Gallstone Formation Follows a Different Trajectory in Bariatric Patients Compared to Nonbariatric Patients
Abstract
:1. Introduction
2. Results
2.1. Study Population
2.2. Stones
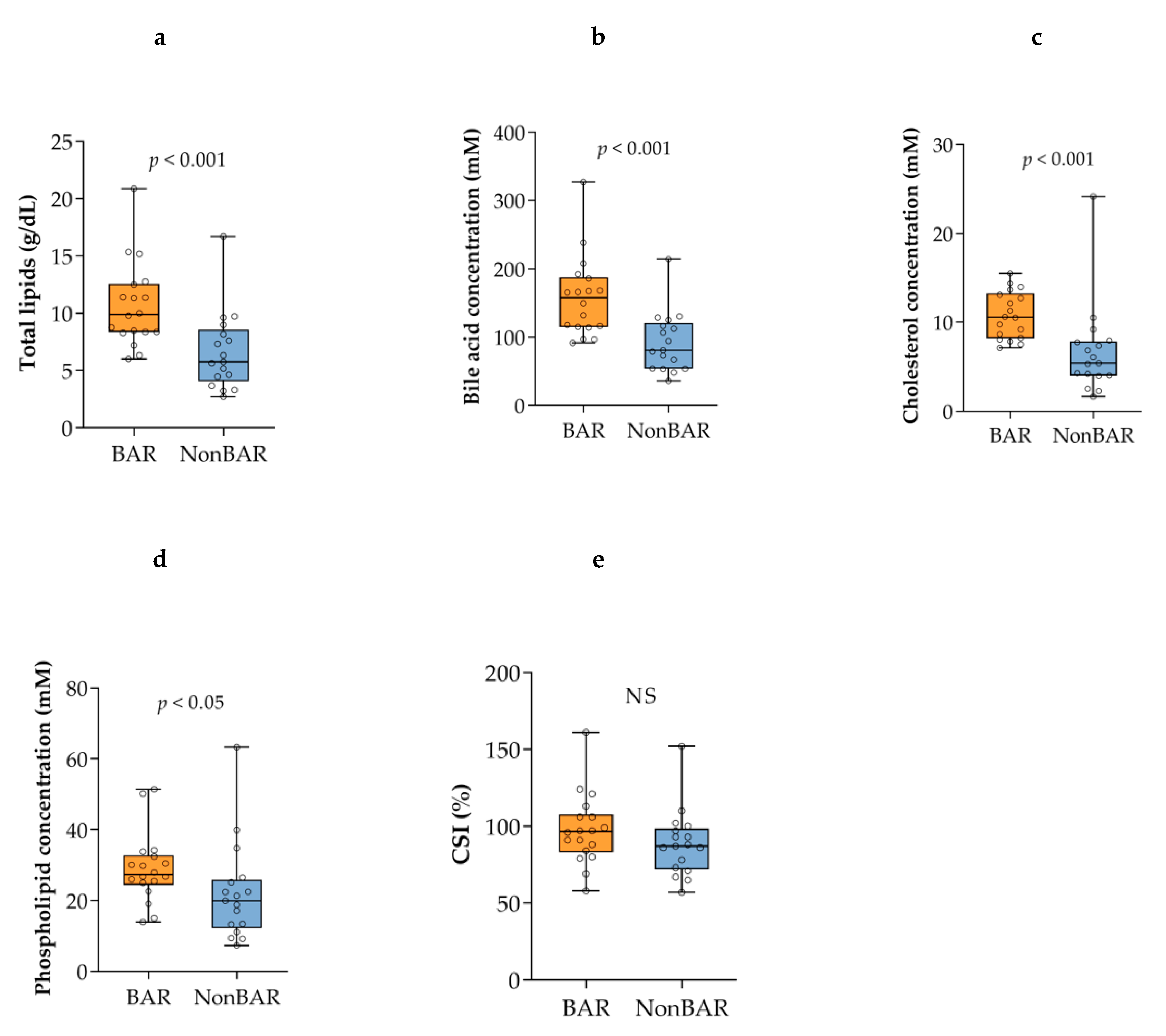
2.3. Biliary Lipid Composition, Cholesterol Saturation, and Cholesterol Crystals
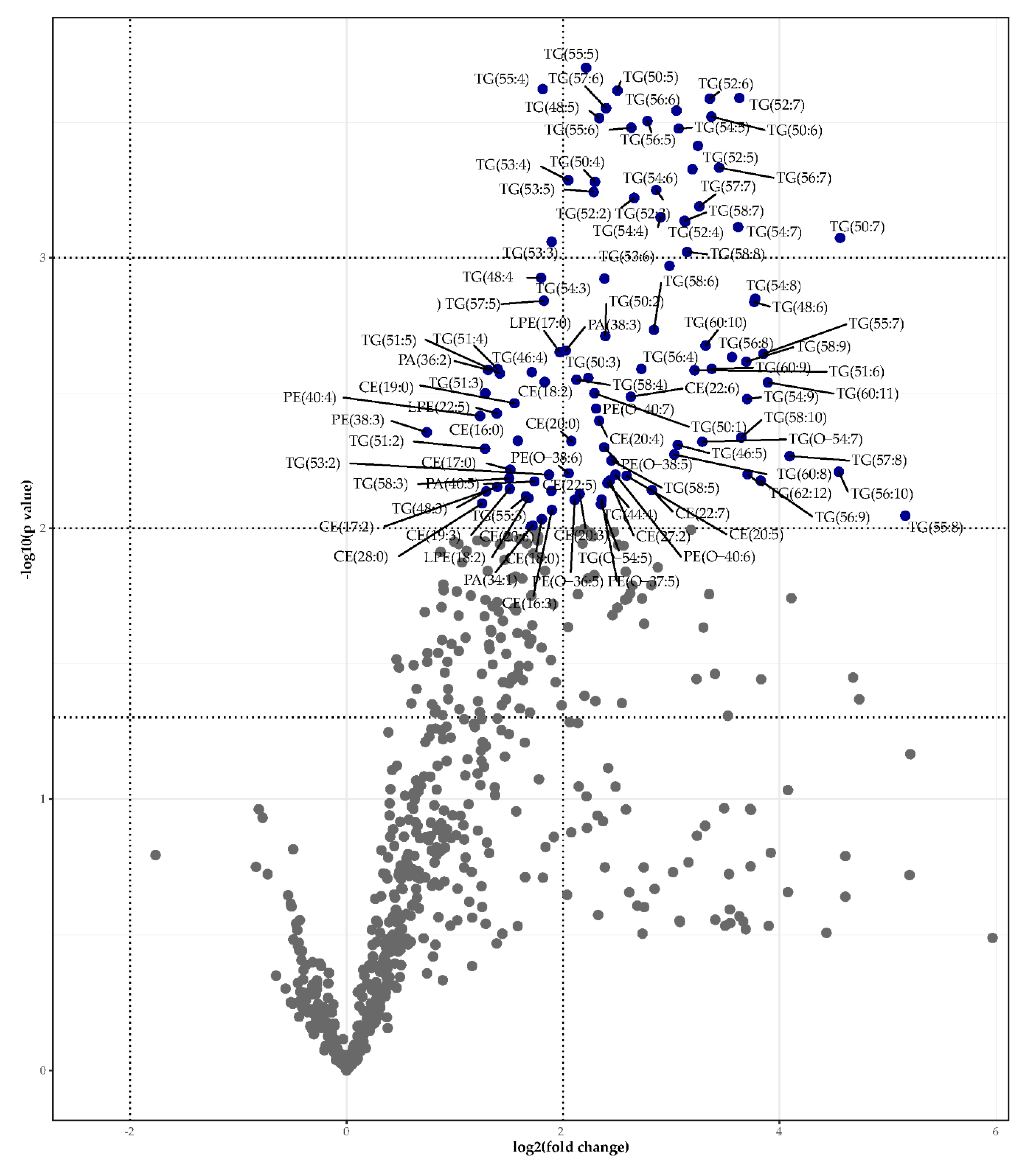
2.4. Lipidomics
2.5. Apolipoproteins
3. Discussion
3.1. Main Findings
3.2. Interpretations
3.3. Limitations
3.4. Conclusion
4. Materials and Methods
4.1. Patients
4.2. Sample Collection
4.3. Gallstone Composition
4.4. Biliary Lipid Composition, CSI, Cholesterol Crystals, and Apolipoproteins
4.5. Lipidomics Analysis
4.5.1. One-Phase Lipidomic Extraction
4.5.2. Internal Standards
4.5.3. Method
4.5.4. Processing
4.5.5. Identification
4.6. Statistical Analysis
Lipidomics Data
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Portincasa, P.; Moschetta, A.; Palasciano, G. Cholesterol Gallstone Disease. Lancet 2006, 368, 230–239. [Google Scholar] [CrossRef]
- Di Ciaula, A.; Wang, D.Q.-H.; Portincasa, P. An update on the pathogenesis of cholesterol gallstone disease. Curr. Opin. Gastroenterol. 2018, 34, 71–80. [Google Scholar] [CrossRef] [PubMed]
- Holan, K.R.; Holzbach, R.T.; E Hermann, R.; Cooperman, A.M.; Claffey, W.J. Nucleation time: A key factor in the pathogenesis of cholesterol gallstone disease. Gastroenterololy 1979, 77, 611–617. [Google Scholar] [CrossRef]
- Holzbach, R.T.; Marsh, M.; Olszewski, M.; Holan, K. Cholesterol Solubility in Bile. Evidence that supersaturated bile is frequent in healthy man. J. Clin. Investig. 1973, 52, 1467–1479. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Adams, L.B.; Chang, C.; Pope, J.; Kim, Y.; Liu, P.; Yates, A. Randomized, Prospective Comparison of Ursodeoxycholic Acid for the Prevention of Gallstones after Sleeve Gastrectomy. Obes. Surg. 2015, 26, 990–994. [Google Scholar] [CrossRef] [PubMed]
- Nabil, T.M.; Khalil, A.H.; Gamal, K. Effect of oral ursodeoxycholic acid on cholelithiasis following laparoscopic sleeve gastrectomy for morbid obesity. Surg. Obes. Relat. Dis. 2019, 15, 827–831. [Google Scholar] [CrossRef]
- Sakran, N.; Dar, R.; Assalia, A.; Neeman, Z.; Farraj, M.; Sherf-Dagan, S.; Gralnek, I.M.; Hazzan, R.; Mokary, S.E.; Nevo-Aboody, H.; et al. The use of Ursolit for gallstone prophylaxis following bariatric surgery: A randomized-controlled trial. Updat. Surg. 2020, 72, 1125–1133. [Google Scholar] [CrossRef]
