Classical Examples of the Concept of the ASIA Syndrome
Abstract
1. Introduction
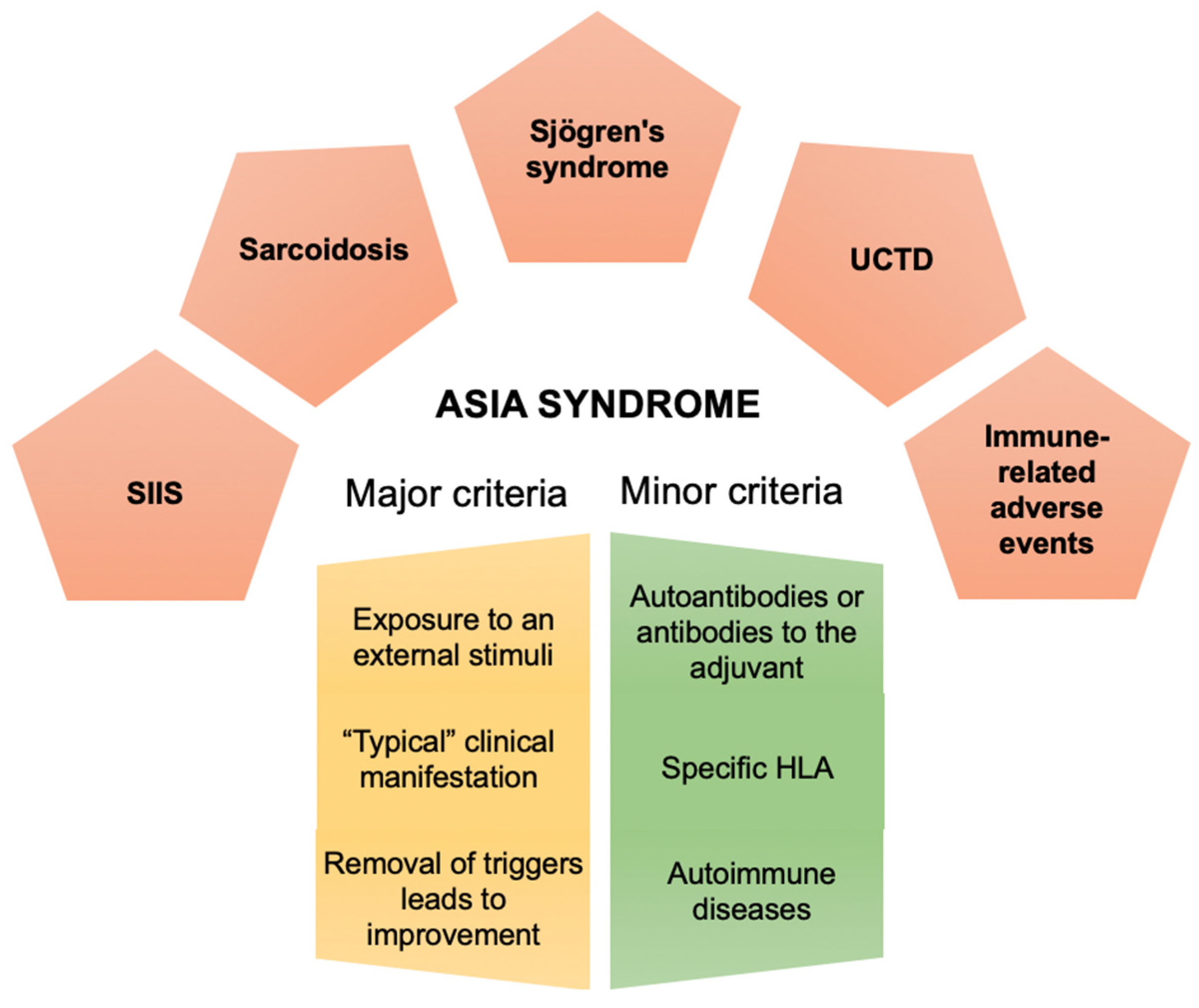
2. Classical Examples of the ASIA Syndrome
2.1. Sarcoidosis
2.2. Silicone Implant Incompatibility Syndrome
- Circulating autoantibodies against G protein-coupled receptors of the autonomic nervous systems such as adrenergic and muscarinic acetylcholine receptors have been found in the sera of these women, which we believe, may explain, at least in part, some of the enigmatic, subjective and undefined clinical manifestations reported by these women (personal communication). It is also worth mentioning that some studies reported that removal of the silicone breast implants led to significant improvements in clinical manifestation [64,65].
- Five women with SBIs have been diagnosed with SFN after evaluation of their skin biopsies. These two new objective findings (autoantibodies against the autonomic nervous system and SFN) have been found both in other ASIA-related entities (sarcoidosis, SS etc.) and other suspected autoimmune dysautonomic-related disorders. Therefore, it should be regarded as a new objective criterion of ASIA syndrome [17].
