The Effect of 9-Week Dietary Intervention on Anthropometric Parameters and Blood Pressure in Children with Excessive Body Weight
Abstract
1. Introduction
2. Materials and Methods
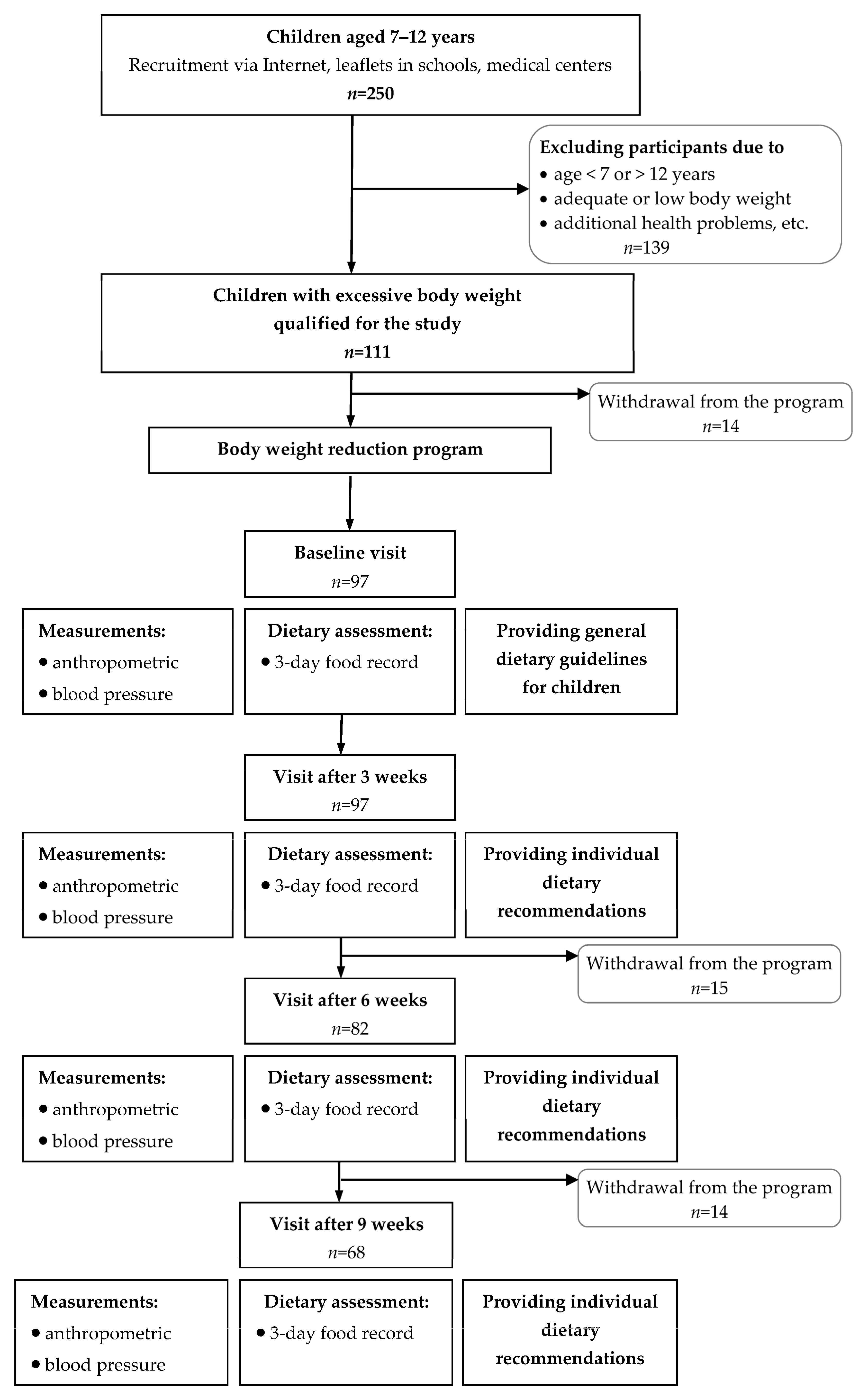
2.1. Study Design and Participants
2.2. Dietary Intervention
- Limited purchasing and consumption of sugar, sweets, candied fruit, sweetened beverages, fruit juices, high-fat products, fast food, and savory snacks;
- Increased access to and consumption of products such as vegetables, especially raw ones, and fruit, with special attention paid to GI;
- Introducing whole-grain products like bread, oats, groats, and whole-grain pasta to reduce the feeling of hunger;
- Drinking the appropriate amount of fluids, mainly water;
- Eating daily at least three portions of protein food sources like low-fat dairy, eggs, pulses, lean meats, and fatty fish;
- Greater variety in diet;
- Using appropriate culinary technics for meal/dish preparation, avoiding frying with fat;
- Mindful eating without any disruptors like phones, TV, etc.
