Total Keratin-18 (M65) as a Potential, Early, Non-Invasive Biomarker of Hepatocyte Injury in Alcohol Intoxicated Adolescents—A Preliminary Study
Abstract
1. Introduction
2. Materials and Methods
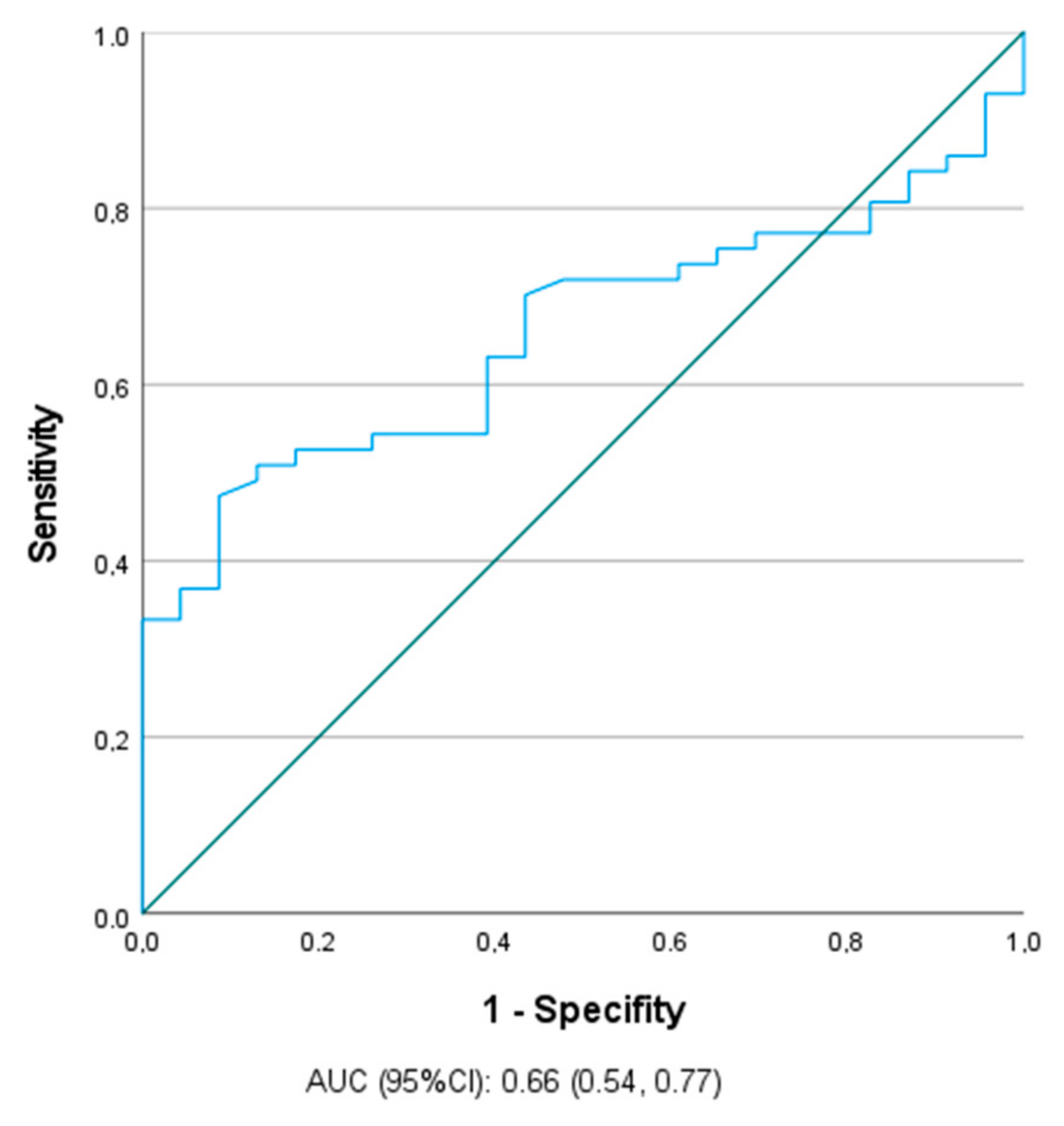
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Varlinskaya, E.I.; Kim, E.U.; Spear, L.P. Chronic intermittent ethanol exposure during adolescence: Effects on stress-induced social alterations and social drinking in adulthood. Brain Res. 2017, 1654 Pt B, 145–156. [Google Scholar] [CrossRef]
- World Health Organization. Global Status Report on Alcohol and Health 2018; World Health Organization: Geneva, Switzerland, 2018. [Google Scholar]
- Sartor, C.E.; Lynskey, M.T.; Heath, A.C.; Jacob, T.; True, W. The role of childhood risk factors in initiation of alcohol use and progression to alcohol dependence. Addiction 2007, 102, 216–225. [Google Scholar] [CrossRef]
- Irons, B.L. Alcohol use disorders: A clinical update. Adolesc. Med. Clin. 2006, 17, 259–282. [Google Scholar]
- Spear, L.P. Effects of adolescent alcohol consumption on the brain and behaviour. Nat. Rev. Neurosci. 2018, 19, 197–214. [Google Scholar] [CrossRef]
- Temple, J.L.; Cordero, P.; Li, J.; Nguyen, V.; Oben, J.A. A Guide to Non-Alcoholic Fatty Liver Disease in Childhood and Adolescence. Int. J. Mol. Sci. 2016, 17, 947. [Google Scholar] [CrossRef] [PubMed]
- Doycheva, I.; Watt, K.D.; Rifai, G.; Mrad, R.A.; Lopez, R.; Zein, N.N.; Carey, W.D.; Alkhouri, N. Increasing Burden of Chronic Liver Disease Among Adolescents and Young Adults in the USA: A Silent Epidemic. Dig. Dis. Sci. 2017, 62, 1373–1380. [Google Scholar] [CrossRef] [PubMed]
- Hagström, H.; Hemmingsson, T.; Discacciati, A.; Andreasson, A. Alcohol consumption in late adolescence is associated with an increased risk of severe liver disease later in life. J. Hepatol. 2018, 68, 505–510. [Google Scholar] [CrossRef] [PubMed]
- Ku, N.O.; Strnad, P.; Zhong, B.H.; Tao, G.Z.; Omary, M.B. Keratins let liver live: Mutations predispose to liver disease and crosslinking generates Mallory-Denk bodies. Hepatology 2007, 46, 1639–1649. [Google Scholar] [CrossRef]
- Ku, N.-O.; Strnad, P.; Bantel, H.; Omary, B. Keratins: Biomarkers and modulators of apoptotic and necrotic cell death in the liver. Hepatology 2016, 64, 966–976. [Google Scholar] [CrossRef]
