Protective Effects of Chromium Picolinate Against Diabetic-Induced Renal Dysfunction and Renal Fibrosis in Streptozotocin-Induced Diabetic Rats
Abstract
1. Introduction
2. Materials and Methods
2.1. Chemicals and Reagents
2.2. Animals
2.3. Diabetic Nephropathy Induction and CrPic Administration
2.4. Renal Function Assessment
2.5. Blood Glucose and Serum Insulin Measurement
2.6. Renal MDA, SOD, CAT, and GPX Determinations
2.7. Histological Evaluation of Renal Pathological Changes
2.8. Masson’s Trichrome Staining for Evaluation of Renal Interstitial Fibrosis
2.9. PAS Staining for Evaluation of Glomerulosclerosis
2.10. Immunohistochemistry (IHC)
2.11. Statistical Analysis
3. Results
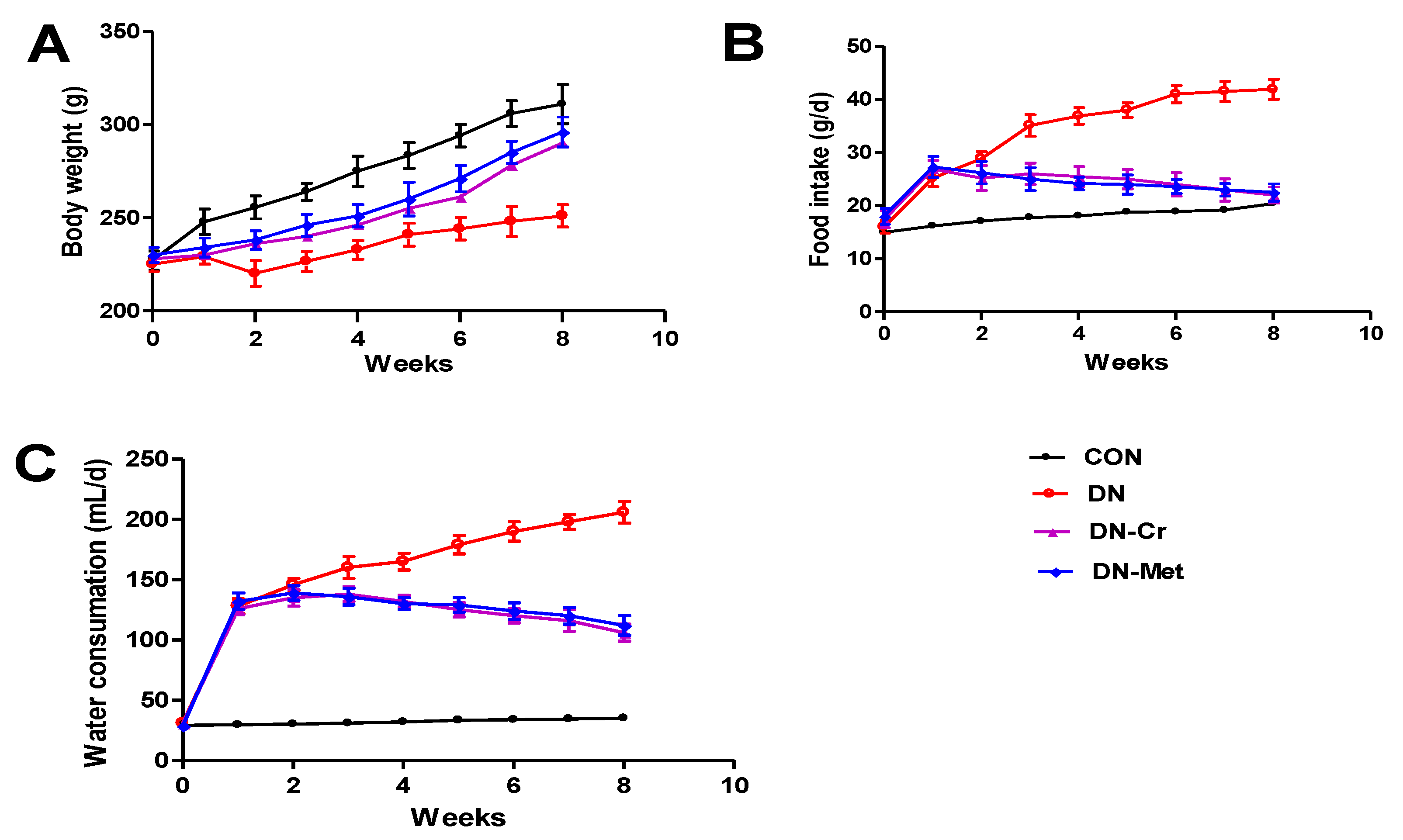
3.1. CrPic Increases Body Weight and Decreases Food Intake and Water Consumption in Diabetic Nephropathy Rats
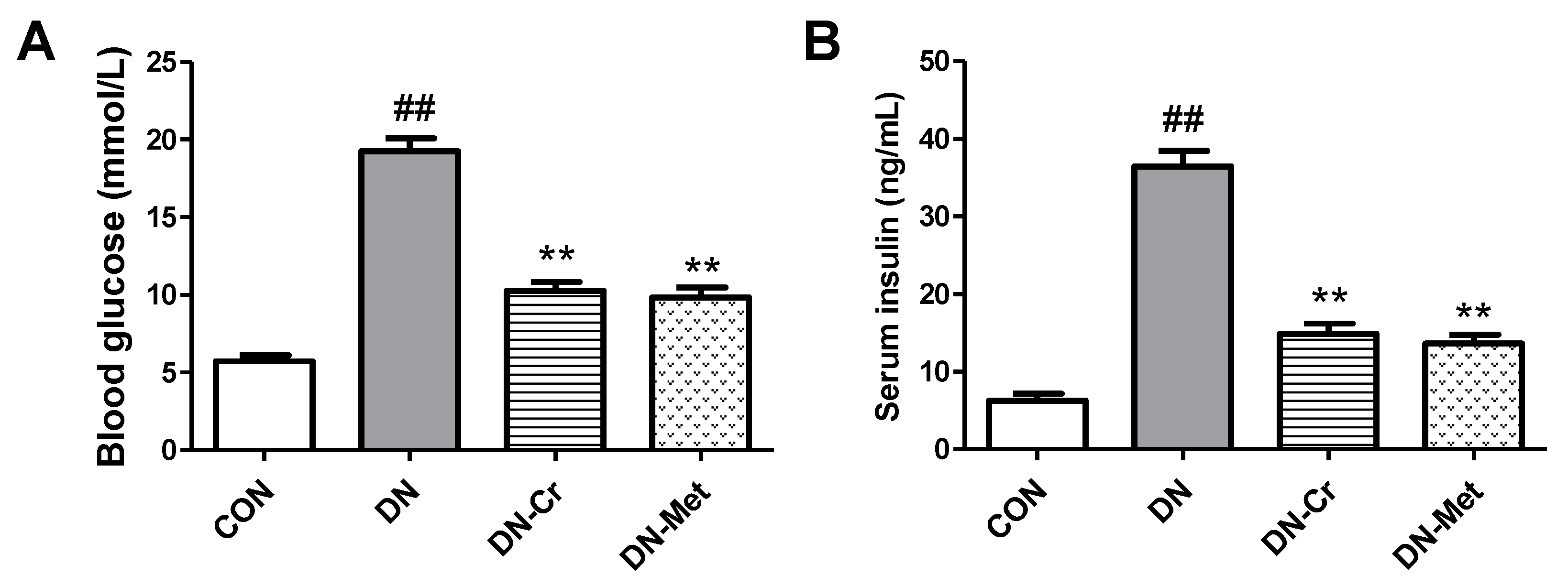
3.2. CrPic Decreases Blood Glucose and Serum Insulin Levels in Diabetic Nephropathy Rats
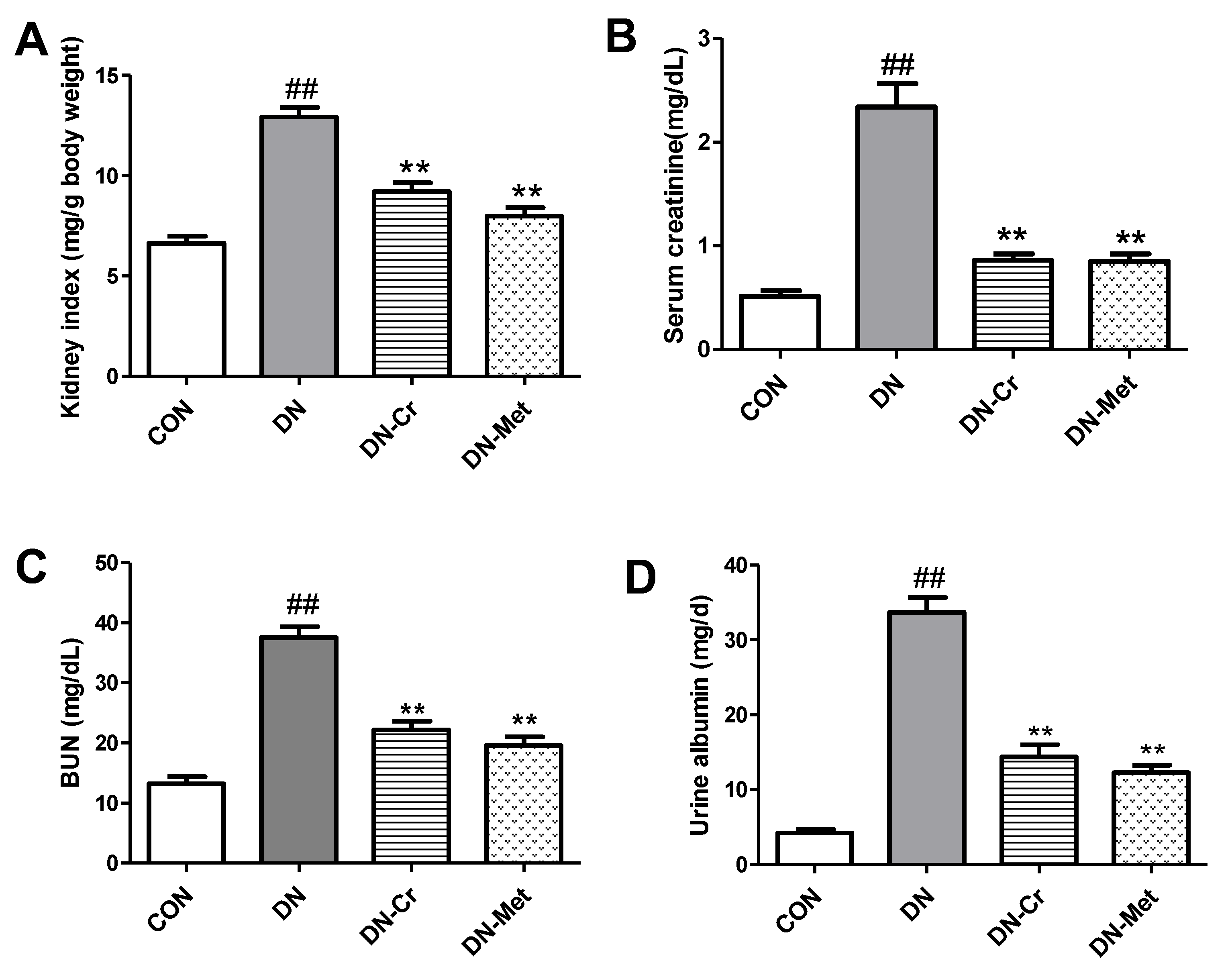
3.3. CrPic Decreases Kidney Index and Improves Renal Dysfunction in Diabetic Nephropathy Rats
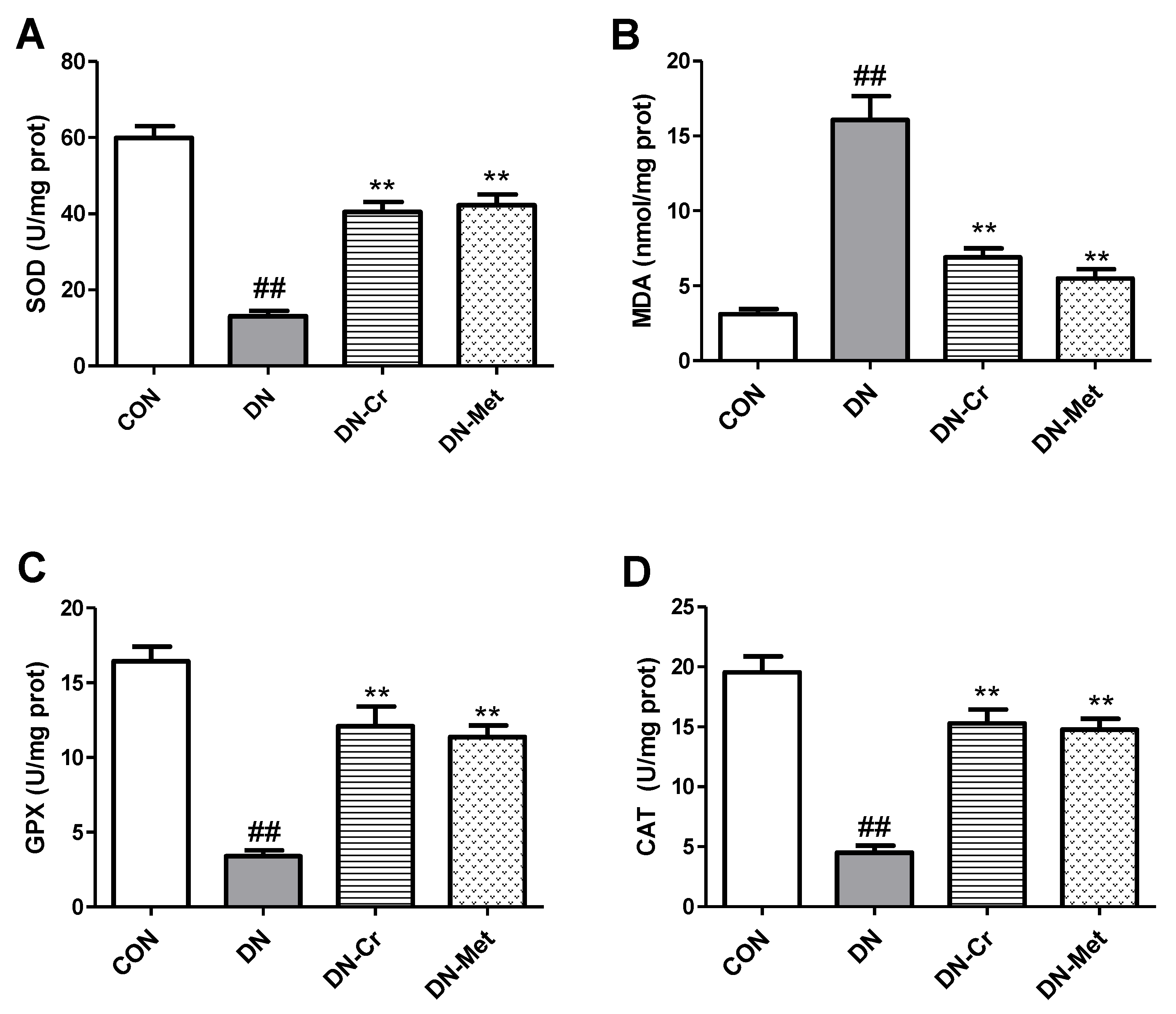
3.4. CrPic Inhibits Renal Oxidative Stress in Diabetic Nephropathy Rats
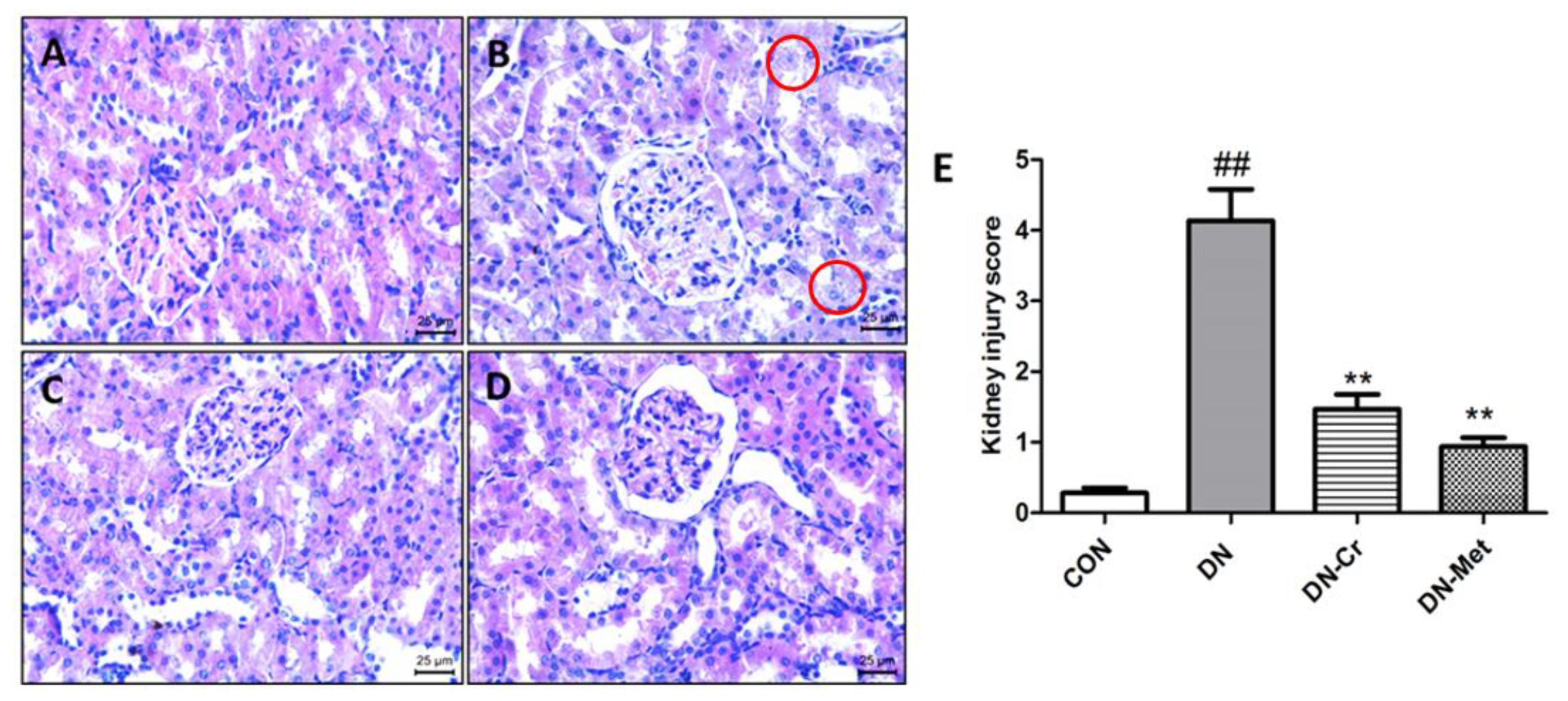
3.5. CrPic Improves Renal Tissue Pathological Changes in Diabetic Nephropathy Rats
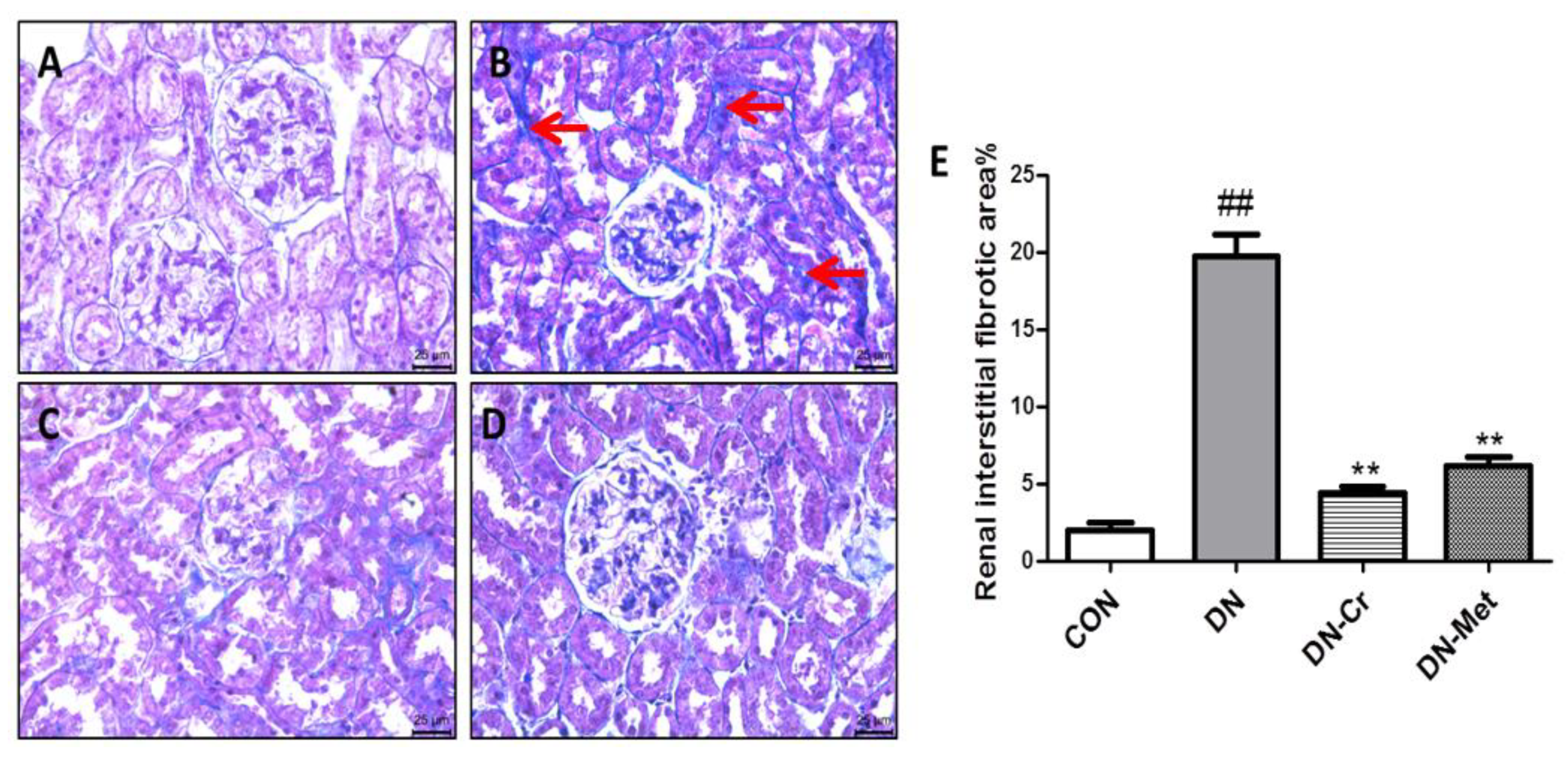
3.6. CrPic Inhibits Renal Interstitial Fibrosis in Diabetic Nephropathy Rats