2.3. Nutrition Education
2.4. Dietary Assessment
2.5. Anthropometric and Blood Pressure Measurements
2.6. Statistical Analysis
3. Results
3.1. Characteristics of Particpants
3.2. Dietary Changes as Effects of the Intervention
3.3. Anthropometric and Fat Mass Changes as Effects of the Intervention
3.4. Blood Pressure Changes as Effects of the Intervention
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Lobstein, T.; Jackson-Leach, R.; Moodie, M.L.; Hall, K.D.; Gortmaker, S.L.; Swinburn, B.A.; James, W.P.; Wang, Y.; McPherson, K. Child and adolescent obesity: Part of a bigger picture. Lancet 2015, 385, 2510–2520. [Google Scholar] [CrossRef]
- WHO. WHO Acceleration Plan to Stop Obesity; WHO: Geneva, Switzerland, 2022. [Google Scholar]
- World Health Organization. Obesity and Overweight. Available online: https://www.who.int/news-room/fact-sheets/detail/obesity-and-overweight (accessed on 3 July 2025).
- Brief Review of Results from Round 6 of COSI (WHO European Childhood Obesity Surveillance Initiative) 2022–2024. Available online: https://www.who.int/europe/publications/m/item/brief-review-of-results-from-round-6-of-cosi-2022-2024 (accessed on 3 July 2025).
- Gudelj Rakić, J.; Hamrik, Z.; Dzielska, A.; Felder-Puig, R.; Oja, L.; Bakalár, P.; Nardone, P.; Ciardullo, S.; Abdrakhmanova, S.; Adayeva, A.; et al. A Focus on Adolescent Physical Activity, Eating Behaviours, Weight Status and Body Image in Europe, Central Asia and Canada: Health Behaviour in School-aged Children International Report from the 2021/2022 Survey. Volume 4. World Health Organization. Regional Office for Europe. Available online: https://iris.who.int/handle/10665/376772 (accessed on 3 July 2025).
- Lobstein, T.; Jackson-Leach, R.; Powis, J.; Brinsden, H.; Gray, M. World Obesity Atlas 2023; World Obesity Federation: London, UK, 2023. [Google Scholar]
- World Health Organization. European Food and Nutrition Action Plan 2015–2020. Available online: https://www.who.int/europe/publications/i/item/9789289051231 (accessed on 3 July 2025).
- Uzogara, S.G. Obesity Epidemic, Medical and Quality of Life Consequences: A Review. Int. J. Public Health Res. 2017, 5, 1–12. [Google Scholar]
- Williams, E.P.; Mesidor, M.; Winters, K.; Dubbert, P.M.; Wyatt, S.B. Overweight and obesity: Prevalence, consequences, and causes of a growing public health problem. Curr. Obes. Rep. 2015, 4, 363–370. [Google Scholar] [CrossRef]
- Galler, A.; Thönnes, A.; Joas, J.; Joisten, C.; Körner, A.; Reinehr, T.; Röbl, M.; Schauerte, G.; Siegfried, W.; Weghuber, D.; et al. Clinical characteristics and outcomes of children, adolescents and young adults with overweight or obesity and mental health disorders. Int. J. Obes. 2024, 48, 423–432. [Google Scholar] [CrossRef]
