 130.9, 126.7, 120.1, 119.0, 114.4, 110.5, 90.6, 85.6, 83.9, 79.6, 66.6, 65.1, 59.6, 52.31, 44.8, 28.4, 25.4, 21.8. HRMS (ESI): calculated for C33H43N8O7 [M + H]+ 691.3568, found 691.3573.
Isopropyl-(S)-4-((((3aR,4R,6R,6aR)-6-(6-amino-9H-purin-9-yl)-2,2-dimethyl-tetrahydrofuro[3,4-d][1,3]dioxol-4-yl)methyl)((E)-3-(4-cyanophenyl)allyl)amino)-2-((tert-butoxycarbonyl)amino)butanoate (11e). Following the procedure described for compound 11b, coupling compound 10 (50 mg, 0.11 mmol) with 5e (34 mg, 0.13 mmol) afforded compound 11e as a white powder (47 mg, 62% yield). 1H NMR (400 MHz, CDCl3) δ 8.16 (s, 1H), 7.92 (s, 1H), 7.45 (d, J = 8.3 Hz, 2H), 7.24 (d, J = 8.4 Hz, 2H), 6.62 (br s, 2H), 6.32 (br s, 1H), 6.24-6.16 (m, 1H), 6.04–5.99 (m, 1H), 5.91 (d, J = 8.1 Hz, 1H), 5.40 (t, J = 8.1 Hz, 2H), 4.33-4.25(m, 2H), 3.61 (d, J = 2.3 Hz, 1H), 3.56 (d, J = 3.6 Hz, 2H), 3.44 (s, 3H), 3.20 (t, J = 5.6 Hz, 2H), 3.09 (d, J = 4.8 Hz, 1H), 2.78–2.52 (m, 6H), 2.49 (s, 3H), 1.85–1.62 (m, 3H), 1.53 (s, 3H), 1.34 (br s, 20H). 13C NMR (101 MHz, CDCl3) δ 172.7, 156.1, 153.0, 132.29, 141.3, 132.3, 130.9, 126.6, 119.0, 114.3, 110.4, 90.6, 85.6, 83.9, 83.2, 59.7, 52.3, 51.0, 44.8, 29.2, 28.3, 27.1, 25.4. HRMS (ESI): calculated for C33H43N8O7 [M + H]+ 691.3568, found 691.3577.
Benzyl-(S)-4-((((3aR,4R,6R,6aR)-6-(6-amino-9H-purin-9-yl)-2,2-dimethyl-tetrahydrofuro[3,4-d][1,3]dioxol-4-yl)methyl)((E)-3-(4-cyanophenyl)allyl)amino)-2-((tert-butoxycarbonyl)amino)butanoate (11f). Following the procedure described for compound 11b, coupling compound 5f (50 mg, 0.11 mmol) with compound 10 (40 mg, 0.13 mmol) afforded compound 11f as a white powder (54 mg, 66% yield). 1H NMR (400 MHz, CDCl3) δ 8.18 (s, 1H), 7.91 (s, 1H), 7.48 (d, J = 8.4 Hz, 2H), 7.25 (s, 7H), 6.48 (s, 2H), 6.02 (s, 1H), 5.92 (d, J = 8.1 Hz, 1H), 5.38 (d, J = 6.4 Hz, 2H), 5.19–4.99 (m, 2H), 4.98–4.90 (m, 1H), 4.38–4.31 (br m, 2H), 3.78–3.68 (m, 2H), 3.66 (s, 1H), 3.60 (d, J = 3.9 Hz, 3H), 3.48 (s, 5H), 3.23-3.17 (m, 2H), 2.79–2.59 (m, 6H), 1.88–1.82 (m, 2H), 1.74-1.69 (m, 2H), 1.56 (s, 3H), 1.38 (br, 12H). 13C NMR (101 MHz, CDCl3) δ 172.6, 156.1, 155.8, 153.0, 149.0, 141.2, 135.5, 132.3, 128.2, 126.7, 120.0, 90.6, 85.6, 83.9, 83.3, 66.9, 65.1, 59.8, 56.6, 56.1, 52.4, 44.8, 28.4, 27.2, 25.4. HRMS (ESI): calculated for C33H43N8O7 [M + H]+ 739.3568, found 739.3571.