- Altieri, M.S.; Yang, J.; Nie, L.; Docimo, S.; Talamini, M.; Pryor, A.D. Incidence of cholecystectomy after bariatric surgery. Surg. Obes. Relat. Dis. 2018, 14, 992–996. [Google Scholar] [CrossRef]
- Coupaye, M.; Calabrese, D.; Sami, O.; Msika, S.; Ledoux, S. Evaluation of incidence of cholelithiasis after bariatric surgery in subjects treated or not treated with ursodeoxycholic acid. Surg. Obes. Relat. Dis. 2017, 13, 681–685. [Google Scholar] [CrossRef]
- Portenier, D.D.; Grant, J.P.; Blackwood, H.S.; Pryor, A.; McMahon, R.L.; DeMaria, E. Expectant management of the asymptomatic gallbladder at Roux-en-Y gastric bypass. Surg. Obes. Relat. Dis. 2007, 3, 476–479. [Google Scholar] [CrossRef]
- Shiffman, M.L.; Sugerman, H.J.; Kellum, J.M.; Brewer, W.H.; Moore, E.W. Gallstone formation after rapid weight loss: A prospective study in patients undergoing gastric bypass surgery for treatment of morbid obesity. Am. J. Gastroenterol. 1991, 86, 1000–1005. [Google Scholar]
- Östlund, M.P.; Wenger, U.; Mattsson, F.; Ebrahim, F.; Botha, A.; Lagergren, J. Population-based study of the need for cholecystectomy after obesity surgery. BJS 2012, 99, 864–869. [Google Scholar] [CrossRef]
- Tsirline, V.B.; Keilani, Z.M.; El Djouzi, S.; Phillips, R.C.; Kuwada, T.S.; Gersin, K.; Simms, C.; Stefanidis, D. How frequently and when do patients undergo cholecystectomy after bariatric surgery? Surg. Obes. Relat. Dis. 2014, 10, 313–321. [Google Scholar] [CrossRef] [PubMed]
- Bennion, L.J.; Grundy, S.M. Effects of obesity and caloric intake on biliary lipid metabolism in man. J. Clin. Investig. 1975, 56, 996–1011. [Google Scholar] [CrossRef] [PubMed]
- Broomfield, P.H.; Chopra, R.; Sheinbaum, R.C.; Bonorris, G.G.; Silverman, A.; Schoenfield, L.J.; Marks, J.W. Effects of Ursodeoxycholic Acid and Aspirin on the Formation of Lithogenic Bile and Gallstones during Loss of Weight. New Engl. J. Med. 1988, 319, 1567–1572. [Google Scholar] [CrossRef] [PubMed]
- Festi, D.; Colecchia, A.; Orsini, M.; Sangermano, A.; Sottili, S.; Simoni, P.; Mazzella, G.; Villanova, N.; Bazzoli, F.; Lapenna, D.; et al. Gallbladder motility and gallstone formation in obese patients following very low calorie diets. Use it (fat) to lose it (well). Int. J. Obes. 1998, 22, 592–600. [Google Scholar] [CrossRef] [Green Version]
