Chronic Kidney Disease of Unknown Etiology (CKDu) in Sri Lanka: Hematological Changes and Pro-Inflammation Suggest Likely Predictors of Advance Disease, as Renal Outcomes Show Prevalent Normoalbuminuria
Abstract
1. Introduction
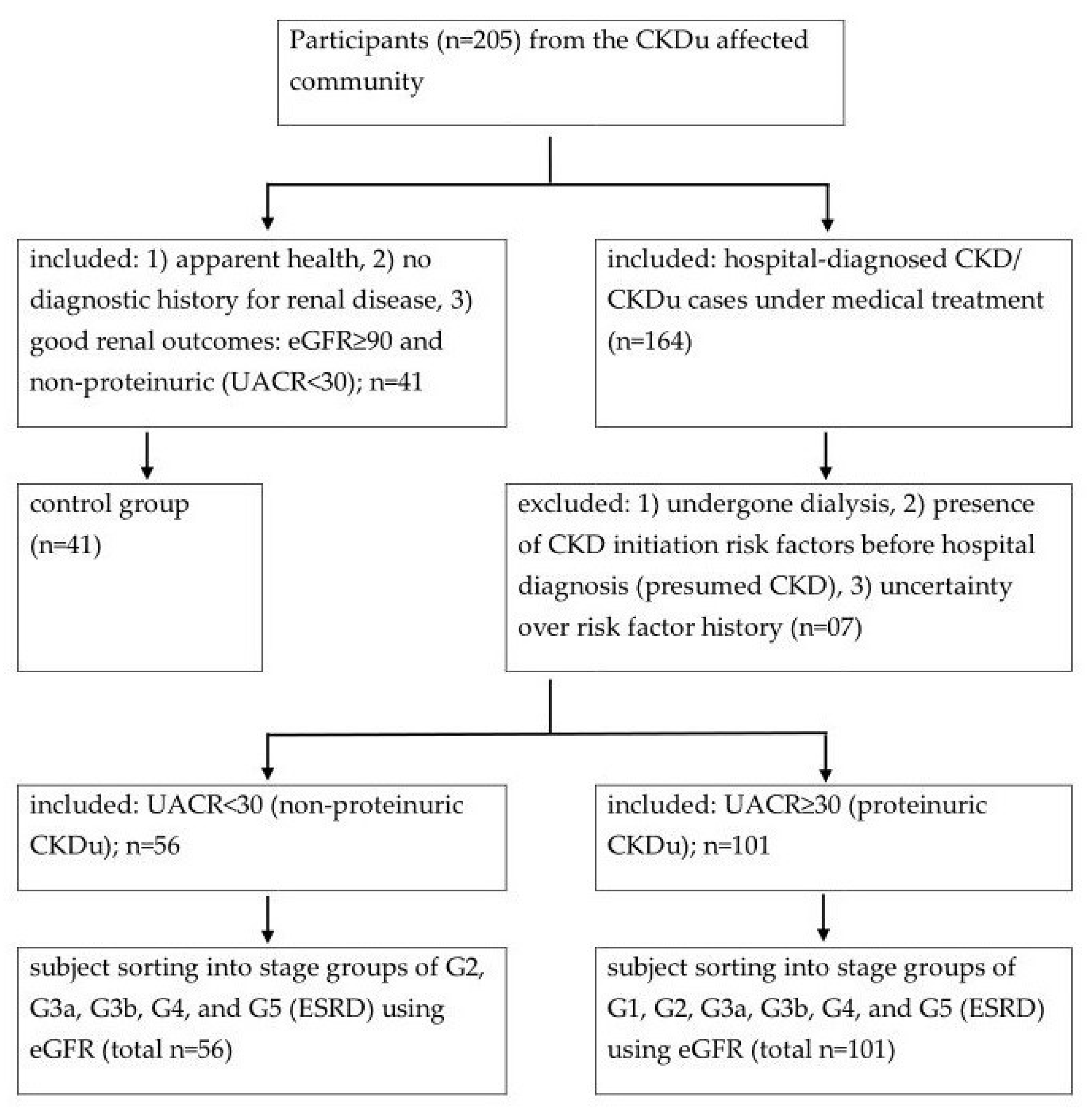
2. Materials and Methods
2.1. Initial Sample Processing
2.2. Kidney Dysfunction Markers
2.3. Subject Sorting into Study Groups
2.4. Cytokine Measurements
2.5. Statistical Analyses
2.6. Assessment of Nonproteinuria
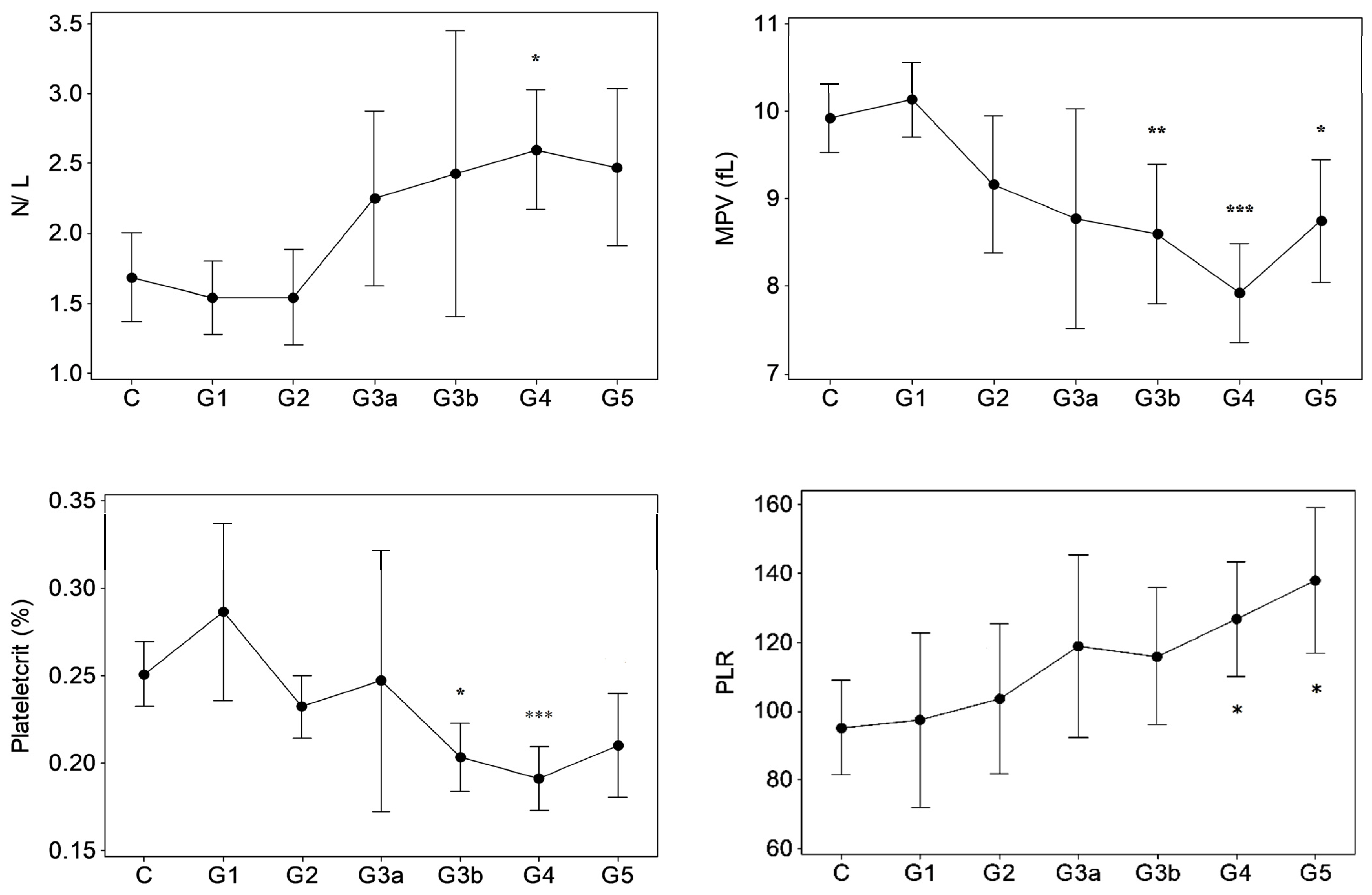
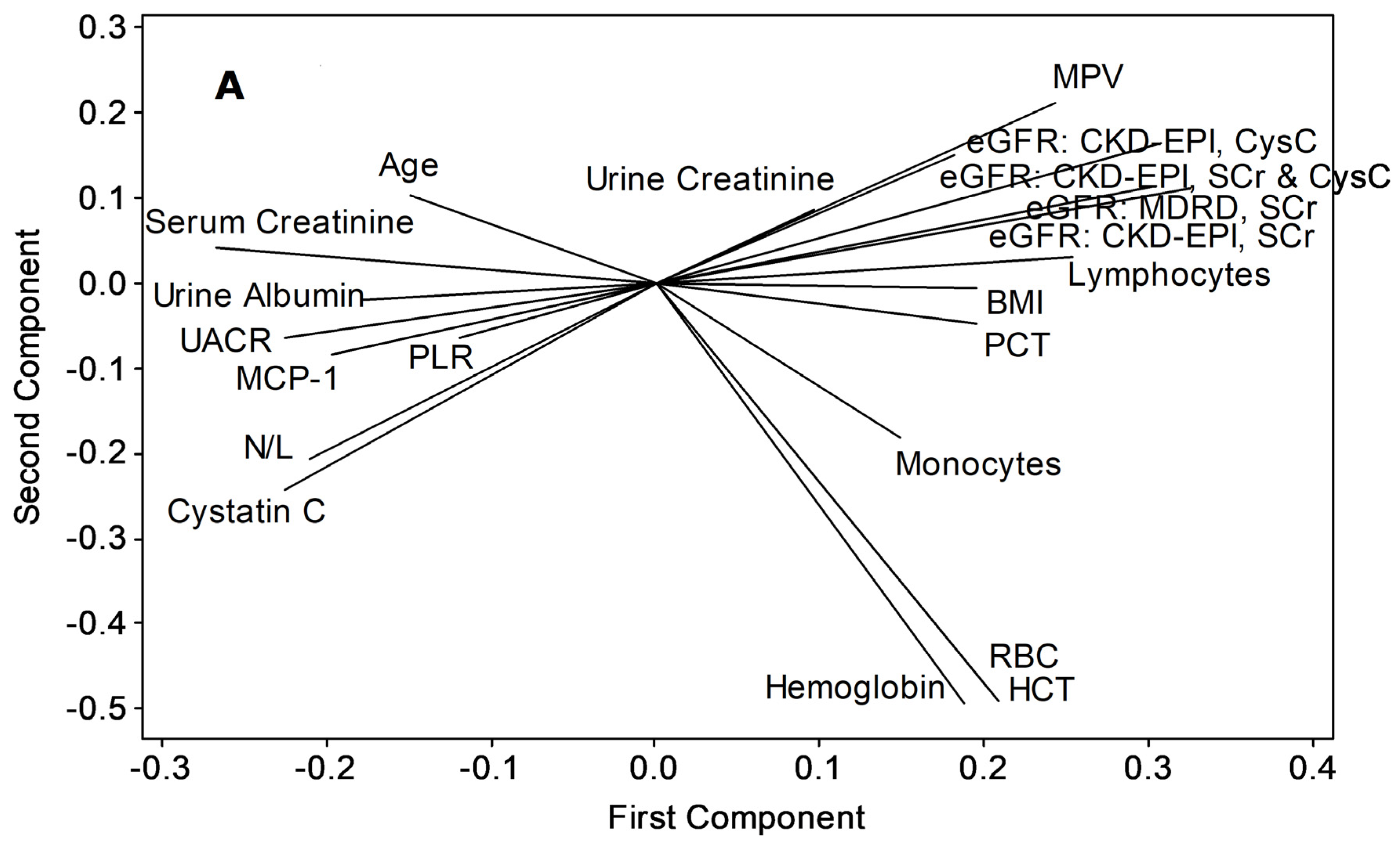
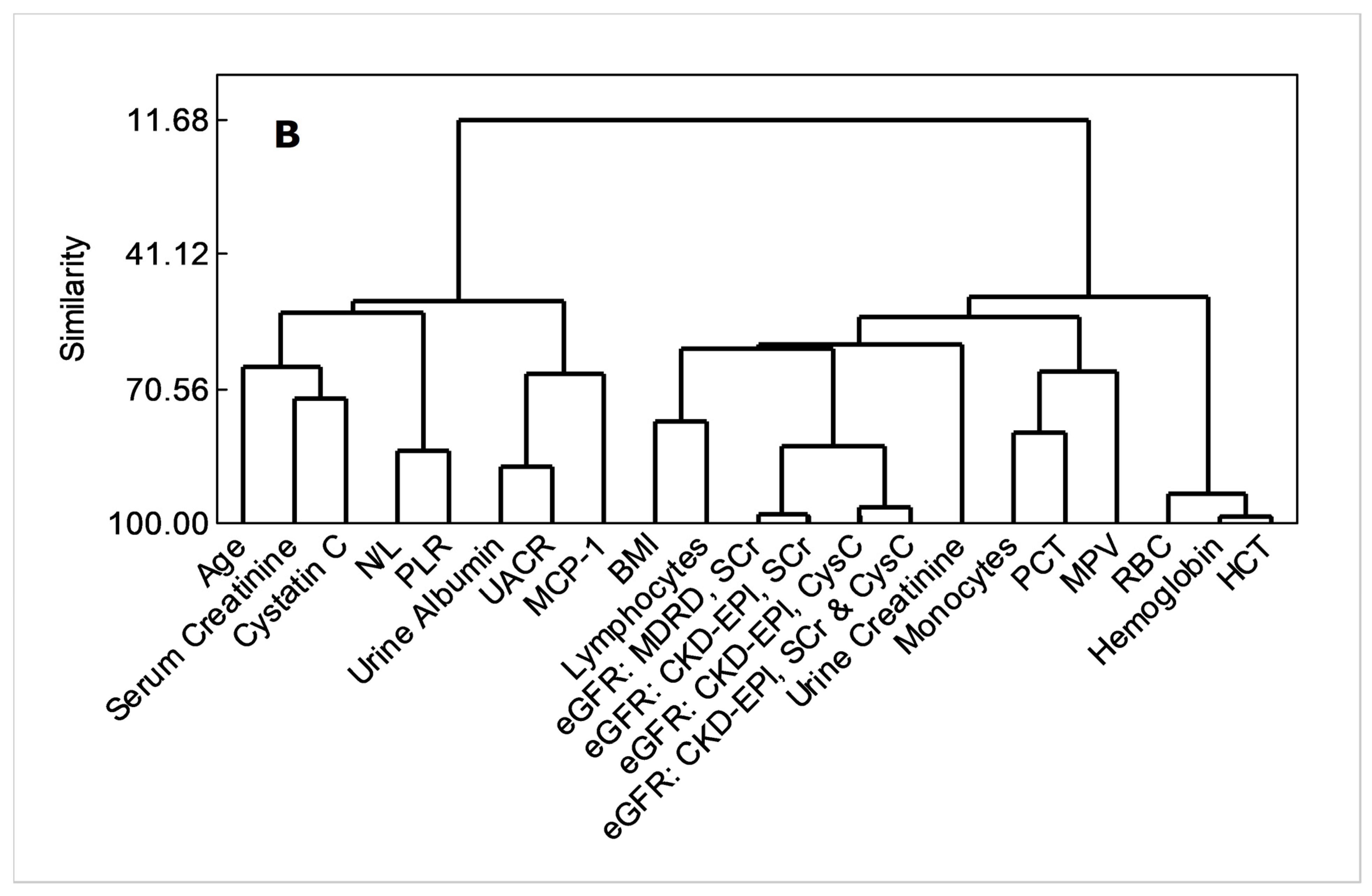
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Ranasinghe, A.V.; Kumara, G.W.G.P.; Karunarathna, R.H.; de Silva, A.P.; Sachintani, K.G.D.; Gunawardena, J.M.C.N.; Kumari, S.K.C.R.; Sarjana, M.S.F.; Chandraguptha, J.S.; de Silva, M.V.C. The incidence, prevalence and trends of chronic kidney disease and chronic kidney disease of uncertain aetiology (CKDu) in the north central province of Sri Lanka: An analysis of 30,566 patients. BMC Nephrol. 2019, 20, 338. [Google Scholar] [CrossRef] [PubMed]
- Kafle, K.; Balasubramanya, S.; Horbulyk, T. Prevalence of chronic kidney disease in Sri Lanka: A profile of affected districts reliant on groundwater. Sci. Total Environ. 2019, 694, 133767. [Google Scholar] [CrossRef] [PubMed]
- Stevens, P.E.; Levin, A. Evaluation and management of chronic kidney disease: Synopsis of the kidney disease: Improving global outcomes 2012 clinical practice guideline. Ann. Intern. Med. 2013, 158, 825–830. [Google Scholar] [CrossRef] [PubMed]
