A Comprehensive Review of Candidemia and Invasive Candidiasis in Adults: Focus on the Emerging Multidrug-Resistant Fungus Candida auris
Abstract
1. Methodology
2. Introduction
3. Epidemiology
Epidemiology of Candida auris
4. Risk Factors for Candidemia
4.1. Intensive Care
4.2. Immunosuppression
4.3. COVID-19-Associated Candidemia
4.4. Intravenous Drug Use (IVDU)
4.5. Host Factors
4.6. Risk Factors for C. auris Infection
5. Pathogenesis
6. Clinical Evaluation
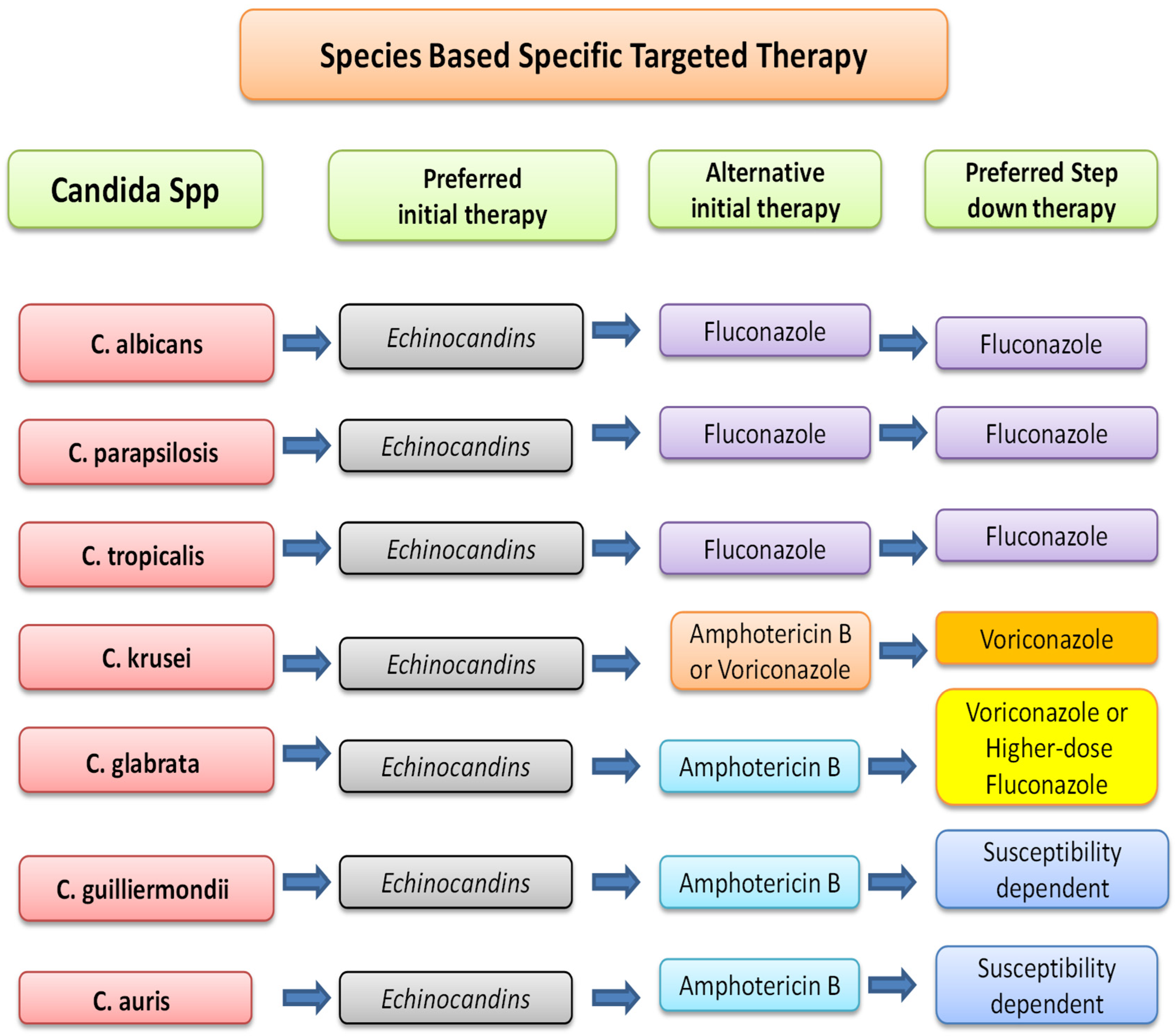
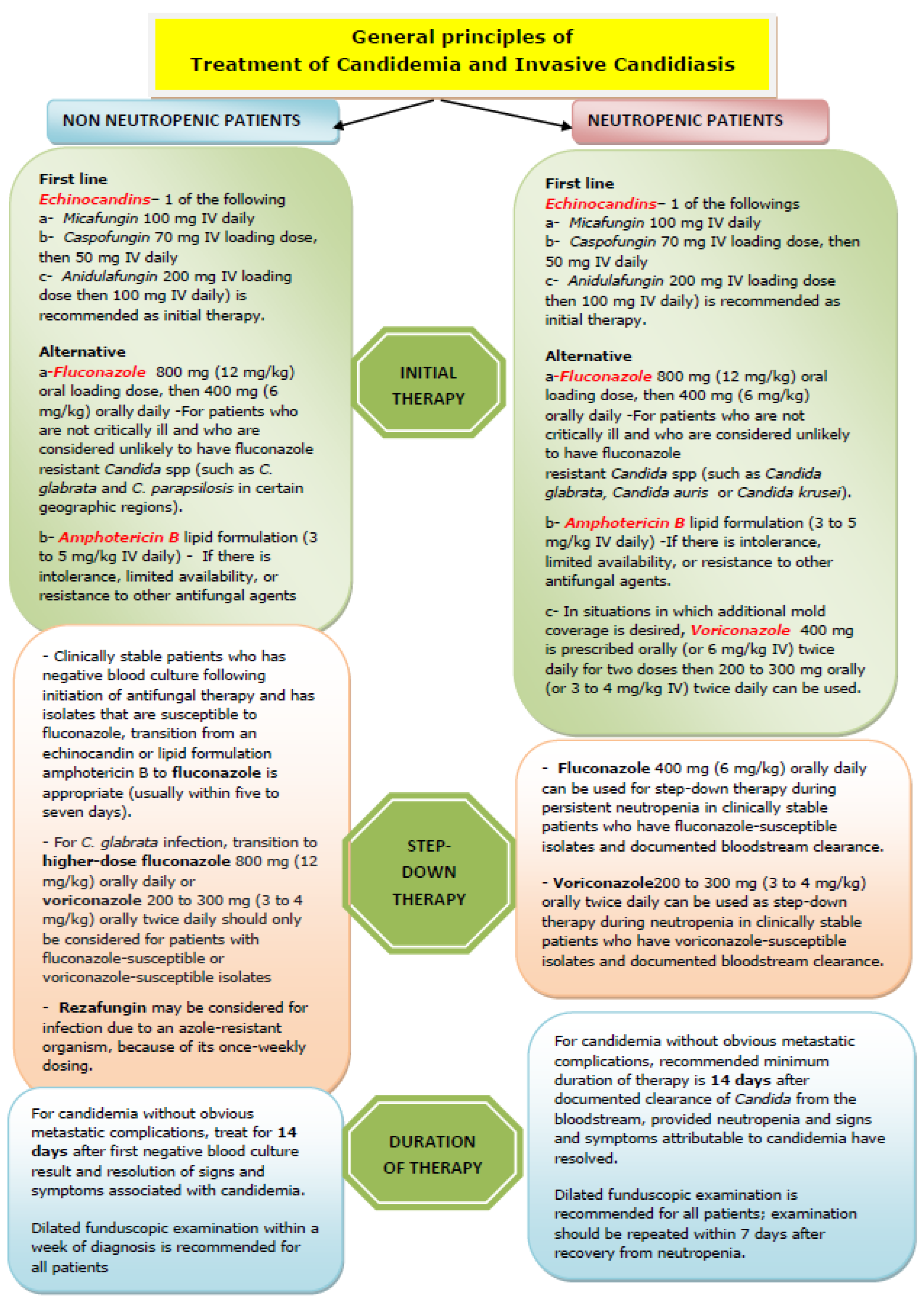
7. Management of Candidemia and Invasive Candidiasis
8. Diagnosis and Management Challenges of Multidrug-Resistant Candida auris Infection
8.1. Diagnostic Challenges of C. auris
8.2. Treatment Challenges of C. auris
8.3. Colonization of C. auris
- Maintain high standards of care for central and peripheral lines, urinary catheters, and tracheostomies.
