Abstract
The prevalence of poor metabolic health is growing exponentially worldwide. This condition is associated with complex comorbidities that lead to a compromised quality of life. One of the contributing factors recently gaining attention is exposure to environmental chemicals, such as endocrine-disrupting chemicals (EDCs). Considerable evidence suggests that EDCs can alter the endocrine system through immunomodulation. More concerning, EDC exposure during the fetal development stage has prominent adverse effects later in life, which may pass on to subsequent generations. Although the mechanism of action for this phenomenon is mostly unexplored, recent reports implicate that non-coding RNAs, such as microRNAs (miRs), may play a vital role in this scenario. MiRs are significant contributors in post-transcriptional regulation of gene expression. Studies demonstrating the immunomodulation of EDCs via miRs in metabolic health or towards the Developmental Origins of Health and Disease (DOHaD) Hypothesis are still deficient. The aim of the current review was to focus on studies that demonstrate the impact of EDCs primarily on innate immunity and the potential role of miRs in metabolic health.
1. Introduction
Deteriorated metabolic health is rapidly becoming a serious public health burden across all genders, ages, and socioeconomic groups [1]. Currently, obesity is one of the leading causes of death, which impacts 35% of the US population and is predicted to increase to 42% by 2030 [2]. Additionally, medical expenditures for obesity-related conditions are expected to exceed 1 trillion USD by 2025 [3]. It is evident that the effort to treat and prevent obesity still requires improvement. Obesity has been primarily attributed to overnutrition, sedentary lifestyle, and genetic inheritance; however, it is unlikely that these are the only factors responsible for this exponential rise of the epidemic in recent years [4,5]. Emerging evidence suggests that chronic exposure to environmental chemicals may contribute to the rapid rise in the prevalence of metabolic disorders [6,7]. Additionally, disturbances during crucial developmental windows can promote subtle changes in gene expression, leading to modifications in biological and molecular processes. Ultimately, these modifications alter the developmental trajectory, leaving permanent, long-lasting metabolic dysfunction that may persist from adolescence to subsequent generations [8]. The aim of the current review was to recognize the impact of endocrine-disrupting chemicals (EDCs) primarily on innate immunity and the potential role of miRs in metabolic health.
One group of environmental chemicals that has gained widespread attention is EDCs. EDCs are abundantly present in the environment, and they can be found in food packaging, personal care products, and other manufactured products [9]. Each year, new compounds identified as endocrine modulators add to the gravity of further research to be conducted [10]. EDCs are a threat to global human health due to their carcinogenic and mutagenic properties. However, the implications of EDC’s behavior contributing to metabolic health are not fully understood [11]. They can interfere with normal bodily functions by mimicking, blocking, or interfering with the hormonal activity involved in the endocrine system [12]. In addition to these traditional pathways, recent evidence suggests that EDCs can modulate via epigenetic regulations or non-coding RNA mediated pathways [13].
Exposure to EDCs has been proven to alter normal immune processes that are essential for metabolic homeostasis [14]. The unique tissue architecture of adipose and its close proximity to immune cells facilitates their interaction for survival during periods of starvation and immunological challenge [15,16]. This crosstalk between the immune system and adipocytes is one of the key mechanisms in the progression of metabolic disease and any perturbations in this communication can contribute to the immunomodulation of metabolic health [16]. Furthermore, the impact of EDCs on the immune cells and immunity has also been demonstrated [17]. Several reports confirm the effect of these chemicals on the function, development, and lifespan of immune cells [18,19,20]. It has been primarily suggested that EDCs bind to the transporting proteins in the blood and subsequently to the nuclear receptors, thus modifying the permeability of the ion influx and leading to abnormal immune function [19,21,22].
EDCs are also known to interfere with the hormone homeostasis and endocrine signaling, both of which directly govern embryonic development during pregnancy [23]. Accumulating evidence reveals that exposure to EDCs in early life can propagate non-communicable diseases throughout one’s lifetime [24]. This is in line with the DOHaD hypothesis, which suggests that exposure to environmental disturbances during pregnancy can lead to offspring adaptations, potentially leading to the development of chronic diseases in the later stages of life [24]. These adaptations are majorly thought to be through epigenetic modifications, including histone modification and DNA methylation [25,26]. In addition to epigenetic modifications, the impact of EDCs on non-coding RNAs (ncRNA) is being studied [27,28,29,30,31,32,33]. However, among all the ncRNA types, miRs have gained interest for their putative regulation by EDCs in metabolic disturbances.
In the current review, we highlight the impact of EDCs exposure on immunomodulation via miR regulation in metabolic disease. We discuss the scenario in the same generation, as well as multigenerational and transgenerational changes. From the literature, we also include a list of EDCs with a potential direct or indirect role in the alteration of the immune system and metabolism via miRs. Finally, we propose the link between EDCs, miRs, immune response, and metabolism (Figure 1) to complement the existing knowledge of the detrimental effect of EDCs on immunomodulation of metabolic health.
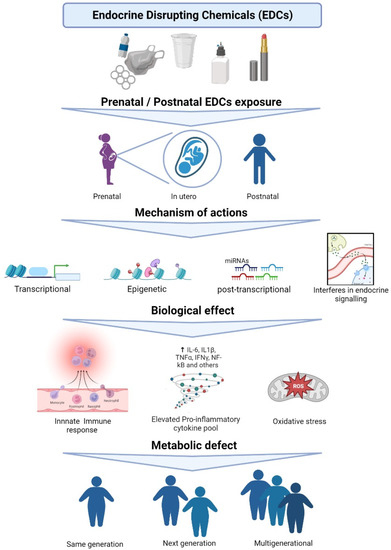
Figure 1.
Various mechanisms of actions of EDC leading to metabolic health defects.
2. EDCs Exposure and the Immune System
The progression of disease due to EDC exposure during development has been associated with alterations in the immune system of humans [34]. The immune system is a collaborative network of cells and proteins that protect the body against anything that is identified as non-self or foreign. It comprises bone marrow, the thymus, the spleen, white blood cells, antibodies, the complement system, and the lymphatic system [8]. The complementary machineries within the immune system are innate immunity and adaptive immunity. The innate immune response is the first line of defense that is activated to destroy intruding material. It is non-specific and acts via physical barriers (e.g., skin and mucous membrane, cilia) and chemical barriers (e.g., lysozyme, gastric juice, and saliva). The second line of defense is the adaptive immune response. It is designed to react against specific recognized antigens located on foreign material. It is carried out by the lymphocytes that are responsible for the development of immunological memory. Innate control of adaptive immunity plays a crucial role during the development of immune response, which further contributes to the activation of long-lasting adaptive immunity [35]. Exposure to EDCs can directly affect the innate immune response, contributing to endocrine imbalance [36]. Therefore, we focus on the impact of EDCs on the innate immune system.
The innate immune system consists of monocytes, macrophages, mast cells, neutrophils, and natural killer cells [8]. Monocytes express various receptors capable of monitoring and sensing environmental changes. Typically, a monocyte cell circulates in the blood for about 1–3 days before migrating into the tissues where they differentiate into a macrophage or a dendritic cell. Monocytes and macrophages are one of the major sources of tumor necrosis factor-alpha (TNF-α) [37]. In a mouse macrophage cell line, EDCs can alter the inflammatory response and the host’s defense mechanism against pathogens [38]. Overall, this demonstrates that alteration in the TNF-α secretion pattern by macrophages at local disease sites is accompanied by the development of inflammatory diseases [39]. A study by Kuan et al. showed elevated levels of TNF-α secretion in RAW 264.7 cells exposed to bisphenol A (BPA), an industrial plasticizer [40]. One of the most recent meta-analyses conducted to investigate the link between EDCs and inflammatory markers in humans revealed that BPA exposure is linked to the differential levels of C-reactive protein (CRP) and IL-6 [41]. Di-2-ethylhexyl phthalate (DEHP) enhances TNF-α production from monocytes/macrophages in vitro and in vivo [39]. Studies have shown that EDCs, including DEHP, BPA, and dichlorodiphenyltrichloroethane (DDT), can modulate the production of several interleukins, such as IL-6, IL-8, IL-4, and IL-1β [42]. This implicates EDCs’ role in metabolic dysregulation because alteration in the inflammatory and non-inflammatory cytokine pools is a common scenario in metabolic disorders [43].
In addition to macrophages and monocytes, mast cells mediate inflammatory responses, such as allergic reactions and hypersensitivity. These cells are present throughout the connective tissue of the body. A limited amount of data reveal that degranulation of mast cells and eosinophilic infiltration can be induced by exposure to phthalates [44]. Triclosan, found in cosmetics and personal care products, has been shown to inhibit RBL-2H3 mast cells by decreasing the mitochondrial membrane potential that leads to the inhibition of mitochondrial translocation and ultimately reduces the influx of calcium ions into the cells [45]. Researchers have shown that mast cells can be activated by BPA, resulting in accelerated release of histamines and leukotrienes [46].
Evidence on the impact of EDCs on mast cells implies that the alterations in inflammatory response and mitochondrial function can influence multiple cellular processes associated with inflammation, energy production, and utilization, ultimately, modulating energy homeostasis and leading to metabolic disruption.
EDC exposure also affects another group of inflammatory cells, neutrophils, the most abundant leukocytes in circulation. The impact of phthalates on neutrophils has been demonstrated by Vetrano et al. [47], who compared the effects of phthalate exposure on neonatal neutrophils and adult neutrophils. Neonatal neutrophils are susceptible to phthalate-mediated inhibition of (peroxisome proliferator-activated receptor-gamma (PPAR-γ), which ultimately leads to reduced anti-inflammatory signaling. Additionally, BPA induces neutrophil reactive oxygen species (ROS) production, which also alters neutrophil function by decreasing their chemotaxis ability [48]. An increase in ROS levels is directly associated with the inhibition of anti-oxidation activity, thereby causing oxidative stress [49]. Elevated ROS levels, oxidative stress, and reduced anti-inflammatory cytokines are crucial factors contributing to debilitating metabolic health and therefore, EDCs can stand as a significant factor in this epidemic scenario.
In addition to the aforementioned innate immune cell types, one effector lymphocyte class known as the natural killer (NK) cells are key instigators of the inflammatory response. They are the essential source of inflammatory cytokines such as TNF-α, IL-1β, and IFN-γ. An EDC, tributyltin, at the concentration of 5–100 nM enhances TNF-α production, whereas reduces its secretion at 200 nM [50]. Similarly, another EDC, dibutyltin, increases IL-6 production at a concentration of 0.05 and 0.1 μM but inhibits IL-6 production at 2.5–5 μM range [51]. These reports suggest that there is a differential effect on cytokine secretion with varying concentrations of EDC exposure. Therefore, we speculate that modulations in the cytokine pool can lead to inflammatory milieu, which is one of the hallmarks of metabolic disorder.
Apart from the effects of EDC exposure during development on innate immunity, in utero EDC exposure has been recognized as a threat to metabolic health [52]. Maternal exposure to EDCs has been identified as a risk factor for unknown infertility and complications in pregnancy including preeclampsia, miscarriage, premature birth, and gestational disorders [53]. Schjenken et al. have shown that peripheral blood cytokine levels during the first trimester correlate with the presence of phthalates in urine, but they did not examine the effects of these changes in the babies [12]. Intriguingly, research by Kim et al. connected the presence of phthalates in the first urine sample of the newborn and the body mass index (BMI) of newborns after 3 months [54]; they found that exposure to phthalates (especially, diethyl phthalate) had a positive correlation with BMI surge. Another finding showed a positive association of prenatal urinary concentration of phthalate metabolites with the obese/overweight state of children (4–7 years of age) [55]. A recent study suggests that combinational exposure to BPA and high-fat diet perinatally contributes to cardiovascular and metabolic disorders in the offspring [56]. It is evident from the aforementioned studies that maternal exposure to EDCs can either result in obstacles during pregnancy and/or leave an imprint causing metabolic disease later in life.
In line with these findings, there is growing research interest in the possible impact of EDCs on immunomodulation of metabolic health. In this context, two broadly studied EDCs are phthalate and BPA [57]. Phthalate exposure in a hepatic cell line caused activation of the NLRP3 inflammasome, demonstrating a key role in liver damage that may lead to metabolic imbalance [58]. A recent study showed decreased adiponectin levels along with increased IL-6 and TNF-α secretion in human subcutaneous adipose tissue explants upon exposure to BPA [59]. Another study demonstrated that in 3T3-L1 preadipocytes, BPA stimulates JNK and NFκB pathways, enhances proinflammatory cytokine secretion, and causes insulin resistance [60]. It has also been recognized that EDCs may modulate the therapeutic potential of mesenchymal stem cells (MSCs) by affecting the differentiation potential and other biologic features including enhanced adipogenesis, reduced osteogenesis, elevated oxidative stress, and pro-inflammatory status [61]. In addition, EDCs reduce the immunomodulatory effect of MSCs [62,63,64]. However, the mechanisms through which immunomodulation is achieved by EDCs remain unknown. The effect of EDCs on MSC biology may be attributed to epigenetic modulation, which requires further exploration [61].
In summary, current evidence suggests that exposure to EDCs has an impact on the innate immune system. EDC exposure in utero or during development can result in immunomodulation, potentially leading to metabolic health defects in later life. There are various mechanisms of action of EDCs proposed so far; however, only a few reports suggest the role of EDCs in the immunomodulation of metabolic health via miRs. We will discuss this correlation in the next section.
3. EDCs, MiR, and Innate Immunity
With rapidly developing high-throughput sequencing techniques, scientists have acknowledged that, even without protein-coding function, transcripts synthesized from a large portion of the genome have a pivotal role in many cellular processes [65]. Among other non-coding RNAs, miRs are short, single-stranded RNAs measuring around 19–25 nucleotides [66]. They are the most studied category in the non-coding RNA family [67], and have been shown to be significant regulators of mRNA [68]. They are indeed involved in many cellular functions related to energy metabolism [69,70] and are regarded as one of the key players in metabolic disorders [71].
Interestingly, the role of non-coding RNAs especially miRs in DOHaD gradually drew scientific attention in past decades [72,73,74]. As EDCs accumulate in our living environment and have extensive periods of biodegradation. Furthermore, long-term exposure can occur during the pregestational or gestational stages. Significant consequences on development can be observed in the next generation or across several generations [75]. Multiple sources suggest that the impact of EDC exposure on maternal and fetal miR profiles [76,77,78] is closely linked to the organ development of the offspring [79,80,81]. Studies have also suggested that dysregulation of the immunologic pathways is one of the key features of metabolic diseases, such as obesity and type 2 diabetes [82,83,84]. Furthermore, exposure to EDCs has also been found to induce metabolic disorders [85,86,87]. On the other hand, the role of miRs in regulation of inflammation-related genes, especially during the development of metabolic diseases, is described in many studies listed in Table 1. The above isolated findings show a significant correlation between miRs and EDCs induced immunomodulation during metabolic disease progression, as we have seen rapid growth in the number of studies focusing on the effect of EDCs on immunity via miR regulation [78,88].

Table 1.
MiRs affected by EDCs and their role in immune and metabolic processes.
