Hemodialysis and Plasma Oxylipin Biotransformation in Peripheral Tissue
Abstract
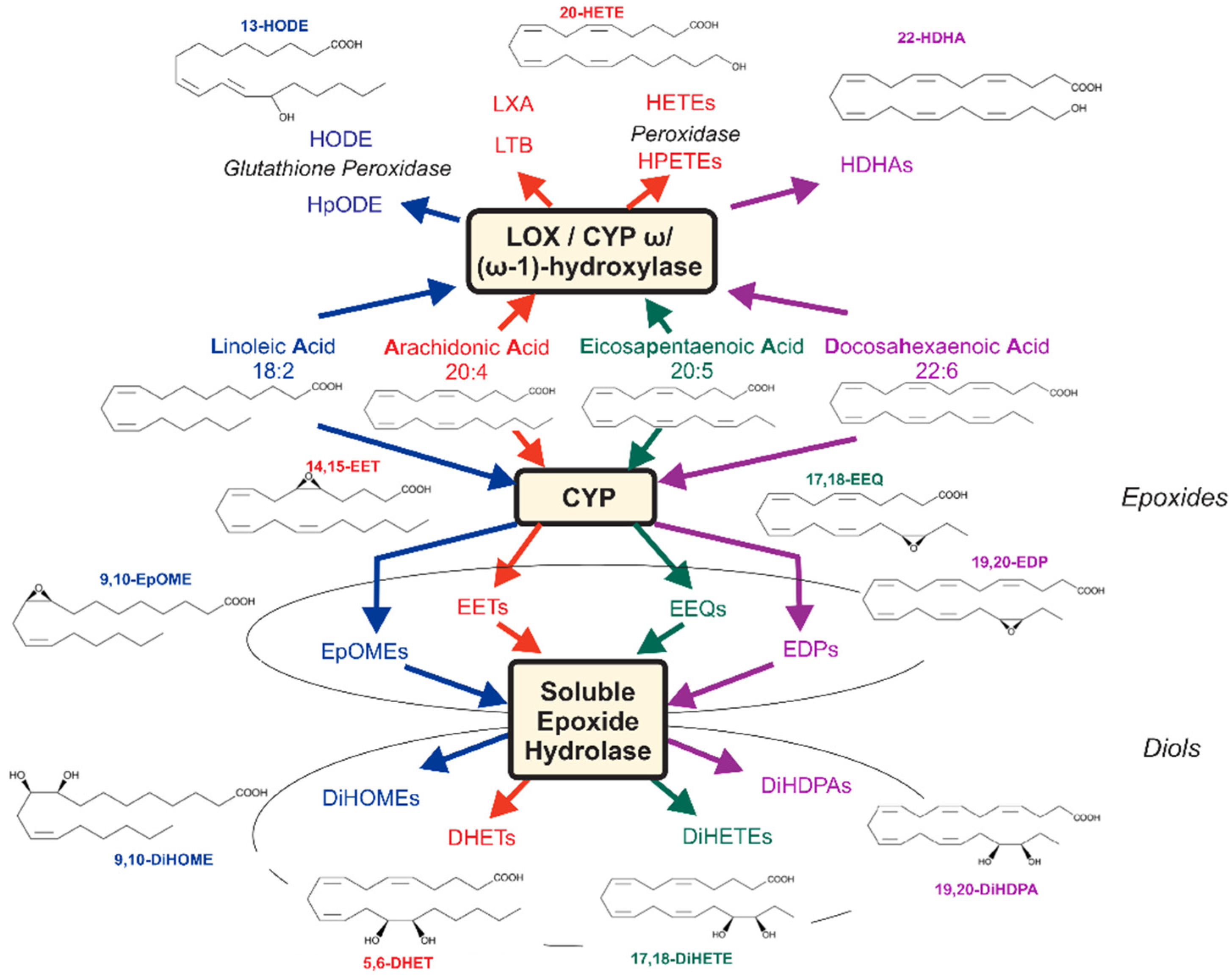
1. Introduction
2. Results
2.1. Clinical Characteristics
2.2. Effects of Hemodialysis
2.2.1. Pre-HD
2.2.2. Post-HD
2.3. Diol/Epoxide Ratios and sEH Activity
3. Discussion
4. Materials and Methods
4.1. Participants
4.2. Assessment
4.3. Determination of Eicosanoid Profiles
4.4. Statistical Analysis
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- McGill, R.L.; Bragg-Gresham, J.L.; He, K.; Lacson, E.K., Jr.; Miskulin, D.C.; Saran, R. Chronic disease burdens of incident U.S. dialysis patients, 1996–2015. Clin. Nephrol. 2020, 93, 1. [Google Scholar] [CrossRef]
- Luft, F.C. Renal disease as a risk factor for cardiovascular disease. Basic Res. Cardiol. 2000, 95, I72–I76. [Google Scholar] [CrossRef]
- Zullig, T.; Trotzmuller, M.; Kofeler, H.C. Lipidomics from sample preparation to data analysis: A primer. Anal. Bioanal. Chem. 2020, 412, 2191–2209. [Google Scholar] [CrossRef]
- Gollasch, B.; Wu, G.; Dogan, I.; Rothe, M.; Gollasch, M.; Luft, F.C. Effects of hemodialysis on plasma oxylipins. Physiol. Rep. 2020, 8, e14447. [Google Scholar] [CrossRef]
- Spector, A.A.; Kim, H.Y. Cytochrome P450 epoxygenase pathway of polyunsaturated fatty acid metabolism. Biochim. Biophys. Acta 2015, 1851, 356–365. [Google Scholar] [CrossRef] [PubMed]
- Arnold, C.; Markovic, M.; Blossey, K.; Wallukat, G.; Fischer, R.; Dechend, R.; Konkel, A.; von Schacky, C.; Luft, F.C.; Muller, D.N.; et al. Arachidonic acid-metabolizing cytochrome P450 enzymes are targets of ω-3 fatty acids. J. Biol. Chem. 2010, 285, 32720–32733. [Google Scholar] [CrossRef] [PubMed]
- Harris, T.R.; Hammock, B.D. Soluble epoxide hydrolase: Gene structure, expression and deletion. Gene 2013, 526, 61–74. [Google Scholar] [CrossRef] [PubMed]
- Spector, A.A.; Fang, X.; Snyder, G.D.; Weintraub, N.L. Epoxyeicosatrienoic acids (EETs): Metabolism and biochemical function. Prog. Lipid Res. 2004, 43, 55–90. [Google Scholar] [CrossRef]
- Gangadhariah, M.H.; Dieckmann, B.W.; Lantier, L.; Kang, L.; Wasserman, D.H.; Chiusa, M.; Caskey, C.F.; Dickerson, J.; Luo, P.; Gamboa, J.L.; et al. Cytochrome P450 epoxygenase-derived epoxyeicosatrienoic acids contribute to insulin sensitivity in mice and in humans. Diabetologia 2017, 60, 1066–1075. [Google Scholar] [CrossRef]
- Gollasch, B.; Wu, G.; Dogan, I.; Rothe, M.; Gollasch, M.; Luft, F.C. Maximal exercise and erythrocyte epoxy fatty acids: A lipidomics study. Physiol. Rep. 2019, 7, e14275. [Google Scholar] [CrossRef]
- Gollasch, B.; Dogan, I.; Rothe, M.; Gollasch, M.; Luft, F.C. Maximal exercise and plasma cytochrome P450 and lipoxygenase mediators: A lipidomics study. Physiol. Rep. 2019, 7, e14165. [Google Scholar] [CrossRef]
- Agroyannis, B.; Tzanatos, H.; Fourtounas, C.; Kopelias, I.; Katsoudas, S.; Chondros, K. Arteriovenous difference of blood ammonia in uremic patients under hemodialysis. Artif. Organs 1998, 22, 703–705. [Google Scholar] [CrossRef]
- Glassberg, B.Y. The arteriovenous difference on blood sugar content. Arch. Intern. Med. 1930, 46, 605–609. [Google Scholar] [CrossRef]
- Konttinen, A.; Sarajas, H.S.; Frick, M.H.; Rajasalmi, M. Arteriovenous relationship of non-esterified fatty acids, triglycerides, cholesterol and phospholipids in exercise. Ann. Med. Exp. Biol. Fenn. 1962, 40, 250–256. [Google Scholar]
- Ishibashi, T.; Nishizawa, N.; Nomura, M.; Liu, S.; Yang, M.; Miwa, T.; Shinkawa, I.; Yoshida, J.; Kawada, T.; Nishio, M. Arteriovenous differences in NO2− kinetics in anesthetized rabbits. Biol. Pharm. Bull. 2009, 32, 399–404. [Google Scholar] [CrossRef][Green Version]
- Zhang, K.; Liu, Y.; Liu, X.; Chen, J.; Cai, Q.; Wang, J.; Huang, H. Apocynin improving cardiac remodeling in chronic renal failure disease is associated with up-regulation of epoxyeicosatrienoic acids. Oncotarget 2015, 6, 24699–24708. [Google Scholar] [CrossRef] [PubMed]
- Capdevila, J.H.; Falck, J.R.; Harris, R.C. Cytochrome P450 and arachidonic acid bioactivation. Molecular and functional properties of the arachidonate monooxygenase. J. Lipid Res. 2000, 41, 163–181. [Google Scholar] [CrossRef]