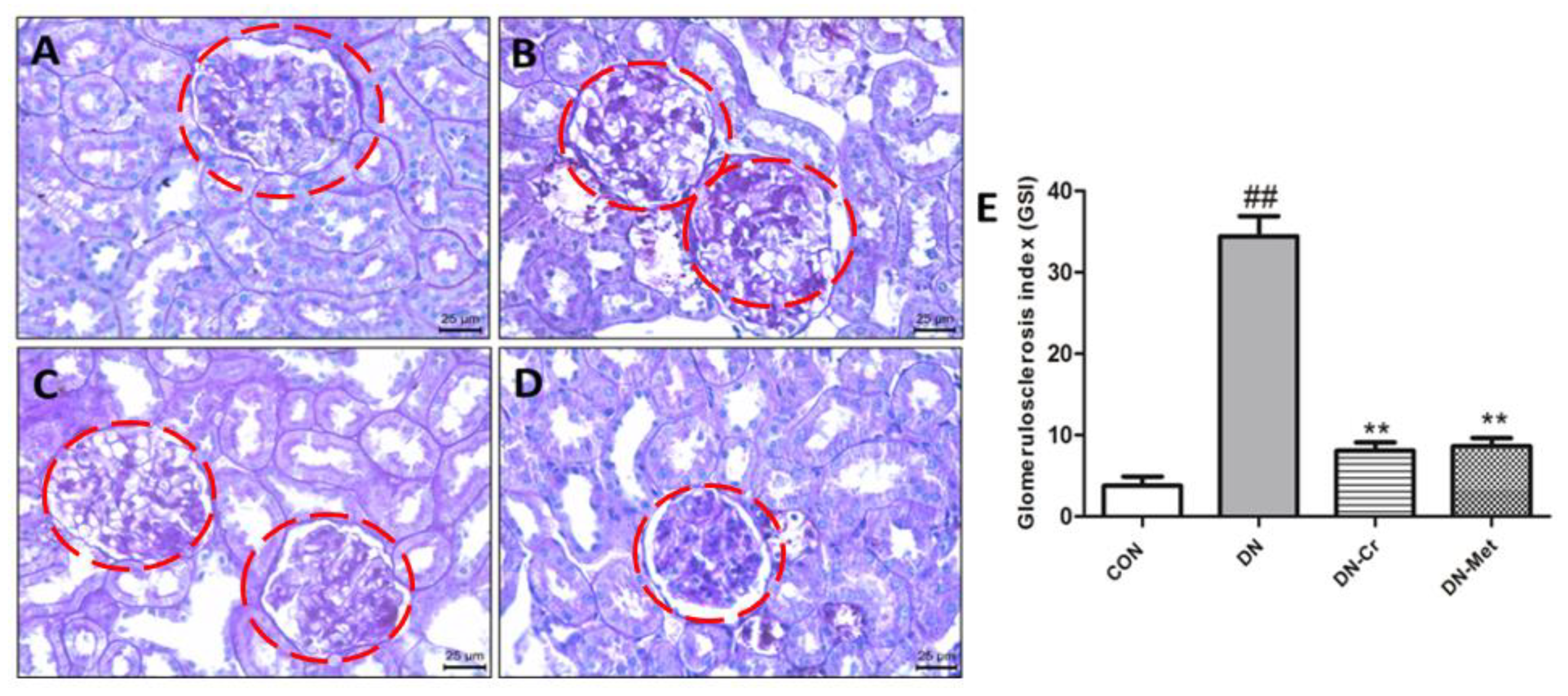
3.7. CrPic Inhibits Glomerulosclerosis in Diabetic Nephropathy Rats
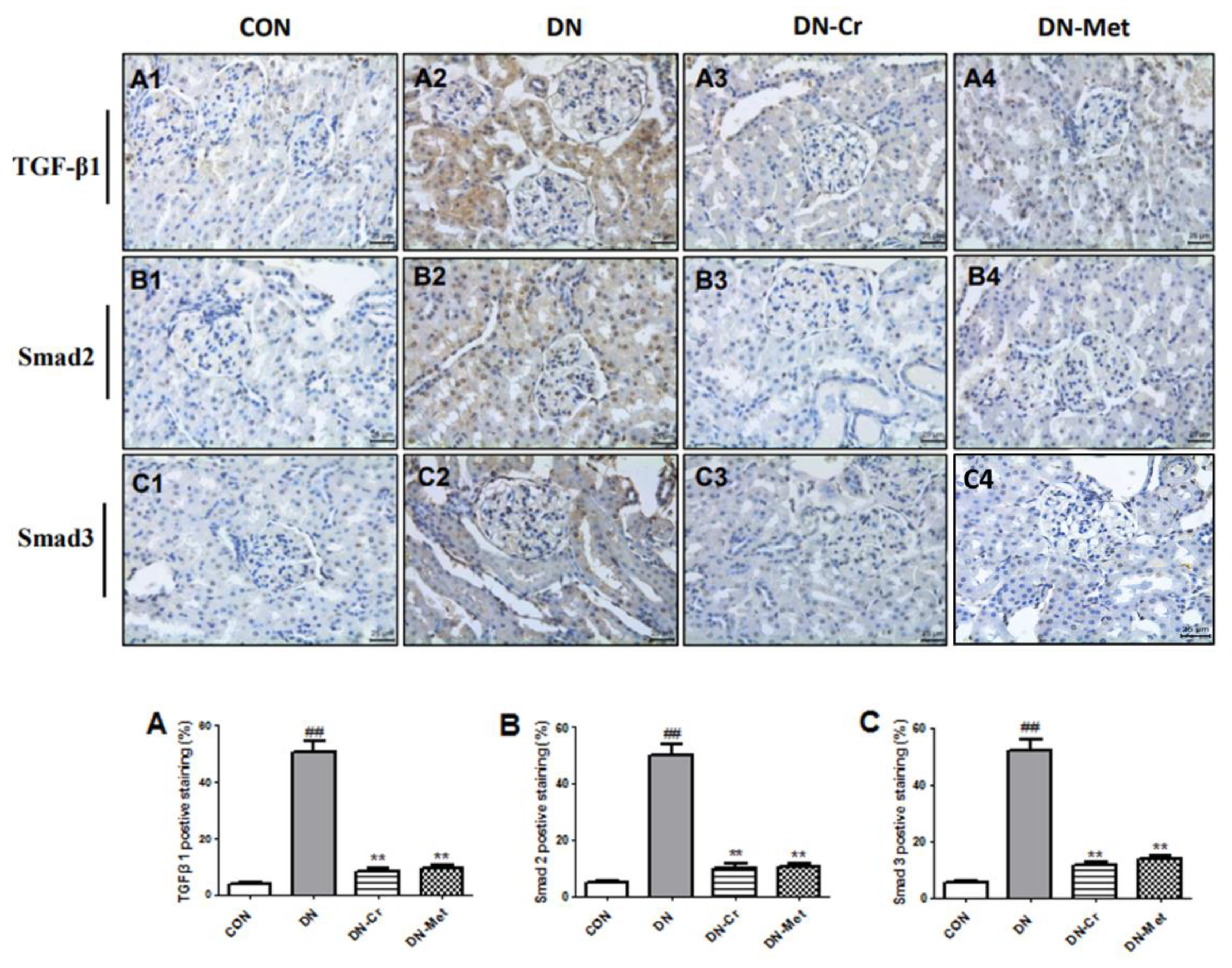
3.8. CrPic Regulates the Renal TGF-β1/Smad Signal Pathway in Diabetic Nephropathy Rats
4. Discussion
5. Conclusions
Author Contributions
Funding
Conflicts of Interest
References
- Ding, S.; Xu, S.; Ma, Y.; Liu, G.; Jang, H.; Fang, J. Modulatory mechanisms of the NLRP3 inflammasomes in diabetes. Biomolecules 2019, 9, 850. [Google Scholar] [CrossRef] [PubMed]
- Ge, C.X.; Xu, M.M.; Qin, Y.T.; Gu, T.T.; Lou, D.S.; Li, Q.; Hu, L.F.; Nie, X.Y.; Wang, M.X.; Tan, J. Fisetin supplementation prevents high fat diet-induced diabetic nephropathy by repressing insulin resistance and RIP3-regulated inflammation. Food Funct. 2019, 10, 2970–2985. [Google Scholar] [CrossRef] [PubMed]
- Dronavalli, S.; Duka, I.; Bakris, G.L. The pathogenesis of diabetic nephropathy. Nat. Clin. Pract. Endocrinol. Metab. 2008, 4, 444–452. [Google Scholar] [CrossRef] [PubMed]
- Chen, G.T.; Yang, M.; Chen, B.B.; Song, Y.; Zhang, W.; Zhang, Y. 2,3,5,4’-Tetrahydroxystilbene -2-O-β-d-glucoside exerted protective effects on diabetic nephropathy in mice with hyperglycemia induced by streptozotocin. Food Funct. 2016, 7, 4628–4636. [Google Scholar] [CrossRef]
- Soldatos, G.; Cooper, M.E. Diabetic nephropathy: Important pathophysiologic mechanisms. Diabetes Res. Clin. Pract. 2008, 82, S75–S79. [Google Scholar] [CrossRef]
