Abstract
The growing burden of non-communicable diseases amidst the largest burden of HIV in South Africa leads to disease combinations of multimorbidity with the complexity of care. We conducted a cross-sectional study to assess multimorbidity, medication adherence, and associated factors among out-patients with chronic diseases in primary health care (PHC) facilities in Tshwane, South Africa. A structured questionnaire was used to collect data on comorbidities and medication adherence, along with socio-demographic and lifestyle factors. Logistic regression models were used to analyse the determinants of multimorbidity and medication adherence. In all 400 patients with chronic diseases (mean age: 47 ± 12 years) living in poor environments, common chronic conditions were hypertension (62%), diabetes (45%), HIV (44%), TB (33%), hypercholesterolemia (18%), and gout (13%). The proportion of concordant comorbidity (i.e., diseases with similar risk profiles and management) was 72%, more than 28% of discordant comorbidity (i.e., diseases not related in pathogenesis or management). Most patients had two coexisting chronic conditions (75%), while few had more than two chronic conditions (23%) and single-occurring conditions (2%). Prevalence rates for common multimorbidity patterns were 25% (HIV and TB), 17% (hypertension and diabetes), 9% (hypertension, diabetes, and hypercholesterolemia), and 2% (hypertension diabetes and HIV), while medication adherence was estimated at 74%. In multivariate analysis, multimorbidity was associated with an older age and lower socio-economic status, while medication non-adherence was associated with a younger age and socio-economic factors. The study highlights the presence of multimorbidity among primary care patients attributed to hypertension, diabetes, HIV, and TB in South Africa with non-adherence to medication in one-third of patients. Policies are needed for education on multimorbidity with a need to optimize lifestyle modifications, perhaps proactive outreach or nursing contact with high-risk patients with public-health-sensitive conditions, such as HIV and/or TB, as well as patients with a history of non-adherence to medications. Considerations should be given to the development of a medication adherence scale for multiple chronic conditions beyond assessing adherence to a single index medication.
1. Background
The concept of multimorbidity has become a priority agenda in various countries due to its dramatic increase and the strain put on health systems to manage patients with multiple chronic diseases [1]. Multimorbidity is the presence of two or more chronic diseases coexisting in an individual [2], affecting approximately 37% of adults, globally [3]. The prevalence rates of multimorbidity vary by socioeconomic status and regions [3], and for quite some time, high-income countries (HICs) were more affected (37%), with alarming rates of non-communicable diseases (NCDs). However, current literature reports an increase of multimorbidity (32.1%) in low-and middle-income countries (LMICs) [3,4], burdened by coexisting chronic diseases due to the aging of the population, but not exclusively affecting the elderly [5], while medication adherence remains low [6,7,8,9].
The absence of integrated chronic care models for the management of multiple coexisting burdens of NCDs and communicable diseases (CDs) among chronic patients in LMICs has been documented. These circumstances have been implicated in the ineffective management of multimorbidity in this region [10,11]. In particular, medication adherence (i.e., commitment to taking the treatment as prescribed) among patients with multimorbidity, which is a determining factor to maintain a longer healthy life, has raised concerns on poor management [8,12,13,14]. Over the past two decades, studies have reported a pill burden/polypharmacy of an average of five medications among multimorbid patients predisposing them to non-adherence [15,16]. Non-adherence to medication gives rise to poor clinical outcomes leading to a poor quality life, high mortality rates, and hospitalization, among others [17,18,19,20,21].
South Africa is currently experiencing a convergence of NCDs and CDs [22,23,24,25,26], causing the burden of multimorbidity to range from 3% to 87% in various group populations. The common multimorbidity patterns in South Africa are combined TB and HIV, hypertension and diabetes, and hypertension and HIV [27], and to a lesser extent, the coexistence of HIV, anaemia hypertension, and/or diabetes has been reported [28]. Although South Africa has put in place a primary health care approach for a better health care since the inception of the democratic government in 1994 [29,30], the country remains burdened with NCDs and CDs coexisting [13,23,25]. Despite the increasing co-occurrence of multiple chronic conditions and poor clinical outcomes among chronic patients [13], minimal research has been conducted on multimorbidity in South Africa [27,28]. While multimorbidity requires a complexity of care [13,31,32], most local studies have reported medication adherence from a single index point of view for hypertension, diabetes, and HIV treatments. The era of an anti-retroviral therapy (ART) programme in South Africa has improved the health of people living with HIV (PLWH) but has come along with cardiometabolic diseases [26,33,34].
The absence of integrated care in South Africa will increase the burden of multimorbidity and worsen the already burdened health systems and continues to affect the quality of individuals’ lives, especially multimorbid patients [23,26]. This calls for prioritized policies on the integrated management of NCDs and CDs [35], especially in a country like South Africa, which has an uneven distribution of healthcare needs from the public and private services, affecting mostly the socio-economically disadvantaged [36]. Therefore, considerations of a context-bound understanding of multimorbidity and treatment for the quality care of chronic patients are urgent [37]. In view of this, we assessed multimorbidity, medication adherence, and associated factors among out-patients with chronic diseases in primary health care (PHC) facilities in Tshwane, South Africa. Diagnosis, awareness and education, lifestyle modification, prescribed medication, and adherence/compliance, for successful clinical management, are pillars in the South African National user guide for the prevention and treatment of chronic diseases [38].
2. Methods
2.1. Study Design and Setting
A cross-sectional study was conducted between January 2022 and September 2022 guided by the Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) [39]. In this study, we used a modified framework on multimorbidity and comorbid non-communicable and infectious chronic diseases (CNCICD) [40], adapted from the Innovative Care for Chronic Conditions (ICCC) framework of the World Health Organization (WHO) [41], focusing on the micro-level, which revolves around patients and the interaction with health facilities [40]. Together with CNCICD, the conceptual model for contributing factors to medication adherence, such as the patient, disease, treatment, healthcare system, and socioeconomic-related factors [42], informed data collection and analysis.
This study was conducted in the City of Tshwane municipality situated in the northern Gauteng Province of South Africa with 22 public PHC facilities [43,44]. Anecdotal information estimated approximately 269,700 patients from the respective facilities in 2019/2020. According to Statistics South Africa [45], a large proportion of the population is Africans (75.4%), followed by White (20.1%), then Coloured (2.0%), and Indian or Asian (1.8%) living across the informal settlements, rural, peri-urban, or urban settings of the City of Tshwane.
