Serum Adipocyte Fatty Acid-Binding Protein Level is Negatively Associated with Vascular Reactivity Index Measured by Digital Thermal Monitoring in Kidney Transplant Patients
Abstract
1. Introduction
2. Results
3. Discussion
4. Materials and Methods
4.1. Participants
4.2. Anthropometric Analysis
4.3. Biochemical Investigations
4.4. Endothelial Function Measurements
4.5. Statistical Analysis
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Kensinger, C.; Bian, A.; Fairchild, M.; Chen, G.; Lipworth, L.; Ikizler, T.A.; Birdwell, K.A. Long term evolution of endothelial function during kidney transplantation. BMC Nephrol. 2016, 17, 160. [Google Scholar] [CrossRef] [PubMed]
- Cardinal, H.; Dieude, M.; Hebert, M.J. Endothelial dysfunction in kidney transplantation. Front. Immunol. 2018, 9, 1130. [Google Scholar] [CrossRef] [PubMed]
- Van Ree, R.M.; Oterdoom, L.H.; de Vries, A.P.; Homan van der Heide, J.J.; van Son, W.J.; Navis, G.; Gans, R.O.; Bakker, S.J. Circulating markers of endothelial dysfunction interact with proteinuria in predicting mortality in renal transplant recipients. Transplantation 2008, 86, 1713–1719. [Google Scholar] [CrossRef] [PubMed]
- Schnabel, R.B.; Schulz, A.; Wild, P.S.; Sinning, C.R.; Wilde, S.; Eleftheriadis, M.; Herkenhoff, S.; Zeller, T.; Lubos, E.; Lackner, K.J.; et al. Noninvasive vascular function measurement in the community: Cross-sectional relations and comparison of methods. Circ. Cardiovasc. Imaging 2011, 4, 371–380. [Google Scholar] [CrossRef] [PubMed]
- Naghavi, M.; Yen, A.A.; Lin, A.W.; Tanaka, H.; Kleis, S. New indices of endothelial function measured by digital thermal monitoring of vascular reactivity: Data from 6084 patients registry. Int. J. Vasc. Med. 2016, 2016, 1348028. [Google Scholar] [CrossRef]
- Celermajer, D.S.; Sorensen, K.E.; Gooch, V.M.; Spiegelhalter, D.J.; Miller, O.I.; Sullivan, I.D.; Lloyd, J.K.; Deanfield, J.E. Non-invasive detection of endothelial dysfunction in children and adults at risk of atherosclerosis. Lancet 1992, 340, 1111–1115. [Google Scholar] [CrossRef]
- Ockner, R.K.; Manning, J.A.; Poppenhausen, R.B.; Ho, W.K. A binding protein for fatty acids in cytosol of intestinal mucosa, liver, myocardium, and other tissues. Science 1972, 177, 56–58. [Google Scholar] [CrossRef]