- Gebhard, R.L.; Prigge, W.F.; Ansel, H.J.; Schlasner, L.; Ketover, S.R.; Sande, D.; Holtmeier, K.; Peterson, F.J. The Role of Gallbladder Emptying in Gallstone Formation During Diet-Induced Rapid Weight Loss. Hepatology 1996, 24, 544–548. [Google Scholar] [CrossRef]
- Gustafsson, U.; Benthin, L.; Granström, L.; Groen, A.K.; Sahlin, S.; Einarsson, C. Changes in gallbladder bile composition and crystal detection time in morbidly obese subjects after bariatric surgery. Hepatology 2005, 41, 1322–1328. [Google Scholar] [CrossRef]
- Marks, J.W.; Bonorris, G.G.; Albers, G.; Schoenfield, L.J. The sequence of biliary events preceding the formation of gallstones in humans. Gastroenterology 1992, 103, 566–570. [Google Scholar] [CrossRef]
- Mazzella, G.; Bazzoli, F.; Festi, D.; Ronchi, M.; Aldini, R.; Roda, A.; Grigolo, B.; Simoni, P.; Villanova, N.; Roda, E. Comparative evaluation of chenodeoxycholic and ursodeoxycholic acids in obese patients. Gastroenterology 1991, 101, 490–496. [Google Scholar] [CrossRef]
- Shiffman, M.L.; Brinkman-Kaplan, V.; Kaplan, G.D.; Vickers, F.F. Prophylaxis against Gallstone Formation with Ursodeoxycholic Acid in Patients Participating in a Very-Low-Calorie Diet Program. Ann. Intern. Med. 1995, 122, 899–905. [Google Scholar] [CrossRef] [PubMed]
- Shiffman, M.L.; Shamburek, R.D.; Schwartz, C.C.; Sugerman, H.J.; Kellum, J.M.; Moore, E.W. Gallbladder mucin, arachidonic acid, and bile lipids in patients who develop gallstones during weight reduction. Gastroenteroloy 1993, 105, 1200–1208. [Google Scholar] [CrossRef]
- Shiffman, M.L.; Sugerman, H.J.; Kellum, J.M.; Moore, E.W. Changes in gallbladder bile composition following gallstone formation and weight reduction. Gastroenterology 1992, 103, 214–221. [Google Scholar] [CrossRef]
- Reuben, A.; Qureshi, Y.; Murphy, G.M.; Dowling, R.H. Effect of obesity and weight reduction on biliary cholesterol saturation and the response to chenodeoxycholic acid. Eur. J. Clin. Investig. 1986, 16, 133–142. [Google Scholar] [CrossRef] [PubMed]
- Shiffman, M.L.; Sugerman, H.J.; Kellum, J.H.; Brewer, W.H.; Moore, E.W. Gallstones in patients with morbid obesity. Relationship to body weight, weight loss and gallbladder bile cholesterol solubility. Int. J. Obes. Relat. Metab. Disord. J. Int. Assoc. Study Obes. 1993, 17, 153–158. [Google Scholar]