2.2. Sample Size, Sampling, and Participants
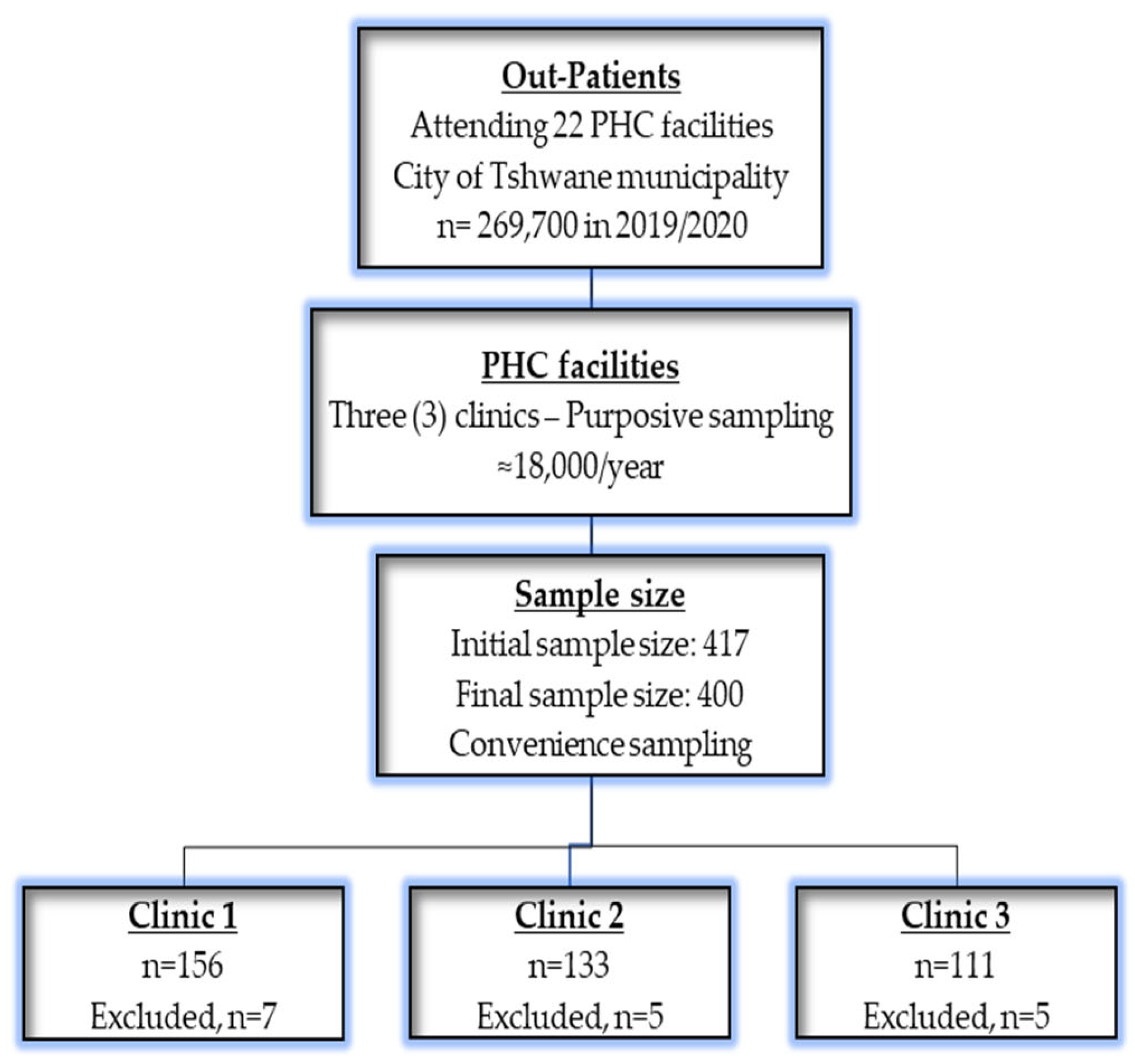
Out-patients with chronic conditions were estimated at approximately 4500 patients in each quarter, per year totalling 18,000 in a year. Considering a confidence level of 95%, 5% margin of error, and 50% response distribution, a minimum representative sample of 377 was calculated using Cochran’s formula using a validated Raosoft sample size calculator [46]. A sample of 377 was buffered with 10% to cater for non-response to increase the sample size to 415 out-patients. Out of the recruited 450 out-patients seeking chronic care at the selected facilities, 417 responded. Upon data capturing, 17 questionnaires had missing data above 10%, mainly on chronic conditions, and were excluded; seven patients were from clinic 1, five from clinic 2, and five from clinic 3, as indicated in Figure 1, below. A final sample size of 400 out-patients seeking chronic care at the selected facilities was eventually obtained.
Figure 1.
A flow chart of recruitment, sampling processes, and exclusions.
First, the three facilities (i.e., Atteridgeville Clinic, Laudium Community Health Centre, and Lyttelton Clinic) where chronic health care services take place from Monday to Friday of every week were purposively selected out of the 22 facilities in the City of Tshwane municipality based on the highest population head count. Second, within the selected facilities, convenience sampling, applicable in clinical research [47], was used to select participants following the difficulty to obtain a random sampling due to long queues in the facilities and due to impatience of the out-patients waiting for hours. These patients were attending chronic care services in these PHC facilities, on treatment for the past 12 months at the times of the study, aged 18 years and above, and they gave informed written consent to participate in this study. A flow chart for recruitment, sampling processes, and exclusions is presented in Figure 1.
2.3. Data Collection and Tools
Following ethical approval by the Sefako Makgatho Health Sciences University Research and Ethics Committee (SMUREC/H/256/2021:PG) and permission from the Tshwane Research Committee in Gauteng Province, South Africa (GP_202112_005), the recruitment of patients started at one facility identified to conduct a pilot study prior to conducting the main study. From each of the three facilities selected, a healthcare worker was assigned to assist with the recruitment of chronic patients while in a queue for consultation in the morning. During recruitment, information leaflets written in three local languages, which are English, Setswana, and isiZulu, were distributed to the patients to explain the objectives of the study while in the chronic waiting area. The information leaflets had the contact numbers of the researcher provided for patients to enquire about the study, if need be, while other patients were able to seek clarity during the time of recruitment and consent to participate after consultation.
Through experts’ judgement, validity based on the content, construct, and face were performed to ensure the suitability of the questionnaire. Research assistants who were eloquent in English, Setswana, and isiZulu were trained to conduct preliminary interviews in a mini pilot study conducted in the smallest facility among 30 out-patients. The pilot study was purposed to assess the feasibility of the planned main study, especially based on recruitment processes, and data collection from chronic out-patients. The results from the pilot study, which were excluded from the analysis of the main study, showed that the questionnaire had relevant measurable variables, with easily arranged questions and layout. Minimal modifications were made to the questionnaire following the piloting outcomes. Therefore, we concluded that the main study would be feasible to be conducted among chronic patients at the selected public PHC facilities and continued to collect data on a larger scale.
The research team was made up of the principal researcher and two tutored research assistants administered a pre-tested questionnaire in either English, Setswana, or isiZulu languages preferred by the patient. The questionnaire was modified from previous similar studies carried out among patients with chronic conditions and collected demographic information and access to treatment and adherence [4,48,49,50,51,52,53,54,55]. Additional medical data were extrapolated from the patients’ file, and any information that was missing in the records was collected through self-reporting from patients.
Socio-demographic information included in the questionnaire entailed sex (male and female), age categories (18–39 years, 40–59 years, and ≥60 years), race (African, White, Coloured, and Asian), place of residence (informal settlements, peri-urban, and urban), marital status (single, married, and divorced), education level (no education, primary, secondary, grade 12, and tertiary education) and education level (i.e., completed grade 12 and tertiary), and employment status (employed, unemployed, or pensioner). Household information included the household income ($266.85; $266.85–$533.80; $533.80–$800.40; >$800.40), household size (<5 and ≥5 members), type of house [shack, RDP (Reconstruction and Development Programme) house and brick], electricity (no or yes), use of a refrigerator (no or yes), water access (no or yes), electricity access (no or yes), and type of a toilet (pit latrine or flush toilet), adapted from other studies conducted on chronic diseases [50,51].
Using WHO standard procedures and classifications [56], weight (using the smart D-quip electronic scale), height (using stadiometer/measuring board), and waist and hip (using a non-stretchable plastic tape measure) were measured three times to the nearest 0.1 from the participants. The calculated body mass index (BMI) defined underweight (<19 kg/m2), normal (19–24.99 kg/m2), overweight (≥25 kg/m2), and obesity, (≥30 kg/m2), while abdominal obesity was defined as waist circumference (WC) ≥88 cm, waist–hip ratio (WHR) ≥0.85, and waist-to-height ratio (WHtR) ≥0.5.
Multimorbidity was determined using a self-administered Co-Questionnaire (SCQ) enlisting medical conditions, such as diabetes, hypertension, heart, kidney, and lung diseases, as well as blood diseases, anaemia, etc. [55]. Participants were asked about the duration of the chronic diseases and the chronic condition that was diagnosed first. In addition to single conditions, patterns of multimorbidity were categorized as two conditions, three conditions, and four conditions of chronic diseases coexisting. Comorbidity classes were categorized as concordant, diseases with a similar risk profile and management (e.g., diabetes and hypertension), whereas discordant was described as diseases not related in pathogenesis or management (e.g., hypertension and HIV) [4,52] and were categorized by the research team based on their expertise.
Medication adherence was estimated using a General Medication Adherence Scale (GMAS) based on questions about treatment and the appointment and scored 0 to 20 in a three-level Likert score of zero to two points. GMAS ≥ 16 (≥80%) was labelled as adherence to medication, while non-adherence was GMAS < 15 (<80%) [48,53,54].
2.4. Data Analysis
STATA version 18 (StataCorp. 2018. Stata Statistical Software: Release 18. College Station, TX, USA) was used to analyse the data. Descriptive statistics (frequencies (n) and proportions (%)) were computed for the demographic, anthropometric, medication adherence, and morbidity characteristics of patients and compared by sex and age using a Chi square (χ2) test. Multimorbidity classes and medication adherence were considered as the two dependent variables, and binary logistic regressions were used to identify their determinants. The covariates were socio-demographic variables, anthropometric measurements, and selected behavioural and biological risk factors. Variables that were found to have an association with dependent variables at p-value < 0.25 in the binary logistic regression were entered into a multivariable logistic regression model. The magnitude of the association between independent and dependent variables was measured using odds ratios and the 95% confidence interval (CI) with the significant level (p-value < 0.05).