- Badurdeen, Z.; Nanayakkara, N.; Ratnatunga, N.V.; Wazil, A.W.; Abeysekera, T.D.; Rajakrishna, P.N.; Alwis, A.P. Chronic kidney disease of uncertain etiology in Sri Lanka is a possible sequel of interstitial nephritis! clinicopathological profile of symptomatic, newly-diagnosed CKDu patients. Clin. Nephrol. 2016, 86 (Suppl. S1), 106–109. [Google Scholar] [CrossRef] [PubMed]
- Nangaku, M. Chronic Hypoxia and Tubulointerstitial Injury: A final common pathway to end-stage renal failure. J. Am. Soc. Nephrol. 2005, 17, 17–25. [Google Scholar] [CrossRef] [PubMed]
- McMurray, J.; Parfrey, P.; Adamson, J.W.; Aljama, P.; Berns, J.S.; Bohlius, J.; Weiss, G. Kidney disease: Improving global outcomes (KDIGO) anemia work group. KDIGO clinical practice guideline for anemia in chronic kidney disease. Kidney Inter. Suppl. 2012, 2, 283–287. [Google Scholar]
- Xiang, F.-F.; Zhu, J.-M.; Cao, X.-S.; Shen, B.; Zou, J.-Z.; Liu, Z.-H.; Zhang, H.; Teng, J.; Liu, H.; Ding, X.-Q. Lymphocyte depletion and subset alteration correlate to renal function in chronic kidney disease patients. Ren. Fail. 2016, 38, 7–14. [Google Scholar] [CrossRef] [PubMed]
- Mihai, S.; Codrici, E.; Popescu, I.D.; Enciu, A.-M.; Albulescu, L.; Necula, L.G.; Mambet, C.; Anton, G.; Tanase, C. Inflammation-related mechanisms in chronic kidney disease prediction, progression, and outcome. J. Immunol. Res. 2018, 2018, 2180373. [Google Scholar] [CrossRef]
- Levey, A.S.; Eckardt, K.-U.; Tsukamoto, Y.; Levin, A.; Coresh, J.; Rossert, J.; Zeeuw, D.D.; Hostetter, T.H.; Lameire, N.; Eknoyan, G. Definition and classification of chronic kidney disease: A position statement from kidney disease: Improving global outcomes (KDIGO). Kidney Int. 2005, 67, 2089–2100. [Google Scholar] [CrossRef]