- Furuhashi, M. Fatty acid-binding protein 4 in cardiovascular and metabolic diseases. J. Atheroscler. Thromb. 2019, 26, 216–232. [Google Scholar] [CrossRef]
- Amri, E.Z.; Bertrand, B.; Ailhaud, G.; Grimaldi, P. Regulation of adipose cell differentiation. I. Fatty acids are inducers of the aP2 gene expression. J. Lipid Res. 1991, 32, 1449–1456. [Google Scholar]
- Terra, X.; Quintero, Y.; Auguet, T.; Porras, J.A.; Hernandez, M.; Sabench, F.; Aguilar, C.; Luna, A.M.; Del Castillo, D.; Richart, C. FABP 4 is associated with inflammatory markers and metabolic syndrome in morbidly obese women. Eur. J. Endocrinol. 2011, 164, 539–547. [Google Scholar] [CrossRef]
- Ota, H.; Furuhashi, M.; Ishimura, S.; Koyama, M.; Okazaki, Y.; Mita, T.; Fuseya, T.; Yamashita, T.; Tanaka, M.; Yoshida, H.; et al. Elevation of fatty acid-binding protein 4 is predisposed by family history of hypertension and contributes to blood pressure elevation. Am. J. Hypertens. 2012, 25, 1124–1130. [Google Scholar] [CrossRef] [PubMed]
- Fuseya, T.; Furuhashi, M.; Yuda, S.; Muranaka, A.; Kawamukai, M.; Mita, T.; Ishimura, S.; Watanabe, Y.; Hoshina, K.; Tanaka, M.; et al. Elevation of circulating fatty acid-binding protein 4 is independently associated with left ventricular diastolic dysfunction in a general population. Cardiovasc. Diabetol. 2014, 13, 126. [Google Scholar] [CrossRef] [PubMed]
- Huang, C.L.; Wu, Y.W.; Hsieh, A.R.; Hung, Y.H.; Chen, W.J.; Yang, W.S. Serum adipocyte fatty acid-binding protein levels in patients with critical illness are associated with insulin resistance and predict mortality. Crit. Care 2013, 17, R22. [Google Scholar] [CrossRef] [PubMed]
- Furuhashi, M.; Saitoh, S.; Shimamoto, K.; Miura, T. Fatty acid-binding protein 4 (FABP4): Pathophysiological insights and potent clinical biomarker of metabolic and cardiovascular diseases. Clin. Med. Insights Cardiol. 2015, 8, 23–33. [Google Scholar] [CrossRef] [PubMed]
- Huang, I.C.; Chang, C.C.; Lee, C.J.; Chen, Y.C.; Lee, M.C.; Hsu, B.G. Positive correlation of serum adipocyte fatty acid binding protein levels with metabolic syndrome in kidney transplantation patients. Int. J. Clin. Exp. Pathol. 2017, 10, 8727–8734. [Google Scholar]