- Horesh, A.; Tsur, A.M.; Bardugo, A.; Twig, G. Adolescent and childhood obesity and excess morbidity and mortality in young adulthood–a systematic review. Curr. Obes. Rep. 2021, 10, 301–310. [Google Scholar] [CrossRef]
- Jebeile, H.; Kelly, A.S.; O’Malley, G.; Baur, L.A. Obesity in children and adolescents: Epidemiology, causes, assessment, and management. Lancet Diabetes Endocrinol. 2022, 10, 351–365. [Google Scholar] [CrossRef]
- Moliterno, P.; Matjazic, J.; Widhalm, K. Improvement of body composition in 8- to 11-year-old schoolboys: Effects of a 6-months lifestyle intervention. A retrospective evaluation of the “EDDY-Kids” prevention study. Child Adolesc. Obes. 2022, 5, 28–41. [Google Scholar] [CrossRef]
- Hassapidou, M.; Duncanson, K.; Shrewsbury, V.; Ells, L.; Mulrooney, H.; Androutsos, O.; Vlassopoulos, A.; Rito, A.; Farpourt, N.; Brown, T.; et al. EASO and EFAD position statement on medical nutrition therapy for the management of overweight and obesity in children and adolescents. Obes. Facts 2023, 16, 29–52. [Google Scholar] [CrossRef]
- Southcombe, F.; Lin, F.; Krstic, S.; Sim, K.A.; Dennis, S.; Lingam, R.; Denney-Wilson, E. Targeted dietary approaches for the management of obesity and severe obesity in children and adolescents: A systematic review and meta-analysis. Clin. Obes. 2023, 13, e12564. [Google Scholar] [CrossRef] [PubMed]
- Kułaga, Z.; Różdżyńska-Świątkowska, A.; Grajda, A.; Gurzkowska, B.; Wojtyło, M.; Góźdź, M.; Świąder-Leśniak, A.; Litwin, M. Percentile charts for growth and nutritional status assessment in polish children and adolescents from birth to 18 year of age. Stand. Med. Pediatr. 2015, 12, 119–134. [Google Scholar]
- Cole, T.J.; Lobstein, T. Extended international (IOTF) body mass index cut-offs for thinness, overweight and obesity. Pediatr. Obes. 2012, 7, 284–294. [Google Scholar] [CrossRef] [PubMed]
- Jarosz, M. Normy Żywienia dla Populacji Polski; Instytut Żywności i Żywienia: Warszawa, Poland, 2017. [Google Scholar]
- Phillips, S.; Edlbeck, A.; Kirby, M.; Goday, P. Ideal body weight in children. Nutr. Clin. Pract. 2007, 22, 240–245. [Google Scholar]
- Parillo, M.; Licenziati, M.R.; Vacca, M.; De Marco, D.; Iannuzzi, A. Metabolic changes after a hypocaloric, low-glycemic-index diet in obese children. J. Endocrinol. Investig. 2012, 35, 629–633. [Google Scholar]
- Jarosz, M. Nutrition Standards for the Polish Population; Institute of Food and Nutrition: Warsaw, Poland, 2012. [Google Scholar]
- Jennings, A.; Welch, A.; van Sluijs, E.M.; Griffin, S.J.; Cassidy, A. Diet quality is independently associated with weight status in children aged 9–10 years. J. Nutr. 2011, 141, 453–459. [Google Scholar] [CrossRef]
- Stewart, A.; Marfell-Jones, M.; Olds, T.; De Ridder, H. International Standards for Anthropometric Assessment; ISAK: Lower Hutt, New Zealand, 2011. [Google Scholar]