- Inker, L.A.; Schmid, C.H.; Tighiouart, H.; Eckfeldt, J.H.; Feldman, H.I.; Greene, T.; Kusek, J.W.; Manzi, J.; van Lente, F.; Zhang, Y.L.; et al. Estimating glomerular filtration rate from serum creatinine and cystatin C. N. Engl. J. Med. 2012, 367, 20–29. [Google Scholar] [CrossRef] [PubMed]
- Levey, A.S.; Coresh, J.; Balk, E.; Kausz, A.T.; Levin, A.; Steffes, M.W.; Hogg, R.J.; Perrone, R.D.; Lau, J.; Eknoyan, G. National kidney foundation practice guidelines for chronic kidney disease: Evaluation, classification, and stratification. Ann. Intern. Med. 2003, 139, 137–147. [Google Scholar] [CrossRef] [PubMed]
- National Kidney Foundation. Kidney Disease. Outcome Quality Initiative (K/DOQI). Clinical practice guidelines for chronic kidney disease: Evaluation, classification, and stratification. Am. J. Kidney Dis. 2002, 2 (Suppl. 1), S1–S266. [Google Scholar]
- Yamanouchi, M.; Furuichi, K.; Hoshino, J.; Ubara, Y.; Wada, T. Nonproteinuric diabetic kidney disease. Clin. Exp. Nephrol. 2020, 24, 573–581. [Google Scholar] [CrossRef] [PubMed]
- Athuraliya, T.N.C.; Abeysekera, D.T.D.J.; Amerasinghe, P.H.; Kumarasiri, P.V.R.; Dissanayake, V. Prevalence of chronic kidney disease in two tertiary care hospitals: High proportion of cases with uncertain aetiology. Ceylon. Med. J. 2009, 54, 23–25. [Google Scholar] [CrossRef] [PubMed]
- Jayasekara, K.B.; Dissanayake, D.M.; Sivakanesan, R.; Ranasinghe, A.; Karunarathna, R.H.; Kumara, G.W.G.P. Epidemiology of chronic kidney disease, with special emphasis on chronic kidney disease of uncertain etiology, in the north central region of Sri Lanka. J. Epidemiol. 2015, 25, 275–280. [Google Scholar] [CrossRef] [PubMed]