- Spector, A.A.; Norris, A.W. Action of epoxyeicosatrienoic acids on cellular function. Am. J. Physiol. Cell Physiol. 2007, 292, C996–C1012. [Google Scholar] [CrossRef]
- Schunck, W.H.; Konkel, A.; Fischer, R.; Weylandt, K.H. Therapeutic potential of omega-3 fatty acid-derived epoxyeicosanoids in cardiovascular and inflammatory diseases. Pharmacol. Ther. 2018, 183, 177–204. [Google Scholar] [CrossRef] [PubMed]
- Jiang, H.; Quilley, J.; Doumad, A.B.; Zhu, A.G.; Falck, J.R.; Hammock, B.D.; Stier, C.T., Jr.; Carroll, M.A. Increases in plasma trans-EETs and blood pressure reduction in spontaneously hypertensive rats. Am. J. Physiol. Heart Circ. Physiol. 2011, 300, H1990–H1996. [Google Scholar] [CrossRef]
- Jiang, H.; Anderson, G.D.; McGiff, J.C. Red blood cells (RBCs), epoxyeicosatrienoic acids (EETs) and adenosine triphosphate (ATP). Pharmacol. Rep. 2010, 62, 468–474. [Google Scholar] [CrossRef]
- Jiang, H.; Anderson, G.D.; McGiff, J.C. The red blood cell participates in regulation of the circulation by producing and releasing epoxyeicosatrienoic acids. Prostaglandins Other Lipid Mediat. 2012, 98, 91–93. [Google Scholar] [CrossRef]
- Morisseau, C.; Kodani, S.D.; Kamita, S.G.; Yang, J.; Lee, K.S.S.; Hammock, B.D. Relative Importance of Soluble and Microsomal Epoxide Hydrolases for the Hydrolysis of Epoxy-Fatty Acids in Human Tissues. Int. J. Mol. Sci. 2021, 22, 4993. [Google Scholar] [CrossRef]
- Node, K.; Huo, Y.; Ruan, X.; Yang, B.; Spiecker, M.; Ley, K.; Zeldin, D.C.; Liao, J.K. Anti-inflammatory properties of cytochrome P450 epoxygenase-derived eicosanoids. Science 1999, 285, 1276–1279. [Google Scholar] [CrossRef] [PubMed]
- Hercule, H.C.; Schunck, W.H.; Gross, V.; Seringer, J.; Leung, F.P.; Weldon, S.M.; Goncalves, A.C.d.C.; Huang, Y.; Luft, F.C.; Gollasch, M. Interaction between P450 eicosanoids and nitric oxide in the control of arterial tone in mice. Arterioscler. Thromb. Vasc. Biol. 2009, 29, 54–60. [Google Scholar] [CrossRef] [PubMed]
- Lu, T.; Katakam, P.V.; VanRollins, M.; Weintraub, N.L.; Spector, A.A.; Lee, H.C. Dihydroxyeicosatrienoic acids are potent activators of Ca2+-activated K+ channels in isolated rat coronary arterial myocytes. J. Physiol. 2001, 534 Pt 3, 651–667. [Google Scholar] [CrossRef] [PubMed]
- Gao, Y.; Feng, J.; Ma, K.; Zhou, Z.; Zhu, Y.; Xu, Q.; Wang, X. 8,9-Epoxyeicosatrienoic acid inhibits antibody production of B lymphocytes in mice. PLoS ONE 2012, 7, e40258. [Google Scholar]
- Osthues, T.; Sisignano, M. Oxidized Lipids in Persistent Pain States. Front. Pharmacol. 2019, 10, 1147. [Google Scholar] [CrossRef]
- Strielkov, I.; Krause, N.C.; Knoepp, F.; Alebrahimdehkordi, N.; Pak, O.; Garcia, C.; Ghofrani, H.A.; Schermuly, R.T.; Seeger, W.; Grimminger, F.; et al. Cytochrome P450 epoxygenase-derived 5,6-epoxyeicosatrienoic acid relaxes pulmonary arteries in normoxia but promotes sustained pulmonary vasoconstriction in hypoxia. Acta Physiol. 2020, 230, e13521. [Google Scholar] [CrossRef]
- Campbell, W.B.; Fleming, I. Epoxyeicosatrienoic acids and endothelium-dependent responses. Pflug. Arch. Eur. J. Physiol. 2010, 459, 881–895. [Google Scholar] [CrossRef]
- Gschwendtner, A.; Ripke, S.; Freilinger, T.; Lichtner, P.; Müller-Myhsok, B.; Wichmann, H.E.; Meitinger, T.; Dichgans, M. Genetic variation in soluble epoxide hydrolase (EPHX2) is associated with an increased risk of ischemic stroke in white Europeans. Stroke J. Cereb. Circ. 2008, 39, 1593–1596. [Google Scholar] [CrossRef] [PubMed]
- Wutzler, A.; Kestler, C.; Perrot, A.; Loehr, L.; Huemer, M.; Parwani, A.S.; Attanasio, P.; Özcelik, C.; Schunck, W.-H.; Gollasch, M.; et al. Variations in the human soluble epoxide hydrolase gene and recurrence of atrial fibrillation after catheter ablation. Int. J. Cardiol. 2013, 168, 3647–3651. [Google Scholar] [CrossRef]
- Hutchens, M.P.; Nakano, T.; Dunlap, J.; Traystman, R.J.; Hurn, P.D.; Alkayed, N.J. Soluble epoxide hydrolase gene deletion reduces survival after cardiac arrest and cardiopulmonary resuscitation. Resuscitation 2008, 76, 89–94. [Google Scholar] [CrossRef] [PubMed]
