Is The Timed-Up and Go Test Feasible in Mobile Devices? A Systematic Review
Abstract
1. Introduction
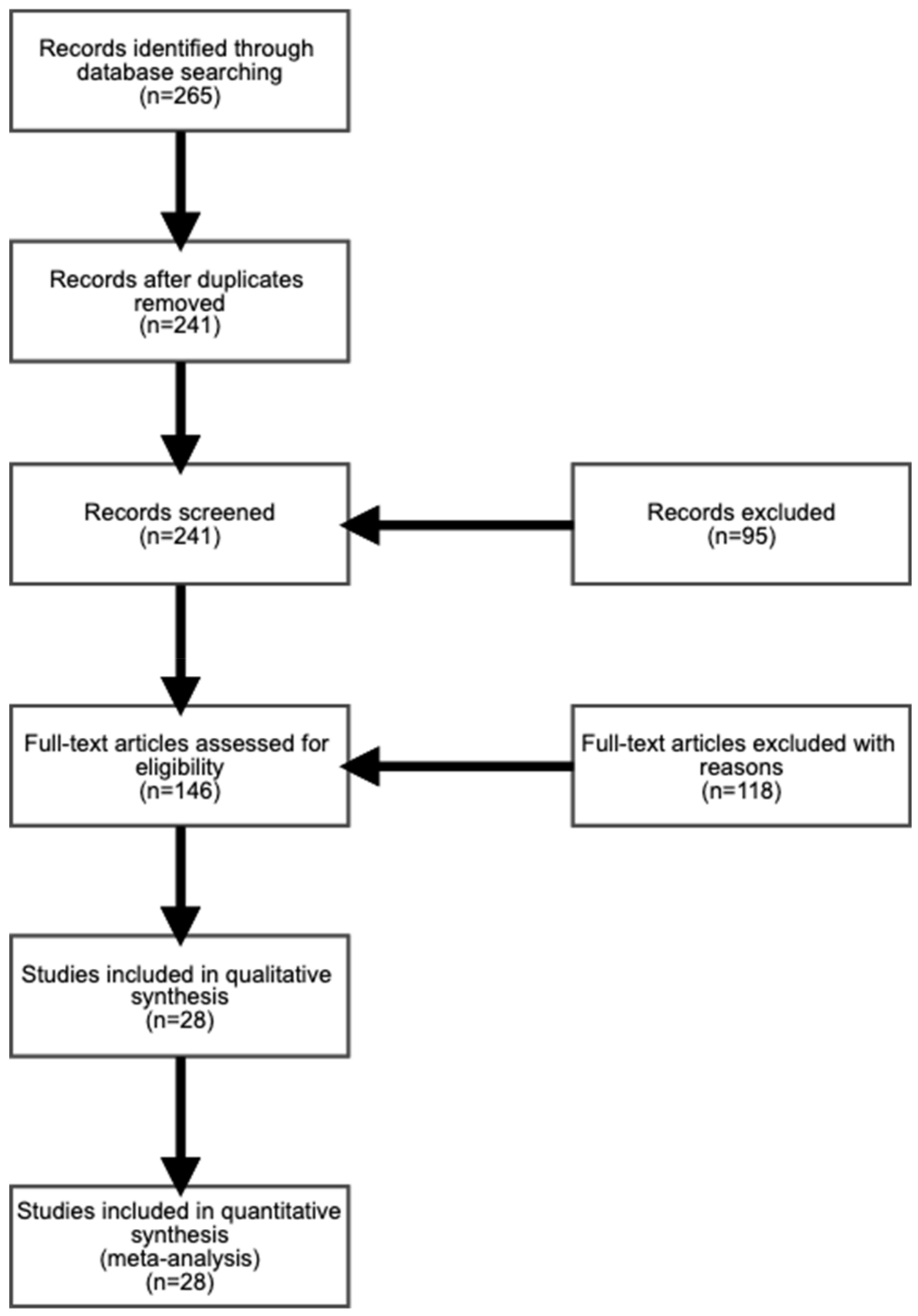
2. Materials and Methods
2.1. Research Questions
2.2. Inclusion Criteria
2.3. Search Strategy
2.4. Extraction of Study Characteristics
3. Results
3.1. Healthy People
3.2. Parkinson Disease
3.3. Frailty Syndrome
3.4. Other Diseases
4. Discussion
- Falling risk in healthy older populations may not affect the measurement of the duration;
- The user may perform the different phases with other involuntary movements or trajectories;
- The effects of the medication therapy and movement deficiencies may not be detected;
- The high reliability and discrimination of the health may not be evaluated in only 3 meters;
- The measurement of the results of the test depends on the personal and environmental conditions;
- The conditions of the chair may also introduce the possibility of different results.
5. Conclusions
- (RQ1) Most of the low-cost IMU sensors used in the TUG tests are the gyroscope, magnetometer, and accelerometer. These sensors are widely used in the physiotherapy domain and can be used to detect all the five phases of the TUG test, which can be identified by sensors available onboard off-the-shelf mobile devices. Moreover, mobile sensors can be a low-cost approach for the TUG test and consecutively to clinical diagnostics of several diseases. The data collected by mobile sensors can be analyzed to create patterns for the evaluation of different diseases.
- (RQ2) The methods and features most used to measure the results are related to the time of the TUG test, the angular velocity and the angular analysis of the body movements, and the number of steps performed.
- (RQ3) One of the main purposes of the TUG test is to help in the recognition of the probability of the risk of falls, where eight studies present the relation between it and the TUG test in elderly people.
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- World Facts and Statistics on Disabilities and Disability Issues. Available online: www.cdc.gov/ncbddd/disabilityandhealth/dhds.html (accessed on 17 December 2018).
- Population Ages 65 and above (% of Total) | Data. Available online: https://data.worldbank.org/indicator/SP.POP.65UP.TO.ZS#fromHistory (accessed on 24 November 2018).