- Huang, S.; Peng, W.; Jiang, X. The effect of chromium picolinate supplementation on the pancreas and macroangiopathy in type II diabetes mellitus rats. J. Diabetes Res. 2014, 5, 717–729. [Google Scholar] [CrossRef]
- Broadhurst, C.; Leigh, D.P. Clinical Studies on Chromium Picolinate supplementation in diabetes mellitus—a review. Diabetes Technol. The. 2016, 6, 677–687. [Google Scholar] [CrossRef]
- Alexander, R.; Ladislav, S.; Nitsa, M.; Richard, A.A. Control of steroid-induced diabetes with supplemental chromium. J. Trace Elem. Exp. Med. 1999, 12, 375–378. [Google Scholar]
- Martin, J.; Wang, Z.Q.; Zhang, X.H. Chromium picolinate supplementation attenuates body weight gain and increases insulin sensitivity in subjects with type 2 diabetes. Diabetes Care 2006, 8, 1826–1832. [Google Scholar] [CrossRef][Green Version]
- Sundaram, B.; Aggarwal, A.; Sandhir, R. Chromium picolinate attenuates hyperglycemia -induced oxidative stress in streptozotocin-induced diabetic rats. J. Trace Elem. Med. Biol. 2013, 2, 117–121. [Google Scholar] [CrossRef]
- Sundaram, B.; Singhal, K.; Sandhir, R. Anti-atherogenic effect of chromium picolinate in streptozotocin-induced experimental diabetes. J. Diabetes 2012, 5, 43–55. [Google Scholar] [CrossRef]
- Meng, Z.Q.; Yan, Y.X.; Tang, Z.H.; Guo, C.G.; Li, N.; Huang, W.Z.; Ding, G.; Wang, Z.Z.; Xiao, W.; Yang, Z. Anti-hyperuricemic and nephroprotective effects of rhein in hyperuricemic mice. Planta Med. 2015, 81, 279–285. [Google Scholar] [CrossRef] [PubMed]