- de Onis, M.; Onyango, A.W.; Borghi, E.; Siyam, A.; Nishida, C.; Siekmann, J. Development of a WHO growth reference for school-aged children and adolescents. Bull World Health Organ. 2007, 85, 660–667. [Google Scholar] [CrossRef]
- Browning, L.M.; Hsieh, S.D.; Ashwell, M. A systematic review of waist-to-height ratio as a screening tool for the prediction of cardiovascular disease and diabetes: 0.5 could be a suitable global boundary value. Nutr. Res. Rev. 2010, 23, 247–269. [Google Scholar] [CrossRef] [PubMed]
- National High Blood Pressure Education Program Working Group on High Blood Pressure in Children and Adolescents. The fourth report on the diagnosis, evaluation, and treatment of high blood pressure in children and adolescents. Pediatrics 2004, 114 (Suppl. 2), 555–576. [Google Scholar] [CrossRef]
- Kułaga, Z.; Grajda, A.; Gurzkowska, B.; Góźdź, M.; Wojtyło, M.; Świąder, A.; Różdżyńska-Świątkowska, A.; Litwin, M.; The OLA Research Group. Centile charts for blood pressure assessment in children and adolescents aged 3–18 years. Stand. Med. Pediatr. 2013, 1, 22–30. [Google Scholar]
- Strączek, K.; Horodnicka-Józwa, A.; Szmit-Domagalska, J.; Jackowski, T.; Safranow, K.; Petriczko, E.; Walczak, M. Familial dietary intervention in children with excess body weight and its impact on eating habits, anthropometric and biochemical parameters. Front. Endocrinol. 2022, 13, 1034148. [Google Scholar] [CrossRef]
- van Middelkoop, M.; Ligthart, K.A.; Paulis, W.D.; van Teeffelen, J.; Kornelisse, K.; Koes, B.W. A multidisciplinary intervention programme for overweight and obese children in deprived areas. Fam. Pract. 2017, 34, 702–707. [Google Scholar] [CrossRef]
- Bryant, M.; Farrin, A.; Christie, D.; Jebb, S.A.; Cooper, A.R.; Rudolf, M. Results of a feasibility randomised controlled trial (RCT) for WATCH IT: A programme for obese children and adolescents. J. Clin. Trials. 2011, 8, 755–764. [Google Scholar] [CrossRef]
- Okreglicka, K.; Bawa, S. Spożycie wybranych mikroskładników pokarmowych przez dzieci i młodzież w wieku 7–13 lat z otyłością prostą przed i po korekcie sposobu żywienia. Rocz. Panstw. Zakl. Hig. 2011, 62, 47–52. [Google Scholar]
- Chen, P.S.; Chang, K.C.; Chang, C.H.; Chen, Y.T.; Huang, H.W.; Tsai, S.M.; Yang, H.R.; Tung, Y.C.; Wu, W.W.; Chen, H.L. The effect of a multidisciplinary lifestyle modification program for obese and overweight children. J. Formos. Med. Assoc. 2022, 121, 1773–1785. [Google Scholar] [CrossRef]
- Pereira, A.R.; Oliveira, A. Dietary interventions to prevent childhood obesity: A literature review. Nutrients 2021, 13, 3447. [Google Scholar] [CrossRef]
- Wolske, G.; Joseph, M.; Rosenauer, H.; Widhalm, K. Hypertension among obese children and youth age 8-12: Project EDDY-Kids 2019. Child Adolesc. Obes. 2021, 4, 117–126. [Google Scholar] [CrossRef]