- Office of Disease Prevention and Health Promotion. 2020 Topics & Objectives: Older Adults; US Department of Health and Human Services: Washington, DC, USA, 2010.
- World Health Organization Ageing and Health. Available online: https://www.who.int/news-room/fact-sheets/detail/ageing-and-health (accessed on 27 December 2019).
- Wu, F.; Li, X.; Sangaiah, A.K.; Xu, L.; Kumari, S.; Wu, L.; Shen, J. A lightweight and robust two-factor authentication scheme for personalized healthcare systems using wireless medical sensor networks. Future Gener. Comput. Syst. 2018, 82, 727–737. [Google Scholar] [CrossRef]
- Jagadeeswari, V.; Subramaniyaswamy, V.; Logesh, R.; Vijayakumar, V. A study on medical Internet of Things and Big Data in personalized healthcare system. Health Inf. Sci. Syst. 2018, 6, 14. [Google Scholar] [CrossRef] [PubMed]
- WHO|Facts about Ageing. Available online: https://www.who.int/ageing/about/facts/en/ (accessed on 7 December 2018).
- Steinhubl, S.R.; Muse, E.D.; Topol, E.J. The emerging field of mobile health. Sci. Transl. Med. 2015, 7, 283rv3. [Google Scholar] [CrossRef] [PubMed]
- Anderson, K.; Burford, O.; Emmerton, L. Mobile Health Apps to Facilitate Self-Care: A Qualitative Study of User Experiences. PLoS ONE 2016, 11, e0156164. [Google Scholar] [CrossRef] [PubMed]
- Zainal, A.; Razak, F.H.A.; Ahmad, N.A. Older People and the Use of Mobile Phones: An Interview Study. In Proceedings of the 2013 International Conference on Advanced Computer Science Applications and Technologies, Kuching, Malaysia, 23–24 December 2013; IEEE: Kuching, Malaysia, 2013; pp. 390–395. [Google Scholar]
- Kurniawan, S.; Mahmud, M.; Nugroho, Y. A study of the use of mobile phones by older persons. In Proceedings of the CHI ’06 Extended Abstracts on Human Factors in Computing Systems—CHI EA ’06, Montreal, QCC, Canada, 22–27 April 2006; ACM Press: New York, NY, USA, 2006; p. 989. [Google Scholar]
- Klimova, B. Acceptance and Use of Mobile Devices and Apps by Elderly People. In Challenges and Opportunities in the Digital Era; Al-Sharhan, S.A., Simintiras, A.C., Dwivedi, Y.K., Janssen, M., Mäntymäki, M., Tahat, L., Moughrabi, I., Ali, T.M., Rana, N.P., Eds.; Springer International Publishing: Cham, Switzerland, 2018; Volume 11195, pp. 30–36. ISBN 978-3-030-02130-6. [Google Scholar]
- Marques, G.; Pitarma, R. Promoting Health and Well-Being Using Wearable and Smartphone Technologies for Ambient Assisted Living Through Internet of Things. In Big Data and Networks Technologies; Farhaoui, Y., Ed.; Springer International Publishing: Cham, Switzerland, 2020; Volume 81, pp. 12–22. ISBN 978-3-030-23671-7. [Google Scholar]
- Kakria, P.; Tripathi, N.K.; Kitipawang, P. A Real-Time Health Monitoring System for Remote Cardiac Patients Using Smartphone and Wearable Sensors. Int. J. Telemed. Appl. 2015, 2015, 373474. [Google Scholar] [CrossRef]
- Majumder, S.; Deen, M.J. Smartphone Sensors for Health Monitoring and Diagnosis. Sensors 2019, 19, 2164. [Google Scholar] [CrossRef]
- Higgins, J.P. Smartphone Applications for Patients’ Health and Fitness. Am. J. Med. 2016, 129, 11–19. [Google Scholar] [CrossRef]
- Ben-Zeev, D.; Scherer, E.A.; Wang, R.; Xie, H.; Campbell, A.T. Next-generation psychiatric assessment: Using smartphone sensors to monitor behavior and mental health. Psychiatr. Rehabil. J. 2015, 38, 218–226. [Google Scholar] [CrossRef]
- Haghi, M.; Thurow, K.; Stoll, R. Wearable Devices in Medical Internet of Things: Scientific Research and Commercially Available Devices. Healthc. Inform. Res. 2017, 23, 4. [Google Scholar] [CrossRef]
- Andrews, R.G. Mobile Sensor Data Measurements and Analysis for Fall Detection in Elderly Health Care. Master’s Thesis, Aalto University, Espoo, Finland, 2017. [Google Scholar]
- Guo, J.; Zhou, X.; Sun, Y.; Ping, G.; Zhao, G.; Li, Z. Smartphone-Based Patients’ Activity Recognition by Using a Self-Learning Scheme for Medical Monitoring. J. Med. Syst. 2016, 40, 140. [Google Scholar] [CrossRef]
- Dziak, D.; Jachimczyk, B.; Kulesza, W. IoT-Based Information System for Healthcare Application: Design Methodology Approach. Appl. Sci. 2017, 7, 596. [Google Scholar] [CrossRef]
- Mellone, S.; Tacconi, C.; Schwickert, L.; Klenk, J.; Becker, C.; Chiari, L. Smartphone-based solutions for fall detection and prevention: The FARSEEING approach. Z. Gerontol. Geriatr. 2012, 45, 722–727. [Google Scholar] [CrossRef] [PubMed]
- Cornet, V.P.; Holden, R.J. Systematic review of smartphone-based passive sensing for health and wellbeing. J. Biomed. Inform. 2018, 77, 120–132. [Google Scholar] [CrossRef] [PubMed]