Methyl-(S)-2-amino-4-((((2R,3S,4R,5R)-5-(6-amino-9H-purin-9-yl)-3,4-dihydroxy-tetrahydrofuran-2-yl)methyl)((E)-3-(4-cyanophenyl)allyl)amino)butanoate (12b). To a solution of compound 11b (30 mg, 0.045 mmol) in 1 mL of CH2Cl2 was added a mixture of 9 mL TFA and 1 mL H2O, and the solution was stirred for 2 h at room temperature. The mixture was concentrated, and the crude product was purified by preparative HPLC affording compound 12b as a white powder (24mg, 93% yield). 1H NMR (400 MHz, CD3OD) δ 8.47 (s, 1H), 8.33 (s, 1H), 7.69 (d, J = 8.4 Hz, 2H), 7.51 (d, J = 8.5 Hz, 2H), 6.84 (d, J = 15.8 Hz, 1H), 6.49 (dt, J = 15.8, 7.2 Hz, 1H), 6.17 (d, J = 3.4 Hz, 1H), 4.70 (dd, J = 4.8, 3.4 Hz, 1H), 4.60–4.53 (m, 2H), 4.25 (dd, J = 7.4, 5.7 Hz, 1H), 4.14 (d, J = 7.3 Hz, 2H), 3.92–3.85 (m, 1H), 3.84 (s, 3H), 3.74–3.66 (m, 1H), 3.64–3.47 (m, 2H), 2.58–2.47 (m, 1H), 2.46–2.34 (m, 1H). 13C NMR (101 MHz, CD3OD) δ 168.3, 161.84, 161.5, 151.6, 148.2, 139.75, 145.5, 143.0, 139.8, 138.4, 132.3, 127.2, 119.8, 118.191.2, 78.7, 73.5, 72.2, 55.5, 54.9, 52.8, 50.2, 49.8, 24.9. HRMS (ESI): calculated for C25H31N8O5 [M + H]+ 523.2417, found 523.2422.
Ethyl-(S)-2-amino-4-((((2R,3S,4R,5R)-5-(6-amino-9H-purin-9-yl)-3,4-dihydroxytetrahydrofuran-2-yl)methyl)((E)-3-(4-cyanophenyl)allyl)amino)butanoate (12c). Following the procedure described for compound 12b, compound 11c (30 mg, 0.044 mmol) was deprotected and purified, affording compound 12c as a white powder (19 mg, 67% yield). 1H NMR (400 MHz, CD3OD) δ 8.42 (s, 1H), 8.30 (s, 1H), 7.70 (d, J = 8.4 Hz, 2H), 7.50 (d, J = 8.4 Hz, 2H), 6.84 (br d, J = 15.9 Hz, 1H), 6.53–6.42 (m, 1H), 6.15 (d, J = 3.4 Hz, 1H), 4.69 (dd, J = 5.1, 3.5 Hz, 1H), 4.59–4.48 (m, 2H), 4.33–4.25 (m, 2H), 4.21 (t, J = 6.6 Hz, 1H), 4.09 (t, J = 7.2 Hz, 2H), 3.80 (dd, J = 13.9, 9.8 Hz, 1H), 3.65–3.61 (dd, J = 13.2, 5.8 Hz, 1H), 3.56–3.44 (m, 2H), 2.52–2.44 (m, 1H), 2.41–2.30 (m, 1H), 1.30 (t, J = 7.1 Hz, 3H). 13C NMR (101 MHz, CD3OD) δ 167.9, 161.6, 152.5, 148.3, 139.8, 138.0, 132.3, 127.2, 121.0, 119.7, 118.1, 111.7, 91.0, 78.8, 73.4, 72.2, 62.9, 55.5, 55.0, 50.4, 49.9, 25.0. HRMS (ESI): calculated for C26H33N8O5 [M + H]+ 537.2574, found 537.2579.
Propyl-(S)-2-amino-4-((((2R,3S,4R,5R)-5-(6-amino-9H-purin-9-yl)-3,4-dihydroxy-tetrahydrofuran-2-yl)methyl)((E)-3-(4-cyanophenyl)allyl)amino)butanoate (12d). Following the procedure described for compound 12b, compound 11d (30 mg, 0.043 mmol) was deprotected and purified, affording compound 12d as a white powder (20 mg, 69% yield). 1H NMR (400 MHz, CD3OD) δ 8.46 (s, 1H), 8.33 (s, 1H), 7.69 (d, J = 8.3 Hz, 2H), 7.51 (d, J = 8.3 Hz, 2H), 6.84 (d, J = 15.8 Hz, 1H), 655-6.45 (m, 1H), 6.16 (d, J = 3.4 Hz, 1H), 4.75–4.67 (m, 1H), 4.59–4.53 (m, 2H), 4.28–4.09 (m, 5H), 3.90–3.77 (m, 1H), 3.69 (d, J = 13.4 Hz, 1H), 3.63–3.47 (m, 2H), 2.57–2.33 (m, 2H), 1.73-1.64 (m, 2H), 1.24 (s, 6H), 0.94 (t, J = 7.4 Hz, 3H). 13C NMR (101 MHz, CD3OD) δ 168.0, 152.0, 148.3, 146.1, 142.8, 139.81, 120.6, 118.1, 111.8, 91.1, 78.8, 73.5, 72.2, 68.3, 55.6, 55.0, 29.8, 25.0, 21.4. HRMS (ESI): calculated for C27H35N8O5 [M + H]+551.2730, found 551.2732.