3.1. Impact of EDC Exposure on MiR Regulation
EDCs, including both natural and synthetic chemicals, are initially found to induce adverse health consequences through interruption of hormone receptors. This includes estrogen receptors and retinoid receptors [9], especially during development, reproductive, and metabolic regulations [187,188]. Some of the EDCs can bind to the receptor proteins directly and can regulate downstream target gene expression [189,190]. Recently, studies have suggested other mechanisms on how EDCs induce the progression of the diseases. MiRs, which are susceptible to cellular stresses and environmental exposures [191], have been found to be influenced by EDCs as well. One of the insightful underlying mechanisms is that EDCs can regulate the miRs through their targeted hormones or receptors. Different studies in cell lines, rodents, and other vertebrates suggest that the expression of miRs can be regulated by hormones [192,193,194,195]. A study using MCF-7 breast cancer cell lines has shown that miR transcriptome alteration was induced by BPA and DDT treatment [97]. In another study, researchers showed that the treatment with perfluorooctanesulfonate alters the expression levels of about 38 miRs that are involved in thyroid hormone dysregulation [193]. A few studies also proposed that EDCs can directly modulate the expression level of miRs in different tissues or cell lines connected to metabolism [28,151,196,197,198]. For example, our recent study showed that the miR-34a-5p level is upregulated by benzyl butyl phthalate (BBP), thus promoting adipogenesis in 3T3-L1 cells through Nampt and sirtuins regulation [151]. Additionally, our data indicated that mono-(2-ethylhexyl) phthalate can induce regulation of several miRs, which are responsive to oxidative stress in vitro [28]. Besides the regulation of metabolism, EDCs also affect the cellular inflammatory response through miR modulation [196,197,199]. An in vitro study demonstrated that BPA treatment can induce the expression of miR-146a-5p, which mediates inflammatory response [197]. Lastly, tetrachlorodibenzo-p-dioxin, a pharmaceutical ligand, was found to induce cholinergic anti-inflammation through the upregulation of miR-132 [106]. One clinical study suggested that polychlorinated biphenyls (PCBs), which have similar structures as dioxin, induce miR-191 expression in peripheral blood mononuclear cells. Pathway analysis also identifies several potential targets of miR-191 that are associated with immunomodulation [113]. Taken together, EDCs may play a substantial role in alteration of miR levels and in the regulation of immune response that possibly contributes to chronic diseases such as obesity.
To understand the health consequences induced by EDCs, research focus has widened from their effect on one generation to their impact on the next generation as well as multiple generations. Since EDCs are persistent in our environment, their impression is more likely to pass through several generations and can even skip one generation and carry through to the next [200,201,202]. Moreover, when considering the prenatal and postnatal effects of EDC exposure, the situation becomes more complicated and is still under development. The transgenerational effects of EDCs on miR expression levels have been reported in several rodent and other mammal models [203,204,205,206]. For example, a mouse study showed genistein and/or BPA exposure at the developmental stage significantly affects the offspring’s miR expression patterns in the brain, leading to behavioral and metabolic alteration [203]. Paternal benzo[a]pyrene exposure led to miR expression pattern alteration in the offspring mice, and pathway analysis showed enriched target genes related to cell metabolism [204].
Several underlying mechanisms have demonstrated how miRs may navigate their effect in the next generation. First, the epigenetic imprint of miR levels can be inherited through the sperm cells [207], as they are sensitive to environmental factors such as EDCs [206,208]. Although there is no direct evidence to show that the miR profiles in oocytes is affected by the maternal environment, the effects of EDCs on DNA methylation and histone modification have been well studied in oocytes [209,210]. A mouse study showed that the oocyte transcriptome is affected in type I diabetic females [211], and alteration of miR levels is very likely to be one of the underlying mechanisms.
Secondly, EDCs can act through modification of placental development to affect fetal intrauterine growth, although the mechanism is not fully understood [212]. One of the hormones that are significantly affected by EDCs, thyroid hormone, plays an important role in placental development [213,214]. Mounting evidence also shows that miRs regulate thyroid hormone signaling by targeting hormone synthesis and the expression level of its receptors [215]. On the other hand, miR expression can also be tuned by thyroid hormone [216,217]. In the mouse model, gestational DEHP exposure leads to thyroid hormone signaling disturbance and placenta malformation; this is accomplished through suppressing Thrα1 and Thrβ1 expression and their activity, ultimately causing fetal intrauterine growth restriction [218]. A cohort study also found that PCBs are associated with induced thyroid-stimulating hormone and thyroid hormone dysregulation in pregnant women [219]. This occurrence may lead to an adverse effect in the next generation, possibly through miR modulation. Other than that, in studies using in vivo or in vitro models, EDCs have been shown to affect other hormones such as human chorionic gonadotropin and corticotropin-releasing hormone along with impacting placental development through mechanisms including miR modulation [28,89,220,221,222]. It has been shown that exposure to BPA leads to miR-146a upregulation in both 3A and HTR-8 cells, potentially implicating its important role in inflammatory response and cell growth [89]. A study in the placental transcriptome also demonstrated that the miR-146a level is significantly upregulated and associated with BPA accumulation [223].
Lastly, Some EDCs can cross the placental barrier and reach the fetus, which would have a notable impact on its development [224,225,226]. EDCs can also be found in breast milk, while others are more likely to accumulate within the adipose tissue due to their hydrophobic nature [227]. These eventually provide prolonged adverse effects to those tissues. Due to this indirect exposure, fetal miR expression levels can be affected in different organs [203,205]. On the other hand, recent studies indicated that maternal miRs can traffic into the fetal side through the placental barrier [228]; this provides a new perspective of how the fetus can be affected by the external environment. These studies together implicate miR regulation in the transgenerational and postnatal effects of EDCs.
3.2. MiR in Innate Immunity
MiRs are expressed in various cells of the innate immune system such as monocytes, macrophages, dendritic cells, granulocytes, and NK cells [229]. They can rapidly respond to external stimuli [90]. Accumulating evidence indicates that miRs modulate immune responses at various steps of the innate immune network, including (1) production and release of cytokines/chemokines; (2) pattern recognition regulation; as well as (3) monocyte development and macrophage polarization.
Inflammatory cytokines are a large family of secretory proteins, which play a key role in immune response regulation and metabolic homeostasis maintenance. Studies have suggested that miRs play an essential role in transcriptional regulation and secretion of cytokines [91,230,231,232,233]. For example, miR-155 was found to promote TNF-α expression by directly binding to the transcripts of its inhibitors in RAW cells [231]. TNF-α can also induce the expression of miR-155 [232], suggesting a reciprocal regulation between miRs and cytokines levels. Furthermore, miR-145 was found to promote TNF-α expression and secretion in human adipocytes [230]; it can also increase the bioactivity of TNF-α through inhibiting metalloprotease 17 [234]. Studies have also shown that miRs are involved in the determination of macrophage inflammatory response, which plays a critical role in obesity [235,236,237,238]. In a study using human monocytes, miR-146b was induced by LPS or IL-10, which led to the further downregulation of a cluster of Toll-like receptor (TLR) signaling genes, suggesting an anti-inflammatory role of miR-146b [237]. In another study, miR-497 treatment was found to inhibit the expression of pro-inflammatory cytokines, such as TNF-α and IL-1β, under in vivo or in vitro settings [238]. These studies suggest that miR regulation on cytokine secretion can further affect immune responses and metabolic health.
Monocytes and macrophages are predominantly derived from hematopoietic stem cells (HSCs) [239], playing an important role in inflammation regulation and homeostasis maintenance in different tissues [240,241,242]. Recently, miRs were found to be involved in the differentiation of bone marrow HSCs and the maturation of circulating monocytes [243,244]. A considerable array of miRs is highly expressed in the HSCs, such as miR-125, miR-126, and miR-146 [245,246,247,248]. Interestingly, overexpression of miR-125a has been shown to enlarge the hematopoietic stem cell pool by targeting pro-apoptotic protein BAK1 [249]. This has been shown to play a role in obesity and other metabolic diseases [250,251]. On the contrary, miR-126 serves as an inhibitor for stem cell proliferation [246]. Furthermore, the HSCs commitment to macrophage progenitors is also related to miR levels, especially controlled by the PU.1, a transcriptional factor. MiR-17p-92 is suppressed by PU.1 during myeloid differentiation, leading to the downregulation of a subset of miRs involved in myeloid progenitor maintenance [252]. These studies suggest a potential role of miRs in controlling major stages of monocyte development from HSCs. Importantly, the stemness and niche size of HSCs are sensitive to metabolic homeostasis and found to be disrupted in obesity along with other metabolic diseases [250,251,253,254]. Therefore, the maintenance of tissue homeostasis is likely to be connected to miR profile integrity and may be a factor in the metabolic scenario.
As we discussed at the beginning of the review, in metabolic tissues, such as the liver and adipose tissue, macrophages are key players in maintaining metabolic homeostasis [255]. Traditionally, macrophages are responsive to environmental cues that induce different pathways of cell differentiation to either M1 or M2. The phenotype associated with polarization towards M1 macrophages and secretion of pro-inflammatory cytokines is well characterized in many chronic diseases, such as obesity and nonalcoholic fatty liver disease [255]. Several reports suggested that miRs regulate either M1 or M2 polarization. For example, knockdown of miR-21 resulted in the reduction in M2 phenotype genes: arginase 1, mannose receptor 1, and IL-4Ra in vitro [256]. Furthermore, adipose tissue can produce or secrete a variety of pro-inflammatory and anti-inflammatory factors. This includes the adipokines leptin, adiponectin; resistin; as well as other cytokines and chemokines, such as TNF-α, IL-6, and MCP-1. These cytokines can stimulate macrophage polarization and produce negative feedback to the adipose tissue, therefore creating a vicious cycle [257,258]. Interestingly, in ewes, maternal obesity causes miR downregulation in the offspring’s muscle and further contributes to the upregulation of inflammatory cytokines [259]. Therefore, miRs can be an inevitable factor in the immune regulation and metabolic dysfunction. Overall, the interaction between miR profiles and inflammatory response has been extensively recognized and their roles in metabolic disease are significant.
In memoriam of Dr. Panzica, we would like to stress that EDCs also impact the neurological system as shown by his lifelong research. On this note, our understanding of miR functions is not limited to the metabolic processes mentioned above; it may also be expanded to include the modulation by miRs in other physiological activities [260,261,262,263]. A great number of studies indicate the tight connection between miRs and neural functions. A study showed that miR-219 was downregulated in a demyelinated mouse model via regulating MCT1 expression [264]. Another study on advanced paternal age (a risk factor for neurodevelopmental disorders) showed that miR-132 and miR-134 were both differentially regulated in rats and humans [265]. EDCs can affect the synthesis of various neuropeptides, hormones and enzymes, which results in an impact on the neural system and brain functions [266,267,268,269]. For example, Panzica group demonstrated that genistein affected the NO-producing cell number and induced significant changes in aggressive and anxiety behaviors in male mice [266]. In addition, whole-body metabolism and reproduction are also influenced by EDCs. Panzica group showed that postnatal genistein exposure induced body weight increase and significantly downregulated leptin and triiodothyronine, while the phenotypes were limited to female mice [267]. These studies suggested a potential mechanism of metabolism regulation by EDCs. Moreover, a study showed that expressions of several miRs in peripheral blood mononuclear cells were changed in anxiety disorder patients [270], suggesting a novel perspective link between miRs, immunity, and cognitive function.
4. Conclusions
In conclusion, immunomodulation is one of the major events implicated in the progression of metabolic diseases where EDCs may play a significant role. Furthermore, several studies indicated miR as one of the mechanisms of action by which EDCs carry out immunomodulation in metabolic and immune tissues. The impact of EDCs on offspring miR levels is also substantial, leading to long-lasting modulation in the next generation. However, there is a lack of information on a comprehensive mechanism of metabolic disease caused by EDC exposure through the regulation of miR. Due to the unspecific nature of miR inhibition of mRNA translation, the complexity of miR profile alteration can be amplified while reflecting on the immune modulation and metabolic dysfunction. Further work is required to define the EDC-induced cellular and physiological sensing via miR in these tissues. Although direct and indirect effects of EDCs on miRs have been illustrated by a few in vivo, in vitro, or observational studies, more molecular regulations remain to be fully addressed by loss-of-function or gain-of-function animal models. Additionally, high throughput screening, big data analysis, and machine learning may provide critical facilitation of in-depth understanding of how immune systems are affected by EDCs through miR modulation and their contribution to metabolic disease progression.
Funding
This research received no external funding.
Acknowledgments
We thank Lauren Gladwell, Anastasia Jerman, Julia Perez, and Susheel Kumar Gunasekar for assisting in constructive editing and critique.
Conflicts of Interest
The authors declare no conflict of interest.