2.5. Ethics Committee
The Research and Ethics Committee, Sefako Makgatho Health Sciences University (SMUREC) approved the study (SMUREC/H/256/2021:PG). Further permission was obtained from Tshwane Research Committee in Gauteng Province, South Africa (GP_202112_005). Patients gave informed written consent for their participation, and the study adhered to ethical principles laid down in the Declaration of Helsinki [57].
3. Results
3.1. Characteristics of Patients
In all, 400 out-patients seeking chronic care at the Tshwane PHC facilities participated in the study. Their mean age was 47 ± 12 years, ranging from 25 to 73 years. Age groups were categorized into younger patients [<35 years, n = 70 (18%)], middle-aged patients [35–59 years, n = 236 (59%)], and older patients [≥60 years, n = 94 (23%)]. Two hundred and thirty-three patients were females [n = 233 (58%)], and one hundred and sixty-seven [n = 167 (42%)] were males. Most patients were Africans [n = 247 (62%)], while 14% (n = 56) were White, 12% (n = 48) were Coloured (i.e., person of mixed White, with either African or Asian ancestry), and 12% (n = 49) were Indians/Asians, residing across various settings, but mostly in the urban setting [n = 162; (41%)]. Being single (43%), attained secondary education (43%), and unemployed (40%) were prevalent characteristics in the sample population. Almost half of the participants came from households with a monthly income of $266.85–$533.80 per month. General overweight (23%), obesity (35%) by weight and height, and abdominal obesity by waist circumference (88%) were observed among the patients, in addition to irregular exercise (64%), salt intake (53%), current alcohol use (72%), and current cigarette smoking (53%) (Table 1).

Table 1.
Characteristics of out-patients with chronic diseases.
3.2. Characteristics of Comorbidity
In Table 2, hypertension was the self-reported first diagnosed (49%) chronic condition and the most common condition (62%), while HIV (37%) was the second diagnosed, followed by diabetes as the third (10%) and the second (45%) prevalent chronic condition. HIV (44%) and TB (33%) were observed among patients. Other reported chronic conditions were hypercholesterolemia (18%), gout (13%), lung diseases (5%), anaemia (0.25%), and prostate cancer (0.25%). Three and more therapies (42%) were common for hypertension and the mostly used medications were Amlodipine besylate and Hydrochlorothiazide. For diabetes, monotherapy was prevalent, and Metformin and Glyburide were commonly used medications. Almost all patients were on ART (99%) for HIV treatment, and RH, Cotrimaxole, and Pyrodixine were used to treat TB. The hospitalization of chronic patients was higher among those with hypertension (17%), followed by diabetes (12%) and HIV (10%), and none with TB were hospitalized due to the condition. Using GMAS, low adherence had a score <15 (<80%) and high adherence had a score ≥16 (≥80%). The overall prevalence of medication adherence among out-patients was estimated at 74% (95%CI: 70–78).

Table 2.
Characteristics of comorbidity among out-patients.
Table 3 shows the prevalence and patterns of morbidity among out-patients with chronic diseases. Patients with single chronic conditions, two conditions, three conditions, and four conditions were classified, as in the study of Pati et al. [58]. Furthermore, we considered the concordant (i.e., diseases with a similar risk profile and management) and discordant (i.e., diseases not related in pathogenesis or management) comorbidities by the known pathophysiologic pathways [4,52]. Thirty-one patterns of morbidities occurring as either single chronic conditions [9 (2%)], two conditions [300 (75%)], three conditions [80 (20%)], or four conditions [11 (3%)] were observed among patients. Concordant multimorbidity [n = 281 (72%)] was more prevalent than the discordant multimorbidity [n = 110 (28%)]. There were 13 patterns of two chronic conditions with the top six being HIV and TB (25%), followed by hypertension and diabetes (17%), hypertension and gout (9%), hypertension and HIV (7%), hypertension and hypercholesterolemia (6%), and diabetes and HIV (3%). The top three chronic conditions of multimorbidity out of the identified 12 patterns were hypertension, diabetes, and hypercholesterolemia (9%), followed by hypertension, diabetes, and gout (3%), hypertension diabetes and HIV (2%), and hypertension, diabetes, and asthma (2%). Very few four-chronic-condition patterns (n = 3) were observed, with hypertension, diabetes, HIV, and hypercholesterolemia as the most occurring pattern.

Table 3.
Prevalence and patterns of morbidity among out-patients, and level of adherence.
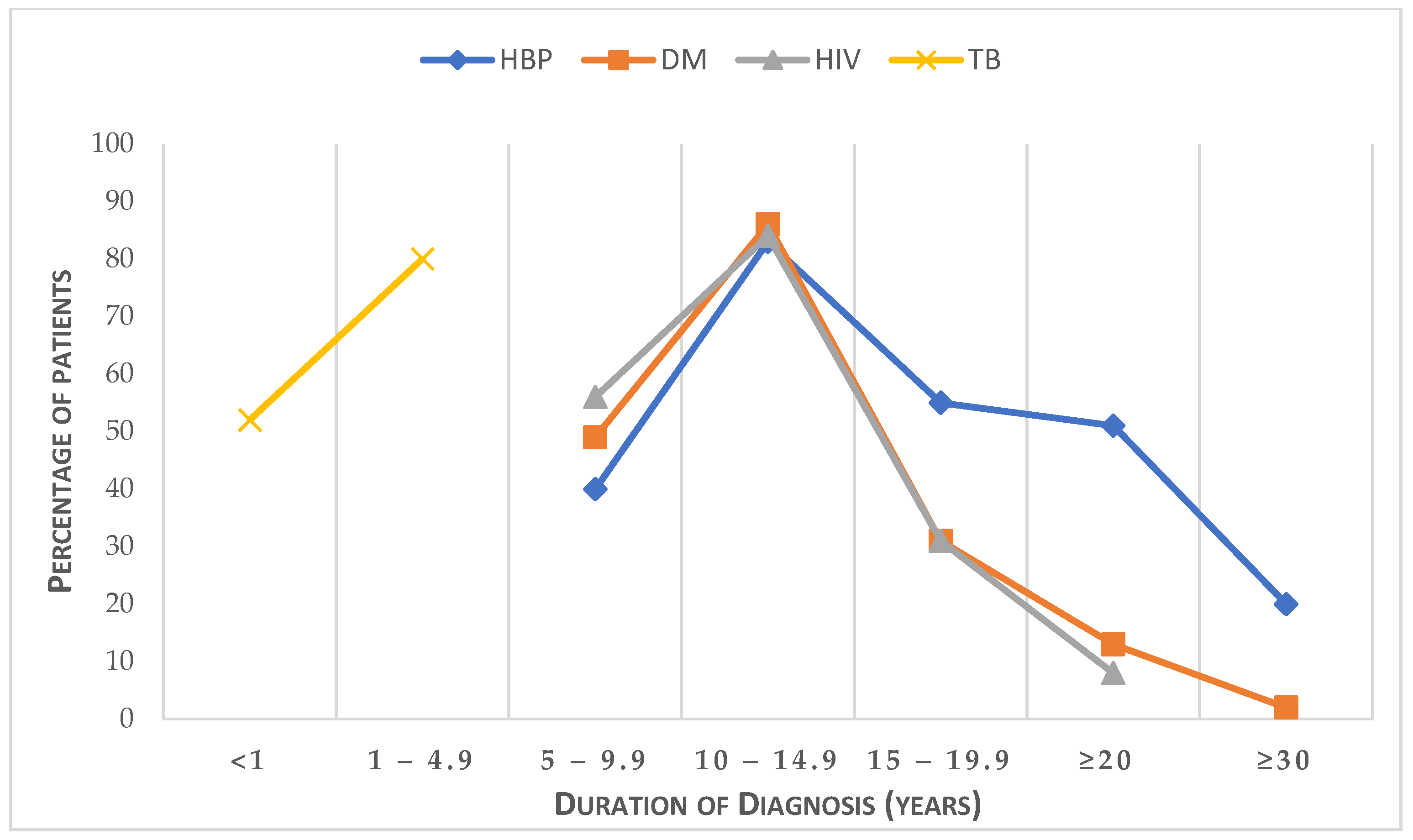
We assessed the duration of the self-reported diagnosis of HBP (i.e., hypertension), DM (i.e., diabetes mellitus), HIV, and TB among chronic out-patients, shown in Figure 2. It was observed that the diagnosis of TB was within one year prior to the study, while most patients with hypertension, diabetes, and HIV were diagnosed within the past 5 to 15 years, and the proportion of patients with chronic conditions decreased with the years of diagnosis, such as HIV (5%) towards 20 years and hypertension (28%) and diabetes (8%) for 20 years and above.