- Oflaz, H.; Turkmen, A.; Turgut, F.; Pamukcu, B.; Umman, S.; Ucar, A.; Akyol, Y.; Uzun, S.; Kazancioglu, R.; Kurt, R.; et al. Changes in endothelial function before and after renal transplantation. Transpl. Int. 2006, 19, 333–337. [Google Scholar] [CrossRef] [PubMed]
- Fisher, R.M.; Eriksson, P.; Hoffstedt, J.; Hotamisligil, G.S.; Thorne, A.; Ryden, M.; Hamsten, A.; Arner, P. Fatty acid binding protein expression in different adipose tissue depots from lean and obese individuals. Diabetologia 2001, 44, 1268–1273. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Makowski, L.; Hotamisligil, G.S. Fatty acid binding proteins--the evolutionary crossroads of inflammatory and metabolic responses. J. Nutr. 2004, 134, 2464S–2468S. [Google Scholar] [CrossRef]
- Lee, M.Y.; Li, H.; Xiao, Y.; Zhou, Z.; Xu, A.; Vanhoutte, P.M. Chronic administration of BMS309403 improves endothelial function in apolipoprotein E-deficient mice and in cultured human endothelial cells. Br. J. Pharmacol. 2011, 162, 1564–1576. [Google Scholar] [CrossRef]
- Svensson, H.; Wetterling, L.; Andersson-Hall, U.; Jennische, E.; Eden, S.; Holmang, A.; Lönn, M. Adipose tissue and body composition in women six years after gestational diabetes: Factors associated with development of type 2 diabetes. Adipocyte 2018, 7, 229–237. [Google Scholar] [CrossRef]
- Furuhashi, M.; Ishimura, S.; Ota, H.; Hayashi, M.; Nishitani, T.; Tanaka, M.; Yoshida, H.; Shimamoto, K.; Hotamisligil, G.S.; Miura, T. Serum fatty acid-binding protein 4 is a predictor of cardiovascular events in end-stage renal disease. PLoS ONE 2011, 6, e27356. [Google Scholar] [CrossRef] [PubMed]
- Huang, I.C.; Hsu, B.G.; Chang, C.C.; Lee, C.J.; Wang, J.H. High levels of serum adipocyte fatty acid-binding protein predict cardiovascular events in coronary artery disease patients. Int. J. Med. Sci. 2018, 15, 1268–1274. [Google Scholar] [CrossRef] [PubMed]
- Makowski, L.; Boord, J.B.; Maeda, K.; Babaev, V.R.; Uysal, K.T.; Morgan, M.A.; Parker, R.A.; Suttles, J.; Fazio, S.; Hotamisligil, G.S.; et al. Lack of macrophage fatty-acid-binding protein aP2 protects mice deficient in apolipoprotein E against atherosclerosis. Nat. Med. 2001, 7, 699–705. [Google Scholar] [CrossRef] [PubMed]