- Rudling, M.; Laskar, A.; Straniero, S. Gallbladder bile supersaturated with cholesterol in gallstone patients preferentially develops from shortage of bile acids. J. Lipid Res. 2019, 60, 498–505. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Nestel, P.J.; Schreibman, P.H.; Ahrens, E.H. Cholesterol Metabolism in Human Obesity. J. Clin. Investig. 1973, 52, 2389–2397. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Schaefer, E.J.; Woo, R.; Kibata, M.; Bjornsen, L.; Schreibman, P.H. Mobilization of triglyceride but not cholesterol or tocopherol from human adipocytes during weight reduction. Am. J. Clin. Nutr. 1983, 37, 749–754. [Google Scholar] [CrossRef] [Green Version]
- VAN Erpecum, K.J.; Stolk, M.F.J.; Broek, A.M.W.C.V.D.; Renooijβ, W.; VAN DE Heijning, B.J.M.; Henegouwen, G.P.V.B. Bile concentration promotes nucleation of cholesterol monohydrate crystals by increasing the cholesterol concentration in the vesicles. Eur. J. Clin. Investig. 1993, 23, 283–288. [Google Scholar] [CrossRef]
- Wang, D.Q.; Carey, M.C. Complete mapping of crystallization pathways during cholesterol precipitation from model bile: Influence of physical-chemical variables of pathophysiologic relevance and identification of a stable liquid crystalline state in cold, dilute and hydrophilic bile salt-containing systems. J. Lipid Res. 1996, 37, 606–630. [Google Scholar]
- Van Erpecum, K.J.; Van Henegouwen, G.P.B.; Stoelwinder, B.; Schmidt, Y.M.G.; Willekens, F.L.H. Bile concentration is a key factor for nucleation of cholesterol crystals and cholesterol saturation index in gallbladder bile of gallstone patients. Hepatology 1990, 11, 1–6. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Hussaini, S.H.; Pereira, S.P.; Murphy, G.M.; Dowling, R.H. Deoxycholic acid influences cholesterol solubilization and microcrystal nucleation time in gallbladder bile. Hepatology 1995, 22, 1735–1744. [Google Scholar] [PubMed]
- Bastouly, M.; Arasaki, C.H.; Ferreira, J.B.; Zanoto, A.; Borges, F.G.H.P.; Del Grande, J.C. Early Changes in Postprandial Gallbladder Emptying in Morbidly Obese Patients Undergoing Roux-en-Y Gastric Bypass: Correlation with the Occurrence of Biliary Sludge and Gallstones. Obes. Surg. 2009, 19, 22–28. [Google Scholar] [CrossRef] [PubMed]
