Vitamin D and Its Metabolites Status before and during Chemotherapy in Caucasian Breast Cancer Patients
Abstract
:1. Introduction
2. Materials and Methods
2.1. Subjects
2.2. Materials
2.3. Apparatus and Chromatographic Conditions
2.4. Serum Sample Preparation
2.5. Data Analysis
2.6. Statistical Analyses
3. Results
3.1. Vitamin D Status in BC Patients before and during Chemotherapy
3.2. Changes in 25(OH)D, 25(OH)D2, 25(OH)D3, 24,25(OH)2D3 and 3-epi-25(OH)D3 Levels during Chemotherapy
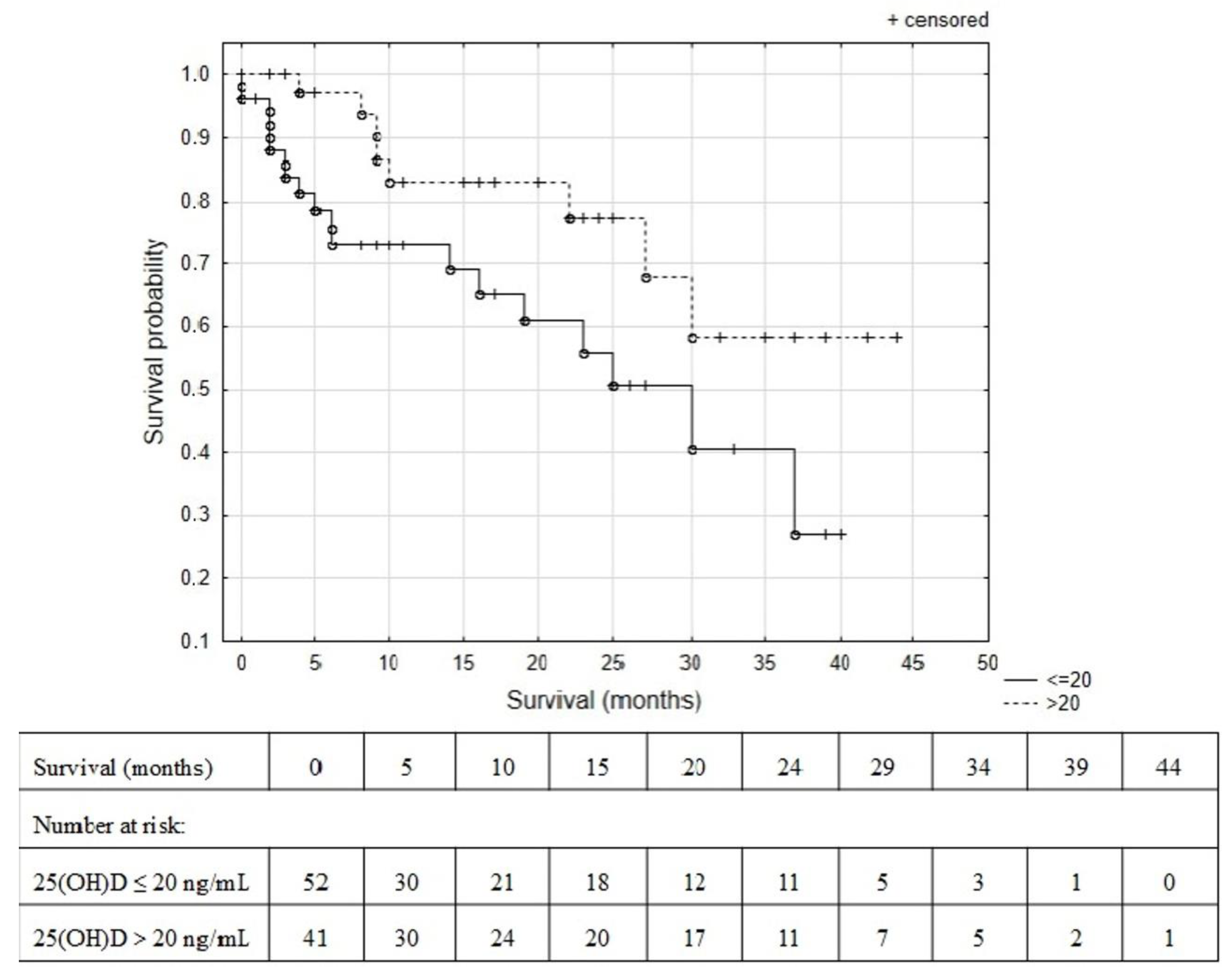
3.3. Predictive Role of Vitamin D Status
4. Discussion
4.1. Vitamin D Status in BC Patients at Baseline and during CTH
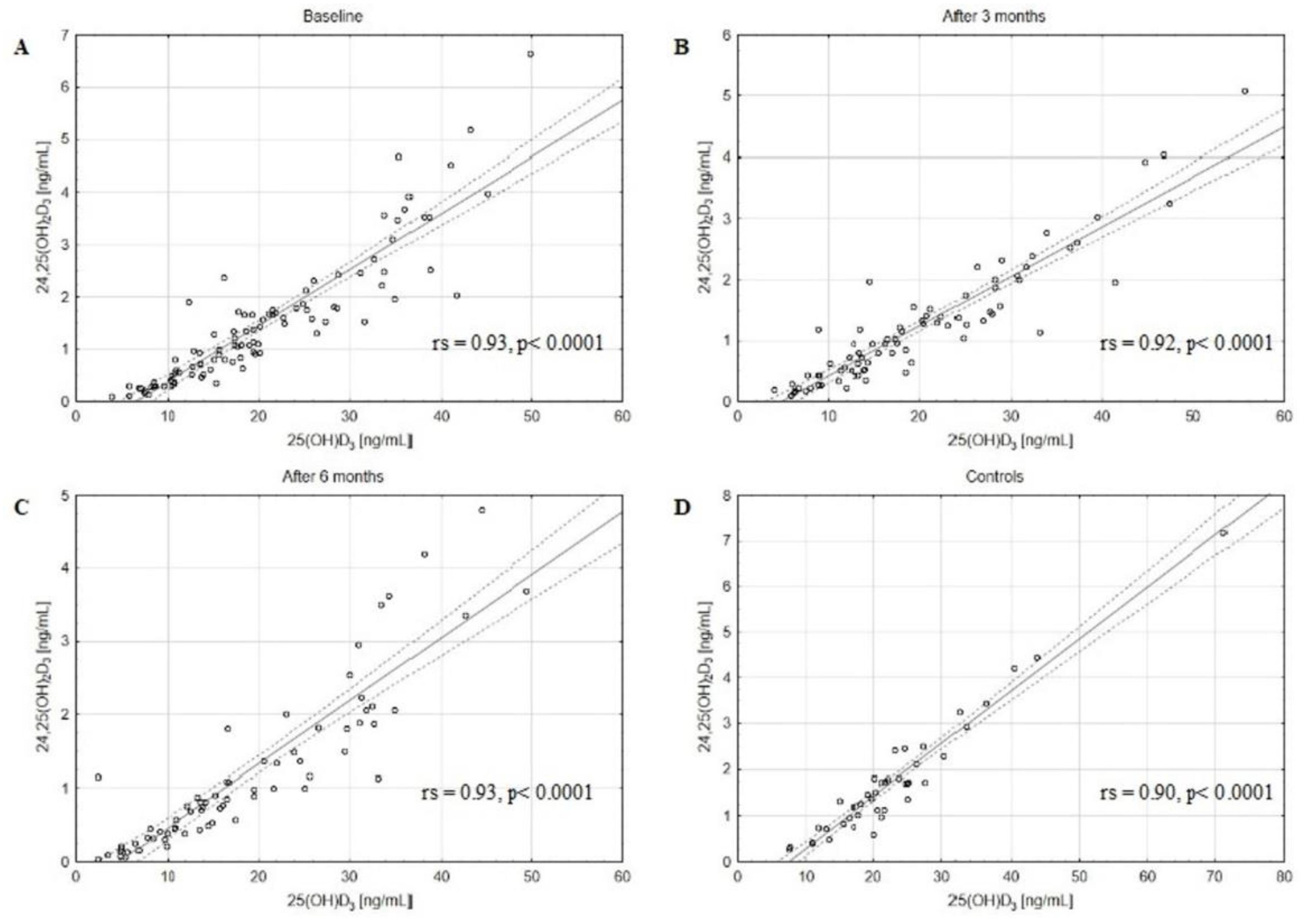
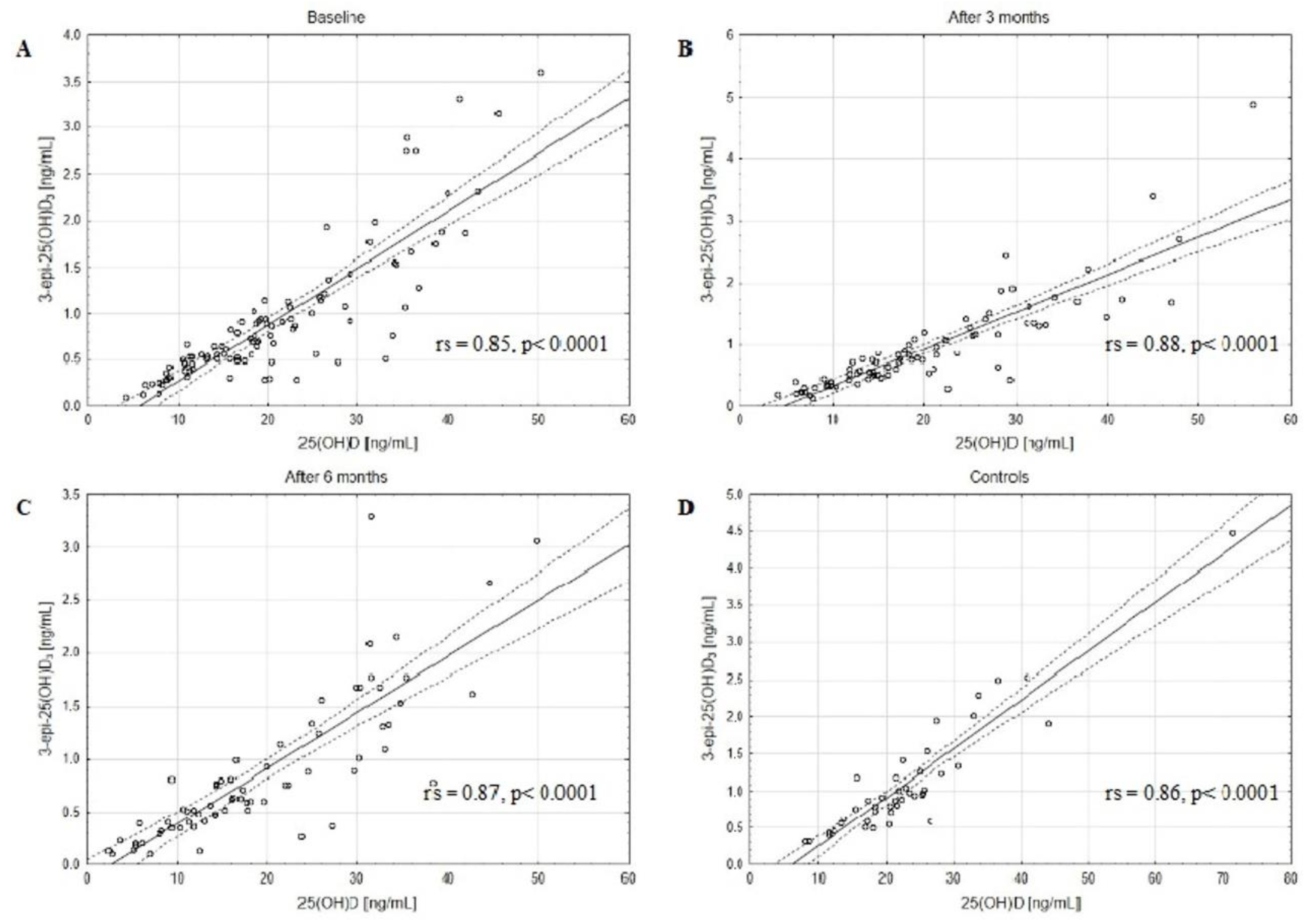
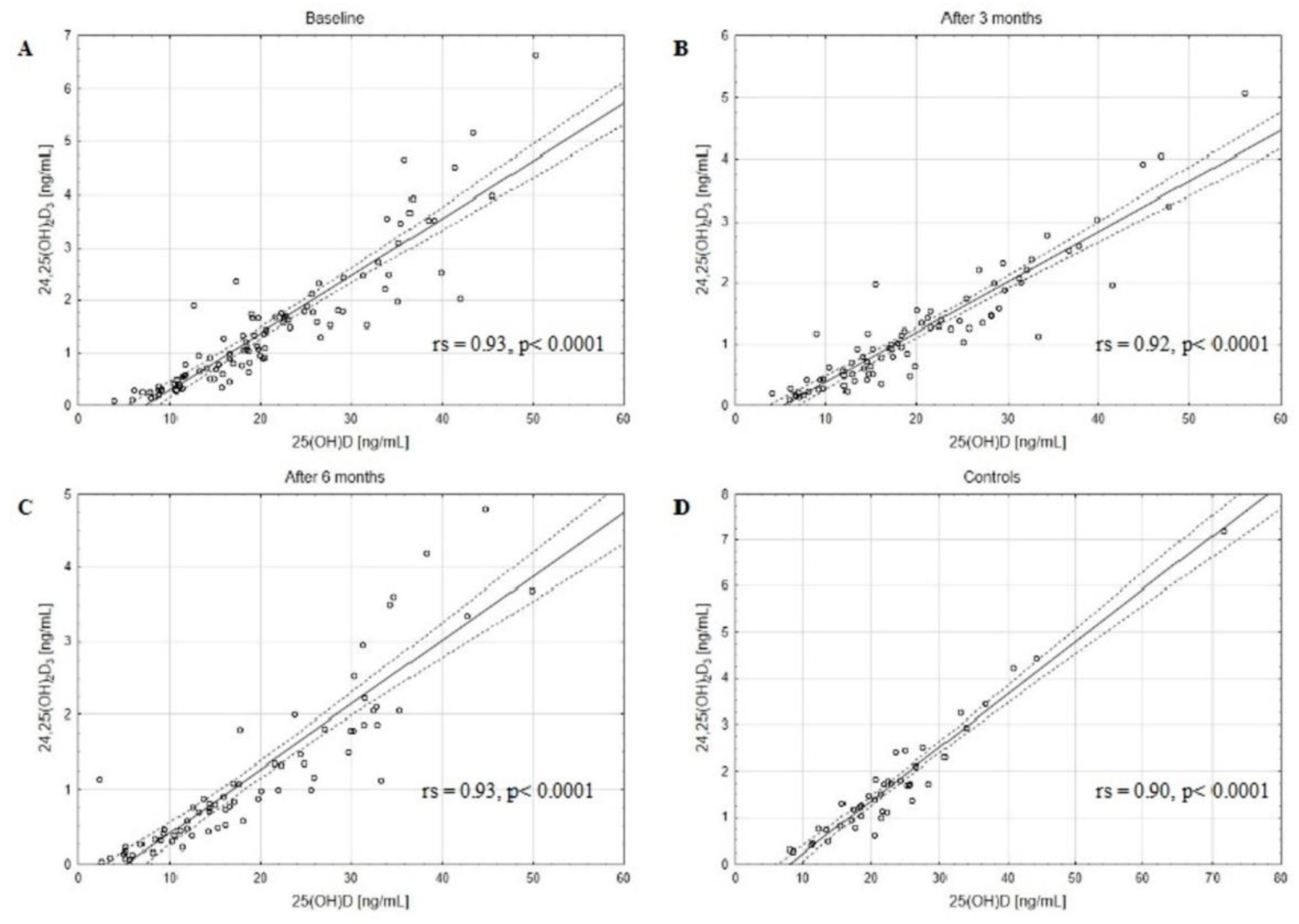
4.2. Catabolites Status of 24,25(OH)2D3 and 3-epi-25(OH)D3 at Baseline and during Chemotherapy
4.3. Predictive Role of Vitamin D Status
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Sung, H.; Ferlay, J.; Siegel, R.L.; Laversanne, M.; Soerjomataram, I.; Jemal, A.; Bray, F. Global Cancer Statistics 2020: GLOBOCAN Estimates of Incidence and Mortality Worldwide for 36 Cancers in 185 Countries. CA Cancer J. Clin. 2021, 71, 209–249. [Google Scholar] [CrossRef] [PubMed]
- Carlberg, C.; Velleuer, E. Vitamin D and the risk for cancer: A molecular analysis. Biochem. Pharmacol. 2022, 196, 114735. [Google Scholar] [CrossRef]
- Fleet, J.C.; Desmet, M.; Johnson, R.; Li, Y. Vitamin D and cancer: A review of molecular mechanisms. Biochem. J. 2012, 441, 61–76. [Google Scholar] [CrossRef]
- Vanhevel, J.; Verlinden, L.; Doms, S.; Wildiers, H.; Verstuyf, A. The role of vitamin D in breast cancer risk and progression. Endocr.-Relat. Cancer 2022, 29, R33–R55. [Google Scholar] [CrossRef] [PubMed]
- Amrein, K.; Scherkl, M.; Hoffmann, M.; Neuwersch-Sommeregger, S.; Köstenberger, M.; Tmava Berisha, A.; Martucci, G.; Pilz, S.; Malle, O. Vitamin D deficiency 2.0: An update on the current status worldwide. Eur. J. Clin. Nutr. 2020, 74, 1498–1513. [Google Scholar] [CrossRef] [PubMed]
- Zheng, W.; Tayyari, F.; Gowda, G.N.; Raftery, D.; McLamore, E.S.; Shi, J.; Porterfield, D.M.; Donkin, S.S.; Bequette, B.; Teegarden, D. 1,25-Dihydroxyvitamin D regulation of glucose metabolism in Harvey-ras transformed MCF10A human breast epithelial cells. J. Steroid Biochem. Mol. Biol. 2013, 138, 81–89. [Google Scholar] [CrossRef]
