Abstract
Introduction: Periodontitis is the most prevalent inflammatory disease worldwide. Its inflammatory levels spread systemically, which can be associated with chronic kidney disease. Biomarkers have the potential to diagnose and correlate periodontitis and chronic kidney disease, helping to monitor systemic inflammation. Thereby, this study aimed to analyze the association between chronic kidney disease and periodontitis by conducting a biomarker analysis on blood and saliva. Material and methods: An electronic search through PubMed/MEDLINE, EMBASE, and Web of Science databases was conducted to identify clinical studies published in the last ten years, with no language restrictions. Twelve articles met all the inclusion criteria, two randomized controlled trials, one cohort study, and nine observational studies. Results: The studies included a total of 117 patients for saliva biomarkers, with a mean age of approximately 57 years old, and 56.68% of the subjects were female. After analyzing all the included studies, it was possible to verify the following biomarkers assessed: CRP, WBC, fibrinogen, IL-4 and -6, cardiac troponin T, NOx, ADMA, albumin, osteocalcin, cystatin C, PGLYRP1, cholesterol, HDL, LDL, triglycerides, and hemoglobin. Conclusion: A direct cause–effect association between periodontitis and CKD could not be established. However, it was possible to conclude that there was a correlating effect present, through the analyzed biomarkers.
1. Introduction
Chronic kidney disease (CKD) consists of a progressive and irreversible change to the normal kidney function and/or damage to the renal parenchyma at the glomerular, tubular, or endocrine level [1,2,3]. It is characterized by the loss of the filtration capacity of the kidneys and the consequent accumulation of organic residues (urea) that cause immunodeficiency due to the increase of toxic substances in the bloodstream. In addition, there is a loss of hormonal production capacity, control of the electrolyte balance, and blood pressure [1,2,3,4].
Moreover, CKD patients have oral manifestations, with radiographic changes in bone density, more significant accumulation of dental plaque [4], bleeding on the oral mucosa associated with alterations in platelet aggregation, and renal anemia [5]. Furthermore, these oral manifestations are related to xerostomia, in which the patients are typically prone to dry mouth and retrograde parotitis. Beyond one-third of hemodialysis patients have halitosis (“uremic fetor”) and experience a metallic taste due to the high content of urea in saliva [4,6].
Furthermore, burning mouth syndrome is frequently seen as an additional symptom in dialysis patients [6]. It presents lesions, localized or generalized erythematous areas, covered by pseudomembranous exudates, that leave an intact or ulcerated mucosa [6]. Moreover, studies [6,7] reported that 4% of patients undergoing hemodialysis suffer from angular cheilitis and lichen planus, which can arise in association with antihypertensive medication.
In addition, CKD positively correlates with periodontal disease viability due to systemic inflammatory burden and low immunity, with a greater predisposition or worsening of the periodontal condition. Furthermore, periodontal disease may be one of the aggravating factors of progression or mortality in CKD patients (bidirectional cause–effect relationship) [1,4,8,9,10,11]. The presence of periodontal disease simultaneously worsens the prognosis due to the increased systemic inflammatory load and bacterial translocation. Still, the treatment and control can act as an adjunct therapy for both [1].
Moreover, cross-sectional studies conducted in different countries reported that severe periodontitis was significantly more frequent, severe, and prevalent among CKD patients [12,13,14,15,16].
However, in periodontal disease and in several chronic systemic diseases, such as CKD, an early diagnosis is essential. Classically, CKD is evidenced by blood and/or urine laboratory tests, or salivary biomarkers [8,17]. The literature has presented crevicular and salivary fluids analyses as laboratory tests to detect periodontitis. Saliva is the biofluid most studied and analyzed by the scientific community [18,19], and is collected in a non-invasive way in order to reduce the patient’s anxiety levels (no needle, which makes it easier and faster) [11,20]. In terms of storage, it is also easier than for blood as saliva does not clot [11,18,21].
Biomarkers exist in various forms belonging to five different fields: genomics, transcriptomics, proteomics, interactomics, and metabolomics. Changes in the concentration, structure, function, or action of the various components can be associated with the onset, progression, or even regression. In this way, salivary biomarkers serve as a valuable and attractive tool in the detection, risk assessment, diagnosis, prognosis, and monitoring of the disease [22,23].
At the salivary level, patients with chronic renal failure, compared to healthy individuals, have an elevated salivary pH, increased systemic inflammatory activity, and higher concentrations of C-reactive protein (CRP), urea, sodium, and potassium, in conjunction with significantly lower calcium values [10,24,25]. Studies have shown that the concentrations of some metabolites in saliva, such as creatinine, urea, and potassium, differ according to the renal failure degree and treatment with dialysis [26].
CKD patients suffer from the suppression of humoral and cellular immune responses, which leads to subnormal immunoglobulin (Ig) A and IgG concentrations [27]. According to studies, it is possible to find changes in the salivary inflammatory biomarkers in patients with CKD by analyzing interleukin (IL) 1β (IL-1β), IL-6, IL-8, tumor necrosis factor-α (TNF-α), interferon-γ (INF-γ), monocyte chemoattractant protein-1 (MCP-1), and intercellular adhesion molecule-1 (sICAM-1) [11]. In addition, the greater part of these cytokines are present in periodontitis, mainly IL-1, IL-6, and TNF-α, which can lead to tissue destruction and the consequent loss of insertion [1,9,11,22,28]. Moreover, other important salivary biomarkers that are increased in periodontitis are metalloproteinase (MMP)-8, MMP-9, and the inflammatory protein of macrophages-1α (MIP-1α or CCL3) [29].
The medical system depends on a correct diagnosis to adequately construct a treatment plan, and the salivary analysis can be relevant in this aspect. It can be applied in many subareas, which can involve kidney disease or periodontitis [11,18,21,22,30,31,32]. Thus, it will allow the clinician to make an informed decision on the diagnosis and treatment choice without wasting hours waiting for classical laboratory exams. Therefore, this systematic review sought to analyze the correlation between CKD and periodontitis within this context, with regards to assessing the existence of and changes in blood and salivary biomarkers.
2. Materials and Methods
This systematic review followed the Preferred Reporting Items for Systematic reviews and Meta-Analysis (PRISMA) guidelines. The focal question was determined according to the Population (P), Intervention (I), Comparison (C), and Outcome (O), PICO strategy. The protocol for this systematic review was registered in the PROSPERO platform (Centre for Reviews and Dissemination/CRD—University of York) and, consequently, accepted with the acceptance number CRD42020168324.