- Marques, G.; Pitarma, R.; Garcia, N.; Pombo, N. Internet of Things Architectures, Technologies, Applications, Challenges, and Future Directions for Enhanced Living Environments and Healthcare Systems: A Review. Electronics 2019, 8, 1081. [Google Scholar] [CrossRef]
- Zdravevski, E.; Lameski, P.; Trajkovik, V.; Kulakov, A.; Chorbev, I.; Goleva, R.; Pombo, N.; Garcia, N. Garcia Improving Activity Recognition Accuracy in Ambient-Assisted Living Systems by Automated Feature Engineering. IEEE Access 2017, 5, 5262–5280. [Google Scholar] [CrossRef]
- Pires, I.M.; Garcia, N.M.; Pombo, N.; Flórez-Revuelta, F. From Data Acquisition to Data Fusion: A Comprehensive Review and a Roadmap for the Identification of Activities of Daily Living Using Mobile Devices. Sensors 2016, 16, 184. [Google Scholar] [CrossRef]
- Pires, I.M.; Santos, R.; Pombo, N.; Garcia, N.M.; Flórez-Revuelta, F.; Spinsante, S.; Goleva, R.; Zdravevski, E. Recognition of activities of daily living based on environmental analyses using audio fingerprinting techniques: A systematic review. Sensors 2018, 18, 160. [Google Scholar] [CrossRef]
- Lameski, P.; Zdravevski, E.; Koceski, S.; Kulakov, A.; Trajkovik, V. Suppression of Intensive Care Unit False Alarms based on the Arterial Blood Pressure Signal. IEEE Access 2017. [Google Scholar] [CrossRef]
- Pires, I.M.; Andrade, M.; Garcia, N.M.; Crisóstomo, R.; Florez-Revuelta, F. Measurement of heel-rise test results using a mobile device. In Proceedings of the 2nd International Conference on Physiological Computing Systems: PhyCS 2015, Angers, France, 11–13 February 2015. [Google Scholar]
- Gautschi, O.P.; Stienen, M.N.; Corniola, M.V.; Joswig, H.; Schaller, K.; Hildebrandt, G.; Smoll, N.R. Assessment of the Minimum Clinically Important Difference in the Timed Up and Go Test After Surgery for Lumbar Degenerative Disc Disease. Neurosurgery 2017, 80, 380–385. [Google Scholar] [CrossRef]
- Whitney, J.C.; Lord, S.R.; Close, J.C.T. Streamlining assessment and intervention in a falls clinic using the Timed Up and Go Test and Physiological Profile Assessments. Age Ageing 2005, 34, 567–571. [Google Scholar] [CrossRef]
- Benavent-Caballer, V.; Sendín-Magdalena, A.; Lisón, J.F.; Rosado-Calatayud, P.; Amer-Cuenca, J.J.; Salvador-Coloma, P.; Segura-Ortí, E. Physical factors underlying the Timed “Up and Go” test in older adults. Geriatr. Nur. (Lond.) 2016, 37, 122–127. [Google Scholar] [CrossRef] [PubMed]
- Weiss, A.; Herman, T.; Plotnik, M.; Brozgol, M.; Giladi, N.; Hausdorff, J.M. An instrumented timed up and go: The added value of an accelerometer for identifying fall risk in idiopathic fallers. Physiol. Meas. 2011, 32, 2003–2018. [Google Scholar] [CrossRef] [PubMed]
- Shumway-Cook, A.; Brauer, S.; Woollacott, M. Predicting the probability for falls in community-dwelling older adults using the Timed Up & Go Test. Phys. Ther. 2000, 80, 896–903. [Google Scholar] [PubMed]
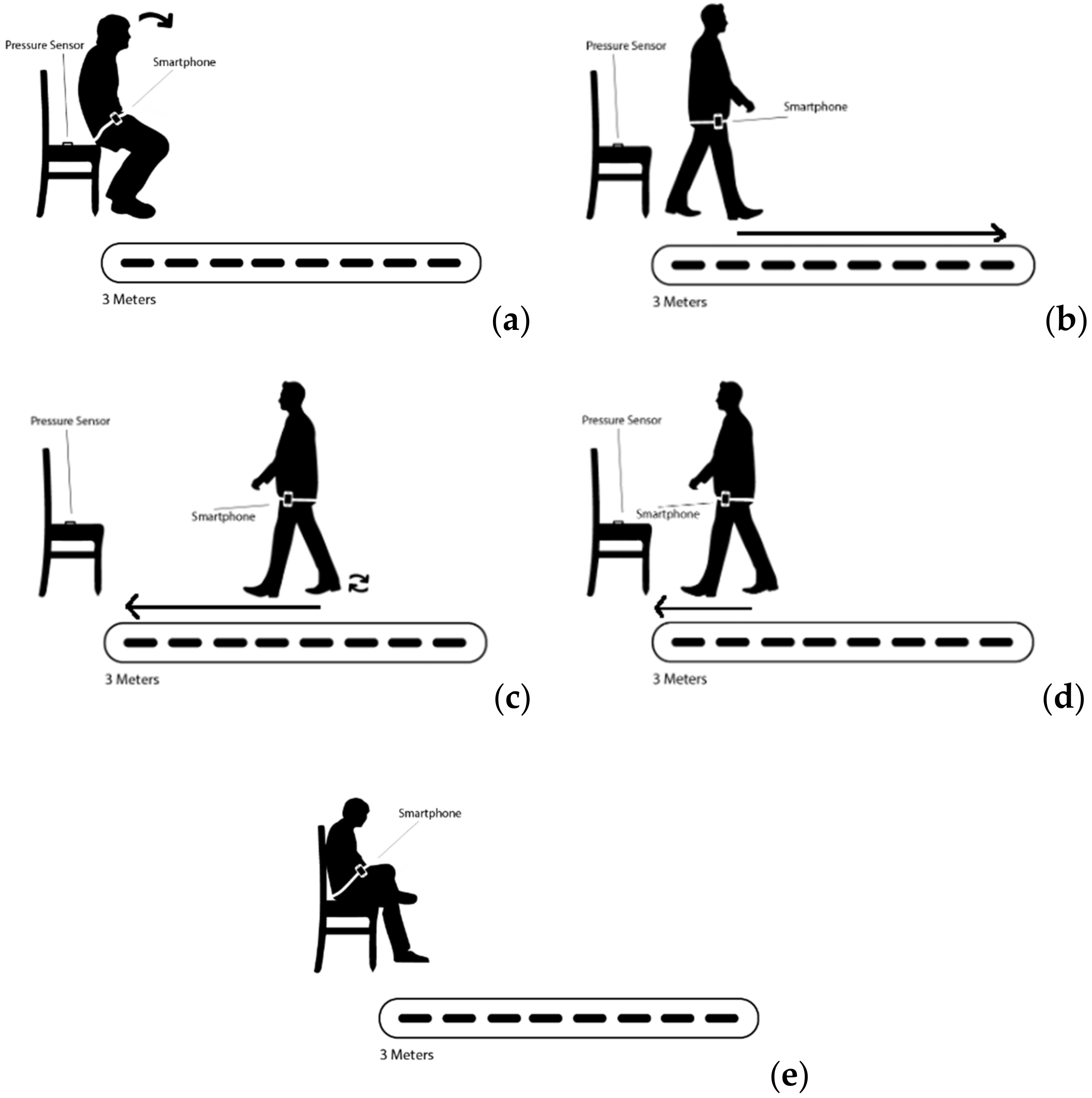
- Ponciano, V.; Pires, I.M.; Ribeiro, F.R.; Garcia, N.M.; Pombo, N.; Spinsante, S.; Crisóstomo, R. Smartphone-based automatic measurement of the results of the Timed-Up and Go test. In Proceedings of the Proceedings of the 5th EAI International Conference on Smart Objects and Technologies for Social Good, Valencia, Spain, 25–27 September 2019; ACM: New York, NY, USA, 2019; pp. 239–242. [Google Scholar]
- Pires, I.M.; Marques, D.; Pombo, N.; Garcia, N.M.; Marques, M.C.; Flórez-Revuelta, F. Measurement of the Reaction Time in the 30-S Chair Stand Test using the Accelerometer Sensor Available in off-the-Shelf Mobile Devices. In Proceedings of the HSP 2018, Funchal, Portugal, 22–23 March 2018. [Google Scholar]
- Helm, J.M.; Swiergosz, A.M.; Haeberle, H.S.; Karnuta, J.M.; Schaffer, J.L.; Krebs, V.E.; Spitzer, A.I.; Ramkumar, P.N. Machine Learning and Artificial Intelligence: Definitions, Applications, and Future Directions. Curr. Rev. Musculoskelet. Med. 2020, 13, 69–76. [Google Scholar] [CrossRef] [PubMed]
- Bloomfield, R.A.; Williams, H.A.; Broberg, J.S.; Lanting, B.A.; McIsaac, K.A.; Teeter, M.G. Machine Learning Groups Patients by Early Functional Improvement Likelihood Based on Wearable Sensor Instrumented Preoperative Timed-Up-and-Go Tests. J. Arthroplasty 2019, 34, 2267–2271. [Google Scholar] [CrossRef]
- Sasani, K.; Catanese, H.N.; Ghods, A.; Rokni, S.A.; Ghasemzadeh, H.; Downey, R.J.; Shahrokni, A. Gait speed and survival of older surgical patient with cancer: Prediction after machine learning. J. Geriatr. Oncol. 2019, 10, 120–125. [Google Scholar] [CrossRef]
