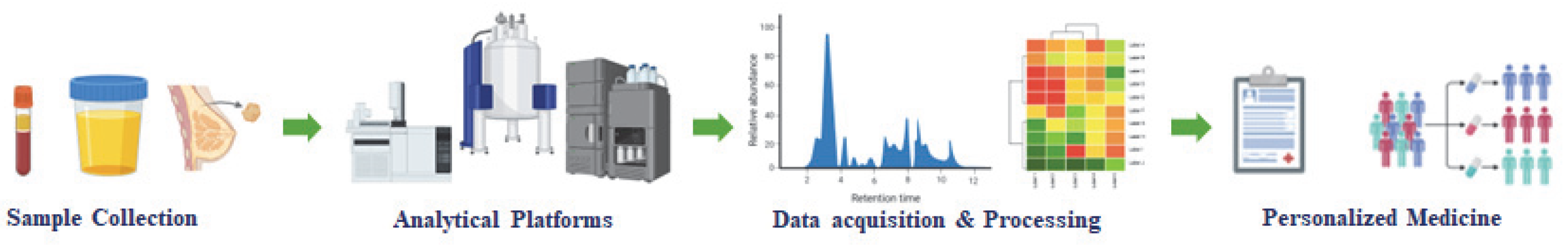
Metabolomics in Breast Cancer: From Biomarker Discovery to Personalized Medicine
Abstract
1. Introduction
2. Metabolomic Biomarkers in BC and Profiling Techniques
3. Metabolic Reprogramming and Therapy Resistance
4. Metabolite-Based Therapeutic Strategies
5. Metabolomics for Personalized Medicine
6. Challenges and Future Directions in Metabolomics for BC
7. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Abbreviations
| BC | Breast cancer |
| MS | Mass spectrometry |
| NMR | Nuclear magnetic resonance |
| IARC | International Agency for Research on Cancer |
| DCIS | Ductal carcinoma in situ |
| CE | Capillary electrophoresis |
| LC | Lung cancer |
| TNBC | Triple-negative breast cancer |
| GC-MS | Gas chromatography–mass spectrometry |
| LC−HRMS | Liquid chromatography coupled with high-resolution mass spectrometry |
| UHPLC-MS/MS | Ultra-high-performance liquid chromatography coupled with mass spectrometry |
| LC−MS/MS | Liquid chromatography coupled with mass spectrometry |
| GC-HRMS | Gas chromatography coupled with high-resolution mass spectrometry |
| CTL | Control |
| MRI | Magnetic resonance imaging |
| FASN | Fatty acid synthase |
| TCA | Tricarboxylic acid |
| HKII | Hexokinase II |
| M2 PKM2 | Pyruvate kinase |
| LDHA | Lactate dehydrogenase A |
| FAO | Fatty acid oxidation |
| RT-qPCR | Real-time quantitative reverse transcription polymerase chain reaction |
| ROS | Reactive oxygen species |
| HIF-1α | Hypoxia-inducible factor 1-alpha |
| KD | Ketogenic diet |
| scRNA-seq | Single-cell RNA sequencing |
| ICP-EOS | Inductively coupled plasma optical emission spectroscopy |
| AUROC | Receiver operating characteristic curve |
| CTBP2 | C-terminal binding protein 2 |
| HR-MAS | High-resolution magic angle spinning |
References
- Bray, F.; Laversanne, M.; Sung, H.; Ferlay, J.; Siegel, R.L.; Soerjomataram, I.; Jemal, A. Global Cancer Statistics 2022: GLOBOCAN Estimates of Incidence and Mortality Worldwide for 36 Cancers in 185 Countries. CA Cancer J. Clin. 2024, 74, 229–263. [Google Scholar] [CrossRef] [PubMed]
- Arnold, M.; Morgan, E.; Rumgay, H.; Mafra, A.; Singh, D.; Laversanne, M.; Vignat, J.; Gralow, J.R.; Cardoso, F.; Siesling, S.; et al. Current and Future Burden of Breast Cancer: Global Statistics for 2020 and 2040. Breast 2022, 66, 15–23. [Google Scholar] [CrossRef]
- Orrantia-Borunda, E.; Anchondo-Nuñez, P.; Acuña-Aguilar, L.E.; Gómez-Valles, F.O.; Ramírez-Valdespino, C.A. Subtypes of Breast Cancer. In Breast Cancer; Exon Publications: Brisbane, Australia, 2022; pp. 31–42. [Google Scholar] [CrossRef]
- Xiong, X.; Zheng, L.W.; Ding, Y.; Chen, Y.F.; Cai, Y.W.; Wang, L.P.; Huang, L.; Liu, C.C.; Shao, Z.M.; Yu, K. Da Breast Cancer: Pathogenesis and Treatments. Signal Transduct. Target. Ther. 2025, 10, 49. [Google Scholar] [CrossRef]
- Danzi, F.; Pacchiana, R.; Mafficini, A.; Scupoli, M.T.; Scarpa, A.; Donadelli, M.; Fiore, A. To Metabolomics and beyond: A Technological Portfolio to Investigate Cancer Metabolism. Signal Transduct. Target. Ther. 2023, 8, 137. [Google Scholar] [CrossRef]
- Kohli, M.; Poulogiannis, G. Harnessing the Power of Metabolomics for Precision Oncology: Current Advances and Future Directions. Cells 2025, 14, 402. [Google Scholar] [CrossRef]
- Zhang, T.N.; Wen, R.; Yang, Y.H.; Yang, N.; Liu, C.F. Integration of Transcriptomic, Proteomic, and Metabolomic Data to Identify LncRNA RPvt1 Associations in Lipopolysaccharide-Treated H9C2 Cardiomyocytes. Front. Genet. 2023, 14, 1278830. [Google Scholar] [CrossRef]
- Wishart, D.S. Metabolomics for Investigating Physiological and Pathophysiological Processes. Physiol. Rev. 2019, 99, 1819–1875. [Google Scholar] [CrossRef] [PubMed]
- Qiu, S.; Cai, Y.; Yao, H.; Lin, C.; Xie, Y.; Tang, S.; Zhang, A. Small Molecule Metabolites: Discovery of Biomarkers and Therapeutic Targets. Signal Transduct. Target. Ther. 2023, 8, 132. [Google Scholar] [CrossRef] [PubMed]
- Zhang, Y.; Guo, L.; Qiu, Z.; Lv, Y.; Chen, G.; Li, E. Early Diagnosis of Breast Cancer from Exhaled Breath by Gas Chromatography-Mass Spectrometry (GC/MS) Analysis: A Prospective Cohort Study. J. Clin. Lab. Anal. 2020, 34, e23526. [Google Scholar] [CrossRef]
- González Olmedo, C.; Díaz Beltrán, L.; Madrid García, V.; Palacios Ferrer, J.L.; Cano Jiménez, A.; Urbano Cubero, R.; Pérez del Palacio, J.; Díaz, C.; Vicente, F.; Sánchez Rovira, P. Assessment of Untargeted Metabolomics by Hydrophilic Interaction Liquid Chromatography−Mass Spectrometry to Define Breast Cancer Liquid Biopsy-Based Biomarkers in Plasma Samples. Int. J. Mol. Sci. 2024, 25, 5098. [Google Scholar] [CrossRef]
- An, R.; Yu, H.; Wang, Y.; Lu, J.; Gao, Y.; Xie, X.; Zhang, J. Integrative Analysis of Plasma Metabolomics and Proteomics Reveals the Metabolic Landscape of Breast Cancer. Cancer Metab. 2022, 10, 13. [Google Scholar] [CrossRef] [PubMed]
- Anh, N.K.; Lee, A.; Phat, N.K.; Yen, N.T.H.; Thu, N.Q.; Tien, N.T.N.; Kim, H.S.; Kim, T.H.; Kim, D.H.; Kim, H.Y.; et al. Combining Metabolomics and Machine Learning to Discover Biomarkers for Early-Stage Breast Cancer Diagnosis. PLoS ONE 2024, 19, e0311810. [Google Scholar] [CrossRef] [PubMed]
- Li, X.; Wen, X.; Luo, Z.; Tian, Y.; Qian, C.; Zhang, J.; Ling, R.; Duan, Y. Development of a Headspace-Solid Phase Microextraction Gas Chromatography-High Resolution Mass Spectrometry Method for Analyzing Volatile Organic Compounds in Urine: Application in Breast Cancer Biomarker Discovery. Clin. Chim. Acta 2023, 540, 117236. [Google Scholar] [CrossRef]
- Silva, C.L.; Perestrelo, R.; Capelinha, F.; Tomás, H.; Câmara, J.S. An Integrative Approach Based on GC–QMS and NMR Metabolomics Data as a Comprehensive Strategy to Search Potential Breast Cancer Biomarkers. Metabolomics 2021, 17, 72. [Google Scholar] [CrossRef]
- Silva, C.; Perestrelo, R.; Silva, P.; Capelinha, F.; Tomás, H.; Câmara, J.S. Volatomic Pattern of Breast Cancer and Cancer-Free Tissues as a Powerful Strategy to Identify Potential Biomarkers. Analyst 2019, 144, 4153–4161. [Google Scholar] [CrossRef]
- Murata, T.; Yanagisawa, T.; Kurihara, T.; Kaneko, M.; Ota, S.; Enomoto, A.; Tomita, M.; Sugimoto, M.; Sunamura, M.; Hayashida, T.; et al. Salivary Metabolomics with Alternative Decision Tree-Based Machine Learning Methods for Breast Cancer Discrimination. Breast Cancer Res. Treat. 2019, 177, 591–601. [Google Scholar] [CrossRef]
- Cavaco, C.; Pereira, J.A.M.; Taunk, K.; Taware, R.; Rapole, S.; Nagarajaram, H.; Câmara, J.S. Screening of Salivary Volatiles for Putative Breast Cancer Discrimination: An Exploratory Study Involving Geographically Distant Populations. Anal. Bioanal. Chem. 2018, 410, 4459–4468. [Google Scholar] [CrossRef] [PubMed]