References
- Paczkowska-Abdulsalam, M.; Kretowski, A. Obesity, Metabolic Health and Omics: Current Status and Future Directions. World J. Diabetes 2021, 12, 420–436. [Google Scholar] [CrossRef]
- Blaszczak, A.M.; Jalilvand, A.; Hsueh, W.A. Adipocytes, Innate Immunity and Obesity: A Mini-Review. Front. Immunol. 2021, 12, 650768. [Google Scholar] [CrossRef]
- The Lancet Diabetes Endocrinol. Metabolic Health: A Priority for the Post-Pandemic Era. Lancet Diabetes Endocrinol. 2021, 9, 189. [Google Scholar] [CrossRef]
- Liang, S.; Ji, L.; Kang, L.; Hu, X. Metabolic Regulation of Innate Immunity. Adv. Immunol. 2020, 145, 129–157. [Google Scholar] [PubMed]
- Paragh, G.; Seres, I.; Harangi, M.; Fülöp, P. Dynamic Interplay between Metabolic Syndrome and Immunity. Adv. Exp. Med. Biol. 2014, 824, 171–190. [Google Scholar] [PubMed]
- Zamora, A.N.; Jansen, E.C.; Tamayo-Ortiz, M.; Goodrich, J.M.; Sánchez, B.N.; Watkins, D.J.; Tamayo-Orozco, J.A.; Téllez-Rojo, M.M.; Mercado-García, A.; Baylin, A.; et al. Exposure to Phenols, Phthalates, and Parabens and Development of Metabolic Syndrome among Mexican Women in Midlife. Front. Public Health 2021, 9, 620769. [Google Scholar] [CrossRef] [PubMed]
- Heindel, J.J.; Blumberg, B.; Cave, M.; Machtinger, R.; Mantovani, A.; Mendez, M.A.; Nadal, A.; Palanza, P.; Panzica, G.; Sargis, R.; et al. Metabolism Disrupting Chemicals and Metabolic Disorders. Rep. Toxicol. 2017, 68, 3–33. [Google Scholar] [CrossRef]
- Nowak, K.; Jabłońska, E.; Ratajczak-Wrona, W. Immunomodulatory Effects of Synthetic Endocrine Disrupting Chemicals on the Development and Functions of Human Immune Cells. Environ. Int. 2019, 125, 350–364. [Google Scholar] [CrossRef]
- Diamanti-Kandarakis, E.; Bourguignon, J.-P.; Giudice, L.C.; Hauser, R.; Prins, G.S.; Soto, A.M.; Zoeller, R.T.; Gore, A.C. Endocrine-Disrupting Chemicals: An Endocrine Society Scientific Statement. Endocr. Rev. 2009, 30, 293–342. [Google Scholar] [CrossRef]
- Kumar, M.; Sarma, D.K.; Shubham, S.; Kumawat, M.; Verma, V.; Prakash, A.; Tiwari, R. Environmental Endocrine-Disrupting Chemical Exposure: Role in Non-Communicable Diseases. Front. Public Health 2020, 8, 553850. [Google Scholar] [CrossRef] [PubMed]
- Bowman, J.D.; Choudhury, M. Phthalates in Neonatal Health: Friend or Foe? J. Dev. Orig. Health Dis. 2016, 7, 652–664. [Google Scholar] [CrossRef] [PubMed]
- Schjenken, J.E.; Green, E.S.; Overduin, T.S.; Mah, C.Y.; Russell, D.L.; Robertson, S.A. Endocrine Disruptor Compounds-a Cause of Impaired Immune Tolerance Driving Inflammatory Disorders of Pregnancy? Front. Endocrinol. 2021, 12, 607539. [Google Scholar] [CrossRef]
- La Merrill, M.A.; Vandenberg, L.N.; Smith, M.T.; Goodson, W.; Browne, P.; Patisaul, H.B.; Guyton, K.Z.; Kortenkamp, A.; Cogliano, V.J.; Woodruff, T.J.; et al. Consensus on the Key Characteristics of Endocrine-Disrupting Chemicals as a Basis for Hazard Identification. Nat. Rev. Endocrinol. 2020, 16, 45–57. [Google Scholar] [CrossRef]
- Kim, J. Regulation of Immune Cell Functions by Metabolic Reprogramming. J. Immunol. Res. 2018, 2018, 8605471. [Google Scholar] [CrossRef]
- Exley, M.A.; Hand, L.; O’shea, D.; Lynch, L. Interplay between the Immune System and Adipose Tissue in Obesity. J. Endocrinol. 2014, 223, R41–R48. [Google Scholar] [CrossRef] [PubMed]
- Huang, N.; Perl, A. Metabolism as a Target for Modulation in Autoimmune Diseases. Trends Immunol. 2018, 39, 562–576. [Google Scholar] [CrossRef]
- Luebke, R.W.; Chen, D.H.; Dietert, R.; Yang, Y.; King, M.; Luster, M.I. The Comparative Immunotoxicity of Five Selected Compounds Following Developmental or Adult Exposure. J. Toxicol. Environ. Health B Crit. Rev. 2006, 9, 1–26. [Google Scholar] [CrossRef]
- Lavastre, V.; Girard, D. Tributyltin Induces Human Neutrophil Apoptosis and Selective Degradation of Cytoskeletal Proteins by Caspases. J. Toxicol. Environ. Health A 2002, 65, 1013–1024. [Google Scholar] [CrossRef] [PubMed]
- Gostner, J.M.; Raggl, E.; Becker, K.; Überall, F.; Schennach, H.; Pease, J.E.; Fuchs, D. Bisphenol a Suppresses Th1-Type Immune Response in Human Peripheral Blood Mononuclear Cells in Vitro. Immunol. Lett. 2015, 168, 285–292. [Google Scholar] [CrossRef]
- Brown, S.; Whalen, M. Tributyltin Alters Secretion of Interleukin 1 Beta from Human Immune Cells. J. Appl. Toxicol. 2015, 35, 895–908. [Google Scholar] [CrossRef]
- Yan, S.; Chen, Y.; Dong, M.; Song, W.; Belcher, S.M.; Wang, H.S. Bisphenol a and 17β-Estradiol Promote Arrhythmia in the Female Heart Via Alteration of Calcium Handling. PLoS ONE 2011, 6, e25455. [Google Scholar] [CrossRef] [PubMed]
- Soriano, S.; Alonso-Magdalena, P.; García-Arévalo, M.; Novials, A.; Muhammed, S.J.; Salehi, A.; Gustafsson, J.-A.; Quesada, I.; Nadal, A. Rapid Insulinotropic Action of Low Doses of Bisphenol-a on Mouse and Human Islets of Langerhans: Role of Estrogen Receptor B. PLoS ONE 2012, 7, e31109. [Google Scholar] [CrossRef] [PubMed]
- O’shaughnessy, K.L.; Fischer, F.; Zenclussen, A.C. Perinatal Exposure to Endocrine Disrupting Chemicals and Neurodevelopment: How Articles of Daily Use Influence the Development of Our Children. Best Pr. Res. Clin. Endocrinol. Metab. 2021, 35, 101568. [Google Scholar] [CrossRef] [PubMed]
- Barker, D.J. The Fetal and Infant Origins of Adult Disease. BMJ 1990, 301, 1111. [Google Scholar] [CrossRef]
- Dover, G.J. The Barker Hypothesis: How Pediatricans Will Diagnose and Prevent Common Adult-Onset Diseases. Trans. Am. Clin. Climatol. Assoc. 2009, 120, 199–207. [Google Scholar]
- Kang, S.C.; Lee, B.M. DNA Methylation of Estrogen Receptor Alpha Gene by Phthalates. J. Toxicol. Environ. Health A 2005, 68, 1995–2003. [Google Scholar] [CrossRef] [PubMed]
- Meruvu, S.; Zhang, J.; Bedi, Y.S.; Choudhury, M. Mono-(2-Ethylhexyl) Phthalate Induces Apoptosis through Mir-16 in Human First Trimester Placental Cell Line Htr-8/Svneo. Toxicol. Vitr. Int. J. Publ. Assoc. BIBRA 2016, 31, 35–42. [Google Scholar] [CrossRef] [PubMed]
- Meruvu, S.; Zhang, J.; Choudhury, M. Mono-(2-Ethylhexyl) Phthalate Increases Oxidative Stress Responsive Mirnas in First Trimester Placental Cell Line Htr8/Svneo. Chem. Res. Toxicol. 2016, 29, 430–435. [Google Scholar] [CrossRef] [PubMed]
- Park, M.H.; Jeong, E.; Choudhury, M. Mono-(2-Ethylhexyl)Phthalate Regulates Cholesterol Efflux Via Micrornas Regulated M(6)a Rna Methylation. Chem. Res. Toxicol. 2020, 33, 461–469. [Google Scholar] [CrossRef] [PubMed]
- Zhang, J.; Ali, H.I.; Bedi, Y.S.; Choudhury, M. The Plasticizer Bbp Selectively Inhibits Epigenetic Regulator Sirtuins. Toxicology 2015, 338, 130–141. [Google Scholar] [CrossRef]
- Zhang, J.; Choudhury, M. The Plasticizer Bbp Selectively Inhibits Epigenetic Regulator Sirtuin During Differentiation of C3h10t1/2 Stem Cell Line. Toxicol. Vitr. Int. J. Publ. Assoc. BIBRA 2017, 39, 75–83. [Google Scholar] [CrossRef] [PubMed]
- Zhang, J.; Choudhury, M. Benzyl Butyl Phthalate Induced Early Lncrna H19 Regulation in C3h10t1/2 Stem Cell Line. Chem. Res. Toxicol. 2021, 34, 54–62. [Google Scholar] [CrossRef] [PubMed]
- Zhang, J.; Powell, C.; Meruvu, S.; Sonkar, R.; Choudhury, M. Pyrroloquinoline Quinone Attenuated Benzyl Butyl Phthalate Induced Metabolic Aberration and a Hepatic Metabolomic Analysis. Biochem. Pharm. 2021, 197, 114883. [Google Scholar] [CrossRef]
- Howard, S.G. Developmental Exposure to Endocrine Disrupting Chemicals and Type 1 Diabetes Mellitus. Front. Endocrinol. 2018, 9, 513. [Google Scholar] [CrossRef]
- Iwasaki, A.; Medzhitov, R. Control of Adaptive Immunity by the Innate Immune System. Nat. Immunol. 2015, 16, 343–353. [Google Scholar] [CrossRef]
- Bennasroune, A.; Rojas, L.; Foucaud, L.; Goulaouic, S.; Laval-Gilly, P.; Fickova, M.; Couleau, N.; Durandet, C.; Henry, S.; Falla, J. Effects of 4-Nonylphenol and/or Diisononylphthalate on Thp-1 Cells: Impact of Endocrine Disruptors on Human Immune System Parameters. Int. J. Immunopathol. Pharm. 2012, 25, 365–376. [Google Scholar] [CrossRef]
- Lee, J.W.; Han, H.K.; Park, S.; Moon, E.Y. Nonylphenol Increases Tumor Formation and Growth by Suppressing Gender-Independent Lymphocyte Proliferation and Macrophage Activation. Environ. Toxicol. 2017, 32, 1679–1687. [Google Scholar] [CrossRef]
- Couleau, N.; Falla, J.; Beillerot, A.; Battaglia, E.; Innocenzo, M.D.; Plancon, S.; Laval-Gilly, P.; Bennasroune, A. Effects of Endocrine Disruptor Compounds, Alone or in Combination, on Human Macrophage-Like Thp-1 Cell Response. PLoS ONE 2015, 10, e0131428. [Google Scholar] [CrossRef]
- Hansen, J.F.; Bendtzen, K.; Boas, M.; Frederiksen, H.; Nielsen, C.H.; Rasmussen, K.; Feldt-Rasmussen, U. Influence of Phthalates on Cytokine Production in Monocytes and Macrophages: A Systematic Review of Experimental Trials. PLoS ONE 2015, 10, e0120083. [Google Scholar] [CrossRef]
- Kuan, Y.H.; Li, Y.C.; Huang, F.M.; Chang, Y.C. The Upregulation of Tumour Necrosis Factor-A and Surface Antigens Expression on Macrophages by Bisphenol a-Glycidyl-Methacrylate. Int. Endod. J. 2012, 45, 619–626. [Google Scholar] [CrossRef]
- Liu, Z.; Lu, Y.; Zhong, K.; Wang, C.; Xu, X. The Associations between Endocrine Disrupting Chemicals and Markers of Inflammation and Immune Responses: A Systematic Review and Meta-Analysis. Ecotoxicol. Environ. Saf. 2022, 234, 113382. [Google Scholar] [CrossRef] [PubMed]
- Ochiai, S.; Roediger, B.; Abtin, A.; Shklovskaya, E.; De St Groth, B.F.; Yamane, H.; Weninger, W.; Le Gros, G.; Ronchese, F. Cd326(Lo)Cd103(Lo)Cd11b(Lo) Dermal Dendritic Cells Are Activated by Thymic Stromal Lymphopoietin During Contact Sensitization in Mice. J. Immunol. 2014, 193, 2504–2511. [Google Scholar] [CrossRef] [PubMed]
- Makki, K.; Froguel, P.; Wolowczuk, I. Adipose Tissue in Obesity-Related Inflammation and Insulin Resistance: Cells, Cytokines, and Chemokines. ISRN Inflamm. 2013, 2013, 139239. [Google Scholar] [CrossRef] [PubMed]
- Bornehag, C.G.; Nanberg, E. Phthalate Exposure and Asthma in Children. Int. J. Androl. 2010, 33, 333–345. [Google Scholar] [CrossRef] [PubMed]
- Weatherly, L.M.; Nelson, A.J.; Shim, J.; Riitano, A.M.; Gerson, E.D.; Hart, A.J.; de Juan-Sanz, J.; Ryan, T.A.; Sher, R.; Hess, S.T.; et al. Antimicrobial Agent Triclosan Disrupts Mitochondrial Structure, Revealed by Super-Resolution Microscopy, and Inhibits Mast Cell Signaling Via Calcium Modulation. Toxicol. Appl. Pharmacol. 2018, 349, 39–54. [Google Scholar] [CrossRef] [PubMed]
- O’brien, E.; Dolinoy, D.C.; Mancuso, P. Bisphenol a at Concentrations Relevant to Human Exposure Enhances Histamine and Cysteinyl Leukotriene Release from Bone Marrow-Derived Mast Cells. J. Immunotoxicol. 2014, 11, 84–89. [Google Scholar] [CrossRef]
- Vetrano, A.M.; Laskin, D.L.; Archer, F.; Syed, K.; Gray, J.P.; Laskin, J.D.; Nwebube, N.; Weinberger, B. Inflammatory Effects of Phthalates in Neonatal Neutrophils. Pediatr. Res. 2010, 68, 134–139. [Google Scholar] [CrossRef]
- Balistrieri, A.; Hobohm, L.; Srivastava, T.; Meier, A.; Corriden, R. Alterations in Human Neutrophil Function Caused by Bisphenol, A. Am. J. Physiol. Cell. Physiol. 2018, 315, C636–C642. [Google Scholar] [CrossRef]
- Zhang, Y.; Mi, K.; Xue, W.; Wei, W.; Yang, H. Acute Bpa Exposure-Induced Oxidative Stress, Depressed Immune Genes Expression and Damage of Hepatopancreas in Red Swamp Crayfish Procambarus Clarkii. Fish. Shellfish. Immunol. 2020, 103, 95–102. [Google Scholar] [CrossRef]