- Aragones, G.; Ferre, R.; Lazaro, I.; Cabre, A.; Plana, N.; Merino, J.; Heras, M.; Girona, J.; Masana, L. Fatty acid-binding protein 4 is associated with endothelial dysfunction in patients with type 2 diabetes. Atherosclerosis 2010, 213, 329–331. [Google Scholar] [CrossRef] [PubMed]
- Furuhashi, M.; Yuda, S.; Muranaka, A.; Kawamukai, M.; Matsumoto, M.; Tanaka, M.; Moniwa, N.; Ohnishi, H.; Saitoh, S.; Shimamoto, K.; et al. Circulating fatty acid-binding protein 4 concentration predicts the progression of carotid atherosclerosis in a general population without medication. Circ. J. 2018, 82, 1121–1129. [Google Scholar] [CrossRef] [PubMed]
- Aragones, G.; Saavedra, P.; Heras, M.; Cabre, A.; Girona, J.; Masana, L. Fatty acid-binding protein 4 impairs the insulin-dependent nitric oxide pathway in vascular endothelial cells. Cardiovasc. Diabetol. 2012, 11, 72. [Google Scholar] [CrossRef] [PubMed]
- Lesniewski, L.A.; Connell, M.L.; Durrant, J.R.; Folian, B.J.; Anderson, M.C.; Donato, A.J.; Seals, D.R. B6D2F1 Mice are a suitable model of oxidative stress-mediated impaired endothelium-dependent dilation with aging. J. Gerontol. Ser. A Biol. Sci. Med. Sci. 2009, 64, 9–20. [Google Scholar] [CrossRef]
- Donato, A.J.; Gano, L.B.; Eskurza, I.; Silver, A.E.; Gates, P.E.; Jablonski, K.; Seals, D.R. Vascular endothelial dysfunction with aging: Endothelin-1 and endothelial nitric oxide synthase. Am. J. Physiol. Heart Circ. Physiol. 2009, 297, H425–H432. [Google Scholar] [CrossRef]
- Kunutsor, S.K.; Apekey, T.A.; Khan, H. Liver enzymes and risk of cardiovascular disease in the general population: A meta-analysis of prospective cohort studies. Atherosclerosis 2014, 236, 7–17. [Google Scholar] [CrossRef]
- Li, J.W.; Xu, C.; Fan, Y.; Wang, Y.; Xiao, Y.B. Can serum levels of alkaline phosphatase and phosphate predict cardiovascular diseases and total mortality in individuals with preserved renal function? A systemic review and meta-analysis. PLoS ONE 2014, 9, e102276. [Google Scholar] [CrossRef]
- Perticone, F.; Perticone, M.; Maio, R.; Sciacqua, A.; Andreucci, M.; Tripepi, G.; Corrao, S.; Mallamaci, F.; Sesti, G.; Zoccali, C. Serum alkaline phosphatase negatively affects endothelium-dependent vasodilation in naive hypertensive patients. Hypertension 2015, 66, 874–880. [Google Scholar] [CrossRef] [PubMed]