- Morin, C.; Fortin, S.; Rousseau, E. 19,20-EpDPE, a bioactive CYP450 metabolite of DHA monoacyglyceride, decreases Ca2+ sensitivity in human pulmonary arteries. Am. J. Physiol. Heart Circ. Physiol. 2011, 301, H1311–H1318. [Google Scholar] [CrossRef] [PubMed]
- Darwesh, A.M.; Jamieson, K.L.; Wang, C.; Samokhvalov, V.; Seubert, J.M. Cardioprotective effects of CYP-derived epoxy metabolites of docosahexaenoic acid involve limiting NLRP3 inflammasome activation. Can. J. Physiol. Pharmacol. 2019, 97, 544–556. [Google Scholar] [CrossRef]
- Liu, Y.; Fang, X.; Zhang, X.; Huang, J.; He, J.; Peng, L.; Ye, C.; Wang, Y.; Xue, F.; Ai, D.; et al. Metabolic profiling of murine plasma reveals eicosapentaenoic acid metabolites protecting against endothelial activation and atherosclerosis. Br. J. Pharmacol. 2018, 175, 1190–1204. [Google Scholar] [CrossRef]
- Samokhvalov, V.; Jamieson, K.L.; Vriend, J.; Quan, S.; Seubert, J.M. CYP epoxygenase metabolites of docosahexaenoic acid protect HL-1 cardiac cells against LPS-induced cytotoxicity through SIRT1. Cell Death Discov. 2015, 97, 544–556. [Google Scholar] [CrossRef]
- Lauterbach, B.; Barbosa-Sicard, E.; Wang, M.H.; Honeck, H.; Kärgel, E.; Theuer, J.; Schwartzman, M.L.; Haller, H.; Luft, F.; Gollasch, M.; et al. Cytochrome P450-dependent eicosapentaenoic acid metabolites are novel BK channel activators. Hypertension 2002, 39 Pt 2, 609–613. [Google Scholar] [CrossRef]
- Hercule, H.C.; Salanova, B.; Essin, K.; Honeck, H.; Falck, J.R.; Sausbier, M.; Ruth, P.; Schunck, W.-H.; Luft, F.C.; Gollasch, M. The vasodilator 17,18-epoxyeicosatetraenoic acid targets the pore-forming BK alpha channel subunit in rodents. Exp. Physiol. 2007, 92, 1067–1076. [Google Scholar] [CrossRef]
- Siegfried, M.R.; Aoki, N.; Lefer, A.M.; Elisseou, E.M.; Zipkin, R.E. Direct cardiovascular actions of two metabolites of linoleic acid. Life Sci. 1990, 46, 427–433. [Google Scholar] [CrossRef]
- Fukushima, A.; Hayakawa, M.; Sugiyama, S.; Ajioka, M.; Ito, T.; Satake, T.; Ozawa, T. Cardiovascular effects of leukotoxin (9,10-epoxy-12-octadecenoate) and free fatty acids in dogs. Cardiovasc. Res. 1988, 22, 213–218. [Google Scholar] [CrossRef]
- Sugiyama, S.; Hayakawa, M.; Nagai, S.; Ajioka, M.; Ozawa, T. Leukotoxin, 9,10-epoxy-12-octadecenoate, causes cardiac failure in dogs. Life Sci. 1987, 40, 225–231. [Google Scholar] [CrossRef]
- Okamura, S.; Ameshima, S.; Demura, Y.; Ishizaki, T.; Matsukawa, S.; Miyamori, I. Leukotoxin-activated human pulmonary artery endothelial cell produces nitric oxide and superoxide anion. Pulm. Pharmacol. Ther. 2002, 15, 25–33. [Google Scholar] [CrossRef] [PubMed]
- Dudda, A.; Spiteller, G.; Kobelt, F. Lipid oxidation products in ischemic porcine heart tissue. Chem. Phys. Lipids 1996, 82, 39–51. [Google Scholar] [CrossRef]
- Fischer, R.; Konkel, A.; Mehling, H.; Blossey, K.; Gapelyuk, A.; Wessel, N.; von Schacky, C.; Dechend, R.; Muller, D.N.; Rothe, M.; et al. Dietary omega-3 fatty acids modulate the eicosanoid profile in man primarily via the CYP-epoxygenase pathway. J. Lipid Res. 2014, 55, 1150–1164. [Google Scholar] [CrossRef] [PubMed]

| HD Patients | |
|---|---|
| Age (years) | 72 ± 12 |
| Sex | |
| Male (n) | 9 |
| Female (n) | 3 |
| Body mass index (kg/m2) | 27 ± 3 |
| Race (n) | Caucasian = 12 |
| Cause of end-stage renal disease | |
| Focal segmental glomerulosclerosis (n) | 6 |
| IgA nephropathy (n) | 1 |
| Renal amyloidosis (n) | 1 |
| Hypertension (n) | 1 |
| Drug induced (n) | 1 |
| ADPKD (n) | 1 |
| Cystic kidneys (n) | 1 |
| Complications | |
| Cardiovascular (n) | 12 |
| Amount ng/mL | Pre-HD A (Mean ± SD) | Pre-HD V (Mean ± SD) | p-Value, t-Test (# Paired Wilcoxon Test) | Pre-HD A-V Difference (Mean ± SD) | Post-HD A (Mean ± SD) | Post-HD V (Mean ± SD) | p-Value, t-Test (# Paired Wilcoxon Test) | Post-HD A-V Difference (Mean ± SD) |
|---|---|---|---|---|---|---|---|---|
| CYP epoxy-metabolites | ||||||||
| 5,6-EET | 25.2403 ± 22.8032 | 16.8013 ± 15.3681 | 0.325 | 8.1596 ± 22.0848 | 37.0725 ± 16.6846 | 61.8386 ± 21.0905 | 0.003 # | −24.7661 ± 17.4189 |