- Thomas, L.D.; Shah, H.; Green, S.A.; Bankhurst, A.D.; Whalen, M.M. Tributyltin Exposure Causes Decreased Granzyme B and Perforin Levels in Human Natural Killer Cells. Toxicology 2004, 200, 221–233. [Google Scholar] [CrossRef]
- Brown, S.; Wilburn, W.; Martin, T.; Whalen, M. Butyltin Compounds Alter Secretion of Interleukin 6 from Human Immune Cells. J. Appl. Toxicol. 2018, 38, 201–218. [Google Scholar] [CrossRef] [PubMed]
- Rolfo, A.; Nuzzo, A.M.; De Amicis, R.; Moretti, L.; Bertoli, S.; Leone, A. Fetal-Maternal Exposure to Endocrine Disruptors: Correlation with Diet Intake and Pregnancy Outcomes. Nutrients 2020, 12, 1744. [Google Scholar] [CrossRef]
- Varshavsky, J.; Smith, A.; Wang, A.; Hom, E.; Izano, M.; Huang, H.; Padula, A.; Woodruff, T.J. Heightened Susceptibility: A Review of How Pregnancy and Chemical Exposures Influence Maternal Health. Rep. Toxicol. 2020, 92, 14–56. [Google Scholar] [CrossRef] [PubMed]
- Kim, J.H.; Park, H.; Lee, J.; Cho, G.; Choi, S.; Choi, G.; Kim, S.Y.; Eun, S.-H.; Suh, E.; Kim, S.K.; et al. Association of Diethylhexyl Phthalate with Obesity-Related Markers and Body Mass Change from Birth to 3 Months of Age. J. Epidemiol. Community. Health 2016, 70, 466–472. [Google Scholar] [CrossRef]
- Buckley, J.P.; Engel, S.M.; Braun, J.M.; Whyatt, R.M.; Daniels, J.L.; Mendez, M.A.; Richardson, D.B.; Xu, Y.; Calafat, A.M.; Wolff, M.S.; et al. Prenatal Phthalate Exposures and Body Mass Index among 4- to 7-Year-Old Children: A Pooled Analysis. Epidemiology 2016, 27, 449–458. [Google Scholar] [CrossRef]
- Liu, J.; Liao, M.; Huang, R.; You, Y.; Lin, X.; Yang, H.; Fan, L.; Zhong, Y.; Li, X.; Li, J.; et al. Perinatal Combinational Exposure to Bisphenol a and a High-Fat Diet Contributes to Transgenerational Dysregulation of Cardiovascular and Metabolic Systems in Mice. Front Cell. Dev. Biol. 2022, 10, 834346. [Google Scholar] [CrossRef] [PubMed]
- Bansal, A.; Henao-Mejia, J.; Simmons, R.A. Immune System: An Emerging Player in Mediating Effects of Endocrine Disruptors on Metabolic Health. Endocrinology 2018, 159, 32–45. [Google Scholar] [CrossRef]
- Ni, J.; Zhang, Z.; Luo, X.; Xiao, L.; Wang, N. Plasticizer Dbp Activates Nlrp3 Inflammasome through the P2x7 Receptor in Hepg2 and L02 Cells. J. Biochem. Mol. Toxicol. 2016, 30, 178–185. [Google Scholar] [CrossRef] [PubMed]
- Kadowaki, T.; Yamauchi, T.; Kubota, N.; Hara, K.; Ueki, K.; Tobe, K. Adiponectin and Adiponectin Receptors in Insulin Resistance, Diabetes, and the Metabolic Syndrome. J. Clin. Invest. 2006, 116, 1784–1792. [Google Scholar] [CrossRef]
- Valentino, R.; D’Esposito, V.; Passaretti, F.; Liotti, A.; Cabaro, S.; Longo, M.; Perruolo, G.; Oriente, F.; Beguinot, F.; Formisano, P. Bisphenol-a Impairs Insulin Action and up-Regulates Inflammatory Pathways in Human Subcutaneous Adipocytes and 3t3-L1 Cells. PLoS ONE 2013, 8, e82099. [Google Scholar] [CrossRef]
- Bateman, M.E.; Strong, A.L.; Mclachlan, J.A.; Burow, M.E.; Bunnell, B.A. The Effects of Endocrine Disruptors on Adipogenesis and Osteogenesis in Mesenchymal Stem Cells: A Review. Front. Endocrinol. 2016, 7, 171. [Google Scholar] [CrossRef]
- Pourgholaminejad, A.; Aghdami, N.; Baharvand, H.; Moazzeni, S.M. The Effect of Pro-Inflammatory Cytokines on Immunophenotype, Differentiation Capacity and Immunomodulatory Functions of Human Mesenchymal Stem Cells. Cytokine 2016, 85, 51–60. [Google Scholar] [CrossRef] [PubMed]
- Szabó, E.; Fajka-Boja, R.; Kriston-Pál; Hornung, A.; Makra, I.; Kudlik, G.; Uher, F.; Katona, R.L.; Monostori, E.; Czibula, A. Licensing by Inflammatory Cytokines Abolishes Heterogeneity of Immunosuppressive Function of Mesenchymal Stem Cell Population. Stem. Cells. Dev. 2015, 24, 2171–2180. [Google Scholar] [CrossRef] [PubMed]
- Crop, M.J.; Baan, C.C.; Korevaar, S.S.; Ijzermans, J.N.M.; Pescatori, M.; Stubbs, A.P.; Van Ijcken, W.F.J.; Dahlke, M.H.; Eggenhofer, E.; Weimar, W.; et al. Inflammatory Conditions Affect Gene Expression and Function of Human Adipose Tissue-Derived Mesenchymal Stem Cells. Clin. Exp. Immunol. 2010, 162, 474–486. [Google Scholar] [CrossRef] [PubMed]
- Mercer, T.R.; Dinger, M.E.; Mattick, J.S. Long Non-Coding Rnas: Insights into Functions. Nat. Rev. Genet. 2009, 10, 155–159. [Google Scholar] [CrossRef] [PubMed]
- Ambros, V.; Bartel, B.; Bartel, D.P.; Burge, C.B.; Carrington, J.C.; Chen, X.; Dreyfuss, G.; Eddy, S.R.; Griffiths-Jones, S.; Marshall, M.; et al. A Uniform System for Microrna Annotation. Rna 2003, 9, 277–279. [Google Scholar] [CrossRef]
- Ling, H.; Fabbri, M.; Calin, G.A. Micrornas and Other Non-Coding Rnas as Targets for Anticancer Drug Development. Nat. Rev. Drug. Discov. 2013, 12, 847–865. [Google Scholar] [CrossRef]
- Huntzinger, E.; Izaurralde, E. Gene Silencing by Micrornas: Contributions of Translational Repression and Mrna Decay. Nat. Rev. Genet. 2011, 12, 99–110. [Google Scholar] [CrossRef]
- Gangaraju, V.K.; Lin, H. Micrornas: Key Regulators of Stem Cells. Nat. Rev. Mol. Cell. Biol. 2009, 10, 116–125. [Google Scholar] [CrossRef]
- Ye, J.; Zou, M.; Li, P.; Liu, H. Microrna Regulation of Energy Metabolism to Induce Chemoresistance in Cancers. Technol. Cancer Res. Treat. 2018, 17, 1533033818805997. [Google Scholar] [CrossRef]
- Vienberg, S.; Geiger, J.; Madsen, S.; Dalgaard, L.T. Micrornas in Metabolism. Acta. Physiol. 2017, 219, 346–361. [Google Scholar] [CrossRef] [PubMed]
- Rassoulzadegan, M.; Grandjean, V.; Gounon, P.; Cuzin, F. Epigenetic Heredity in Mice: Involvement of Rna and Mirnas. J. De La Soc. De Biol. 2007, 201, 397–399. [Google Scholar] [CrossRef] [PubMed]
- Hussain, N. Epigenetic Influences That Modulate Infant Growth, Development, and Disease. Antioxid Redox Signal 2012, 17, 224–236. [Google Scholar] [CrossRef]
- Gillet, V.; Hunting, D.J.; Takser, L. Turing Revisited: Decoding the Microrna Messages in Brain Extracellular Vesicles for Early Detection of Neurodevelopmental Disorders. Curr. Environ. Health Rep. 2016, 3, 188–201. [Google Scholar] [CrossRef] [PubMed]
- Price, T.M.; Murphy, S.K.; Younglai, E.V. Perspectives: The Possible Influence of Assisted Reproductive Technologies on Transgenerational Reproductive Effects of Environmental Endocrine Disruptors. Toxicol. Sci. 2007, 96, 218–226. [Google Scholar] [CrossRef]
- Gluckman, P.D.; Hanson, M.A.; Cooper, C.; Thornburg, K.L. Effect of in Utero and Early-Life Conditions on Adult Health and Disease. N. Engl. J. Med. 2008, 359, 61–73. [Google Scholar] [CrossRef]
- Thornburg, K.L.; Shannon, J.; Thuillier, P.; Turker, M.S. In Utero Life and Epigenetic Predisposition for Disease. Adv. Genet. 2010, 71, 57–78. [Google Scholar]
- Basak, S.; Das, M.K.; Duttaroy, A.K. Plastics Derived Endocrine-Disrupting Compounds and Their Effects on Early Development. Birth. Defects. Res. 2020, 112, 1308–1325. [Google Scholar] [CrossRef]
- Voglova, K.; Bezakova, J.; Herichova, I. Progress in Micro Rna Focused Research in Endocrinology. Endocr. Regul. 2016, 50, 83–105. [Google Scholar] [CrossRef]
- Petri, R.; Malmevik, J.; Fasching, L.; Åkerblom, M.; Jakobsson, J. Mirnas in Brain Development. Exp. Cell Res. 2014, 321, 84–89. [Google Scholar] [CrossRef]
- Rajasekhar, M.; Schmitz, U.; Flamant, S.; Wong, J.J.-L.; Bailey, C.G.; Ritchie, W.; Holst, J.; Rasko, J.E.J. Identifying Microrna Determinants of Human Myelopoiesis. Sci. Rep. 2018, 8, 7264. [Google Scholar] [CrossRef] [PubMed]
- Lontchi-Yimagou, E.; Sobngwi, E.; Matsha, T.E.; Kengne, A.P. Diabetes Mellitus and Inflammation. Curr. Diab. Rep. 2013, 13, 435–444. [Google Scholar] [PubMed]
- Kawai, T.; Autieri, M.V.; Scalia, R. Adipose Tissue Inflammation and Metabolic Dysfunction in Obesity. Am. J. Physiol. Cell. Physiol. 2021, 320, C375–C391. [Google Scholar] [CrossRef]
- Rahman, S.M.; Janssen, R.C.; Choudhury, M.; Baquero, K.C.; Aikens, R.M.; de la Houssaye, B.A.; Friedman, J.E. Ccaat/Enhancer-Binding Protein B (C/Ebpβ) Expression Regulates Dietary-Induced Inflammation in Macrophages and Adipose Tissue in Mice. J. Biol. Chem. 2012, 287, 34349–34360. [Google Scholar] [CrossRef] [PubMed]
- Grün, F.; Blumberg, B. Environmental Obesogens: Organotins and Endocrine Disruption Via Nuclear Receptor Signaling. Endocrinology 2006, 147 (Suppl. 6), S50–S55. [Google Scholar] [CrossRef]
- Rönn, M.; Lind, L.; Örberg, J.; Kullberg, J.; Söderberg, S.; Larsson, A.; Johansson, L.; Ahlström, H.; Lind, P.M. Bisphenol a Is Related to Circulating Levels of Adiponectin, Leptin and Ghrelin, but Not to Fat Mass or Fat Distribution in Humans. Chemosphere 2014, 112, 42–48. [Google Scholar] [CrossRef] [PubMed]
- Zhang, L.; Nichols, R.G.; Correll, J.; Murray, I.A.; Tanaka, N.; Smith, P.B.; Hubbard, T.D.; Sebastian, A.; Albert, I.; Hatzakis, E.; et al. Persistent Organic Pollutants Modify Gut Microbiota-Host Metabolic Homeostasis in Mice through Aryl Hydrocarbon Receptor Activation. Environ. Health Perspect. 2015, 123, 679–688. [Google Scholar] [CrossRef] [PubMed]
- Vidal, O.S.; Deepika, D.; Schuhmacher, M.; Kumar, V. Edc-Induced Mechanisms of Immunotoxicity: A Systematic Review. Crit. Rev. Toxicol. 2021, 51, 634–652. [Google Scholar] [CrossRef] [PubMed]
- Avissar-Whiting, M.; Veiga, K.R.; Uhl, K.M.; Maccani, M.A.; Gagne, L.A.; Moen, E.L.; Marsit, C.J. Bisphenol a Exposure Leads to Specific Microrna Alterations in Placental Cells. Reprod. Toxicol. 2010, 29, 401–406. [Google Scholar] [CrossRef]
- Perry, M.M.; Moschos, S.A.; Williams, A.E.; Shepherd, N.J.; Larner-Svensson, H.M.; Lindsay, M.A. Rapid Changes in Microrna-146a Expression Negatively Regulate the Il-1beta-Induced Inflammatory Response in Human Lung Alveolar Epithelial Cells. J. Immunol. 2008, 180, 5689–5698. [Google Scholar] [CrossRef]
- He, Y.; Sun, X.; Huang, C.; Long, X.-R.; Lin, X.; Zhang, L.; Lv, X.-W.; Li, J. Mir-146a Regulates Il-6 Production in Lipopolysaccharide-Induced Raw264.7 Macrophage Cells by Inhibiting Notch1. Inflammation 2014, 37, 71–82. [Google Scholar] [CrossRef] [PubMed]
- Chen, S.; Feng, B.; Thomas, A.A.; Chakrabarti, S. Mir-146a Regulates Glucose Induced Upregulation of Inflammatory Cytokines Extracellular Matrix Proteins in the Retina and Kidney in Diabetes. PLoS ONE 2017, 12, e0173918. [Google Scholar] [CrossRef] [PubMed]
- Wallet, M.A.; Calderon, N.L.; Alonso, T.R.; Choe, C.S.; Catalfamo, D.L.; Lalane, C.J.; Neiva, K.G.; Panagakos, F.; Wallet, S.M. Triclosan Alters Antimicrobial and Inflammatory Responses of Epithelial Cells. Oral. Dis. 2013, 19, 296–302. [Google Scholar] [CrossRef]
- Wu, D.; Xi, Q.-Y.; Cheng, X.; Dong, T.; Zhu, X.-T.; Shu, G.; Wang, L.-N.; Jiang, Q.-Y.; Zhang, Y.-L. Mir-146a-5p Inhibits Tnf-A-Induced Adipogenesis Via Targeting Insulin Receptor in Primary Porcine Adipocytes. J. Lipid Res. 2016, 57, 1360–1372. [Google Scholar] [CrossRef] [PubMed]
- He, Q.; Song, J.; Cui, C.; Wang, J.; Hu, H.; Guo, X.; Yang, M.; Wang, L.; Yan, F.; Liang, K.; et al. Mesenchymal Stem Cell-Derived Exosomal Mir-146a Reverses Diabetic B-Cell Dedifferentiation. Stem. Cell. Res. Ther. 2021, 12, 449. [Google Scholar] [CrossRef] [PubMed]
- Li, K.; Zhao, B.; Wei, D.; Wang, W.; Cui, Y.; Qian, L.; Liu, G. Mir-146a Improves Hepatic Lipid and Glucose Metabolism by Targeting Med1. Int. J. Mol. Med. 2020, 45, 543–555. [Google Scholar] [CrossRef] [PubMed]