- Roumeliotis, S.K.; Stamou, A.; Panagoutsos, S.; Roumeliotis, A.K.; Thodis, E.; Passadakis, P. Association of red blood distribution width (RDW) with carotid atherosclerosis and deterioration of chronic kidney disease in patients with type 2 diabetes mellitus. Nephrol. Dial. Transpl. 2016, 31 (Suppl. S1), 422–438. [Google Scholar] [CrossRef][Green Version]
- Babitt, J.L.; Lin, H.Y. Mechanisms of Anemia in CKD. J. Am. Soc. Nephrol. 2012, 23, 1631–1634. [Google Scholar] [CrossRef] [PubMed]
- Solak, Y.; Gaipov, A.; Turk, S.; Kayrak, M.; Yilmaz, M.I.; Caglar, K.; Verim, S.; Unal, H.U.; Gok, M.; Demirkaya, E.; et al. Red cell distribution width is independently related to endothelial dysfunction in patients with chronic kidney disease. Am. J. Med. Sci. 2014, 347, 118–124. [Google Scholar] [CrossRef] [PubMed]
- Yoshitomi, R.; Nakayama, M.; Sakoh, T.; Fukui, A.; Katafuchi, E.; Seki, M.; Tsuda, S.; Nakano, T.; Tsuruya, K.; Kitazono, T. High neutrophil/lymphocyte ratio is associated with poor renal outcomes in Japanese patients with chronic kidney disease. Ren. Fail. 2019, 41, 238–243. [Google Scholar] [CrossRef] [PubMed]
- Okyay, G.U.; Inal, S.; Öneç, K.; Er, R.E.; Paşaoğlu, Ö.; Pasaoglu, H.; Derici, U.; Erten, Y. Neutrophil to lymphocyte ratio in evaluation of inflammation in patients with chronic kidney disease. Ren. Fail. 2013, 35, 29–36. [Google Scholar] [CrossRef] [PubMed]