| 8,9-EET | 10.5227 ± 10.8994 | 7.2706 ± 6.6772 | 0.806 | 3.1316 ± 11.4525 | 13.3085 ± 5.6504 | 22.3969 ± 7.8620 | 0.002 # | −9.0884 ± 6.7881 |
| 11,12-EET | 9.9539 ± 10.0802 | 7.0358 ± 6.8420 | 0.806 | 2.7042 ± 10.2183 | 14.2304 ± 6.6762 | 25.6937 ± 9.1845 | 0.002 # | −11.4633 ± 7.4968 |
| 14,15-EET | 12.5615 ± 12.5408 | 9.6655 ± 9.4944 | 0.538 | 2.6286 ± 12.4557 | 19.0872 ± 9.2999 | 35.6871 ± 13.5842 | 0.002 # | −16.6000 ± 10.9006 |
| 5,6-DHET | 1.1450 ± 0.5549 | 1.0727 ± 0.5911 | 0.389 | 0.1175 ± 0.1770 | 1.3684 ± 0.5945 | 1.2782 ± 0.6163 | 0.177 # | 0.0901 ± 0.2165 |
| 8,9-DHET | 1.7434 ± 1.5788 | 1.6063 ± 1.3596 | 0.806 | 0.1581 ± 0.4252 | 1.6086 ± 1.1218 | 1.2535 ± 0.9769 | 0.004 # | 0.3550 ± 0.3980 |
| 11,12-DHET | 0.4366 ± 0.2207 | 0.4188 ± 0.1959 | 0.902 | 0.0311 ± 0.0878 | 0.5221 ± 0.1967 | 0.4683 ± 0.1888 | 0.005 | 0.0538 ± 0.0534 |
| 14,15-DHET | 0.4159 ± 0.0996 | 0.3721 ± 0.0788 | 0.252 | 0.0480 ± 0.0902 | 0.4919 ± 0.1251 | 0.4212 ± 0.1045 | 0.132 | 0.0708 ± 0.1505 |
| 7,8-EDP | 4.5236 ± 4.3719 | 3.2930 ± 3.1818 | 0.951 | 1.1887 ± 4.7923 | 6.0064 ± 2.6897 | 10.4413 ± 3.5636 | 0.002 # | −4.4349 ± 2.2351 |
| 10,11-EDP | 4.4784 ± 4.4009 | 3.3370 ± 3.0863 | 0.806 | 1.0517 ± 4.5614 | 6.6357 ± 3.0803 | 11.9332 ± 3.9274 | <0.001 | −5.2975 ± 2.5243 |
| 13,14-EDP | 3.3860 ± 3.4990 | 2.6621 ± 2.8208 | 0.806 | 0.6491 ± 3.6773 | 4.8226 ± 2.2061 | 7.8177 ± 2.6177 | <0.001 | −2.9952 ± 1.9444 |
| 16,17-EDP | 2.9692 ± 2.8814 | 2.1926 ± 2.0367 | 0.806 | 0.7541 ± 2.8457 | 3.8342 ± 1.6915 | 5.5352 ± 2.0151 | 0.008 | −1.7010 ± 1.8424 |
| 19,20-EDP | 5.5558 ± 5.3859 | 3.9685 ± 3.1487 | 1 | 1.4739 ± 5.6060 | 8.6761 ± 3.8647 | 16.3124 ± 6.2669 | 0.002 # | −7.6363 ± 3.7823 |
| 7,8-DiHDPA | 0.4489 ± 0.2473 | 0.4110 ± 0.2301 | 0.498 | 0.0405 ± 0.0429 | 0.4905 ± 0.2287 | 0.4461 ± 0.2152 | 0.021 | 0.0444 ± 0.0571 |
| 10,11-DiHDPA | 0.1277 ± 0.0387 | 0.1210 ± 0.0346 | 0.664 | 0.0081 ± 0.0169 | 0.1439 ± 0.0452 | 0.1291 ± 0.0539 | 0.031 | 0.0148 ± 0.0207 |
| 13,14-DiHDPA | 0.0892 ± 0.0274 | 0.0846 ± 0.0203 | 0.65 | 0.0051 ± 0.0114 | 0.0989 ± 0.0354 | 0.1040 ± 0.0439 | 0.55 | −0.0051 ± 0.0285 |
| 16,17-DiHDPA | 0.0926 ± 0.0361 | 0.0947 ± 0.0314 | 0.886 | −0.0012 ± 0.0111 | 0.1160 ± 0.0464 | 0.1042 ± 0.0480 | 0.168 | 0.0118 ± 0.0277 |
| 19,20-DiHDPA | 0.8379 ± 0.4051 | 0.8262 ± 0.3658 | 0.943 | 0.0383 ± 0.0710 | 0.9534 ± 0.4118 | 0.9134 ± 0.4345 | 0.393 | 0.0400 ± 0.1559 |
| 5,6-EEQ | 0.0051 ± 0.0039 | 0.0034 ± 0.0026 | 0.23 | −0.0064 ± 0.0048 | 0.0084 ± 0.0052 | 0.0148 ± 0.0050 | 0.004 # | 0.0012 ± 0.0042 |
| 8,9-EEQ | 1.4478 ± 1.2289 | 0.9972 ± 0.6972 | 0.498 | 0.4347 ± 1.3829 | 2.6063 ± 1.7732 | 4.3902 ± 1.5836 | 0.008 # | −1.7839 ± 1.6485 |
| 11,12-EEQ | 0.9541 ± 0.8310 | 0.7197 ± 0.4820 | 0.806 | 0.2294 ± 0.9263 | 1.8077 ± 1.2340 | 3.4951 ± 1.3735 | 0.003 # | −1.6874 ± 1.1790 |
| 14,15-EEQ | 0.9436 ± 0.7146 | 0.7047 ± 0.4467 | 0.343 # | 0.2231 ± 0.8184 | 1.7544 ± 1.2152 | 3.2728 ± 1.3192 | 0.004 # | −1.5184 ± 1.2985 |
| 17,18-EEQ | 1.6849 ± 1.3879 | 1.3915 ± 0.8490 | 0.543 # | 0.2583 ± 1.4915 | 2.9621 ± 2.1045 | 6.2605 ± 2.2755 | 0.002 # | −3.2984 ± 2.0268 |
| 5,6-DiHETE | 1.5299 ± 0.9299 | 1.3695 ± 0.7134 | 0.622 # | 0.3200 ± 0.8708 | 2.0357 ± 1.4971 | 1.6895 ± 0.8335 | 0.53 # | 0.3461 ± 1.2824 |
| 8,9-DiHETE | 0.0908 ± 0.0378 | 0.0908 ± 0.0317 | 0.667 # | 0.0061 ± 0.0374 | 0.1085 ± 0.0552 | 0.0960 ± 0.0386 | 0.36 | 0.0125 ± 0.0455 |
| 11,12-DiHETE | 0.0476 ± 0.0379 | 0.0356 ± 0.0100 | 0.806 | 0.0128 ± 0.0418 | 0.0596 ± 0.0600 | 0.0372 ± 0.0119 | 0.099 # | 0.0224 ± 0.0633 |
| 14,15-DiHETE | 0.0528 ± 0.0201 | 0.0462 ± 0.0135 | 0.364 # | 0.0075 ± 0.0205 | 0.0538 ± 0.0249 | 0.0487 ± 0.0203 | 0.49 | 0.0051 ± 0.0248 |
| 17,18-DiHETE | 0.2149 ± 0.0825 | 0.2141 ± 0.0836 | 0.981 # | 0.0030 ± 0.0659 | 0.2784 ± 0.1176 | 0.2454 ± 0.1082 | 0.253 | 0.0330 ± 0.0948 |
| 9,10-EpOME | 33.0227 ± 31.0831 | 22.5987 ± 12.9602 | 0.806 | 9.9686 ± 32.0264 | 51.7226 ± 18.8433 | 93.5874 ± 36.4954 | 0.002 # | −41.8648 ± 26.9869 |
| 12,13-EpOME | 30.9825 ± 26.7698 | 20.7024 ± 11.0768 | 0.46 | 9.7907 ± 27.7448 | 46.9109 ± 15.0402 | 79.7224 ± 23.6841 | <0.001 | −32.8115 ± 15.3972 |