- Hu, X.; Ma, X.; Luo, Y.; Xu, Y.; Xiong, Q.; Pan, X.; Bao, Y.; Jia, W. Contribution of serum adipocyte fatty acid-binding protein levels to the presence of microalbuminuria in a Chinese hyperglycemic population. J. Diabetes Investig. 2017, 8, 582–589. [Google Scholar] [CrossRef] [PubMed]
- Carminatti, M.; Tedesco-Silva, H.; Silva Fernandes, N.M.; Sanders-Pinheiro, H. Chronic kidney disease progression in kidney transplant recipients: A focus on traditional risk factors. Nephrology 2019, 24, 141–147. [Google Scholar] [CrossRef] [PubMed]
| Characteristics | All Patients (n = 80) | Good Vascular Reactivity (n = 38) | Intermediate Vascular Reactivity (n = 30) | Poor Vascular Reactivity (n = 12) | p Value |
|---|---|---|---|---|---|
| Age (years) | 45.29 ± 10.61 | 45.03 ± 11.32 | 46.97 ± 9.80 | 48.58 ± 10.57 | 0.549 |
| KT duration (months) | 74.80 ± 51.50 | 70.87 ± 44.79 | 87.37 ± 55.15 | 55.83 ± 58.39 | 0.163 |
| Height (cm) | 161.39 ± 7.57 | 160.59 ± 6.96 | 161.40 ± 7.27 | 163.88 ± 10.00 | 0.429 |
| Body weight (kg) | 64.35 ± 13.16 | 64.80 ± 13.33 | 64.40 ± 12.71 | 62.79 ± 14.72 | 0.901 |
| Body mass index (kg/m2) | 24.65 ± 4.48 | 25.13 ± 5.08 | 24.60 ± 3.63 | 23.24 ± 4.45 | 0.448 |
| Vascular reactivity index | 1.87 ± 0.84 | 2.51 ± 0.56 | 1.61 ± 0.26 | 0.46 ± 0.31 | <0.001 * |
| SBP (mmHg) | 144.43 ± 19.00 | 143.05 ± 18.19 | 145.37 ± 21.71 | 146.42 ± 14.93 | 0.821 |
| DBP (mmHg) | 83.66 ± 12.51 | 84.42 ± 13.25 | 82.80 ± 12.73 | 83.42 ± 10.13 | 0.869 |
| Total cholesterol (mg/dL) | 189.94 ± 46.41 | 183.32 ± 37.72 | 200.40 ± 56.47 | 184.75 ± 42.40 | 0.298 |
| Triglyceride (mg/dL) | 127.00 (90.25–192.75) | 114.50 (85.50–198.25) | 128.50 (96.00–186.50) | 155.00 (99.25–194.25) | 0.566 |
| HDL-C (mg/dL) | 49.95 ± 15.48 | 49.55 ± 15.13 | 51.27 ± 16.63 | 47.92 ± 14.58 | 0.803 |
| Fasting glucose (mg/dL) | 96.00 (88.25–113.75) | 95.50 (87.00–107.50) | 99.50 (88.75–134.50) | 94.00 (87.50–122.50) | 0.379 |
| Blood urea nitrogen (mg/dL) | 24.00 (16.00–37.00) | 23.50 (16.75–29.75) | 26.00 (15.50–42.75) | 27.00 (15.00–38.50) | 0.893 |
| Creatinine (mg/dL) | 1.40 (1.00–1.90) | 1.30 (1.00–1.73) | 1.60 (0.98–2.30) | 1.35 (1.15–1.83) | 0.342 |
| eGFR (mL/min) | 56.17 ± 25.91 | 59.95 ± 22.66 | 52.35 ± 29.68 | 57.75 ± 23.55 | 0.596 |