- Kramer, G.; Erdal, H.; Mertens, H.J.M.M.; Nap, M.; Mauermann, J.; Steiner, G.; Marberger, M.; Bivén, K.; Shoshan, M.C.; Linder, S. Differentiation between cell death modes using measurements of different soluble forms of extracellular cytokeratin 18. Cancer Res. 2004, 64, 1751–1756. [Google Scholar] [CrossRef]
- Nanau, R.M.; Neuman, M.G. Biomolecules and Biomarkers Used in Diagnosis of Alcohol Drinking and in Monitoring Therapeutic Interventions. Biomolecules 2015, 5, 1339–1385. [Google Scholar] [CrossRef] [PubMed]
- Siqueira, L.; Smith, V.C. ABUSE COS. Binge Drinking. Pediatrics 2015, 136, e718–e726. [Google Scholar] [CrossRef]
- Wei, X.; Wei, H.; Lin, W.; Hu, Z.; Zhang, J. Cell death biomarker M65 is a useful indicator of liver inflammation and fibrosis in chronic hepatitis B: A cross-sectional study of diagnostic accuracy. Medicine 2017, 96, e6807. [Google Scholar] [CrossRef] [PubMed]
- Gonzalez-Quintela, A.; Mallo, N.; Mella, C.; Campos-Franco, J.; Perez, L.-F.; Lopez-Rodriguez, R.; Tome, S.; Otero, E. Serum levels of cytokeratin-18 (tissue polypeptide-specific antigen) in liver diseases. Liver Int. 2006, 26, 1217–1224. [Google Scholar] [CrossRef]
- Mandelia, C.; Collyer, E.; Mansoor, S.; Lopez, R.; Lappe, S.; Nobili, V.; Alkhouri, N. Plasma Cytokeratin-18 Level as a Novel Biomarker for Liver Fibrosis in Children with Nonalcoholic Fatty Liver Disease. J. Pediatr. Gastroenterol. Nutr. 2016, 63, 181–187. [Google Scholar] [CrossRef] [PubMed]
- Lebensztejn, D.M.; Wierzbicka, A.; Socha, P.; Pronicki, M.; Skiba, E.; Werpachowska, I.; Kaczmarski, M. Cytokeratin-18 and hyaluronic acid levels predict liver fibrosis in children with non-alcoholic fatty liver disease. Acta Biochim. Pol. 2011, 58, 563–566. [Google Scholar] [CrossRef] [PubMed]
- Feldstein, A.E.; Alkhouri, N.; De Vito, R.; Alisi, A.; Lopez, R.; Nobili, V. Serum cytokeratin-18 fragment levels are useful biomarkers for nonalcoholic steatohepatitis in children. Am. J. Gastroenterol. 2013, 108, 1526–1531. [Google Scholar] [CrossRef] [PubMed]
- Bantel, H.; Lügering, A.; Heidemann, J.; Volkmann, X.; Poremba, C.; Strassburg, C.P.; Manns, M.P.; Schulze-Osthoff, K. Detection of apoptotic caspase activation in sera from patients with chronic HCV infection is associated with fibrotic liver injury. Hepatology 2004, 40, 1078–1087. [Google Scholar] [CrossRef]