- Birhanu, A.G. Mass Spectrometry-Based Proteomics as an Emerging Tool in Clinical Laboratories. Clin. Proteom. 2023, 20, 32. [Google Scholar] [CrossRef]
- Almalki, A.H. Recent Analytical Advances for Decoding Metabolic Reprogramming in Lung Cancer. Metabolites 2023, 13, 1037. [Google Scholar] [CrossRef]
- Roca, M.; Alcoriza, M.I.; Garcia-Cañaveras, J.C.; Lahoz, A. Reviewing the Metabolome Coverage Provided by LC-MS: Focus on Sample Preparation and Chromatography-A Tutorial. Anal. Chim. Acta 2021, 1147, 38–55. [Google Scholar] [CrossRef]
- Emwas, A.H.; Roy, R.; McKay, R.T.; Tenori, L.; Saccenti, E.; Nagana Gowda, G.A.; Raftery, D.; Alahmari, F.; Jaremko, L.; Jaremko, M.; et al. NMR Spectroscopy for Metabolomics Research. Metabolites 2019, 9, 123. [Google Scholar] [CrossRef]
- Peng, Y.; Zhang, Z.; He, L.; Li, C.; Liu, M. NMR Spectroscopy for Metabolomics in the Living System: Recent Progress and Future Challenges. Anal. Bioanal. Chem. 2024, 416, 2319–2334. [Google Scholar] [CrossRef]
- Silva, C.L.; Olival, A.; Perestrelo, R.; Silva, P.; Tomás, H.; Câmara, J.S. Untargeted Urinary1H NMR-Based Metabolomic Pattern as a Potential Platform in Breast Cancer Detection. Metabolites 2019, 9, 269. [Google Scholar] [CrossRef] [PubMed]
- Jacob, M.; Lopata, A.L.; Dasouki, M.; Abdel Rahman, A.M. Metabolomics toward Personalized Medicine. Mass. Spectrom. Rev. 2019, 38, 221–238. [Google Scholar] [CrossRef]
- Wojtowicz, W.; Tarkowski, R.; Olczak, A.; Szymczycha-Madeja, A.; Pohl, P.; Maciejczyk, A.; Trembecki; Matkowski, R.; Młynarz, P. Serum Metabolite and Metal Ions Profiles for Breast Cancer Screening. Sci. Rep. 2024, 14, 24559. [Google Scholar] [CrossRef] [PubMed]
- Nagandla, H.; Thomas, C. Estrogen Signals through ERβ in Breast Cancer; What We Have Learned since the Discovery of the Receptor. Receptors 2024, 3, 182–200. [Google Scholar] [CrossRef]
- Sirocchi, C.; Biancucci, F.; Donati, M.; Bogliolo, A.; Magnani, M.; Menotta, M.; Montagna, S. Exploring Machine Learning for Untargeted Metabolomics Using Molecular Fingerprints. Comput. Methods Programs Biomed. 2024, 250, 108163. [Google Scholar] [CrossRef] [PubMed]
- Galal, A.; Talal, M.; Moustafa, A. Applications of Machine Learning in Metabolomics: Disease Modeling and Classification. Front. Genet. 2022, 13, 1017340. [Google Scholar] [CrossRef]
- Yao, N.; Li, W.; Xu, G.; Duan, N.; Yu, G.; Qu, J. Choline Metabolism and Its Implications in Cancer. Front. Oncol. 2023, 13, 1234887. [Google Scholar] [CrossRef]
- Hirschhaeuser, F.; Sattler, U.G.A.; Mueller-Klieser, W. Lactate: A Metabolic Key Player in Cancer. Cancer Res. 2011, 71, 6921–6925. [Google Scholar] [CrossRef]
- Lv, Y.; Yang, X.; Song, Y.; Yang, D.; Zheng, K.; Zhou, S.; Xie, H.; Guo, R.; Tang, S. The Correlation Between Essential Amino Acid Tryptophan, Lysine, Phenylalanine and Chemotherapy of Breast Cancer. Technol. Cancer Res. Treat. 2024, 23, 15330338241286872. [Google Scholar] [CrossRef]
- Gadwal, A.; Panigrahi, P.; Khokhar, M.; Sharma, V.; Setia, P.; Vishnoi, J.R.; Elhence, P.; Purohit, P. A Critical Appraisal of the Role of Metabolomics in Breast Cancer Research and Diagnostics. Clin. Chim. Acta 2024, 561, 119836. [Google Scholar] [CrossRef]
- Koopaie, M.; Kolahdooz, S.; Fatahzadeh, M.; Manifar, S. Salivary Biomarkers in Breast Cancer Diagnosis: A Systematic Review and Diagnostic Meta-analysis. Cancer Med. 2022, 11, 2644. [Google Scholar] [CrossRef] [PubMed]
- Dougan, M.M.; Li, Y.; Chu, L.W.; Haile, R.W.; Whittemore, A.S.; Han, S.S.; Moore, S.C.; Sampson, J.N.; Andrulis, I.L.; John, E.M.; et al. Metabolomic Profiles in Breast Cancer: A Pilot Case-Control Study in the Breast Cancer Family Registry. BMC Cancer 2018, 18, 532. [Google Scholar] [CrossRef] [PubMed]
- Song, H.; Tang, X.; Liu, M.; Wang, G.; Yuan, Y.; Pang, R.; Wang, C.; Zhou, J.; Yang, Y.; Zhang, M.; et al. Multi-Omic Analysis Identifies Metabolic Biomarkers for the Early Detection of Breast Cancer and Therapeutic Response Prediction. iScience 2024, 27, 110682. [Google Scholar] [CrossRef]
- Schmidt, D.R.; Patel, R.; Kirsch, D.G.; Lewis, C.A.; Vander Heiden, M.G.; Locasale, J.W. Metabolomics in Cancer Research and Emerging Applications in Clinical Oncology. CA Cancer J. Clin. 2021, 71, 333–358. [Google Scholar] [CrossRef]
- Kaur, R.; Gupta, S.; Kulshrestha, S.; Khandelwal, V.; Pandey, S.; Kumar, A.; Sharma, G.; Kumar, U.; Parashar, D.; Das, K. Metabolomics-Driven Biomarker Discovery for Breast Cancer Prognosis and Diagnosis. Cells 2024, 14, 5. [Google Scholar] [CrossRef]
- Yu, D.; Zhong, Q.; Wang, Y.; Yin, C.; Bai, M.; Zhu, J.; Chen, J.; Li, H.; Hong, W. Lactylation: The Metabolic Accomplice Shaping Cancer’s Response to Radiotherapy and Immunotherapy. Ageing Res. Rev. 2025, 104, 102670. [Google Scholar] [CrossRef] [PubMed]
- Chen, J.; Huang, Z.; Chen, Y.; Tian, H.; Chai, P.; Shen, Y.; Yao, Y.; Xu, S.; Ge, S.; Jia, R. Lactate and Lactylation in Cancer. Signal Transduct. Target. Ther. 2025, 10, 38. [Google Scholar] [CrossRef]
- Saadatmand, S.; Geuzinge, H.A.; Rutgers, E.J.T.; Mann, R.M.; de Roy van Zuidewijn, D.B.W.; Zonderland, H.M.; Tollenaar, R.A.E.M.; Lobbes, M.B.I.; Ausems, M.G.E.M.; van ’t Riet, M.; et al. MRI versus Mammography for Breast Cancer Screening in Women with Familial Risk (FaMRIsc): A Multicentre, Randomised, Controlled Trial. Lancet Oncol. 2019, 20, 1136–1147. [Google Scholar] [CrossRef]
- Shi, J.; Li, J.; Gao, Y.; Chen, W.; Zhao, L.; Li, N.; Tian, J. The Screening Value of Mammography for Breast Cancer: An Overview of 28 Systematic Reviews with Evidence Mapping. J. Cancer Res. Clin. Oncol. 2025, 151, 102. [Google Scholar] [CrossRef] [PubMed]
- Suri, G.S.; Kaur, G.; Carbone, G.M.; Shinde, D. Metabolomics in Oncology. Cancer Rep. 2023, 6, e1795. [Google Scholar] [CrossRef]
- Faubert, B.; Solmonson, A.; DeBerardinis, R.J. Metabolic Reprogramming and Cancer Progression. Science 2020, 368, eaaw5473. [Google Scholar] [CrossRef]
- de Visser, K.E.; Joyce, J.A. The Evolving Tumor Microenvironment: From Cancer Initiation to Metastatic Outgrowth. Cancer Cell 2023, 41, 374–403. [Google Scholar] [CrossRef]
- Lim, S.; Liu, H.; Da Silva, L.M.; Arora, R.; Liu, Z.; Phillips, J.B.; Schmitt, D.C.; Vu, T.; Mcclellan, S.; Lin, Y.; et al. Immunoregulatory Protein B7-H3 Reprograms Glucose Metabolism in Cancer Cells by ROS-Mediated Stabilization of HIF1α. Cancer Res. 2016, 76, 2231–2242. [Google Scholar] [CrossRef] [PubMed]