Isopropyl-(S)-2-amino-4-((((2R,3S,4R,5R)-5-(6-amino-9H-purin-9-yl)-3,4-dihydroxytetrahydrofuran-2-yl)methyl)((E)-3-(4-cyanophenyl)allyl)amino)butanoate (12e). Following the procedure described for compound 12b, compound 11e (30 mg, 0.043 mmol) was deprotected and purified, affording compound 12e as a white powder (21 mg, 73% yield). 1H NMR (400 MHz, CD3OD) δ 8.41 (s, 1H), 8.30 (s, 1H), 7.70 (d, J = 8.4 Hz, 2H), 7.50 (d, J = 8.3 Hz, 2H), 6.84 (br d, J = 15.8 Hz, 1H), 6.53–6.42 (m, 1H), 6.14 (d, J = 3.4 Hz, 1H), 5.14–5.07 (m, 1H), 4.70 (dd, J = 5.1, 3.5 Hz, 1H), 4.59–4.54 (m, 1H), 4.54–4.48 (m, 1H), 4.18 (t, J = 6.6 Hz, 1H), 4.07 (d, J = 7.1 Hz, 2H), 2.51–2.29 (m, 2H), 1.29 (t, J = 6.1 Hz, 6H). 13C NMR (101 MHz, CD3OD) δ 167.5, 152.7, 139.8, 137.8, 132.3, 127.2, 119.7, 118.1, 111.7, 91.0, 78.9, 73.4, 72.2, 71.4, 55.1, 50.6, 50.0, 25.1, 20.3. HRMS (ESI): calculated for C27H35N8O5 [M + H]+ 551.2730, found 551.2734.
Benzyl-(S)-2-amino-4-((((2R,3S,4R,5R)-5-(6-amino-9H-purin-9-yl)-3,4-dihydroxy-tetrahydrofuran-2-yl)methyl)((E)-3-(4-cyanophenyl)allyl)amino)butanoate (12f). Following the procedure described for compound 12b, compound 11f (30 mg, 0.041 mmol) was deprotected and purified, affording compound 12f as a white powder (22 mg, 77% yield). 1H NMR (400 MHz, CD3OD) δ 8.41 (s, 1H), 8.29 (s, 1H), 7.48 (s, 1H), 7.46 (s, 1H), 7.43–7.36 (m, 5H), 6.79 (br d, J = 15.9 Hz, 1H), 6.47–6.37 (m, 1H), 6.13 (d, J = 3.4 Hz, 1H), 5.29 (d, J = 2.8 Hz, 2H), 4.67 (dd, J = 5.1, 3.4 Hz, 1H), 4.57–4.45 (m, 2H), 4.28 (t, J = 6.6 Hz, 1H), 4.03 (d, J = 7.2 Hz, 2H), 3.76 (dd, J = 13.9, 9.9 Hz, 1H), 3.60 (br d, J = 12.8 Hz, 1H), 3.53–3.40 (m, 2H), 2.54–2.33 (m, 2H). 13C NMR (101 MHz, CD3OD) δ 167.9, 152.1, 148.2, 134.7, 132.3, 119.7, 118.1, 111.78, 91.0, 78.8, 73.4, 72.2, 68.2, 55.5, 54.9, 50.4, 49.9, 25.0. HRMS (ESI): calculated for C31H34N8O5 [M + H]+598.2652, found 598.2656.