| Total Calcium (mg/dL) | 9.14 ± 0.69 | 9.13 ± 0.66 | 9.12 ± 0.75 | 9.20 ± 0.66 | 0.938 |
| Phosphorus (mg/dL) | 3.36 ± 0.81 | 3.33 ± 0.80 | 3.41 ± 0.87 | 3.35 ± 0.73 | 0.925 |
| Alkaline phosphate (IU/L) | 79.13 ± 29.99 | 70.39 ± 24.38 | 82.47 ± 34.61 | 98.42 ± 27.61 | 0.012 * |
| GGT (U/L) | 30.00 (20.00–52.00) | 24.50 (17.00–42.50) | 23.00 (20.00–52.25) | 54.00 (33.25–81.75) | 0.032 * |
| A-FABP (ng/mL) | 34.34 (26.13–54.14) | 30.80 (17.30–37.93) | 35.07 (31.91–57.95) | 127.02 (35.11–166.03) | <0.001 * |
| iPTH (pg/mL) | 101.45 (57.28–160.65) | 91.15 (56.08–144.93) | 116.80 (59.75–173.00) | 90.50 (42.25–179.65) | 0.477 |
| Female, n (%) | 40 (50.0) | 22 (57.9) | 14 (46.7) | 4 (33.3) | 0.299 |
| Diabetes mellitus, n (%) | 39 (48.8) | 18 (47.4) | 16 (53.3) | 5 (41.7) | 0.770 |
| Hypertension, n (%) | 31 (38.8) | 11 (28.9) | 15 (50.0) | 5 (41.7) | 0.205 |
| Living donor, n (%) | 16 (20.0) | 4 (10.5) | 9 (30.0) | 3 (25.0) | 0.123 |
| Statin use, n (%) | 33 (41.2) | 13 (34.2) | 14 (46.7) | 6 (50) | 0.468 |
| Smoking, n (%) | 6 (7.5%) | 1 (2.6) | 3 (10) | 2 (16.7) | 0.221 |
| Tacrolimus use, n (%) | 53 (60.3) | 26 (68.4) | 20 (66.7) | 7 (58.3) | 0.811 |
| MMF use, n (%) | 48 (60.0) | 22 (55.9) | 19 (63.3) | 7 (58.3) | 0.895 |
| Steroid use, n (%) | 68 (85.0) | 32 (84.2) | 26 (86.7) | 10 (83.3) | 0.946 |
| Rapamycin use, n (%) | 8 (10.0) | 2 (5.3) | 5 (16.7) | 1 (8.3) | 0.291 |
| Cyclosporine use, n (%) | 14 (17.5) | 8 (21.1) | 3 (10.0) | 3 (25.0) | 0.374 |
| Variables | Vascular Reactivity Index | ||||
|---|---|---|---|---|---|
| Simple Linear Regression | Multivariable Linear Regression | ||||
| r | p Value | Beta | Adjusted R2 Change | p Value | |
| Female | 0.170 | 0.131 | - | - | - |
| Diabetes mellitus | −0.034 | 0.765 | - | - | - |
| Hypertension | −0.183 | 0.104 | - | - | - |
| Living donor | −0.111 | 0.329 | - | - | - |
| Statin use | −0.159 | 0.159 | - | - | - |
| Smoking | −0.145 | 0.199 | - | - | - |
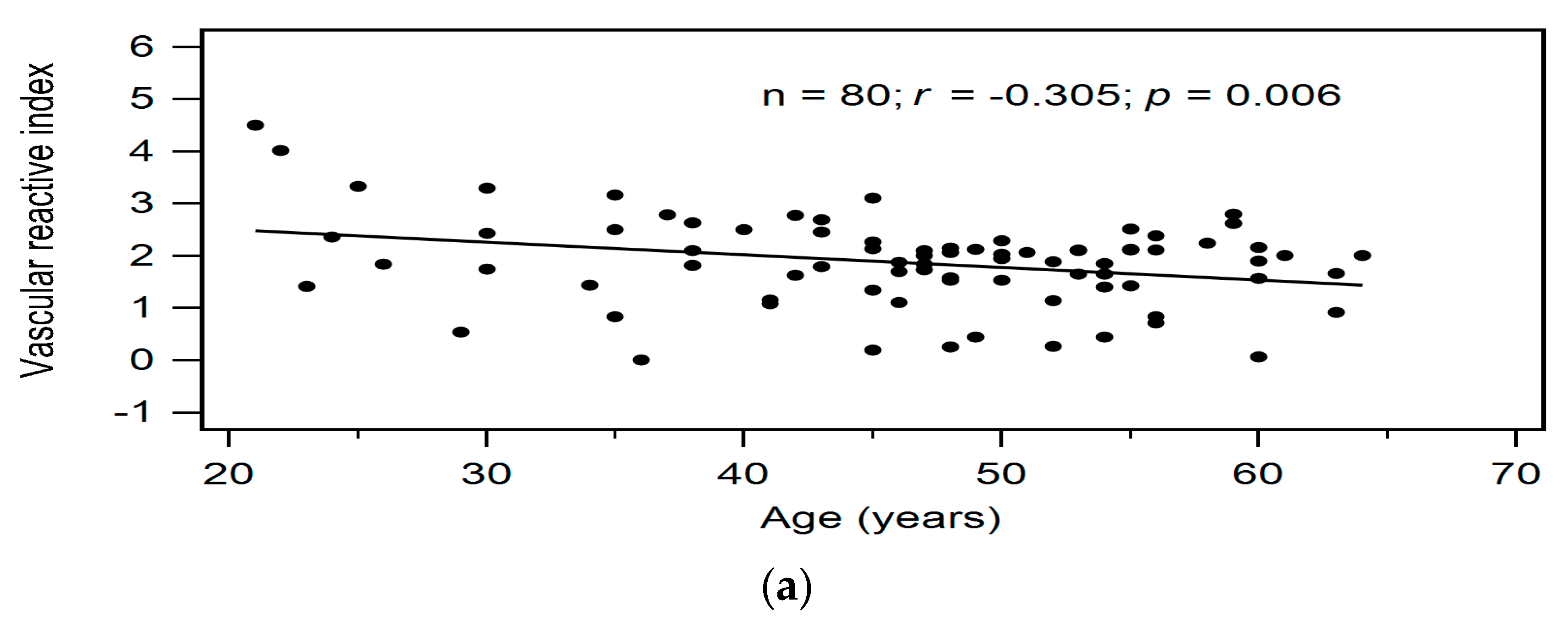
| Age (years) | −0.305 | 0.006 * | −0.283 | 0.072 | 0.003 * |
| KT duration (months) | −0.093 | 0.412 | - | - | - |
| Height (cm) | −0.138 | 0.224 | - | - | - |
| Body weight (kg) | −0.034 | 0.764 | - | - | - |