- Tilghman, S.L.; Bratton, M.R.; Segar, H.C.; Martin, E.C.; Rhodes, L.V.; Li, M.; McLachlan, J.A.; Wiese, T.E.; Nephew, K.P.; Burow, M.E. Endocrine Disruptor Regulation of Microrna Expression in Breast Carcinoma Cells. PLoS ONE 2012, 7, e32754. [Google Scholar] [CrossRef]
- Al-Badrani, M.; Seth, R.K.; Sarkar, S.; Kimono, D.; Mondal, A.; Bose, D.; Porter, D.E.; Scott, G.I.; Brooks, B.; Raychoudhury, S.; et al. Exogenous Pp2a Inhibitor Exacerbates the Progression of Nonalcoholic Fatty Liver Disease Via Nox2-Dependent Activation of Mir21. Am. J. Physiol. Gastrointest Liver. Physiol. 2019, 317, G408–G428. [Google Scholar] [CrossRef]
- Lai, C.Y.; Yeh, K.Y.; Lin, C.Y.; Hsieh, Y.W.; Lai, H.H.; Chen, J.R.; Hsu, C.C.; Her, G.G. Microrna-21 Plays Multiple Oncometabolic Roles in the Process of Nafld-Related Hepatocellular Carcinoma Via Pi3k/Akt, Tgf-B, and Stat3 Signaling. Cancers 2021, 13, 940. [Google Scholar] [CrossRef]
- Sun, C.; Huang, F.; Liu, X.; Xiao, X.; Yang, M.; Hu, G.; Liu, H.; Liao, L. Mir-21 Regulates Triglyceride and Cholesterol Metabolism in Non-Alcoholic Fatty Liver Disease by Targeting Hmgcr. Int. J. Mol. Med. 2015, 35, 847–853. [Google Scholar] [CrossRef]
- Lhamyani, S.; Gentile, A.-M.; Giráldez-Pérez, R.M.; Feijóo-Cuaresma, M.; Romero-Zerbo, S.Y.; Clemente-Postigo, M.; Zayed, H.; Oliva-Olivera, W.; Bermúdez-Silva, F.J.; Salas, J.; et al. Mir-21 Mimic Blocks Obesity in Mice: A Novel Therapeutic Option. Mol. Ther. Nucleic. Acids. 2021, 26, 401–416. [Google Scholar] [CrossRef] [PubMed]
- Dong, W.; Gao, W.; Cui, J.; Xu, T.; Sun, Y. Microrna-148 Is Involved in Nf-Κb Signaling Pathway Regulation after Lps Stimulation by Targeting Il-1β in Miiuy Croaker. Fish Shellfish. Immunol. 2021, 118, 66–71. [Google Scholar] [CrossRef] [PubMed]
- Yin, Q.; Wang, P.; Wu, X. Microrna -148 Alleviates Cardiac Dysfunction, Immune Disorders and Myocardial Apoptosis in Myocardial Ischemia-Reperfusion (Mi/R) Injury by Targeting Pyruvate Dehydrogenase Kinase (Pdk4). Bioengineered 2021, 12, 5552–5565. [Google Scholar] [CrossRef] [PubMed]
- Zhang, L.; Cheng, H.; Yue, Y.; Li, S.; Zhang, D.; He, R. H19 Knockdown Suppresses Proliferation and Induces Apoptosis by Regulating Mir-148b/Wnt/B-Catenin in Ox-Ldl -Stimulated Vascular Smooth Muscle Cells. J. Biomed. Sci. 2018, 25, 11. [Google Scholar] [CrossRef] [PubMed]
- Melkman-Zehavi, T.; Oren, R.; Kredo-Russo, S.; Shapira, T.; Mandelbaum, A.D.; Rivkin, N.; Nir, T.; Lennox, K.A.; Behlke, M.A.; Dor, Y.; et al. miRNAs Control Insulin Content in Pancreatic B-Cells Via Downregulation of Transcriptional Repressors. Embo. J. 2011, 30, 835–845. [Google Scholar] [CrossRef]
- Hanieh, H.; Alzahrani, A. Microrna-132 Suppresses Autoimmune Encephalomyelitis by Inducing Cholinergic Anti-Inflammation: A New Ahr-Based Exploration. Eur. J. Immunol. 2013, 43, 2771–2782. [Google Scholar]
- Liu, F.; Li, Y.; Jiang, R.; Nie, C.; Zeng, Z.; Zhao, N.; Huang, C.; Shao, Q.; Ding, C.; Qing, C.; et al. Mir-132 Inhibits Lipopolysaccharide-Induced Inflammation in Alveolar Macrophages by the Cholinergic Anti-Inflammatory Pathway. Exp. Lung. Res. 2015, 41, 261–269. [Google Scholar] [CrossRef]
- Mziaut, H.; Henniger, G.; Ganss, K.; Hempel, S.; Wolk, S.; McChord, J.; Chowdhury, K.; Ravassard, P.; Knoch, K.-P.; Krautz, C.; et al. Mir-132 Controls Pancreatic Beta Cell Proliferation and Survival through Pten/Akt/Foxo3 Signaling. Mol. Metab. 2020, 31, 150–162. [Google Scholar] [CrossRef]
- Smith, P.Y.; Hernandez-Rapp, J.; Jolivette, F.; Lecours, C.; Bisht, K.; Goupil, C.; Dorval, V.; Parsi, S.; Morin, F.; Planel, E.; et al. Mir-132/212 Deficiency Impairs Tau Metabolism and Promotes Pathological Aggregation in Vivo. Hum. Mol. Genet. 2015, 24, 6721–6735. [Google Scholar] [CrossRef]
- Heo, J.S.; Kim, S. Human Adipose Mesenchymal Stem Cells Modulate Inflammation and Angiogenesis through Exosomes. Sci. Rep. 2022, 12, 2776. [Google Scholar] [CrossRef]
- Liu, H.; Zhang, L.; Li, M.; Zhao, F.; Lu, F.; Zhang, F.; Chen, S.; Guo, J.; Zhang, R.; Yin, H. Bone Mesenchymal Stem Cell-Derived Extracellular Vesicles Inhibit Dapk1-Mediated Inflammation by Delivering Mir-191 to Macrophages. Biochem. Biophys. Res. Commun. 2022, 598, 32–39. [Google Scholar] [CrossRef] [PubMed]
- Xu, Y.; Zou, Z.; Liu, Y.; Wang, Q.; Sun, B.; Zeng, Q.; Liu, Q.; Zhang, A. Mir-191 Is Involved in Renal Dysfunction in Arsenic-Exposed Populations by Regulating Inflammatory Response Caused by Arsenic from Burning Arsenic-Contaminated Coal. Hum. Exp. Toxicol. 2020, 39, 37–46. [Google Scholar] [CrossRef] [PubMed]
- Guida, M.; Marra, M.; Zullo, F.; Guida, M.; Trifuoggi, M.; Biffali, E.; Borra, M.; De Mieri, G.; D’Alessandro, R.; De Felice, B. Association between Exposure to Dioxin-Like Polychlorinated Biphenyls and Mir-191 Expression in Human Peripheral Blood Mononuclear Cells. Mutat. Res. 2013, 753, 36–41. [Google Scholar] [CrossRef] [PubMed]
- Du, K.; Zhao, C.; Wang, L.; Wang, Y.; Zhang, K.-Z.; Shen, X.-Y.; Sun, H.-X.; Gao, W.; Lu, X. Mir-191 Inhibit Angiogenesis after Acute Ischemic Stroke Targeting Vezf1. Aging 2019, 11, 2762–2786. [Google Scholar] [CrossRef]
- Gu, Y.; Ampofo, E.; Menger, M.D.; Laschke, M.W. Mir-191 Suppresses Angiogenesis by Activation of Nf-Κb Signaling. Faseb. J. 2017, 31, 3321–3333. [Google Scholar] [CrossRef]
- Xu, X.; Zhou, X.; Zhang, J.; Li, H.; Cao, Y.; Tan, X.; Zhu, X.; Yang, J. Microrna-191 Modulates Cisplatin-Induced DNA Damage Response by Targeting Rcc2. Faseb. J. 2020, 34, 13573–13585. [Google Scholar] [CrossRef]
- Li, W.; Wu, L.; Sun, Q.; Yang, Q.; Xue, J.; Shi, M.; Tang, H.; Zhang, J.; Liu, Q. Microrna-191 Blocking the Translocation of Glut4 Is Involved in Arsenite-Induced Hepatic Insulin Resistance through Inhibiting the Irs1/Akt Pathway. Ecotoxicol. Environ. Saf. 2021, 215, 112130. [Google Scholar] [CrossRef]
- Badry, A.; Jaspers, V.L.B.; Waugh, C.A. Environmental Pollutants Modulate Rna and DNA Virus-Activated Mirna-155 Expression and Innate Immune System Responses: Insights into New Immunomodulative Mechanisms. J. Immunotoxicol. 2020, 17, 86–93. [Google Scholar] [CrossRef]
- Waugh, C.A.; Arukwe, A.; Jaspers, V.L.B. Deregulation of Microrna-155 and Its Transcription Factor Nf-Kb by Polychlorinated Biphenyls During Viral Infections. Apmis 2018, 126, 234–240. [Google Scholar] [CrossRef]
- Yang, X.; Wan, J.; Li, N.; He, C.; Zhang, Y.; Ren, Y.; Li, X.; Zhu, Y.; Liu, F.; Xia, L.; et al. Mir155 Disrupts the Intestinal Barrier by Inducing Intestinal Inflammation and Altering the Intestinal Microecology in Severe Acute Pancreatitis. Dig. Dis. Sci. 2021, 67, 2209–2219. [Google Scholar] [CrossRef]
- Wang, Y.-Z.; Feng, X.-G.; Shi, Q.-G.; Hao, Y.-L.; Yang, Y.; Zhang, A.-M.; Kong, Q.-X. Silencing of Mir155 Promotes the Production of Inflammatory Mediators in Guillain-Barré Syndrome in Vitro. Inflammation 2013, 36, 337–345. [Google Scholar] [CrossRef] [PubMed]
- Bala, S.; Csak, T.; Saha, B.; Zatsiorsky, J.; Kodys, K.; Catalano, D.; Satishchandran, A.; Szabo, G. The Pro-Inflammatory Effects of Mir-155 Promote Liver Fibrosis and Alcohol-Induced Steatohepatitis. J. Hepatol. 2016, 64, 1378–1387. [Google Scholar] [CrossRef] [PubMed]
- Du, F.; Yu, F.; Wang, Y.; Hui, Y.; Carnevale, K.; Fu, M.; Lu, H.; Fan, D. Microrna-155 Deficiency Results in Decreased Macrophage Inflammation and Attenuated Atherogenesis in Apolipoprotein E-Deficient Mice. Arter. Thromb. Vasc. Biol. 2014, 34, 759–767. [Google Scholar] [CrossRef] [PubMed]
- Zheng, C.; Zhang, J.; Chen, X.; Zhang, J.; Ding, X.; You, X.; Fan, L.; Chen, C.; Zhou, Y. Microrna-155 Mediates Obesity-Induced Renal Inflammation and Dysfunction. Inflammation 2019, 42, 994–1003. [Google Scholar] [CrossRef]
- Wu, N.; Ye, C.; Zheng, F.; Wan, G.-W.; Wu, L.-L.; Chen, Q.; Li, Y.-H.; Kang, Y.-M.; Zhu, G.-Q. Mir155-5p Inhibits Cell Migration and Oxidative Stress in Vascular Smooth Muscle Cells of Spontaneously Hypertensive Rats. Antioxidants 2020, 9, 204. [Google Scholar] [CrossRef]
- Zhang, X.; Hua, F.; Yang, Z.; Chen, Y.; Teng, X.; Huang, H.; Zhao, Y.; Shen, Z. Enhancement of Immunoregulatory Function of Modified Bone Marrow Mesenchymal Stem Cells by Targeting Socs1. Biomed. Res. Int. 2018, 2018, 3530647. [Google Scholar] [CrossRef]
- Velázquez, K.T.; Enos, R.T.; Carson, M.S.; Cranford, T.L.; Bader, J.E.; Sougiannis, A.T.; Pritchett, C.; Fan, D.; Carson, J.A.; Murphy, E.A. Mir155 Deficiency Aggravates High-Fat Diet-Induced Adipose Tissue Fibrosis in Male Mice. Physiol. Rep. 2017, 5, e13412. [Google Scholar] [CrossRef]
- Zhang, C.; Yu, S.; Zheng, B.; Liu, D.; Wan, F.; Ma, Y.; Wang, J.; Gao, Z.; Shan, Z. Mir-30c-5p Reduces Renal Ischemia-Reperfusion Involving Macrophage. Med. Sci. Monit. 2019, 25, 4362–4369. [Google Scholar] [CrossRef]
- Demolli, S.; Doebele, C.; Doddaballapur, A.; Lang, V.; Fisslthaler, B.; Chavakis, E.; Vinciguerra, M.; Sciacca, S.; Henschler, R.; Hecker, M.; et al. Microrna-30 Mediates Anti-Inflammatory Effects of Shear Stress and Klf2 Via Repression of Angiopoietin 2. J. Mol. Cell. Cardiol. 2015, 88, 111–119. [Google Scholar] [CrossRef]
- Lin, X.; Yu, S.; Ren, P.; Sun, X.; Jin, M. Human Microrna-30 Inhibits Influenza Virus Infection by Suppressing the Expression of Socs1, Socs3, and Nedd4. Cell. Microbiol. 2020, 22, e13150. [Google Scholar] [CrossRef]
- Wu, Y.; Sun, Q.; Dai, L. Immune Regulation of Mir-30 on the Mycobacterium Tuberculosis-Induced Tlr/Myd88 Signaling Pathway in Thp-1 Cells. Exp. Ther. Med. 2017, 14, 3299–3303. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Duan, Z.Q.; Shi, J.D.; Wu, M.N.; Hu, N.Z.; Hu, Y.Z. Influence of Mir-30b Regulating Humoral Immune Response by Genetic Difference. Immunol. Res. 2016, 64, 181–190. [Google Scholar] [CrossRef] [PubMed]
- Koh, E.-H.; Chernis, N.; Saha, P.K.; Xiao, L.; Bader, D.A.; Zhu, B.; Rajapakshe, K.; Hamilton, M.P.; Liu, X.; Perera, D.; et al. Mir-30a Remodels Subcutaneous Adipose Tissue Inflammation to Improve Insulin Sensitivity in Obesity. Diabetes 2018, 67, 2541–2553. [Google Scholar] [CrossRef] [PubMed]
- Mahjoor, M.; Afkhami, H.; Mollaei, M.; Nasr, A.; Shahriary, S.; Khorrami, S. Microrna-30c Delivered by Bone Marrow-Mesenchymal Stem Cells Induced Apoptosis and Diminished Cell Invasion in U-251 Glioblastoma Cell Line. Life Sci. 2021, 279, 119643. [Google Scholar] [CrossRef]
- Li, W.F.; Dai, H.; Ou, Q.; Zuo, G.Q.; Liu, C.A. Overexpression of Microrna-30a-5p Inhibits Liver Cancer Cell Proliferation and Induces Apoptosis by Targeting Mtdh/Pten/Akt Pathway. Tumour. Biol. 2016, 37, 5885–5895. [Google Scholar] [CrossRef]
- Saha, P.K.; Hamilton, M.P.; Rajapakshe, K.; Putluri, V.; Felix, J.B.; Masschelin, P.; Cox, A.R.; Bajaj, M.; Putluri, N.; Coarfa, C.; et al. Mir-30a Targets Gene Networks That Promote Browning of Human and Mouse Adipocytes. Am. J. Physiol. Endocrinol. Metab. 2020, 319, E667–E677. [Google Scholar] [CrossRef]
- Miranda, K.; Yang, X.; Bam, M.; Murphy, E.A.; Nagarkatti, P.S.; Nagarkatti, M. Microrna-30 Modulates Metabolic Inflammation by Regulating Notch Signaling in Adipose Tissue Macrophages. Int. J. Obes. 2018, 42, 1140–1150. [Google Scholar] [CrossRef]
- Zhang, Q.; Ma, X.-F.; Dong, M.-Z.; Tan, J.; Zhang, J.; Zhuang, L.-K.; Liu, S.-S.; Xin, Y.-N. Mir-30b-5p Regulates the Lipid Metabolism by Targeting Ppargc1a in Huh-7 Cell Line. Lipids. Health Dis. 2020, 19, 76. [Google Scholar] [CrossRef]