- Stolk, M.F.; Van Erpecum, K.J.; Renooij, W.; Portincasa, P.; Van De Heijning, B.J.; Vanberge-Henegouwen, G.P. Gallbladder emptying in vivo, bile composition, and nucleation of cholesterol crystals in patients with cholesterol gallstones. Gastroenterology 1995, 108, 1882–1888. [Google Scholar] [CrossRef]
- Haal, S.; Guman, M.; Boerlage, T.; Acherman, Y.; de Brauw, M.; Bruin, S.; de Castro, S.; van Hooft, J.E.; van de Laar, A.; Moes, D.; et al. 355 ursodeoxycholic acid for the prevention of symptomatic gallstone disease after bariatric surgery: A multicenter, randomized, placebo-controlled, double-blind superiority trial (upgrade trial). Gastroenterology 2021, 160, s0016–s5085. [Google Scholar] [CrossRef]
- Tietz-Bogert, P.S.; Kim, M.; Cheung, A.; Tabibian, J.H.; Heimbach, J.K.; Rosen, C.B.; Nandakumar, M.; Lazaridis, K.N.; LaRusso, N.F.; Sung, J.; et al. Metabolomic Profiling of Portal Blood and Bile Reveals Metabolic Signatures of Primary Sclerosing Cholangitis. Int. J. Mol. Sci. 2018, 19, 3188. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Urman, J.M.; Herranz, J.M.; Uriarte, I.; Rullán, M.; Oyón, D.; González, B.; Fernandez-Urién, I.; Carrascosa, J.; Bolado, F.; Zabalza, L.; et al. Pilot Multi-Omic Analysis of Human Bile from Benign and Malignant Biliary Strictures: A Machine-Learning Approach. Cancers 2020, 12, 1644. [Google Scholar] [CrossRef]
- Sewell, R.B.; Mao, S.J.; Kawamoto, T.; LaRusso, N.F. Apolipoproteins of high, low, and very low density lipoproteins in human bile. J. Lipid Res. 1983, 24, 391–401. [Google Scholar] [CrossRef]
- Kim, I.S.; Myung, S.J.; Lee, S.S.; Lee, S.K.; Kim, M.H. Classification and Nomenclature of Gallstones Revisited. Yonsei Med. J. 2003, 44, 561–570. [Google Scholar] [CrossRef]
- Groen, A.K.; Van Wijland, M.J.; Frederiks, W.M.; Smit, J.J.; Schinkel, A.H.; Elferink, R.P.O. Regulation of protein secretion into bile: Studies in mice with a disrupted mdr2 p-glycoprotein gene. Gastroenterology 1995, 109, 1997–2006. [Google Scholar] [CrossRef]
- Carey, M.C. Critical tables for calculating the cholesterol saturation of native bile. J. Lipid Res. 1978, 19, 945–955. [Google Scholar] [CrossRef]
