Predictors of Escalation of Lipid-Lowering Therapy with Subanalysis of the Influence of Lipoprotein (a) on the Decision-Making Process
Abstract
1. Introduction
2. Materials and Methods
2.1. Statistical Analysis
2.2. Ethics
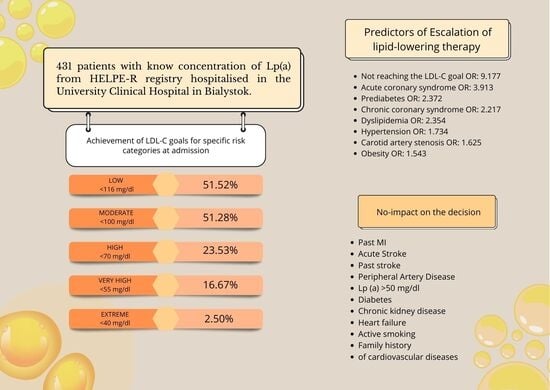
3. Results
4. Discussion
4.1. Decision-Making Process in Light of Current Guidelines
4.2. Search for Factors Influencing the Decision Regarding the Escalation
5. Limitations
6. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Naghavi, M.; Kyu, H.H.; Aalipour, M.A.; Aalruz, H.; Ababneh, H.S.; Abafita, B.J.; Abaraogu, U.O.; Abbafati, C.; Abbasi, M.; Abbaspour, F.; et al. Global burden of 292 causes of death in 204 countries and territories and 660 subnational locations, 1990-2023: A systematic analysis for the Global Burden of Disease Study 2023. Lancet 2025, 406, 1811–1872. [Google Scholar] [CrossRef]
- Alam, K.; Naghavi, M.; Ong, K.L.; Aali, A.; Ababneh, H.S.; Abate, Y.H.; Abbafati, C.; Abbasgholizadeh, R.; Abbasian, M.; Abbasi-Kangevari, M.; et al. Global burden of 288 causes of death and life expectancy decomposition in 204 countries and territories and 811 subnational locations, 1990-2021: A systematic analysis for the Global Burden of Disease Study 2021. Lancet 2024, 403, 2100–2132. [Google Scholar] [CrossRef]
- Visseren, F.L.J.; Mach, F.; Smulders, Y.M.; Carballo, D.; Koskinas, K.C.; Bäck, M.; Benetos, A.; Biffi, A.; Boavida, J.-M.; Capodanno, D.; et al. 2021 ESC Guidelines on cardiovascular disease prevention in clinical practice: Developed by the Task Force for cardiovascular disease prevention in clinical practice with representatives of the European Society of Cardiology and 12 medical societies With the special contribution of the European Association of Preventive Cardiology (EAPC). Eur. Heart J. 2021, 42, 3227–3337. [Google Scholar] [CrossRef] [PubMed]
- Mach, F.; Koskinas, K.C.; Roeters van Lennep, J.E.; Tokgözoğlu, L.; Badimon, L.; Baigent, C.; Benn, M.; Binder, C.J.; Catapano, A.L.; De Backer, G.G.; et al. 2025 Focused Update of the 2019 ESC/EAS Guidelines for the management of dyslipidaemias: Developed by the task force for the management of dyslipidaemias of the European Society of Cardiology (ESC) and the European Atherosclerosis Society (EAS). Eur. Heart J. 2025, 46, 4359–4378. [Google Scholar] [CrossRef] [PubMed]
- Mach, F.; Baigent, C.; Catapano, A.L.; Koskinas, K.C.; Casula, M.; Badimon, L.; Chapman, M.J.; De Backer, G.G.; Delgado, V.; Ference, B.A.; et al. 2019 ESC/EAS Guidelines for the management of dyslipidaemias: Lipid modification to reduce cardiovascular risk: The Task Force for the management of dyslipidaemias of the European Society of Cardiology (ESC) and European Atherosclerosis Society (EAS). Eur. Heart J. 2019, 41, 111–188. [Google Scholar] [CrossRef]
- Aguiar, C.; Vilaro, M.; Komen, J.; Catapano, A.L.; Ray, K.K. Predictors of lipid-lowering therapy intensification over 1 year of prospective follow-up in Europe: Insights from the SANTORINI study. Eur. Heart J. 2025, 46, ehaf784.3714. [Google Scholar] [CrossRef]