- Staartjes, V.E.; Quddusi, A.; Klukowska, A.M.; Schröder, M.L. Initial classification of low back and leg pain based on objective functional testing: A pilot study of machine learning applied to diagnostics. Eur. Spine J. 2020. [Google Scholar] [CrossRef]
- De Vos, M.; Prince, J.; Buchanan, T.; FitzGerald, J.J.; Antoniades, C.A. Discriminating progressive supranuclear palsy from Parkinson’s disease using wearable technology and machine learning. Gait Posture 2020, 77, 257–263. [Google Scholar] [CrossRef]
- Zdravevski, E.; Risteska Stojkoska, B.; Standl, M.; Schulz, H. Automatic machine-learning based identification of jogging periods from accelerometer measurements of adolescents under field conditions. PLoS ONE 2017, 12, e0184216. [Google Scholar] [CrossRef]
- Reis, S.; Felizardo, V.; Pombo, N.; Garcia, N. Elderly mobility analysis during Timed Up and Go test using biosignals. In Proceedings of the 7th International Conference on Software Development and Technologies for Enhancing Accessibility and Fighting Info-exclusion, Real, Portugal, 1–3 December 2016; pp. 240–245. [Google Scholar]
- Beauchet, O.; Fantino, B.; Allali, G.; Muir, S.W.; Montero-Odasso, M.; Annweiler, C. Timed up and go test and risk of falls in older adults: A systematic review. J. Nutr. Health Aging 2011, 15, 933–938. [Google Scholar] [CrossRef]
- Sprint, G.; Cook, D.J.; Weeks, D.L. Toward Automating Clinical Assessments: A Survey of the Timed Up and Go. IEEE Rev. Biomed. Eng. 2015, 8, 64–77. [Google Scholar] [CrossRef] [PubMed]
- Pantelopoulos, A.; Bourbakis, N.G. A survey on wearable sensor-based systems for health monitoring and prognosis. IEEE Trans. Syst. Man Cybern. Part C Appl. Rev. 2010, 40, 1–12. [Google Scholar] [CrossRef]
- Christensen, L.; Vøllestad, N.K.; Veierød, M.B.; Stuge, B.; Cabri, J.; Robinson, H.S. The Timed Up & Go test in pregnant women with pelvic girdle pain compared to asymptomatic pregnant and non-pregnant women. Musculoskelet. Sci. Pract. 2019, 43, 110–116. [Google Scholar] [PubMed]
- Åhman, H.B.; Giedraitis, V.; Cedervall, Y.; Lennhed, B.; Berglund, L.; McKee, K.; Kilander, L.; Rosendahl, E.; Ingelsson, M.; Åberg, A.C. Dual-Task Performance and Neurodegeneration: Correlations Between Timed Up-and-Go Dual-Task Test Outcomes and Alzheimer’s Disease Cerebrospinal Fluid Biomarkers. J. Alzheimers Dis. 2019, 71, S75–S83. [Google Scholar] [CrossRef]
- Bustam, I.G.; Suriyaamarit, D.; Boonyong, S. Timed Up and Go test in typically developing children: Protocol choice influences the outcome. Gait Posture 2019, 73, 258–261. [Google Scholar] [CrossRef]
- Langeard, A.; Houdeib, R.; Saillant, K.; Kaushal, N.; Lussier, M.; Bherer, L. Switching Ability Mediates the Age-Related Difference in Timed Up and Go Performance. J. Alzheimers Dis. 2019, 71, S23–S28. [Google Scholar] [CrossRef]
- Jakobsson, M.; Brisby, H.; Gutke, A.; Lundberg, M.; Smeets, R. One-minute stair climbing, 50-foot walk, and timed up-and-go were responsive measures for patients with chronic low back pain undergoing lumbar fusion surgery. BMC Musculoskelet. Disord. 2019, 20, 137. [Google Scholar] [CrossRef]
- Hatch, J.; Veneri, D. The effect of rolling walker use on interpretation of Timed Up and Go test scores: A preliminary study. Int. J. Rehabil. Res. 2020, 43, 95–98. [Google Scholar] [CrossRef]
- Galán-Mercant, A.; Barón-López, F.J.; Labajos-Manzanares, M.T.; Cuesta-Vargas, A.I. Reliability and criterion-related validity with a smartphone used in timed-up-and-go test. Biomed. Eng. OnLine 2014, 13, 156. [Google Scholar] [CrossRef]
- Yang, Z.; Song, C.; Lin, F.; Langan, J.; Xu, W. Empowering a Gait Feature-Rich Timed-Up-and-Go System for Complex Ecological Environments. In Proceedings of the 2017 IEEE/ACM International Conference on Connected Health: Applications, Systems and Engineering Technologies (CHASE), Philadelphia, PA, USA, 17–19 July 2017; pp. 340–347. [Google Scholar]
- Higashi, Y.; Yamakoshi, K.; Fujimoto, T.; Sekine, M.; Tamura, T. Quantitative evaluation of movement using the timed up-and-go test. IEEE Eng. Med. Biol. Mag. 2008, 27, 38–46. [Google Scholar] [CrossRef]
- Yang, Z.; Song, C.; Lin, F.; Langan, J.; Xu, W. A Smart Environment-Adapting Timed-Up-and-Go System Powered by Sensor-Embedded Insoles. IEEE Internet Things J. 2018, 6, 1298–1305. [Google Scholar] [CrossRef]