- Promptly remove venous cannulas at the first sign of infection.
- Adhere to strict aseptic techniques for wound care.
- Use chlorhexidine washes for skin decontamination in critically ill patients.
8.4. Screening for C. auris
- Groin and axilla;
- Urine;
- Nose and throat;
- Perineal swab;
- Rectal swab or stool sample.
8.5. Infection Prevention and Control (IPC) for C. auris
9. Conclusions
Author Contributions
Funding
Conflicts of Interest
References
- Pappas, P.G.; Kauffman, C.A.; Andes, D.R.; Clancy, C.J.; Marr, K.A.; Ostrosky-Zeichner, L.; Reboli, A.C.; Schuster, M.G.; Vazquez, J.A.; Walsh, T.J.; et al. Clinical practice guideline for the management of candidiasis: 2016 update by the Infectious Diseases Society of America. Clin. Infect. Dis. 2016, 62, e1–e50. [Google Scholar] [PubMed]
- Centers for Disease Control and Prevention. Clinical Alert to U.S. Healthcare Facilities—Global Emergence of Invasive Infections Caused by the Multidrug-Resistant Yeast Candida auris. Available online: https://www.cdc.gov/fungal/candida-auris/candida-auris-alert.html (accessed on 1 December 2024).
- Public Health England. Candida auris identified in England. Available online: https://www.gov.uk/government/publications/candida-auris-emergence-in-england/candida-auris-identified-in-england (accessed on 1 December 2024).
- Kathuria, S.; Singh, P.K.; Sharma, C.; Prakash, A.; Masih, A.; Kumar, A.; Meis, J.F.; Chowdhary, A. Multidrug-Resistant Candida auris Misidentified as Candida haemulonii: Characterization by Matrix-Assisted Laser Desorption Ionization-Time of Flight Mass Spectrometry and DNA Sequencing and Its Antifungal Susceptibility Profile Variability by Vitek 2, CLSI Broth Microdilution, and Etest Method. J. Clin. Micro. 2015, 53, 1823–1830. [Google Scholar]
- Bongomin, F.; Gago, S.; Oladele, R.O.; Denning, D.W. Global and multi-national prevalence of fungal diseases—Estimateprecision. J. Fungi. 2017, 4, 57. [Google Scholar]
- Tsay, S.V.; Mu, Y.; Williams, S.; Epson, E.; Nadle, J.; Bamberg, W.M.; Barter, D.M.; Johnston, H.L.; Farley, M.M.; Harb, S.; et al. Burden of Candidemia in the United States, 2017. Clin. Infect. Dis. 2020, 71, e449–e453. [Google Scholar] [CrossRef]
- Toda, M.; Williams, S.R.; Berkow, E.L.; Farley, M.M.; Harrison, L.H.; Bonner, L.; Marceaux, K.M.; Hollick, R.; Zhang, A.Y.; Schaffner, W.; et al. Population-Based Active Surveillance for Culture-Confirmed Candidemia—Four Sites, United States, 2012–2016. MMWR Surveill. Summ. 2019, 68, 1–15. [Google Scholar] [CrossRef]
- Samra, Z.; Yardeni, M.; Peled, N.; Bishara, J. Species distribution and antifungal susceptibility of Candida bloodstream isolates in a tertiary medical center in Israel. Eur. J. Clin. Microbiol. Infect. Dis. 2005, 24, 592–595. [Google Scholar] [CrossRef]
- Zhong, L.; Zhang, S.; Tang, K.; Zhou, F.; Zheng, C.; Zhang, K.; Cai, J.; Zhou, H.; Wang, Y.; Tian, B.; et al. Clinical characteristics, risk factors and outcomes of mixed Candida albicans/bacterial bloodstream infections. BMC Infect. Dis. 2020, 20, 810. [Google Scholar] [CrossRef]
- Satoh, K.; Makimura, K.; Hasumi, Y.; Nishiyama, Y.; Uchida, K.; Yamaguchi, H. Candida aurissp. nov., a novel ascomycetous yeast isolated from the external ear canal of an inpatient in a Japanese hospital. Microbiol. Immunol. 2009, 53, 41–44, Erratum in Microbiol. Immunol. 2018, 62, 205. [Google Scholar] [CrossRef]
- Lee, W.G.; Shin, J.H.; Uh, Y.; Kang, M.G.; Kim, S.H.; Park, K.H.; Jang, H.-C. First three reported cases of nosocomial fungemia caused by Candida auris. J. Clin. Micro. 2011, 49, 3139–3142. [Google Scholar]
- Centers for Disease Control and Prevention. Tracking Candida auris. Updated 2023. Available online: https://www.cdc.gov/fungal/candida-auris/tracking-c-auris.html (accessed on 1 December 2024).