- Yuan, Q.; Wang, J.; Peng, Z.; Zhou, Q.; Xiao, X.; Xie, Y.; Wang, W.; Huang, L.; Tang, W.; Sun, D.; et al. Neutrophil-to-lymphocyte ratio and incident end-stage renal disease in chinese patients with chronic kidney disease: Results from the chinese cohort study of chronic kidney disease (C-STRIDE). J. Transl. Med. 2019, 17, 1–8. [Google Scholar] [CrossRef]
- Agarwal, R.; Light, R.P. Patterns and prognostic value of total and differential leukocyte count in chronic kidney disease. Clin. J. Am. Soc. Nephrol. 2011, 6, 1393–1399. [Google Scholar] [CrossRef]
- Litjens, N.H.; van Druningen, C.J.; Betjes, M. Progressive loss of renal function is associated with activation and depletion of naive T lymphocytes. Clin. Immunol. 2006, 118, 83–91. [Google Scholar] [CrossRef] [PubMed]
- Kato, S.; Chmielewski, M.; Honda, H.; Pecoits-Filho, R.; Matsuo, S.; Yuzawa, Y.; Tranaeus, A.; Stenvinkel, P.; Lindholm, B. Aspects of Immune dysfunction in end-stage renal disease. Clin. J. Am. Soc. Nephrol. 2008, 3, 1526–1533. [Google Scholar] [CrossRef] [PubMed]
- Eardley, K.; Zehnder, D.; Quinkler, M.; Lepenies, J.; Bates, R.; Savage, C.; Howie, A.; Adu, D.; Cockwell, P. The relationship between albuminuria, MCP-1/CCL2, and interstitial macrophages in chronic kidney disease. Kidney Int. 2006, 69, 1189–1197. [Google Scholar] [CrossRef] [PubMed]
- Heine, G.H.; Ortiz, A.; Massy, Z.A.; Lindholm, B.; Wiecek, A.; Martínez-Castelao, A.; Fliser, D.; Covic, A.; Goldsmith, D.; Süleymanlar, G.; et al. Monocyte subpopulations and cardiovas-cular risk in chronic kidney disease. Nat. Rev. Nephrol. 2012, 8, 362–369. [Google Scholar] [CrossRef] [PubMed]