- Luo, H.; Chen, C.-Y.; Li, X.; Zhang, X.; Su, C.-W.; Liu, Y.; Cao, T.; Hao, L.; Wang, M.; Kang, J.X. Increased Lipogenesis Is Critical for self-renewal and Growth of Breast Cancer Stem Cells: Impact of Omega-3 Fatty Acids. Stem Cells 2021, 39, 1660–1670. [Google Scholar] [CrossRef]
- Schmidt, K.; Thatcher, A.; Grobe, A.; Broussard, P.; Hicks, L.; Gu, H.; Ellies, L.G.; Sears, D.D.; Kalachev, L.; Kroll, E. The Combined Treatment with Ketogenic Diet and Metformin Slows Tumor Growth in Two Mouse Models of Triple Negative Breast Cancer. Transl. Med. Commun. 2024, 9, 21. [Google Scholar] [CrossRef] [PubMed]
- Son, D.-S.; Done, K.A.; Son, J.; Izban, M.G.; Virgous, C.; Lee, E.-S.; Adunyah, S.E. Intermittent Fasting Attenuates Obesity-Induced Triple-Negative Breast Cancer Progression by Disrupting Cell Cycle, Epithelial–Mesenchymal Transition, Immune Contexture, and Proinflammatory Signature. Nutrients 2024, 16, 2101. [Google Scholar] [CrossRef]
- Dai, C.; Arceo, J.; Arnold, J.; Sreekumar, A.; Dovichi, N.J.; Li, J.; Littlepage, L.E. Metabolomics of Oncogene-Specific Metabolic Reprogramming during Breast Cancer. Cancer Metab. 2018, 6, 5. [Google Scholar] [CrossRef]
- Buga, A.; Harper, D.G.; Sapper, T.N.; Hyde, P.N.; Fell, B.; Dickerson, R.; Stoner, J.T.; Kackley, M.L.; Crabtree, C.D.; Decker, D.D.; et al. Feasibility and Metabolic Outcomes of a Well-Formulated Ketogenic Diet as an Adjuvant Therapeutic Intervention for Women with Stage IV Metastatic Breast Cancer: The Keto-CARE Trial. PLoS ONE 2024, 19, e0296523. [Google Scholar] [CrossRef]
- Paixão, E.M.d.S.; Oliveira, A.C.d.M.; Pizato, N.; Muniz-Junqueira, M.I.; Magalhães, K.G.; Nakano, E.Y.; Ito, M.K. The Effects of EPA and DHA Enriched Fish Oil on Nutritional and Immunological Markers of Treatment Naïve Breast Cancer Patients: A Randomized Double-Blind Controlled Trial. Nutr. J. 2017, 16, 71. [Google Scholar] [CrossRef]
- Liu, X.; Meng, Q.; Fan, W.; Ning, L.; Ge, L. The Effects of Intermittent Fasting on Anthropometric Indices, Glycemic Profile, Chemotherapy-Related Toxicity, and Subjective Perception in Gynecological and Breast Cancer Patients: A Systematic Review and Meta-Analysis. BMC Cancer 2025, 25, 419. [Google Scholar] [CrossRef]
- Lee, J.; Campbell, E.K.; Culakova, E.; Blanchard, L.M.; Wixom, N.; Peppone, L.J.; Campbell, T.M. Changes in the Consumption of Isoflavones, Omega-6, and Omega-3 Fatty Acids in Women with Metastatic Breast Cancer Adopting a Whole-Food, Plant-Based Diet: Post-Hoc Analysis of Nutrient Intake Data from an 8-Week Randomized Controlled Trial. Front. Nutr. 2024, 11, 1338392. [Google Scholar] [CrossRef] [PubMed]
- Zhao, T.; Mu, X.; You, Q. Succinate: An Initiator in Tumorigenesis and Progression. Oncotarget 2017, 8, 53819. [Google Scholar] [CrossRef] [PubMed]
- Clay, R.; Li, K.; Jin, L. Metabolic Signaling in the Tumor Microenvironment. Cancers 2025, 17, 155. [Google Scholar] [CrossRef]
- Liu, S.; Li, Y.; Yuan, M.; Song, Q.; Liu, M. Correlation between the Warburg Effect and Progression of Triple-Negative Breast Cancer. Front. Oncol. 2023, 12, 1060495. [Google Scholar] [CrossRef] [PubMed]
- Liao, M.; Yao, D.; Wu, L.; Luo, C.; Wang, Z.; Zhang, J.; Liu, B. Targeting the Warburg Effect: A Revisited Perspective from Molecular Mechanisms to Traditional and Innovative Therapeutic Strategies in Cancer. Acta Pharm. Sin. B 2024, 14, 953–1008. [Google Scholar] [CrossRef]
- Hammond, N.G.; Cameron, R.B.; Faubert, B. Beyond Glucose and Warburg: Finding the Sweet Spot in Cancer Metabolism Models. Npj Metab. Health Dis. 2024, 2, 11. [Google Scholar] [CrossRef]
- Liu, B.; Peng, Q.; Wang, Y.W.; Qiu, J.; Zhu, J.; Ma, R. Prognostic and Clinicopathological Significance of Fatty Acid Synthase in Breast Cancer: A Systematic Review and Meta-Analysis. Front. Oncol. 2023, 13, 1153076. [Google Scholar] [CrossRef]
- Vanauberg, D.; Schulz, C.; Lefebvre, T. Involvement of the Pro-Oncogenic Enzyme Fatty Acid Synthase in the Hallmarks of Cancer: A Promising Target in Anti-Cancer Therapies. Oncogenesis 2023, 12, 16. [Google Scholar] [CrossRef]
- Chen, C.I.; Chan, H.W.; Shen, C.Y.; Chuang, H.Y. Targeting Fatty Acid Synthase to Halt Tumor Progression and Enhance Radiosensitivity in Breast Cancer Cells. J. Med. Biol. Eng. 2024, 44, 903–913. [Google Scholar] [CrossRef]
- Yoo, H.C.; Yu, Y.C.; Sung, Y.; Han, J.M. Glutamine Reliance in Cell Metabolism. Exp. Mol. Med. 2020, 52, 1496–1516. [Google Scholar] [CrossRef]
- Hanahan, D. Hallmarks of Cancer: New Dimensions. Cancer Discov. 2022, 12, 31–46. [Google Scholar] [CrossRef] [PubMed]
- de Heer, E.C.; Jalving, M.; Harris, A.L. HIFs, Angiogenesis, and Metabolism: Elusive Enemies in Breast Cancer. J. Clin. Investig. 2020, 130, 5074. [Google Scholar] [CrossRef] [PubMed]
- Liberti, M.V.; Locasale, J.W. The Warburg Effect: How Does It Benefit Cancer Cells? Trends Biochem. Sci. 2016, 41, 211. [Google Scholar] [CrossRef]
- Heiden, M.G.V.; Cantley, L.C.; Thompson, C.B. Understanding the Warburg Effect: The Metabolic Requirements of Cell Proliferation. Science 2009, 324, 1029–1033. [Google Scholar] [CrossRef]
- Nong, S.; Han, X.; Xiang, Y.; Qian, Y.; Wei, Y.; Zhang, T.; Tian, K.; Shen, K.; Yang, J.; Ma, X. Metabolic Reprogramming in Cancer: Mechanisms and Therapeutics. MedComm 2023, 4, e218. [Google Scholar] [CrossRef]
- Monaco, M.E. Fatty Acid Metabolism in Breast Cancer Subtypes. Oncotarget 2017, 8, 29487. [Google Scholar] [CrossRef]
- Vogel, F.C.E.; Chaves-Filho, A.B.; Schulze, A. Lipids as Mediators of Cancer Progression and Metastasis. Nat. Cancer 2024, 5, 16–29. [Google Scholar] [CrossRef]
- Ma, Y.; Temkin, S.M.; Hawkridge, A.M.; Guo, C.; Wang, W.; Wang, X.Y.; Fang, X. Fatty Acid Oxidation: An Emerging Facet of Metabolic Transformation in Cancer. Cancer Lett. 2018, 435, 92. [Google Scholar] [CrossRef]
- Georgakopoulos-Soares, I.; Chartoumpekis, D.V.; Kyriazopoulou, V.; Zaravinos, A. EMT Factors and Metabolic Pathways in Cancer. Front. Oncol. 2020, 10, 499. [Google Scholar] [CrossRef] [PubMed]
- Alwahsh, M.; Hamadneh, Y.; Marchan, R.; Dahabiyeh, L.A.; Alhusban, A.A.; Hasan, A.; Alrawabdeh, J.; Hergenröder, R.; Hamadneh, L. Glutathione and Xanthine Metabolic Changes in Tamoxifen Resistant Breast Cancer Cell Lines Are Mediated by Down-Regulation of GSS and XDH and Correlated to Poor Prognosis. J. Cancer 2024, 15, 4047–4058. [Google Scholar] [CrossRef] [PubMed]
- Zhang, N.; Huang, Y.; Wang, G.; Xiang, Y.; Jing, Z.; Zeng, J.; Yu, F.; Pan, X.; Zhou, W.; Zeng, X. Metabolomics Assisted by Transcriptomics Analysis to Reveal Metabolic Characteristics and Potential Biomarkers Associated with Treatment Response of Neoadjuvant Therapy with TCbHP Regimen in HER2 + Breast Cancer. Breast Cancer Res. 2024, 26, 64. [Google Scholar] [CrossRef]