Figure 2.
Self-reported duration of the diagnosis of HBP, DM, HIV, and TB among out-patients.
3.3. Factors Associated with Medication Adherence in Patients with Morbidity
In Table 4, chronic diseases among patients were compared by sex and age groups using a Chi-square test. There was an association between multimorbidity patterns with age (p ≤ 0.0001). Single chronic conditions were prevalent among the younger patients (9%) compared to the middle aged (1%) and older patients (0%), while three and four chronic conditions increased significantly with age. The association with multimorbidity was further observed in both men and women (p = 0.005), with no single chronic condition among men (0%) compared to women (4%), while the presence of two, three, and four conditions varied between men and women. Women (77%) exhibited better medication adherence than men (71%), although it was not significantly different (p = 0.164).

Table 4.
Prevalence and patterns of morbidity among out-patients by sex and age group.
Table 5 shows the determinants of multimorbidity. First, univariate analysis (COR) showed associations of multimorbidity with age, marital status, education, employment, and household income (p < 0.25). After controlling for potential confounders (AOR), logistic regression showed multimorbidity associated with an older age [AOR = 14.95; 95%CI: 3.28–68.19] and higher income [AOR = 0.16; 95%CI: 0.03–0.71].

Table 5.
Association of multimorbidity with covariates among patients.
Table 6 shows the determinants of medication adherence. Univariate analysis (COR) showed an association of medication adherence with age, sex, residential area, marital status, education, employment, income, house type, household size, refrigerator use, current alcohol use, current cigarette smoking, BMI, WC, and WHtR (p < 0.25). After controlling for potential confounders, logistic regression showed that the odds of adherence to medication increased with age [≥60 years: AOR = 3.20; 95%CI: 1.03–9.94], marital status [cohabiting: AOR = 2.17; 95%CI: 1.02–4.63, married: AOR = 5.01; 95%CI: 1.97–12.69, and divorced: AOR = 8.84; 95%CI: 3.07–25.78], education [secondary: AOR = 3.06; 95%CI: 1.50–6.23, grade 12: AOR = 9.81; 95%CI: 3.35–28.77, and tertiary: AOR = 9.40; 95%CI: 3.39–26.82] and decreased with household size [AOR = 0.28; 95%CI: 0.15–0.55] and current cigarette smoking [AOR = 0.42; 95%CI: 0.23–0.76].

Table 6.
Determinants of medication adherence among patients.
4. Discussion
This study assessed multimorbidity, medication adherence, and associated factors among out-patients with chronic diseases. The findings of this study showed the presence of multimorbidity patterns and classes among primary care out-patients in Tshwane, South Africa. The most common condition was hypertension (62%), which was self-reported as diagnosed first among almost half of the patients (49%), followed by diabetes (45%) as the second most prevalent chronic condition. High prevalence rates (21% to 77.9%) have been recorded in South Africa and remain the highest in the Southern Africa region [59,60], while the prevalence of diabetes has tripled since 2000 to date [61,62,63,64] with concerns of self-management [51,65]. The prevalence of hypertension and diabetes have been reported to increase significantly with age in South Africa [66,67] and in other countries, such as Kenya, [66] Ghana [66], Tanzania [68], and the United Arab Emirates (UAE) [48]. The current study also recorded a high occurrence of HIV as the condition that was diagnosed second among over one-third of the patients, and it was prevalent in younger patients, as reported previously [69]. South Africa has the highest HIV prevalence (18%) and supports the largest antiretroviral therapy (ART) [70]. The country is included in the WHO’s list of 30 high-burden tuberculosis countries and has one of the highest incidence rates of notified tuberculosis in the world with 55% attributed to HIV [71]. A growing burden of NCDs coexisting with CDs is currently leading to multimorbidity [23,24,72].
A poor socioeconomic status in terms of low household income per month, unemployment, and dependence on old age pension grants was observed in this study. Social inequalities have been associated with multimorbidity, suggesting that individuals who are socioeconomically deprived tend to have more chronic conditions than the least deprived ones [73,74,75]. This was corroborated in the current study showing that patients who came from households with high monthly income had lower odds of multimorbidity compared to those coming from households with low monthly income. Similarly, previous studies have reported an earlier onset of multimorbidity in patients living in the most deprived areas compared with the most affluent areas [10,76,77]. Therefore, addressing inequalities regarding healthcare use is critical to achieve better health outcomes for multimorbid patients living in poor backgrounds [78]. Furthermore, the current study showed a high prevalence of poor lifestyle factors, such as overweight/obesity, salt intake, irregular exercise, alcohol use, and smoking, which are implicated in the development and progression of chronic diseases [10]. These lifestyle factors have been associated with an increase in multimorbidity, in addition to population ageing [10,79]. In particular, alarming rates of overweight/obesity are being observed in South Africa, higher than in other Africa continues, and almost similar as in HIC countries [51,80,81].
The current study further showed that single chronic conditions (2%) were diminishing among the chronic patients, while concordant comorbidity (72%), mainly combined diabetes and hypertension, was common than the discordant class (28%). Concordant comorbidity was prevalent among older patients (≥60 years of age), while discordant multimorbidity was common among younger patients (≤35 years). Prior studies showed similar patterns of disease with hypertension and diabetes being the most common concordant comorbidity disease cluster [14,58,82]. Hypertension and diabetes are known to frequently co-occur and share common risk factors and complications that include microvascular and macrovascular disorders [83,84]. The prevalence of concordant comorbidity was higher compared to reports in South Africa (6%) [85] and Africa (55.8%) [4], but lower than in countries, like India (84%) [58], Spain (82%) [86], the Netherlands (84.6%) [87], and USA (88.5%) [88].
Regarding multimorbidity patterns, our study indicated that a large component of multimorbidity was sequentially attributed to hypertension, diabetes, HIV, and TB. Three quarters of the patients had two chronic conditions, one quarter had more than two conditions, and very few had single conditions. Coexisting HIV and TB was the common pattern of two chronic conditions. That was followed by hypertension and diabetes, hypertension and gout, and hypertension and HIV. The three-condition patterns of multimorbidity were hypertension, diabetes, and hypercholesterolemia, hypertension, diabetes, and gout, and hypertension, diabetes, and HIV. A systematic review on multimorbidity in South Africa has reported hypertension as the most frequent condition, and it is associated with other diseases [27]. Furthermore, most of the above-mentioned multimorbidity patterns have been reported in South Africa [27] and occur commonly among primary care patients in South Africa [13,14,51,82,89]. The occurrence of multimorbidity is further consistent with the findings from several countries, like Brazil [19], India [90] Ghana [91], and the UAE [48]. The prevalence of multimorbidity, as reported in previous studies in South Africa, ranged from 3% to 87% [27,82,89], attributed to the difference in the methodologies used, the target population with various chronic diseases, and the context of socio-demographic variations [4,92]. Our findings are similar to several studies that reported higher odds of having multimorbidity among older out-patients compared to the younger group [4,10]. Therefore, it was not a surprise that no chronic condition occurred on a singular level in older patients (≥60 years). However, it is worth noting that over half of the patients in this study were below 60 years of age, emphasizing that multimorbidity is not just a feature of ageing [10,93]. Therefore, diseases can coexist in the same individual for several reasons, including common risk factors or mechanisms and iatrogenic conditions [94].
We further observed adherence to medication estimated at 74%, almost similar to the prevalence reported among patients with multimorbidity in the United Arab Emirates (78%) [48]. The challenge remains that we are not able to compare our findings with other studies in South Africa and African countries, since most studies reported medication adherence to a single chronic illness. One-third of patients with multimorbidity in this study were not adhering to medication, supporting the notion of the complexity of medication adherence and the self-management of multimorbidity among patients. This is consistent with a recent south African study that reported poor diabetic self-management among diabetes patients with two and three coexisting chronic conditions [51]. Adherence to medication was associated with older age, marital status, higher education, lower socioeconomic status, and current cigarette smoking. Clearly, these results demonstrate the multifactorial determinants involved in medication adherence, as reported by other researchers [48]. Similar to one study conducted in the UAE [48], we found that the odds of adherence to medication increased with age, and patients aged 60 years old and above were three times more likely to adhere to medication than their younger counterparts.