- Gregg, L.P.; Tio, M.C.; Li, X.; Adams-Huet, B.; de Lemos, J.A.; Hedayati, S.S. Association of monocyte chemoattractant protein-1 with death and atherosclerotic events in chronic kidney disease. Am. J. Nephrol. 2018, 47, 395–405. [Google Scholar] [CrossRef]
- Coyne, D.W.; Fleming, R. Will targeting interleukin-6 in the anemia of CKD change our treatment paradigm? J. Am. Soc. Nephrol. 2021, 32, 6–8. [Google Scholar] [CrossRef] [PubMed]
- Su, H.; Lei, C.-T.; Zhang, C. Interleukin-6 signaling pathway and its role in kidney disease: An update. Front. Immunol. 2017, 8, 405. [Google Scholar] [CrossRef] [PubMed]
- Kaw, D.; Malhotra, D. Platelet dysfunction and end-stage renal disease. Semin. Dial. 2006, 19, 317–322. [Google Scholar] [CrossRef] [PubMed]
- Linthorst, G.E.; Avis, H.J.; Levi, M. Uremic thrombocytopathy is not about urea. J. Am. Soc. Nephrol. 2010, 21, 753–755. [Google Scholar] [CrossRef] [PubMed]
- Ju, H.Y.; Kim, J.K.; Hur, S.M.; Woo, S.A.; Park, K.A.; Park, M.Y.; Choi, S.J.; Hwang, S.D. Could mean platelet volume be a promising biomarker of progression of chronic kidney disease? Platelets 2015, 26, 143–147. [Google Scholar] [CrossRef]
- Van Bladel, E.R.; de Jager, R.L.; Walter, D.; Cornelissen, L.; Gaillard, C.A.; Boven, L.A.; Fijnheer, R.; Roest, M. Platelets of patients with chronic kidney disease demonstrate deficient platelet reactivity in vitro. BMC Nephrol. 2012, 13, 127. [Google Scholar] [CrossRef] [PubMed]
- Li, P.; Xia, C.; Liu, P.; Peng, Z.; Huang, H.; Wu, J.; He, Z. Neutrophil-to-lymphocyte ratio and platelet-to-lymphocyte ratio in evaluation of inflammation in non-dialysis patients with end-stage renal disease (ESRD). BMC Nephrol. 2020, 21, 1–8. [Google Scholar] [CrossRef] [PubMed]