2.1. Focal Question
The focal question for the present review was as follows: “In clinical studies of patients with chronic kidney disease and periodontitis (P), will the analysis of saliva biomarkers (I), or of blood biomarkers (C), exhibit important outcomes (O)?
2.2. Information Sources and Search Strategy
A systematic search of the literature published in the last eleven years was carried out (1 January 2010–31 January 2021). Three bibliographic databases were used to search as thoroughly as possible (PubMed, Web of Science, and Embase). In each search engine, the search was adapted to its characteristics, based on Boolean operators (AND, OR) to combine searches for mesh terms, Emtree terms, and common terms. In PubMed, Web of Science, and Embase, the following terms were used: (“chronic kidney disease” OR “chronic renal disease”) AND (periodontitis OR “periodontal disease”) AND (“inflammatory biomarkers”) AND (“blood biomarkers” OR “salivary biomarkers”). Articles written in any language were included (Table 1). Searches in the reference lists of the included studies (cross-referencing) were also conducted. All used articles were stored in the bibliographic management platform Mendeley.

Table 1.
Search strategy carried out and filters applied.
2.3. Inclusion and Exclusion Criteria
Inclusion and exclusion criteria were designed to permit replicability. Only human studies were included. Furthermore, articles from different languages and with less than ten years of publication were analyzed to get the most recent evidence possible.
Exclusion criteria consisted of previously performed systematic reviews and meta-analyses, studies unrelated to patients with CKD and/or periodontitis, and studies that did not address salivary/blood biomarkers. Moreover, studies that did not involve humans, and only analyzed crevicular fluid or urine, were also excluded.
2.4. Study Selection
The selection of studies was carried out based on strict selection criteria, date of publication, and target population. In order to be transparent and replicable, the study selection followed the inclusion and exclusion criteria detailed in Table 2.

Table 2.
Inclusion and exclusion criteria used for selection of the articles.
Duplicate articles were excluded, and the remaining were elected through the initial reading of the title and abstract. The reviewers (L.T.R.T. and S.M.S.R.P.S.) individually screened the papers, and any disagreements between reviewers were discussed with a third reviewer (G.V.O.F.), who made the final decision.
2.5. Data Extraction and Assessment of Bias
Included were trials that enrolled patients with CKD and periodontitis for the analysis of salivary/blood biomarkers. Two reviewers extracted the following data: year of publication, study design, participants (population setting), study period, summary characteristics of study participants (age, gender, periodontal disease, CKD stage, HbA1c, smoking habits), biofluid analysis, biomarkers analyzed, and study results.
Assessment of risk of bias and study quality of the included investigations was performed independently by two reviewers (L.T.R.T. and G.V.O.F.), where the STROBE Statement was applied. The guidelines featured 22 items that were answered with one of four options: (1) yes, (2) no, (3) cannot answer, and (4) not applicable. Only items with option (1) generated the score. Therefore, each article could obtain a score of between 0 (no criteria fulfilled) and 22 (all criteria fulfilled).
The data collected using the STROBE statement was rated as low quality if it scored 0–7 out of 18 points, moderate quality if it scored 8–15, or high quality if it scored between 16 and 22. The ratings obtained were verified by a third reviewer (N.J.V.), and any discrepancy was resolved by discussion with another reviewer (J.F.L.M.).
3. Results
3.1. Study Selection
A total of 7051 articles were identified through database searching, 467 from PubMed, 4221 from Web of Science, and 2363 from Embase. A further 16 publications were considered from the manual search through the references of the included articles. From 7067 articles, 108 were excluded due to duplication. Therefore, 6959 articles were screened by title and abstract based on the inclusion and exclusion criteria (Table 2). After the title and abstract screening, 43 articles were included for further analysis. Subsequently, there was a full-text assessment, in which 31 articles were excluded based on the exclusion criteria detailed in Table 3. Twelve articles [33,34,35,36,37,38,39,40,41,42,43,44] met the inclusion criteria and were included in the current review (Figure 1).

Table 3.
Excluded studies and reason for exclusions.
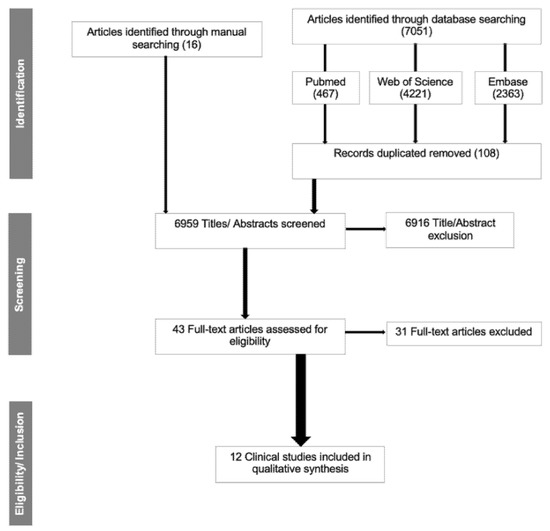
Figure 1.
Flow diagram for the search strategy and selection process.
3.2. Study Characteristics
Within the 12 studies selected for analysis, only two were randomized controlled trials (RCT), one was a cohort study (CS), and nine were observational studies (OB) (seven out of nine were cross-sectional studies, CSS), all published between January 2010 and January 2021. The studies included a total of 102,000 patients for blood biomarkers and 117 patients for saliva biomarkers, with a mean age of approximately 57 years old (ranging between 23 and 86 years), and 56.68% of the subjects were female.
All the investigations studied the periodontitis and CKD condition of the patients. Regarding the CKD condition, from 12 studies, all patients had a compromised kidney function, varying from CKD stage 1 to end-stage renal disease (ESRD) or required renal replacement therapy (RRT). Only one study used a completely healthy control group [33]. Six studies compared healthy oral patients and patients with different levels of periodontitis. Most of the studies also considered other health markers, such as diabetes and smoking habits (Table 4).

Table 4.
Description of the factors investigated in the included studies.
Of the 12 studies, 11 conducted a blood collection, and only one [43] used saliva to obtain the required data. Different types of biomarkers were analyzed, such as metabolism, nutritional, inflammatory, and bacterial biomarkers.
3.3. Chronic Kidney Disease (CKD) and Periodontal Disease
Regarding CKD, in eight articles, the subjects required RRT, and most of them were undergoing hemodialysis (HD) [33,34,35,36,37,38,43,45]. Perozini et al. [36] was the only study that managed to examine the patients at all stages of the disease (from CKD stage 1 to stage 5). Chen et al. [44] defined patients with CKD as having an estimated glomerular filtration rate (eGFR) of 68.76 (±17.6 mL/min/1.73 m2), which means that patients’ conditions were between CKD stage 2 and stage 3.