- Darweesh, S.K.; AbdElAziz, R.A.; Abd-ElFatah, D.S.; AbdElazim, N.A.; Fathi, S.A.; Attia, D.; AbdAllah, M. Serum cytokeratin-18 and its relation to liver fibrosis and steatosis diagnosed by FibroScan and controlled attenuation parameter in nonalcoholic fatty liver disease and hepatitis C virus patients. Eur. J. Gastroenterol. Hepatol. 2019, 31, 633–641. [Google Scholar] [CrossRef] [PubMed]
- Yilmaz, B.; Aktas, B.; Altinbas, A.; Ginis, Z.; Ozturk, G.; Ekiz, F.; Kilincalp, S.; Deveci, M.; Simsek, Z.; Coban, S.; et al. The Role of M30 in Predicting the Severity of Liver Fibrosis and Inflammation in Chronic Hepatitis B Patients. Hepat. Mon. 2016, 16, e35640. [Google Scholar] [CrossRef]
- Jefferis, B.J.; Power, C.; Manor, O. Adolescent drinking level and adult binge drinking in a national birth cohort. Addiction 2005, 100, 543–549. [Google Scholar] [CrossRef] [PubMed]
- Silins, E.; Horwood, L.J.; Najman, J.M.; Patton, G.; Toumbourou, J.W.; Olsson, C.A.; Hutchinson, D.M.; Degenhardt, L.; Fergusson, D.; Becker, D.; et al. Adverse adult consequences of different alcohol use patterns in adolescence: An integrative analysis of data to age 30 years from four Australasian cohorts. Addiction 2018, 113, 1811–1825. [Google Scholar] [CrossRef] [PubMed]
- Campollo, O. Alcohol and the Liver: The Return of the Prodigal Son. Ann. Hepatol. 2019, 18, 6–10. [Google Scholar] [CrossRef]
- Atkinson, S.R.; Grove, J.I.; Liebig, S.; Astbury, S.; Vergis, N.; Goldin, R.; Quaglia, A.; Bantel, H.; Guha, I.N.; Thursz, M.R.; et al. In Severe Alcoholic Hepatitis, Serum Keratin-18 Fragments Are Diagnostic, Prognostic, and Theragnostic Biomarkers. Am. J. Gastroenterol. 2020, 115, 1857–1868. [Google Scholar] [CrossRef]
- Woolbright, B.L.; Bridges, B.W.; Dunn, W.; Olson, J.C.; Weinman, S.A.; Jaeschke, H. Cell Death and Prognosis of Mortality in Alcoholic Hepatitis Patients Using Plasma Keratin-18. Gene Expr. 2017, 17, 301–312. [Google Scholar] [CrossRef]
- Vatsalya, V.; Cave, M.C.; Kong, M.; Gobejishvili, L.; Falkner, K.C.; Craycroft, J.; Mitchell, M.; Szabo, G.; McCullough, A.; Dasarathy, S.; et al. Keratin 18 Is a Diagnostic and Prognostic Factor for Acute Alcoholic Hepatitis. Clin. Gastroenterol. Hepatol. 2020, 18, 2046–2054. [Google Scholar] [CrossRef]