| 9,10-DiHOME | 4.1455 ± 1.7899 | 3.2993 ± 1.7108 | 0.085 | 0.7458 ± 0.9866 | 5.5991 ± 2.7877 | 5.6467 ± 2.4652 | 0.954 # | −0.0476 ± 2.7904 |
| 12,13-DiHOME | 4.9809 ± 1.9437 | 3.8968 ± 1.6289 | 0.161 # | 0.9906 ± 1.6559 | 6.9594 ± 3.7873 | 6.9340 ± 3.3774 | 0.875 # | 0.0254 ± 2.8341 |
| LOX metabolites | ||||||||
| 5-HETE | 10.1945 ± 2.9568 | 8.9008 ± 2.5521 | 0.273 # | 1.3211 ± 1.9205 | 11.6499 ± 3.0694 | 11.2376 ± 3.5321 | 0.53 # | 0.4123 ± 3.1451 |
| 8-HETE | 3.1627 ± 0.8646 | 2.9701 ± 0.9371 | 0.46 # | 0.1954 ± 0.4666 | 3.5068 ± 1.3221 | 2.9656 ± 1.1078 | 0.185 | 0.5413 ± 1.3245 |
| 9-HETE | 6.2378 ± 2.4916 | 5.0812 ± 2.0444 | 0.235 # | 1.1362 ± 1.8189 | 6.6115 ± 2.5626 | 5.7522 ± 2.1829 | 0.209 # | 0.8593 ± 2.1644 |
| 11-HETE | 4.3689 ± 1.3795 | 3.4094 ± 1.1668 | 0.027 | 0.9124 ± 0.8519 | 4.5454 ± 1.4621 | 4.0433 ± 1.4575 | 0.071 # | 0.5021 ± 1.5746 |
| 12-HETE | 5.1343 ± 1.7200 | 5.8545 ± 2.6463 | 0.452 # | −0.7233 ± 1.8003 | 6.0063 ± 2.3467 | 4.7972 ± 2.3597 | 0.023 # | 1.2091 ± 1.8582 |
| 15-HETE | 6.1984 ± 1.9171 | 4.9051 ± 1.5388 | 0.085 | 1.2806 ± 1.1112 | 6.1869 ± 1.8919 | 5.7417 ± 3.2394 | 0.06 # | 0.4452 ± 2.9529 |
| 4-HDHA | 2.3149 ± 0.6472 | 2.1630 ± 0.5977 | 0.565 # | 0.1653 ± 0.5413 | 2.4431 ± 0.9794 | 2.5609 ± 1.2943 | 0.875 # | −0.1178 ± 0.8863 |
| 7-HDHA | 2.1060 ± 0.6072 | 1.7319 ± 0.5209 | 0.11 | 0.3892 ± 0.4553 | 2.1783 ± 0.8143 | 2.0061 ± 0.6765 | 0.259 | 0.1722 ± 0.5011 |
| 8-HDHA | 1.2263 ± 0.4487 | 1.0900 ± 0.3821 | 0.44 | 0.1357 ± 0.1780 | 1.2990 ± 0.5943 | 1.1141 ± 0.4935 | 0.182 # | 0.1849 ± 0.5362 |
| 10-HDHA | 0.7721 ± 0.2512 | 0.6877 ± 0.2059 | 0.387 | 0.0793 ± 0.0990 | 0.7940 ± 0.3187 | 0.7020 ± 0.2701 | 0.196 | 0.0920 ± 0.2312 |
| 11-HDHA | 1.0995 ± 0.3769 | 1.0493 ± 0.3586 | 0.902 | 0.0545 ± 0.2055 | 1.0862 ± 0.4291 | 1.0103 ± 0.3687 | 0.136 # | 0.0758 ± 0.4079 |
| 13-HDHA | 0.9168 ± 0.2861 | 0.8168 ± 0.2303 | 0.364 | 0.0963 ± 0.1441 | 0.9169 ± 0.3765 | 0.8015 ± 0.3238 | 0.259 # | 0.1154 ± 0.3361 |
| 14-HDHA | 1.1312 ± 0.4384 | 1.0678 ± 0.4203 | 0.727 | 0.0541 ± 0.2125 | 1.1712 ± 0.5441 | 0.9981 ± 0.5062 | 0.084 # | 0.1732 ± 0.3398 |
| 16-HDHA | 1.1430 ± 0.3468 | 0.9559 ± 0.3037 | 0.182 | 0.1782 ± 0.1994 | 1.1459 ± 0.4227 | 1.0653 ± 0.4675 | 0.117 # | 0.0806 ± 0.4293 |
| 17-HDHA | 1.4069 ± 0.4032 | 1.1633 ± 0.3601 | 0.141 | 0.2414 ± 0.2051 | 1.4601 ± 0.5780 | 1.2773 ± 0.5100 | 0.041 # | 0.1828 ± 0.5168 |
| 20-HDHA | 2.8698 ± 0.7707 | 2.4726 ± 0.7079 | 0.212 # | 0.3802 ± 0.4872 | 2.9700 ± 0.9600 | 2.7939 ± 1.1603 | 0.084 # | 0.1761 ± 0.9553 |
| 5-HEPE | 1.4608 ± 0.5576 | 1.3111 ± 0.4406 | 0.481 | 0.1804 ± 0.3543 | 1.5968 ± 0.9534 | 1.4799 ± 0.6337 | 0.875 # | 0.1170 ± 0.8054 |
| 8-HEPE | 0.2118 ± 0.0669 | 0.1959 ± 0.0421 | 0.712 | 0.0193 ± 0.0428 | 0.2061 ± 0.1012 | 0.1817 ± 0.0752 | 0.329 # | 0.0244 ± 0.0829 |
| 9-HEPE | 0.4018 ± 0.1460 | 0.3661 ± 0.1209 | 0.528 | 0.0400 ± 0.1177 | 0.3664 ± 0.2280 | 0.3335 ± 0.1318 | 0.875 # | 0.0329 ± 0.1871 |
| 11-HEPE | 0.2752 ± 0.0907 | 0.2520 ± 0.0448 | 0.538 | 0.0217 ± 0.0697 | 0.2531 ± 0.1150 | 0.2364 ± 0.0928 | 0.388 # | 0.0167 ± 0.1077 |
| 12-HEPE | 0.5039 ± 0.1762 | 0.5213 ± 0.1704 | 0.812 | −0.0162 ± 0.1369 | 0.4619 ± 0.2576 | 0.4038 ± 0.1731 | 0.638 # | 0.0580 ± 0.2070 |
| 15-HEPE | 0.3150 ± 0.1086 | 0.3142 ± 0.0634 | 0.983 | 0.0029 ± 0.0850 | 0.2890 ± 0.1524 | 0.2596 ± 0.1144 | 0.433 # | 0.0294 ± 0.1342 |
| 18-HEPE | 0.8580 ± 0.2946 | 0.8418 ± 0.2239 | 0.883 # | 0.0156 ± 0.2704 | 0.7714 ± 0.3717 | 0.7502 ± 0.4476 | 0.53 # | 0.0212 ± 0.3909 |
| 9-HODE | 22.0631 ± 7.3185 | 17.1239 ± 6.0628 | 0.091 # | 4.7896 ± 3.9253 | 36.2855 ± 21.5709 | 34.0942 ± 21.6186 | 0.071 # | 2.1913 ± 11.7721 |
| 13-HODE | 17.7783 ± 6.0021 | 13.5081 ± 4.2496 | 0.012 | 4.0845 ± 3.1626 | 25.0606 ± 10.8578 | 25.1650 ± 13.2212 | 0.48 # | −0.1044 ± 8.7534 |
| CYP ω/(ω−1) metabolites | ||||||||
| 16-HETE | 0.2346 ± 0.0507 | 0.2175 ± 0.0583 | 0.462 # | 0.0186 ± 0.0590 | 0.2194 ± 0.0562 | 0.2184 ± 0.0828 | 0.875 # | 0.0010 ± 0.0660 |
| 17-HETE | 0.0565 ± 0.0112 | 0.0560 ± 0.0145 | 0.922 # | 0.0010 ± 0.0109 | 0.0602 ± 0.0182 | 0.0517 ± 0.0147 | 0.071 # | 0.0085 ± 0.0161 |