- McNamara, M.; Rosenberger, K.D. The Significance of Vitamin D Status in Breast Cancer: A State of the Science Review. J. Midwifery Women’s Health 2019, 64, 276–288. [Google Scholar] [CrossRef] [PubMed]
- Voutsadakis, I.A. Vitamin D baseline levels at diagnosis of breast cancer: A systematic review and meta-analysis. Hematol. Oncol. Stem Cell Ther. 2020, 14, 16–26. [Google Scholar] [CrossRef]
- Tokunaga, E.; Masuda, T.; Ijichi, H.; Tajiri, W.; Koga, C.; Koi, Y.; Nakamura, Y.; Ohno, S.; Taguchi, K.; Okamoto, M. Impact of serum vitamin D on the response and prognosis in breast cancer patients treated with neoadjuvant chemotherapy. Breast Cancer 2022, 29, 156–163. [Google Scholar] [CrossRef]
- Bikle, D.D. Vitamin D Metabolism, Mechanism of Action, and Clinical Applications. Chem. Biol. 2014, 21, 319–329. [Google Scholar] [CrossRef]
- Jones, K.S.; Assar, S.; Harnpanich, D.; Bouillon, R.; Lambrechts, D.; Prentice, A.; Schoenmakers, I. 25(OH)D2 Half-Life Is Shorter Than 25(OH)D3 Half-Life and Is Influenced by DBP Concentration and Genotype. J. Clin. Endocrinol. Metab. 2014, 99, 3373–3381. [Google Scholar] [CrossRef]
- Lee, J.H.; Choi, J.-H.; Kweon, O.J.; Park, A.J. Discrepancy between Vitamin D Total Immunoassays due to Various Cross-reactivities. J. Bone Metab. 2015, 22, 107–112. [Google Scholar] [CrossRef]
- Dirks, N.F.; Ackermans, M.T.; Lips, P.; De Jongh, R.T.; Vervloet, M.G.; De Jonge, R.; Heijboer, A.C. The When, What & How of Measuring Vitamin D Metabolism in Clinical Medicine. Nutrients 2018, 10, 482. [Google Scholar] [CrossRef] [PubMed]
- Shah, I.; Akhtar, M.K.; Hisaindee, S.; Rauf, M.A.; Sadig, M.; Ashraf, S.S. Clinical diagnostic tools for vitamin D assessment. J. Steroid Biochem. Mol. Biol. 2018, 180, 105–117. [Google Scholar] [CrossRef] [PubMed]
- Zelzer, S.; Goessler, W.; Herrmann, M. Measurement of vitamin D metabolites by mass spectrometry, an analytical challenge. J. Lab. Precis. Med. 2018, 3, 99. [Google Scholar] [CrossRef]
- Puspitaningtyas, H.; Sulistyoningrum, D.C.; Witaningrum, R.; Widodo, I.; Hardianti, M.S.; Taroeno-Hariadi, K.W.; Kurnianda, J.; Purwanto, I.; Hutajulu, S.H. Vitamin D status in breast cancer cases following chemotherapy: A pre and post observational study in a tertiary hospital in Yogyakarta, Indonesia. PLoS ONE 2022, 17, e0270507. [Google Scholar] [CrossRef]