- Raij, L.; Azar, S.; Keane, W. Mesangial immune injury, hypertension, and progessive glomerular damage in Dahl rats. Kidney Int. 1984, 26, 137–143. [Google Scholar] [CrossRef] [PubMed]
- Qi, S.S.; He, J.; Zheng, H.X.; Chen, C.; Lan, S.Q. Icariin prevents diabetes-induced bone loss in rats by reducing blood glucose and suppressing bone turnover. Molecules 2019, 24, 1871. [Google Scholar] [CrossRef]
- Xie, R.; Zhang, H.; Wang, X.Z.; Yang, X.Z.; Wu, S.N.; Wang, H.G.; Shen, P.; Ma, T.H. The protective effect of betulinic acid (BA) diabetic nephropathy on streptozotocin (STZ)-induced diabetic rats. Food Funct. 2017, 8, 299–306. [Google Scholar] [CrossRef] [PubMed]
- Zhang, L.; Mao, W.; Guo, X.F.; Wu, Y.F.; Li, C.; Lu, Z.Y.; Su, G.B.; Li, X.Y.; Liu, Z.Z.; Guo, R.; et al. Ginkgo biloba extract for patients with early diabetic nephropathy: A systematic review. Evid. Based Complement. Altermat. Med. 2013, 2013, 689142. [Google Scholar]
- Jain, S.K.; Rains, J.L.; Croad, J.L. Effect of chromium niacinate and chromium picolinate supplementation on lipid peroxidation, TNF-α, IL-6, CRP, glycated hemoglobin, triglycerides, and cholesterol levels in blood of streptozotocin-treated diabetic rats. Free Radic. Biol. Med. 2007, 8, 1124–1131. [Google Scholar] [CrossRef]