- Banach, M.; Surma, S.; Guzik, T.J.; Penson, P.E.; Blaha, M.J.; Pinto, F.J.; Sperling, L.S. Upfront lipid-lowering combination therapy in high cardiovascular risk patients: A route to effective atherosclerotic cardiovascular disease prevention. Cardiovasc. Res. 2025, 121, 851–859. [Google Scholar] [CrossRef]
- Monguillon, V.; Kelly, P.; O’Donoghue, M.L.; Park, J.-G.; Bohula, E.A.; Saver, J.L.; Atar, D.; Keech, A.C.; Sever, P.S.; Wang, H.; et al. Efficacy and Safety of Very Low Achieved LDL-Cholesterol in Patients with Prior Ischemic Stroke. Circulation 2025, 152. [Google Scholar] [CrossRef]
- Di Fusco, S.A.; Volpe, M.; Nardi, F.; Matteucci, A.; Aquilani, S.; Marino, G.; Aiello, A.; Colivicchi, F. Reducing LDL-Cholesterol to Very Low Levels: Sailing Between Established Benefits and Potential Risks. High Blood Press. Cardiovasc. Prev. 2025, 32, 139–149. [Google Scholar] [CrossRef]
- Pedro-Botet, J.; Pintó, X. LDL-cholesterol: The lower the better. Clin. Investig. Arter. 2019, 31, 16–27. [Google Scholar] [CrossRef]
- Mazur, M.; Kolarczyk-Haczyk, A.; Sochań, P.; Grajek, M.; Gąsior, M.; Rogala, M.; Kaźmierczak, P.; Jankowski, P.; Milewski, K.; Buszman, P.E.; et al. Analysis of secondary cardiac prevention in patients after myocardial infarction enrolled in the Coordinated Care Program in Patients after Myocardial Infarction (KOS-MI): A single-center experience. Postep. Kardiol. Interwencyjnej 2025, 21, 358–365. [Google Scholar] [CrossRef] [PubMed]
- Roth, G.A.; Mensah, G.A.; Johnson, C.O.; Addolorato, G.; Ammirati, E.; Baddour, L.M.; Barengo, N.C.; Beaton, A.Z.; Benjamin, E.J.; Benziger, C.P.; et al. Global Burden of Cardiovascular Diseases and Risk Factors, 1990–2019: Update From the GBD 2019 Study. J. Am. Coll. Cardiol. 2020, 76, 2982–3021. [Google Scholar] [CrossRef]
- KDIGO 2024 Clinical Practice Guideline for the Evaluation and Management of Chronic Kidney Disease. Kidney Int. 2024, 105, S117–S314. [CrossRef] [PubMed]
- Wanner, C.; Tonelli, M. KDIGO Clinical Practice Guideline for Lipid Management in CKD: Summary of recommendation statements and clinical approach to the patient. Kidney Int. 2014, 85, 1303–1309. [Google Scholar] [CrossRef] [PubMed]
- Dobrowolski, P.; Prejbisz, A.; Kuryłowicz, A.; Baska, A.; Burchardt, P.; Chlebus, K.; Dzida, G.; Jankowski, P.; Jaroszewicz, J.; Jaworski, P.; et al. Metabolic syndrome—A new definition and management guidelines. Arch. Med. Sci. 2022, 18, 1133–1156. [Google Scholar] [CrossRef]
- Sosnowska, B.; Stepinska, J.; Mitkowski, P.; Bielecka-Dabrowa, A.; Bobrowska, B.; Budzianowski, J.; Burchardt, P.; Chlebus, K.; Dobrowolski, P.; Gasior, M.; et al. Recommendations of the Experts of the Polish Cardiac Society (PCS) and the Polish Lipid Association (PoLA) on the diagnosis and management of elevated lipoprotein(a) levels. Arch. Med. Sci. 2024, 20, 8–27. [Google Scholar] [CrossRef]
- Greco, A.; Finocchiaro, S.; Spagnolo, M.; Faro, D.C.; Mauro, M.S.; Raffo, C.; Sangiorgio, G.; Imbesi, A.; Laudani, C.; Mazzone, P.M.; et al. Lipoprotein(a) as a Pharmacological Target: Premises, Promises, and Prospects. Circulation 2025, 151, 400–415. [Google Scholar] [CrossRef]