- Rajjo, T.; Almasri, J.; Al Nofal, A.; Farah, W.; Alsawas, M.; Ahmed, A.T.; Mohammed, K.; Kanwar, A.; Asi, N.; Wang, Z.; et al. The association of weight loss and cardiometabolic outcomes in obese children: Systematic review and meta-regression. J. Clin. Endocrinol. Metab. 2017, 102, 758–762. [Google Scholar] [CrossRef] [PubMed]
- Dixon, L.B.; Tershakovec, A.M.; McKenzie, J.; Shannon, B. Diet quality of young children who received nutrition education promoting lower dietary fat. Public Health Nutr. 2000, 3, 411–416. [Google Scholar] [CrossRef]
- Drenowatz, C.; Shook, R.P.; Hand, G.A.; Hébert, J.R.; Blair, S.N. The independent association between diet quality and body composition. Sci Rep. 2014, 4, 4928. [Google Scholar] [CrossRef] [PubMed]
- Echouffo-Tcheugui, J.B.; Ahima, R.S. Does diet quality or nutrient quantity contribute more to health? J. Clin. Investig. 2019, 129, 3969–3970. [Google Scholar] [CrossRef] [PubMed]
- Magalhães, P.; Vilas, C.; Pereira, B.; Silva, C.; Oliveira, H.; Aguiar, C.; Rosário, P. Children’s Perceived Barriers to a Healthy Diet: The Influence of Child and Community-Related Factors. Int. J. Environ. Res. Public Health 2022, 19, 2069. [Google Scholar] [CrossRef]
- Enright, G.; Allman-Farinelli, M.; Redfern, J. Effectiveness of family-based behavior change interventions on obesity-related behavior change in children: A realist synthesis. Int. J. Environ. Res. Public Health 2020, 17, 4099. [Google Scholar] [CrossRef] [PubMed]
| No. | Intake | Score | ||
|---|---|---|---|---|
| 0 | 1 | 2 | ||
| 1 | Total fat (% of energy/d) | <30 | 30–40 | >40 |
| 2 | Saturated fat (% of energy/d) | <10 | 10–13 | >13 |
| 3 | Cholesterol (mg/d) | <300 | 300–400 | >400 |
| 4 | Fruit and vegetables (servings/d) | ≥5 | 3–4 | 0–2 |
| 5 | Breads and cereals (servings/d) | ≥6 | 4–5 | 0–3 |
| 6 | Protein (% RDA) | <200 | 200–250 | >250 |
| 7 | Sodium (mg/d) | <2400 | 2400–3400 | >3400 |
| 8 | Calcium (% RDA) | >100 | 67–100 | <67 |
| Sum | 0–16 | |||
| Variable | Population | |||
|---|---|---|---|---|
| Total, n = 68 | Girls, n = 38 | Boys, n = 30 | p-Value * | |
| Children’s age: 7–9 years 10–12 years | 41.2 58.8 | 48.1 51.9 | 33.3 66.7 | NS |
| Living area: Town City | 52.6 47.4 | 53.8 46.2 | 51.1 48.9 | NS |
| Maternal age: 19–30 years 31–45 years | 72.2 27.8 | 69.2 30.8 | 75.6 24.4 | NS |
| Parental age: 19–30 years 31–45 years | 51.5 48.5 | 55.8 44.2 | 46.7 53.3 | NS |
| Maternal education: Vocational Secondary University | 26.8 42.3 30.9 | 26.9 40.4 32.7 | 26.7 44.4 28.9 | NS |
| Parental education: Vocational Secondary University | 43.3 35.1 21.6 | 44.2 32.7 23.1 | 42.2 37.8 20.0 | NS |