tert-Butyl-(S)-2-(3-(2-acetoxy-4,6-dimethylphenyl)-3-methylbutanamido)-4-((((3aR,4R,6R,6aR)-6-(6-amino-9H-purin-9-yl)-2,2-dimethyltetrahydrofuro[3,4-d][1,3]dioxol-4-yl)methyl)((E)-3-(4-cyanophenyl)allyl)amino)butanoate (13a). Following the procedure described for compound 11b, coupling compound 10 (95 mg, 0.21 mmol, 1.1 eq) with compound 9a (80 mg, 0.19 mmol, 1.0 eq) afforded compound 13a as a yellowish oil (55 mg, 34% yield). 1H NMR (400 MHz, CDCl3) δ 8.24 (s, 1H), 7.90 (s, 1H), 7.55 (d, J = 8.4 Hz, 1H), 7.31 (d, J = 8.4 Hz, 2H), 6.79 (d, J = 2.1 Hz, 1H), 6.58 (d, J = 2.1 Hz, 1H), 6.43–6.19 (m, 3H), 6.14 (s, 2H), 6.04 (d, J = 2.0 Hz, 1H), 5.44 (dd, J = 6.4, 2.0 Hz, 1H), 4.98 (dd, J = 6.4, 3.6 Hz, 1H), 4.38–4.27 (m, 2H), 3.21 (d, J = 6.3 Hz, 2H), 2.77–2.66 (m, 2H), 2.57 (q, J = 13.5 Hz, 2H), 2.49 (s, 3H), 2.31 (s, 3H), 2.20 (s, 3H), 1.85–1.73 (m, 1H), 1.67–1.56 (m, 11H), 1.52–1.38 (m, 16H), 1.26 (s, 9H). 13C NMR (101 MHz, CDCl3) δ 171.15, 170.94, 170.76, 155.65, 153.02, 149.87, 149.12, 141.25, 140.14, 138.46, 136.51, 133.68, 132.73, 132.39, 130.90, 126.69, 124.82, 123.39, 119.05, 114.43, 114.13, 110.59, 90.80, 85.71, 83.96, 83.25, 81.71, 56.83, 56.01, 51.56, 50.84, 49.26, 43.53, 39.80, 31.97, 31.81, 31.69, 30.35, 29.74, 29.55, 29.46, 27.96, 27.94, 27.20, 25.53, 25.43, 21.97, 20.27. HRMS (ESI): calculated for C46H59N8O8 [M + H]+ 851.4450, found 851.4456.
Methyl-(S)-2-(3-(2-acetoxy-4,6-dimethylphenyl)-3-methylbutanamido)-4-((((3aR,4R,6R,6aR)-6-(6-amino-9H-purin-9-yl)-2,2-dimethyltetrahydrofuro[3,4-d][1,3]dioxol-4-yl)methyl)((E)-3-(4-cyanophenyl)allyl)amino)butanoate (13b). To a solution of compound 11b (30 mg, 0.045 mmol) in 9 mL dry of CH2Cl2 was added a 1 mL TFA and the solution was stirred for 1 h at room temperature. The mixture was concentrated. An amount of 5 mL CH2Cl2 was added to the mixture, followed by adding benzotriazol-1-yloxytris(dimethylamino)phosphonium hexafluorophosphate (BOP, 20 mg), 3-(2-acetoxy-4,6-dimethylphenyl)-3-methylbutanoic acid 7 (TML acid, 0.045 mmol, 12 mg), and 0.5 mL Et3N. The reaction mixture was stirred for 2 h at r.t., 10 mL water was added, extracted with CH2Cl2 (10 mL × 3), then the combined organic phase was dried over Na2SO4. The solvent was evaporated, and the crude product was purified by column chromatography (100% EtOAc) to give compound 13b as a white powder (15 mg, 42% yield over 2 steps). 1H NMR (400 MHz, CDCl3) δ 8.20 (s, 1H), 7.91 (s, 1H), 7.54 (d, J = 8.3 Hz, 2H), 7.30 (d, J = 8.5 Hz, 2H), 6.79 (d, J = 1.5 Hz, 1H), 6.58 (d, J = 7.3 Hz, 3H), 6.43–6.32 (m, 2H), 6.27–6.17 (m, 1H), 6.04 (d, J = 2.0 Hz, 1H), 5.43 (dd, J = 6.4, 2.0 Hz, 1H), 4.97 (dd, J = 6.4, 3.4 Hz, 1H), 4.48-4.43 (m, 1H), 4.37-4.32 (m, 1H), 3.62 (s, 3H), 3.19 (d, J = 6.2 Hz, 2H), 2.69 (d, J = 6.8 Hz, 2H), 2.55 (d, J = 4.8 Hz, 2H), 2.48 (s, 3H), 2.41–2.32 (m, 1H), 2.30 (s, 3H), 2.19 (s, 3H), 2.12 (s, 1H), 1.81-1.74 (m, 1H), 1.69–1.55 (m, 9H), 1.38 (s, 3H). 13C NMR (101 MHz, CDCl3) δ 172.5, 171.1, 155.8, 152.7, 149.9, 141.2, 140.1, 138.5, 136.6, 132.7, 133.6, 132.4, 131.0, 130.9, 126.7, 123.4, 114.4, 110.6, 90.9, 85.6, 83.9, 83.2, 56.4, 55.9, 52.2, 50.9, 49.2, 39.8, 31.7, 29.1, 27.2, 25.5, 25.3, 22.0, 20.2. HRMS (ESI): calculated for C43H53N8O8 [M + H]+809.3986, found 809.3991.