2.3. Sjögren’s Syndrome
2.4. Undifferentiated Connective Tissue Disease
2.5. Immune-Related Adverse Events
3. Redefining ASIA Syndrome Concept
4. Conclusions
Supplementary Materials
Author Contributions
Funding
Conflicts of Interest
Abbreviations
| AID | Autoimmune diseases |
| ANA | Antinuclear antibody |
| Anti-CCP | Anti-cyclic citrullinated peptide |
| ASIA | Autoimmune/Inflammatory syndrome induced by adjuvants |
| ASMA | Anti-smooth muscle antibody |
| CI | Confidence interval |
| CPI | Check-point inhibitors |
| CTLA | Cytotoxic T lymphocyte antigen |
| ENA | Extractable nuclear antigens |
| HBV | Hepatitis B virus |
| HLA | Human leukocyte antigen |
| ICIs | Immune checkpoint inhibitors |
| IFN-γ | Interferon gamma |
| IL | Interleukin |
| irAEs | Immune-related adverse events |
| NZB | New Zealand black |
| NZM | New Zealand mixed |
| OR | Odds ratio |
| PD-1 | Programmed cell death receptor-1 |
| PFS | Progression free survival |
| RF | Rheumatoid factor |
| SADs | Systemic autoimmune diseases |
| SBIs | Silicone breast implants |
| SFN | Small fiber neuropathy |
| SIIS | Silicone implant incompatibility syndrome |
| SS | Sjogren’s syndrome |
| SSc | Systemic sclerosis |
| TGF-β | Transforming growth factor β |
| Th | T helper lymphocytes |
| TLR-4 | Toll-like receptor 4 |
| TNF-α | Tumor necrosis factor α |
| UCTD | Undifferentiated connective tissue disease |
References
- Shoenfeld, Y.; Agmon-Levin, N. ‘ASIA’—Autoimmune/inflammatory syndrome induced by adjuvants. J. Autoimmun. 2011, 36, 4–8. [Google Scholar] [CrossRef] [PubMed]
- Watad, A.; Sharif, K.; Shoenfeld, Y. The ASIA syndrome: Basic concepts. Mediterr. J. Rheumatol. 2017, 28, 64–69. [Google Scholar] [CrossRef] [PubMed]
- Arango, M.T.; Perricone, C.; Kivity, S.; Cipriano, E.; Ceccarelli, F.; Valesini, G.; Shoenfeld, Y. HLA-DRB1 the notorious gene in the mosaic of autoimmunity. Immunol. Res. 2017, 65, 82–98. [Google Scholar] [CrossRef] [PubMed]
- Molina, V.; Shoenfeld, Y. Infection, vaccines and other environmental triggers of autoimmunity. Autoimmunity 2005, 38, 235–245. [Google Scholar] [CrossRef]
- Terhune, T.D.; Deth, R.C. Aluminum adjuvant-containing vaccines in the context of the hygiene hypothesis: A risk factor for eosinophilia and allergy in a genetically susceptible subpopulation? Int. J. Environ. Res. Public Health 2018, 15, 901. [Google Scholar] [CrossRef]
- Nancy, A.L.; Shoenfeld, Y. Chronic fatigue syndrome with autoantibodies—The result of an augmented adjuvant effect of hepatitis-B vaccine and silicone implant. Autoimmun. Rev. 2008, 8, 52–55. [Google Scholar] [CrossRef]
- Inbar, R.; Weiss, R.; Tomljenovic, L.; Arango, M.-T.; Deri, Y.; Shaw, C.A.; Chapman, J.; Blank, M.; Shoenfeld, Y. Behavioral abnormalities in female mice following administration of aluminum adjuvants and the human papillomavirus (HPV) vaccine Gardasil. Immunol. Res. 2017, 65, 136–149. [Google Scholar] [CrossRef]
- Sela, O.; Shoenfeld, Y. The association of infecting agents and autoimmune diseases. Harefuah 1987, 112, 285–288. [Google Scholar]
- Zinger, H.; Sherer, Y.; Goddard, G.; Berkun, Y.; Barzilai, O.; Agmon-Levin, N.; Ram, M.; Blank, M.; Tincani, A.; Rozman, B.; et al. Common infectious agents prevalence in antiphospholipid syndrome. Lupus 2009, 18, 1149–1153. [Google Scholar] [CrossRef]
- Caravantes-Cortes, M.I.; Roldan-Valadez, E.; Zwojewski-Martinez, R.D.; Salazar-Ruiz, S.Y.; Carballo-Zarate, A.A. Breast Prosthesis Syndrome: Pathophysiology and Management Algorithm. Aestheti. Plast. Surg. 2020, 1423, 44–1437. [Google Scholar] [CrossRef]
- Watad, A.; Quaresma, M.; Brown, S.; Cohen Tervaert, J.W.; Rodríguez-Pint, I.; Cervera, R.; Perricone, C.; Shoenfeld, Y. Autoimmune/inflammatory syndrome induced by adjuvants (Shoenfeld’s syndrome)—An update. Lupus 2017, 26, 675–681. [Google Scholar] [CrossRef] [PubMed]
- Jara, L.J.; García-Collinot, G.; Medina, G.; Cruz-Domínguez, M.; Vera-Lastra, O.; Carranza-Muleiro, R.A.; Saavedra, M.A. Severe manifestations of autoimmune syndrome induced by adjuvants (Shoenfeld’s syndrome). Immunol. Res. 2017, 65, 8–16. [Google Scholar] [CrossRef] [PubMed]
- Steiner, S.; Becker, S.C.; Hartwig, J.; Sotzny, F.; Lorenz, S.; Bauer, S.; Löbel, M.; Stittrich, A.B.; Grabowski, P.; Scheibenbogen, C. Autoimmunity-Related Risk Variants in PTPN22 and CTLA4 Are Associated with ME/CFS with Infectious Onset. Front. Immunol. 2020, 11. [Google Scholar] [CrossRef]
- Cárdenas-Roldán, J.; Rojas-Villarraga, A.; Anaya, J.M. How do autoimmune diseases cluster in families? A systematic review and meta-analysis. BMC Med. 2013, 11, 73. [Google Scholar] [CrossRef]
- Watad, A.; Bragazzi, N.L.; Amital, H.; Shoenfeld, Y. Hyperstimulation of adaptive immunity as the common pathway for silicone breast implants, autoimmunity; and lymphoma of the breast. Isr. Med. Assoc. J. 2019, 21, 517–519. [Google Scholar] [PubMed]
- Watad, A.; Bragazzi, N.L.; McGonagle, D.; Adawi, M.; Bridgewood, C.; Damiani, G.; Alijotas-Reig, J.; Esteve-Valverde, E.; Quaresma, M.; Amital, H.; et al. Autoimmune/inflammatory syndrome induced by adjuvants (ASIA) demonstrates distinct autoimmune and autoinflammatory disease associations according to the adjuvant subtype: Insights from an analysis of 500 cases. Clin. Immunol. 2019, 203, 1–8. [Google Scholar] [CrossRef]