- Ni, J.; Xi, X.; Xiao, S.; Xiao, X. Silencing of CircHIPK3 Sensitizes Paclitaxel-Resistant Breast Cancer Cells to Chemotherapy by Regulating HK2 Through Targeting MiR-1286. Cancer Manag. Res. 2021, 13, 5573. [Google Scholar] [CrossRef]
- Gu, Y.; Yang, R.; Zhang, Y.; Guo, M.; Takehiro, K.; Zhan, M.; Yang, L.; Wang, H. Molecular Mechanisms and Therapeutic Strategies in Overcoming Chemotherapy Resistance in Cancer. Mol. Biomed. 2025, 6, 2. [Google Scholar] [CrossRef] [PubMed]
- Liu, S.; Zhang, X.; Wang, W.; Li, X.; Sun, X.; Zhao, Y.; Wang, Q.; Li, Y.; Hu, F.; Ren, H. Metabolic Reprogramming and Therapeutic Resistance in Primary and Metastatic Breast Cancer. Mol. Cancer 2024, 23, 261. [Google Scholar] [CrossRef] [PubMed]
- Panda, V.K.; Mishra, B.; Mahapatra, S.; Swain, B.; Malhotra, D.; Saha, S.; Khanra, S.; Mishra, P.; Majhi, S.; Kumari, K.; et al. Molecular Insights on Signaling Cascades in Breast Cancer: A Comprehensive Review. Cancers 2025, 17, 234. [Google Scholar] [CrossRef] [PubMed]
- Pavitra, E.; Kancharla, J.; Gupta, V.K.; Prasad, K.; Sung, J.Y.; Kim, J.; Tej, M.B.; Choi, R.; Lee, J.H.; Han, Y.K.; et al. The Role of NF-ΚB in Breast Cancer Initiation, Growth, Metastasis, and Resistance to Chemotherapy. Biomed. Pharmacother. 2023, 163, 114822. [Google Scholar] [CrossRef] [PubMed]
- Wang, Z.H.; Zheng, Z.Q.; Jia, S.; Liu, S.N.; Xiao, X.F.; Chen, G.Y.; Liang, W.Q.; Lu, X.F. Trastuzumab Resistance in HER2-Positive Breast Cancer: Mechanisms, Emerging Biomarkers and Targeting Agents. Front. Oncol. 2022, 12, 1006429. [Google Scholar] [CrossRef]
- Currie, E.; Schulze, A.; Zechner, R.; Walther, T.C.; Farese, R.V. Cellular Fatty Acid Metabolism and Cancer. Cell Metab. 2013, 18, 153–161. [Google Scholar] [CrossRef]
- Flavin, R.; Peluso, S.; Nguyen, P.L.; Loda, M. Fatty Acid Synthase as a Potential Therapeutic Target in Cancer. Future Oncol. 2010, 6, 551–562. [Google Scholar] [CrossRef] [PubMed]
- Fisusi, F.A.; Akala, E.O. Drug Combinations in Breast Cancer Therapy. Pharm. Nanotechnol. 2019, 7, 3. [Google Scholar] [CrossRef] [PubMed]
- Li, Y.; Li, Z. Potential Mechanism Underlying the Role of Mitochondria in Breast Cancer Drug Resistance and Its Related Treatment Prospects. Front. Oncol. 2021, 11, 629614. [Google Scholar] [CrossRef] [PubMed]
- Taneja, N.; Chauhan, A.; Kulshreshtha, R.; Singh, S. HIF-1 Mediated Metabolic Reprogramming in Cancer: Mechanisms and Therapeutic Implications. Life Sci. 2024, 352, 122890. [Google Scholar] [CrossRef]
- Abdelmaksoud, N.M.; Abulsoud, A.I.; Doghish, A.S.; Abdelghany, T.M. From Resistance to Resilience: Uncovering Chemotherapeutic Resistance Mechanisms; Insights from Established Models. Biochim. Biophys. Acta (BBA)-Rev. Cancer 2023, 1878, 188993. [Google Scholar] [CrossRef]
- Kar, A.; Agarwal, S.; Singh, A.; Bajaj, A.; Dasgupta, U. Insights into Molecular Mechanisms of Chemotherapy Resistance in Cancer. Transl. Oncol. 2024, 42, 101901. [Google Scholar] [CrossRef]
- Godel, M.; Ortone, G.; Anobile, D.P.; Pasino, M.; Randazzo, G.; Riganti, C.; Kopecka, J. Targeting Mitochondrial Oncometabolites: A New Approach to Overcome Drug Resistance in Cancer. Pharmaceutics 2021, 13, 762. [Google Scholar] [CrossRef]
- Liu, T.; Song, S.; Wang, X.; Hao, J. Small-Molecule Inhibitors of Breast Cancer-Related Targets: Potential Therapeutic Agents for Breast Cancer. Eur. J. Med. Chem. 2021, 210, 112954. [Google Scholar] [CrossRef]
- Chhipa, A.S.; Patel, S. Targeting Pyruvate Kinase Muscle Isoform 2 (PKM2) in Cancer: What Do We Know so Far? Life Sci. 2021, 280, 119694. [Google Scholar] [CrossRef]
- Zhang, L.; Yao, Y.; Liu, S. Targeting Fatty Acid Metabolism for Cancer Therapy. Fundam. Res. 2024, in press. [CrossRef]
- Samaan, T.M.A.; Samec, M.; Liskova, A.; Kubatka, P.; Büsselberg, D. Paclitaxel’s Mechanistic and Clinical Effects on Breast Cancer. Biomolecules 2019, 9, 789. [Google Scholar] [CrossRef] [PubMed]
- Shrestha, R.; Johnson, E.; Byrne, F.L. Exploring the Therapeutic Potential of Mitochondrial Uncouplers in Cancer. Mol. Metab. 2021, 51, 101222. [Google Scholar] [CrossRef] [PubMed]
- Zhi, S.; Chen, C.; Huang, H.; Zhang, Z.; Zeng, F.; Zhang, S. Hypoxia-Inducible Factor in Breast Cancer: Role and Target for Breast Cancer Treatment. Front. Immunol. 2024, 15, 1370800. [Google Scholar] [CrossRef]
- Mirzaei, S.; Ranjbar, B.; Tackallou, S.H.; Aref, A.R. Hypoxia Inducible Factor-1α (HIF-1α) in Breast Cancer: The Crosstalk with Oncogenic and Onco-Suppressor Factors in Regulation of Cancer Hallmarks. Pathol. Res. Pract. 2023, 248, 154676. [Google Scholar] [CrossRef] [PubMed]
- Navarro, C.; Ortega, Á.; Santeliz, R.; Garrido, B.; Chacín, M.; Galban, N.; Vera, I.; De Sanctis, J.B.; Bermúdez, V. Metabolic Reprogramming in Cancer Cells: Emerging Molecular Mechanisms and Novel Therapeutic Approaches. Pharmaceutics 2022, 14, 1303. [Google Scholar] [CrossRef]
- Tufail, M.; Jiang, C.-H.; Li, N. Altered Metabolism in Cancer: Insights into Energy Pathways and Therapeutic Targets. Mol. Cancer 2024, 23, 203. [Google Scholar] [CrossRef]
- Wang, Z.; Liu, F.; Fan, N.; Zhou, C.; Li, D.; Macvicar, T.; Dong, Q.; Bruns, C.J.; Zhao, Y. Targeting Glutaminolysis: New Perspectives to Understand Cancer Development and Novel Strategies for Potential Target Therapies. Front. Oncol. 2020, 10, 589508. [Google Scholar] [CrossRef]
- Luo, S.; Jiang, Y.; Zheng, A.; Zhao, Y.; Wu, X.; Li, M.; Du, F.; Chen, Y.; Deng, S.; Chen, M.; et al. Targeting Hypoxia-Inducible Factors for Breast Cancer Therapy: A Narrative Review. Front. Pharmacol. 2022, 13, 1064661. [Google Scholar] [CrossRef]
- Stipp, M.C.; Acco, A. C-Myc-Targeted Therapy in Breast Cancer: A Review of Fundamentals and Pharmacological Insights. Gene 2025, 941, 149209. [Google Scholar] [CrossRef]
- Cui, J.; Jiang, H. Prediction of Postoperative Survival of Triple-Negative Breast Cancer Based on Nomogram Model Combined with Expression of HIF-1α and c-Myc. Medicine 2019, 98, e17370. [Google Scholar] [CrossRef]
- Wang, P.; Fu, Y.; Chen, Y.; Li, Q.; Hong, Y.; Liu, T.; Ding, Z. Nomogram Personalizes and Visualizes the Overall Survival of Patients with Triple-Negative Breast Cancer Based on the Immune Genome. Biomed. Res. Int. 2020, 2020, 4029062. [Google Scholar] [CrossRef] [PubMed]
- Matés, J.M.; Di Paola, F.J.; Campos-Sandoval, J.A.; Mazurek, S.; Márquez, J. Therapeutic Targeting of Glutaminolysis as an Essential Strategy to Combat Cancer. Semin. Cell Dev. Biol. 2020, 98, 34–43. [Google Scholar] [CrossRef]