Ethyl-(S)-2-(3-(2-acetoxy-4,6-dimethylphenyl)-3-methylbutanamido)-4-((((3aR,4R,6R,6aR)-6-(6-amino-9H-purin-9-yl)-2,2-dimethyltetrahydrofuro[3,4-d][1,3]dioxol-4-yl)methyl)((E)-3-(4-cyanophenyl)allyl)amino)butanoate (13c). Following the procedure described for compound 13b, compound 11c (85 mg, 0.126 mmol) was selectively deprotected and coupled with TML acid 7 (40 mg, 0.15 mmol), affording crude 13c which was used in the next step without further purification.
Propyl-(S)-2-(3-(2-acetoxy-4,6-dimethylphenyl)-3-methylbutanamido)-4-((((3aR,4R,6R,6aR)-6-(6-amino-9H-purin-9-yl)-2,2-dimethyltetrahydrofuro[3,4-d][1,3]dioxol-4-yl)methyl)((E)-3-(4-cyanophenyl)allyl)amino)butanoate (13d). Following the procedure described for compound 13b, compound 11d (31 mg, 0.045 mmol) was selectively deprotected and coupled with TML acid 7 (12 mg, 0.045 mmol), affording crude 13d which was used in the next step without further purification.
Isopropyl-(S)-2-(3-(2-acetoxy-4,6-dimethylphenyl)-3-methylbutanamido)-4-((((3aR,4R,6R,6aR)-6-(6-amino-9H-purin-9-yl)-2,2-dimethyltetrahydrofuro[3,4-d][1,3]dioxol-4-yl)methyl)((E)-3-(4-cyanophenyl)allyl)amino)butanoate (13e). Following the procedure described for compound 13b, compound 11e (31 mg, 0.045 mmol) was selectively deprotected and coupled with TML acid 7 (15 mg, 0.045 mmol), affording compound 13e as a white powder (18 mg, 39% yield over 2 steps). 1H NMR (400 MHz, CDCl3) δ 8.22 (s, 1H), 7.90 (s, 1H), 7.54 (d, J = 8.3 Hz, 2H), 7.30 (d, J = 6.4 Hz, 2H), 6.79 (d, J = 1.6 Hz, 1H), 6.59 (d, J = 1.6 Hz, 1H), 6.43–6.32 (m, 4H), 6.23 (dt, J = 15.9, 6.4 Hz, 1H), 6.04 (d, J = 2.0 Hz, 1H), 5.44 (dd, J = 6.4, 2.0 Hz, 1H), 5.01–4.92 (m, 2H), 4.46–4.30 (m, 2H), 3.20 (d, J = 6.2 Hz, 2H), 2.70 (d, J = 7.9 Hz, 2H), 2.64–2.51 (m, 3H), 2.49 (s, 3H), 2.41–2.36 (m, 2H), 2.30 (s, 3H), 2.20 (s, 3H), 1.83–1.78 (m, 1H), 1.67–1.57 (m, 11H), 1.38 (s, 3H), 1.26 (s, 4H), 1.20 (d, J = 6.3 Hz, 3H), 1.15 (d, J = 6.2 Hz, 3H). 13C NMR (101 MHz, CDCl3) δ 171.6, 171.0, 170.8, 155.7, 152.9, 149.9, 141.2, 140.1, 138.6, 132.7, 132.4, 123.42, 120.2, 119.0, 114.4, 109.8, 90.9, 85.7, 84.0, 83.2, 68.9, 56.7, 56.0, 51.1, 50.8, 49.2, 39.8, 31.7, 29.7, 27.2, 25.5, 25.4, 22.0, 21.7, 20.3. HRMS (ESI): calculated for C45H57N8O8 [M + H]+ 837.4299, found 837.4303.