Lastly, most of the chronic patients in South Africa use PHC facilities for primary care treatment accessed through the Centralised Chronic Medicine Dispensing and Distribution Programme (CCMDD), and adherence to the treatment of single conditions is suboptimal, except for HIV [13,65,95]. The World Health Organization (WHO) calls for universal health insurance and health service coverage in LMICs, particularly for vulnerable groups [96], as well as the United Nations (UN)’ sustainable development goals (SDG) 3 on Good Health and Well-Being to ensure healthy lives and promote well-being for all at all ages [97]. The fact remains that treatment plans in patients with multimorbidity are complex and multifactorial. Therefore, improving medication adherence requires a multilevel approach from patient to healthcare factors.
5. Limitations
There are some limitations to this study. First, the proposed sample size calculation used in this study is for a simple random sampling strategy. Therefore, the use of non-probability sampling might have introduced selection bias, which we mitigated by obtaining a larger sample size of the participants. Second, in self-reported surveys, patients may overestimate their adherence to medications due to social desirability bias. Nevertheless, this might have been mitigated by using well-trained research assistants and a robust validated questionnaire with identified options to questions. Third, the lifestyle factor assessment depended largely on self-report measures, which can also be subject to social desirability bias, and hence, the result must be treated with caution. Fourth, a causal relationship of medical adherence and its correlates cannot be ascertained, given the cross-sectional design method adopted in the study. Furthermore, assessing salt intake, alcohol intake, and physical activity using standardized methods, such as biochemical parameters of sodium, the Alcohol Use Disorders Identification Test (AUDIT), and the Global Physical Activity Questionnaire (GPAQ), respectively, could have added more objectivity. Additional qualitative methodology for future research will enrich and improve the robustness in understanding the multidimensional factors related to medication adherence. Lastly, the findings may not be generalizable to the general population because this study used hospital out-patients. Nonetheless, in addition to reporting concordant versus discordant comorbidities, and multimorbidity patterns among out-patients in PHC facilities in Tshwane, this study has showed factors associated with medication adherence among multimorbid patients. Although, there is no standard criterion available to assess medication adherence in patients receiving multiple treatments, rendering an appropriate measurement of multiple medication adherence a challenge, to our knowledge, our study is among the very few in South Africa that has attempted to assess medication adherence among multimorbid patients, rather than for one single chronic condition.
6. Conclusions
This study highlights the presence of multimorbidity among primary care patients in Tshwane facilities, South Africa. A total of thirty-one multimorbidity patterns were observed among patients of all ages from the younger, to middle-aged, and older patients. Our study indicated that a large component of multimorbidity was sequentially attributed to hypertension, diabetes, and HIV. Almost one-third of chronic patients were non-adherent to medication, with increased odds among patients who are younger and with marital status, education, household size, and current cigarette smoking. Policies are perhaps needed for education on multimorbidity with a need to optimize lifestyle modifications, in addition to proactive outreach or nursing contact with high-risk patients with public-health-sensitive conditions, such as HIV and/or TB, as well as patients with a history of non-adherence to medications. Considerations should be given to the development of a medication adherence scale for multiple chronic conditions beyond assessing adherence to a single index medication.
Author Contributions
T.W.M.: proposal writing, conceptualization, methodology, investigation, resources, project management, and writing—original draft. P.M.: Conceptualization, methodology, formal analysis, software, validation, supervision, writing—original draft, and writing—review and editing. K.M. validation and writing—review and editing. S.M.: Conceptualization, methodology, writing—original draft, and writing—review and editing. R.A.R.: validation and writing—review and editing. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
The Research and Ethics Committee, Sefako Makgatho Health Sciences University (SMUREC), approved the study (SMUREC/H/256/2021:PG). Further permission was obtained from the Tshwane Research Committee in Gauteng Province, South Africa (GP_202112_005). Patients gave informed written consent for their participation, and the study adhered to ethical principles laid down in the Declaration of Helsinki [57].
Informed Consent Statement
Informed consent was obtained from all subjects involved in the study.
Data Availability Statement
The dataset for chronic patients generated and analysed during the current study are available from the corresponding author upon reasonable request.
Acknowledgments
The authors wish to thank all the patients who participated in the study. We also thank the Tshwane Research Committee, Gauteng Province, South Africa, and the managers of the health facilities for giving us the permission to conduct the study and the research assistants for data collection.
Conflicts of Interest
The authors declare no conflict of interest.
References
- Navickas, R.; Petric, V.K.; Feigl, A.B.; Seychell, M. Multimorbidity: What do we know? What should we do? J. Comorbidity 2016, 6, 4–11. [Google Scholar] [CrossRef] [PubMed]
- Academy of Medical Sciences. Multimorbidity: A Priority for Global Health Research; Academy of Medical Sciences: London, UK, 2018. [Google Scholar]
- Chowdhury, S.R.; Chandra Das, D.; Sunna, T.C.; Beyene, J.; Hossain, A. Global and regional prevalence of multimorbidity in the adult population in community settings: A systematic review and meta-analysis. E-Clin. Med. 2023, 57, 101860. [Google Scholar] [CrossRef]
- Ejeta, A.; Abdosh, T.; Hawulte, B.; Lamessa, A.; Belete Fite, M.; Fekadu, G. Diabetes Concordant Comorbidities and Associated Factors Among Adult Diabetic Out-Patients at Hiwot Fana Specialized University Hospital, Harar, Eastern Ethiopia: A Cross-Sectional Study. Diabetes Metab. Syndr. Obes. Targets Ther. 2021, 14, 2281–2289. [Google Scholar] [CrossRef]
- Violan, C.; Foguet-Boreu, Q.; Flores-Mateo, G.; Salisbury, C.; Blom, J.; Freitag, M.; Glynn, L.; Muth, C.; Valderas, J.M. Prevalence, determinants and patterns of multimorbidity in primary care: A systematic review of observational studies. PLoS ONE 2014, 9, e102149. [Google Scholar] [CrossRef] [PubMed]
- Gouda, H.N.; Charlson, F.; Sorsdahl, K.; Ahmadzada, S.; Ferrari, A.J.; Erskine, H.; Leung, J.; Santamauro, D.; Lund, C.; Aminde, L.N.; et al. Burden of non-communicable diseases in sub-Saharan Africa, 1990–2017: Results from the Global Burden of Disease Study 2017. Lancet Global Health. 2019, 7, e1375–e1387. [Google Scholar] [CrossRef] [PubMed]
- Kengne, A.P.; June-Rose McHiza, Z.; Amoah, A.G.; Mbanya, J.C. Cardiovascular diseases and diabetes as economic and developmental challenges in Africa. Prog. Cardiovasc. Dis. 2013, 56, 302–313. [Google Scholar] [CrossRef] [PubMed]
- Chauke, G.D.; Nakwafila, O.; Chibi, B.; Sartorius, B.; Mashamba-Thompson, T. Factors influencing poor medication adherence amongst patients with chronic disease in low-and-middle-income countries: A systematic scoping review. Heliyon 2022, 8, e09716. [Google Scholar] [CrossRef]