- Mueller, S.; Nahon, P.; Rausch, V.; Peccerella, T.; Silva, I.; Yagmur, E.; Straub, B.K.; Lackner, C.; Seitz, H.K.; Rufat, P.; et al. Caspase-cleaved keratin-18 fragments increase during alcohol withdrawal and predict liver-related death in patients with alcoholic liver disease. Hepatology 2017, 66, 96–107. [Google Scholar] [CrossRef] [PubMed]
- Schlossberger, V.; Worni, M.; Kihm, C.; Montani, M.; Datz, C.; Hampe, J.; Stickel, F. Plasma Levels of K18 Fragments Do Not Correlate with Alcoholic Liver Fibrosis. Gut Liver. 2019, 13, 77–82. [Google Scholar] [CrossRef]
- Bissonnette, J.; Altamirano, J.; Devue, C.; Roux, O.; Payancé, A.; Lebrec, D.; Bedossa, P.; Valla, D.; Durand, F.; Ait-Oufella, H.; et al. A prospective study of the utility of plasma biomarkers to diagnose alcoholic hepatitis. Hepatology 2017, 66, 555–563. [Google Scholar] [CrossRef] [PubMed]
- Dezsőfi, A.; Baumann, U.; Dhawan, A.; Durmaz, O.; Fischler, B.; Hadzic, N.; Hierro, L.; Lacaille, F.; McLin, V.A.; Nobili, V.; et al. Liver biopsy in children: Position paper of the ESPGHAN Hepatology Committee. J. Pediatr. Gastroenterol. Nutr. 2015, 60, 408–420. [Google Scholar] [CrossRef] [PubMed]
| Parameter | Study Group (n = 57) | Control Group (n = 24) | p |
|---|---|---|---|
| Alcohol (g/L) | 1.78 (1.27–2.22) | - | NA |
| Age (years) | 15 (14–17) | 16 (14.5–16.5) | NS |
| ALT (IU/L) | 13 (10–16) | 13 (12–14) | NS |
| AST (IU/L) | 22 (18–26) | 20 (17–23) | NS |
| M30 (U/mL) | 109.271 (87.988–131.651) | 111.981 (95.058–134.055) | NS |
| M65 (U/mL) | 156.878 (114.029–249.763) | 120.01 (95.921–145.9) | 0.03 |
| Parameter | Boys (n = 28) | Girls (n = 29) | p |
|---|---|---|---|
| Age (years) | 15 (14–17) | 16 (15–17) | NS |
| Alcohol (g/L) | 1.825 (1.5–2.18) | 1.74 (1.17–2.22) | NS |
| ALT (IU/L) | 14 (12–20.5) | 12 (10–14) | 0.008 |
| AST (IU/L) | 24 (21–28) | 19 (16–22) | 0.004 |
| M30 (U/mL) | 95.058 (85.89–115.5385) | 125.014 (87.988–134.989) | NS |
| M65 (U/mL) | 164.886 (119.254–236.394) | 140.756 (98.959–258.175) | NS |
| Parameter | 12–15 Years (n = 30) | 16–17 Years (n = 27) | p |
|---|---|---|---|
| Alcohol (g/L) | 1.64 (1.1–1.96) | 2.05 (1.57.227) | 0.02 |
| ALT (IU/L) | 13 (10.5–15.5) | 13 (10–21) | NS |
| AST (IU/L) | 21 (17–27) | 22 (19–25) | NS |
| M30 (U/mL) | 98.9595 (85.905–131.651) | 109.271 (87.988–133.28) | NS |