- Singh, N.P.; Miranda, K.; Singh, U.P.; Nagarkatti, P.; Nagarkatti, M. Diethylstilbestrol (Des) Induces Autophagy in Thymocytes by Regulating Beclin-1 Expression through Epigenetic Modulation. Toxicology 2018, 410, 49–58. [Google Scholar] [CrossRef]
- Zhong, J.; Baccarelli, A.A.; Mansur, A.; Adir, M.; Nahum, R.; Hauser, R.; Bollati, V.; Racowsky, C.; Machtinger, R. Maternal Phthalate and Personal Care Products Exposure Alters Extracellular Placental Mirna Profile in Twin Pregnancies. Reprod. Sci. 2019, 26, 289–294. [Google Scholar] [CrossRef]
- Waterhouse, N.J.; Sedelies, K.A.; Browne, K.A.; Wowk, M.E.; Newbold, A.; Sutton, V.R.; Clarke, C.J.P.; Oliaro, J.; Lindemann, R.K.; Bird, P.; et al. A Central Role for Bid in Granzyme B-Induced Apoptosis. J. Biol. Chem. 2005, 280, 4476–4482. [Google Scholar] [CrossRef] [PubMed]
- Zhang, W.; Zhong, B.; Zhang, C.; Luo, C.; Zhan, Y. Mir-373 Regulates Inflammatory Cytokine-Mediated Chondrocyte Proliferation in Osteoarthritis by Targeting the P2x7 Receptor. FEBS Open Bio. 2018, 8, 325–331. [Google Scholar] [CrossRef] [PubMed]
- Yin, Q.H.; Zhou, Y.; Li, Z.H.Y. Mir-373 Suppresses Cell Proliferation and Apoptosis Via Regulation of Sirt1/Pgc-1α/Nrf2 Axis in Pancreatic Cancer. Cell J. 2021, 23, 199–210. [Google Scholar] [PubMed]
- Peng, T.; Wang, T.; Liu, G.; Zhou, L. Effects of Mir-373 Inhibition on Glioblastoma Growth by Reducing Limk1 in Vitro. J Immunol Res. 2020, 2020, 7671502. [Google Scholar] [CrossRef]
- Lv, P.; Luo, Y.; Zhou, W.; Liu, B.; Zhou, Z.; Shi, Y.; Huang, R.; Peng, C.; He, Z.; Wang, J.; et al. Mir-373 Inhibits Autophagy and Further Promotes Apoptosis of Cholangiocarcinoma Cells by Targeting Ulk1. Kaohsiung J. Med. Sci. 2020, 36, 429–440. [Google Scholar] [CrossRef] [PubMed]
- Li, C.H.; Tang, S.C.; Wong, C.H.; Wang, Y.; Jiang, J.D.; Chen, Y. Berberine Induces Mir-373 Expression in Hepatocytes to Inactivate Hepatic Steatosis Associated Akt-S6 Kinase Pathway. Eur. J. Pharmacol. 2018, 825, 107–118. [Google Scholar] [CrossRef] [PubMed]
- Hart, M.; Walch-Rückheim, B.; Friedmann, K.S.; Rheinheimer, S.; Tänzer, T.; Glombitza, B.; Sester, M.; Lenhof, H.; Hoth, M.; Schwarz, E.C.; et al. Mir-34a: A New Player in the Regulation of T Cell Function by Modulation of Nf-Κb Signaling. Cell. Death. Dis. 2019, 10, 46. [Google Scholar] [CrossRef]
- Wu, J.; Li, X.; Li, D.; Ren, X.; Li, Y.; Herter, E.K.; Qian, M.; Toma, M.-A.; Wintler, A.-M.; Sérézal, I.G.; et al. Microrna-34 Family Enhances Wound Inflammation by Targeting Lgr4. J. Invest. Derm. 2020, 140, 465–476.e11. [Google Scholar] [CrossRef]
- Dehghan, R.; Najafi, R.; Jalilian, F.A.; Saidijam, M.; Radaei, Z.; Zamani, A.; Ezati, R.; Asna-Ashari, F.; Amini, R. A Promising Effect of Zerumbone with Improved Anti-Tumor-Promoting Inflammation Activity of Mir-34a in Colorectal Cancer Cell Lines. Mol. Biol. Rep. 2021, 48, 203–218. [Google Scholar] [CrossRef]
- Ostrycharz, E.; Wasik, U.; Kempinska-Podhorodecka, A.; Banales, J.M.; Milkiewicz, P.; Milkiewicz, M. Melatonin Protects Cholangiocytes from Oxidative Stress-Induced Proapoptotic and Proinflammatory Stimuli Via Mir-132 and Mir-34. Int. J. Mol. Sci. 2020, 21, 9667. [Google Scholar] [CrossRef]
- Meruvu, S.; Zhang, J.; Choudhury, M. Butyl Benzyl Phthalate Promotes Adipogenesis in 3t3-L1 Cells Via the Mirna-34a-5p Signaling Pathway in the Absence of Exogenous Adipogenic Stimuli. Chem. Res. Toxicol. 2021, 34, 2251–2260. [Google Scholar] [CrossRef] [PubMed]
- Kim, H.R.; Roe, J.S.; Lee, J.E.; Cho, E.J.; Youn, H.D. P53 Regulates Glucose Metabolism by Mir-34a. Biochem. Biophys. Res. Commun 2013, 437, 225–231. [Google Scholar] [CrossRef] [PubMed]
- Kaller, M.; Liffers, S.-T.; Oeljeklaus, S.; Kuhlmann, K.; Roeh, S.; Hoffmann, R.; Warscheid, B.; Hermeking, H. Genome-Wide Characterization of Mir-34a Induced Changes in Protein and Mrna Expression by a Combined Pulsed Silac and Microarray Analysis. Mol. Cell. Proteom. 2011, 10, M111.010462. [Google Scholar] [CrossRef] [PubMed]
- Liu, R.; Lu, Z.; Gu, J.; Liu, J.; Huang, E.; Liu, X.; Wang, L.; Yang, J.; Deng, Y.; Qian, J.; et al. Micrornas 15a and 16-1 Activate Signaling Pathways That Mediate Chemotaxis of Immune Regulatory B Cells To colorectal Tumors. Gastroenterology 2018, 154, 637–651.e7. [Google Scholar] [CrossRef]
- Tian, Y.; Cui, L.; Lin, C.; Wang, Y.; Liu, Z.; Miao, X. Lncrna Cdkn2b-As1 Relieved Inflammation of Ulcerative Colitis Via Sponging Mir-16 and Mir-195. Int. Immunopharmacol. 2020, 88, 106970. [Google Scholar] [CrossRef]
- Li, X.; Chu, Q.; Wang, H. Microrna-16 Regulates Lipopolysaccharide-Induced Inflammatory Factor Expression by Targeting Tlr4 in Normal Human Bronchial Epithelial Cells. Exp. Ther. Med. 2021, 22, 982. [Google Scholar] [CrossRef]
- Wang, M.; Li, J.; Cai, J.; Cheng, L.; Wang, X.; Xu, P.; Li, G.; Liang, X. Overexpression of Microrna-16 Alleviates Atherosclerosis by Inhibition of Inflammatory Pathways. Biomed Res. Int. 2020, 2020, 8504238. [Google Scholar] [CrossRef]
- Du, K.; He, X.; Deng, J. Microrna-16 Inhibits the Lipopolysaccharide-Induced Inflammatory Response in Nucleus Pulposus Cells of the Intervertebral Disc by Targeting Tab3. Arch. Med. Sci. 2021, 17, 500–513. [Google Scholar] [CrossRef]
- Liu, L. The Anti-Inflammatory Effect of Mir-16 through Targeting C- Reactive Protein Is Regulated by Hur in Vascular Smooth Muscle Cells. Biochem. Biophys. Res. Commun. 2020, 528, 636–643. [Google Scholar] [CrossRef]
- Wang, D.W.; Wang, Y.Q.; Shu, H.S. Mir-16 Inhibits Pituitary Adenoma Cell Proliferation Via the Suppression of Erk/Mapk Signal Pathway. Eur. Rev. Med. Pharmacol. Sci. 2020, 24, 9236. [Google Scholar]
- Wu, R.; Li, X.; Li, S.; Tang, G.; Zhang, S.; Zhu, Y.; Zhang, X.; Deng, M.; Tan, S.; Luo, S.; et al. Decreased Microrna-126 Expression in Psoriatic Cd4(+) T Cells Promotes T-Helper 17 Cell Differentiation and the Formation of Dermatitis in Imiquimod-Induced Psoriasis-Like Mice. J. Dermatol. 2021, 49, 432–440. [Google Scholar] [CrossRef] [PubMed]
- Chu, F.; Hu, Y.; Zhou, Y.; Guo, M.; Lu, J.; Zheng, W.; Xu, H.; Zhao, J.; Xu, L. Microrna-126 Deficiency Enhanced the Activation and Function of Cd4(+) T Cells by Elevating Irs-1 Pathway. Clin. Exp. Immunol. 2018, 191, 166–179. [Google Scholar] [CrossRef] [PubMed]
- Liu, J.; Wei, E.; Wei, J.; Zhou, W.; Webster, K.A.; Zhang, B.; Li, D.; Zhang, G.; Wei, Y.; Long, Y.; et al. Mir-126-Hmgb1-Hif-1 Axis Regulates Endothelial Cell Inflammation During Exposure to Hypoxia-Acidosis. Dis. Markers 2021, 2021, 4933194. [Google Scholar] [CrossRef] [PubMed]
- Tomasetti, M.; Monaco, F.; Manzella, N.; Rohlena, J.; Rohlenova, K.; Staffolani, S.; Gaetani, S.; Ciarapica, V.; Amati, M.; Bracci, M.; et al. Microrna-126 Induces Autophagy by Altering Cell Metabolism in Malignant Mesothelioma. Oncotarget 2016, 7, 36338–36352. [Google Scholar] [CrossRef]
- Shi, C.C.; Pan, L.Y.; Peng, Z.Y.; Li, J.G. Mir-126 Regulated Myocardial Autophagy on Myocardial Infarction. Eur. Rev. Med. Pharmacol. Sci. 2020, 24, 6971–6979. [Google Scholar]
- Najm, A.; Masson, F.; Preuss, P.; Georges, S.; Ory, B.; Quillard, T.; Sood, S.; Goodyear, C.S.; Veale, D.J.; Fearon, U.; et al. Microrna-17-5p Reduces Inflammation and Bone Erosions in Mice with Collagen-Induced Arthritis and Directly Targets the Jak/Stat Pathway in Rheumatoid Arthritis Fibroblast-Like Synoviocytes. Arthritis Rheumatol. 2020, 72, 2030–2039. [Google Scholar] [CrossRef]
- Liu, Y.; Lou, G.; Li, A.; Zhang, T.; Qi, J.; Ye, D.; Zheng, M.; Chen, Z. Amsc-Derived Exosomes Alleviate Lipopolysaccharide/D-Galactosamine-Induced Acute Liver Failure by Mir-17-Mediated Reduction of Txnip/Nlrp3 Inflammasome Activation in Macrophages. EBioMedicine 2018, 36, 140–150. [Google Scholar] [CrossRef]
- Zhang, X.; Liu, J.; Wu, L.; Hu, X. Micrornas of the Mir-17~9 Family Maintain Adipose Tissue Macrophage Homeostasis by Sustaining Il-10 Expression. eLife 2020, 9, 55676. [Google Scholar] [CrossRef]
- Benhamou, D.; Labi, V.; Novak, R.; Dai, I.; Shafir-Alon, S.; Weiss, A.; Gaujoux, R.; Arnold, R.; Shen-Orr, S.S.; Rajewsky, K.; et al. A C-Myc/Mir17-92/Pten Axis Controls Pi3k-Mediated Positive and Negative Selection in B Cell Development and Reconstitutes Cd19 Deficiency. Cell. Rep. 2016, 16, 419–431. [Google Scholar] [CrossRef]
- Benhamou, D.; Labi, V.; Getahun, A.; Benchetrit, E.; Dowery, R.; Rajewsky, K.; Cambier, J.C.; Melamed, D. The C-Myc/Mir17-92/Pten Axis Tunes Pi3k Activity to Control Expression of Recombination Activating Genes in Early B Cell Development. Front. Immunol. 2018, 9, 2715. [Google Scholar] [CrossRef]
- Huang, Y.; Zhang, H.; Dong, M.; Zhang, L.; Lin, J.; Ye, R.; Zhou, H.; Liu, X.; Jin, W. Mir17-92 Cluster Drives White Adipose Tissue Browning. J. Mol. Endocrinol. 2020, 65, 97–107. [Google Scholar] [CrossRef] [PubMed]
- Zhang, C.; Qian, D.; Zhao, H.; Lv, N.; Yu, P.; Sun, Z. Mir17 Improves Insulin Sensitivity through Inhibiting Expression of Ask1 and Anti-Inflammation of Macrophages. Biomed. Pharm. 2018, 100, 448–454. [Google Scholar] [CrossRef] [PubMed]
- Chiba, T.; Cerqueira, D.M.; Li, Y.; Bodnar, A.J.; Mukherjee, E.; Pfister, K.; Phua, Y.L.; Shaikh, K.; Sanders, B.T.; Hemker, S.L.; et al. Endothelial-Derived Mir-17∼92 Promotes Angiogenesis to Protect against Renal Ischemia-Reperfusion Injury. J. Am. Soc. Nephrol. 2021, 32, 553–562. [Google Scholar] [CrossRef]
- Akkouch, A.; Zhu, M.; Romero-Bustillos, M.; Eliason, S.; Qian, F.; Salem, A.K.; Amendt, B.A.; Hong, L. Microrna-200c Attenuates Periodontitis by Modulating Proinflammatory and Osteoclastogenic Mediators. Stem. Cells. Dev. 2019, 28, 1026–1036. [Google Scholar] [CrossRef] [PubMed]
- Reddy, M.A.; Jin, W.; Villeneuve, L.; Wang, M.; Lanting, L.; Todorov, I.; Kato, M.; Natarajan, R. Pro-Inflammatory Role of Microrna-200 in Vascular Smooth Muscle Cells from Diabetic Mice. Arter. Thromb. Vasc. Biol. 2012, 32, 721–729. [Google Scholar] [CrossRef]
- Chen, L.; Gibbons, D.L.; Goswami, S.; Cortez, M.A.; Ahn, Y.H.; Byers, L.A.; Zhang, X.; Yi, X.; Dwyer, D.; Lin, W.; et al. Metastasis Is Regulated Via Microrna-200/Zeb1 Axis Control of Tumour Cell Pd-L1 Expression and Intratumoral Immunosuppression. Nat. Commun. 2014, 5, 5241. [Google Scholar] [CrossRef]
- Wang, Y.; Wen, Y.; Xiao, P.; Sun, J.; Chen, M.; Gu, C.; Kong, Y.; Gu, A.; Zhang, J.; Wang, Y. Di-N-Butyl Phthalate Promotes Lipid Accumulation Via the Mir200c-5p-Abca1 Pathway in Thp-1 Macrophages. Environ. Pollut. 2020, 264, 114723. [Google Scholar] [CrossRef]
- Tao, C.; Ren, H.; Xu, P.; Cheng, J.; Huang, S.; Zhou, R.; Mu, Y.; Yang, S.; Qi, D.; Wang, Y.; et al. Adipocyte Mir-200b/a/429 Ablation in Mice Leads to High-Fat-Diet-Induced Obesity. Oncotarget 2016, 7, 67796–67807. [Google Scholar] [CrossRef]
- Jones, R.; Watson, K.; Bruce, A.; Nersesian, S.; Kitz, J.; Moorehead, R. Re-Expression of Mir-200c Suppresses Proliferation, Colony Formation and in Vivo Tumor Growth of Murine Claudin-Low Mammary Tumor Cells. Oncotarget 2017, 8, 23727–23749. [Google Scholar] [CrossRef]
- Zhao, C.; Xie, R.; Qian, Q.; Yan, J.; Wang, H.; Wang, X. Triclosan Induced Zebrafish Immunotoxicity by Targeting Mir-19a and Its Gene Socs3b to Activate Il-6/Stat3 Signaling Pathway. Sci. Total. Environ. 2022, 815, 152916. [Google Scholar] [CrossRef]
- Mu, N.; Gu, J.; Huang, T.; Zhang, C.; Shu, Z.; Li, M.; Hao, Q.; Li, W.; Zhang, W.; Zhao, J.; et al. A Novel Nf-Κb/Yy1/Microrna-10a Regulatory Circuit in Fibroblast-Like Synoviocytes Regulates Inflammation in Rheumatoid Arthritis. Sci. Rep. 2016, 6, 20059. [Google Scholar] [CrossRef]