- Atal, S.; Joshi, R.; Misra, S.; Fatima, Z.; Sharma, S.; Balakrishnan, S.; Singh, P. Patterns of drug therapy, glycemic control, and predictors of escalation—Non-escalation of treatment among diabetes outpatients at a tertiary care center. J. Basic Clin. Physiol. Pharmacol. 2022, 33, 803–814. [Google Scholar] [CrossRef]
- Buchholz, C.; Kahle-Stephan, M.; Meier, J.J.; Nauck, M.A. Clinical Predictors of the Need for Further Treatment Escalation in Patients with Type 2 Diabetes on Basal Insulin Therapy—A Retrospective Observational Study. Exp. Clin. Endocrinol. Diabetes 2019, 127, 663–671. [Google Scholar] [CrossRef]
- Aronow, H.D.; Novaro, G.M.; Lauer, M.S.; Brennan, D.M.; Lincoff, A.M.; Topol, E.J.; Kereiakes, D.J.; Nissen, S.E. In-Hospital Initiation of Lipid-Lowering Therapy After Coronary Intervention as a Predictor of Long-term Utilization: A Propensity Analysis. Arch. Intern. Med. 2003, 163, 2576–2582. [Google Scholar] [CrossRef][Green Version]
- Makhmudova, U.; Samadifar, B.; Maloku, A.; Haxhikadrija, P.; Geiling, J.-A.; Römer, R.; Lauer, B.; Möbius-Winkler, S.; Otto, S.; Schulze, P.C.; et al. Intensive lipid-lowering therapy for early achievement of guideline-recommended LDL-cholesterol levels in patients with ST-elevation myocardial infarction (“Jena auf Ziel”). Clin. Res. Cardiol. 2023, 112, 1212–1219. [Google Scholar] [CrossRef]
- Merenich, J.A.; Lousberg, T.R.; Brennan, S.H.; Calonge, N.B. Optimizing treatment of dyslipidemia in patients with coronary artery disease in the managed-care environment (the Rocky Mountain Kaiser Permanente Experience). Am. J. Cardiol. 2000, 85, 36–42. [Google Scholar] [CrossRef] [PubMed]
- Kardas, P.; Kwiatek, A.; Włodarczyk, P.; Urbański, F.; Ciabiada-Bryła, B. Is the KOS-Zawał coordinated care program effective in reducing long-term cardiovascular risk in coronary artery disease patients in Poland? Insights from analysis of statin persistence in a nationwide cohort. Kardiol. Pol. 2024, 82, 852–860. [Google Scholar] [CrossRef] [PubMed]
- Wita, K.; Kułach, A.; Wita, M.; Wybraniec, M.T.; Wilkosz, K.; Polak, M.; Matla, M.; Maciejewski, Ł.; Fluder, J.; Kalańska-Łukasik, B.; et al. Managed Care after Acute Myocardial Infarction (KOS-zawał) reduces major adverse cardiovascular events by 45% in 3-month follow-up—Single-center results of Poland’s National Health Fund program of comprehensive post-myocardial infarction care. Arch. Med. Sci. 2020, 16, 551–558. [Google Scholar] [CrossRef]
- MacDougall, D.E.; Tybjærg-Hansen, A.; Knowles, J.W.; Stern, T.P.; Hartsuff, B.K.; McGowan, M.P.; Baum, S.J.; Wilemon, K.A.; Nordestgaard, B.G. Lipoprotein(a) and recurrent atherosclerotic cardiovascular events: The US Family Heart Database. Eur. Heart J. 2025, 46, ehaf297. [Google Scholar] [CrossRef] [PubMed]
- Saniewski, T.; Zimodro, J.M.; Procyk, G.; Wasilewska, O.; Mroczyk, B.; Lis, M.; Banach, M.; Gąsecka, A. Incorporating lipoprotein (a) into patient care: Polish landscape in light of national recommendations and the updated ESC/EAS guidelines. Arch. Med. Sci. 2025. [Google Scholar] [CrossRef]