Concerning periodontal disease, all studies included patients with periodontitis. Seven out of 12 studies made a comparison between patients with periodontitis and patients without periodontitis [33,34,35,37,38,39,46]. None of the studies classified periodontal disease by the new classification of the World Workshop on the Classification of Periodontal and Peri-implant Diseases and Conditions [47]. Furthermore, one study (Hou et al., 2017) did not distinguish gingivitis from periodontitis, due to their similar pathologies.
3.4. Biomarkers
After analyzing all the included studies (Table S2), it was possible to verify the following biomarkers that were assessed: (i) C-reactive protein (CRP), (ii) white blood cells (WBC), (iii) fibrinogen, (iv) IL-4, (v) IL-6, (vi) cardiac troponin T (TnT), (vii) nitric oxide (NOx), (viii) asymmetric dimethylarginine (ADMA), (ix) albumin, (x) osteocalcin, (xi) cystatin C, (xii) peptidoglycan recognition protein 1 (PGLYRP1), (xiii) cholesterol, (xiv) high-density lipoprotein (HDL), (xv) low-density lipoprotein (LDL), (xvi) triglycerides, and (xvii) hemoglobin. In order to describe these biomarkers and verify the relationships among them, further analysis, presented in Table S1 and Figure S1, was performed.
CRP, an inflammatory biomarker, was studied in seven articles [34,35,36,37,38,40,41], making up 58.33% of the investigated studies. In Cotic et al. [34], 63.1% of the patients with CKD had a CRP higher than 3 mg/L. Therefore, this study did not prove any significant relationship between elevated CRP levels and periodontal disease and observed that early tooth loss resulting from an oral infection was the possible cause of levels higher than 10 mg/L in edentulous patients. Likewise, in Perozini et al. [36], CRP levels were higher than the reference value, although no significance was found. On the other hand, the other articles showed significantly higher levels of CRP in patients with periodontitis. According to Veisa et al. [38], the CKD patient’s periodontitis led to high levels of CRP, decreasing the patients’ quality of life. Grubbs et al. [40] demonstrated that intensive and local periodontal treatment reduces the CRP levels.
One study considered WBC count [37] and reported a significantly elevated quantity of WBCs in CKD patients with periodontitis. Although fibrinogen is also a biomarker of inflammatory activity, only Perozini et al. [36] incorporated it into their analysis. They found that fibrinogen appeared to be higher in the predialysis patients with periodontitis, although, despite this, they were still within the reference values. The article by Ksiazek et al. [33] showed that changes in 3VNTR polymorphism in the IL-4 gene might be a risk factor in the progression of CKD and periodontitis. Regarding IL-6, another cytokine involved in the inflammatory response and directly linked to periodontitis, Grubbs et al. [40] showed that IL-6 concentration decreased after intensive periodontal treatment.
Cotic et al. [34] could not make a direct association between the influence of oral health on the cardiovascular biomarkers that are usually elevated in CKD patients, such as cardiac troponin T (TnT) and nitric oxide (NOx). Conversely, Grubbs et al. [40] found that asymmetric dimethylarginine (ADMA), an endothelial dysfunction marker, decreased after periodontal treatment in CKD patients. Hemoglobin was used as a biomarker by Hou et al. [37] and Chen et al. [44]; however, the values were normal in CKD patients with and without periodontitis in both studies.
Five articles studied albumin as a biomarker [35,38,39,42,44]. Two of them pointed to a possible association between periodontitis in CKD patients and hypoalbuminemia [35,38]. Garneata et al. [35] reported that 93% of malnourished patients (albumin < 3.5 g/dL) had periodontitis. Rodrigues et al. [39] also studied phosphorous concentration and concluded that CKD patients without periodontitis had a higher concentration than patients with periodontitis. Nevertheless, Hou et al. [37] did not find any significance in the variation of phosphorous concentration. Regarding bone metabolism, Yoshihara et al. [41] studied osteocalcin as a biomarker. They found that osteocalcin in patients with CKD had a significant positive relationship with periodontitis, in which the worst periodontal condition meant higher levels of osteocalcin.
Cystatin C is a biomarker of kidney function; only one article [41] used it to define kidney function (cystatin C > 0.91 mg/L indicates poor kidney function). The authors found a significant positive association between serum cystatin C and periodontal disease, concluding that patients with decreased kidney function had a higher probability of periodontal disease.
Arenious et al. [43] conducted a sequential study based on four previously published studies. This was the only study in the present analysis that collected saliva as a source for analysis. In this study, the authors found that complications related to peritoneal dialysis had no relationship with periodontal disease. Still, complications related to HD were associated with Staphylococcus aureus and, consequently, with high levels of peptidoglycan recognition protein 1 (PGLYRP1).
Total cholesterol, and high-density lipoprotein (HDL) and low-density lipoprotein (LDL) levels were studied in two of the twelve articles [37,39]. Only Hou et al. [37] found a statistical significance for total cholesterol between CKD patients with or without periodontitis, documenting higher levels in the periodontitis group. In Chen et al. [44], HDL and total cholesterol were statistically lower in the non-periodontitis group. Triglycerides were also used as a metabolic biomarker [36,37,44]. Significantly high levels of triglycerides in predialysis and HD patients with periodontitis were reported by Perozini et al. [36]. On the other hand, Hou et al. [37] and Chen et al. [44] did not find any significance in the variation of triglyceride levels.
Overall, our study results indicate that periodontal disease is highly prevalent in CKD patients, and that there is a relationship between them [33,34,35,36,37,38,39,40,41,42,43,44,46]. Yoshihara et al. [41] concluded that CKD and periodontitis could have a reciprocal effect. In three studies, the authors discovered that an interdisciplinary treatment must be done in order to improve oral and systemic health [36,39,40]. Chen et al. [44] and Cotic et al. [34] added that periodontal disease increased the cardiovascular mortality risk in CKD patients, while Veisa et al. [38] concluded that the presence of periodontal disease in CKD patients reduced their quality of life.
3.5. Other Health Risk Factors (Smoking and Diabetes)
Although several studies have taken into account smoking habits and diabetes, only two studies found significant results [35,37]. These studies also reported that patients with diabetes and that smoked had increased probabilities of having periodontal disease.