- Kilburn, S.; Innes, G.; Quinn, M.; Southwick, K.; Ostrowsky, B.; Greenko, J.A.; Lutterloh, E.; Greeley, R.; Magleby, R.; Chaturvedi, V.; et al. Antifungal Resistance Trends of Candida auris Clinical Isolates in New York and New Jersey from 2016 to 2020. Antimicrob. Agents Chemother. 2022, 66, e0224221. [Google Scholar]
- Eyre, D.W.; Sheppard, A.E.; Madder, H.; Moir, I.; Moroney, R.; Quan, P.; Griffiths, D.; George, S.; Butcher, L.; Morgan, M.; et al. A Candida auris Outbreak and Its Control in an Intensive Care Setting. N. Engl. J. Med. 2018, 379, 1322–1331. [Google Scholar] [CrossRef] [PubMed]
- Govender, N.P.; Magobo, R.E.; Mpembe, R.; Mhlanga, M.; Matlapeng, P.; Corcoran, C.; Govind, C.; Lowman, W.; Senekal, M.; Thomas, J. Candida auris in South Africa, 2012–2016. Emerg. Infect. Dis. 2018, 24, 2036–2040. [Google Scholar] [CrossRef] [PubMed]
- Ali, U.; Tareen, H.K.; Sarfraz, Z.; Safraz, A.; Bano, S. Act Now: The Global Threat of Candida Auris and the Urgent Need for Effective Countermeasures. J. Community Hosp. Intern. Med. Perspect. 2024, 14, 22–123. [Google Scholar] [CrossRef]
- Thomas-Rüddel, D.O.; Schlattmann, P.; Pletz, M.; Kurzai, O.; Bloos, F. Risk Factors for Invasive Candida Infection in Critically Ill Patients. Chest 2021, 161, 345–355. [Google Scholar] [CrossRef] [PubMed]
- Kullberg, B.J.; Arendrup, M.C. Invasive candidiasis. N. Engl. J. Med. 2015, 373, 1445–1456. [Google Scholar] [CrossRef]
- Soriano, A.; Honore, P.M.; Puerta-Alcalde, P.; Garcia-Vidal, C.; Pagotto, A.; Gonçalves-Bradley, D.C.; E Verweij, P. Invasive candidiasis: Current clinical challenges and unmet needs in adult populations. J. Antimicrob. Chemother. 2023, 78, 1569–1585. [Google Scholar] [CrossRef]
- Zhang, A.Y.; Shrum, S.; Williams, S.; Petnic, S.; Nadle, J.; Johnston, H.; Barter, D.; Vonbank, B.; Bonner, L.; Hollick, R.; et al. The Changing Epidemiology of Candidemia in the United States: Injection Drug Use as an Increasingly Common Risk Factor-Active Surveillance in Selected Sites, United States, 2014–2017. Clin. Infect. Dis. 2020, 71, 1732–1737. [Google Scholar] [CrossRef]
- Johnson, M.D.; Plantinga, T.S.; van de Vosse, E.; Edwards, D.R.V.; Smith, P.B.; Alexander, B.D.; Yang, J.C.; Kremer, D.; Laird, G.M.; Oosting, M.; et al. Cytokine gene polymorphisms and the outcome of invasive candidiasis: A prospective cohort study. Clin. Infect. Dis. 2011, 54, 502–510. [Google Scholar] [CrossRef]
- Gaziano, R.; Sabbatini, S.; Monari, C. The Interplay between Candida albicans, Vaginal Mucosa, Host Immunity and Resident Microbiota in Health and Disease: An Overview and Future Perspectives. Microorganisms 2023, 11, 1211. [Google Scholar] [CrossRef]
- Ahmad, S.; Alfouzan, W. Candida auris: Epidemiology, Diagnosis, Pathogenesis, Antifungal Susceptibility, and Infection Control Measures to Combat the Spread of Infections in Healthcare Facilities. Microorganisms 2021, 9, 807. [Google Scholar] [CrossRef]