| Body mass index (kg/m2) | 0.038 | 0.740 | - | - | - |
| Systolic blood pressure (mmHg) | −0.160 | 0.156 | - | - | - |
| Diastolic blood pressure (mmHg) | 0.046 | 0.683 | - | - | - |
| Total cholesterol (mg/dL) | −0.096 | 0.397 | - | - | - |
| Log-Triglyceride (mg/dL) | −0.205 | 0.069 | - | - | - |
| HDL-C (mg/dL) | 0.079 | 0.487 | - | - | - |
| Log-Glucose (mg/dL) | −0.155 | 0.169 | - | - | - |
| Log-Blood urea nitrogen (mg/dL) | −0.111 | 0.329 | - | - | - |
| Log-Creatinine (mg/dL) | −0.084 | 0.458 | - | - | - |
| eGFR (mL/min) | 0.082 | 0.470 | - | - | - |
| Total Calcium (mg/dL) | −0.013 | 0.907 | - | - | - |
| Phosphorus (mg/dL) | 0.001 | 0.992 | - | - | - |
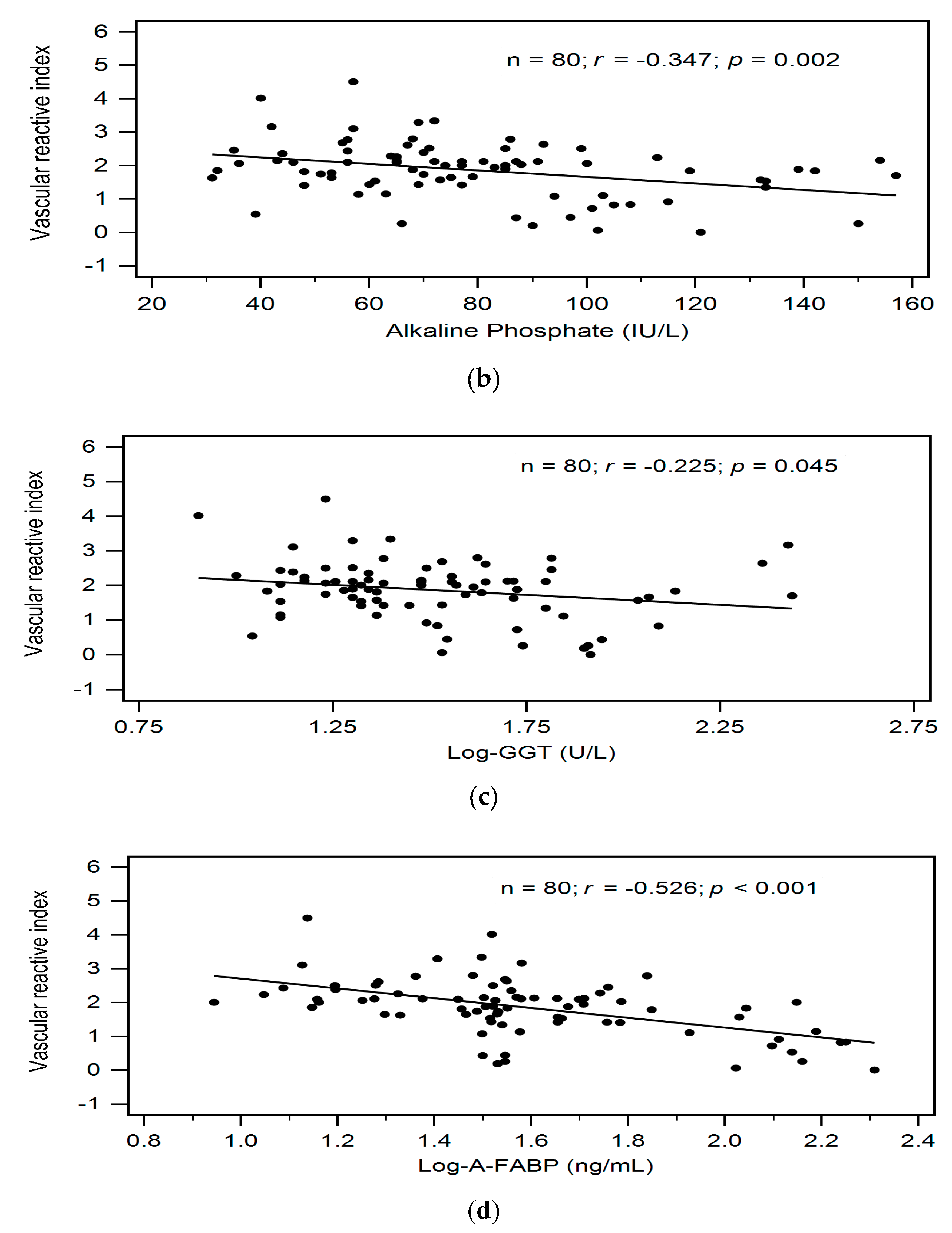
| Alkaline phosphate (IU/L) | −0.347 | 0.002 * | - | - | - |
| Log-GGT (U/L) | −0.225 | 0.045 * | - | - | - |
| Log-A-FABP (ng/mL) | −0.526 | <0.001 * | −0.514 | 0.268 | <0.001 * |
| Log-iPTH (pg/mL) | 0.033 | 0.775 | - | - | - |
© 2019 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Chen, T.-L.; Lee, M.-C.; Ho, C.-C.; Hsu, B.-G.; Tsai, J.-P. Serum Adipocyte Fatty Acid-Binding Protein Level is Negatively Associated with Vascular Reactivity Index Measured by Digital Thermal Monitoring in Kidney Transplant Patients. Metabolites 2019, 9, 159. https://doi.org/10.3390/metabo9080159
Chen T-L, Lee M-C, Ho C-C, Hsu B-G, Tsai J-P. Serum Adipocyte Fatty Acid-Binding Protein Level is Negatively Associated with Vascular Reactivity Index Measured by Digital Thermal Monitoring in Kidney Transplant Patients. Metabolites. 2019; 9(8):159. https://doi.org/10.3390/metabo9080159
Chicago/Turabian StyleChen, Tai-Li, Ming-Che Lee, Ching-Chung Ho, Bang-Gee Hsu, and Jen-Pi Tsai. 2019. "Serum Adipocyte Fatty Acid-Binding Protein Level is Negatively Associated with Vascular Reactivity Index Measured by Digital Thermal Monitoring in Kidney Transplant Patients" Metabolites 9, no. 8: 159. https://doi.org/10.3390/metabo9080159
APA StyleChen, T.-L., Lee, M.-C., Ho, C.-C., Hsu, B.-G., & Tsai, J.-P. (2019). Serum Adipocyte Fatty Acid-Binding Protein Level is Negatively Associated with Vascular Reactivity Index Measured by Digital Thermal Monitoring in Kidney Transplant Patients. Metabolites, 9(8), 159. https://doi.org/10.3390/metabo9080159