- Ferrières, J.; Lautsch, D.; Gitt, A.K.; De Ferrari, G.; Toplak, H.; Elisaf, M.; Drexel, H.; Horack, M.; Baxter, C.; Ambegaonkar, B.; et al. Body mass index impacts the choice of lipid-lowering treatment with no correlation to blood cholesterol—Findings from 52,916 patients in the Dyslipidemia International Study (DYSIS). Diabetes Obes. Metab. 2018, 20, 2670–2674. [Google Scholar] [CrossRef]
- Banach, M.; Mastalerz-Migas, A.; Wita, K.; Myśliwiec, M. Poland Takes a Lead in Effective Lipid Disorders Management Healthcare Programmes in Europe. Am. J. Prev. Cardiol. 2025, 24, 101346. [Google Scholar] [CrossRef]
- Carratala-Munuera, C.; Gil-Guillen, V.F.; Orozco-Beltran, D.; Maiques-Galan, A.; Lago-Deibe, F.; Lobos-Bejarano, J.M.; Brotons-Cuixart, C.; Martin-Rioboo, E.; Alvarez-Guisasola, F.; Lopez-Pineda, A. Barriers to improved dyslipidemia control: Delphi survey of a multidisciplinary panel. Fam. Pract. 2015, 32, 672–680. [Google Scholar] [CrossRef][Green Version]
- Lopes, J.; Santos, P. Determinants of Non-Adherence to the Medications for Dyslipidemia: A Systematic Review. Patient Prefer. Adherence 2021, 15, 1853–1871. [Google Scholar] [CrossRef]
- Kiortsis, D.N.; Giral, P.; Bruckert, E.; Turpin, G. Factors associated with low compliance with lipid-lowering drugs in hyperlipidemic patients. J. Clin. Pharm. Ther. 2000, 25, 445–451. [Google Scholar] [CrossRef] [PubMed]
- Pallarés-Carratalá, V.; Barrios, V.; Fierro-González, D.; Polo-García, J.; Cinza-Sanjurjo, S. Cardiovascular Risk in Patients with Dyslipidemia and Their Degree of Control as Perceived by Primary Care Physicians in a Survey—TERESA-Opinion Study. Int. J. Environ. Res. Public Health 2023, 20, 2388. [Google Scholar] [CrossRef] [PubMed]
- van Wyk, J.T.; van Wijk, M.A.M.; Sturkenboom, M.C.J.M.; Mosseveld, M.; Moorman, P.W.; van der Lei, J. Electronic Alerts Versus On-Demand Decision Support to Improve Dyslipidemia Treatment. Circulation 2008, 117, 371–378. [Google Scholar] [CrossRef] [PubMed]
| Diseases with Specific Cardiovascular Risk | ||
|---|---|---|
| ||
| Risk modifiers | ||
| 2019 ESC/EAS Guidelines for the management of dyslipidaemias [5] | 2021 ESC Guidelines on cardiovascular disease prevention in clinical practice [3] | 2025 Focused Update of the 2019 ESC/EAS Guidelines for the management of dyslipidaemias [4] |
|
|
|
| Variable | Total n = 431 | Escalation of Lipid-Lowering Therapy n = 209 | No-Escalation of Lipid-Lowering Therapy n = 222 | Odds Ratio | 95% CI | p Value |
|---|---|---|---|---|---|---|
| Age [y.] | 69.00± 19.00 | 68.00 ± 15.00 | 69.50 ± 24.00 | 1.007 | 0.995–1.020 | 0.969 |
| Sex (male) | 45.01% (194) | 47.37% (99) | 42.79% (95) | 1.203 | 0.823–1.759 | 0.340 |
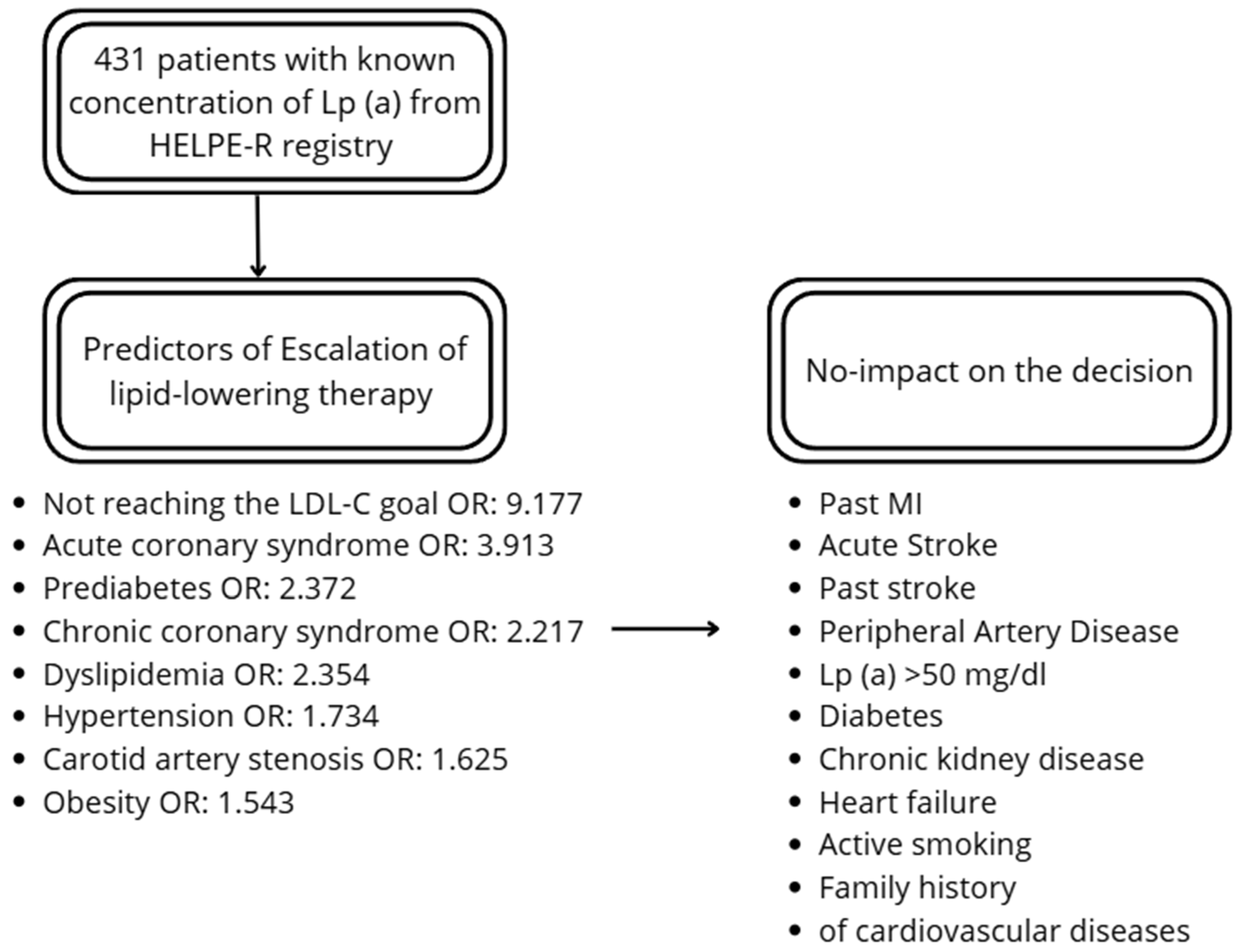
| Chronic coronary syndrome | 29.00% (125) | 37.32% (78) | 21.17% (47) | 2.217 | 1.447–3.398 | <0.001 |
| Acute coronary syndrome | 4.18% (18) | 6.70% (14) | 1.80% (4) | 3.913 | 1.267–12.087 | 0.018 |
| Past MI | 12.99% (56) | 12.92% (27) | 13.06% (29) | 0.987 | 0.563–1.732 | 0.964 |
| Acute stroke | 5.34% (23) | 6.70% (14) | 4.05% (9) | 1.699 | 0.719–4.014 | 0.227 |
| Past stroke | 9.74% (42) | 9.09% (19) | 10.36% (23) | 0.865 | 0.457–1.640 | 0.657 |