4. Discussion
This systematic review analyzed the correlation between CKD and periodontitis with regards to blood and salivary biomarkers, which permitted the inclusion of 12 articles. To the best of our knowledge, this is the first systematic review that evaluates the current evidence for the association between chronic kidney disease and periodontitis by analyzing either saliva or blood as biomarkers. The included articles were led by different principles; however, they all examined the relationship between periodontal disease and CKD. Unfortunately, some studies did not distinguish periodontitis from gingivitis, which may lead to bias. Furthermore, it is important to highlight the scientific evidence that showed that diabetes and smoking habits increased the possibility of having periodontal disease [48,49,50]. Moreover, it is important to emphasize that treating periodontitis in a CKD patient will reduce the systemic inflammation level beyond improving the oral condition.
CRP is a well-known inflammatory protein, and it can be found in the blood and the saliva. This protein influences systemic diseases, such as CKD, and oral infections, such as periodontitis [51,52,53]. Although two studies did not find statistically significant results for this biomarker, other studies reported that patients with CKD and periodontitis had higher levels of CRP, causing a high level of chronic inflammation, with undesirable consequences for the patients’ health [26,27].
Romandini et al. [54] concluded that periodontitis influences WBC count by an increase in systemic inflammation, and Arai et al. [55] concluded that WBC is independently associated with CKD progression. These two articles that studied WBC showed high levels in patients with periodontitis, suggesting a systemic inflammation caused by periodontitis [37,46,56,57].
Similar to CRP, fibrinogen is a biomarker of inflammatory activity [36]. The study that analyzed fibrinogen as a biomarker discovered that values were higher in patients with periodontal disease; otherwise, the values were within the reference values [36]. Moreover, IL-4 and IL-6 are important cytokines in systemic inflammation, and studies have demonstrated that high levels of these cytokines are present in patients with periodontitis [11,58]. Further studies regarding proinflammatory cytokines must be conducted.
Asymmetric dimethylarginine (ADMA) is one of the endothelial disfunction markers responsible for atherosclerosis in CKD patients [59]. One study showed a decrease in ADMA after periodontal treatment, demonstrating that periodontal therapy can be essential to maintain systemic health [60].
Hypoalbuminemia is considered a strong predictor of an adverse prognosis in CKD patients [61]. The article that analyzed albumin concentration found that CKD patients with periodontitis had lower albumin levels, indicating that their health was at risk [62]. Another study regarding albumin levels supports these results and found that there might be an inverse relationship between periodontal disease and serum albumin concentration [63].
Phosphorous concentration was taken into consideration in one of the included studies. Individuals with higher a phosphorous concentration tended to more easily develop dental calculus [64]. Therefore, it was expected that CKD patients with periodontitis had higher phosphorus concentrations; however, studies reported that periodontitis had a lower concentration of phosphorus. These results would mean a positive correlation, in which having periodontitis would lead to the CKD patient having a low phosphorus concentration and, consequently, to better health of the patient. It is known that phosphorus concentration reduction is particularly important to prevent bone impairment and CVD in patients with CKD [65,66]. Rodrigues et al. [39] had some limitations in their study and proposed the development of new studies will enable us to draw accurate conclusions.
One of the studies found that osteocalcin level had a significant positive relationship with periodontitis in CKD patients, with the worst periodontal condition correlated to a higher level of osteocalcin [41]. Conversely, a recently published study concluded a nonsignificant correlation between osteocalcin level and periodontitis severity [67]. Osteocalcin is a bone-forming biomarker, and periodontitis is a chronic disease characterized by the loss of periodontal attachment; thereby, there is a contrast between the effects associated with periodontitis and the presence of higher osteocalcin levels. However, higher osteocalcin levels in CKD meant a higher osteoclast activity, which may lead to bone loss [68].
A significant positive association between the serum cystatin C and periodontal disease was found in one study. These results supported a previous study showing that the level of cystatin C could be used as a marker in chronic periodontitis [41,69]. In addition, increased levels of cystatin C are associated with decreased kidney function, meaning that in the presence of both diseases (periodontitis and CKD), cystatin C was higher, and this can lead to the worst periodontal condition and kidney function [70].
HD complications were related to Staphylococcus aureus and, consequently, with high levels of peptidoglycan recognition protein 1 (PGLYRP1) [6], showing a possible relationship between HD complications and oral infection. PGLYRP1 functions as a ligand that activates TREM-1 during illness, so the high values of this biomarker indicate that the patient is probably suffering from systematic inflammation due to periodontitis [71,72,73,74]. Higher values of this biomarker may lead to, or worsen, the prognosis of several diseases, such as rheumatoid arthritis, systemic lupus erythematosus, inflammatory bowel disease, type 1 diabetes, psoriasis cystic fibrosis, sepsis, and even atherosclerotic complications, the latter being one of the leading causes of mortality in patients with CKD [71,72,75].
The results related to total cholesterol, and high-density lipoprotein (HDL) and low-density lipoprotein (LDL) levels, proved subjective and insufficient, as they were contradictory. It is crucial that these biomarkers are studied further, as high concentrations may increase the risk of atherosclerosis, the leading cause of death in CKD patients [10,76,77].
Combining the present study’s conclusions, periodontal disease is highly prevalent in CKD patients, and there is a possible cause–consequence relationship between them [33,34,35,36,39,40,41,43,46]. Interdisciplinary treatment is essential and must be delivered in order to improve oral and systemic health [36,39,40,46]. Cardiovascular disease is one of the main causes of mortality in CKD patients, and periodontitis can influence the prognosis [34,46]. Furthermore, it was found that the presence of periodontal disease in CKD patients lowered their QoL [38].
Finally, the limitations of this study involved the low number of included articles; thus, analysis was confined to the limited data obtained, indicating considerable heterogeneity. Moreover, the lack of standardization regarding the types of proteins analyzed made it difficult to conduct comparisons among studies.
5. Conclusions
Within the limitations of this systematic study, it was still possible to realize its importance, due to the systemic inflammation caused by the increase in the proinflammatory response in the presence of periodontitis. The included articles were not enough to establish a direct cause–effect association between periodontitis and CKD, or vice-versa, although promising results were found regarding the biomarkers linking both diseases. Thereby, it was concluded that periodontal treatment therapy can help CKD patient’s prognoses and improve their quality of life, and it must be taken into consideration.
More clinical studies analyzing biomarkers should be performed in order to achieve more predictable and accurate prognoses during the treatment of patients with CKD by controlling the persistent systematic inflammation caused by periodontal disease, first using basic periodontal treatment and targeted therapies.