- Shoenfeld, Y.; Ryabkova, V.A.; Scheibenbogen, C.; Brinth, L.; Martinez-Lavin, M.; Ikeda, S.; Heidecke, H.; Watad, A.; Bragazzi, N.L.; Chapman, J.; et al. Complex syndromes of chronic pain, fatigue and cognitive impairment linked to autoimmune dysautonomia and small fiber neuropathy. Clin. Immunol. 2020, 214, 108384. [Google Scholar] [CrossRef]
- Heinle, R.; Chang, C. Diagnostic criteria for sarcoidosis. Autoimmun. Rev. 2014, 13, 383–387. [Google Scholar] [CrossRef]
- Bindoli, S.; Dagan, A.; Torres-Ruiz, J.J.; Perricone, C.; Bizjak, M.; Doria, A.; Shoenfeld, Y. Sarcoidosis and autoimmunity: From genetic background to environmental factors. Isr. Med. Assoc. J. 2016, 18, 197–202. [Google Scholar]
- Valeyre, D.; Prasse, A.; Nunes, H.; Uzunhan, Y.; Brillet, P.-Y.; Müller-Quernheim, J. Sarcoidosis. Lancet 2014, 383, 1155–1167. [Google Scholar] [CrossRef]
- Jain, R.; Yadav, D.; Puranik, N.; Guleria, R.; Jin, J.-O. Sarcoidosis: Causes, Diagnosis, Clinical Features, and Treatments. J. Clin. Med. 2020, 9, 1081. [Google Scholar] [CrossRef]
- Moller, D.R.; Rybicki, B.A.; Hamzeh, N.Y.; Montgomery, C.G.; Chen, E.S.; Drake, W.; Fontenot, A.P. Genetic, immunologic, and environmental basis of sarcoidosis. Ann. Am. Thorac. Soc. 2017, 14, S429–S436. [Google Scholar] [CrossRef] [PubMed]
- Ahmadzai, H.; Cameron, B.; Chui, J.J.; Lloyd, A.; Wakefield, D.; Thomas, P.S. Peripheral blood responses to specific antigens and CD28 in sarcoidosis. Respir. Med. 2012, 106, 701–709. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Ramos-Casals, M.; Kostov, B.; Brito-Zerón, P.; Sisó-Almirall, A.; Baughman, R.P. How the Frequency and Phenotype of Sarcoidosis is Driven by Environmental Determinants. Lung 2019, 197, 427–436. [Google Scholar] [CrossRef] [PubMed]
- Watad, A.; Rosenberg, V.; Tiosano, S.; Cohen Tervaert, J.W.; Yavne, Y.; Shoenfeld, Y.; Shalev, V.; Chodick, G.; Amital, H. Silicone breast implants and the risk of autoimmune/rheumatic disorders: A real-world analysis. Int. J. Epidemiol. 2018, 47, 1846–1854. [Google Scholar] [CrossRef]
- Musaelyan, A.; Lapin, S.; Nazarov, V.; Tkachenko, O.; Gilburd, B.; Mazing, A.; Mikhailova, L.; Shoenfeld, Y. Vimentin as antigenic target in autoimmunity: A comprehensive review. Autoimmun. Rev. 2018, 17, 926–934. [Google Scholar] [CrossRef] [PubMed]
- Wahlström, J.; Dengjel, J.; Persson, B.; Duyar, H.; Rammensee, H.-G.; Stevanović, S.; Eklund, A.; Weissert, R.; Grunewald, J. Identification of HLA-DR-bound peptides presented by human bronchoalveolar lavage cells in sarcoidosis. J. Clin. Investig. 2007, 117, 3576–3582. [Google Scholar] [CrossRef]
- Eberhardt, C.; Thillai, M.; Parker, R.; Siddiqui, N.; Potiphar, L.; Goldin, R.; Timms, J.F.; Wells, A.U.; Kon, O.M.; Wickremasinghe, M.; et al. Proteomic analysis of Kveim reagent identifies targets of cellular immunity in sarcoidosis. PLoS ONE 2017, 12, e0170285. [Google Scholar] [CrossRef]
- Sakthivel, P.; Bruder, D. Mechanism of granuloma formation in sarcoidosis. Curr. Opin. Hematol. 2017, 24, 59–65. [Google Scholar] [CrossRef]
- Grunewald, J.; Grutters, J.C.; Arkema, E.V.; Saketkoo, L.A.; Moller, D.R.; Müller-Quernheim, J. Sarcoidosis. Nat. Rev. Dis. Primers 2019, 5, 45. [Google Scholar] [CrossRef]
- Belhomme, N.; Jouneau, S.; Bouzillé, G.; Decaux, O.; Lederlin, M.; Guillot, S.; Perlat, A.; Jégo, P. Role of serum immunoglobulins for predicting sarcoidosis outcome: A cohort study. PLoS ONE 2018, 13, e0193122. [Google Scholar] [CrossRef] [PubMed]
- Huang, H.; Lu, Z.; Jiang, C.; Liu, J.; Wang, Y.; Xu, Z. Imbalance between Th17 and regulatory T-cells in sarcoidosis. Int. J. Mol. Sci. 2013, 14, 21463–21473. [Google Scholar] [CrossRef] [PubMed]
- Mortaz, E.; Rezayat, F.; Amani, D.; Kiani, A.; Garssen, J.; Adcock, I.M.; Velayati, A. The roles of T helper 1, T helper 17 and regulatory T cells in the pathogenesis of sarcoidosis. Iran. J. Allergy Asthma Immunol. 2016, 15, 334–339. [Google Scholar] [PubMed]
- Stadhouders, R.; Lubberts, E.; Hendriks, R.W. A cellular and molecular view of T helper 17 cell plasticity in autoimmunity. J. Autoimmun. 2018, 87, 1–15. [Google Scholar] [CrossRef] [PubMed]
- Ramstein, J.; Broos, C.E.; Simpson, L.J.; Ansel, K.M.; Sun, S.A.; Ho, M.E.; Woodruff, P.G.; Bhakta, N.R.; Christian, L.; Nguyen, C.P.; et al. IFN-γ-producing t-helper 17.1 cells are increased in sarcoidosis and are more prevalent than t-helper type 1 cells. Am. J. Respir. Crit. Care Med. 2016, 193, 1281–1291. [Google Scholar] [CrossRef] [PubMed]
- Kobak, S.; Yilmaz, H.; Sever, F.; Duran, A.; Sen, N.; Karaarslan, A. The Prevalence of Antinuclear Antibodies in Patients with Sarcoidosis. Autoimmune Dis. 2014, 2014, 351852. [Google Scholar] [CrossRef] [PubMed]
- Kudryavtsev, I.; Serebriakova, M.; Starshinova, A.; Zinchenko, Y.; Basantsova, N.; Malkova, A.; Soprun, L.; Churilov, L.P.; Toubi, E.; Yablonskiy, P.; et al. Imbalance in B cell and T Follicular Helper Cell Subsets in Pulmonary Sarcoidosis. Sci. Rep. 2020, 10, 1059 . [Google Scholar] [CrossRef]