- Singer, G.M.; Geohas, J. The effect of chromium picolinate and biotin supplementation on glycemic control in poorly controlled patients with type 2 diabetes mellitus: A placebo-controlled, double-blinded, randomized trial. Diabetes Technol. The. 2006, 6, 636–643. [Google Scholar] [CrossRef]
- Shinde, U.A.; Goyal, R.K. Effect of chromium picolinate on histopathological alterations in STZ and neonatal STZ diabetic rats. J. Cell. Mol. Med. 2003, 7, 322–329. [Google Scholar] [CrossRef]
- Sahin, K.; Tuzcu, M.; Orhan, C. Anti-diabetic activity of chromium picolinate and biotin in rats with type 2 diabetes induced by high-fat diet and streptozotocin. Br. J. Nutr. 2013, 110, 197–205. [Google Scholar] [CrossRef]
- Cohen, M.P.; Clements, R.S.; Cohen, J.A.; Shearman, C.W. Prevention of decline in renal function in the diabetic db/db mouse. Diabetologia 1996, 39, 270–274. [Google Scholar] [CrossRef] [PubMed]
- Tashiro, K.; Koyanagi, I.; Saitoh, A.; Shimizu, A.; Shike, T.; Ishiguro, C.; Koizumi, M.; Funabiki, K.; Horikoshi, S.; Shirato, I.; et al. Urinary levels of monocyte chemoattractant protein-1 (MCP-1) and interleukin-8 (IL-8), and renal injuries in patients with type 2 diabetic nephropathy. J. Clin. Lab. Anal. 2002, 16, 1–4. [Google Scholar] [CrossRef] [PubMed]
- Oh, S.W.; Kim, S.; Na, K.Y.; Chae, D.W.; Kim, S.; Jin, D.C.; Chin, H.J. Clinical implications of pathologic diagnosis and classification for diabetic nephropathy. Diabetes Res. Clin. Pract. 2012, 97, 418–424. [Google Scholar] [CrossRef] [PubMed]