| 18-HETE | 0.1620 ± 0.0463 | 0.1499 ± 0.0282 | 0.538 # | 0.0154 ± 0.0455 | 0.1651 ± 0.0450 | 0.1493 ± 0.0421 | 0.272 # | 0.0158 ± 0.0416 |
| 19-HETE | 0.1441 ± 0.0810 | 0.1354 ± 0.0411 | 0.854 | 0.0133 ± 0.0689 | 0.1599 ± 0.0533 | 0.1662 ± 0.0571 | 0.693 | −0.0064 ± 0.0546 |
| 20-HETE | 0.4738 ± 0.2011 | 0.3992 ± 0.2211 | 0.408 # | 0.0787 ± 0.1668 | 0.4803 ± 0.1680 | 0.4787 ± 0.2014 | 0.958 | 0.0016 ± 0.1021 |
| 22-HDHA | 0.0994 ± 0.0832 | 0.0763 ± 0.0603 | 0.325 | 0.0216 ± 0.0282 | 0.1067 ± 0.0758 | 0.1115 ± 0.0824 | 0.695 # | −0.0048 ± 0.0562 |
| 20-HEPE | 0.1460 ± 0.0808 | 0.1343 ± 0.0692 | 0.713 # | 0.0119 ± 0.0403 | 0.1550 ± 0.0963 | 0.1485 ± 0.0768 | 0.608 | 0.0065 ± 0.0426 |
| Amount ng/ml | Pre-HD A (Mean ± SD) | Pre-HD V (Mean ± SD) | p-Value, t-Test (# Paired Wilcoxon test) | Pre-HD A-V Difference (Mean ± SD) | Post-HD A (Mean ± SD) | Post-HD V (Mean ± SD) | p-Value, t-test (# Paired Wilcoxon Test) | Pre-HD A-V Difference (Mean ± SD) |
|---|---|---|---|---|---|---|---|---|
| 5,6-EET + 5,6-DHET | 26.3853 ± 22.7488 | 17.8740 ± 15.3357 | 0.325 # | 8.2771 ± 22.0947 | 38.4409 ± 16.7998 | 63.1169 ± 21.0481 | 0.003 # | −24.6760 ± 17.5393 |
| 8,9-EET + 8,9-DHET | 12.2661 ± 10.8593 | 8.8769 ± 6.7288 | 0.758 # | 3.2897 ± 11.3985 | 14.9171 ± 6.2221 | 23.6504 ± 7.8856 | 0.003 # | −8.7333 ± 7.0409 |
| 11,12-EET + 11,12-DHET | 10.3905 ± 10.0509 | 7.4546 ± 6.8226 | 0.902 # | 2.7353 ± 10.2061 | 14.7525 ± 6.7118 | 26.1620 ± 9.1754 | 0.002 # | −11.4095 ± 7.5222 |
| 14,15-EET + 14,15-DHET | 12.9774 ± 12.5015 | 10.0376 ± 9.5061 | 0.667 # | 2.6766 ± 12.4408 | 19.5791 ± 9.2852 | 36.1083 ± 13.6146 | 0.002 # | −16.5292 ± 10.9098 |
| 7,8-EDP + 7,8-DiHDPA | 4.9725 ± 4.3744 | 3.7040 ± 3.1733 | 0.854 # | 1.2292 ± 4.8036 | 6.4969 ± 2.8052 | 10.8874 ± 3.5963 | 0.002 # | −4.3904 ± 2.2808 |
| 10,11-EDP + 10,11-DiHDPA | 4.6062 ± 4.3839 | 3.4580 ± 3.0889 | 0.806 # | 1.0598 ± 4.5591 | 6.7795 ± 3.0931 | 12.0623 ± 3.9527 | <0.001 | −5.2828 ± 2.5347 |
| 13,14-EDP + 13,14-DiHDPA | 3.4752 ± 3.4913 | 2.7467 ± 2.8205 | 0.854 # | 0.6542 ± 3.6762 | 4.9215 ± 2.2192 | 7.9218 ± 2.6423 | <0.001 | −3.0002 ± 1.9422 |
| 16,17-EDP + 16,17-DiHDPA | 3.0618 ± 2.8699 | 2.2873 ± 2.0344 | 0.712 # | 0.7529 ± 2.8441 | 3.9502 ± 1.7125 | 5.6394 ± 2.0354 | 0.009 | −1.6892 ± 1.8365 |
| 19,20-EDP + 19,20-DiHDPA | 6.3937 ± 5.2944 | 4.7947 ± 3.1021 | 1 # | 1.5121 ± 5.6027 | 9.6295 ± 4.0652 | 17.2258 ± 6.4814 | <0.001 | −7.5963 ± 3.8630 |
| 5,6-EEQ + 5,6-DiHETE | 1.5350 ± 0.9296 | 1.3729 ± 0.7133 | 0.622 # | 0.3217 ± 0.8716 | 2.0440 ± 1.5009 | 1.7043 ± 0.8338 | 0.388 # | 0.3397 ± 1.2857 |
| 8,9-EEQ + 8,9-DiHETE | 1.5386 ± 1.2263 | 1.0880 ± 0.6966 | 0.285 | 0.4408 ± 1.3934 | 2.7148 ± 1.8146 | 4.4861 ± 1.6000 | 0.008 # | −1.7714 ± 1.6800 |
| 11,12-EEQ + 11,12-DiHETE | 1.0017 ± 0.8179 | 0.7552 ± 0.4846 | 0.758 # | 0.2422 ± 0.9263 | 1.8673 ± 1.2279 | 3.5323 ± 1.3814 | 0.003 # | −1.6651 ± 1.1940 |
| 14,15-EEQ + 14,15-DiHETE | 0.9963 ± 0.7071 | 0.7508 ± 0.4514 | 0.328 | 0.2305 ± 0.8200 | 1.8082 ± 1.2226 | 3.3214 ± 1.3339 | 0.004 # | −1.5133 ± 1.3083 |
| 17,18-EEQ + 17,18-DiHETE | 1.8998 ± 1.3591 | 1.6056 ± 0.8496 | 0.536 | 0.2613 ± 1.5047 | 3.2405 ± 2.1560 | 6.5059 ± 2.3420 | 0.003 # | −3.2654 ± 2.0580 |
| 9,10-EpOME + 9,10-DiHOME | 37.1683 ± 31.3783 | 25.8981 ± 13.6496 | 0.712 # | 10.7144 ± 32.1530 | 57.3217 ± 18.9513 | 99.2342 ± 38.1881 | 0.002 # | −41.9125 ± 28.5066 |
| 12,13-EpOME + 12,13-DiHOME | 35.9634 ± 27.1475 | 24.5992 ± 12.1650 | 0.424 # | 10.7813 ± 27.9218 | 53.8703 ± 15.3169 | 86.6564 ± 25.6785 | <0.001 | −32.7861 ± 16.4280 |
| 5,6-DHET/5,6-EET | 0.0749 ± 0.0518 | 0.0864 ± 0.0565 | 0.617 | 0.0431 ± 0.0261 | 0.0222 ± 0.0120 | 0.002 # | ||
| 8,9-DHET/8,9-EET | 0.2737 ± 0.2578 | 0.2858 ± 0.2519 | 0.854 # | 0.1253 ± 0.0630 | 0.0599 ± 0.0480 | 0.002 # | ||
| 11,12-DHET/11,12-EET | 0.0827 ± 0.0649 | 0.0874 ± 0.0650 | 0.926 # | 0.0426 ± 0.0205 | 0.0198 ± 0.0099 | 0.002 # | ||
| 14,15-DHET/14,15-EET | 0.0654 ± 0.0409 | 0.0550 ± 0.0284 | 0.485 | 0.0326 ± 0.0210 | 0.0127 ± 0.0047 | 0.002 # | ||
| 7,8-DiHDPA/7,8-EDP | 0.1650 ± 0.1420 | 0.5745 ± 1.4719 | 0.622 # | 0.0892 ± 0.0353 | 0.0458 ± 0.0285 | 0.002 # | ||