| PAD | 5.34% (23) | 6.22% (13) | 4.50% (10) | 1.406 | 0.603–3.280 | 0.430 |
| Carotid artery stenosis | 22.04% (95) | 26.32% (55) | 18.02% (40) | 1.625 | 1.026–2.575 | 0.039 |
| Hypertension | 75.17% (324) | 80.38% (168) | 70.27% (156) | 1.734 | 1.109–2.709 | 0.016 |
| Systolic blood pressure [mmHg] | 138.50 ± 2.72 | 138.00 ± 4.15 | 140.00 ± 2.86 | 0.991 | 0.956–1.029 | 0.657 |
| Diastolic blood pressure [mmHg] | 80.00 ± 2.07 | 80.00 ± 2.44 | 79.50 ± 3.75 | 0.998 | 0.951–1.048 | 0.949 |
| Dyslipidemia | 74.71% (322) | 82.78% (173) | 67.12% (149) | 2.354 | 1.493–3.712 | <0.001 |
| Lp (a) [mg/dL] | 13.80 ± 31.70 | 14.90 ± 34.10 | 12.20 ± 27.70 | 1.001 | 0.996–1.005 | 0.777 |
| Lp (a) > 50 mg/dL | 21.11% (91) | 21.05% (44) | 21.17% (47) | 0.993 | 0.625–1.577 | 0.976 |
| Lp (a) > 180 mg/dL | 1.86% (8) | 1.44% (3) | 2.25% (5) | 0.632 | 0.149–2.678 | 0.533 |
| TC [mg/dL] | 162.00 ± 68.00 | 176.00 ± 69.00 | 145.00 ± 59.00 | 1.015 | 1.011–1.020 | <0.001 |
| LDL-C [mg/dL] | 95.00 ± 61.00 | 112.00 ± 62.00 | 82.00 ± 45.00 | 1.021 | 1.015–1.027 | <0.001 |
| HDL-C [mg/dL] | 51.00 ± 20.00 | 50.00 ± 19.00 | 51.00 ± 20.00 | 0.999 | 0.987–1.010 | 0.818 |
| TG [mg/dL] | 106.00 ± 66.00 | 115.00 ± 73.00 | 99.00 ± 58.00 | 1.002 | 1.000–1.003 | 0.125 |
| Non-HDL-C [mg/dL] | 108.00 ± 59.00 | 122.00 ± 59.00 | 95.50 ± 47.00 | 1.018 | 1.013–1.023 | <0.001 |
| Distance from LDL-C goal | 31.00 ± 60.00 | 56.5 ± 63.00 | 12.00 ± 42.00 | 1.029 | 1.022–1.036 | <0.001 |
| Not-reached LDL-C goal | 77.49% (334) | 93.78% (196) | 62.16% (138) | 9.177 | 4.920–17.119 | <0.001 |
| Prediabetes | 7.89% (34) | 11.00% (23) | 4.95% (11) | 2.372 | 1.126–4.997 | 0.023 |
| Diabetes | 27.84% (120) | 27.75% (58) | 27.93% (62) | 0.991 | 0.650–1.510 | 0.967 |
| Glycemia | 102.00 ± 2.44 | 103.00 ± 2.57 | 99.5 ± 4.01 | 0.999 | 0.996–1.003 | 0.758 |
| HbA1C [%] | 5.6 ± 0.28 | 5.7 ± 0.13 | 5.6 ± 0.53 | 0.986 | 0.949–1.025 | 0.484 |
| Obesity | 31.55% (136) | 36.36% (76) | 27.03% (60) | 1.543 | 1.025–2.322 | 0.038 |
| BMI | 28.63 ±0.28 | 29.76 ± 0.44 | 28.29 ± 0.36 | 1.042 | 1.005–1.081 | 0.027 |
| Chronic kidney disease | 24.36% (105) | 23.44% (49) | 25.23% (56) | 0.908 | 0.584–1.411 | 0.667 |
| GFR [mL/min] | 81.00 ± 1.51 | 81.00 ± 1.87 | 81.00 ± 231 | 0.998 | 0.992–1.003 | 0.392 |
| Heart failure | 41.53% (179) | 42.58% (89) | 40.54% (90) | 1.088 | 0.741–1.596 | 0.667 |
| NT-pro BNP [pg/mL] | 350.70 ± 116.75 | 340.65 ± 163.60 | 359.15 ± 166.39 | 1.000 | 0.999–1.000 | 0.941 |
| LVEF [%] | 55.00 ± 0.87 | 55.00 ± 1.38 | 55.00 ± 1.07 | 0.985 | 0.956–1.015 | 0.329 |
| Atrial fibrillation | 33.87% (146) | 30.14% (63) | 37.39% (83) | 0.7226 | 0.484–1.080 | 0.1128 |
| Asthma | 4.87% (21) | 5.26% (11) | 4.50% (10) | 1.1778 | 0.490–2.833 | 0.7149 |
| COPD | 6.03% (26) | 7.66% (16) | 4.50% (10) | 1.7575 | 0.779–3.966 | 0.1744 |
| Active smoking | 14.85% (64) | 16.75% (35) | 13.06% (29) | 1.339 | 0.786–2.281 | 0.284 |
| History of smoking | 29.93% (129) | 33.97% (71) | 26.13% (58) | 1.455 | 0.961–2.201 | 0.076 |
| Family history of cardiovascular diseases | 33.64% (145) | 34.93% (73) | 32.43% (72) | 1.118 | 0.750–1.668 | 0.584 |