- Han, H.; Cao, A.; Wang, L. Huangqi decoction ameliorates streptozotocin-induced rat diabetic nephropathy through antioxidant and regulation of the TGF-β/MAPK/PPAR-γ signaling. Cell. Physiol. Biochem. 2017, 5, 1934–1944. [Google Scholar] [CrossRef] [PubMed]
- Zhang, Q.; Lu, Y.; Ma, Z.; Li, Y.; Guo, J.; Meng, Q.; Bian, H. A novel formula from mulberry leaf ameliorates diabetic nephropathy in rats via inhibiting the TGF-β1 pathway. Food Funct. 2015, 6, 3307–3315. [Google Scholar] [CrossRef] [PubMed]
- Qian, Y.; Feldman, E.; Pennathur, S.; Kretzler, M.; Brosius, F.C. From fibrosis to sclerosis: Mechanisms of glomerulosclerosis in diabetic nephropathy. Diabetes 2008, 57, 1439–1445. [Google Scholar] [CrossRef] [PubMed]
- Ha, H.; Hwang, I.A.; Park, J.H.; Lee, H.B. Role of reactive oxygen species in the pathogenesis of diabetic nephropathy. Diabetes Res. Clin. Pract. 2008, 82, S42–S45. [Google Scholar] [CrossRef]
- Singh, D.K.; Winocour, P.; Farrington, K. Oxidative stress in early diabetic nephropathy: Fueling the fire. Nat. Rev. Endocrinol. 2011, 7, 176–184. [Google Scholar] [CrossRef]
- Cao, A.L.; Wang, L.; Chen, X.; Guo, H.J.; Chu, S.; Zhang, X.M.; Peng, W. Ursodeoxycholic acid ameliorated diabetic nephropathy by attenuating hyperglycemia-mediated oxidative stress. Biol. Pharm. Bull. 2016, 39, 1300–1308. [Google Scholar] [CrossRef]
- Olatunji, O.J.; Chen, H.X.; Zhou, Y.F. Lycium chinense, leaves extract ameliorates diabetic nephropathy by suppressing hyperglycemia mediated renal oxidative stress and inflammation. Biomed. Pharmacother. 2018, 102, 1145–1151. [Google Scholar] [CrossRef]