- Hauser, K.; Walsh, D.; Shrotriya, S.; Karafa, M. Low 25-hydroxyvitamin D levels in people with a solid tumor cancer diagnosis: The tip of the iceberg? Support Care Cancer 2014, 22, 1931–1939. [Google Scholar] [CrossRef]
- Kailajärvi, M.E.H.; Salminen, E.K.; Paija, O.M.M.; Virtanent, A.M.; Leino, A.E.; Irjala, K.A. Serum bone markers in breast cancer patients during 5-fluorouracil, epirubicin and cyclophosphamide (FEC) therapy. Anticancer Res. 2004, 24, 1271–1274. [Google Scholar]
- Hatse, S.; Lambrechts, D.; Verstuyf, A.; Smeets, A.; Brouwers, B.; Vandorpe, T.; Brouckaert, O.; Peuteman, G.; Laenen, A.; Verlinden, L.; et al. Vitamin D status at breast cancer diagnosis: Correlation with tumor characteristics, disease outcome, and genetic determinants of vitamin D insufficiency. Carcinogenesis 2012, 33, 1319–1326. [Google Scholar] [CrossRef]
- Janbabai, G.; Shekarriz, R.; Hassanzadeh, H.; Aarabi, M.; Borhani, S.S. A survey on the relationship between serum 25-hydroxy vitamin D level and tumor characteristics in patients with breast cancer. Int. J. Hematol. Stem Cell Res. 2016, 10, 30–36. [Google Scholar]
- Imtiaz, S.; Siddiqui, N.; Raza, S.A.; Loya, A.; Muhammad, A. Vitamin D deficiency in newly diagnosed breast cancer patients. Indian J. Endocrinol. Metab. 2012, 16, 409–413. [Google Scholar] [CrossRef] [PubMed]
- Al-Zohily, B.; Al-Menhali, A.; Gariballa, S.; Haq, A.; Shah, I. Epimers of Vitamin D: A Review. Int. J. Mol. Sci. 2020, 21, 470. [Google Scholar] [CrossRef] [PubMed]
- Nygaard, R.H.; Nielsen, M.C.; Antonsen, K.W.; Højskov, C.S.; Sørensen, B.S.; Møller, H.J. Metabolism of 25-Hydroxy-Vitamin D in Human Macrophages Is Highly Dependent on Macrophage Polarization. Int. J. Mol. Sci. 2022, 23, 10943. [Google Scholar] [CrossRef]
- Molnár, F.; Sigüeiro, R.; Sato, Y.; Araujo, C.; Schuster, I.; Antony, P.; Peluso, J.; Muller, C.; Mouriño, A.; Moras, D.; et al. 1α,25(OH)2-3-Epi-Vitamin D3, a Natural Physiological Metabolite of Vitamin D3: Its Synthesis, Biological Activity and Crystal Structure with Its Receptor. PLoS ONE 2011, 6, e18124. [Google Scholar] [CrossRef] [PubMed]