Supplementary Materials
The following supporting information can be downloaded at: https://www.mdpi.com/article/10.3390/diseases10010012/s1, Figure S1: Proteins found in the included studies (cross-link). Table S1: Details about the proteins and other biological indicators used as biomarkers in the included studies. Table S2: Biomarkers analyzed in the included studies.
Author Contributions
Conceptualization, G.V.d.O.F. and L.T.R.T.; methodology, G.V.d.O.F.; validation, L.T.R.T., M.S.-S. and G.V.d.O.F.; formal analysis, L.T.R.T., M.S.-S. and G.V.d.O.F.; investigation, L.T.R.T., M.S.-S. and G.V.d.O.F.; data curation, L.T.R.T., M.S.-S. and G.V.d.O.F.; writing—original draft preparation, L.T.R.T. and G.V.d.O.F.; writing—review and editing, G.V.d.O.F., L.T.R.T. and R.d.M.C.; supervision, G.V.d.O.F. and J.F.L.-M.; project administration, L.T.R.T., M.S.-S. and G.V.d.O.F.; funding acquisition, N.J.V. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Not applicable.
Data Availability Statement
All original data were obtained from the articles cited in the respective text. No other value was used or added.
Conflicts of Interest
The authors report there are no competing interests to declare.
References
- Frazão, C.M.F.Q.; Delgado, M.F.; Araújo, M.G.A.; Silva, F.B.B.L.; Sá, J.D.; Lira, A.L.B.C. Nursing care for chronic renal patients on hemodialysis. Rev. Rene. 2014, 15, 701–709. [Google Scholar] [CrossRef]
- Schmalz, G.; Schiffers, N.; Schwabe, S.; Vasko, R.; Müller, G.A.; Haak, R.; Mausberg, R.F.; Ziebolz, D. Dental and periodontal health, and microbiological and salivary conditions in patients with or without diabetes undergoing haemodialysis. Int. Dent. J. 2017, 67, 186–193. [Google Scholar] [CrossRef] [PubMed]
- Altamimi, A.; AlBakr, S.; Alanazi, T.; Alshahrani, F.; Chalisserry, E.; Anil, S. Prevalence of Periodontitis in Patients Undergoing Hemodialysis: A Case Control Study. Mater. Sociomed. 2018, 30, 58–61. [Google Scholar] [CrossRef] [PubMed]
- Schmalz, G.; Kauffels, A.; Kollmar, O.; Slotta, J.E.; Vasko, R.; Müller, G.A.; Haak, R.; Ziebolz, D. Oral behavior, dental, periodontal and microbiological findings in patients undergoing hemodialysis and after kidney transplantation. BMC Oral Health 2016, 16, 72. [Google Scholar] [CrossRef]
- Bostanci, N.; Selevsek, N.; Wolski, W.; Grossmann, J.; Bao, K.; Wahlander, A.; Trachsel, C.; Schlapbach, R.; Öztürk, V.Ö.; Afacan, B.; et al. Targeted proteomics guided by label-free quantitative proteome analysis in saliva reveal transition signatures from health to periodontal disease. Mol. Cell. Proteom. 2018, 17, 1392–1409. [Google Scholar] [CrossRef]
- Ramirez, J.; Higuera, N.; Mancilla, M.; Coronilla, G.; Bustamante, J.; López, A. Use of Biomarkers for the Diagnosis of Periodontitis. In Periodontal Disease-Diagnostic and Adjunctive Non-Surgical Considerations; IntechOpen: London, UK, 2019; pp. 1–21. [Google Scholar]
- Kaczor-Urbanowicz, K.E.; Martin Carreras-Presas, C.; Aro, K.; Tu, M.; Garcia-Godoy, F.; Wong, D.T.W. Saliva diagnostics—Current views and directions. Exp. Biol. Med. 2017, 242, 459–472. [Google Scholar] [CrossRef]
- Tomás, I.; Marinho, J.S.; Limeres, J.; Santos, M.J.; Araújo, L.; Diz, P. Changes in salivary composition in patients with renal failure. Arch. Oral Biol. 2008, 53, 528–532. [Google Scholar] [CrossRef]
- Donato, H.; Donato, M. Stages for undertaking a systematic review. Acta Med. Port. 2019, 32, 227–235. [Google Scholar] [CrossRef]
- Poli, F.E.; Gulsin, G.S.; McCann, G.P.; Burton, J.O.; Graham-Brown, M.P. The assessment of coronary artery disease in patients with end-stage renal disease. Clin. Kidney J. 2019, 12, 721–734. [Google Scholar] [CrossRef]
- Prasad, S.; Tyagi, A.K.; Aggarwal, B.B. Detection of inflammatory biomarkers in saliva and urine: Potential in diagnosis, prevention, and treatment for chronic diseases. Exp. Biol. Med. 2016, 241, 783–799. [Google Scholar] [CrossRef]
- Klassen, J.T.; Krasko, B.M. The dental health status of dialysis patients. J. Can. Dent. Assoc. 2002, 68, 34–38. [Google Scholar] [PubMed]
- Duran, I.; Erdemir, E.O. Periodontal treatment needs of patients with renal disease receiving haemodialysis. Int. Dent. J. 2004, 54, 274–278. [Google Scholar] [CrossRef] [PubMed]
- Souza, C.R.; Liberio, S.A.; Guerra, R.N.; Monteiro, S.; Silveira, E.J.; Pereira, A.L. Assessment of periodontal condition of kidney patients in hemodialysis. Rev. Assoc. Med. Bras. 2005, 51, 285–289. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Chen, L.P.; Chiang, C.K.; Chan, C.P.; Hung, K.Y.; Huang, C.S. Does periodontitis reflect inflammation and malnutrition status in hemodialysis patients? Am. J. Kidney Dis. 2006, 47, 815–822. [Google Scholar] [CrossRef] [PubMed]
- Craig, R.G. Interactions between chronic renal disease and periodontal disease. Oral Dis. 2008, 14, 1–7. [Google Scholar] [CrossRef]
- Kinney, J.S.; Morelli, T.; Braun, T.; Ramseier, C.A.; Herr, A.E.; Sugai, J.V.; Shelburne, C.E.; Rayburn, L.A.; Singh, A.K.; Giannobile, W.V. Saliva/Pathogen Biomarker Signatures and Periodontal Disease Progressio. J. Dent. Res. 2011, 90, 752–758. [Google Scholar] [CrossRef] [PubMed]