- Gross, M.I.; Demo, S.D.; Dennison, J.B.; Chen, L.; Chernov-Rogan, T.; Goyal, B.; Janes, J.R.; Laidig, G.J.; Lewis, E.R.; Li, J.; et al. Antitumor Activity of the Glutaminase Inhibitor CB-839 in Triple-Negative Breast Cancer. Mol. Cancer Ther. 2014, 13, 890–901. [Google Scholar] [CrossRef]
- Birnboim-Perach, R.; Benhar, I. Using Combination Therapy to Overcome Diverse Challenges of Immune Checkpoint Inhibitors Treatment. Int. J. Biol. Sci. 2024, 20, 3911–3922. [Google Scholar] [CrossRef]
- Yu, W.; Yang, X.; Zhang, Q.; Sun, L.; Yuan, S.; Xin, Y. Targeting GLS1 to Cancer Therapy through Glutamine Metabolism. Clin. Transl. Oncol. 2021, 23, 2253–2268. [Google Scholar] [CrossRef] [PubMed]
- Zipinotti dos Santos, D.; de Souza, J.C.; Pimenta, T.M.; da Silva Martins, B.; Junior, R.S.R.; Butzene, S.M.S.; Tessarolo, N.G.; Cilas, P.M.L.; Silva, I.V.; Rangel, L.B.A. The Impact of Lipid Metabolism on Breast Cancer: A Review about Its Role in Tumorigenesis and Immune Escape. Cell Commun. Signal. 2023, 21, 161. [Google Scholar] [CrossRef]
- Huang, X.; Liu, B.; Shen, S. Lipid Metabolism in Breast Cancer: From Basic Research to Clinical Application. Cancers 2025, 17, 650. [Google Scholar] [CrossRef] [PubMed]
- Li, D.; Jin, P.; Cai, Y.; Wu, S.; Guo, X.; Zhang, Z.; Liu, K.; Li, P.; Hu, Y.; Zhou, Y. Clinical Significance of Lipid Pathway-Targeted Therapy in Breast Cancer. Front. Pharmacol. 2025, 15, 1514811. [Google Scholar] [CrossRef]
- Mukha, D.; Dessain, J.; O’Connor, S.; Pniewski, K.; Bertolazzi, F.; Patel, J.; Mullins, M.; Schug, Z.T. Identification of Fasnall as a Therapeutically Effective Complex I Inhibitor. bioRxiv 2024. [Google Scholar] [CrossRef]
- Serhan, H.A.; Bao, L.; Cheng, X.; Qin, Z.; Liu, C.-J.; Heth, J.A.; Udager, A.M.; Soellner, M.B.; Merajver, S.D.; Morikawa, A.; et al. Targeting Fatty Acid Synthase in Preclinical Models of TNBC Brain Metastases Synergizes with SN-38 and Impairs Invasion. NPJ Breast Cancer 2024, 10, 43. [Google Scholar] [CrossRef]
- Klement, R.J. The Influence of Ketogenic Therapy on the 5 R’s of Radiobiology. Int. J. Radiat. Biol. 2019, 95, 394–407. [Google Scholar] [CrossRef] [PubMed]
- Weber, D.D.; Aminzadeh-Gohari, S.; Tulipan, J.; Catalano, L.; Feichtinger, R.G.; Kofler, B. Ketogenic Diet in the Treatment of Cancer–Where Do We Stand? Mol. Metab. 2020, 33, 102–121. [Google Scholar] [CrossRef] [PubMed]
- Marchio, V.; Augimeri, G.; Morelli, C.; Vivacqua, A.; Giordano, C.; Catalano, S.; Sisci, D.; Barone, I.; Bonofiglio, D. Omega-3 Fatty Acids: Molecular Weapons against Chemoresistance in Breast Cancer. Cell Mol. Biol. Lett. 2025, 30, 11. [Google Scholar] [CrossRef]
- Osouli-Tabrizi, S.; Mehdizadeh, A.; Naghdi, M.; Sanaat, Z.; Vahed, N.; Farshbaf-Khalili, A. The Effectiveness of Omega-3 Fatty Acids on Health Outcomes in Women with Breast Cancer: A Systematic Review. Food Sci. Nutr. 2023, 11, 4355–4371. [Google Scholar] [CrossRef]
- Morshed, A.K.M.H.; Al Azad, S.; Mia, M.d.A.R.; Uddin, M.F.; Ema, T.I.; Yeasin, R.B.; Srishti, S.A.; Sarker, P.; Aurthi, R.Y.; Jamil, F.; et al. Oncoinformatic Screening of the Gene Clusters Involved in the HER2-Positive Breast Cancer Formation along with the in Silico Pharmacodynamic Profiling of Selective Long-Chain Omega-3 Fatty Acids as the Metastatic Antagonists. Mol. Divers. 2023, 27, 2651–2672. [Google Scholar] [CrossRef]
- Anemoulis, M.; Vlastos, A.; Kachtsidis, V.; Karras, S.N. Intermittent Fasting in Breast Cancer: A Systematic Review and Critical Update of Available Studies. Nutrients 2023, 15, 532. [Google Scholar] [CrossRef]
- Omar, E.M.; Omran, G.A.; Mustafa, M.F.; El-Khodary, N.M. Intermittent Fasting during Adjuvant Chemotherapy May Promote Differential Stress Resistance in Breast Cancer Patients. J. Egypt. Natl. Canc Inst. 2022, 34, 38. [Google Scholar] [CrossRef] [PubMed]
- Carmona, A.; Mitri, S.; James, T.A.; Ubellacker, J.M. Lipidomics and Metabolomics as Potential Biomarkers for Breast Cancer Progression. npj Metab. Health Dis. 2024, 2, 24. [Google Scholar] [CrossRef]
- Cappelletti, V.; Iorio, E.; Miodini, P.; Silvestri, M.; Dugo, M.; Daidone, M.G. Metabolic Footprints and Molecular Subtypes in Breast Cancer. Dis. Markers 2017, 2017, 7687851. [Google Scholar] [CrossRef]
- Pang, H.; Hu, Z. Metabolomics in Drug Research and Development: The Recent Advances in Technologies and Applications. Acta Pharm. Sin. B 2023, 13, 3238–3251. [Google Scholar] [CrossRef] [PubMed]
- Seydel, C. Single-Cell Metabolomics Hits Its Stride. Nat. Methods 2021, 18, 1452–1456. [Google Scholar] [CrossRef] [PubMed]
- Castelli, F.A.; Rosati, G.; Moguet, C.; Fuentes, C.; Marrugo-Ramírez, J.; Lefebvre, T.; Volland, H.; Merkoçi, A.; Simon, S.; Fenaille, F.; et al. Metabolomics for Personalized Medicine: The Input of Analytical Chemistry from Biomarker Discovery to Point-of-Care Tests. Anal. Bioanal. Chem. 2022, 414, 759–789. [Google Scholar] [CrossRef] [PubMed]
- Sharaf, B.M.; Giddey, A.D.; Al-Hroub, H.M.; Menon, V.; Okendo, J.; El-Awady, R.; Mousa, M.; Almehdi, A.; Semreen, M.H.; Soares, N.C. Mass Spectroscopy-Based Proteomics and Metabolomics Analysis of Triple-Positive Breast Cancer Cells Treated with Tamoxifen and/or Trastuzumab. Cancer Chemother. Pharmacol. 2022, 90, 467–488. [Google Scholar] [CrossRef]
- Díaz-Beltrán, L.; González-Olmedo, C.; Luque-Caro, N.; Díaz, C.; Martín-Blázquez, A.; Fernández-Navarro, M.; Ortega-Granados, A.L.; Gálvez-Montosa, F.; Vicente, F.; Pérez del Palacio, J.; et al. Human Plasma Metabolomics for Biomarker Discovery: Targeting the Molecular Subtypes in Breast Cancer. Cancers 2021, 13, 147. [Google Scholar] [CrossRef]
- Joshi, S.; Garlapati, C.; Bhattarai, S.; Su, Y.; Rios-Colon, L.; Deep, G.; Torres, M.A.; Aneja, R. Exosomal Metabolic Signatures Are Associated with Differential Response to Neoadjuvant Chemotherapy in Patients with Breast Cancer. Int. J. Mol. Sci. 2022, 23, 5324. [Google Scholar] [CrossRef]
- Díaz, C.; González-Olmedo, C.; Díaz-Beltrán, L.; Camacho, J.; Mena García, P.; Martín-Blázquez, A.; Fernández-Navarro, M.; Ortega-Granados, A.L.; Gálvez-Montosa, F.; Marchal, J.A.; et al. Predicting Dynamic Response to Neoadjuvant Chemotherapy in Breast Cancer: A Novel Metabolomics Approach. Mol. Oncol. 2022, 16, 2658–2671. [Google Scholar] [CrossRef] [PubMed]
- Zhou, J.; Wang, Y.; Zhang, X.; Zhou, J.; Wang, Y.; Zhang, X. Metabonomics Studies on Serum and Urine of Patients with Breast Cancer Using 1 H-NMR Spectroscopy. Oncotarget 2017, 5. [Google Scholar] [CrossRef][Green Version]