| 10,11-DiHDPA/10,11-EDP | 0.0538 ± 0.0350 | 0.0514 ± 0.0285 | 0.859 | 0.0256 ± 0.0118 | 0.0110 ± 0.0041 | 0.002 # | ||
| 13,14-DiHDPA/13,14-EDP | 0.0506 ± 0.0302 | 0.0484 ± 0.0269 | 0.855 | 0.0237 ± 0.0101 | 0.0134 ± 0.0039 | 0.01 # | ||
| 16,17-DiHDPA/16,17-EDP | 0.0552 ± 0.0392 | 0.0601 ± 0.0343 | 0.755 | 0.0335 ± 0.0139 | 0.0194 ± 0.0071 | 0.008 | ||
| 19,20-DiHDPA/19,20-EDP | 0.2730 ± 0.2232 | 0.2905 ± 0.1983 | 0.806 # | 0.1212 ± 0.0480 | 0.0580 ± 0.0264 | 0.002 # | ||
| 5,6-DiHETE/5,6-EEQ | 483.3002 ± 348.2197 | 599.0058 ± 431.5977 | 0.49 | 274.7175 ± 163.7055 | 121.8920 ± 63.0904 | 0.001 | ||
| 8,9-DiHETE/8,9-EEQ | 0.1037 ± 0.0654 | 0.1332 ± 0.0872 | 0.372 | 0.0502 ± 0.0261 | 0.0229 ± 0.0107 | 0.002 # | ||
| 11,12-DiHETE/11,12-EEQ | 0.1107 ± 0.1548 | 0.0634 ± 0.0260 | 0.806 # | 0.0596 ± 0.1111 | 0.0112 ± 0.0032 | 0.002 # | ||
| 14,15-DiHETE/14,15-EEQ | 0.1012 ± 0.0933 | 0.0817 ± 0.0318 | 0.854 # | 0.0436 ± 0.0466 | 0.0153 ± 0.0044 | 0.003 # | ||
| 17,18-DiHETE/17,18-EEQ | 0.2320 ± 0.1551 | 0.2159 ± 0.1591 | 0.667 # | 0.1399 ± 0.1461 | 0.0397 ± 0.0133 | 0.002 # | ||
| 9,10-DiHOME/9,10-EpOME | 0.1799 ± 0.0860 | 0.1731 ± 0.1090 | 0.58 # | 0.1260 ± 0.0918 | 0.0617 ± 0.0222 | 0.01 # | ||
| 12,13-DiHOME/12,13-EpOME | 0.2255 ± 0.0981 | 0.2087 ± 0.0951 | 0.356 # | 0.1627 ± 0.1101 | 0.0877 ± 0.0327 | 0.008 # | ||
| Ratio(5,6-DHET+8,9-DHET+11,12-DHET+14,15-DHET) / (5,6-EET+8,9-EET +11,12 EET +14,15-EET) | 0.1104 ± 0.0878 | 0.1188 ± 0.0946 | 1 # | 0.0541 ± 0.0262 | 0.0253 ± 0.0143 | 0.002 # | ||
| Ratio(7,8-DiHDPA+10,11-DiHDPA +13,14-DiHDPA+16,17-DiHDPA+19,20-DiHDPA) / (7,8-EDP+10,11-EDP+13,14-EDP+16,17-EDP+19,20-EDP) | 0.1369 ± 0.1095 | 0.1478 ± 0.1106 | 0.902 # | 0.0666 ± 0.0240 | 0.0336 ± 0.0143 | 0.002 # | ||
| Ratio(5,6-DiHETE+8,9-DiHETE+11,12-DiHETE+14,15-DiHETE+17,18-DiHETE) / (5,6-EEQ+ 8,9-EEQ+11,12-EEQ+14,15-EEQ+17,18-EEQ) | 0.6541 ± 0.4424 | 0.6335 ± 0.4128 | 0.909 | 0.3403 ± 0.2022 | 0.1315 ± 0.0660 | 0.002 # | ||
| Ratio (9,10-DiHOME+12,13-DiHOME) / (9,10-EpOME+12,13-EpOME) | 0.2017 ± 0.0845 | 0.1904 ± 0.1007 | 0.58 # | 0.1445 ± 0.1017 | 0.0741 ± 0.0258 | 0.008 # |
| Post-HD A (Mean ± SD) | Post-HD V (Mean ± SD) | p-Value, t-Test (# Paired Wilcoxon Test) | Post-HD A-V Difference (Mean ± SD) | |
|---|---|---|---|---|
| CYP epoxy-metabolites | ||||
| 5,6-EET | 0.2022 ± 0.0733 | 0.2317 ± 0.0812 | 0.303 | −0.0295 ± 0.0945 |
| 8,9-EET | 0.2672 ± 0.1586 | 0.2517 ± 0.1676 | 0.814 # | 0.0155 ± 0.1947 |
| 11,12-EET | 0.1754 ± 0.0675 | 0.2403 ± 0.1094 | 0.051 | −0.0649 ± 0.1029 |
| 14,15-EET | 0.2573 ± 0.1199 | 0.3791 ± 0.2067 | 0.049 | −0.1219 ± 0.1913 |
| 5,6-DHET | 0.0324 ± 0.0085 | 0.0321 ± 0.0104 | 0.814 # | 0.0002 ± 0.0047 |
| 8,9-DHET | 0.0910 ± 0.0281 | 0.0847 ± 0.0241 | 0.388 # | 0.0063 ± 0.0207 |
| 11,12-DHET | 0.1486 ± 0.0443 | 0.1454 ± 0.0379 | 0.631 | 0.0032 ± 0.0226 |
| 14,15-DHET | 0.2038 ± 0.0569 | 0.2062 ± 0.0477 | 0.854 | −0.0024 ± 0.0444 |
| 7,8-EDP | 0.1852 ± 0.1197 | 0.2412 ± 0.1309 | 0.076 | −0.0560 ± 0.0993 |
| 10,11-EDP | 0.1358 ± 0.0948 | 0.1805 ± 0.1004 | 0.079 | −0.0447 ± 0.0800 |
| 13,14-EDP | 0.1273 ± 0.0808 | 0.1452 ± 0.0769 | 0.439 | −0.0179 ± 0.0774 |
| 16,17-EDP | 0.1922 ± 0.0843 | 0.2284 ± 0.0893 | 0.124 | −0.0362 ± 0.0753 |
| 19,20-EDP | 0.2899 ± 0.1669 | 0.3587 ± 0.1754 | 0.096 | −0.0688 ± 0.1311 |
| 7,8-DiHDPA | 0.0234 ± 0.0210 | 0.0330 ± 0.0115 | 0.388 # | −0.0097 ± 0.0267 |
| 10,11-DiHDPA | 0.0581 ± 0.0148 | 0.0554 ± 0.0125 | 0.182 # | 0.0027 ± 0.0067 |
| 13,14-DiHDPA | 0.0696 ± 0.0222 | 0.0661 ± 0.0178 | 0.272 # | 0.0035 ± 0.0090 |
| 16,17-DiHDPA | 0.0865 ± 0.0293 | 0.0809 ± 0.0206 | 0.695 # | 0.0056 ± 0.0148 |
| 19,20-DiHDPA | 0.7042 ± 0.3142 | 0.6061 ± 0.2823 | 0.06 # | 0.0981 ± 0.1753 |
| 8,9-EEQ | 0.0663 ± 0.0419 | 0.0700 ± 0.0284 | 0.791 | −0.0037 ± 0.0472 |
| 11,12-EEQ | 0.0435 ± 0.0354 | 0.0490 ± 0.0252 | 0.388 # | −0.0055 ± 0.0418 |
| 14,15-EEQ | 0.0607 ± 0.0349 | 0.0655 ± 0.0298 | 0.651 | −0.0049 ± 0.0363 |
| 17,18-EEQ | 0.0830 ± 0.0590 | 0.0936 ± 0.0518 | 0.602 | −0.0106 ± 0.0684 |
| 5,6-DiHETE | 0.0980 ± 0.0508 | 0.0799 ± 0.0403 | 0.01 | 0.0181 ± 0.0322 |