| Maternal BMI status: Normal weight Overweight Obesity | 44.3 42.3 13.4 | 48.1 36.5 15.4 | 40.0 48.9 11.1 | NS |
| Parental BMI status: Normal weight Overweight Obesity | 45.4 36.1 18.5 | 50.0 26.9 23.1 | 40.0 46.7 13.3 | NS |
| Nutrients | Dietary Intervention | p-Value * | Change (%) | ||
|---|---|---|---|---|---|
| Recommendations [18] | Baseline n = 68 | 9 Weeks n = 68 | |||
| Energy (kcal) 1 | 1550–2050 | 1899 ± 147 | 1612 ± 155 | ||
| 1936 | 1626 | <0.001 | ↓ 16.1% | ||
| 1285–2294 | 1190–2085 | ||||
| Protein % of total energy intake | 10–20 | 18.9 ± 1.7 | 19.0 ± 2.0 | NS | ↑ 0.5% |
| 19.0 | 18.9 | ||||
| 14.8–22.5 | 14.7–23.5 | ||||
| Fat % of total energy intake | <30 | 28.0 ± 3.2 | 25.7 ± 2.9 | <0.001 | ↓ 8.5% |
| 27.9 | 25.4 | ||||
| 19.3–34.6 | 19.5–31.9 | ||||
| Carbohydrates % of total energy intake | 45–65 | 53.1 ± 3.5 | 55.4 ± 3.2 | <0.001 | ↑ 4.3% |
| 53.3 | 55.4 | ||||
| 46.3–63.7 | 49.0–61.7 | ||||
| Saccharose (g) | <10% of total energy for total sugars | 23.1 ± 7.7 | 20.0 ± 7.4 | 0.006 | ↓ 13.4% |
| 23.1 | 19.5 | ||||
| 4.7–43.6 | 6.4–41.8 | ||||
| Dietary fiber (g) | 16 (7–9 years) 19 (10–12 years) | 15.0 ± 3.0 | 16.7 ± 3.2 | 0.001 | ↑ 11.3% |
| 15.1 | 16.3 | ||||
| 7.1–22.5 | 10.9–26.3 | ||||
| Calcium (mg) | 800 (7–9 years) 1100 (10–12 years) | 458.8 ± 128.3 454.7 158.9–863.5 | 507.7 ± 139.3 506.2 187.2–1027.3 | 0.021 | ↑ 10.7% |
| Iron (mg) | 4 (7–9 years) 7–8 (10–12 years) | 6.6 ± 1.1 6.5 4.5–10.2 | 7.9 ± 1.1 8.0 5.6–10.2 | <0.001 | ↑ 19.7% |
| Vitamin C (mg) | 40 | 52.7 ± 15.3 51.5 21.8–101.1 | 58.7 ± 23.0 55.9 27.6–135.4 | <0.001 | ↑ 11.4% |
| Population | Diet Quality | Dietary Intervention | p-Value * | |||
|---|---|---|---|---|---|---|
| Baseline | 9 Weeks | |||||
| n | % | n | % | |||
| Total n = 68 | - Good | 0 | 0.0 | 8 | 11.8 | <0.001 |
| - Sufficient | 60 | 88.2 | 60 | 88.2 | ||
| - Poor | 8 | 11.8 | 0 | 0.0 | ||
| Girls n = 38 | - Good | 0 | 0.0 | 4 | 10.5 | 0.014 |
| - Sufficient | 36 | 94.7 | 34 | 89.5 | ||
| - Poor | 2 | 5.3 | 0 | 0.0 | ||
| Boys n = 30 | - Good | 0 | 0.0 | 4 | 13.3 | 0.002 |
| - Sufficient | 24 | 80.0 | 26 | 86.7 | ||
| - Poor | 6 | 20.0 | 0 | 0.0 | ||
| p-Value ** | NS | NS | ||||
| Group | Dietary Intervention | p-Value * | Change (%) | |||
|---|---|---|---|---|---|---|
| Baseline | 3 Weeks | 6 Weeks | 9 Weeks | |||
| BMI z-score | ||||||
| Total 1 n = 68 | 2.80 ± 1.1 a | 2.59 ± 1.1 b | 2.56 ± 1.0 c | 2.50 ± 1.1 d | 0.001 | ↓ 10.7% |
| 2.51 | 2.41 | 2.44 | 2.44 | |||
| 0.7–5.6 | 0.5–5.6 | 0.4–5.3 | 0.3–5.1 | |||
| Girls n = 38 | 2.80 ± 1.1 a | 2.60 ± 1.1 b | 2.51 ± 0.9 b | 2.40 ± 1.0 c | 0.001 | ↓ 14.3% |
| 2.52 | 2.40 | 2.44 | 2.37 | |||
| 1.0–5.6 | 0.8–5.6 | 0.8–5.3 | 0.8–5.1 | |||
| Boys n = 30 | 2.72 ± 1.1 a | 2.57 ± 1.1 b | 2.62 ± 1.1 b | 2.64 ± 1.2 c | 0.001 | ↓ 3.0% |
| 2.52 | 2.41 | 2.42 | 2.63 | |||