- Cole, G.T.; Halawa, A.A.; Anaissie, E.J. The Role of the Gastrointestinal Tract in Hematogenous Candidiasis: From the Laboratory to the Bedside. Clin. Infect. Dis. 1996, 22, S73–S88. [Google Scholar] [CrossRef]
- Cavalheiro, M.; Teixeira, M.C. Candida Biofilms: Threats, Challenges, and Promising Strategies. Front. Med. 2018, 5, 28. [Google Scholar] [CrossRef]
- Hillenbrand, M.; Mendy, A.; Patel, K.; Wilkinson, R.; Liao, S.; Robertson, J.; Apewokin, S. The Incidence of Ocular Complications in Candidemic Patients and Implications for the Practice of Routine Eye Exams. Open Form. Infect. Dis. 2022, 9, ofac045. [Google Scholar]
- Garnacho-Montero, J.; Díaz-Martín, A.; García-Cabrera, E.; de Pipaón, M.R.P.; Hernández-Caballero, C.; Lepe-Jiménez, J.A. Impact on hospital mortality of catheter removal and adequate antifungal therapy in Candida spp. bloodstream infections. J. Antimicrob. Chemother. 2012, 68, 206–213. [Google Scholar] [CrossRef]
- Morrell, M.; Fraser, V.J.; Kollef, M.H. Delaying the empiric treatment of candida bloodstream infection until positive blood culture results are obtained: A potential risk factor for hospital mortality. Antimicrob. Agents Chemother. 2005, 49, 3640–3645. [Google Scholar]
- Cornely, O.A.; Bassetti, M.; Calandra, T.; Garbino, J.; Kullberg, B.J.; Lortholary, O.; Meersseman, W.; Akova, M.; Arendrup, M.C.; Arikan-Akdagli, S.; et al. ESCMID* guideline for the diagnosis and management of Candida diseases 2012: Non-neutropenic adult patients. Clin. Micro Infect. 2012, 18 (Suppl. 7), 19–37. [Google Scholar]
- Abdolrasouli, A.; Fraser, M.A. Candida auris Identification and Profiling by MALDI-ToF Mass Spectrometry. Methods Mol. Biol. 2022, 2517, 21–32. [Google Scholar] [CrossRef] [PubMed]
- Lockhart, S.R.; Etienne, K.A.; Vallabhaneni, S.; Farooqi, J.; Chowdhary, A.; Govender, N.P.; Colombo, A.L.; Calvo, B.; Cuomo, C.A.; Desjardins, C.A.; et al. Simultaneous Emergence of Multidrug-Resistant Candida auris on 3 Continents Confirmed by Whole-Genome Sequencing and Epidemiological Analyses. Clin. Infect. Dis. 2017, 64, 134–140. [Google Scholar] [CrossRef]
- Spivak, E.S.; Hanson, K.E. Candida auris: An Emerging Fungal Pathogen. J. Clin. Microbiol. 2018, 56. [Google Scholar] [CrossRef]
- Jeffery-Smith, A.; Taori, S.K.; Schelenz, S.; Jeffery, K.; Johnson, E.M.; Borman, A.; Manuel, R.; Brown, C.S. Candida auris: A Review of the Literature. Clin Micro Rev. 2017, 31, e00029-17. [Google Scholar] [CrossRef]
- Lyman, M.; Forsberg, K.; Reuben, J.; Dang, T.; Free, R.; Seagle, E.E.; Sexton, D.J.; Soda, E.; Jones, H.; Hawkins, D.; et al. Notes from the Field: Transmission of Pan-Resistant and Echinocandin-Resistant Candida auris in Health Care Facilities—Texas and the District of Columbia, January–April 2021. MMWR Morb. Mortal. Wkly. Rep. 2021, 70, 996–999. [Google Scholar] [CrossRef]
- CDC. Antifungal Susceptibility Testing for C. auris. Available online: https://www.cdc.gov/fungal/candida-auris/c-auris-antifungal.html (accessed on 1 December 2024).