- Malamud, D. Saliva as a Diagnostic Fluid. Dent. Clin. N. Am. 2011, 55, 159–178. [Google Scholar] [CrossRef]
- Siddaway, A.P.; Wood, A.M.; Hedges, L.V. How to Do a Systematic Review: A Best Practice Guide for Conducting and Reporting Narrative Reviews, Meta-Analyses, and Meta-Syntheses. Annu. Rev. Psychol. 2018, 70, 747–770. [Google Scholar] [CrossRef]
- Celec, P.; Tóthová, L.; Šebeková, K.; Podracká, L.; Boor, P. Salivary markers of kidney function—Potentials and limitations. Clin. Chim. Acta 2016, 453, 28–37. [Google Scholar] [CrossRef]
- Maciejczyk, M.; Szulimowska, J.; Skutnik, A.; Taranta-Janusz, K.; Wasilewska, A.; Wiśniewska, N.; Zalewska, A. Salivary Biomarkers of Oxidative Stress in Children with Chronic Kidney Disease. J. Clin. Med. 2018, 7, 209. [Google Scholar] [CrossRef]
- Kim, J.J.; Kim, C.J.; Camargo, P.M. Salivary biomarkers in the diagnosis of periodontal diseases. J. Calif. Dent. Assoc. 2013, 41, 119–124. [Google Scholar] [PubMed]
- Lee, J.Y.; Antoniazzi, M.C.C.; Perozini, C.; Ruivo, G.F.; Pallos, D. Prevalence of carotid artery calcification in patients with chronic renal disease identified by panoramic radiography. Oral Surg. Oral Med. Oral Pathol. Oral Radiol. 2014, 118, 612–618. [Google Scholar] [CrossRef] [PubMed]
- Pallos, D.; Leao, M.V.; Togeiro, F.C.; Alegre, L.; Ricardo, L.H.; Perozini, C.; Ruivo, G.F. Salivary markers in patients with chronic renal failure. Arch. Oral Biol. 2015, 60, 1784–1788. [Google Scholar] [CrossRef] [PubMed]
- Costantinides, F.; Castronovo, G.; Vettori, E.; Frattini, C.; Artero, M.L.; Bevilacqua, L.; Berton, F.; Nicolin, V.; Di Lenarda, R. Dental care for patients with end-stage renal disease and undergoing hemodialysis. Int. J. Dent. 2018, 2018, 9610892. [Google Scholar] [CrossRef]
- Rysz, J.; Gluba-Brzózka, A.; Franczyk, B.; Jablonowski, Z.; Cialkowska-Rysz, A. Novel biomarkers in the diagnosis of chronic kidney disease and the prediction of its outcome. Int. J. Mol. Sci. 2017, 18, 1702. [Google Scholar] [CrossRef]
- Akar, H.; Akar, G.C.; Carrero, J.J.; Stenvinkel, P.; Lindholm, B. Systemic consequences of poor oral health in chronic kidney disease patients. Clin. J. Am. Soc. Nephrol. 2011, 6, 218–226. [Google Scholar] [CrossRef]
- Nylund, K.M.; Ruokonen, H.; Sorsa, T.; Heikkinen, A.M.; Meurman, J.H.; Ortiz, F.; Tervahartiala, T.; Furuholm, J.; Bostanci, N. Association of the Salivary Triggering Receptor Expressed on Myeloid Cells/ its Ligand Peptidoglycan Recognition Protein 1 Axis with Oral Inflammation Kidney Disease. J. Periodontol. 2018, 89, 117–129. [Google Scholar] [CrossRef] [PubMed]
- Nylund, K.M.; Meurman, J.H.; Heikkinen, A.M.; Honkanen, E.; Vesterinen, M.; Furuholm, J.O.; Tervahartiala, T.; Sorsa, T.; Ruokonen, H.M. Periodontal Inflammatory Burden and Salivary MMP-8 Concentration Among Chronic Kidney Disease Patients at Predialysis Stage. J. Periodontol. 2015, 86, 1212–1220. [Google Scholar] [CrossRef]
- Ebersole, J.L.; Nagarajan, R.; Akers, D.; Miller, C.S. Targeted salivary biomarkers for discrimination of periodontal health and disease(s). Front. Cell. Infect. Microbiol. 2015, 5, 1–12. [Google Scholar] [CrossRef]
- Ji, S.; Choi, Y. Point-of-care diagnosis of periodontitis using saliva: Technically feasible but still a challenge. Front. Cell. Infect. Microbiol. 2015, 5, 1–9. [Google Scholar] [CrossRef]
- Akram, Z.; Abduljabbar, T.; Abu Hassan, M.I.; Javed, F.; Vohra, F. Cytokine profile in chronic periodontitis patients with and without obesity: A systematic review and meta-analysis. Dis. Markers. 2016, 2016, 4801418. [Google Scholar] [CrossRef] [PubMed]
- Ksiazek, K.; Blaszczak, J.; Buraczynska, M. IL4 gene VNTR polymorphism in chronic periodontitis in end-stage renal disease patients. Oral Dis. 2019, 25, 258–264. [Google Scholar] [CrossRef] [PubMed]
- Cotič, J.; Ferran, M.; Karišik, J.; Jerin, A.; Pussinen, P.J.; Nemec, A.; Pavlica, Z.; Buturović-Ponikvar, J.; Petelin, M. Oral health and systemic inflammatory, cardiac and nitroxid biomarkers in hemodialysis patients. Med. Oral Patol. Oral Cir. Bucal. 2017, 22, e432–e439. [Google Scholar] [CrossRef] [PubMed]
- Garneata, L.; Slusanschi, O.; Preoteasa, E.; Corbu-stancu, A.; Mircescu, G. Periodontal status, inflammation, and malnutrition in hemodialysis patients—Is there a link? J. Ren. Nutr. 2014, 25, 1–8. [Google Scholar] [CrossRef] [PubMed]
- Perozini, C.; Ruivo, G.F.; Ricardo, L.H.; Pavesi, L.A.; Kim, Y.J.; Pallos, D. Medical and periodontal clinical parameters in patients at different levels of chronic renal failure. Int. J. Dent. 2017, 2017, 9858073. [Google Scholar] [CrossRef]
- Hou, Y.; Wang, X.; Zhang, C.X.; Wei, Y.D.; Jiang, L.L.; Zhu, X.Y.; Du, Y.J. Risk factors of periodontal disease in maintenance hemodialysis patients. Medicine 2017, 96, 1–5. [Google Scholar] [CrossRef]