| 0.7–5.6 | 0.5–5.4 | 0.4–5.1 | 0.3–5.1 | |||
| p-Value ** | NS | NS | NS | NS | ||
| LMS (%) | ||||||
| Total n = 68 | 151.9 ± 18.9 a | 148.8 ± 18.4 b | 148.2 ± 17.8 c | 146.7 ± 18.4 d | 0.001 | ↓ 3.4% |
| 149.1 | 146.2 | 145.7 | 144.9 | |||
| 116–197 | 113–197 | 112–192 | 111–189 | |||
| Girls n = 38 | 150.3 ± 19.5 a | 146.9 ± 18.6 b | 145.0 ± 16.5 b | 143.0 ± 17.1 c | 0.001 | ↓ 4.9% |
| 146.5 | 142.9 | 141.4 | 141.2 | |||
| 120–197 | 117–197 | 117–192 | 117–189 | |||
| Boys n = 30 | 153.6 ± 18.2 a | 151.8 ± 18.1 b | 151.8 ± 18.8 b | 151.3 ± 19.2 c | 0.001 | ↓ 1.5% |
| 151.4 | 151.3 | 149.9 | 152.3 | |||
| 116–194 | 113–191 | 112–186 | 111–186 | |||
| p-Value ** | NS | NS | NS | NS | ||
| WC (cm) | ||||||
| Total n = 68 | 87.7 ± 10.0 a | 86.7 ± 10.2 b | 86.2 ± 9.6 c | 85.2 ± 9.8 d | 0.001 | ↓ 2.9% |
| 86.0 | 86.0 | 85.0 | 83.5 | |||
| 66–112 | 66–112 | 68–107 | 63–107 | |||
| Girls n = 38 | 86.2 ± 10.3 a | 85.3 ± 10.5 b | 84.3 ± 9.2 c | 83.3 ± 9.9 d | 0.001 | ↓ 3.4% |
| 84.0 | 83.0 | 82.0 | 82.0 | |||
| 66–112 | 66–112 | 68–107 | 63–107 | |||
| Boys n = 30 | 89.5 ± 9.4 a | 88.5 ± 9.6 b | 88.3 ± 9.8 c | 87.5 ± 9.3 d | 0.001 | ↓ 2.2% |
| 89.0 | 90.0 | 88.5 | 87.5 | |||
| 72–110 | 71–106 | 70–105 | 69–103 | |||
| p-Value ** | NS | NS | NS | NS | ||
| WHtR | ||||||
| Total n = 68 | 0.53 ± 0.04 a | 0.52 ± 0.04 b | 0.52 ± 0.04 c | 0.51 ± 0.05 d | 0.001 | ↓ 3.7% |
| 0.52 | 0.52 | 0.51 | 0.50 | |||
| 0.42–0.66 | 0.43–0.65 | 0.43–0.64 | 0.43–0.64 | |||
| Girls n = 38 | 0.52 ± 0.04 a | 0.51 ± 0.04 b | 0.51 ± 0.04 c | 0.50 ± 0.04 d | 0.001 | ↓ 3.8% |
| 0.52 | 0.51 | 0.50 | 0.50 | |||
| 0.42–0.63 | 0.43–0.61 | 0.43–0.60 | 0.43–0.60 | |||
| Boys n = 30 | 0.54 ± 0.04 a | 0.53 ± 0.04 b | 0.53 ± 0.05 c | 0.52 ± 0.05 d | 0.001 | ↓ 3.7% |
| 0.53 | 0.53 | 0.52 | 0.52 | |||
| 0.47–0.66 | 0.47–0.65 | 0.45–0.65 | 0.45–0.64 | |||
| p-Value ** | NS | NS | NS | NS | ||
| Group | Dietary Intervention | p-Value * | Change (%) | |||
|---|---|---|---|---|---|---|
| Baseline | 3 Weeks | 6 Weeks | 9 Weeks | |||
| FM (kg) | ||||||
| Total 1 n = 68 | 19.7 ± 7.5 a | 18.6 ± 6.9 b | 18.5 ± 6.5 c | 18.2 ± 6.6 c | 0.001 | ↓ 7.6% |
| 18.4 | 17.6 | 17.2 | 16.8 | |||
| 7–43 | 7–37 | 7–35 | 7–36 | |||
| Girls n = 38 | 18.7 ± 7.9 a | 17.6 ± 7.1 b | 17.0 ± 6.3 c | 17.0 ± 6.7 c | 0.001 | ↓ 9.1% |
| 16.8 | 16.0 | 15.8 | 15.6 | |||
| 7–43 | 7–37 | 7–35 | 7–36 | |||
| Boys n = 30 | 20.9 ± 6.8 a | 19.8 ± 6.5 b | 20.1 ± 6.4 b | 19.7 ± 6.2 b | 0.001 | ↓ 5.7% |
| 20.0 | 19.0 | 20.6 | 19.7 | |||
| 10–39 | 10–33 | 9–32 | 10–31 | |||
| p-Value ** | NS | NS | 0.032 | NS | ||
| FMI (kg/m2) | ||||||
| Total n = 68 | 9.0 ± 2.8 a | 8.5 ± 2.6 b | 8.4 ± 2.5 c | 8.4 ± 2.6 c | 0.001 | ↓ 6.7% |
| 8.5 | 7.9 | 7.9 | 7.8 | |||
| 5–17 | 5–16 | 4–15 | 5–15 | |||