- Jones, C.R.; Neill, C.; Borman, A.M.; Budd, E.L.; Cummins, M.; Fry, C.; Guy, R.L.; Jeffery, K.; Johnson, E.M.; Manuel, R.; et al. The laboratory investigation, management, and infection prevention and control of Candida auris: A narrative review to inform the2024 national guidance update in England. J. Med. Micro. 2024, 73, 001820. [Google Scholar] [CrossRef]
- Ostrowsky, B.; Greenko, J.; Adams, E.; Quinn, M.; O’Brien, B.; Chaturvedi, V.; Berkow, E.; Vallabhaneni, S.; Forsberg, K.; Chaturvedi, S.; et al. Candida auris Isolates Resistant to Three Classes of Antifungal Medications—New York, 2019. MMWR Morb. Mortal. Wkly. Rep. 2020, 69, 6–9. [Google Scholar] [CrossRef]
- Szekely, A.; Johnson, E.M.; Warnock, D.W. Comparison of E-Test and Broth Microdilution Methods for Antifungal Drug Susceptibility Testing of Molds. J. Clin. Microbiol. 1999, 37, 1480–1483. [Google Scholar] [CrossRef]
- Arendrup, M.C.; Prakash, A.; Meletiadis, J.; Sharma, C.; Chowdhary, A. Comparison of EUCAST and CLSI Reference Microdilution MICs of Eight Antifungal Compounds for Candida auris and Associated Tentative Epidemiological Cutoff Values. Antimicrob. Agents Chemother. 2017, 61, e00485-17. [Google Scholar] [CrossRef]
- Gafter-Gvili, A.; Vidal, L.; Goldberg, E.; Leibovici, L.; Paul, M. Treatment of Invasive Candidal Infections: Systematic Review and Meta-analysis. Mayo Clin. Proc. 2008, 83, 1011–1021. [Google Scholar] [CrossRef]
- Centers for Disease Control and Prevention. Infection Prevention and Control for Candida auris. Updated 2023. Available online: https://www.cdc.gov/fungal/candida-auris/c-auris-infection-control.html (accessed on 1 December 2024).
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Mallick, D.C.; Kaushik, N.; Goyal, L.; Mallick, L.; Singh, P. A Comprehensive Review of Candidemia and Invasive Candidiasis in Adults: Focus on the Emerging Multidrug-Resistant Fungus Candida auris. Diseases 2025, 13, 93. https://doi.org/10.3390/diseases13040093
Mallick DC, Kaushik N, Goyal L, Mallick L, Singh P. A Comprehensive Review of Candidemia and Invasive Candidiasis in Adults: Focus on the Emerging Multidrug-Resistant Fungus Candida auris. Diseases. 2025; 13(4):93. https://doi.org/10.3390/diseases13040093
Chicago/Turabian StyleMallick, Deobrat Chandra, Nayanjyoti Kaushik, Lokesh Goyal, Lipika Mallick, and Prabhat Singh. 2025. "A Comprehensive Review of Candidemia and Invasive Candidiasis in Adults: Focus on the Emerging Multidrug-Resistant Fungus Candida auris" Diseases 13, no. 4: 93. https://doi.org/10.3390/diseases13040093
APA StyleMallick, D. C., Kaushik, N., Goyal, L., Mallick, L., & Singh, P. (2025). A Comprehensive Review of Candidemia and Invasive Candidiasis in Adults: Focus on the Emerging Multidrug-Resistant Fungus Candida auris. Diseases, 13(4), 93. https://doi.org/10.3390/diseases13040093