- Wang, W.; Zhan, R.; Zhou, J.; Wang, J.; Chen, S. Mir-10 Targets Ngr to Modulate the Proliferation of Microglial Cells and the Secretion of Inflammatory Cytokines. Exp. Mol. Pathol. 2018, 105, 357–363. [Google Scholar] [CrossRef] [PubMed]
- Cho, Y.K.; Son, Y.; Kim, S.-N.; Song, H.-D.; Kim, M.; Park, J.-H.; Jung, Y.-S.; Ahn, S.-Y.; Saha, A.; Granneman, J.G.; et al. Microrna-10a-5p Regulates Macrophage Polarization and Promotes Therapeutic Adipose Tissue Remodeling. Mol. Metab. 2019, 29, 86–98. [Google Scholar] [CrossRef] [PubMed]
- Xu, D.; Li, W.; Zhang, T.; Wang, G. Mir-10a Overexpression Aggravates Renal Ischemia-Reperfusion Injury Associated with Decreased Pik3ca Expression. BMC Nephrol. 2020, 21, 248. [Google Scholar] [CrossRef] [PubMed]
- Jiajie, T.; Yanzhou, Y.; Hoi-Hung, A.C.; Zi-Jiang, C.; Wai-Yee, C. Conserved Mir-10 Family Represses Proliferation and Induces Apoptosis in Ovarian Granulosa Cells. Sci. Rep. 2017, 7, 41304. [Google Scholar] [CrossRef] [PubMed]
- Singh, R.; Ha, S.E.; Wei, L.; Jin, B.; Zogg, H.; Poudrier, S.M.; Jorgensen, B.G.; Park, C.; Ronkon, C.F.; Bartlett, A.; et al. Mir-10b-5p Rescues Diabetes and Gastrointestinal Dysmotility. Gastroenterology 2021, 160, 1662–1678.e18. [Google Scholar] [CrossRef]
- Gouesse, R.J.; Plante, I. Environmental Exposure to Bfrs: Unraveling Endocrine and Mammary Gland Effects That May Increase Disease Risk. Toxicol. Sci. 2022, 186, 190–207. [Google Scholar] [CrossRef]
- Ehrlich, S.; Lambers, D.; Baccarelli, A.; Khoury, J.; Macaluso, M.; Ho, S.M. Endocrine Disruptors: A Potential Risk Factor for Gestational Diabetes Mellitus. Am. J. Perinatol. 2016, 33, 1313–1318. [Google Scholar]
- Wolstenholme, J.T.; Rissman, E.F.; Connelly, J.J. The Role of Bisphenol a in Shaping the Brain, Epigenome and Behavior. Horm. Behav. 2011, 59, 296–305. [Google Scholar] [CrossRef]
- Hafezi, S.A.; Abdel-Rahman, W.M. The Endocrine Disruptor Bisphenol a (Bpa) Exerts a Wide Range of Effects in Carcinogenesis and Response to Therapy. Curr. Mol. Pharmacol. 2019, 12, 230–238. [Google Scholar] [CrossRef]
- Miguel, V.; Cui, J.Y.; Daimiel-Ruiz, L.; Espinosa-Díez, C.; Fernández-Hernando, C.; Kavanagh, T.J.; Lamas, S. The Role of Micrornas in Environmental Risk Factors, Noise-Induced Hearing Loss, and Mental Stress. Antioxid Redox. Signal. 2018, 28, 773–796. [Google Scholar] [CrossRef] [PubMed]
- McAllister, J.M.; Han, A.X.; Modi, B.; Teves, M.E.; Mavodza, G.R.; Anderson, Z.L.; Shen, T.; Christenson, L.K.; Archer, K.J.; Strauss, J.F. Mirna Profiling Reveals Mirna-130b-3p Mediates Dennd1a Variant 2 Expression and Androgen Biosynthesis. Endocrinology 2019, 160, 1964–1981. [Google Scholar] [CrossRef]
- Dong, H.; Curran, I.; Williams, A.; Bondy, G.; Yauk, C.L.; Wade, M.G. Hepatic Mirna Profiles and Thyroid Hormone Homeostasis in Rats Exposed to Dietary Potassium Perfluorooctanesulfonate (Pfos). Environ. Toxicol. Pharmacol. 2016, 41, 201–210. [Google Scholar] [CrossRef]
- Wang, X.; Yang, L.; Wang, H.; Shao, F.; Yu, J.; Jiang, H.; Han, Y.; Gong, D.; Gu, Z. Growth Hormone-Regulated Mrnas and Mirnas in Chicken Hepatocytes. PLoS ONE 2014, 9, e112896. [Google Scholar] [CrossRef] [PubMed]
- Aliberti, P.; Sethi, R.; Belgorosky, A.; Chandran, U.R.; Plant, T.M.; Walker, W.H. Gonadotrophin-Mediated Mirna Expression in Testis at Onset of Puberty in Rhesus Monkey: Predictions on Regulation of Thyroid Hormone Activity and Dlk1-Dio3 Locus. Mol. Hum. Reprod. 2019, 25, 124–136. [Google Scholar] [CrossRef] [PubMed]
- Lo, W.-Y.; Peng, C.-T.; Wang, H.-J. Microrna-146a-5p Mediates High Glucose-Induced Endothelial Inflammation Via Targeting Interleukin-1 Receptor-Associated Kinase 1 Expression. Front Physiol. 2017, 8, 551. [Google Scholar] [CrossRef]
- Gao, G.-Z.; Zhao, Y.; Li, H.-X.; Li, W. Bisphenol a-Elicited Mir-146a-5p Impairs Murine Testicular Steroidogenesis through Negative Regulation of Mta3 Signaling. Biochem. Biophys. Res. Commun. 2018, 501, 478–485. [Google Scholar] [CrossRef]
- Larocca, J.; Binder, A.M.; Mcelrath, T.F.; Michels, K.B. First-Trimester Urine Concentrations of Phthalate Metabolites and Phenols and Placenta Mirna Expression in a Cohort of Us Women. Environ. Health Perspect. 2016, 124, 380–387. [Google Scholar] [CrossRef]
- Park, M.H.; Gutiérrez-García, A.K.; Choudhury, M. Mono-(2-Ethylhexyl) Phthalate Aggravates Inflammatory Response Via Sirtuin Regulation and Inflammasome Activation in Raw 264.7 Cells. Chem. Res. Toxicol. 2019, 32, 935–942. [Google Scholar] [CrossRef]
- Li, G.; Chang, H.; Xia, W.; Mao, Z.; Li, Y.; Xu, S. F0 Maternal Bpa Exposure Induced Glucose Intolerance of F2 Generation through DNA Methylation Change in Gck. Toxicol. Lett. 2014, 228, 192–199. [Google Scholar] [CrossRef]
- Skinner, M.K.; Manikkam, M.; Tracey, R.; Guerrero-Bosagna, C.; Haque, M.; Nilsson, E.E. Ancestral Dichlorodiphenyltrichloroethane (Ddt) Exposure Promotes Epigenetic Transgenerational Inheritance of Obesity. BMC Med. 2013, 11, 228. [Google Scholar] [CrossRef] [PubMed]
- Crews, D.; Mclachlan, J.A. Epigenetics, Evolution, Endocrine Disruption, Health, and Disease. Endocrinology 2006, 147 (Suppl. 6), S4–S10. [Google Scholar] [CrossRef]
- Kaur, S.; Kinkade, J.A.; Green, M.T.; Martin, R.E.; Willemse, T.E.; Bivens, N.J.; Schenk, A.K.; Helferich, W.G.; Trainor, B.C.; Fass, J.; et al. Disruption of Global Hypothalamic Microrna (Mir) Profiles and Associated Behavioral Changes in California Mice (Peromyscus Californicus) Developmentally Exposed to Endocrine Disrupting Chemicals. Horm. Behav. 2021, 128, 104890. [Google Scholar] [CrossRef]
- Brevik, A.; Lindeman, B.; Brunborg, G.; Duale, N. Paternal Benzo[a]Pyrene Exposure Modulates Microrna Expression Patterns in the Developing Mouse Embryo. Int. J. Cell Biol. 2012, 2012, 407431. [Google Scholar] [CrossRef] [PubMed]
- Veiga-Lopez, A.; Luense, L.J.; Christenson, L.K.; Padmanabhan, V. Developmental Programming: Gestational Bisphenol-a Treatment Alters Trajectory of Fetal Ovarian Gene Expression. Endocrinology 2013, 154, 1873–1884. [Google Scholar] [CrossRef]
- Brieño-Enríquez, M.A.; García-López, J.; Cárdenas, D.B.; Guibert, S.; Cleroux, E.; Děd, L.; Hourcade, J.D.D.; Pěknicová, J.; Weber, M.; del Mazo, J. Exposure to Endocrine Disruptor Induces Transgenerational Epigenetic Deregulation of Micrornas in Primordial Germ Cells. PLoS ONE 2015, 10, e0124296. [Google Scholar] [CrossRef]
- Fullston, T.; Teague, E.M.C.O.; Palmer, N.O.; DeBlasio, M.J.; Mitchell, M.; Corbett, M.; Print, C.G.; Owens, J.A.; Lane, M. Paternal Obesity Initiates Metabolic Disturbances in Two Generations of Mice with Incomplete Penetrance to the F2 Generation and Alters the Transcriptional Profile of Testis and Sperm Microrna Content. Faseb. J. 2013, 27, 4226–4243. [Google Scholar] [CrossRef] [PubMed]
- Ho, S.-M.; Cheong, A.; Adgent, M.A.; Veevers, J.; Suen, A.A.; Tam, N.N.C.; Leung, Y.-K.; Jefferson, W.N.; Williams, C.J. Environmental Factors, Epigenetics, and Developmental Origin of Reproductive Disorders. Reprod. Toxicol. 2017, 68, 85–104. [Google Scholar] [CrossRef] [PubMed]
- Kelly, T.L.; Trasler, J.M. Reproductive Epigenetics. Clin. Genet. 2004, 65, 247–260. [Google Scholar] [CrossRef] [PubMed]
- Bredfeldt, T.G.; Greathouse, K.L.; Safe, S.H.; Hung, M.C.; Bedford, M.T.; Walker, C.L. Xenoestrogen-Induced Regulation of Ezh2 and Histone Methylation Via Estrogen Receptor Signaling to Pi3k/Akt. Mol Endocrinol. 2010, 24, 993–1006. [Google Scholar] [CrossRef] [PubMed]
- Ma, J.-Y.; Li, M.; Ge, Z.-J.; Luo, Y.; Ou, X.-H.; Song, S.; Tian, D.; Yang, J.; Zhang, B.; Ou-Yang, Y.-C.; et al. Whole Transcriptome Analysis of the Effects of Type I Diabetes on Mouse Oocytes. PLoS ONE 2012, 7, e41981. [Google Scholar] [CrossRef] [PubMed]
- Yang, C.; Song, G.; Lim, W. A Mechanism for the Effect of Endocrine Disrupting Chemicals on Placentation. Chemosphere 2019, 231, 326–336. [Google Scholar] [CrossRef] [PubMed]
- Chen, C.Y.; Chen, C.P.; Lin, K.H. Biological Functions of Thyroid Hormone in Placenta. Int. J. Mol. Sci. 2015, 16, 4161–4179. [Google Scholar] [CrossRef]
- Zoeller, R.T. Endocrine Disrupting Chemicals and Thyroid Hormone Action. Adv. Pharmacol. 2021, 92, 401–417. [Google Scholar] [PubMed]
- Aranda, A. Micrornas and Thyroid Hormone Action. Mol. Cell Endocrinol. 2021, 525, 111175. [Google Scholar] [CrossRef] [PubMed]
- Lin, Y.-H.; Wu, M.-H.; Liao, C.-J.; Huang, Y.-H.; Chi, H.-C.; Wu, S.-M.; Chen, C.-Y.; Tseng, Y.-H.; Tsai, C.-Y.; Chung, I.-H.; et al. Repression of Microrna-130b by Thyroid Hormone Enhances Cell Motility. J. Hepatol. 2015, 62, 1328–1340. [Google Scholar] [CrossRef]
- Jazdzewski, K.; Boguslawska, J.; Jendrzejewski, J.; Liyanarachchi, S.; Pachucki, J.; Wardyn, K.A.; Nauman, A.; de la Chapelle, A. Thyroid Hormone Receptor B (Thrb) Is a Major Target Gene for Micrornas Deregulated in Papillary Thyroid Carcinoma (Ptc). J. Clin. Endocrinol. Metab. 2011, 96, E546–E553. [Google Scholar] [CrossRef]
- Yu, Z.; Han, Y.; Shen, R.; Huang, K.; Xu, Y.-Y.; Wang, Q.-N.; Zhou, S.-S.; Xu, D.-X.; Tao, F.-B. Gestational Di-(2-Ethylhexyl) Phthalate Exposure Causes Fetal Intrauterine Growth Restriction through Disturbing Placental Thyroid Hormone Receptor Signaling. Toxicol. Lett. 2018, 294, 1–10. [Google Scholar] [CrossRef]
- Berlin, M.; Barchel, D.; Brik, A.; Kohn, E.; Livne, A.; Keidar, R.; Tovbin, J.; Betser, M.; Moskovich, M.; Mandel, D.; et al. Maternal and Newborn Thyroid Hormone, and the Association with Polychlorinated Biphenyls (Pcbs) Burden: The Ehf (Environmental Health Fund) Birth Cohort. Front Pediatr. 2021, 9, 705395. [Google Scholar] [CrossRef]
- Wang, X.K.; Agarwal, M.; Parobchak, N.; Rosen, A.; Vetrano, A.M.; Srinivasan, A.; Wang, B.; Rosen, T. Mono-(2-Ethylhexyl) Phthalate Promotes Pro-Labor Gene Expression in the Human Placenta. PLoS ONE 2016, 11, e0147013. [Google Scholar] [CrossRef]
- Shoaito, H.; Petit, J.; Chissey, A.; Auzeil, N.; Guibourdenche, J.; Gil, S.; Laprévote, O.; Fournier, T.; Degrelle, S.A. The Role of Peroxisome Proliferator–Activated Receptor Gamma (Pparγ) in Mono(2-Ethylhexyl) Phthalate (Mehp)-Mediated Cytotrophoblast Differentiation. Environ. Health Perspect. 2019, 127, 27003. [Google Scholar] [CrossRef] [PubMed]
- Petit, J.; Wakx, A.; Gil, S.; Fournier, T.; Auzeil, N.; Rat, P.; Laprévote, O. Lipidome-Wide Disturbances of Human Placental Jeg-3 Cells by the Presence of Mehp. Biochimie 2018, 149, 1–8. [Google Scholar] [CrossRef] [PubMed]
- De Felice, B.; Manfellotto, F.; Palumbo, A.R.; Troisi, J.; Zullo, F.; Di Carlo, C.; Sardo, A.D.S.; De Stefano, N.; Ferbo, U.; Guida, M.; et al. Genome-Wide Microrna Expression Profiling in Placentas from Pregnant Women Exposed to Bpa. BMC Med. Genom. 2015, 8, 56. [Google Scholar] [CrossRef]
- Vizcaino, E.; Grimalt, J.O.; Fernández-Somoano, A.; Tardon, A. Transport of Persistent Organic Pollutants across the Human Placenta. Environ. Int. 2014, 65, 107–115. [Google Scholar] [CrossRef] [PubMed]
- Cariou, R.; Veyrand, B.; Yamada, A.; Berrebi, A.; Zalko, D.; Durand, S.; Pollono, C.; Marchand, P.; Leblanc, J.-C.; Antignac, J.-P.; et al. Perfluoroalkyl Acid (Pfaa) Levels and Profiles in Breast Milk, Maternal and Cord Serum of French Women and Their Newborns. Environ. Int. 2015, 84, 71–81. [Google Scholar] [CrossRef]