| Age at the first episode [y.] | 62.00 ± 24.00 | 62.00 ± 21.00 | 66.00 ± 26.00 | 0.974 | 0.936–1.014 | 0.990 |
| Premature Cardiovascular disease (M < 55 y., F < 60 y.) | 11.60% (50) | 10.53% (22) | 12.61% (28) | 0.815 | 0.450–1.476 | 0.500 |
| Total n = 431 | Escalation of Lipid-Lowering Therapy n = 209 | No Escalation of Lipid-Lowering Therapy n = 222 | p Value | |
|---|---|---|---|---|
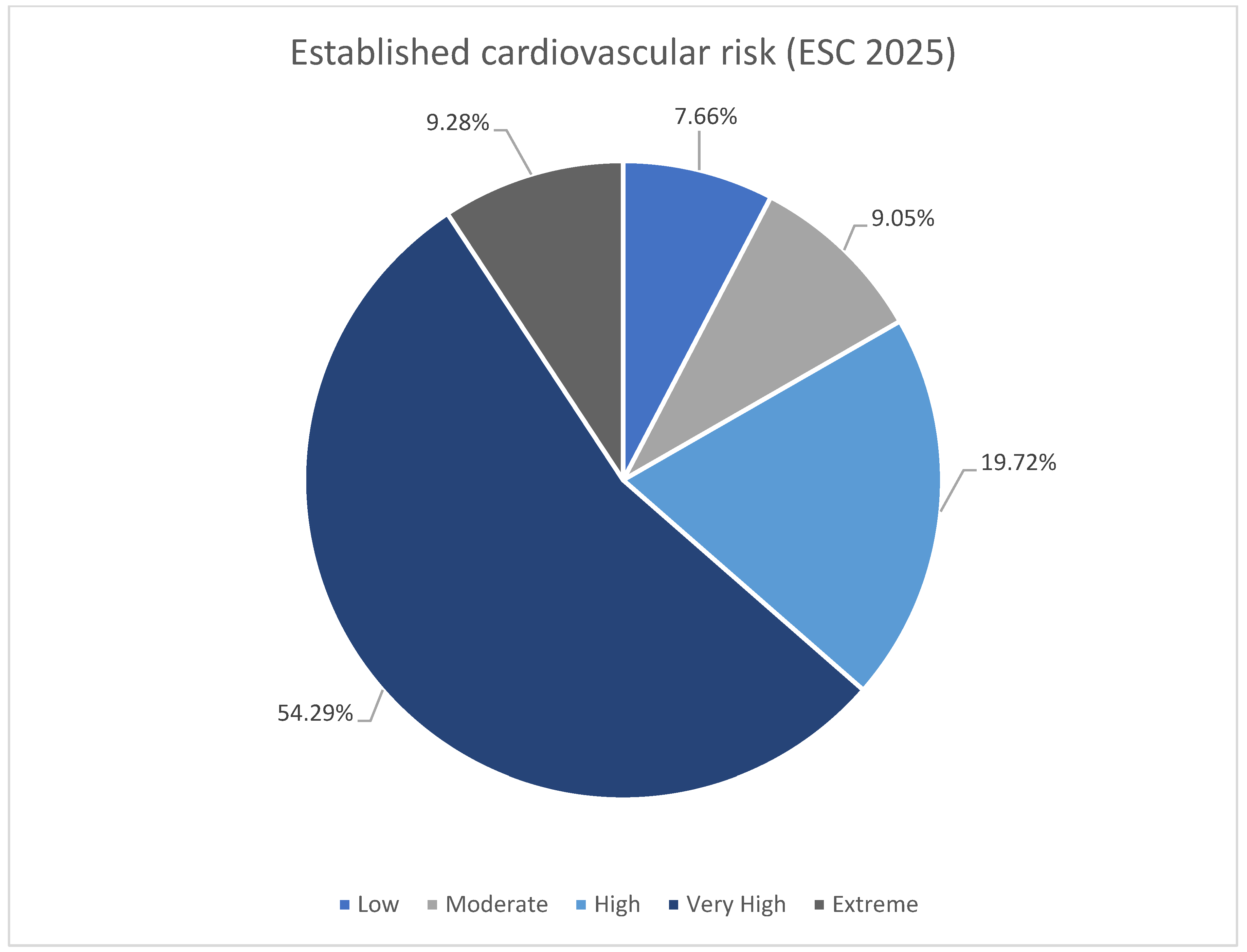
| Low cardiovascular risk | 7.66% (33) | 2.39% (5) | 12.61% (28) | <0.001 |
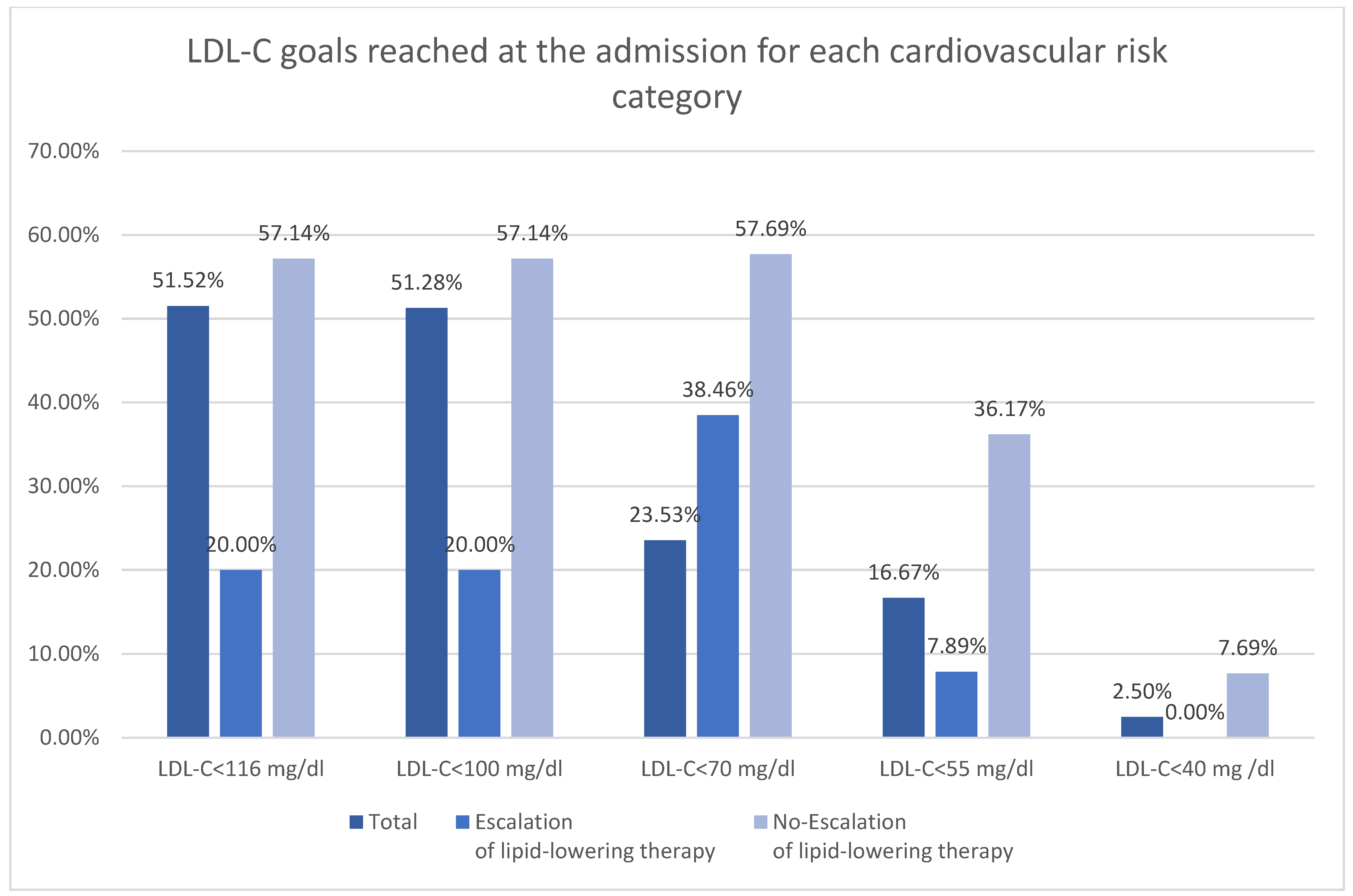
| Reached specific LDL-C goal for low risk (<116 mg/dL) | 51.52% (17) | 20.00% (1) | 57.14% (16) | 0.125 |
| Moderate cardiovascular risk | 9.05% (39) | 6.22% (13) | 11.71% (26) | 0.047 |
| Reached specific LDL-C goal for moderate risk (<100 mg/dL) | 51.28% (20) | 38.46% (5) | 57.69% (15) | 0.257 |
| High cardiovascular risk | 19.72% (85) | 18.18% (38) | 21.17% (47) | 0.436 |
| Reached specific LDL-C goal for High risk (LDL-C < 70 mg/dL) | 23.53% (20) | 7.89% (3) | 36.17% (17) | 0.002 |
| Very high cardiovascular risk | 54.29% (234) | 59.81% (125) | 49.10% (109) | 0.026 |
| Reached specific LDL-C goal for very high risk (<55 mg/dL) | 16.67% (39) | 2.40% (3) | 33.03% (36) | <0.001 |
| Extreme cardiovascular risk | 9.28% (40) | 12.92% (27) | 5.86% (13) | 0.012 |
| Reached specific LDL-C goal for extreme risk (<40 mg/dL) | 2.50% (1) | 0.00% (0) | 7.69% (1) | 0.144 |
| Variable | Odds Ratio | 95% CI | p Value |
|---|---|---|---|
| LDL-C > 100 mg/dL | |||
| Lp (a) | 0.997 | 0.991–1.004 | 0.478 |
| TC | 1.005 | 0.997–1.013 | 0.247 |
| LDL-C | 1.007 | 0.997–1.017 | 0.180 |
| HDL-C | 0.990 | 0.972–1.008 | 0.264 |
| TG | 1.004 | 0.999–1.009 | 0.086 |
| Non-HDL-C | 1.007 | 0.998–1.015 | 0.117 |
| LDL-C > 70 mg/dL | |||
| Lp (a) | 1.001 | 0.995–1.006 | 0.769 |
| TC | 1.011 | 1.005–1.016 | <0.001 |
| LDL-C | 1.015 | 1.008–1.022 | <0.001 |
| HDL-C | 0.989 | 0.976–1.003 | 0.125 |
| TG | 1.005 | 1.001–1.0091 | 0.008 |
| Non-HDL-C | 1.014 | 1.007–1.021 | <0.001 |
| LDL-C > 55 mg/dL | |||
| Lp (a) | 1.001 | 0.996–1.006 | 0.689 |
| TC | 1.011 | 1.006–1.016 | <0.001 |
| LDL-C | 1.016 | 1.009–1.022 | <0.001 |
| HDL-C | 0.991 | 0.979–1.003 | 0.156 |
| TG | 1.001 | 0.999–1.003 | 0.212 |
| Non-HDL-C | 1.014 | 1.008–1.019 | <0.001 |
| Not within target LDL-C goal | |||
| Lp (a) | 1.000 | 0.995–1.005 | 0.951 |
| TC | 1.011 | 1.005–1.016 | <0.001 |
| LDL-C | 1.014 | 1.009–1.021 | <0.001 |
| HDL-C | 0.980 | 0.938–1.024 | 0.359 |
| TG | 1.001 | 0.999–1.002 | 0.399 |
| Non-HDL-C | 1.012 | 1.007–1.018 | <0.001 |
| Pharmacotherapy | Initial Treatment | Discharge Treatment | p Value |
|---|---|---|---|
| Statin | 45.94% (198) | 74.71% (322) | <0.001 |
| Simvastatin | 1.86% (8) | 0.23% (1) | 0.019 |
| Pitavastatin | 0.70% (3) | 2.09% (9) | 0.081 |
| Rosuvastatin | 23.20% (100) | 40.60% (175) | <0.001 |
| Atorvastatin | 20.19% (87) | 31.79% (137) | <0.001 |
| Low-to-moderate intensity statin | 26.68% (115) | 32.95% (142) | 0.044 |
| Simvastatin 20 mg | 1.39% (6) | 0.23% (1) | 0.058 |
| Simvastatin 40 mg | 0.46% (2) | 0.00% (0) | 0.157 |
| Pitavastatin 2 mg | 0.46% (2) | 1.62% (7) | 0.094 |