- Bolignano, D.; Zoccali, C. Non-proteinuric rather than proteinuric renal diseases are the leading cause of end-stage kidney disease. Nephrol. Dial. Transplant. 2017, 32, ii194–ii199. [Google Scholar] [CrossRef] [PubMed]
- Jayatilake, N.; Mendis, S.; Maheepala, P.; Mehta, F.R. Chronic kidney disease of uncertain aetiology: Prevalence and causative factors in a developing country. BMC Nephrol. 2013, 14, 180. [Google Scholar] [CrossRef] [PubMed]
- Redmon, J.H.; Elledge, M.F.; Womack, D.S.; Wickremashinghe, R.; Wanigasuriya, K.P.; Peiris-John, R.J.; Lunyera, J.; Smith, K.; Raymer, J.H.; Levine, K.E. Additional perspectives on chronic kidney disease of unknown aetiology (CKDu) in Sri Lanka –lessons learned from the WHO CKDu population prevalence study. BMC Nephrol. 2014, 15, 125. [Google Scholar] [CrossRef] [PubMed]



| eGFR (MDRD, sCr) mL/min/1.73 m2 | eGFR (CKD-EPI, sCr) mL/min/1.73 m2 | UACR mg/g | |
|---|---|---|---|
| MCHC (g/dL) | −0.303 * | −0.343 * | |
| Basophils (103 µL) | −0.308 * | ||
| Lymphocytes (103 µL) | 0.382 * | 0.411 * | |
| Monocytes (103 µL) | 0.318 * | 0.304 * | |
| N/L | −0.331 * | ||
| MPV (fL) | 0.461 * | 0.480 * | −0.357 * |
| PCT (%) | 0.396 * | 0.425 * | |
| PLR | −0.329 * |
| Control 1 | G2 1 | G3a 1 | G3b 1 | G4 1 | G5 | eGFR (MDRD, sCr) 2 | eGFR (CKD-EPI, sCr) 2 | |
|---|---|---|---|---|---|---|---|---|
| Basophils (103/µL) | 0.03 ± 0.17 | 0.02 ± 0.02 | 0.07 ± 0.03 *** | 0.05 ± 0.03 | 0.05 (0.03) | 0.08 (NA) | r = −0.30 ** | r = −0.36 *** |
| Lymphocytes (103/µL) | 2.76 ± 1.15 | 2.21 ± 1.24 | 2.93 ± 0.68 | 2.73 ± 0.47 | 1.83 ± 1.15 * | 2.38 (NA) | NS | NS |