- Bao, T.; Carender, W.J.; Kinnaird, C.; Barone, V.J.; Peethambaran, G.; Whitney, S.L.; Kabeto, M.; Seidler, R.D.; Sienko, K.H. Effects of long-term balance training with vibrotactile sensory augmentation among community-dwelling healthy older adults: A randomized preliminary study. J. Neuroeng. Rehabil. 2018, 15, 5. [Google Scholar] [CrossRef] [PubMed]
- Silva, J.; Sousa, I. Instrumented timed up and go: Fall risk assessment based on inertial wearable sensors. In Proceedings of the 2016 IEEE International Symposium on Medical Measurements and Applications (MeMeA), Benevento, Italy, 15–18 May 2016; pp. 1–6. [Google Scholar]
- Hellmers, S.; Izadpanah, B.; Dasenbrock, L.; Diekmann, R.; Bauer, J.M.; Hein, A.; Fudickar, S. Towards an Automated Unsupervised Mobility Assessment for Older People Based on Inertial TUG Measurements. Sensors 2018, 18, 3310. [Google Scholar] [CrossRef] [PubMed]
- Chigateri, N.G.; Kerse, N.; Wheeler, L.; MacDonald, B.; Klenk, J. Validation of an accelerometer for measurement of activity in frail older people. Gait Posture 2018, 66, 114–117. [Google Scholar] [CrossRef] [PubMed]
- Mellone, S.; Tacconi, C.; Chiari, L. Validity of a Smartphone-based instrumented Timed Up and Go. Gait Posture 2012, 36, 163–165. [Google Scholar] [CrossRef] [PubMed]
- Madhushri, P.; Jovanov, E.; Milenkovic, A.; Shtessel, Y. A model based analysis of optimality of sit-to-stand transition. In Proceedings of the 2017 39th Annual International Conference of the IEEE Engineering in Medicine and Biology Society (EMBC), Jeju Island, Korea, 11–15 July 2017; pp. 2398–2401. [Google Scholar]
- Beyea, J.; McGibbon, C.A.; Sexton, A.; Noble, J.; O’Connell, C. Convergent Validity of a Wearable Sensor System for Measuring Sub-Task Performance during the Timed Up-and-Go Test. Sensors 2017, 17, 934. [Google Scholar] [CrossRef]
- SConi, A.; Mellone, S.; Colpo, M.; Bandinelli, S.; Chiari, L. Influence of age and gender on sensor-based functional measures: A factor analysis approach. In Proceedings of the 2015 37th Annual International Conference of the IEEE Engineering in Medicine and Biology Society (EMBC), Milan, Italy, 25–29 August 2015; pp. 5054–5057. [Google Scholar]
- Salarian, A.; Horak, F.B.; Zampieri, C.; Carlson-Kuhta, P.; Nutt, J.G.; Aminian, K. iTUG, a Sensitive and Reliable Measure of Mobility. IEEE Trans. Neural Syst. Rehabil. Eng. 2010, 18, 303–310. [Google Scholar] [CrossRef]
- Suppa, A.; Kita, A.; Leodori, G.; Zampogna, A.; Nicolini, E.; Lorenzi, P.; Rao, R.; Irrera, F. l-DOPA and Freezing of Gait in Parkinson’s Disease: Objective Assessment through a Wearable Wireless System. Front. Neurol. 2017, 8, 406. [Google Scholar] [CrossRef]
- Madhushri, P.; Dzhagaryan, A.A.; Jovanov, E.; Milenkovic, A. A Smartphone Application Suite for Assessing Mobility. In Proceedings of the 2016 38th Annual International Conference of the IEEE Engineering in Medicine and Biology Society (EMBC), Orlando, FL, USA, 16–20 August 2016; pp. 3117–3120. [Google Scholar]
- Cippitelli, E.; Gasparrini, S.; Gambi, E.; Spinsante, S. An Integrated Approach to Fall Detection and Fall Risk Estimation Based on RGB-Depth and Inertial Sensors. In Proceedings of the 7th International Conference on Software Development and Technologies for Enhancing Accessibility and Fighting Info-exclusion, Real, Portugal, 1–3 December 2016; ACM: New York, NY, USA, 2016; pp. 246–253. [Google Scholar]
- Williams, B.; Allen, B.; True, H.; Fell, N.; Levine, D.; Sartipi, M. A real-time, mobile timed up and go system. In Proceedings of the 2015 IEEE 12th International Conference on Wearable and Implantable Body Sensor Networks (BSN), Cambridge, MA, USA, 9–12 June 2015; pp. 1–6. [Google Scholar]
- Galan-Mercant, A.; Cuesta-Vargas, A.I. Clinical frailty syndrome assessment using inertial sensors embedded in smartphones. Physiol. Meas. 2015, 36, 1929. [Google Scholar]
- Milosevic, M.; Jovanov, E.; Milenković, A. Quantifying Timed-Up-and-Go test: A smartphone implementation. In Proceedings of the 2013 IEEE International Conference on Body Sensor Networks, Cambridge, MA, USA, 6–9 May 2013; pp. 1–6. [Google Scholar]
- Dzhagaryan, A.; Milenkovic, A.; Jovanov, E.; Milosevic, M. Smart Button: A wearable system for assessing mobility in elderly. In Proceedings of the 2015 17th International Conference on E-health Networking, Application & Services (HealthCom), Bostonv, MA, USA, 14–17 October 2015; pp. 416–421. [Google Scholar]
- Greene, B.R.; Doheny, E.P.; Kenny, R.A.; Caulfield, B. Classification of frailty and falls history using a combination of sensor-based mobility assessments. Physiol. Meas. 2014, 35, 2053. [Google Scholar] [CrossRef]