- Tarasidis, A.; Arce, S. Immune response biomarkers as indicators of sarcoidosis presence, prognosis, and possible treatment: An Immunopathogenic perspective. Autoimmun. Rev. 2020, 19, 102462. [Google Scholar] [CrossRef]
- Terkelsen, A.J.; Karlsson, P.; Lauria, G.; Freeman, R.; Finnerup, N.B.; Jensen, T.S. The diagnostic challenge of small fibre neuropathy: Clinical presentations, evaluations, and causes. Lancet Neurol. 2017, 16, 934–944. [Google Scholar] [CrossRef]
- Basantsova, N.Y.; Starshinova, A.A.; Dori, A.; Zinchenko, Y.S.; Yablonskiy, P.K.; Shoenfeld, Y. Small-fiber neuropathy definition, diagnosis, and treatment. Neurol. Sci. 2019, 40, 1343–1350. [Google Scholar] [CrossRef]
- Doria, A.; Zen, M.; Bettio, S.; Gatto, M.; Bassi, N.; Nalotto, L.; Ghirardello, A.; Iaccarino, L.; Punzi, L. Autoinflammation and autoimmunity: Bridging the divide. Autoimmun. Rev. 2012, 12, 22–30. [Google Scholar] [CrossRef]
- Bridges, A.J.; Vasey, F.B. Silicone breast implants: History, safety, and potential complications. Arch. Intern. Med. 1993, 153, 2638–2644. [Google Scholar] [CrossRef] [PubMed]
- Kumagai, Y.; Abe, C.; Shiokawa, Y. Scleroderma after cosmetic surgery: Four cases of human adjuvant disease. Arthritis Rheumatol. 1979, 22, 532–537. [Google Scholar] [CrossRef] [PubMed]
- Kumagai, Y.; Shiokawa, Y.; Medsger, T.A.; Rodnan, G.P. Clinical spectrum of connective tissue disease after cosmetic surgery. Observations on eighteen patients and a review of the Japanese literature. Arthritis Rheumatol. 1984, 27, 1–12. [Google Scholar] [CrossRef]
- Bizjak, M.; Selmi, C.; Praprotnik, S.; Bruck, O.; Perricone, C.; Ehrenfeld, M.; Shoenfeld, Y. Silicone implants and lymphoma: The role of inflammation. J. Autoimmun. 2015, 65, 64–73. [Google Scholar] [CrossRef]
- Levy, Y.; Rotman-Pikielny, P.; Ehrenfeld, M.; Shoenfeld, Y. Silicone breast implantation-induced scleroderma: Description of four patients and a critical review of the literature. Lupus 2009, 18, 1226–1232. [Google Scholar] [CrossRef]
- Soriano, A.; Butnaru, D.; Shoenfeld, Y. Long-term inflammatory conditions following silicone exposure: The expanding spectrum of the autoimmune/inflammatory syndrome induced by adjuvants (ASIA). Clin. Exp. Rheumatol. 2014, 32, 151–154. [Google Scholar] [PubMed]
- Nesher, G.; Soriano, A.; Shlomai, G.; Iadgarov, Y.; Shulimzon, T.R.; Borella, E.; Dicker, D.; Shoenfeld, Y. Severe Asia syndrome associated with lymph node, thoracic, and pulmonary silicone infiltration following breast implant rupture: Experience with four cases. Lupus 2015, 24, 463–468. [Google Scholar] [CrossRef]
- Goren, I.; Segal, G.; Shoenfeld, Y. Autoimmune/inflammatory syndrome induced by adjuvant (ASIA) evolution after silicone implants. Who is at risk? Clin. Rheumatol. 2015, 34, 1661–1666. [Google Scholar] [CrossRef] [PubMed]
- Shons, A.R.; Schubert, W. Silicone breast implants and immune disease. Ann. Plast. Surg. 1992, 28, 491–501. [Google Scholar] [CrossRef]
- Yoshida, S.H.; Swan, S.; Teuber, S.S.; Gershwin, M.E. Silicone breast implants: Immunotoxic and epidemiologic issues. Life Sci. 1995, 56, 1299–1310. [Google Scholar] [CrossRef]
- Aharon-Maor, A.; Levy, Y.; Schoenfeld, Y. Fibrosarcoma after silicone breast augmentation: Is there a connection? Harefuah 1998, 134, 339–341. [Google Scholar] [PubMed]
- Versini, M.; Shoenfeld, Y. The dark side of beauty: About breast implants and lymphoma. Isr. Med. Assoc. J. 2017, 19, 380–381. [Google Scholar] [PubMed]
- Meier, L.G.; Barthel, H.R.M.; Seidl, C. Development of polyarthritis after insertion of silicone breast implants followed by remission after implant removal in 2 HLA-identical sisters bearing rheumatoid arthritis susceptibility genes. J. Rheumatol. 1997, 24, 1838–1841. [Google Scholar] [PubMed]
- O’Hanlon, T.; Koneru, B.; Bayat, E.; Love, L.; Targoff, I.; Malley, J.; Malley, K.; Miller, F. Immunogenetic differences between caucasian women with and those without silicone implants in whom myositis develops. Arthritis Rheumatol. 2004, 50, 3646–3650. [Google Scholar] [CrossRef] [PubMed]
- Ueki, A.; Isozaki, Y.; Tomokuni, A.; Ueki, H.; Kusaka, M.; Tanaka, S.; Otsuki, T.; Sakaguchi, H.; Hyodoh, F. Different distribution of HLA class II alleles in anti-topoisomerase I autoantibody responders between silicosis and systemic sclerosis patients, with a common distinct amino acid sequence in the HLA-DQB1 domain. Immunobiology 2001, 204, 458–465. [Google Scholar] [CrossRef]
- Young, V.L.; Nemecek, J.R.; Schwartz, B.D.; Phelan, D.L.; Schorr, M.W. Hla typing in women with breast implants. Plast. Reconstr. Surg. 1995, 96, 1497–1519. [Google Scholar] [CrossRef] [PubMed]
- Schaefer, C.J.; Lawrence, W.D.; Wooley, P.H. Influence of long term silicone implantation on type II collagen induced arthritis in mice. Ann. Rheum. Dis. 1999, 58, 503–509. [Google Scholar] [CrossRef]
- Schaefer, C.J.; Wooley, P.H. The influence of silicone implantation on murine lupus in MRL lpr/lpr mice. J. Rheumatol. 1999, 26, 2215–2221. [Google Scholar]
- Watad, A.; Quaresma, M.; Bragazzi, N.L.; Cervera, R.; Cohen Tervaert, J.W.; Amital, H.; Shoenfeld, Y. The autoimmune/inflammatory syndrome induced by adjuvants (ASIA)/Shoenfeld’s syndrome: Descriptive analysis of 300 patients from the international ASIA syndrome registry. Clin. Rheumatol. 2018, 37, 483–493. [Google Scholar] [CrossRef]