| N/L | 1.66 ± 0.96 | 1.60 ± 0.49 | 1.77 ± 0.60 | 1.57 ± 0.36 | 2.69 ± 1.43 ** | 2.04 (NA) | NS | NS |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Gunawickrama, S.H.N.P.; Hewavitharana, K.I.G.; Nanayakkara, P.G.C.L.; Gunawickrama, K.B.S. Chronic Kidney Disease of Unknown Etiology (CKDu) in Sri Lanka: Hematological Changes and Pro-Inflammation Suggest Likely Predictors of Advance Disease, as Renal Outcomes Show Prevalent Normoalbuminuria. Diseases 2022, 10, 2. https://doi.org/10.3390/diseases10010002
Gunawickrama SHNP, Hewavitharana KIG, Nanayakkara PGCL, Gunawickrama KBS. Chronic Kidney Disease of Unknown Etiology (CKDu) in Sri Lanka: Hematological Changes and Pro-Inflammation Suggest Likely Predictors of Advance Disease, as Renal Outcomes Show Prevalent Normoalbuminuria. Diseases. 2022; 10(1):2. https://doi.org/10.3390/diseases10010002
Chicago/Turabian StyleGunawickrama, S. H. Nandana P., K. Imesha G. Hewavitharana, P. G. Chandra L. Nanayakkara, and K. B. Suneetha Gunawickrama. 2022. "Chronic Kidney Disease of Unknown Etiology (CKDu) in Sri Lanka: Hematological Changes and Pro-Inflammation Suggest Likely Predictors of Advance Disease, as Renal Outcomes Show Prevalent Normoalbuminuria" Diseases 10, no. 1: 2. https://doi.org/10.3390/diseases10010002
APA StyleGunawickrama, S. H. N. P., Hewavitharana, K. I. G., Nanayakkara, P. G. C. L., & Gunawickrama, K. B. S. (2022). Chronic Kidney Disease of Unknown Etiology (CKDu) in Sri Lanka: Hematological Changes and Pro-Inflammation Suggest Likely Predictors of Advance Disease, as Renal Outcomes Show Prevalent Normoalbuminuria. Diseases, 10(1), 2. https://doi.org/10.3390/diseases10010002