- Stepman, H.C.; Vanderroost, A.; Stöckl, D.; Thienpont, L.M. Fullscan mass spectral evidence for 3-epi-25-hydroxyvitamin D3 in serum of infants and adults. Clin. Chem. Lab. Med. 2011, 49, 253–256. [Google Scholar] [CrossRef]
- Hu, K.; Callen, D.F.; Li, J.; Zheng, H. Circulating Vitamin D and Overall Survival in Breast Cancer Patients: A Dose-Response Meta-Analysis of Cohort Studies. Integr. Cancer Ther. 2017, 17, 217–225. [Google Scholar] [CrossRef] [PubMed]
- Gradishar, W.J.; Anderson, B.O.; Blair, S.L.; Burstein, H.J.; Cyr, A.; Elias, A.D.; Farrar, W.B.; Forero, A.; Giordano, S.H.; Goldstein, L.J.; et al. Breast Cancer Version 3.2014. J. Natl. Compr. Cancer Netw. 2014, 12, 542–590. [Google Scholar] [CrossRef]
- Rola, R.; Kowalski, K.; Bieńkowski, T.; Studzińska, S. Improved sample preparation method for fast LC-MS/MS analysis of vitamin D metabolites in serum. J. Pharm. Biomed. Anal. 2020, 190, 113529. [Google Scholar] [CrossRef]
- Rola, R.; Kowalski, K.; Bieńkowski, T.; Witwicki, J.; Studzińska, S. Evaluation of different biological matrices to assess the vitamin D status in newborns using LC-MS/MS. Microchem. J. 2021, 168, 106368. [Google Scholar] [CrossRef]
- Rusińska, A.; Płudowski, P.; Walczak, M.; Borszewska-Kornacka, M.K.; Bossowski, A.; Chlebna-Sokół, D.; Czech-Kowalska, J.; Dobrzańska, A.; Franek, E.; Helwich, E.; et al. Vitamin D Supplementation Guidelines for General Population and Groups at Risk of Vitamin D Deficiency in Poland-Recommendations of the Polish Society of Pediatric Endocrinology and Diabetes and the Expert Panel with Participation of National Specialist Consultants and Representatives of Scientific Societies-2018 Update. Front. Endocrinol. 2018, 9, 246. [Google Scholar]
- Holick, M.F. The vitamin D deficiency pandemic: Approaches for diagnosis, treatment and prevention. Rev. Endocr. Metab. Disord. 2017, 18, 153–165. [Google Scholar] [CrossRef] [PubMed]
- Jacot, W.; Pouderoux, S.; Thezenas, S.; Chapelle, A.; Bleuse, J.P.; Romieu, G.; Lamy, P.J. Increased prevalence of vitamin D in-sufficiency in patients with breast cancer after neoadjuvant chemotherapy. Breast Cancer Res. Treat. 2012, 134, 709–717. [Google Scholar] [CrossRef]