- Scanzi, F.; Andreoli, L.; Martinelli, M.; Taraborelli, M.; Cavazzana, I.; Carabellese, N.; Ottaviani, R.; Allegri, F.; Franceschini, F.; Agmon-Levin, N. Are the autoimmune/inflammatory syndrome induced by adjuvants (ASIA) and the undifferentiated connective tissue disease (UCTD) related to each other? A case-control study of environmental exposures. Immunol. Res. 2017, 65, 150–156. [Google Scholar] [CrossRef] [PubMed]
- Zandman-Goddard, G.; Blank, M.; Ehrenfeld, M.; Gilburd, B.; Peter, J.; Shoenfeld, Y. A comparison of autoantibody production in asymptomatic and symptomatic women with silicone breast implants. J. Rheumatol. 1999, 26, 73–77. [Google Scholar] [PubMed]
- Dagan, A.; Kogan, M.; Shoenfeld, Y.; Segal, G. When uncommon and common coalesce: Adult onset Still’s disease associated with breast augmentation as part of autoimmune syndrome induced by adjuvants (ASIA). Clin. Rheumatol. 2016, 35, 1643–1648. [Google Scholar] [CrossRef] [PubMed]
- De Boer, M.; Colaris, M.; van der Hulst, R.R.W.J.; Cohen Tervaert, J.W. Is explantation of silicone breast implants useful in patients with complaints? Immunol. Res. 2017, 65, 25–36. [Google Scholar] [CrossRef] [PubMed]
- Peters, W.; Smith, D.; Fornasier, V.; Lugowski, S.; Ibanez, D. An outcome analysis of 100 women after explantation of silicone gel breast implants. Ann. Plast. Surg. 1997, 39, 9–19. [Google Scholar] [CrossRef]
- Luciano, N.; Valentini, V.; Calabrò, A.; Elefante, E.; Vitale, A.; Baldini, C.; Bartoloni, E. One year in review 2015: Sjögren’s syndrome. Clin. Exp. Rheumatol. 2015, 33, 259–271. [Google Scholar]
- Colafrancesco, S.; Perricone, C.; Priori, R.; Valesini, G.; Shoenfeld, Y. Sjögren’s syndrome: Another facet of the autoimmune/inflammatory syndrome induced by adjuvants (ASIA). J. Autoimmun. 2014, 51, 10–16. [Google Scholar] [CrossRef]
- Colafrancesco, S.; Perricone, C.; Shoenfeld, Y. Autoimmune/inflammatory syndrome induced by adjuvants and sjögren’s syndrome. Isr. Med. Assoc. J. 2016, 18, 150–153. [Google Scholar]
- Van Assen, S.; Agmon Levin, N.; Elkayam, O.; Cervera, R.; Doran, M.F.; Dougados, M.; Emery, P.; Geborek, P.; Ioannidis, J.P.A.; Jayne, D.R.W.; et al. EULAR recommendations for vaccination in adult patients with autoimmune inflammatory rheumatic diseases. Ann. Rheum. Dis. 2011, 70, 414–422. [Google Scholar] [CrossRef]
- Furer, V.; Rondaan, C.; Heijstek, M.W.; Agmon-Levin, N.; van Assen, S.; Bijl, M.; Breedveld, F.C.; D’Amelio, R.; Dougados, M.; Kapetanovic, M.C.; et al. 2019 update of EULAR recommendations for vaccination in adult patients with autoimmune inflammatory rheumatic diseases. Ann. Rheum. Dis. 2020, 79, 39–52. [Google Scholar] [CrossRef]
- Toussirot, E.; Lohse, A.; Wendling, D.; Mougin, C. Sjogren’s syndrome occurring after hepatitis B vaccination. Arthritis Rheumatol. 2000, 43, 2139–2140. [Google Scholar] [CrossRef]
- Tabache, F.; El Kartouti, A.; Naitlhou, A.; Hassikou, H.; Tarib, A.; Baaj, M.; Cherrah, Y. Acute polyarthritis after influenza A (H1N1) immunization. Jt. Bone Spine 2011, 78, 321–322. [Google Scholar] [CrossRef] [PubMed]
- Narváez, J.; Castro-Bohorquez, F.J.; Vilaseca-Momplet, J. Sjögren’s-like syndrome following intravesical bacillus Calmette-Guérin immunotherapy. Am. J. Med. 2003, 115, 418–420. [Google Scholar] [CrossRef]
- Pasoto, S.G.; Ribeiro, A.C.; Santos Trindade Viana, V.; Pires Leon, E.; Bueno, C.; Levy Neto, M.; Precioso, A.R.; Sampaio Tavares Timenetsky, M.d.C.; Bonfa, E. Short and long-term effects of pandemic unadjuvanted influenza A(H1N1)pdm09 vaccine on clinical manifestations and autoantibody profile in primary Sjögren’s syndrome. Vaccine 2013, 31, 1793–1798. [Google Scholar] [CrossRef] [PubMed]
- Astudillo, L.; Sailler, L.; Ecoiffier, M.; Giron, J.; Couret, B.; Arlet-Suau, E. Exposure to silica and primary Sjögren’s syndrome in a dental technician. Rheumatology 2003, 42, 1268–1269. [Google Scholar] [CrossRef] [PubMed]
- Orriols, R.; Ferrer, J.; Tura, J.M.; Xaus, C.; Coloma, R. Sicca syndrome and silicoproteinosis in a dental technician. Eur. Respir. J. 1997, 10, 731–734. [Google Scholar]
- Sanchez-Roman, J.; Wichmann, I.; Salaberri, J.; Varela, J.M.; Nuñez-Roldan, A. Multiple clinical and biological autoimmune manifestations in 50 workers after occupational exposure to silica. Ann. Rheum. Dis. 1993, 52, 534–538. [Google Scholar] [CrossRef]
- Puisieux, F.; Hachulla, E.; Brouillard, M.; Hatron, P.Y.; Devulder, B. Silicosis and primary Gougerot-Sjogren syndrome. Rev. Med. Interne 1994, 15, 575–579. [Google Scholar] [CrossRef]
- Akyol, L.; Onem, S.; Ozgen, M.; Sayarlioglu, M. Sjögren’s syndrome after silicone breast implantation. Eur. J. Rheumatol. 2015, 2, 165–166. [Google Scholar] [CrossRef]
- Balk, E.M.; Earley, A.; Avendano, E.A.; Raman, G. Long-term health outcomes in women with silicone gel breast implants. Ann. Intern. Med. 2016, 164, 164–175. [Google Scholar] [CrossRef]
- Janowsky, E.C.; Kupper, L.L.; Hulka, B.S. Meta-analyses of the relation between silicone breast implants and the risk of connective-tissue diseases. N. Engl. J. Med. 2000, 342, 781–790. [Google Scholar] [CrossRef] [PubMed]