- Pednekar, P.P.; Agh, T.; Malmenäs, M.; Raval, A.D.; Bennett, B.M.; Borah, B.J.; Hutchins, D.S.; Manias, E.; Williams, A.F.; Hiligsmann, M. Methods for measuring multiple medication adherence: A systematic review–report of the ISPOR medication adherence and persistence special interest group. Value Health 2019, 22, 139–156. [Google Scholar] [CrossRef]
- Barnett, K.; Mercer, S.W.; Norbury, M.; Watt, G.; Wyke, S.; Guthrie, B. Epidemiology of multimorbidity and implications for health care, research, and medical education: A cross-sectional study. Lancet 2012, 380, 37–43. [Google Scholar] [CrossRef]
- De-Graft Aikins, A.; Unwin, N.; Agyemang, C.; Allotey, P.; Campbell, C.; Arhinful, D. Tackling Africa’s chronic disease burden: From the local to the global. Glob. Health 2010, 6, 5. [Google Scholar] [CrossRef]
- Lam, W.Y.; Fresco, P. Medication Adherence Measures: An Overview. BioMed Res. Int. 2015, 2015, 217047. [Google Scholar] [CrossRef]
- Wong, E.B.; Olivier, S.; Gunda, R.; Koole, O.; Surujdeen, A.; Gareta, D.; Munatsi, D.; Modise, T.H.; Dreyer, J.; Nxumalo, S.; et al. Convergence of infectious and non-communicable disease epidemics in rural South Africa: A cross-sectional, population-based multimorbidity study. Lancet Glob. Health 2021, 9, e967–e976. [Google Scholar] [CrossRef] [PubMed]
- Oni, T.; Youngblood, E.; Boulle, A.; McGrath, N.; Wilkinson, R.J.; Levitt, N.S. Patterns of HIV, TB, and non-communicable disease multi-morbidity in peri-urban South Africa- a cross sectional study. BMC Infect. Dis. 2015, 15, 20. [Google Scholar] [CrossRef]
- While, A. Medication adherence: Understanding the issues and finding solutions. Br. J. Community Nurs. 2020, 25, 474–479. [Google Scholar] [CrossRef]
- Claxton, A.J.; Cramer, J.; Pierce, C. A systematic review of the associations between dose regimens and medication compliance. Clin. Ther. 2001, 23, 1296–1310. [Google Scholar] [CrossRef] [PubMed]
- Makovski, T.T.; Schmitz, S.; Zeegers, M.P.; Stranges, S.; van den Akker, M. Multimorbidity and quality of life: Systematic literature review and meta-analysis. Ageing Res. Rev. 2019, 53, 100903. [Google Scholar] [CrossRef]
- McPhail, S.M. Multimorbidity in chronic disease: Impact on health care resources and costs. Risk Manag. Healthc. Policy 2016, 9, 143–156. [Google Scholar] [CrossRef] [PubMed]
- Nunes, B.P.; Flores, T.R.; Mielke, G.I.; Thumé, E.; Facchini, L.A. Multimorbidity and mortality in older adults: A systematic review and meta-analysis. Arch. Gerontol. Geriatr. 2016, 67, 130–138. [Google Scholar] [CrossRef]
- Nguyen, Q.D.; Wu, C.; Odden, M.C.; Kim, D.H. Multimorbidity Patterns, Frailty, and Survival in Community-Dwelling Older Adults. J. Gerontol. Ser. A 2018, 74, 1265–1270. [Google Scholar] [CrossRef]
- Aggarwal, P.; Woolford, S.J.; Patel, H.P. Multi-Morbidity and Polypharmacy in Older People: Challenges and Opportunities for Clinical Practice. Geriatrics 2020, 5, 85. [Google Scholar] [CrossRef]
- Kengne, A.P.; Mayosi, B.M. Readiness of the primary care system for non-communicable diseases in sub-Saharan Africa. Lancet Glob. Health 2014, 2, e247–e248. [Google Scholar] [CrossRef]
- Modjadji, P. Communicable and non-communicable diseases coexisting in South Africa. Lancet Glob. Health 2021, 9, e889–e890. [Google Scholar] [CrossRef]
- Peer, N. The converging burdens of infectious and non-communicable diseases in rural-to-urban migrant Sub-Saharan African populations: A focus on HIV/AIDS, tuberculosis and cardio-metabolic diseases. Trop. Dis. Travel Med. Vaccines 2015, 1, 6. [Google Scholar] [CrossRef] [PubMed]
- Mayosi, B.M.; Flisher, A.J.; Lalloo, U.G.; Sitas, F.; Tollman, S.M.; Bradshaw, D. The burden of non-communicable diseases in South Africa. Lancet 2009, 374, 934–947. [Google Scholar] [CrossRef]
- Modjadji, P.; Mokgalaboni, K.; Nonterah, E.A.; Lebelo, S.L.; Mchiza, Z.J.-R.; Madiba, S.; Kengne, A.P. A Systematic Review on Cardiometabolic Risks and Perinatal Outcomes among Pregnant Women Living with HIV in the Era of Antiretroviral Therapy. Viruses 2023, 15, 1441. [Google Scholar]
- Rifqah Abeeda, R.; Brian van, W.; Eunice Bolanle, T.; Victoria Pillay-van, W. Multimorbidity in South Africa: A systematic review of prevalence studies. BMJ Open 2021, 11, e048676. [Google Scholar]
- Roomaney, R.A.; van Wyk, B.; Cois, A.; Pillay van-Wyk, V. Multimorbidity patterns in South Africa: A latent class analysis. Front. Public Health 2023, 10, 1082587. [Google Scholar] [CrossRef] [PubMed]
- National Department of Health. South Africa Demographic and Health Survey 2003; Department of Health: Pretoria, South Africa, 2007.
- Peltzer, K. Patient experiences and health system responsiveness in South Africa. BMC Health Serv. Res. 2009, 9, 117. [Google Scholar] [CrossRef] [PubMed]
- Inauen, J.; Bierbauer, W.; Lüscher, J.; König, C.; Tobias, R.; Ihle, A.; Zimmerli, L.; Holzer, B.M.; Battegay, E.; Siebenhüner, K.; et al. Assessing adherence to multiple medications and in daily life among patients with multimorbidity. Psychol. Health 2017, 32, 1233–1248. [Google Scholar] [CrossRef]
- González-Bueno, J.; Sevilla-Sánchez, D.; Puigoriol-Juvanteny, E.; Molist-Brunet, N.; Codina-Jané, C.; Espaulella-Panicot, J. Factors Associated with Medication Non-Adherence among Patients with Multimorbidity and Polypharmacy Admitted to an Intermediate Care Center. Int. J. Environ. Res. Public Health 2021, 18, 9606. [Google Scholar]
- UNAIDS. Country Factsheets; UNAIDS: Geneva, Switzerland, 2018. [Google Scholar]
- Kazooba, P.; Kasamba, I.; Mayanja, B.N.; Lutaakome, J.; Namakoola, I.; Salome, T.; Kaleebu, P.; Munderi, P. Cardiometabolic risk among HIV-POSITIVE Ugandan adults: Prevalence, predictors and effect of long-term antiretroviral therapy. Pan Afr. Med. J. 2017, 27, 40. [Google Scholar] [CrossRef] [PubMed]
- Kemp, C.G.; Weiner, B.J.; Sherr, K.H.; Kupfer, L.E.; Cherutich, P.K.; Wilson, D.; Geng, E.H.; Wasserheit, J.N. Implementation science for integration of HIV and non-communicable disease services in sub-Saharan Africa: A systematic review. AIDS 2018, 32, S93–S105. [Google Scholar]
- Gordon, T.; Booysen, F.; Mbonigaba, J. Socio-economic inequalities in the multiple dimensions of access to healthcare: The case of South Africa. BMC Public Health 2020, 20, 289. [Google Scholar] [CrossRef]
- Forslund, T.; Carlsson, A.C.; Ljunggren, G.; Ärnlöv, J.; Wachtler, C. Patterns of multimorbidity and pharmacotherapy: A total population cross-sectional study. Fam. Pract. 2021, 38, 132–140. [Google Scholar] [PubMed]
- National Department of Health South Africa. National User Guide on the Prevention and Treatment of Hypertension in Adults at the PHC. 2023. Available online: https://knowledgehubhealthgovza/system/files/elibdownloads/2023-04/HYPERTENSION%2520USER%2520GUIDE%2520FINAL%2520COPYpdf (accessed on 29 April 2023).
- Bruno, R.d.C.; Myriam, C.; Douglas, G.A.; Anne, W.S.R.; Matthias, E. Uses and misuses of the STROBE statement: Bibliographic study. BMJ Open 2011, 1, e000048. [Google Scholar]
- Oni T, McGrath N, BeLue R, Roderick P, Colagiuri S, May CR, Levitt NS: Chronic diseases and multi-morbidity—A conceptual modification to the WHO ICCC model for countries in health transition. BMC Public Health 2014, 14, 575.
- Sabaté, E.; Sabaté, E. Adherence to Long-Term Therapies: Evidence for Action; World Health Organization: Geneva, Switzerland, 2003. [Google Scholar]
- Peh, K.Q.E.; Kwan, Y.H.; Goh, H.; Ramchandani, H.; Phang, J.K.; Lim, Z.Y.; Loh, D.H.F.; Østbye, T.; Blalock, D.V.; Yoon, S.; et al. An Adaptable Framework for Factors Contributing to Medication Adherence: Results from a Systematic Review of 102 Conceptual Frameworks. J. Gen. Intern. Med. 2021, 36, 2784–2795. [Google Scholar] [PubMed]
- Tshwane, Co. Primary Healthcare Clinic Services. 2023. Available online: https://wwwtshwanegovza/?page_id=649 (accessed on 12 January 2023).