- Kok, D.E.; van den Berg, M.M.G.A.; Posthuma, L.; van’t Erve, I.; van Duijnhoven, F.J.B.; de Roos, W.K.; Grosfeld, S.; Los, M.; Sommeijer, D.W.; van Laarhoven, H.W.M.; et al. Changes in Circulating Levels of 25-hydroxyvitamin D3 in Breast Cancer Patients Receiving Chemotherapy. Nutr. Cancer 2019, 71, 756–766. [Google Scholar] [CrossRef] [PubMed]
- Chen, Y.; Xu, G.; Yang, F. Effect of Neoadjuvant Chemotherapy on the Serum Levels of Bone Turnover Markers in Women with Early-Stage Breast Cancer. PLoS ONE 2015, 10, e0126053. [Google Scholar] [CrossRef] [PubMed]
- Pineda-Moncusí, M.; Garcia-Perez, M.A.; Rial, A.; Casamayor, G.; Cos, M.L.; Servitja, S.; Tusquets, I.; Diez-Perez, A.; Cano, A.; Garcia-Giralt, N. Vitamin D levels in Mediterranean breast cancer patients compared with those in healthy women. Maturitas 2018, 116, 83–88. [Google Scholar] [CrossRef]
- Gabr, H.M.; Marei, E.S. Vitamin D Level in Breast Cancer Premenopausal Patients before and after Adjuvant Therapy. Egypt. J. Radiat. Sci. Appl. 2017, 30, 85–93. [Google Scholar] [CrossRef]
- Peppone, L.J.; Huston, A.J.; Reid, M.E.; Rosier, R.N.; Zakharia, Y.; Trump, D.L.; Mustian, K.M.; Janelsins, M.C.; Purnell, J.Q.; Morrow, G.R. The effect of various vitamin D supple-mentation regimens in breast cancer patients. Breast Cancer Res. Treat. 2011, 127, 171–177. [Google Scholar] [CrossRef]
- Alco, G.; Igdem, S.; Dincer, M.; Ozmen, V.; Saglam, S.; Selamoglu, D.; Erdogan, Z.; Ordu, C.; Pilanci, K.N.; Bozdogan, A.; et al. Vitamin D levels in patients with breast cancer: Importance of dressing style. Asian Pac. J. Cancer Prev. 2014, 15, 1357–1362. [Google Scholar] [CrossRef] [PubMed]
- Goodwin, P.J.; Ennis, M.; Pritchard, K.I.; Koo, J.; Hood, N. Prognostic Effects of 25-Hydroxyvitamin D Levels in Early Breast Cancer. J. Clin. Oncol. 2009, 27, 3757–3763. [Google Scholar] [CrossRef]
- Kim, H.J.; Koh, B.S.; Yu, J.H.; Lee, J.W.; Son, B.H.; Kim, S.B.; Ahn, S.H. Changes in serum hydroxyvitamin D levels of breast cancer patients during tamoxifen treatment or chemotherapy in premenopausal breast cancer patients. Eur. J. Cancer 2014, 50, 1403–1411. [Google Scholar] [CrossRef]
- El-Bassiouny, N.A.; Helmy, M.W.; Hassan, M.A.E.; Khedr, G.A. The Cardioprotective Effect of Vitamin D in Breast Cancer Patients Receiving Adjuvant Doxorubicin Based Chemotherapy. Clin. Breast Cancer 2022, 22, 359–366. [Google Scholar] [CrossRef] [PubMed]