- Lipworth, L.; Tarone, R.E.; McLaughlin, J.K. Silicone breast implants and connective tissue disease: An updated review of the epidemiologic evidence. Ann. Plast. Surg. 2004, 52, 598–601. [Google Scholar] [CrossRef] [PubMed]
- Coroneos, C.J.; Selber, J.C.; Offodile, A.C.; Butler, C.E.; Clemens, M.W. US FDA Breast Implant Postapproval Studies: Long-term Outcomes in 99,993 Patients. Ann. Surg. 2019, 269, 30–36. [Google Scholar] [CrossRef] [PubMed]
- Okano, Y.; Nishikai, M.; Sato, A. Scleroderma, primary biliary cirrhosis, and Sjogren’s syndrome after cosmetic breast augmentation with silicone injection: A case report of possible human adjuvant disease. Ann. Rheum. Dis. 1984, 43, 520–522. [Google Scholar] [CrossRef]
- Contant, C.M.E.; Swaak, A.J.G.; Obdeijn, A.I.M.; van der Holt, B.; Tjong Joe Wai, R.; van Geel, A.N.; Eggermont, A.M.M. A prospective study on silicone breast implants and the silicone-related symptom complex. Clin. Rheumatol. 2002, 21, 215–219. [Google Scholar] [CrossRef]
- Cohen Tervaert, J.W.; Kappel, R.M. Silicone implant incompatibility syndrome (SIIS): A frequent cause of ASIA (Shoenfeld’s syndrome). Immunol. Res. 2013, 56, 293–298. [Google Scholar] [CrossRef]
- Colaris, M.J.L.; de Boer, M.; van der Hulst, R.R.; Cohen Tervaert, J.W. Two hundreds cases of ASIA syndrome following silicone implants: A comparative study of 30 years and a review of current literature. Immunol. Res. 2017, 65, 120–128. [Google Scholar] [CrossRef]
- Kappel, R.M.; Pruijn, G.J.M. The monobloc hydrogel breast implant, experiences and ideas. Eur. J. Plast. Surg. 2012, 35, 229–233. [Google Scholar] [CrossRef]
- Alijotas-Reig, J.; Garcia-Gimenez, V.; Llurba, E.; Vilardell-Tarrés, M. Autoimmune/inflammatory syndrome (ASIA) induced by biomaterials injection other than silicone medical grade. Lupus 2012, 21, 1326–1334. [Google Scholar] [CrossRef]
- Alijotas-Reig, J.; Esteve-Valverde, E.; Gil-Aliberas, N.; Garcia-Gimenez, V. Autoimmune/inflammatory syndrome induced by adjuvants—ASIA—Related to biomaterials: Analysis of 45 cases and comprehensive review of the literature. Immunol. Res. 2018, 66, 120–140. [Google Scholar] [CrossRef]
- Antunes, M.; Scirè, C.A.; Talarico, R.; Alexander, T.; Avcin, T.; Belocchi, C.; Doria, A.; Franceschini, F.; Galetti, I.; Govoni, M.; et al. Undifferentiated connective tissue disease: State of the art on clinical practice guidelines. RMD Open 2019, 4, e000786. [Google Scholar] [CrossRef]
- Ferri, C.; Manfredi, A.; Sebastiani, M.; Colaci, M.; Giuggioli, D.; Vacchi, C.; Della Casa, G.; Cerri, S.; Torricelli, P.; Luppi, F. Interstitial pneumonia with autoimmune features and undifferentiated connective tissue disease: Our interdisciplinary rheumatology-pneumology experience, and review of the literature. Autoimmun. Rev. 2016, 15, 61–70. [Google Scholar] [CrossRef] [PubMed]
- Mosca, M.; Tani, C.; Talarico, R.; Bombardieri, S. Undifferentiated connective tissue diseases (UCTD): Simplified systemic autoimmune diseases. Autoimmun. Rev. 2011, 10, 256–258. [Google Scholar] [CrossRef] [PubMed]
- Mosca, M.; Tani, C.; Vagnani, S.; Carli, L.; Bombardieri, S. The diagnosis and classification of undifferentiated connective tissue diseases. J. Autoimmun. 2014, 48, 50–52. [Google Scholar] [CrossRef] [PubMed]
- Perricone, C.; Colafrancesco, S.; Mazor, R.D.; Soriano, A.; Agmon-Levin, N.; Shoenfeld, Y. Autoimmune/inflammatory syndrome induced by adjuvants (ASIA) 2013: Unveiling the pathogenic, clinical and diagnostic aspects. J. Autoimmun. 2013, 47, 1–16. [Google Scholar] [CrossRef] [PubMed]
- Segal, Y.; Dahan, S.; Sharif, K.; Bragazzi, N.L.; Watad, A.; Amital, H. The value of Autoimmune Syndrome Induced by Adjuvant (ASIA)—Shedding light on orphan diseases in autoimmunity. Autoimmun. Rev. 2018, 17, 440–448. [Google Scholar] [CrossRef] [PubMed]
- Pellegrino, P.; Clementi, E.; Radice, S. On vaccine’s adjuvants and autoimmunity: Current evidence and future perspectives. Autoimmun. Rev. 2015, 14, 880–888. [Google Scholar] [CrossRef]
- Guimarães, L.E.; Baker, B.; Perricone, C.; Shoenfeld, Y. Vaccines, adjuvants and autoimmunity. Pharmacol. Res. 2015, 100, 190–209. [Google Scholar] [CrossRef]
- Bruzzese, V.; Zullo, A.; Hassan, C. Connective tissue disease following hepatitis B vaccination. J. Clin. Rheumatol. 2013, 19, 280–281. [Google Scholar] [CrossRef]
- Perricone, C.; Shoenfeld, Y. Hepatitis B vaccination and undifferentiated connective tissue disease: Another brick in the wall of the autoimmune/inflammatory syndrome induced by adjuvants (Asia). J. Clin. Rheumatol. 2013, 19, 231–233. [Google Scholar] [CrossRef]
- Cruz-Tapias, P.; Blank, M.; Anaya, J.M.; Shoenfeld, Y. Infections and vaccines in the etiology of antiphospholipid syndrome. Curr. Opin. Rheumatol. 2012, 24, 389–393. [Google Scholar] [CrossRef] [PubMed]
- Bettencourt, A.; Carvalho, C.; Leal, B.; Brás, S.; Lopes, D.; Martins Da Silva, A.; Da Silva, B.M. The protective role of HLA-DRB1 13 in autoimmune diseases. J. Immunol. Res. 2015, 2015, 948723. [Google Scholar] [CrossRef] [PubMed]