- He, X.; Gu, J.; Zou, D.; Yang, H.; Zhang, Y.; Ding, Y.; Teng, L. NMR-Based Metabolomics Analysis Predicts Response to Neoadjuvant Chemotherapy for Triple-Negative Breast Cancer. Front. Mol. Biosci. 2021, 8, 708052. [Google Scholar] [CrossRef]
- Lin, X.; Xu, R.; Mao, S.; Zhang, Y.; Dai, Y.; Guo, Q.; Song, X.; Zhang, Q.; Li, L.; Chen, Q. Metabolic Biomarker Signature for Predicting the Effect of Neoadjuvant Chemotherapy of Breast Cancer. Ann. Transl. Med. 2019, 7, 670. [Google Scholar] [CrossRef]
- Fang, Z.; Ren, G.; Ke, S.; Xu, Q.; Chen, Y.; Shi, X.; Guo, C.; Huang, J. Serum Metabolomic Profiling for Predicting Therapeutic Response and Toxicity in Breast Cancer Neoadjuvant Chemotherapy: A Retrospective Longitudinal Study. Breast Cancer Res. 2025, 27, 2. [Google Scholar] [CrossRef]
- Eniu, D.T.; Chiorean, A.R.; Socaciu, A.I.; Staicu, A.; Rachieriu, C.; Goidescu, I.; Buiga, R.; Eniu, D.; Socaciu, C.; Chira, R. Blood and Urine Biomarkers in Invasive Ductal Breast Cancer: Mass Spectrometry Applied to Identify Metabolic Alterations. J. Mol. Struct. 2022, 1247, 131369. [Google Scholar] [CrossRef]
- Zheng, Y.; Xu, R.; Chen, X.; Lu, Y.; Zheng, J.; Lin, Y.; Lin, P.; Zhao, X.; Cui, L. Metabolic Gatekeepers: Harnessing Tumor-Derived Metabolites to Optimize T Cell-Based Immunotherapy Efficacy in the Tumor Microenvironment. Cell Death Dis. 2024, 15, 775. [Google Scholar] [CrossRef]
- Santiappillai, N.T.; Abuhammad, S.; Slater, A.; Kirby, L.; McArthur, G.A.; Sheppard, K.E.; Smith, L.K. CDK4/6 Inhibition Reprograms Mitochondrial Metabolism in BRAFV600 Melanoma via a P53 Dependent Pathway. Cancers 2021, 13, 524. [Google Scholar] [CrossRef] [PubMed]
- Irajizad, E.; Wu, R.; Vykoukal, J.; Murage, E.; Spencer, R.; Dennison, J.B.; Moulder, S.; Ravenberg, E.; Lim, B.; Litton, J.; et al. Application of Artificial Intelligence to Plasma Metabolomics Profiles to Predict Response to Neoadjuvant Chemotherapy in Triple-Negative Breast Cancer. Front. Artif. Intell. 2022, 5, 876100. [Google Scholar] [CrossRef]
- Neagu, A.-N.; Whitham, D.; Buonanno, E.; Jenkins, A.; Alexa-Stratulat, T.; Tamba, B.I.; Darie, C.C. Proteomics and Its Applications in Breast Cancer. Am. J. Cancer Res. 2021, 11, 4006–4049. [Google Scholar] [PubMed]
- Mehmood, S.; Faheem, M.; Ismail, H.; Farhat, S.M.; Ali, M.; Younis, S.; Asghar, M.N. ‘Breast Cancer Resistance Likelihood and Personalized Treatment Through Integrated Multiomics’. Front. Mol. Biosci. 2022, 9, 783494. [Google Scholar] [CrossRef]
- Gómez-Cebrián, N.; Domingo-Ortí, I.; Poveda, J.L.; Vicent, M.J.; Puchades-Carrasco, L.; Pineda-Lucena, A. Multi-Omic Approaches to Breast Cancer Metabolic Phenotyping: Applications in Diagnosis, Prognosis, and the Development of Novel Treatments. Cancers 2021, 13, 4544. [Google Scholar] [CrossRef]
- Rossi, C.; Cicalini, I.; Cufaro, M.C.; Consalvo, A.; Upadhyaya, P.; Sala, G.; Antonucci, I.; Del Boccio, P.; Stuppia, L.; De Laurenzi, V. Breast Cancer in the Era of Integrating “Omics” Approaches. Oncogenesis 2022, 11, 17. [Google Scholar] [CrossRef]
- Auslander, N.; Yizhak, K.; Weinstock, A.; Budhu, A.; Tang, W.; Wang, X.W.; Ambs, S.; Ruppin, E. A Joint Analysis of Transcriptomic and Metabolomic Data Uncovers Enhanced Enzyme-Metabolite Coupling in Breast Cancer. Sci. Rep. 2016, 6, 29662. [Google Scholar] [CrossRef]
- Bonanomi, M.; Salmistraro, N.; Fiscon, G.; Conte, F.; Paci, P.; Bravatà, V.; Forte, G.I.; Volpari, T.; Scorza, M.; Mastroianni, F.; et al. Transcriptomics and Metabolomics Integration Reveals Redox-Dependent Metabolic Rewiring in Breast Cancer Cells. Cancers 2021, 13, 5058. [Google Scholar] [CrossRef]
- Xiao, Y.; Ma, D.; Yang, Y.-S.; Yang, F.; Ding, J.-H.; Gong, Y.; Jiang, L.; Ge, L.-P.; Wu, S.-Y.; Yu, Q.; et al. Comprehensive Metabolomics Expands Precision Medicine for Triple-Negative Breast Cancer. Cell Res. 2022, 32, 477–490. [Google Scholar] [CrossRef] [PubMed]
- González-Domínguez, R.; González-Domínguez, Á.; Sayago, A.; Fernández-Recamales, Á. Recommendations and Best Practices for Standardizing the Pre-Analytical Processing of Blood and Urine Samples in Metabolomics. Metabolites 2020, 10, 229. [Google Scholar] [CrossRef]
- Ahn, J.S.; Shin, S.; Yang, S.-A.; Park, E.K.; Kim, K.H.; Cho, S.I.; Ock, C.-Y.; Kim, S. Artificial Intelligence in Breast Cancer Diagnosis and Personalized Medicine. J. Breast Cancer 2023, 26, 405. [Google Scholar] [CrossRef] [PubMed]
- Polónia, A.; Campelos, S.; Ribeiro, A.; Aymore, I.; Pinto, D.; Biskup-Fruzynska, M.; Veiga, R.S.; Canas-Marques, R.; Aresta, G.; Araújo, T.; et al. Artificial Intelligence Improves the Accuracy in Histologic Classification of Breast Lesions. Am. J. Clin. Pathol. 2021, 155, 527–536. [Google Scholar] [CrossRef] [PubMed]
- Uzun Ozsahin, D.; Ikechukwu Emegano, D.; Uzun, B.; Ozsahin, I. The Systematic Review of Artificial Intelligence Applications in Breast Cancer Diagnosis. Diagnostics 2022, 13, 45. [Google Scholar] [CrossRef]
- Eisemann, N.; Bunk, S.; Mukama, T.; Baltus, H.; Elsner, S.A.; Gomille, T.; Hecht, G.; Heywang-Köbrunner, S.; Rathmann, R.; Siegmann-Luz, K.; et al. Nationwide Real-World Implementation of AI for Cancer Detection in Population-Based Mammography Screening. Nat. Med. 2025, 31, 917–924. [Google Scholar] [CrossRef]
- Letertre, M.P.M.; Giraudeau, P.; de Tullio, P. Nuclear Magnetic Resonance Spectroscopy in Clinical Metabolomics and Personalized Medicine: Current Challenges and Perspectives. Front. Mol. Biosci. 2021, 8, 698337. [Google Scholar] [CrossRef]
- Borges, R.M.; Teixeira, A.M. On the Part That NMR Should Play in Mass Spectrometry Metabolomics in Natural Products Studies. Front. Nat. Prod. 2024, 3, 1359151. [Google Scholar] [CrossRef]
- Shah, T.; Wildes, F.; Penet, M.F.; Winnard, P.T.; Glunde, K.; Artemov, D.; Ackerstaff, E.; Gimi, B.; Kakkad, S.; Raman, V.; et al. Choline Kinase Overexpression Increases Invasiveness and Drug Resistance of Human Breast Cancer Cells. NMR Biomed. 2010, 23, 633. [Google Scholar] [CrossRef]
- Carosi, F.; Broseghini, E.; Fabbri, L.; Corradi, G.; Gili, R.; Forte, V.; Roncarati, R.; Filippini, D.M.; Ferracin, M. Targeting Isocitrate Dehydrogenase (IDH) in Solid Tumors: Current Evidence and Future Perspectives. Cancers 2024, 16, 2752. [Google Scholar] [CrossRef]
- Wang, Y.; An, R.; Yu, H.; Dai, Y.; Lou, L.; Quan, S.; Chen, R.; Ding, Y.; Zhao, H.; Wu, X.; et al. Largescale Multicenter Study of a Serum Metabolite Biomarker Panel for the Diagnosis of Breast Cancer. iScience 2024, 27, 110345. [Google Scholar] [CrossRef] [PubMed]