- Schleicher, R.L.; Sternberg, M.R.; Looker, A.C.; Yetley, E.A.; Lacher, D.A.; Sempos, C.T.; Taylor, C.L.; Durazo-Arvizu, R.A.; Maw, K.L.; Chaudhary-Webb, M.; et al. National Estimates of Serum Total 25-Hydroxyvitamin D and Metabolite Concentrations Measured by Liquid Chromatography-Tandem Mass Spectrome-try in the US Population during 2007–2010. J. Nutr. 2016, 146, 1051–1061. [Google Scholar] [CrossRef] [PubMed]
- Lutsey, P.L.; Eckfeldt, J.H.; Ogagarue, E.R.; Folsom, A.R.; Michos, E.D.; Gross, M. The 25-hydroxyvitamin D3 C-3 epimer: Distribution, correlates, and reclassification of 25-hydroxyvitamin D status in the population-based Atherosclerosis Risk in Communities Study (ARIC). Clin. Chim. Acta 2015, 442, 75–81. [Google Scholar] [CrossRef]
- Cashman, K.D.; Kinsella, M.; Walton, J.; Flynn, A.; Hayes, A.; Lucey, A.J.; Seamans, K.M.; Kiely, M. The 3 Epimer of 25-Hydroxycholecalciferol Is Present in the Circulation of the Majority of Adults in a Nationally Representative Sample and Has Endogenous Origins. J. Nutr. 2014, 144, 1050–1057. [Google Scholar] [CrossRef]
- Robsahm, T.E.; Tretli, S.; Torjesen, P.A.; Babigumira, R.; Schwartz, G.G. Serum 25-hydroxyvitamin D levels predict cancer survival: A prospective cohort with measurements prior to and at the time of cancer diagnosis. Clin. Epidemiol. 2019, 11, 695–705. [Google Scholar] [CrossRef] [PubMed]
- Kim, Y.; Je, Y. Vitamin D intake, blood 25(OH)D levels, and breast cancer risk or mortality: A meta-analysis. Br. J. Cancer 2014, 110, 2772–2784. [Google Scholar] [CrossRef]
- Villaseñor, A.; Ballard-Barbash, R.; Ambs, A.; Bernstein, L.; Baumgartner, K.; Baumgartner, R.; Ulrich, C.M.; Hollis, B.W.; McTiernan, A.; Neuhouser, M.L. Associations of serum 25-hydroxyvitamin D with overall and breast cancer–specific mortality in a multiethnic cohort of breast cancer survivors. Cancer Causes Control 2013, 24, 759–767. [Google Scholar] [CrossRef]
- Vrieling, A.; Hein, R.; Abbas, S.; Schneeweiss, A.; Flesch-Janys, D.; Chang-Claude, J. Serum 25-hydroxyvitamin D and post-menopausal breast cancer survival: A prospective patient cohort study. Breast Cancer Res. 2011, 13, R74. [Google Scholar] [CrossRef]