- Mørck, T.J.; Sorda, G.; Bechi, N.; Rasmussen, B.S.; Nielsen, J.B.; Ietta, F.; Rytting, E.; Mathiesen, L.; Paulesu, L.; Knudsen, L.E. Placental Transport and in Vitro Effects of Bisphenol A. Reprod. Toxicol. 2010, 30, 131–137. [Google Scholar] [CrossRef]
- Stefanidou, M.; Maravelias, C.; Spiliopoulou, C. Human Exposure to Endocrine Disruptors and Breast Milk. Endocr. Metab. Immune Disord Drug Targets 2009, 9, 269–276. [Google Scholar] [CrossRef]
- Chang, G.; Mouillet, J.-F.; Mishima, T.; Chu, T.; Sadovsky, E.; Coyne, C.B.; Parks, W.T.; Surti, U.; Sadovsky, Y. Expression and Trafficking of Placental Micrornas at the Feto-Maternal Interface. FASEB J. 2017, 31, 2760–2770. [Google Scholar] [CrossRef]
- Tsitsiou, E.; Lindsay, M.A. Micrornas and the Immune Response. Curr. Opin Pharm. 2009, 9, 514–520. [Google Scholar] [CrossRef]
- Lorente-Cebrián, S.; Mejhert, N.; Kulyté, A.; Laurencikiene, J.; Åström, G.; Hedén, P.; Ryden, M.; Arner, P. Micrornas Regulate Human Adipocyte Lipolysis: Effects of Mir-145 Are Linked to Tnf-A. PLoS ONE 2014, 9, e86800. [Google Scholar] [CrossRef]
- Tili, E.; Michaille, J.J.; Cimino, A.; Costinean, S.; Dumitru, C.D.; Adair, B.; Fabbri, M.; Alder, H.; Liu, C.G.; Calin, G.A.; et al. Modulation of Mir-155 and Mir-125b Levels Following Lipopolysaccharide/Tnf-Alpha Stimulation and Their Possible Roles in Regulating the Response to Endotoxin Shock. J. Immunol. 2007, 179, 5082–5089. [Google Scholar] [CrossRef] [PubMed]
- Imaizumi, T.; Tanaka, H.; Tajima, A.; Yokono, Y.; Matsumiya, T.; Yoshida, H.; Tsuruga, K.; Aizawa-Yashiro, T.; Hayakari, R.; Inoue, I.; et al. Ifn-Γ and Tnf-A Synergistically Induce Microrna-155 Which Regulates Tab2/Ip-10 Expression in Human Mesangial Cells. Am. J. Nephrol. 2010, 32, 462–468. [Google Scholar] [CrossRef]
- Xie, Y.F.; Shu, R.; Jiang, S.Y.; Liu, D.L.; Ni, J.; Zhang, X.L. Microrna-146 Inhibits Pro-Inflammatory Cytokine Secretion through Il-1 Receptor-Associated Kinase 1 in Human Gingival Fibroblasts. J. Inflamm. 2013, 10, 20. [Google Scholar] [CrossRef] [PubMed]
- Doberstein, K.; Steinmeyer, N.; Hartmetz, A.-K.; Eberhardt, W.; Mittelbronn, M.; Harter, P.N.; Juengel, E.; Blaheta, R.; Pfeilschifter, J.; Gutwein, P. Microrna-145 Targets the Metalloprotease Adam17 and Is Suppressed in Renal Cell Carcinoma Patients. Neoplasia 2013, 15, 218–230. [Google Scholar] [CrossRef] [PubMed]
- Liu, Y.C.; Zou, X.B.; Chai, Y.F.; Yao, Y.M. Macrophage Polarization in Inflammatory Diseases. Int. J. Biol. Sci. 2014, 10, 520–529. [Google Scholar] [CrossRef] [PubMed]
- Essandoh, K.; Li, Y.; Huo, J.; Fan, G.C. Mirna-Mediated Macrophage Polarization and Its Potential Role in the Regulation of Inflammatory Response. Shock 2016, 46, 122–131. [Google Scholar] [CrossRef]
- Curtale, G.; Mirolo, M.; Renzi, T.A.; Rossato, M.; Bazzoni, F.; Locati, M. Negative Regulation of Toll-Like Receptor 4 Signaling by Il-10-Dependent Microrna-146b. Proc. Natl. Acad. Sci. USA 2013, 110, 11499–11504. [Google Scholar] [CrossRef]
- Ban, E.; Jeong, S.; Park, M.; Kwon, H.; Park, J.; Song, E.J.; Kim, A. Accelerated Wound Healing in Diabetic Mice by Mirna-497 and Its Anti-Inflammatory Activity. Biomed. Pharm. 2020, 121, 109613. [Google Scholar] [CrossRef]
- Gordon, S.; Taylor, P.R. Monocyte and Macrophage Heterogeneity. Nat. Rev. Immunol. 2005, 5, 953–964. [Google Scholar] [CrossRef]
- Mantovani, A.; Biswas, S.K.; Galdiero, M.R.; Sica, A.; Locati, M. Macrophage Plasticity and Polarization in Tissue Repair and Remodelling. J. Pathol. 2013, 229, 176–185. [Google Scholar] [CrossRef]
- Ginhoux, F.; Greter, M.; Leboeuf, M.; Nandi, S.; See, P.; Gokhan, S.; Mehler, M.F.; Conway, S.J.; Ng, L.G.; Stanley, E.R.; et al. Fate Mapping Analysis Reveals That Adult Microglia Derive from Primitive Macrophages. Science 2010, 330, 841–845. [Google Scholar] [CrossRef] [PubMed]
- Hoeffel, G.; Wang, Y.; Greter, M.; See, P.; Teo, P.; Malleret, B.; Leboeuf, M.; Low, D.; Oller, G.; Almeida, F.; et al. Adult Langerhans Cells Derive Predominantly from Embryonic Fetal Liver Monocytes with a Minor Contribution of Yolk Sac–Derived Macrophages. J. Exp. Med. 2012, 209, 1167–1181. [Google Scholar] [CrossRef] [PubMed]
- Luinenburg, D.G.; De Haan, G. Micrornas in Hematopoietic Stem Cell Aging. Mech. Ageing Dev. 2020, 189, 111281. [Google Scholar] [CrossRef] [PubMed]
- Lazare, S.S.; Wojtowicz, E.E.; Bystrykh, L.V.; De Haan, G. Micrornas in Hematopoiesis. Exp. Cell. Res. 2014, 329, 234–238. [Google Scholar] [CrossRef] [PubMed]
- Gerrits, A.; Walasek, M.A.; Olthof, S.; Weersing, E.; Ritsema, M.; Zwart, E.; Van Os, R.; Bystrykh, L.V.; de Haan, G. Genetic Screen Identifies Microrna Cluster 99b/Let-7e/125a as a Regulator of Primitive Hematopoietic Cells. Blood 2012, 119, 377–387. [Google Scholar] [CrossRef]
- Lechman, E.R.; Gentner, B.; van Galen, P.; Giustacchini, A.; Saini, M.; Boccalatte, F.E.; Hiramatsu, H.; Restuccia, U.; Bachi, A.; Voisin, V.; et al. Attenuation of Mir-126 Activity Expands Hsc in Vivo without Exhaustion. Cell. Stem. Cell. 2012, 11, 799–811. [Google Scholar] [CrossRef]
- Lechman, E.R.; Gentner, B.; Ng, S.W.; Schoof, E.M.; van Galen, P.; Kennedy, J.A.; Nucera, S.; Ciceri, F.; Kaufmann, K.B.; Takayama, N.; et al. Mir-126 Regulates Distinct Self-Renewal Outcomes in Normal and Malignant Hematopoietic Stem Cells. Cancer Cell 2016, 29, 214–228. [Google Scholar] [CrossRef]
- Starczynowski, D.T.; Kuchenbauer, F.; Argiropoulos, B.; Sung, S.; Morin, R.; Muranyi, A.; Hirst, M.; Hogge, D.; Marra, M.; Wells, R.A.; et al. Identification of Mir-145 and Mir-146a as Mediators of the 5q- Syndrome Phenotype. Nat. Med. 2010, 16, 49–58. [Google Scholar] [CrossRef]
- Guo, S.; Lu, J.; Schlanger, R.; Zhang, H.; Wang, J.Y.; Fox, M.C.; Purton, L.E.; Fleming, H.H.; Cobb, B.; Merkenschlager, M.; et al. Microrna Mir-125a Controls Hematopoietic Stem Cell Number. Proc. Natl. Acad. Sci. USA 2010, 107, 14229–14234. [Google Scholar] [CrossRef]
- Bowers, E.; Singer, K. Obesity-Induced Inflammation: The Impact of the Hematopoietic Stem Cell Niche. JCI Insight. 2021, 6, e145295. [Google Scholar] [CrossRef]
- Vinci, M.C.; Gambini, E.; Bassetti, B.; Genovese, S.; Pompilio, G. When Good Guys Turn Bad: Bone Marrow’s and Hematopoietic Stem Cells’ Role in the Pathobiology of Diabetic Complications. Int. J. Mol. Sci. 2020, 21, 3864. [Google Scholar] [CrossRef] [PubMed]
- Pospisil, V.; Vargova, K.S.; Kokavec, J.; Rybarova, J.; Savvulidi, F.G.; Jonasova, A.; Nečas, E.; Zavadil, J.; Laslo, P.; Stopka, T. Epigenetic Silencing of the Oncogenic Mir-17-92 Cluster During Pu.1-Directed Macrophage Differentiation. Embo. J. 2011, 30, 4450–4464. [Google Scholar] [CrossRef] [PubMed]
- Berg, S.M.; Seijkens, T.T.P.; Kusters, P.J.H.; Beckers, L.; Toom, M.; Smeets, E.; Levels, J.; Winther, M.P.J.; Lutgens, E. Diet-Induced Obesity in Mice Diminishes Hematopoietic Stem and Progenitor Cells in the Bone Marrow. Faseb. J. 2016, 30, 1779–1788. [Google Scholar] [CrossRef] [PubMed]
- Lee, J.-M.; Govindarajah, V.; Goddard, B.; Hinge, A.; Muench, D.E.; Filippi, M.-D.; Aronow, B.; Cancelas, J.A.; Salomonis, N.; Grimes, H.L.; et al. Obesity Alters the Long-Term Fitness of the Hematopoietic Stem Cell Compartment through Modulation of Gfi1 Expression. J. Exp. Med. 2018, 215, 627–644. [Google Scholar] [CrossRef] [PubMed]
- Wynn, T.A.; Chawla, A.; Pollard, J.W. Macrophage Biology in Development, Homeostasis and Disease. Nature 2013, 496, 445–455. [Google Scholar] [CrossRef]
- Caescu, C.I.; Guo, X.; Tesfa, L.; Bhagat, T.D.; Verma, A.; Zheng, D.; Stanley, E.R. Colony Stimulating Factor-1 Receptor Signaling Networks Inhibit Mouse Macrophage Inflammatory Responses by Induction of Microrna-21. Blood 2015, 125, e1–e13. [Google Scholar] [CrossRef]
- Lafontan, M. Fat Cells: Afferent and Efferent Messages Define New Approaches to Treat Obesity. Annu. Rev. Pharmacol. Toxicol. 2005, 45, 119–146. [Google Scholar] [CrossRef]
- Longo, M.; Zatterale, F.; Naderi, J.; Parrillo, L.; Formisano, P.; Raciti, G.A.; Beguinot, F.; Miele, C. Adipose Tissue Dysfunction as Determinant of Obesity-Associated Metabolic Complications. Int. J. Mol. Sci. 2019, 20, 2538. [Google Scholar] [CrossRef]
- Yan, X.; Huang, Y.; Zhao, J.-X.; Rogers, C.J.; Zhu, M.-J.; Ford, S.P.; Nathanielsz, P.W.; Du, M. Maternal Obesity Downregulates Microrna Let-7g Expression, a Possible Mechanism for Enhanced Adipogenesis During Ovine Fetal Skeletal Muscle Development. Int. J. Obes. 2013, 37, 568–575. [Google Scholar] [CrossRef]
- Yasmin, F.; Sahito, A.M.; Mir, S.L.; Khatri, G.; Shaikh, S.; Gul, A.; Hassan, S.A.; Koritala, T.; Surani, S. Electrical Neuromodulation Therapy for Inflammatory Bowel Disease. World J. Gastrointest Pathophysiol. 2022, 13, 128–142. [Google Scholar] [CrossRef]
- Wang, J.; Long, R.; Han, Y. The Role of Exosomes in the Tumour Microenvironment on Macrophage Polarisation. Biochim. Biophys Acta. Rev. Cancer. 2022, 1877, 188811. [Google Scholar] [CrossRef] [PubMed]
- Ghafouri-Fard, S.; Niazi, V.; Taheri, M. Role of Mirnas and Lncrnas in Hematopoietic Stem Cell Differentiation. Noncoding RNA Res. 2021, 6, 8–14. [Google Scholar] [CrossRef] [PubMed]
- Chu, A.J.; Williams, J.M. Astrocytic Microrna in Ageing, Inflammation, and Neurodegenerative Disease. Front. Physiol. 2021, 12, 826697. [Google Scholar] [CrossRef] [PubMed]
- Liu, S.; Ren, C.; Qu, X.; Wu, X.; Dong, F.; Chand, Y.K.; Fan, H.; Yao, R.; Geng, D. Mir-219 Attenuates Demyelination in Cuprizone-Induced Demyelinated Mice by Regulating Monocarboxylate Transporter 1. Eur. J. Neurosci. 2017, 45, 249–259. [Google Scholar] [CrossRef] [PubMed]
- Krug, A.; Wöhr, M.; Seffer, D.; Rippberger, H.; Sungur, A.; Dietsche, B.; Stein, F.; Sivalingam, S.; Forstner, A.J.; Witt, S.H.; et al. Advanced Paternal Age as a Risk Factor for Neurodevelopmental Disorders: A Translational Study. Mol. Autism. 2020, 11, 54. [Google Scholar] [CrossRef]
- Rodriguez-Gomez, A.; Filice, F.; Gotti, S.; Panzica, G. Perinatal Exposure to Genistein Affects the Normal Development of Anxiety and Aggressive Behaviors and Nitric Oxide System in Cd1 Male Mice. Physiol. Behav. 2014, 133, 107–114. [Google Scholar] [CrossRef]
- Marraudino, M.; Ponti, G.; Moussu, C.; Farinetti, A.; Macchi, E.; Accornero, P.; Gotti, S.; Collado, P.; Keller, M.; Panzica, G. Early Postnatal Genistein Administration Affects Mice Metabolism and Reproduction in a Sexually Dimorphic Way. Metabolites 2021, 11, 449. [Google Scholar] [CrossRef]
- Zhou, P.; Wu, S.; Huang, D.; Wang, K.; Su, X.; Yang, R.; Shao, C.; Wu, J. Oral Exposure to Dehp May Stimulate Prostatic Hyperplasia Associated with Upregulation of Cox-2 and L-Pgds Expressions in Male Adult Rats. Reprod. Toxicol. 2022, 112, 160–170. [Google Scholar] [CrossRef]
- Singh, V.; Cortes-Ramirez, J.; Toms, L.M.; Sooriyagoda, T.; Karatela, S. Effects of Polybrominated Diphenyl Ethers on Hormonal and Reproductive Health in E-Waste-Exposed Population: A Systematic Review. Int. J. Environ. Res. Public Health 2022, 19, 7820. [Google Scholar] [CrossRef]
- Chen, S.-D.; Sun, X.-Y.; Niu, W.; Kong, L.-M.; He, M.-J.; Fan, H.-M.; Li, W.-S.; Zhong, A.-F.; Zhang, L.-Y.; Lu, J. Correlation between the Level of Microrna Expression in Peripheral Blood Mononuclear Cells and Symptomatology in Patients with Generalized Anxiety Disorder. Compr. Psychiatry 2016, 69, 216–224. [Google Scholar] [CrossRef]
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).