- Wikipedia. City of Tshwane Metropolitan Municipality. 2023. Available online: https://enwikipediaorg/wiki/City_of_Tshwane_Metropolitan_Municipality#cite_note-adrianfrith-8 (accessed on 12 April 2023).
- Statistic South Africa. Data Reworked by Adrian Frith Tshwane—Census. 2011. Available online: https://census2011adrianfrithcom/place/799 (accessed on 11 March 2020).
- RAOSOFT.COM. Raosoft Sample Size Calculator. 2004. Available online: http://wwwraosoftcom/samplesizehtml (accessed on 10 March 2020).
- Elfil, M.; Negida, A. Sampling methods in Clinical Research; an Educational Review. Emergency 2017, 5, e52. [Google Scholar]
- Allaham, K.K.; Feyasa, M.B.; Govender, R.D.; Musa, A.M.A.; AlKaabi, A.J.; ElBarazi, I.; AlSheryani, S.D.; Al Falasi, R.J.; Khan, M.A.B. Medication Adherence Among Patients with Multimorbidity in the United Arab Emirates. Patient Prefer. Adherence 2022, 16, 1187–1200. [Google Scholar] [CrossRef]
- Diederichs, C.; Berger, K.; Bartels, D.B. The measurement of multiple chronic diseases—A systematic review on existing multimorbidity indices. J. Gerontol. Ser. A Biol. Sci. Med. Sci. 2011, 66, 301–311. [Google Scholar] [CrossRef]
- Maimela, E.; Alberts, M.; Modjadji, S.E.P.; Choma, S.S.R.; Dikotope, S.A.; Ntuli, T.S.; Van Geertruyden, J.-P. The Prevalence and Determinants of Chronic Non-Communicable Disease Risk Factors amongst Adults in the Dikgale Health Demographic and Surveillance System (HDSS) Site, Limpopo Province of South Africa. PLoS ONE 2016, 11, e0147926. [Google Scholar] [CrossRef]
- Zwane, J.; Modjadji, P.; Madiba, S.; Moropeng, L.; Mokgalaboni, K.; Mphekgwana, P.M.; Kengne, A.P.; Mchiza, Z.J.-R. Self-Management of Diabetes and Associated Factors among Patients Seeking Chronic Care in Tshwane, South Africa: A Facility-Based Study. Int. J. Environ. Res. Public Health 2023, 20, 5887. [Google Scholar] [CrossRef] [PubMed]
- Chang, A.Y.; Gómez-Olivé, F.X.; Payne, C.; Rohr, J.K.; Manne-Goehler, J.; Wade, A.N.; Wagner, R.G.; Montana, L.; Tollman, S.; Salomon, J.A. Chronic multimorbidity among older adults in rural South Africa. BMJ Glob. Health 2019, 4, e001386. [Google Scholar] [CrossRef]
- Kwan, Y.H.; Weng, S.D.; Loh, D.H.F.; Phang, J.K.; Oo, L.J.Y.; Blalock, D.V.; Chew, E.H.; Yap, K.Z.; Tan, C.Y.K.; Yoon, S.; et al. Measurement Properties of Existing Patient-Reported Outcome Measures on Medication Adherence: Systematic Review. J. Med. Internet Res. 2020, 22, e19179. [Google Scholar] [CrossRef]
- Naqvi, A.A.; Hassali, M.A.; Rizvi, M.; Zehra, A.; Iffat, W.; Haseeb, A.; Jamshed, S. Development and Validation of a Novel General Medication Adherence Scale (GMAS) for Chronic Illness Patients in Pakistan. Front. Pharmacol. 2018, 9, 1124. [Google Scholar] [CrossRef] [PubMed]
- Sangha, O.; Stucki, G.; Liang, M.H.; Fossel, A.H.; Katz, J.N. The Self-Administered Comorbidity Questionnaire: A new method to assess comorbidity for clinical and health services research. Arthritis Rheum. 2003, 49, 156–163. [Google Scholar] [CrossRef] [PubMed]
- WHO. Physical Status: The Use and Interpretation of Anthropometry; WHO: Geneva, Switzerland, 1995. [Google Scholar]
- WMA. Declaration of Helsinki. Ethical principles for medical research involving human subjects. Jahrb. Wiss. Ethik 2009, 14, 233–238. [Google Scholar]
- Pati, S.; Swain, S.; Metsemakers, J.; Knottnerus, J.A.; van den Akker, M. Pattern and severity of multimorbidity among patients attending primary care settings in Odisha, India. PLoS ONE 2017, 12, e0183966. [Google Scholar] [CrossRef]
- Mphekgwana, P.M.; Malema, N.; Monyeki, K.D.; Mothiba, T.M.; Makgahlela, M.; Kgatla, N.; Makgato, I.; Sodi, T. Hypertension Prevalence and Determinants among Black South African Adults in Semi-Urban and Rural Areas. Int. J. Environ. Res. Public Health 2020, 17, 7463. [Google Scholar] [CrossRef]
- Lloyd-Sherlock, P.; Beard, J.; Minicuci, N.; Ebrahim, S.; Chatterji, S. Hypertension among older adults in low-and middle-income countries: Prevalence, awareness and control. Int. J. Epidemiol. 2014, 43, 116–128. [Google Scholar] [CrossRef]
- Bertram, M.Y.; Jaswal, A.V.; Van Wyk, V.P.; Levitt, N.S.; Hofman, K.J. The non-fatal disease burden caused by type 2 diabetes in South Africa, 2009. Glob. Health Action 2013, 6, 19244. [Google Scholar] [CrossRef] [PubMed]
- Bradshaw, D.; Norman, R.; Pieterse, D.; Levitt, N.S. Estimating the burden of disease attributable to diabetes in South Africa in 2000. S. Afr. Med. J. 2007, 97, 700–706. [Google Scholar] [CrossRef] [PubMed]
- Pheiffer, C.; Pillay-van Wyk, V.; Turawa, E.; Levitt, N.; Kengne, A.P.; Bradshaw, D. Prevalence of Type 2 Diabetes in South Africa: A Systematic Review and Meta-Analysis. Int. J. Environ. Res. Public Health 2021, 18, 5868. [Google Scholar] [CrossRef]
- IDF. IDF Diabetes Atlas, 8th ed.; International Diabetes Federation: Brussels, Belgium, 2017. [Google Scholar]
- Mutyambizi, C.; Pavlova, M.; Hongoro, C.; Groot, W. Inequalities and factors associated with adherence to diabetes self-care practices amongst patients at two public hospitals in Gauteng, South Africa. BMC Endocr. Disord. 2020, 20, 15. [Google Scholar] [CrossRef] [PubMed]
- Gómez-Olivé, F.X.; Ali, S.A.; Made, F.; Kyobutungi, C.; Nonterah, E.; Micklesfield, L.; Alberts, M.; Boua, R.; Hazelhurst, S.; Debpuur, C.; et al. Regional and Sex Differences in the Prevalence and Awareness of Hypertension: An H3Africa AWI-Gen Study Across 6 Sites in Sub-Saharan Africa. Glob. Heart 2017, 12, 81–90. [Google Scholar] [CrossRef]
- Modjadji, P.; Salane, M.C.; Mokwena, K.E.; Mudau, T.S.; Mphekgwana, P.M. Utility of Obesity Indicators for Predicting Hypertension among Older Persons in Limpopo Province, South Africa. Appl. Sci. 2022, 12, 4697. [Google Scholar] [CrossRef]
- Stieglitz, L.-M.; Bärnighausen, T.; Leyna, G.H.; Kazonda, P.; Killewo, J.; Rohr, J.K.; Kohler, S. Patterns of comorbidity and multimorbidity among middle-aged and elderly women in peri-urban Tanzania. J. Multimorb. Comorbidity 2022, 12, 26335565221076254. [Google Scholar] [CrossRef]
- Mabaso, M.; Makola, L.; Naidoo, I.; Mlangeni, L.L.; Jooste, S.; Simbayi, L. HIV prevalence in South Africa through gender and racial lenses: Results from the 2012 population-based national household survey. Int. J. Equity Health 2019, 18, 167. [Google Scholar] [CrossRef]
- Moosa, A.; Gengiah, T.N.; Lewis, L.; Naidoo, K. Long-term adherence to antiretroviral therapy in a South African adult patient cohort: A retrospective study. BMC Infect. Dis. 2019, 19, 775. [Google Scholar] [CrossRef] [PubMed]