- Molenaars, M.; Schomakers, B.V.; Elfrink, H.L.; Gao, A.W.; Vervaart, M.A.T.; Pras-Raves, M.L.; Luyf, A.C.; Smith, R.L.; Sterken, M.G.; Kammenga, J.E.; et al. Metabolomics and lipidomics in Caenorhabditis elegans using a single-sample preparation. Dis. Model. Mech. 2021, 14. [Google Scholar] [CrossRef] [PubMed]
- Chambers, M.C.; Maclean, B.; Burke, R.; Amodei, D.; Ruderman, D.L.; Neumann, S.; Gatto, L.; Fischer, B.; Pratt, B.; Egertson, J.; et al. A cross-platform toolkit for mass spectrometry and proteomics. Nat. Biotechnol. 2012, 30, 918–920. [Google Scholar] [CrossRef]




| ALL (n = 35) | BAR 1 (n = 18) | NonBAR2 (n = 17) | |
|---|---|---|---|
| Age in years | 46.0 [28.0–54.0] | 41.0 [25.0–47.3] | 48.0 [35.5–61.0] |
| Female gender, n (%) | 33 (94) | 17 (94) | 16 (94) |
| BMI 3 at cholecystectomy | 28.0 [26.0–31.0] | 27.5 [26.0–31.0] | 28.0 [26.0–35.0] |
| BMI 3 at bariatric surgery | NA | 42.9 [38.5–44.8] | NA |
| Days between bariatric surgery and cholecystectomy | NA | 492 [261–716] | NA |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Haal, S.; Guman, M.S.S.; Acherman, Y.I.Z.; Jansen, J.P.G.; van Weeghel, M.; van Lenthe, H.; Wever, E.J.M.; Gerdes, V.E.A.; Voermans, R.P.; Groen, A.K. Gallstone Formation Follows a Different Trajectory in Bariatric Patients Compared to Nonbariatric Patients. Metabolites 2021, 11, 682. https://doi.org/10.3390/metabo11100682
Haal S, Guman MSS, Acherman YIZ, Jansen JPG, van Weeghel M, van Lenthe H, Wever EJM, Gerdes VEA, Voermans RP, Groen AK. Gallstone Formation Follows a Different Trajectory in Bariatric Patients Compared to Nonbariatric Patients. Metabolites. 2021; 11(10):682. https://doi.org/10.3390/metabo11100682
Chicago/Turabian StyleHaal, Sylke, Maimoena S. S. Guman, Yair I. Z. Acherman, Johannes P. G. Jansen, Michel van Weeghel, Henk van Lenthe, Eric J. M. Wever, Victor E. A. Gerdes, Rogier P. Voermans, and Albert K. Groen. 2021. "Gallstone Formation Follows a Different Trajectory in Bariatric Patients Compared to Nonbariatric Patients" Metabolites 11, no. 10: 682. https://doi.org/10.3390/metabo11100682
APA StyleHaal, S., Guman, M. S. S., Acherman, Y. I. Z., Jansen, J. P. G., van Weeghel, M., van Lenthe, H., Wever, E. J. M., Gerdes, V. E. A., Voermans, R. P., & Groen, A. K. (2021). Gallstone Formation Follows a Different Trajectory in Bariatric Patients Compared to Nonbariatric Patients. Metabolites, 11(10), 682. https://doi.org/10.3390/metabo11100682