- Yao, S.; Kwan, M.L.; Ergas, I.J.; Roh, J.M.; Cheng, T.-Y.D.; Hong, C.-C.; McCann, S.E.; Tang, L.; Davis, W.; Liu, S.; et al. Association of Serum Level of Vitamin D at Diagnosis with Breast Cancer Survival: A Case-Cohort Analysis in the Pathways Study. JAMA Oncol. 2017, 3, 351–357. [Google Scholar] [CrossRef]
- Kanellopoulou, A.; Riza, E.; Samoli, E.; Benetou, V. Dietary Supplement Use after Cancer Diagnosis in Relation to Total Mortality, Cancer Mortality and Recurrence: A Systematic Review and Meta-Analysis. Nutr. Cancer 2020, 73, 16–30. [Google Scholar] [CrossRef]
- Madden, J.M.; Murphy, L.; Zgaga, L.; Bennett, K. De novo vitamin D supplement use post-diagnosis is associated with breast cancer survival. Breast Cancer Res. Treat. 2018, 172, 179–190. [Google Scholar] [CrossRef] [PubMed]

| Parameter | BC Patients N = 98 | 25(OH)D ≤ 20 ng/mL N = 55 | 25(OH)D > 20 ng/mL N = 43 | p-Value 4 |
|---|---|---|---|---|
| Age [years] | 58.4 ± 11.0 | 58.1 ± 12.0 | 58.9 ± 9.8 | 0.72 1 |
| Body mass index [kg/m2] | 26.7 (24.5–29.9) | 26.4 (24.3–30.1) | 27.0 (24.6–29.9) | 0.77 2 |
| Clinical stage: | 0.06 3 | |||
| I | 14 (14%) | 11 (20%) | 3 (7%) | |
| II | 44 (45%) | 18 (33%) | 26 (60%) | |
| III | 29 (30%) | 18 (33%) | 11 (26%) | |
| IV | 8 (8%) | 5 (9%) | 3 (7%) | |
| n/a | 2 (2%) | 2 (4%) | 0 (0%) | |
| Histological subtype: | 0.30 3 | |||
| NST | 74 (76%) | 41 (76%) | 33 (77%) | |
| lobular | 17 (18%) | 8 (15%) | 9 (21%) | |
| others | 6 (6%) | 5 (9%) | 1 (2%) | |
| Biological subtype: | 0.43 3 | |||
| luminal A | 19 (20%) | 7 (13%) | 12 (28%) | |
| luminal B | 33 (34%) | 20 (37%) | 13 (30%) | |
| luminal B HER2 positive | 16 (16%) | 9 (17%) | 7 (16%) | |
| non-luminal HER2 positive | 13 (13%) | 8 (15%) | 5 (12%) | |
| triple negative | 16 (16%) | 10 (19%) | 6 (14%) | |
| Chemotherapy: | 0.25 3 | |||
| neoadjuvant | 23 (24%) | 12 (23%) | 11 (26%) | |
| adjuvant | 41 (43%) | 20 (38%) | 21 (50%) | |
| palliative | 31 (33%) | 21 (40%) | 10 (24%) |
| Vitamin D Status (25(OH)D [ng/mL]) | Control Group N (%) | Breast Cancer Patient Group N (%) | |||||
|---|---|---|---|---|---|---|---|
| Baseline | p-Value 1 | after 3 Months | p-Value 1 | after 6 Months | p-Value 1 | ||
| Severe deficiency (≤10) | 2 (4.7%) | 12 (12.2%) | 0.04 | 15 (18.5%) | 0.03 | 15 (21.4%) | 0.002 |