- Veisa, G.; Tasmoc, A.; Nistor, I.; Segall, L.; Siriopol, D.; Solomon, S.M.; Donciu, M.D.; Voroneanu, L.; Nastasa, A.; Covic, A. The impact of periodontal disease on physical and psychological domains in long-term hemodialysis patients: A cross-sectional study. Int. Urol. Nephrol. 2017, 49, 1261–1266. [Google Scholar] [CrossRef]
- Rodrigues, V.P.; Libério, S.A.; Lopes, F.F.; Thomaz, E.B.; Guerra, R.N.; Gomes-Filho, I.S.; Pereira, A.L. Periodontal status and serum biomarkers levels in haemodialysis patients. J. Clin. Periodontol. 2014, 41, 862–868. [Google Scholar] [CrossRef]
- Grubbs, V.; Garcia, F.; Vittinghoff, E.; Jue, B.L.; Ryder, M.; Lovett, D.H.; Offenbacher, S.; Taylor, G.; Ganz, P.; Bibbins-Domingo, K.; et al. Nonsurgical Periodontal Therapy in CKD: Findings of the Kidney and Periodontal Disease (KAPD) Pilot Randomized Controlled Trial. Kidney Med. 2019, 2, 49–58. [Google Scholar] [CrossRef]
- Yoshihara, A.; Iwasaki, M.; Miyazaki, H.; Nakamura, K. Bidirectional relationship between renal function and periodontal disease in older Japanese women. J. Clin. Periodontol. 2016, 43, 720–726. [Google Scholar] [CrossRef]
- Ausavarungnirun, R.; Wisetsin, S.; Rongkiettechakorn, N.; Chaichalermsak, S.; Udompol, U.; Rattanasompattikul, M. Association of dental and periodontal disease with chronic kidney disease in patients of a single, tertiary care centre in Thailand. BMJ Open 2016, 6, e011836. [Google Scholar] [CrossRef] [PubMed]
- Arenius, I.; Ruokonen, H.; Ortiz, F.; Furuholm, J.; Välimaa, H.; Bostanci, N.; Eskola, M.; Maria Heikkinen, A.; Meurman, J.H.; Sorsa, T.; et al. The relationship between oral diseases and infectious complications in patients under dialysis. Oral Dis. 2020, 26, 1045–1052. [Google Scholar] [CrossRef] [PubMed]
- Chen, Y.T.; Shih, C.J.; Ou, S.M.; Hung, S.C.; Lin, C.H.; Tarng, D.C. Periodontal Disease and Risks of Kidney Function Decline and Mortality in Older People: A community-based cohort study. Am. J. Kidney Dis. 2015, 66, 223–230. [Google Scholar]
- Rodrigues Gomes, S.S.; Barretobezerra, A.C.; Maia Prado, A.C. Salivary biomarkers, vital signs and behaviour of pre-school children during their first dental visit. Eur. J. Paediatr. Dent. 2013, 14, 279–283. [Google Scholar]
- Kshirsagar, A.V.; Grubbs, V. Periodontal disease and CKD-associated morbidity: Is there now enough evidence to move from observation to intervention? Am. J. Kidney Dis. 2015, 66, 181–183. [Google Scholar]
- Caton, J.G.; Armitage, G.; Berglundh, T.; Chapple, I.L.; Jepsen, S.; Kornman, K.S.; Mealey, B.L.; Papapanou, P.N.; Sanz, M.; Tonetti, M.S.; et al. A new classification scheme for periodontal and peri-implant diseases and conditions—Introduction and key changes from the 1999 classification. J. Periodontol. 2018, 89 (Suppl. 1), S1–S8. [Google Scholar] [CrossRef]
- García, E.; Padilla, A.; Romo, S.; Ramírez, M. Oral mucosa symptoms, signs and lesions, in end stage renal disease and non-end stage renal disease diabetic patients. Med. Oral Patol. Oral Cir. Bucal. 2006, 11, 467–473. [Google Scholar]
- Becherucci, F.; Roperto, R.M.; Materassi, M.; Romagnani, P. Chronic kidney disease in children. Clin. Kidney J. 2016, 9, 583–591. [Google Scholar] [CrossRef]
- Coelho, J.M.F.; Miranda, S.S.; da Cruz, S.S.; Dos Santos, D.N.; Trindade, S.C.; Cerqueira, E.D.M.; Passos-Soares, J.D.S.; Costa, M.D.C.N.; Figueiredo, A.C.M.; Hintz, A.M.; et al. Common mental disorder is associated with periodontitis. J. Periodontal Res. 2020, 55, 221–228. [Google Scholar] [CrossRef]
- Cavelti-Weder, C.; Babians-Brunner, A.; Keller, C.; Stahel, M.A.; Kurz-Levin, M.; Zayed, H.; Solinger, A.M.; Mandrup-Poulsen, T.; Dinarello, C.A.; Donath, M.Y.; et al. Effects of Gevokizumab on Glycemia and infalmatory Markers in Type 2 Diabetes. Diabetes Care 2012, 35, 1654–1662. [Google Scholar] [CrossRef]
- Zhao, G.; Dharmadhikari, G.; Maedler, K.; Meyer-Hermann, M. Possible Role of Interleukin-1 b in Type 2 Diabetes Onset and Implications for Anti-inflammatory Therapy Strategies. PLoS Comput. Biol. 2014, 10, e1003798. [Google Scholar] [CrossRef] [PubMed]
- Dioguardi, M.; Caloro, G.A.; Troiano, G.; Giannatempo, G.; Laino, L.; Petruzzi, M.; Lo Muzio, L. Oral manifestations in chronic uremia patients. Ren. Fail. 2015, 38, 1–6. [Google Scholar] [CrossRef] [PubMed]
- Romandini, M.; Cordaro, M.; Laforí, A.; Romandini, P.; Baima, G. Periodontitis and platelet count: A new potential link with cardiovascular and other systemic inflammatory diseases. J. Clin. Periodontol. 2018, 45, 1299–1310. [Google Scholar] [CrossRef] [PubMed]
- Arai, Y.; Kanda, E.; Iimori, S.; Naito, S. Low white blood cell count is independently associated with chronic kidney disease progression in the elderly: The CKD-ROUTE study. Clin. Exp. Nephrol. 2018, 22, 291–298. [Google Scholar] [CrossRef] [PubMed]
- Gupta, M.; Gupta, M. Oral conditions in renal disorders and treatment considerations—A review for pediatric dentist. Saudi Dent. J. 2015, 27, 113–119. [Google Scholar] [CrossRef] [PubMed]