| M65 (U/mL) | 142.9615 (75.976–262.372) | 164.159 (127.451–248.359) | NS |
| BAC (g/L) | M30 (U/mL) | p | M65 (U/mL) | p |
|---|---|---|---|---|
| ≤1.15 vs. >1.15 (n = 11) vs. (n = 46) | 90.042 (60.496–130.01) vs. 109.271 (87.988–134.898) | NS | 151.032 (75.976–197.331) vs. 162.705 (117.022–267.96) | NS |
| ≤1.50 vs. >1.50 (n = 18) vs. (n = 39) | 127.512 (85.905–136.504) vs. 99.929 (87.988–130.01) | NS | 144.421 (89.825–197.331) vs. 164.159 (114.029–267.96) | NS |
| ≤1.78 vs. >1.78 (n = 29) vs. (n = 28) | 109.271 (87.988–131.651) vs. 108.356 (87.988–133.275) | NS | 137.809 (124.479–197.331) vs. 180 (106.494–271.446) | NS |
| ≤2.00 vs. >2.00 (n = 36) vs. (n = 27) | 109.271(90.042–131.651) vs. 92.069 (86.905–134.898) | NS | 148.1 (126.709–225.08) vs. 164.159 (89.825–267.96) | NS |
| ≤2.20 vs. >2.20 (n = 42) vs. (n = 21) | 109.271 (87.989–131.651) vs. 92.069 (84.8175–132.454) | NS | 136.333 (117.022–217.291) vs. 156.878 (114.029–249.763) | NS |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Zdanowicz, K.; Olanski, W.; Kowalczuk-Kryston, M.; Bobrus-Chociej, A.; Werpachowska, I.; Lebensztejn, D.M. Total Keratin-18 (M65) as a Potential, Early, Non-Invasive Biomarker of Hepatocyte Injury in Alcohol Intoxicated Adolescents—A Preliminary Study. Biomolecules 2021, 11, 911. https://doi.org/10.3390/biom11060911
Zdanowicz K, Olanski W, Kowalczuk-Kryston M, Bobrus-Chociej A, Werpachowska I, Lebensztejn DM. Total Keratin-18 (M65) as a Potential, Early, Non-Invasive Biomarker of Hepatocyte Injury in Alcohol Intoxicated Adolescents—A Preliminary Study. Biomolecules. 2021; 11(6):911. https://doi.org/10.3390/biom11060911
Chicago/Turabian StyleZdanowicz, Katarzyna, Witold Olanski, Monika Kowalczuk-Kryston, Anna Bobrus-Chociej, Irena Werpachowska, and Dariusz Marek Lebensztejn. 2021. "Total Keratin-18 (M65) as a Potential, Early, Non-Invasive Biomarker of Hepatocyte Injury in Alcohol Intoxicated Adolescents—A Preliminary Study" Biomolecules 11, no. 6: 911. https://doi.org/10.3390/biom11060911
APA StyleZdanowicz, K., Olanski, W., Kowalczuk-Kryston, M., Bobrus-Chociej, A., Werpachowska, I., & Lebensztejn, D. M. (2021). Total Keratin-18 (M65) as a Potential, Early, Non-Invasive Biomarker of Hepatocyte Injury in Alcohol Intoxicated Adolescents—A Preliminary Study. Biomolecules, 11(6), 911. https://doi.org/10.3390/biom11060911