| Deficiency (10–20) | 14 (32.5%) | 43 (43.9%) | 33 (40.7%) | 27 (38.6%) | |||
| Insufficiency (20–30) | 20 (46.5%) | 23 (23.5%) | 19 (23.5%) | 11 (15.7%) | |||
| Sufficiency (>30) | 7 (16.3%) | 20 (20.4%) | 14 (17.3%) | 17 (24.3%) | |||
| Vitamin D and Vitamin D Metabolites [ng/mL] 2 | Control Group | Breast Cancer Patient Group | |||||
| Baseline | after 3 Months | after 6 Months | |||||
| 25(OH)D | 21.45 (17.23–25.94) | 18.91 (13.07–26.60) | 17.85 (12.66–27.11) | 16.63 (11.00–29.91) | |||
| 25(OH)D2 | 0.44 (0.29–0.70) | 0.44 (0.29–0.71) | 0.42 (0.27–0.63) | 0.38 (0.26–0.59) | |||
| 25(OH)D3 | 21.08 (16.90–25.10) | 18.31 (12.69–26.34) | 17.39 (12.23–26.92) | 16.30 (9.84–29.64) | |||
| 24,25(OH)2D3 | 1.47 (0.96–2.12) | 1.18 (0.57–1.88) | 1.02 (0.51–1.56) | 0.89 (0.44–1.81) | |||
| 3-epi-25(OH)D3 | 0.92 (0.59–1.27) | 0.71 (0.48–1.14) | 0.74 (0.45–1.29) | 0.65 (0.40–1.25) | |||
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kimsa-Furdzik, M.; Bednarek, A.; Hibner, G.; Czajka-Francuz, P.; Cisoń-Jurek, S.; Karawasiecka, D.; Szymczak, B.; Wojnar, J.; Chudek, J.; Francuz, T. Vitamin D and Its Metabolites Status before and during Chemotherapy in Caucasian Breast Cancer Patients. Metabolites 2023, 13, 996. https://doi.org/10.3390/metabo13090996
Kimsa-Furdzik M, Bednarek A, Hibner G, Czajka-Francuz P, Cisoń-Jurek S, Karawasiecka D, Szymczak B, Wojnar J, Chudek J, Francuz T. Vitamin D and Its Metabolites Status before and during Chemotherapy in Caucasian Breast Cancer Patients. Metabolites. 2023; 13(9):996. https://doi.org/10.3390/metabo13090996
Chicago/Turabian StyleKimsa-Furdzik, Małgorzata, Anna Bednarek, Grzegorz Hibner, Paulina Czajka-Francuz, Sylwia Cisoń-Jurek, Dobromiła Karawasiecka, Bożena Szymczak, Jerzy Wojnar, Jerzy Chudek, and Tomasz Francuz. 2023. "Vitamin D and Its Metabolites Status before and during Chemotherapy in Caucasian Breast Cancer Patients" Metabolites 13, no. 9: 996. https://doi.org/10.3390/metabo13090996
APA StyleKimsa-Furdzik, M., Bednarek, A., Hibner, G., Czajka-Francuz, P., Cisoń-Jurek, S., Karawasiecka, D., Szymczak, B., Wojnar, J., Chudek, J., & Francuz, T. (2023). Vitamin D and Its Metabolites Status before and during Chemotherapy in Caucasian Breast Cancer Patients. Metabolites, 13(9), 996. https://doi.org/10.3390/metabo13090996