- Galán-Mercant, A.; Cuesta-Vargas, A.I. Differences in trunk accelerometry between frail and non-frail elderly persons in functional tasks. BMC Res. Notes 2014, 7, 100. [Google Scholar] [CrossRef] [PubMed]
- Galán-Mercant, A.; Cuesta-Vargas, A.I. Mobile Romberg test assessment (mRomberg). BMC Res. Notes 2014, 7, 640. [Google Scholar] [CrossRef] [PubMed]
- Greene, B.R.; Healy, M.; Rutledge, S.; Caulfield, B.; Tubridy, N. Quantitative assessment of multiple sclerosis using inertial sensors and the TUG test. In Proceedings of the 2014 36th Annual International Conference of the IEEE Engineering in Medicine and Biology Society, Chicago, IL, USA, 26–30 August 2014; pp. 2977–2980. [Google Scholar]
- Tacconi, C.; Mellone, S.; Chiari, L. Smartphone-based applications for investigating falls and mobility. In Proceedings of the 2011 5th International Conference on Pervasive Computing Technologies for Healthcare (Pervasive Health) and Workshops, Dublin, Ireland, 23–26 May 2011; pp. 258–261. [Google Scholar]
- Bernhard, F.P.; Sartor, J.; Bettecken, K.; Hobert, M.A.; Arnold, C.; Weber, Y.G.; Poli, S.; Margraf, N.G.; Schlenstedt, C.; Hansen, C.; et al. Wearables for gait and balance assessment in the neurological ward—Study design and first results of a prospective cross-sectional feasibility study with 384 inpatients. BMC Neurol. 2018, 18, 114. [Google Scholar] [CrossRef] [PubMed]
- Palmerini, L.; Mellone, S.; Rocchi, L.; Chiari, L. Dimensionality reduction for the quantitative evaluation of a smartphone-based Timed Up and Go test. In Proceedings of the 2011 Annual International Conference of the IEEE Engineering in Medicine and Biology Society, Boston, MA, USA, 30 August–3 September 2011; pp. 7179–7182. [Google Scholar]
- King, R.C.; Atallah, L.; Wong, C.; Miskelly, F.; Yang, G. Elderly Risk Assessment of Falls with BSN. In Proceedings of the 2010 International Conference on Body Sensor Networks, Singapore, 7–9 June 2010; pp. 30–35. [Google Scholar]
- Ribeiro, M.; Singh, S.; Guestrin, C. Local Interpretable Model-Agnostic Explanations (LIME): An Introduction. arXiv 2019, arXiv:1810.02678. [Google Scholar]
- Lundberg, S.M.; Lee, S.-I. A unified approach to interpreting model predictions. In Proceedings of the Advances in Neural Information Processing Systems, Long Beach, CA, USA, 4–9 December 2017; pp. 4765–4774. [Google Scholar]
| Paper | Year of Publication | Population | Purpose of the Study | Devices | Sensors | Raw Data Available | Source Code Available | Implementation | Studied Diseases |
|---|---|---|---|---|---|---|---|---|---|
| Yang et al. [56] | 2018 | 10 patients aged between 19 and 44 years old | Prevention of fall risks in the elderly subjects with the TUG test | Smartphone | Accelerometer Gyroscope Magnetometer | no | no | Calculation of the features | Healthy people |
| Bao et al. [57] | 2018 | 12 subjects aged between 65 and 85 years old | Shows the efficacy of the balance training to help the elderly, using the TUG test | Smartphone | Accelerometer Gyroscope | no | no | Calculation of the features | Healthy people |
| Yang et al. [54] | 2018 | 6 subjects with unknown age | Appreciate the feasibility of the TUG test and using a complex system | Smartphone | Accelerometer Gyroscope | yes | yes | Implementation of machine learning methods | Healthy people |
| Silva et al. [58] | 2018 | 18 older adults aged between 68 and 78 years old | Methodology to prevent and identify fall risks, using sensors and based on the TUG test | Smartphone | Accelerometer Gyroscope | no | no | Calculation of the features | Rheumatic diseases; chronic pain; hypertension; dizziness; polypharmacy |
| Hellmers et al. [59] | 2018 | 157 subjects aged between 70 and 85 years old | Automated analyses using inertial measurement units and the TUG test | Smartphone | Accelerometer Gyroscope Magnetometer | no | no | Calculation of the features | Parkinson disease |
| Chigateri et al. [60] | 2018 | 23 older adults aged 75 years old or over | Measure the fall risk using sensors and the TUG test | Mobiles devices | Accelerometer | no | no | Calculation of the features | Healthy people |
| Mellone et al. [61] | 2018 | 49 subjects aged between 43 and 75 years old | Validate a method for measuring the TUG test | Smartphone | Accelerometer | no | no | Calculation of the features | Parkinson disease |
| Madhushri et al. [62] | 2017 | 10 geriatric patients aged between 78 and 86 years old | Mobility assessment with the TUG test | Smartphone | Gyroscope Accelerometer | no | no | Calculation of the features | Mobility problems |