- Afshari, A.T.; Shirpoor, A.; Farshid, A.; Saadatian, R.; Rasmi, Y.; Saboory, E.; Ilkhanizadeh, B.; Allameh, A. The effect of ginger on diabetic nephropathy, plasma antioxidant capacity and lipid peroxidation in rats. Food Chem. 2007, 101, 148–153. [Google Scholar] [CrossRef]
- Al-Onazi, A.S.; Al-Rasheed, N.M.; Attia, H.A.; Al-Rasheed, N.M.; Ahmed, R.M.; Al-Amin, M.A.; Poizat, C. Ruboxistaurin attenuates diabetic nephropathy via modulation of TGF-β1/Smad and GRAP pathways. J. Pharm. Pharmacol. 2016, 68, 219–232. [Google Scholar] [CrossRef] [PubMed]
- Wang, D.D.; Zhang, G.Y.; Chen, X.; Wei, T.; Liu, C.X.; Chen, C.; Gong, Y.H.; Wei, Q.L. Sitagliptin ameliorates diabetic nephropathy by blocking TGF-β1/Smad signaling pathway. Int. J. Mol. Med. 2018, 41, 2784–2792. [Google Scholar] [CrossRef]
- Yang, X.; Song, J.; Yan, L.J. Chronic inhibition of mitochondrial dihydrolipoamide dehydrogenase (DLDH) as an approach to managing diabetic oxidative stress. Antioxidants 2019, 8, 32. [Google Scholar] [CrossRef] [PubMed]
- Sonia, S.F.; Enrique, P.T.D.; Sandra, C.I.; Alejandra, G.M.D. Oxidative stress, apoptosis, and mitochondrial function in diabetic nephropathy. Int. J. Endocrinol. 2018, 2018, 1875870. [Google Scholar]
- Elmarakby, A.A.; Sullivan, J.C. Relationship between oxidative stress and inflammatory cytokines in diabetic nephropathy. Cardiovasc. Ther. 2012, 30, 49–59. [Google Scholar] [CrossRef]