- Bai, M.; Sun, C. Determination of Breast Metabolic Phenotypes and Their Associations with Immunotherapy and Drug-Targeted Therapy: Analysis of Single-Cell and Bulk Sequences. Front. Cell Dev. Biol. 2022, 10, 829029. [Google Scholar] [CrossRef] [PubMed]
- Yoon, H.; Yoon, D.; Yun, M.; Choi, J.S.; Park, V.Y.; Kim, E.-K.; Jeong, J.; Koo, J.S.; Yoon, J.H.; Moon, H.J.; et al. Metabolomics of Breast Cancer Using High-Resolution Magic Angle Spinning Magnetic Resonance Spectroscopy: Correlations with 18F-FDG Positron Emission Tomography-Computed Tomography, Dynamic Contrast-Enhanced and Diffusion-Weighted Imaging MRI. PLoS ONE 2016, 11, e0159949. [Google Scholar] [CrossRef] [PubMed]
- Ahmad Qureshi, M.D.; Ramzan, M.F.; Amjad, F.; Haider, N. Artificial Intelligence in Metabolomics for Disease Profiling: A Machine Learning Approach to Biomarker Discovery. Indus J. Biosci. Res. 2024, 2, 87–96. [Google Scholar] [CrossRef]
- Buentzel, J.; Klemp, H.G.; Kraetzner, R.; Schulz, M.; Dihazi, G.H.; Streit, F.; Bleckmann, A.; Menck, K.; Wlochowitz, D.; Binder, C. Metabolomic Profiling of Blood-Derived Microvesicles in Breast Cancer Patients. Int. J. Mol. Sci. 2021, 22, 13540. [Google Scholar] [CrossRef]
- D’Mello, R.; Hüttmann, N.; Minic, Z.; V Berezovski, M. Untargeted Metabolomic Profiling of Small Extracellular Vesicles Reveals Potential New Biomarkers for Triple Negative Breast Cancer. Metabolomics 2024, 20, 123. [Google Scholar] [CrossRef]
| Biological Fluids | Stage/Subtype | Analytical Tools | Main Conclusions | Ref. |
|---|---|---|---|---|
| Alveolar breath (n = 149) | 13 Ductal carcinoma in situ (DCIS) 31 lymph node metastasis-negative 27 lymph node metastasis-positive 78 controls | GC-MS | (S)-1,2-propanediol, cyclopentanone, ethylene carbonate, 3-methoxy-1,2-propanediol, 3-methylpyridine, phenol, and tetramethylsilane can be used for early BC diagnosis VOC set showed 80.8% sensitivity and 100% specificity in identifying BC | [10] |
| Plasma (n = 270) | 2 IA 54 IIA 48 IIB 15 IIIA 6 IIIB 4 IV 5 n.d. 136 controls | LC−HRMS | Two candidate biomarkers were identified with strong discriminatory power (VIP > 1 and AUC = 0.958), suggesting their potential for early diagnosis and molecular stratification of BC in future studies. | [11] |
| Plasma (n = 125) | 31 I 33 II 11 III 20 controls 30 benign patients | UHPLC-MS/MS | Identified 47 plasma metabolites, including sphingomyelins, glutamate, and cysteine, as potential diagnostic biomarkers for BC. These metabolites likewise demonstrated a reasonably high predictive power in the testing cohort between benign vs. control (AUC = 0.879) and BC vs. control (AUC = 0.794). | [12] |
| Plasma (n = 44) | 1 T0 1 T1a 1 T1b 5 T1c 4 T2 1 Tis 7N0 5 N1a 1 Nx 18 benign patients | LC-MS/MS | Ether-linked phosphatidylcholine showed a significant difference between invasive ductal carcinoma and benign tumors. Dysregulated hydrophilic metabolites included glutamate, glycochenodeoxycholate, and dimethyluric acid Machine learning models accurately distinguished between cancerous and benign cases using these metabolic markers. | [13] |
| Urine (n= 168) | 80 biopsy-confirmed BC patients 88 controls | GC-HRMS | Variable selection (VIP > 1.5, p < 0.05 and FDR < 0.05) identified eight potential VOC biomarkers. Of these, three VOCs showed upregulation, and the remaining five VOCs showed downregulation in BC patients. VOC set showed 76.3% sensitivity and 85.4% specificity in identifying BC. | [14] |
| Urine (n = 60) Tissue (n= 60) | 5 IA 10 IIA 1 IIIA 7 IIB 5 IIIB 2 IIIC 30 controls | GC-MS NMR | Acetone, 3-hexanone, 4-heptanone, 2-methyl-5-(methylthio)-furan and acetate can be potential BC biomarkers using this dual-platform approach. | [15] |
| Tissue (n = 30) | 5 IA 10IIA 1 IIIA 7 IIB 5 IIIB 2 IIIC 30 controls | GC-MS | Limonene, decanoic acid, acetic acid, and furfural were identified as potential BC biomarkers with strong discriminatory power (VIP > 1 and AUC = 0.966). | [16] |
| Saliva (n = 162) | 23 Tis 44 I 46 II 5 III 2 IV 42 Controls | CE LC- MS | Of the 260 quantified metabolites, polyamines were significantly elevated in the saliva of patients with breast cancer. Spermine showed the highest area under the receiver operating characteristic curves. In addition to spermine, polyamines and their acetylated forms were elevated in IC only. | [17] |
| Saliva (n = 106) | 66 confirmed BC patients 40 controls | GC-MS | 3-methyl-pentanoic acid, 4-methyl-pentanoic acid, phenol and p-tert-butyl-phenol (Portuguese samples) and acetic, propanoic, benzoic acids, 1,2-decanediol, 2-decanone, and decanal (Indian samples), statistically relevant for the discrimination of BC patients in the populations analyzed. | [18] |
| Subjects | Main Conclusions | Ref. |
|---|---|---|
| Cell lines (MDA-MB-231, SKBR3, MDA-MB-468) | Identified B7-H3 as a key promoter of metabolic reprogramming in cancer cells, suggesting potential for targeting B7-H3 in cancer therapy beyond immune modulation. | [46] |
| Cell lines (MCF-7-CSC) Mice (n = 7) | Targeting aberrant lipid metabolism, especially SCD1 activity, is a viable strategy to impair BC stem cell function, and omega-3 fatty acids offer a potent, non-toxic approach for this purpose. | [47] |
| Cell line (MET-1 cells) Mice (n = 60) | The study demonstrates that jointly reducing systemic glucose through diet and pharmacology can effectively inhibit tumor progression and enhance survival. | [48] |
| Cell lines (MDA-MB-231, MDA-MB-468) Mice (n = -) | Mimicking fasting conditions reduced cell proliferation, disrupted cell cycle progression, and decreased migration and invasion of TNBC cells. Intermittent fasting significantly reduced macrophage accumulation, pro-inflammatory signaling, and expression of key markers (cyclin B1, vimentin), reflecting a less aggressive tumor environment. | [49] |
| Tissue (n = -) | Metabolic differences between normal and tumor tissues were not primarily driven by tissue heterogeneity, suggesting intrinsic tumor-specific metabolic reprogramming. C3-TAg tumors exhibited a unique 10-metabolite signature with prognostic value in human BC. Gene expression analysis identified candidate genes potentially driving metabolic reprogramming in tumors. | [50] |
| Persons (n = 20) | Significant improvements were observed in fasting plasma glucose, insulin levels, and insulin resistance after three months, with these effects persisting at six months. The well-formulated ketogenic diet was successfully transitioned from a supervised to a self-administered model in Phase II, indicating potential for long-term adherence with appropriate support. | [51] |