Benzyl-(S)-2-(3-(2-acetoxy-4,6-dimethylphenyl)-3-methylbutanamido)-4-((((3aR,4R,6R,6aR)-6-(6-amino-9H-purin-9-yl)-2,2-dimethyltetrahydrofuro[3,4-d][1,3]dioxol-4-yl)methyl)((E)-3-(4-cyanophenyl)allyl)amino)butanoate (13f). Following the procedure described for compound 13b, compound 11f (82 mg, 0.13 mmol) was selectively deprotected and coupled with TML acid 7 (34 mg, 0.13 mmol), affording crude 13f which was used in the next step without further purification.
(S)-2-(3-(2-acetoxy-4,6-dimethylphenyl)-3-methylbutanamido)-4-((((2R,3S,4R,5R)-5-(6-amino-9H-purin-9-yl)-3,4-dihydroxytetrahydrofuran-2-yl)methyl)((E)-3-(4-cyanophenyl)allyl)amino)butanoic acid (14a). Following the procedure described for compound 12a, compound 13a (55 mg, 0.065 mmol) was deprotected and purified, affording compound 14a as a white powder (28 mg, 54% yield). 1H NMR (400 MHz, CD3OD) δ 8.47 (s, 1H), 8.35 (s, 1H), 7.72 (d, J = 8.1 Hz, 2H), 7.54 (d, J = 8.1 Hz, 2H), 6.85–6.75 (m, 2H), 6.61 (d, J = 2.1 Hz, 1H), 6.44–6.34 (m, 1H), 6.15 (d, J = 3.5 Hz, 1H), 4.54–4.47 (m, 2H), 4.32 (dd, J = 8.6, 4.8 Hz, 1H), 3.93 (d, J = 7.5 Hz, 2H), 3.84–3.76 (m, 1H), 3.62 (d, J = 13.8 Hz, 1H), 3.27–3.16 (m, 2H), 2.76 (d, J = 14.9 Hz, 1H), 2.69–2.60 (m, 1H), 2.55 (s, 3H), 2.33 (s, 3H), 2.16 (s, 3H), 2.08–1.96 (m, 1H), 1.60 (s, 3H), 1.56 (s, 3H). 13C NMR (101 MHz, CD3OD) δ 175.2, 171.7, 162.9, 157.1, 150.4, 147.3, 139.6, 138.7, 138.3, 136.0, 134.4, 133.0, 132.3, 131.9, 127.3, 123.0, 119.8, 118.1, 117.7, 114.8, 112.4, 91.1, 77.0, 73.4, 71.7, 54.9, 50.9, 50.5, 36.9, 31.0, 29.7, 26.3, 20.5, 18.5. HRMS (ESI): calculated for C39H47N8O8 [M + H]+ 755.3511, found 755.3508.
Methyl-(S)-2-(3-(2-acetoxy-4,6-dimethylphenyl)-3-methylbutanamido)-4-((((2R,3S,4R,5R)-5-(6-amino-9H-purin-9-yl)-3,4-dihydroxytetrahydrofuran-2-yl)methyl)((E)-3-(4-cyanophenyl)allyl)amino)butanoate (14b). Following the procedure described for compound 12a, compound 13b (10 mg, 0.012 mmol) was deprotected and purified, affording compound 14b as a white powder (5 mg, 48% yield). 1H NMR (400 MHz, CD3OD) δ 8.48 (s, 1H), 8.36 (s, 1H), 7.70 (d, J = 8.3 Hz, 2H), 7.53 (d, J = 8.1 Hz, 2H), 6.87–6.77 (m, 2H), 6.61 (d, J = 1.5 Hz, 1H), 6.42–6.35 (m, 1H), 6.17 (d, J = 3.5 Hz, 1H), 4.69 (t, J = 3.8 Hz, 1H), 4.51 (d, J = 6.6 Hz, 2H), 4.40 (dd, J = 8.7, 5.0 Hz, 1H), 3.95 (br s, 2H), 3.82–3.74 (m, 1H), 3.69 (s, 3H), 3.62 (br d, J = 13.6 Hz, 1H), 3.25–3.18 (m, 2H), 2.76 (d, J = 14.9 Hz, 1H), 2.64 (br d, J = 14.8 Hz, 1H), 2.54 (s, 3H), 2.16 (s, 3H), 2.00 (s, 1H), 1.61 (s, 3H), 1.55 (s, 3H). 13C NMR (101 MHz, CD3OD) δ 172.9, 170.9, 160.96, 161.3, 161.0, 160.6, 160.2, 151.1, 149.7, 148.1, 139.66, 138.7, 136.0, 133.6, 132.3, 131.9, 127.3, 123.0, 119.9, 118.1, 117.7, 114.8, 111.9, 91.1, 78.5, 73.4, 72.2, 54.3, 51.8, 49.5, 39.1, 31.1, 30.8, 26.1, 24.4, 20.6, 18.9. HRMS (ESI): calculated for C40H49N8O8 [M + H]+ 769.3673, found 769.3681.