- Kubjane, M.; Osman, M.; Boulle, A.; Johnson, L.F. The impact of HIV and tuberculosis interventions on South African adult tuberculosis trends, 1990–2019: A mathematical modeling analysis. Int. Soc. Infect. Dis. 2022, 122, 811–819. [Google Scholar] [CrossRef]
- Roomaney, R.A.; van Wyk, B.; Turawa, E.B.; Pillay-van Wyk, V. Prevalence of multimorbidity in South Africa: A systematic review protocol. BMJ Open 2020, 10, e042889. [Google Scholar] [CrossRef]
- Agborsangaya, C.B.; Lau, D.; Lahtinen, M.; Cooke, T.; Johnson, J.A. Multimorbidity prevalence and patterns across socioeconomic determinants: A cross-sectional survey. BMC Public Health 2012, 12, 201. [Google Scholar] [CrossRef] [PubMed]
- Charlton, J.; Rudisill, C.; Bhattarai, N.; Gulliford, M. Impact of deprivation on occurrence, outcomes and health care costs of people with multiple morbidity. J. Health Serv. Res. Policy 2013, 18, 215–223. [Google Scholar] [CrossRef] [PubMed]
- Moin, J.S.; Moineddin, R.; Upshur, R.E.G. Measuring the association between marginalization and multimorbidity in Ontario, Canada: A cross-sectional study. J. Comorbidity 2018, 8, 2235042X18814939. [Google Scholar] [CrossRef] [PubMed]
- Tetzlaff, J.; Epping, J.; Sperlich, S.; Eberhard, S.; Stahmeyer, J.T.; Geyer, S. Widening inequalities in multimorbidity? Time trends among the working population between 2005 and 2015 based on German health insurance data. Int. J. Equity Health 2018, 17, 103. [Google Scholar] [CrossRef]
- Schiøtz, M.L.; Stockmarr, A.; Høst, D.; Glümer, C.; Frølich, A. Social disparities in the prevalence of multimorbidity—A register-based population study. BMC Public Health 2017, 17, 422. [Google Scholar] [CrossRef]
- Arpey, N.C.; Gaglioti, A.H.; Rosenbaum, M.E. How Socioeconomic Status Affects Patient Perceptions of Health Care: A Qualitative Study. J. Prim. Care Community Health 2017, 8, 169–175. [Google Scholar] [CrossRef]
- Vos, T.; Lim, S.S.; Abbafati, C.; Abbas, K.M.; Abbasi, M.; Abbasifard, M.; Abbasi-Kangevari, M.; Abbastabar, H.; Abd-Allah, F.; Abdelalim, A. Global burden of 369 diseases and injuries in 204 countries and territories, 1990–2019: A systematic analysis for the Global Burden of Disease Study 2019. Lancet 2020, 396, 1204–1222. [Google Scholar] [CrossRef] [PubMed]
- Modjadji, P. Socio-demographic Determinants of Overweight and Obesity Among Mothers of Primary School Children Living in a Rural Health and Demographic Surveillance System Site, South Africa. Open Public Health J. 2020, 13, 518–528. [Google Scholar] [CrossRef]
- Mphekgwana, P.M.; Sono-Setati, M.E.; Mokgophi, T.V.; Kifle, Y.G.; Madiba, S.; Modjadji, P. Retrospective Analysis of the Outcome of Hospitalized COVID-19 Patients with Coexisting Metabolic Syndrome and HIV Using Multinomial Logistic Regression. Int. J. Environ. Res. Public Health 2023, 20, 5799. [Google Scholar] [CrossRef]
- Weimann, A.; Dai, D.; Oni, T. A cross-sectional and spatial analysis of the prevalence of multimorbidity and its association with socioeconomic disadvantage in South Africa: A comparison between 2008 and 2012. Soc. Sci. Med. 2016, 163, 144–156. [Google Scholar] [CrossRef]
- Long, A.N.; Dagogo-Jack, S. Comorbidities of diabetes and hypertension: Mechanisms and approach to target organ protection. J. Clin. Hypertens. 2011, 13, 244–251. [Google Scholar] [CrossRef]
- Kim, M.-J.; Lim, N.-K.; Choi, S.-J.; Park, H.-Y. Hypertension is an independent risk factor for type 2 diabetes: The Korean genome and epidemiology study. Hypertens. Res. 2015, 38, 783–789. [Google Scholar] [CrossRef]
- Kushitor, S.B.; Sanuade, O.A.; Baatiema, L.; Kushitor, M.K.; Afrifa-Anane, E.K.; Awuah, R.B. Non-communicable disease comorbidities in KwaZulu-Natal Province, South Africa. S. Afr. Med. J. 2021, 111, 149–158. [Google Scholar] [CrossRef] [PubMed]
- Mata-Cases M, Franch-Nadal J, Real J, Cedenilla M, Mauricio D: Prevalence and coprevalence of chronic comorbid conditions in patients with type 2 diabetes in Catalonia: A population-based cross-sectional study. BMJ Open. 2019, 9, e031281.
- Luijks, H.; Schermer, T.; Bor, H.; van Weel, C.; Lagro-Janssen, T.; Biermans, M.; de Grauw, W. Prevalence and incidence density rates of chronic comorbidity in type 2 diabetes patients: An exploratory cohort study. BMC Med. 2012, 10, 128. [Google Scholar] [CrossRef]
- Iglay, K.; Hannachi, H.; Joseph Howie, P.; Xu, J.; Li, X.; Engel, S.S.; Moore, L.M.; Rajpathak, S. Prevalence and co-prevalence of comorbidities among patients with type 2 diabetes mellitus. Curr. Med. Res. Opin. 2016, 32, 1243–1252. [Google Scholar] [CrossRef]
- Lalkhen, H.; Mash, R. Multimorbidity in non-communicable diseases in South African primary healthcare. S. Afr. Med. J. 2015, 105, 134–138. [Google Scholar] [CrossRef] [PubMed]
- Banjare, P.; Pradhan, J. Socio-economic inequalities in the prevalence of multi-morbidity among the rural elderly in Bargarh District of Odisha (India). PLoS ONE 2014, 9, e97832. [Google Scholar] [CrossRef] [PubMed]
- Nimako, B.A.; Baiden, F.; Sackey, S.O.; Binka, F. Multimorbidity of chronic diseases among adult patients presenting to an inner-city clinic in Ghana. Glob. Health 2013, 9, 61. [Google Scholar] [CrossRef] [PubMed]
- Papanas, N.; Ziegler, D. Risk factors and comorbidities in diabetic neuropathy: An update 2015. Rev. Diabet. Stud. RDS 2015, 12, 48. [Google Scholar] [CrossRef]
- Ryan, B.L.; Bray Jenkyn, K.; Shariff, S.Z.; Allen, B.; Glazier, R.H.; Zwarenstein, M.; Fortin, M.; Stewart, M. Beyond the grey tsunami: A cross-sectional population-based study of multimorbidity in Ontario. Can. J. Public Health 2018, 109, 845–854. [Google Scholar] [CrossRef] [PubMed]
- Fabbri, E.; Zoli, M.; Gonzalez-Freire, M.; Salive, M.E.; Studenski, S.A.; Ferrucci, L. Aging and Multimorbidity: New Tasks, Priorities, and Frontiers for Integrated Gerontological and Clinical Research. J. Am. Med. Dir. Assoc. 2015, 16, 640–647. [Google Scholar] [CrossRef] [PubMed]
- Enslin, D.; Mallya, P. Factors influencing treatment adherence in hypertension and HIV management in South Africa: A Comparative Literature Review. S. Afr. Fam. Pract. 2022, 64, 5434. [Google Scholar] [CrossRef] [PubMed]
- WHO. Multimorbidity: Technical Series on Safer Primary Care; World Health Organization: Geneva, Switzerland, 2016; Available online: http://apps.who.int/iris/bitstream/10665/252275/1/9789241511650-eng.pdf (accessed on 7 April 2023).
- WHO/UN. Monitoring Health for the SDGs; World Health Organization: Geneva, Switzerland, 2022; Available online: https://www.who.int/data/gho/data/themes/sustainable-development-goals (accessed on 11 April 2023).
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).