| 8,9-DiHETE | 0.0233 ± 0.0063 | 0.0202 ± 0.0041 | 0.174 | 0.0031 ± 0.0074 |
| 11,12-DiHETE | 0.0160 ± 0.0026 | 0.0155 ± 0.0023 | 0.461 | 0.0004 ± 0.0020 |
| 14,15-DiHETE | 0.0181 ± 0.0080 | 0.0167 ± 0.0073 | 0.525 | 0.0015 ± 0.0078 |
| 17,18-DiHETE | 0.1661 ± 0.0704 | 0.1476 ± 0.0603 | 0.337 | 0.0185 ± 0.0640 |
| 9,10-EpOME | 4.6969 ± 3.1153 | 6.2952 ± 5.0363 | 0.182 # | −1.5984 ± 3.6422 |
| 12,13-EpOME | 6.8441 ± 3.8513 | 8.4182 ± 6.5171 | 0.239 # | −1.5740 ± 4.1754 |
| 9,10-DiHOME | 1.7695 ± 1.1345 | 1.7400 ± 1.1665 | 0.754 # | 0.0295 ± 0.2442 |
| 12,13-DiHOME | 3.3260 ± 2.0952 | 3.4845 ± 2.2350 | 0.347 # | −0.1585 ± 0.4498 |
| LOX metabolites | ||||
| 5-HETE | 0.1100 ± 0.0465 | 0.1147 ± 0.0494 | 0.365 | −0.0046 ± 0.0169 |
| 8-HETE | 0.0672 ± 0.0281 | 0.0667 ± 0.0298 | 0.943 | 0.0006 ± 0.0273 |
| 9-HETE | 0.1016 ± 0.0158 | 0.1058 ± 0.0218 | 0.31 | −0.0042 ± 0.0136 |
| 11-HETE | 0.0739 ± 0.0265 | 0.0800 ± 0.0305 | 0.262 | −0.0061 ± 0.0180 |
| 12-HETE | 0.5660 ± 0.3630 | 0.4319 ± 0.2449 | 0.094 | 0.1341 ± 0.2531 |
| 15-HETE | 0.1789 ± 0.0583 | 0.1841 ± 0.0689 | 0.536 | −0.0052 ± 0.0282 |
| 4-HDHA | 0.0821 ± 0.0209 | 0.0844 ± 0.0239 | 0.695 # | −0.0023 ± 0.0109 |
| 7-HDHA | 0.0852 ± 0.0189 | 0.0875 ± 0.0186 | 0.594 | −0.0024 ± 0.0148 |
| 8-HDHA | 0.0779 ± 0.0221 | 0.0763 ± 0.0241 | 0.584 | 0.0016 ± 0.0098 |
| 10-HDHA | 0.0622 ± 0.0148 | 0.0636 ± 0.0173 | 0.658 | −0.0014 ± 0.0105 |
| 11-HDHA | 0.0722 ± 0.0107 | 0.0766 ± 0.0117 | 0.081 | −0.0044 ± 0.0079 |
| 13-HDHA | 0.0653 ± 0.0131 | 0.0671 ± 0.0143 | 0.272 # | −0.0018 ± 0.0065 |
| 14-HDHA | 0.1165 ± 0.0638 | 0.1098 ± 0.0627 | 0.308 # | 0.0067 ± 0.0218 |
| 16-HDHA | 0.0589 ± 0.0142 | 0.0610 ± 0.0122 | 0.389 | −0.0022 ± 0.0083 |
| 17-HDHA | 0.1191 ± 0.0301 | 0.1196 ± 0.0325 | 0.924 | −0.0005 ± 0.0174 |
| 20-HDHA | 0.2074 ± 0.0539 | 0.2079 ± 0.0489 | 0.347 # | −0.0004 ± 0.0370 |
| 5-HEPE | 0.1032 ± 0.0315 | 0.0962 ± 0.0336 | 0.171 | 0.0070 ± 0.0166 |
| 8-HEPE | 0.0352 ± 0.0045 | 0.0327 ± 0.0051 | 0.128 | 0.0025 ± 0.0053 |
| 9-HEPE | 0.0756 ± 0.0137 | 0.0703 ± 0.0095 | 0.155 | 0.0053 ± 0.0121 |
| 11-HEPE | 0.0847 ± 0.0025 | 0.0856 ± 0.0035 | 0.875 # | −0.0008 ± 0.0045 |
| 12-HEPE | 0.1595 ± 0.0220 | 0.1540 ± 0.0228 | 0.136 # | 0.0055 ± 0.0158 |
| 15-HEPE | 0.1078 ± 0.0123 | 0.1036 ± 0.0105 | 0.084 # | 0.0042 ± 0.0085 |
| 18-HEPE | 0.1779 ± 0.0413 | 0.1596 ± 0.0278 | 0.07 # | 0.0183 ± 0.0316 |
| 9-HODE | 8.5190 ± 13.8940 | 8.3464 ± 12.8721 | 0.347 # | 0.1726 ± 1.8733 |
| 13-HODE | 4.3069 ± 3.0614 | 4.4488 ± 2.9851 | 0.53 # | −0.1419 ± 0.6334 |
| CYP ω/(ω−1) metabolites | ||||
| 16-HETE | 0.0626 ± 0.0120 | 0.0631 ± 0.0114 | 0.772 | −0.0006 ± 0.0069 |
| 17-HETE | 0.0242 ± 0.0028 | 0.0240 ± 0.0029 | 0.713 | 0.0002 ± 0.0018 |
| 18-HETE | 0.0456 ± 0.0082 | 0.0451 ± 0.0072 | 0.684 | 0.0005 ± 0.0044 |
| 19-HETE | 0.0387 ± 0.0291 | 0.0392 ± 0.0269 | 0.638 # | −0.0005 ± 0.0216 |
| 20-HETE | 0.1457 ± 0.1239 | 0.0709 ± 0.0885 | 0.084 # | 0.0747 ± 0.1464 |
| 22-HDHA | 0.0843 ± 0.0662 | 0.0754 ± 0.0632 | 0.177 | 0.0089 ± 0.0213 |
| 20-HEPE | 0.0900 ± 0.0271 | 0.0856 ± 0.0284 | 0.638 # | 0.0045 ± 0.0171 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Liu, T.; Dogan, I.; Rothe, M.; Kunz, J.V.; Knauf, F.; Gollasch, M.; Luft, F.C.; Gollasch, B. Hemodialysis and Plasma Oxylipin Biotransformation in Peripheral Tissue. Metabolites 2022, 12, 34. https://doi.org/10.3390/metabo12010034
Liu T, Dogan I, Rothe M, Kunz JV, Knauf F, Gollasch M, Luft FC, Gollasch B. Hemodialysis and Plasma Oxylipin Biotransformation in Peripheral Tissue. Metabolites. 2022; 12(1):34. https://doi.org/10.3390/metabo12010034
Chicago/Turabian StyleLiu, Tong, Inci Dogan, Michael Rothe, Julius V. Kunz, Felix Knauf, Maik Gollasch, Friedrich C. Luft, and Benjamin Gollasch. 2022. "Hemodialysis and Plasma Oxylipin Biotransformation in Peripheral Tissue" Metabolites 12, no. 1: 34. https://doi.org/10.3390/metabo12010034
APA StyleLiu, T., Dogan, I., Rothe, M., Kunz, J. V., Knauf, F., Gollasch, M., Luft, F. C., & Gollasch, B. (2022). Hemodialysis and Plasma Oxylipin Biotransformation in Peripheral Tissue. Metabolites, 12(1), 34. https://doi.org/10.3390/metabo12010034