Ethyl-(S)-2-(3-(2-acetoxy-4,6-dimethylphenyl)-3-methylbutanamido)-4-((((2R,3S,4R,5R)-5-(6-amino-9H-purin-9-yl)-3,4-dihydroxytetrahydrofuran-2-yl)methyl)((E)-3-(4-cyanophenyl)allyl)amino)butanoate (14c). Following the procedure described for compound 12a, compound 13c (10 mg, 0.012 mmol) was deprotected and purified, affording compound 14c as a white powder (6 mg, 56% yield). 1H NMR (400 MHz, Methanol-d4) δ 8.46 (s, 1H), 8.34 (s, 1H), 7.72 (d, J = 8.4 Hz, 2H), 7.53 (d, J = 8.2 Hz, 2H), 6.86–6.78 (m, 2H), 6.61 (d, J = 2.1 Hz, 1H), 6.42–6.31 (m, 1H), 6.16 (d, J = 3.6 Hz, 1H), 4.70 (s, 1H), 4.55–4.46 (m, 2H), 4.38 (dd, J = 8.8, 5.0 Hz, 1H), 4.18–4.13 (m, 2H), 3.93 (s, 2H), 3.81–3.75 (m, 1H), 3.61 (br d, J = 14.9 Hz, 1H), 3.26–3.15 (m, 2H), 2.55 (s, 3H), 2.34 (s, 3H), 2.16 (s, 3H), 1.62 (s, 3H), 1.56 (s, 3H), 1.24 (t, J = 7.1 Hz, 3H). 13C NMR (101 MHz, Methanol-d4) δ 172.9, 171.0, 151.6, 149.7, 147.1, 139.6, 138.7, 138.3, 136.0, 133.6, 132.7, 131.9, 128.1, 123.6, 119.8, 118.9, 112.0, 91.0, 78.5, 78.5, 73.4, 72.2, 61.6, 55.5, 50.9, 49.6, 39.1, 29.9, 26.1, 24.4, 20.6, 18.8. HRMS (ESI): calculated for C41H51N8O8 [M + H]+ 783.3830, found 783.3835.
Propyl-(S)-2-(3-(2-acetoxy-4,6-dimethylphenyl)-3-methylbutanamido)-4-((((2R,3S,4R,5R)-5-(6-amino-9H-purin-9-yl)-3,4-dihydroxytetrahydrofuran-2-yl)methyl)((E)-3-(4-cyanophenyl)allyl)amino)butanoate (14d). Following the procedure described for compound 12a, compound 13d (10 mg, 0.012 mmol) was deprotected and purified, affording compound 14d as a white powder (4 mg, 42% yield). 1H NMR (500 MHz, CD3OD) δ 8.45 (s, 1H), 8.34 (s, 1H), 7.70 (d, J = 8.3 Hz, 2H), 7.51 (d, J = 8.1 Hz, 2H), 6.85–6.78 (m, 2H), 6.60 (d, J = 1.8 Hz, 1H), 6.40–6.34 (m, 1H), 6.15 (d, J = 3.5 Hz, 1H), 4.68 (t, J = 4.0 Hz, 1H), 4.52 –4.47 (m, 2H), 4.37 (dd, J = 8.6, 5.1 Hz, 1H), 4.04 (t, J = 6.7 Hz, 2H), 3.97–3.89 (m, 2H), 3.79–3.74 (m, 1H), 3.64–3.57 (m, 1H), 3.24–3.17 (m, 2H), 2.79–2.70 (m, 2H), 2.67 (d, J = 4.2 Hz, 1H), 2.64 (s, 1H), 2.53 (s, 3H), 2.32 (s, 3H), 2.15 (s, 3H), 2.04–1.94 (m, 1H), 1.67–1.58 (m, 6H), 1.54 (s, 3H), 0.91 (t, J = 7.4 Hz, 3H). 13C NMR (126 MHz, CD3OD) δ 172.9, 171.1, 170.6, 149.8, 139.7, 138.4, 136.1, 133.7, 134.4, 132.0, 127.4, 123.1, 119.9, 118.1, 112.0, 91.1, 78.6, 73.5, 72.3, 67.1, 54.5, 50.9, 49.7, 39.2, 31.1, 30.9, 24.5, 21.6, 20.7, 18.9. HRMS (ESI): calculated for C42H53N8O8 [M + H]+ 783.3986, found 797.3991.