| Beyea et al. [63] | 2017 | 12 individuals aged between 21 and 64 years old | A mobile device using sensors and the TUG test separated in the different phases of the test | Mobiles devices | Accelerometer Gyroscope Magnetometer | no | no | Calculation of the features | Healthy people |
| Coni et al. [64] | 2017 | 239 subjects aged between 65 and 93 years old | Study the decline associated with the evolution of age using the TUG test and sensors | Smartphone | Accelerometer Gyroscope | no | no | Implementation of machine learning methods | Healthy people |
| Salarian et al. [65] | 2017 | 28 subjects aged between 52 and 68 years old | Instrumented the TUG test using sensors in people with Parkinson’s disease | Mobiles devices | Accelerometer | no | no | Calculation of the features | Parkinson disease |
| Suppa et al. [66] | 2017 | 28 patients aged between 63 and 77 years old | Inspect and associate the gait in people with Parkinson’s disease using the TUG test and the sensors | Mobiles devices | Microsoft Kinect Accelerometer Gyroscope | no | no | Implementation of machine learning methods | Parkinson disease |
| Madhushri et al. [67] | 2016 | 2 patients with unknown age | Application for mobility assessment helping the elderly to use the TUG test | Smartphone | Accelerometer Gyroscope | no | no | Calculation of the features | Mobility problems |
| Cippitelli et al. [68] | 2016 | 20 subjects aged between 22 and 39 years old | Quantify the possibility of the falls using data captured with sensors and tested with TUG test | Computer mobile devices | Microsoft Kinect Accelerometer | yes | no | Implementation of machine learning methods | Healthy people |
| Williams et al. [69] | 2015 | 5 subjects aged between 21 and 36 years old | The system that helps the subjects in stroke rehabilitation using the TUG test | Smartphone | Accelerometer Gyroscope Magnetometer | no | no | Calculation of the features | Healthy people |
| Cuesta-Vargas et al. [70] | 2015 | 30 subjects over 65 years old | Evaluation of the people and their mobility difficulty using sensors embedded in the smartphone and using the TUG test. | Smartphone | Accelerometer | no | no | Calculation of the features | Frailty syndrome |
| Milosevic et al. [71] | 2015 | 7 subjects with unknown age | Application to automate instrumented the TUG test using sensors | Smartphone | Accelerometer Gyroscope | no | no | Calculation of the features | Parkinson disease |
| Dzhagaryan et al. [72] | 2015 | 4 subjects with unknown age | Wearable system for older adults using the TUG test | Small wearable computing; smartphone | Accelerometer Gyroscope Magnetometer | no | no | Calculation of the features | Healthy people |
| Greene et al. [73] | 2014 | 124 older adults aged between 69 and 83 years old | The mobile platform using inertial and pressure sensors to check the mobility of older adults, using the TUG test | Mobiles devices | Accelerometer Gyroscope | no | no | Implementation of machine learning methods | Frailty syndrome |
| Galán-Mercant et al. [74] | 2014 | 30 subjects aged over 65 years old | Quantify and describe the acceleration, angular velocity and the motions of the body using a smartphone and the TUG test | Smartphone | Accelerometer | no | no | Implementation of machine learning methods | Frailty syndrome |
| Galán-Mercant et al. [75] | 2014 | 18 subjects aged over 70 years old | Quantify and define the magnitude of inertial sensors using a smartphone test assessment, based on the TUG test | Smartphone | Accelerometer Gyroscope Magnetometer | no | no | Calculation of the features | Frailty syndrome |
| Greene et al. [76] | 2014 | 21 patients aged between 18 and 60 years old | Examine the consistency of the quantifiable measures derivate of sensors and utilizing the TUG test | Smartphone | Accelerometer Gyroscope | no | no | Calculation of the features | Multiple sclerosis |
| Galán-Mercant et al. [53] | 2014 | 5 subjects aged over 65 years old | Analyze and quantify the reliability criterion-related with the utilization of sensors and using the extended TUG test | Smartphone | Accelerometer | yes | no | Implementation of machine learning methods | Healthy people |
| Tacconi et al. [77] | 2014 | 3 subjects with unknown age | System to analyze the human falls using the TUG test | Smartphone | Accelerometer | no | no | Calculation of the features | Healthy people |