| Girls n = 38 | 8.7 ± 2.9 a | 8.2 ± 2.6 b | 7.9 ± 2.4 b | 7.9 ± 2.5 b | 0.001 | ↓ 9.2% |
| 8.1 | 7.5 | 7.4 | 7.2 | |||
| 5–17 | 5–16 | 5–15 | 5–15 | |||
| Boys n = 30 | 9.4 ± 2.6 a | 8.9 ± 2.5 b | 8.9 ± 2.6 bc | 8.9 ± 2.6 c | 0.001 | ↓ 5.3% |
| 9.1 | 8.7 | 8.9 | 8.7 | |||
| 5–16 | 5–14 | 4–14 | 5–14 | |||
| p-Value ** | NS | NS | NS | NS | ||
| Group | Dietary Intervention | p-Value * | Change (%) | |||
|---|---|---|---|---|---|---|
| Baseline | 3 Weeks | 6 Weeks | 9 Weeks | |||
| SBP (mm/Hg) | ||||||
| Total 1 n = 68 | 109.2 ± 11.4 a | 107.9 ± 9.2 a | 104.7 ± 10.7 b | 105.3 ± 7.9 ab | 0.001 | ↓ 3.6% |
| 109.0 | 107.3 | 105.0 | 104.3 | |||
| 69–140 | 77–127 | 73–129 | 87–125 | |||
| Girls n = 38 | 108.8 ± 10.7 | 107.5 ± 7.7 | 104.8 ± 10.8 | 104.7 ± 8.4 | NS | ↓ 3.2% |
| 107.2 | 106.3 | 104.7 | 103.7 | |||
| 86–133 | 94–126 | 73–129 | 87–125 | |||
| Boys n = 30 | 109.7 ± 12.2 a | 107.0 ± 10.8 a | 104.5 ± 10.8 b | 106.2 ± 7.2 ab | 0.028 | ↓ 3.2% |
| 111.0 | 109.0 | 106.2 | 106.3 | |||
| 69–140 | 77–127 | 73–121 | 87–119 | |||
| p-Value ** | NS | NS | NS | NS | ||
| DBP (mm/Hg) | ||||||
| Total n = 68 | 73.8 ± 9.9 a | 71.3 ± 7.4 a | 69.9 ± 7.9 b | 69.8 ± 7.6 b | 0.002 | ↓ 5.4% |
| 73.7 | 70.3 | 69.0 | 69.7 | |||
| 43–114 | 57–91 | 56–88 | 48–84 | |||
| Girls n = 38 | 72.8 ± 8.4 | 71.4 ± 7.7 | 70.1 ± 8.4 | 69.1 ± 8.7 | NS | ↓ 5.1% |
| 72.0 | 71.0 | 69.2 | 69.0 | |||
| 53–89 | 58–91 | 56–88 | 48–84 | |||
| Boys n = 30 | 74.9 ± 11.5 a | 71.1 ± 7.1 a | 69.6 ± 7.4 b | 70.6 ± 5.8 b | 0.010 | ↓ 5.7% |
| 74.7 | 70.0 | 69.0 | 71.5 | |||
| 43–114 | 57–89 | 58–88 | 61–82 | |||
| p-Value ** | NS | NS | NS | NS | ||
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Gajda, K.; Jeruszka-Bielak, M.; Górnicka, M.; Keser, I.; Hamulka, J. The Effect of 9-Week Dietary Intervention on Anthropometric Parameters and Blood Pressure in Children with Excessive Body Weight. Metabolites 2025, 15, 621. https://doi.org/10.3390/metabo15090621
Gajda K, Jeruszka-Bielak M, Górnicka M, Keser I, Hamulka J. The Effect of 9-Week Dietary Intervention on Anthropometric Parameters and Blood Pressure in Children with Excessive Body Weight. Metabolites. 2025; 15(9):621. https://doi.org/10.3390/metabo15090621
Chicago/Turabian StyleGajda, Karolina, Marta Jeruszka-Bielak, Magdalena Górnicka, Irena Keser, and Jadwiga Hamulka. 2025. "The Effect of 9-Week Dietary Intervention on Anthropometric Parameters and Blood Pressure in Children with Excessive Body Weight" Metabolites 15, no. 9: 621. https://doi.org/10.3390/metabo15090621
APA StyleGajda, K., Jeruszka-Bielak, M., Górnicka, M., Keser, I., & Hamulka, J. (2025). The Effect of 9-Week Dietary Intervention on Anthropometric Parameters and Blood Pressure in Children with Excessive Body Weight. Metabolites, 15(9), 621. https://doi.org/10.3390/metabo15090621