- Akira, M. Inflammation and oxidative stress in diabetic nephropathy: New insights on its inhibition as new therapeutic targets. J. Diabetes Res. 2013, 2013, 248563. [Google Scholar]
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Qi, S.S.; Zheng, H.X.; Jiang, H.; Yuan, L.P.; Dong, L.C. Protective Effects of Chromium Picolinate Against Diabetic-Induced Renal Dysfunction and Renal Fibrosis in Streptozotocin-Induced Diabetic Rats. Biomolecules 2020, 10, 398. https://doi.org/10.3390/biom10030398
Qi SS, Zheng HX, Jiang H, Yuan LP, Dong LC. Protective Effects of Chromium Picolinate Against Diabetic-Induced Renal Dysfunction and Renal Fibrosis in Streptozotocin-Induced Diabetic Rats. Biomolecules. 2020; 10(3):398. https://doi.org/10.3390/biom10030398
Chicago/Turabian StyleQi, Shan Shan, Hong Xing Zheng, Hai Jiang, Li Ping Yuan, and Le Chen Dong. 2020. "Protective Effects of Chromium Picolinate Against Diabetic-Induced Renal Dysfunction and Renal Fibrosis in Streptozotocin-Induced Diabetic Rats" Biomolecules 10, no. 3: 398. https://doi.org/10.3390/biom10030398
APA StyleQi, S. S., Zheng, H. X., Jiang, H., Yuan, L. P., & Dong, L. C. (2020). Protective Effects of Chromium Picolinate Against Diabetic-Induced Renal Dysfunction and Renal Fibrosis in Streptozotocin-Induced Diabetic Rats. Biomolecules, 10(3), 398. https://doi.org/10.3390/biom10030398