- Rudick, C.P.; Miyamoto, T.; Lang, M.S.; Agrawal, D.K. Triggering receptor expressed on myeloid cells in the pathogenesis of periodontitis: Potential novel treatment strategies. Expert Rev. Clin. Immunol. 2017, 13, 1189–1197. [Google Scholar] [CrossRef]
- Opal, S.M.; Depalo, V.A. Anti-Inflammatory Cytokines. Chest 2000, 117, 1162–1172. [Google Scholar] [CrossRef]
- Jamieson, L.; Skilton, M.; Maple-Brown, L.; Kapellas, K.; Askie, L.; Hughes, J.; Arrow, P.; Cherian, S.; Fernandes, D.; Pawar, B.; et al. Periodontal disease and chronic kidney disease among Aboriginal adults; An RCT. BMC Nephrol. 2015, 16, 181. [Google Scholar] [CrossRef]
- Iwagami, M.; Mansfield, K.E.; Hayes, J.F.; Walters, K.; Osborn, D.P.; Smeeth, L.; Nitsch, D.; Tomlinson, L.A. Severe mental illness and chronic kidney disease: A cross-sectional study in the United Kingdom. Clin. Epidemiol. 2018, 10, 421–429. [Google Scholar] [CrossRef]
- Zhao, D.; Khawaja, A.T.; Jin, L.; Li, K.Y.; Tonetti, M.; Pelekos, G. The directional and non-directional associations of periodontitis with chronic kidney disease: A systematic review and meta-analysis of observational studies. J. Periodontal Res. 2018, 53, 682–704. [Google Scholar] [CrossRef]
- Fitzpatrick, A.; Mohammadi, F.; Jesudason, S. Managing pregnancy in chronic kidney disease: Improving outcomes for mother and baby. Int. J. Women’s Health 2016, 8, 273–285. [Google Scholar]
- Deschamps-Lenhardt, S.; Martin-Cabezas, R.; Hannedouche, T.; Huck, O. Association between periodontitis and chronic kidney disease: Systematic review and meta-analysis. Oral Dis. 2019, 25, 385–402. [Google Scholar] [CrossRef] [PubMed]
- Sharma, P.; Dietrich, T.; Ferro, C.J.; Cockwell, P.; Chapple, I.L.C. Association between periodontitis and mortality in stages 3–5 chronic kidney disease: NHANES III and linked mortality study. J. Clin. Periodontol. 2016, 43, 104–113. [Google Scholar] [CrossRef] [PubMed]
- Machowska, A.; Carrero, J.J.; Lindholm, B.; Stenvinkel, P. Therapeutics targeting persistent inflammation in chronic kidney disease. Transl. Res. 2016, 167, 204–213. [Google Scholar] [CrossRef]
- Grubbs, V.; Garcia, F.; Jue, B.L.; Vittinghoff, E.; Ryder, M.; Lovett, D.; Carrillo, J.; Offenbacher, S.; Ganz, P.; Bibbins-Domingo, K.; et al. The Kidney and Periodontal Disease (KAPD) study: A pilot randomized controlled trial testing the effect of non-surgical periodontal therapy on chronic kidney disease. Contemp. Clin. Trials 2017, 53, 143–150. [Google Scholar] [CrossRef]
- Kaneko, N.; Kurata, M.; Yamamoto, T.; Morikawa, S.; Masumoto, J. The role of interleukin-1 in general pathology. Inflamm. Regen. 2019, 39, 1–16. [Google Scholar] [CrossRef]
- Dinarello, C.A. Interleukin-1 in the pathogenesis and treatment of inflammatory diseases. Blood 2011, 117, 3720–3732. [Google Scholar] [CrossRef]
- Farivar, S.; Hassani, M.; Shiari, R. Interleukin-1 as a key factor in the development of inflammatory diseases. Arch. Pediatr. Infect. Dis. 2014, 2, 1–5. [Google Scholar] [CrossRef]
- Zakiyanov, O.; Kalousová, M.; Zima, T.; Tesař, V. Matrix metalloproteinases in renal diseases: A critical appraisal. Kidney Blood Press Res. 2019, 44, 298–330. [Google Scholar] [CrossRef]
- Dai, X.; Zeng, Z.; Fu, C.; Zhang, S.; Cai, Y.; Chen, Z. Diagnostic value of neutrophil gelatinase-associated lipocalin, cystatin C, and soluble triggering receptor expressed on myeloid cells-1 in critically ill patients with sepsis-associated acute kidney injury. Crit. Care 2015, 19, 1–10. [Google Scholar] [CrossRef]
- Tammaro, A.; Derive, M.; Gibot, S.; Leemans, J.C.; Florquin, S.; Dessing, M.C. TREM-1 and its potential ligands in non-infectious diseases: From biology to clinical perspectives. Pharmacol. Ther. 2017, 177, 81–95. [Google Scholar] [CrossRef] [PubMed]
- Raivisto, T.; Heikkinen, A.M.; Silbereisen, A.; Kovanen, L.; Ruokonen, H.; Tervahartiala, T.; Haukka, J.; Sorsa, T.; Bostanci, N. Regulation of Salivary Peptidoglycan Recognition Protein1in Adolescents. JDR Clin. Transl. Res. 2019, 20, 1–10. [Google Scholar]
- Cheng, R.; Wu, Z.; Li, M.; Shao, M.; Hu, T. Interleukin-1β is a potential therapeutic target for periodontitis: A narrative review. Int. J. Oral Sci. 2020, 12, 1–9. [Google Scholar] [CrossRef] [PubMed]
- Basu, R.K.; Donaworth, E.; Siroky, B.; Devarajan, P.; Wong, H.R. Loss of matrix metalloproteinase-8 is associated with worsened recovery after ischemic kidney injury. Ren. Fail. 2015, 37, 469–475. [Google Scholar] [CrossRef] [PubMed]
- Cruz, M.C.; Andrade, C.; Urrutia, M.; Draibe, S.; Nogueira-Martins, L.A.; Sesso, R.D.C.C. Quality of life in patients with chronic kidney disease. Clinics 2011, 66, 991–995. [Google Scholar] [CrossRef]
- Ismail, F.B.; Ismail, G.; Dumitriu, A.S.; Baston, C.; Berbecar, V.; Jurubita, R.; Andronesi, A.; Dumitriu, H.T.; Sinescu, I. Identification of subgingival periodontal pathogens and association with the severity of periodontitis in patients with chronic kidney diseases: A cross-sectional study. Biomed. Res. Int. 2015, 2015, 370314. [Google Scholar] [CrossRef]
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).