Isopropyl-(S)-2-(3-(2-acetoxy-4,6-dimethylphenyl)-3-methylbutanamido)-4-((((2R,3S,4R,5R)-5-(6-amino-9H-purin-9-yl)-3,4-dihydroxytetrahydrofuran-2-yl)methyl)((E)-3-(4-cyanophenyl)allyl)amino)butanoate (14e). Following the procedure described for compound 12a, compound 13e (10 mg, 0.012 mmol) was deprotected and purified, affording compound 14e as a white powder (5.3 mg, 49% yield). 1H NMR (400 MHz, CD3OD) δ 8.47 (s, 1H), 8.35 (s, 1H), 7.71 (d, J = 8.1 Hz, 2H), 7.53 (d, J = 8.1 Hz, 2H), 6.86–6.77 (m, 2H), 6.61 (d, J = 2.1 Hz, 1H), 6.42–6.35 (m, 1H), 6.17 (d, J = 3.5 Hz, 1H), 4.72–4.66 (m, 1H), 4.54–4.49 (m, 2H), 4.33 (dd, J = 8.8, 5.0 Hz, 1H), 3.93 (d, J = 7.5 Hz, 2H), 3.78 (dd, J = 14.0, 9.6 Hz, 1H), 3.62 (d, J = 13.8 Hz, 1H), 3.27–3.17 (m, 2H), 2.77 (d, J = 14.9 Hz, 1H), 2.64 (br d, J = 14.9 Hz, 1H), 2.55 (s, 3H), 2.33 (s, 3H), 2.16 (s, 3H), 2.07–1.93 (m, 1H), 1.61 (s, 3H), 1.56 (s, 3H), 1.22 (dd, J = 6.3, 1.8 Hz, 6H). 13C NMR (101 MHz, CD3OD) δ 175.2, 171.7, 162.9, 157.1, 150.4, 147.3, 139.6, 138.7, 138.3, 136.0, 134.4, 133.0, 132.3, 131.9, 127.3, 123.0, 119.8, 118.1, 117.7, 114.8, 112.4, 91.1, 77.0, 73.4, 71.7, 69.2, 54.9, 50.9, 50.5, 36.9, 31.0, 29.7, 26.3, 24.4, 20.5, 18.5. HRMS (ESI): calculated for C42H53N8O8 [M + H]+ 783.3986, found 797.3994.
Benzyl-(S)-2-(3-(2-acetoxy-4,6-dimethylphenyl)-3-methylbutanamido)-4-((((2R,3S,4R,5R)-5-(6-amino-9H-purin-9-yl)-3,4-dihydroxytetrahydrofuran-2-yl)methyl)((E)-3-(4-cyanophenyl)allyl)amino)butanoate (14f). Compound 13f (13mg, 0.015 mmol) was deprotected and purified, affording compound 14f as a white powder (5 mg, 39%). 1H NMR (500 MHz, CD3OD) δ 8.41 (s, 1H), 8.31 (s, 1H), 7.69 (d, J = 6.3 Hz, 2H), 7.49 (d, J = 8.1 Hz, 2H), 7.33 (d, J = 9.1 Hz, 5H), 6.82–6.75 (m, 2H), 6.57 (d, J = 2.1 Hz, 1H), 6.36–6.27 (m, 1H), 6.12 (d, J = 3.5 Hz, 1H), 5.12 (d, J = 2.9 Hz, 2H), 4.65 (t, J = 4.2 Hz, 1H), 4.50–4.38 (m, 3H), 3.89 (d, J = 11.8 Hz, 2H), 3.76–3.70(m, 1H), 3.56 (br d, J = 14.6 Hz, 1H), 3.35 (s, 1H), 3.23–3.11 (m, 2H), 2.28 (s, 3H), 2.12 (s, 3H), 2.01–1.93 (m, 1H), 1.56 (s, 3H), 1.49 (s, 3H). 13C NMR (126 MHz, CD3OD) δ 171.1, 149.8, 139.6, 138.4, 136.1, 133.7, 1132.4, 128.3, 128.1, 123.1, 91.1, 72.3, 67.1, 42.4, 31.7, 24.4, 20.6, 18.9. HRMS (ESI): calculated for C46H52N8O8 [M + H]+ 844.3908, found 844.3911.