| Pitavastatin 4 mg | 0.23% (1) | 0.46% (2) | 0.563 |
| Rosuvastatin 5–15 mg | 9.28% (40) | 12.06% (52) | 0.185 |
| Atorvastatin 10–30 mg | 14.85% (64) | 18.56% (80) | 0.144 |
| High-intensity statin | 19.26% (83) | 41.76% (180) | <0.001 |
| Rosuvastatin 20–40 mg | 13.92% (60) | 28.54% (123) | <0.001 |
| Atorvastatin 40–80 mg | 5.34% (23) | 13.23% (57) | <0.001 |
| Ezetimibe | 7.89% (34) | 14.15% (61) | 0.003 |
| Ezetimibe and statin | 6.26% (27) | 12.76% (55) | 0.001 |
| PCSK-9i | 0.46% (2) | 1.39% (6) | 0.155 |
| Statin, ezetimibe, and PCSK-9i) | 0.23% (1) | 0.93% (4) | 0.178 |
| Fibrate | 2.78% (12) | 3.48% (15) | 0.558 |
| Pharmacotherapy | Within LDL-C Goal n = 97 | Not within LDL-C Goal n = 334 | p Value |
|---|---|---|---|
| Statin | 62.89% (61) | 41.02% (137) | <0.001 |
| Simvastatin | 1.03% (1) | 2.10% (7) | 0.494 |
| Pitavastatin | 0.00% (0) | 0.90% (3) | 0.349 |
| Rosuvastatin | 35.05% (34) | 19.76% (66) | 0.002 |
| Atorvastatin | 26.80% (26) | 18.26% (61) | 0.065 |
| Low-to-moderate intensity statin | 36.08% (35) | 23.95% (80) | 0.017 |
| Simvastatin 20 mg | 0.00% (0) | 1.80% (6) | 0.183 |
| Simvastatin 40 mg | 1.03% (1) | 0.30% (1) | 0.351 |
| Pitavastatin 2 mg | 0.00% (0) | 0.60% (2) | 0.445 |
| Pitavastatin 4 mg | 0.00% (0) | 0.30% (1) | 0.590 |
| Rosuvastatin 5–15 mg | 14.43% (14) | 7.78% (26) | 0.047 |
| Atorvastatin 10–30 mg | 20.62% (20) | 13.17% (44) | 0.069 |
| High-intensity statin | 26.80% (26) | 17.07% (57) | 0.032 |
| Rosuvastatin 20–40 mg | 20.62% (20) | 11.98% (40) | 0.030 |
| Atorvastatin 40–80 mg | 6.19% (6) | 5.09% (17) | 0.672 |
| Ezetimibe | 13.40% (13) | 6.29% (21) | 0.022 |
| Ezetimibe and statin | 12.37% (12) | 4.49% (15) | 0.005 |
| PCSK-9i | 1.03% (1) | 0.30% (1) | 0.351 |
| Statin, ezetimibe, and PCSK-9i) | 1.03% (1) | 4.49% (0) | 0.063 |
| Fibrate | 2.06% (2) | 2.99% (10) | 0.623 |
| Pharmacotherapy | Low Risk n = 33 | Moderate Risk n = 39 | High Risk n = 85 | Very High Risk n = 234 | Extreme Risk n = 40 | p Value |
|---|---|---|---|---|---|---|
| Statin | 21.21% (7) | 48.72% (19) | 76.47% (65) | 83.33% (195) | 90.00% (36) | <0.001 |
| Simvastatin | 0.00% (0) | 0.00% (0) | 0.00% (0) | 0.43% (1) | 0.00% (0) | 0.932 |
| Pitavastatin | 0.00% (0) | 5.13% (2) | 0.00% (0) | 2.14% (5) | 5.00% (2) | 0.204 |
| Rosuvastatin | 9.09% (3) | 23.08% (9) | 35.29% (30) | 47.01% (110) | 57.50% (23) | <0.001 |
| Atorvastatin | 12.12% (4) | 20.51% (8) | 41.18% (35) | 33.76% (79) | 27.50% (11) | 0.015 |
| Low-to-moderate intensity statin | 18.18% (6) | 33.33% (13) | 40.00% (34) | 32.91% (77) | 30.00% (12) | 0.255 |
| Simvastatin 20 mg | 0.00% (0) | 0.00% (0) | 0.00% (0) | 0.43% (1) | 0.00% (0) | 0.932 |
| Simvastatin 40 mg | 0.00% (0) | 0.00% (0) | 0.00% (0) | 0.00% (0) | 0.00% (0) | 1.000 |
| Pitavastatin 2 mg | 0.00% (0) | 5.13% (2) | 0.00% (0) | 1.28% (3) | 5.00% (2) | 0.093 |
| Pitavastatin 4 mg | 0.00% (0) | 0.00% (0) | 0.00% (0) | 0.85% (2) | 0.00% (0) | 0.792 |
| Rosuvastatin 5–15 mg | 6.06% (2) | 10.26% (4) | 15.29% (13) | 12.39% (29) | 10.00% (4) | 0.688 |
| Atorvastatin 10–30 mg | 12.12% (4) | 17.95% (7) | 24.71% (21) | 17.95% (42) | 15.00% (6) | 0.488 |