- Yang, H.; Yao, Z.; Zhou, X.; Zhang, W.; Zhang, X.; Zhang, F. Immune-related adverse events of checkpoint inhibitors: Insights into immunological dysregulation. Clin. Immunol. 2020, 213, 108377. [Google Scholar] [CrossRef] [PubMed]
- Mazzarella, L.; Duso, B.A.; Trapani, D.; Belli, C.; D’Amico, P.; Ferraro, E.; Viale, G.; Curigliano, G. The evolving landscape of ‘next-generation’ immune checkpoint inhibitors: A review. Eur. J. Cancer 2019, 117, 14–31. [Google Scholar] [CrossRef]
- Michot, J.M.; Bigenwald, C.; Champiat, S.; Collins, M.; Carbonnel, F.; Postel-Vinay, S.; Berdelou, A.; Varga, A.; Bahleda, R.; Hollebecque, A.; et al. Immune-related adverse events with immune checkpoint blockade: A comprehensive review. Eur. J. Cancer 2016, 54, 139–148. [Google Scholar] [CrossRef]
- Jiang, Y.; Zhang, N.; Pang, H.; Gao, X.; Zhang, H. Risk and incidence of fatal adverse events associated with immune checkpoint inhibitors: A systematic review and meta-analysis. Ther. Clin. Risk Manag. 2019, 15, 293–302. [Google Scholar] [CrossRef]
- Nishino, M.; Sholl, L.M.; Hodi, F.S. Anti-PD-1-related pneumonitis during cancer immunotherapy. N. Engl. J. Med. 2015, 373, 288–290. [Google Scholar] [CrossRef]
- Haanen, J.B.A.G.; Carbonnel, F.; Robert, C.; Kerr, K.; Peters, S.; Larkin, J.; Jordan, K. Management of toxicities from immunotherapy: ESMO Clinical Practice Guidelines for diagnosis, treatment and follow-up. Ann. Oncol. 2017, 28, iv119–iv142. [Google Scholar] [CrossRef]
- Weber, J.S.; Dummer, R.; de Pril, V.; Lebbé, C.; Hodi, F.S. MDX010-20 Investigators. Patterns of onset and resolution of immune-related adverse events of special interest with ipilimumab: Detailed safety analysis from a phase 3 trial in patients with advanced melanoma. Cancer 2013, 119, 1675–1682. [Google Scholar] [CrossRef]
- Trinh, S.; Le, A.; Gowani, S.; La-Beck, N. Management of Immune-Related Adverse Events Associated with Immune Checkpoint Inhibitor Therapy: A Minireview of Current Clinical Guidelines. Asia Pac. J. Oncol. Nurs. 2019, 6, 154–160. [Google Scholar] [CrossRef]
- Darnell, E.P.; Mooradian, M.J.; Baruch, E.N.; Yilmaz, M.; Reynolds, K.L. Immune-Related Adverse Events (irAEs): Diagnosis, Management, and Clinical Pearls. Curr. Oncol. Rep. 2020, 22, 39. [Google Scholar] [CrossRef]
- Kanai, O.; Fujita, K.; Okamura, M.; Horimoto, K.; Takeda, K.; Hashimoto, K.; Nakatani, K.; Sawai, S.; Mio, T. Impact of nivolumab-induced fever on the treatment effect: A retrospective study. Eur. Respir. J. 2019, 54, PA368. [Google Scholar] [CrossRef]
- McGinnis, G.J.; Raber, J. CNS side effects of immune checkpoint inhibitors: Preclinical models, genetics and multimodality therapy. Immunotherapy 2017, 9, 929–941. [Google Scholar] [CrossRef] [PubMed]
- Byun, D.J.; Wolchok, J.D.; Rosenberg, L.M.; Girotra, M. Cancer immunotherapy-immune checkpoint blockade and associated endocrinopathies. Nat. Rev. Endocrinol. 2017, 13, 195–207. [Google Scholar] [CrossRef] [PubMed]
- De Moel, E.C.; Rozeman, E.A.; Kapiteijn, E.H.; Verdegaal, E.M.E.; Grummels, A.; Bakker, J.A.; Huizinga, T.W.J.; Haanen, J.B.; Toes, R.E.M.; van der Woude, D. Autoantibody development under treatment with immune-checkpoint inhibitors. Cancer Immunol. Res. 2019, 7, 6–11. [Google Scholar] [CrossRef] [PubMed]
- Giannicola, R.; D’Arrigo, G.; Botta, C.; Agostino, R.; Del Medico, P.; Falzea, A.C.; Barbieri, V.; Staropoli, N.; Del Giudice, T.; Pastina, P.; et al. Early blood rise in auto-antibodies to nuclear and smooth muscle antigens is predictive of prolonged survival and autoimmunity in metastatic-non-small cell lung cancer patients treated with PD-1 immune-check point blockade by nivolumab. Mol. Clin. Oncol. 2019, 11, 81–90. [Google Scholar] [CrossRef]
- Tahir, S.A.; Gao, J.; Miura, Y.; Blando, J.; Tidwell, R.S.S.; Zhao, H.; Subudhi, S.K.; Tawbi, H.; Keung, E.; Wargo, J.; et al. Autoimmune antibodies correlate with immune checkpoint therapy-induced toxicities. Proc. Natl. Acad. Sci. USA 2019, 116, 22246–22251. [Google Scholar] [CrossRef]
- Von Itzstein, M.S.; Khan, S.; Gerber, D.E. Investigational Biomarkers for Checkpoint Inhibitor Immune-Related Adverse Event Prediction and Diagnosis. Clin. Chem. 2020, 66, 779–793. [Google Scholar] [CrossRef]
- Hasan Ali, O.; Berner, F.; Bomze, D.; Fässler, M.; Diem, S.; Cozzio, A.; Jörger, M.; Früh, M.; Driessen, C.; Lenz, T.L.; et al. Human leukocyte antigen variation is associated with adverse events of checkpoint inhibitors. Eur. J. Cancer 2019, 107, 8–14. [Google Scholar] [CrossRef]
- Hoefsmit, E.P.; Rozeman, E.A.; Haanen, J.B.A.G.; Blank, C.U. Susceptible loci associated with autoimmune disease as potential biomarkers for checkpoint inhibitor-induced immune-related adverse events. ESMO Open 2019, 4, e000472. [Google Scholar] [CrossRef]
- Johnson, D.B.; Sullivan, R.J.; Ott, P.A.; Carlino, M.S.; Khushalani, N.I.; Ye, F.; Guminski, A.; Puzanov, I.; Lawrence, D.P.; Buchbinder, E.I.; et al. Ipilimumab therapy in patients with advanced melanoma and preexisting autoimmune disorders. JAMA Oncol. 2016, 2, 234–240. [Google Scholar] [CrossRef] [PubMed]
- Boland, P.; Pavlick, A.C.; Weber, J.; Sandigursky, S. Immunotherapy to treat malignancy in patients with pre-existing autoimmunity. J. Immunother. Cancer 2020, 8, e000356. [Google Scholar] [CrossRef]