| Mellone et al. [22] | 2014 | 200 subjects aged over 65 years old | Smartphone solutions to prevent and detect the human falls using the TUG test | Smartphone | Accelerometer Gyroscope | no | no | Implementation of machine learning methods | Healthy people |
| Bernhard et al. [78] | 2012 | 384 subjects aged between 40 and 89 years old | Analyses the effectiveness of mobile devices using sensors and the TUG test | Smartwatch | Accelerometer Gyroscope Magnetometer | no | no | Calculation of the features | Parkinson’s disease; stroke; epilepsy; pain syndromes; multiple sclerosis; tumors; polyneuropathy; vertigo; dementia; meningitis; encephalitis |
| Palmerini et al. [79] | 2011 | 49 subjects aged between 28 and 87 years old | Motion analysis systems incorporated in a smartphone, to study the possibility of falls for people with Parkinson’s disease using the TUG test and inertial sensors | Smartphone | Accelerometer | no | no | Calculation of the features | Healthy people |
| King et al. [80] | 2010 | 28 subjects with unknown age | Predict the risks of falls, using a BSN attached with inertial sensors using the TUG test | Mobiles devices | Accelerometer Gyroscope | no | no | Calculation of the features | Healthy people |
| Features | Interpretation | Number of Studies | ||
|---|---|---|---|---|
| TUG | Extended TUG | Smart Insole TUG | ||
| Duration | Quantitative | 6 | 3 | 6 |
| Number of steps | 2 | 1 | ||
| Stride length | 2 | |||
| Step time | 1 | |||
| Orientation | 1 | |||
| Position | 1 | |||
| Step length | 1 | |||
| Cadence | 1 | |||
| Turning duration | 1 | |||
| Time to perform turn-to-sit | 1 | |||
| Reaction time | 1 | |||
| Contact times (i.e., initial, forefoot, rearfoot, full, foot-ground, and non-foot-ground) | 1 | |||
| Distance | 1 | |||
| Threshold | 1 | |||
| Standard deviation of the step time | Quantitative + Statistic | 1 | ||
| Cadence standard deviation | 1 | |||
| Cadence coefficient of variation | 1 | |||
| Mean cadence | 1 | |||
| Averages of time | 1 | |||
| Mean stride length | 1 | |||
| Medio-lateral and medio-lateral interstride autocorrelations | 1 | |||
| Maximum change of the trunk angle | 1 | |||
| Acceleration | Dynamic balance | 2 | ||
| Maximum angular velocity | 2 | 1 | 1 | |
| Average speed | 1 | |||
| Averages of the sit-to-stand transition | 1 | |||
| Real velocity | 1 | |||
| Average velocity | 1 | |||
| Angular velocity of arm-swing | 1 | |||
| Gait speed | Gait properties | 2 | ||
| Gait duration | 1 | |||
| Gait cycle time | 1 | |||
| Gait cycle count | 1 | |||
| Gait cycle pace | 1 | |||
| Real angles of the sit-to-stand transition | State transitions | 2 | ||
| Range of sit-to-stand transition | 1 | |||
| Jerk | 1 | |||
| Mean of raw data | Raw statistic | 3 | ||
| Standard deviation | 3 | |||
| Root mean square (RMS) | 3 | 1 | ||
| Signal energy | 2 | |||
| Signal magnitude area (SMA) | 2 | |||
| Signal vector magnitude (SVM) | 2 | |||
| Spectral entropy | 2 | |||
| Variance | 1 | |||
| Number of peaks | 1 | |||
| Median deviation | 1 | |||
| Interquartile range (IQR) | 1 | |||
| Skewness | 1 | |||
| Kurtosis | 1 | |||
| Number of times the magnitude signal crosses the mean value | 1 | |||
| Maximum frequency of the FFT | 1 | |||
| Maximum amplitude of the FFT | 1 | |||
| Minimum average | 1 | |||
| Maximum average | 1 | |||
| Average of the peak height | 1 | |||
| Energy | 1 | |||
| Entropy | 1 | |||
| Angles | 1 | |||
| Maximum change of trunk angle | 1 | |||
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Ponciano, V.; Pires, I.M.; Ribeiro, F.R.; Marques, G.; Garcia, N.M.; Pombo, N.; Spinsante, S.; Zdravevski, E. Is The Timed-Up and Go Test Feasible in Mobile Devices? A Systematic Review. Electronics 2020, 9, 528. https://doi.org/10.3390/electronics9030528
Ponciano V, Pires IM, Ribeiro FR, Marques G, Garcia NM, Pombo N, Spinsante S, Zdravevski E. Is The Timed-Up and Go Test Feasible in Mobile Devices? A Systematic Review. Electronics. 2020; 9(3):528. https://doi.org/10.3390/electronics9030528
Chicago/Turabian StylePonciano, Vasco, Ivan Miguel Pires, Fernando Reinaldo Ribeiro, Gonçalo Marques, Nuno M. Garcia, Nuno Pombo, Susanna Spinsante, and Eftim Zdravevski. 2020. "Is The Timed-Up and Go Test Feasible in Mobile Devices? A Systematic Review" Electronics 9, no. 3: 528. https://doi.org/10.3390/electronics9030528
APA StylePonciano, V., Pires, I. M., Ribeiro, F. R., Marques, G., Garcia, N. M., Pombo, N., Spinsante, S., & Zdravevski, E. (2020). Is The Timed-Up and Go Test Feasible in Mobile Devices? A Systematic Review. Electronics, 9(3), 528. https://doi.org/10.3390/electronics9030528