| High-intensity statin | 3.03% (1) | 15.38% (6) | 36.47% (31) | 50.43% (118) | 60.00% (24) | <0.001 |
| Rosuvastatin 20–40 mg | 3.03% (1) | 12.82% (5) | 20.00% (17) | 34.62% (81) | 47.50% (19) | <0.001 |
| Atorvastatin 40–80 mg | 0.00% (0) | 2.56% (1) | 16.47% (14) | 15.81% (37) | 12.50% (5) | 0.026 |
| Ezetimibe | 0.00% (0) | 2.56% (1) | 5.88% (5) | 14.96% (35) | 50.00% (20) | <0.001 |
| Ezetimibe and statin | 0.00% (0) | 2.56% (1) | 4.71% (4) | 14.53% (34) | 40.00% (16) | <0.001 |
| PCSK-9i | 0.00% (0) | 0.00% (0) | 0.00% (0) | 0.85% (2) | 10.00% (4) | <0.001 |
| Triple therapy (statin, ezetimibe, and PCSK-9i) | 0.00% (0) | 0.00% (0) | 0.00% (0) | 0.43% (1) | 7.50% (3) | <0.001 |
| Fibrate | 3.03% (1) | 2.56% (1) | 4.71% (4) | 2.99% (7) | 2.50% (1) | 0.944 |
| Escalation of Lipid-Lowering Therapy | Total 48.49% n = 209 | Distance to LDL-C Goal < 50 mg/dL n = 92 | Distance to LDL-C Goal ≥ 50 mg/dL n = 117 | p Value |
|---|---|---|---|---|
| Statin initiation | 39.71% (83) | 53.26% (49) | 29.06% (34) | <0.001 |
| Dose increasing | 26.32% (55) | 38.04% (35) | 17.09% (20) | <0.001 |
| Low-to-moderate into high intensity statin | 2.87% (6) | 2.17% (2) | 3.42% (4) | 0.593 |
| Ezetimibe initiation | 12.92% (27) | 9.78% (9) | 15.38% (18) | 0.231 |
| Up-front, combined lipid therapy (statin and ezetimibe) | 5.26% (11) | 1.09% (1) | 8.55% (10) | 0.017 |
| PCSK-9i initiation | 1.91% (4) | 0.00% (0) | 3.42% (4) | 0.073 |
| Fibrate initiation | 1.91% (4) | 1.09% (1) | 2.56% (3) | 0.439 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license.
Share and Cite
Muszyński, P.; Dudzińska, K.N.; Święcicka, M.; Grądzka-Matys, W.; Chlabicz, M.; Musiałowska, D.; Kruszyńska, J.; Kazberuk, P.; Bajda, U.; Tomaszuk-Kazberuk, A. Predictors of Escalation of Lipid-Lowering Therapy with Subanalysis of the Influence of Lipoprotein (a) on the Decision-Making Process. Diseases 2026, 14, 8. https://doi.org/10.3390/diseases14010008
Muszyński P, Dudzińska KN, Święcicka M, Grądzka-Matys W, Chlabicz M, Musiałowska D, Kruszyńska J, Kazberuk P, Bajda U, Tomaszuk-Kazberuk A. Predictors of Escalation of Lipid-Lowering Therapy with Subanalysis of the Influence of Lipoprotein (a) on the Decision-Making Process. Diseases. 2026; 14(1):8. https://doi.org/10.3390/diseases14010008
Chicago/Turabian StyleMuszyński, Paweł, Kinga Natalia Dudzińska, Marlena Święcicka, Wiktoria Grądzka-Matys, Małgorzata Chlabicz, Dominika Musiałowska, Joanna Kruszyńska, Piotr Kazberuk, Urszula Bajda, and Anna Tomaszuk-Kazberuk. 2026. "Predictors of Escalation of Lipid-Lowering Therapy with Subanalysis of the Influence of Lipoprotein (a) on the Decision-Making Process" Diseases 14, no. 1: 8. https://doi.org/10.3390/diseases14010008
APA StyleMuszyński, P., Dudzińska, K. N., Święcicka, M., Grądzka-Matys, W., Chlabicz, M., Musiałowska, D., Kruszyńska, J., Kazberuk, P., Bajda, U., & Tomaszuk-Kazberuk, A. (2026). Predictors of Escalation of Lipid-Lowering Therapy with Subanalysis of the Influence of Lipoprotein (a) on the Decision-Making Process. Diseases, 14(1), 8. https://doi.org/10.3390/diseases14010008