| Persons (n = 45) | Short-term (30-day) eicosapentaenoic acid and docosahexaenoic acid supplementation led to beneficial changes in plasma fatty acid composition, immune preservation, and reduced inflammatory progression, supporting its role as a nutritional and immunological support in early-stage BC patients. | [52] |
| Persons (n = 625) | Meta-analysis revealed that intermittent fasting significantly reduced body weight, blood glucose levels, and insulin concentrations. No significant increase in chemotherapy-related adverse effects, indicating that intermittent fasting may be safe during cancer treatment, though evidence is inconclusive. | [53] |
| Persons (n = 32) | A whole-food, plant-based diet specifically impacts isoflavone and polyunsaturated fatty acid (omega-3 and 6) intake in women with advanced BC, which are associated with potential BC benefits. | [54] |
| Biological Fluids | Analytical Tools | Main Conclusions | Ref. |
|---|---|---|---|
| Cell lines (MCF-7) | NMR | Metabolic and genetic markers may serve as potential targets or predictors for overcoming tamoxifen resistance in BC therapy. | [73] |
| Serum (n = 120) | GC-MS LC-MS | Thirty-nine dysregulated pathways were uncovered in 9 patients, providing deep insights into HER2+ BrCa biology and treatment resistance mechanisms. Paves the way for developing novel treatment targets for patients resistant to the TCbHP (taxane, carboplatin, trastuzumab, and pertuzumab) regimen. | [74] |
| Tissue (n = 76) | qRT-PCR | Silencing circHIPK3 can overcome paclitaxel resistance in BC by regulating the miR-1286/HK2 pathway, suggesting a potential therapeutic target. | [75] |
| Biological Samples | Molecular Subtype | Analytical Tools | Main Conclusions | Ref. |
|---|---|---|---|---|
| Cell lines (BT-474) | Triple-positive BC cell model | LC-MS/MS | Tamoxifen and trastuzumab (separately or in combination) exert potent anti-growth effects by modulating key pathways associated with cell proliferation, apoptosis, metabolism, and chemoresistance in triple-positive BC cells. These insights may guide the development of more personalized and less aggressive therapeutic strategies. | [124] |
| Cell lines (BT-20, BT-549, Hs578T, HCC38, HCC1806, HCC70, MDA-MB-231, MDA-MB-436, HMC-1–8, HCC1395, HCC1187, Hs739.T, MDA-MB-468, HCC1954, MCF-7, Hs343.T, HCC1428, DU4475, AU-565, T47D, Sk-Br-3, MDA-MB-175-VII) | Triple-negative BC cell model | LC-MS/MS | CB-839 exhibited significant antitumor activity in two xenograft models: a patient-derived TNBC model and a HER2(+) basal-like model (JIMT-1), both as a monotherapy and in combination with paclitaxel. Strong rationale for clinical development of CB-839 as a targeted therapy for TNBC and other glutamine-dependent cancers. | [104] |
| Plasma, tissue (n = 999) | Plasma: 200 BC 100 Controls Training cohort: 283 BC and 140 controls test cohort: 150 BC and 126 controls | scRNA-seq LC-MS/MS | Distinguished metabolic and immune features between TNBC and non-TNBC patients. Nucleotide metabolism correlated with regulatory T-cell activation in the tumor microenvironment via the A2AR-Treg pathway. Inosine and uridine predict response to neoadjuvant chemotherapy in TNBC patients. | [36] |
| Plasma (n = 165) | 2 IA 54 IIA 15 IIIA 50 IIB 6 IIIB 4 IC 34 controls | LC-HRMS | Identified specific metabolite panels for each BC subtype: 5 metabolites for LA, 7 for LB, 5 for HER2+ and 3 for TN. The data obtained showed the clinical utility of metabolomics for individualized diagnosis and therapy planning, contributing to personalized medicine in BC. | [125] |
| Plasma (n = 16) | 1 IA 3 IIA 2 IIIA 1 IB 4 IIB 3 IIIB 2 IIIC | LC-MS | Only 30% of patients achieved pathologic complete response (pCR); the rest had residual disease (RD). Plasma exosomal metabolomics could serve as a non-invasive biomarker to predict neoadjuvant chemotherapy response. | [126] |
| Plasma (n = 92) | 48 LB 23 HER2+ 21 TN | LC-HRMS | Metabolomics demonstrated potential for early detection of chemoresistance. Findings contribute to advancing personalized treatment and follow-up strategies in BC care. | [127] |
| Urine, serum (n = 22) | 11 BC 11 controls | NMR | Identified 9 significantly altered serum metabolites (e.g., choline, glucose, histidine) and 3 significantly altered urine metabolites (phenylacetylglycine, guanidoacetate, citrate) in BC patients. NMR-based metabolomics shows promise as a diagnostic or monitoring tool for BC. | [128] |
| Serum (n = 52) | 1 I 8 II 18 III 25 IV | NMR | Three significantly altered metabolic pathways were identified that are associated with chemotherapy response. Potential of metabolic phenotyping can be used as a tool to guide personalized treatment strategies for TNBC, especially in determining suitability for neoadjuvant chemotherapy. | [129] |
| Serum (n = 35) | 18 IIIA 1 IIIB 16 IIIC | LC-MS | 9 key metabolites associated with chemotherapy response were identified (e.g., oleic acid amide, ethyl docosahexaenoate). Serum metabolomics can be applied as a non-invasive tool to predict neoadjuvant chemotherapy outcomes in BC. | [130] |
| Serum (n = 322) | 161 BC 161 controls | NMR ICP-EOS | 24 metabolites and 4 metal ions significantly differentiated BC patients from controls. Four metabolites linked to BC progression. Significant differences across age/menopausal subgroups. | [26] |
| Serum (n = 50) | 22 IIB 13 IIIA 11 IIIB 4 IIIC | LC-MS/MS | Metabolic changes associated with response to neoadjuvant chemotherapy were identified, providing potential predictive biomarkers. | [131] |
| Serum (n = 50) | 7 IIA 9 IIB 10 IIIA 9 IIIB 15 controls | LC-MS/MS | Metabolites allowed the differentiation between invasive ductal carcinoma patients and healthy controls, which aids in diagnosis and potentially in assessing therapy response. | [132] |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Perestrelo, R.; Luís, C. Metabolomics in Breast Cancer: From Biomarker Discovery to Personalized Medicine. Metabolites 2025, 15, 428. https://doi.org/10.3390/metabo15070428
Perestrelo R, Luís C. Metabolomics in Breast Cancer: From Biomarker Discovery to Personalized Medicine. Metabolites. 2025; 15(7):428. https://doi.org/10.3390/metabo15070428
Chicago/Turabian StylePerestrelo, Rosa, and Catarina Luís. 2025. "Metabolomics in Breast Cancer: From Biomarker Discovery to Personalized Medicine" Metabolites 15, no. 7: 428. https://doi.org/10.3390/metabo15070428
APA StylePerestrelo, R., & Luís, C. (2025). Metabolomics in Breast Cancer: From Biomarker Discovery to Personalized Medicine. Metabolites, 15(7), 428. https://doi.org/10.3390/metabo15070428