- Toi, Y.; Sugawara, S.; Sugisaka, J.; Ono, H.; Kawashima, Y.; Aiba, T.; Kawana, S.; Saito, R.; Aso, M.; Tsurumi, K.; et al. Profiling Preexisting Antibodies in Patients Treated with Anti-PD-1 Therapy for Advanced Non-Small Cell Lung Cancer. JAMA Oncol. 2019, 5, 376–383. [Google Scholar] [CrossRef] [PubMed]
- Lidar, M.; Giat, E.; Garelick, D.; Horowitz, Y.; Amital, H.; Steinberg-Silman, Y.; Schachter, J.; Shappira-Frommer, R.; Markel, G. Rheumatic manifestations among cancer patients treated with immune checkpoint inhibitors. Autoimmun. Rev. 2018, 17, 284–289. [Google Scholar] [CrossRef] [PubMed]
- Naidoo, J.; Cappelli, L.C.; Forde, P.M.; Marrone, K.A.; Lipson, E.J.; Hammers, H.J.; Sharfman, W.H.; Le, D.T.; Baer, A.N.; Shah, A.A.; et al. Inflammatory Arthritis: A Newly Recognized Adverse Event of Immune Checkpoint Blockade. Oncologist 2017, 22, 627–630. [Google Scholar] [CrossRef]
- Puzanov, I.; Diab, A.; Abdallah, K.; Bingham, C.O., III; Brogdon, C.; Dadu, R.; Hamad, L.; Kim, S.; Lacouture, M.E.; LeBoeuf, N.R.; et al. Managing toxicities associated with immune checkpoint inhibitors: Consensus recommendations from the Society for Immunotherapy of Cancer (SITC) Toxicity Management Working Group. J. Immunother. Cancer 2017, 5, 95. [Google Scholar] [CrossRef]
- Hughes, J.; Vudattu, N.; Sznol, M.; Gettinger, S.; Kluger, H.; Lupsa, B.; Herold, K.C. Precipitation of autoimmune diabetes with anti-PD-1 immunotherapy. Diabetes Care 2015, 38, e55–e57. [Google Scholar] [CrossRef]
- Foley, P.J.; McGrath, D.S.; Puscinska, E.; Petrek, M.; Kolek, V.; Drabek, J.; Lympany, P.A.; Pantelidis, P.; Welsh, K.I.; Zielinski, J.; et al. Human leukocyte antigen-DRB1 position 11 residues are a common protective marker for sarcoidosis. Am. J. Respir. Cell Mol. Biol. 2001, 25, 272–277. [Google Scholar] [CrossRef]
- Kishore, A.; Petrek, M. Next-Generation Sequencing Based HLA Typing: Deciphering Immunogenetic Aspects of Sarcoidosis. Front. Genet. 2018, 9, 503. [Google Scholar] [CrossRef]
- Fingerlin, T.E.; Hamzeh, N.; Maier, L.A. Genetics of Sarcoidosis. Clin. Chest Med. 2015, 36, 569–584. [Google Scholar] [CrossRef]
- Grunewald, J.; Eklund, A.; Olerup, O. Human Leukocyte Antigen Class I Alleles and the Disease Course in Sarcoidosis Patients. Am. J. Respir. Crit. Care Med. 2004, 169, 696–702. [Google Scholar] [CrossRef]
- Lahtela, E.; Kankainen, M.; Sinisalo, J.; Selroos, O.; Lokki, M.L. Exome Sequencing Identifies Susceptibility Loci for Sarcoidosis Prognosis. Front. Immunol. 2019, 10, 2964. [Google Scholar] [CrossRef] [PubMed]
- Bogunia-Kubik, K.; Tomeczko, J.; Suchnicki, K.; Lange, A. HLA-DRB1*03, DRB1*11 or DRB1*12 and their respective DRB3 specificities in clinical variants of sarcoidosis. Tissue Antigens 2001, 57, 87–90. [Google Scholar] [CrossRef] [PubMed]
- Planck, A.; Eklund, A.; Yamaguchi, E.; Grunewald, J. Angiotensin-converting enzyme gene polymorphism in relation to HLA-DR in sarcoidosis. J. Intern. Med. 2002, 251, 217–222. [Google Scholar] [CrossRef] [PubMed]

| Shared Features between UCTD and ASIA | Main Findings |
|---|---|
| (A) UCTD patients had more environmental exposures to adjuvants as compared to controls. | UCTD were significantly more exposed to: (1) tetanus vaccination; (2) HBV vaccination; (3) metal implants; (4) proximity to metal factories and foundries (home located less than 1 km). Cigarette smoking and allergies were more frequent in UCTD. |
| (B) Half of UCTD exposed to major ASIA triggers. | Fifty-seven percent of patients with UCTD had been exposed to either vaccines containing adjuvants or silicone implants. |
| (C) UCTD exposed to major ASIA triggers displayed typical features of ASIA. | As compared with non-exposed UCTD patients, those exposed to major ASIA triggers displayed more frequently general weakness, chronic fatigue, irritable bowel syndrome. |
| (D) UCTD exposed to major ASIA triggers had familiarity for autoimmunity. | As compared with non-exposed UCTD patients, those exposed to major ASIA triggers had more frequently first-degree relatives with autoimmune diseases (56% vs. 33%). |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Borba, V.; Malkova, A.; Basantsova, N.; Halpert, G.; Andreoli, L.; Tincani, A.; Amital, H.; Shoenfeld, Y. Classical Examples of the Concept of the ASIA Syndrome. Biomolecules 2020, 10, 1436. https://doi.org/10.3390/biom10101436
Borba V, Malkova A, Basantsova N, Halpert G, Andreoli L, Tincani A, Amital H, Shoenfeld Y. Classical Examples of the Concept of the ASIA Syndrome. Biomolecules. 2020; 10(10):1436. https://doi.org/10.3390/biom10101436
Chicago/Turabian StyleBorba, Vânia, Anna Malkova, Natalia Basantsova, Gilad Halpert, Laura Andreoli, Angela Tincani, Howard Amital, and Yehuda Shoenfeld. 2020. "Classical Examples of the Concept of the ASIA Syndrome" Biomolecules 10, no. 10: 1436. https://doi.org/10.3390/biom10101436
APA StyleBorba, V., Malkova, A., Basantsova, N., Halpert, G., Andreoli, L., Tincani, A., Amital, H., & Shoenfeld, Y. (2020). Classical Examples of the Concept of the ASIA Syndrome. Biomolecules, 10(10), 1436. https://doi.org/10.3390/biom10101436






