A Non-Contact Integrated Body-Ambient Temperature Sensors Platform to Contrast COVID-19
Abstract
1. Introduction
- Initial human temperature screening during the triage process in a public health emergency, to determine the significance of fever and elevated temperature with respect to possible affection;
- Temperature assessment within high throughput areas, such as business structures, airports, etc.
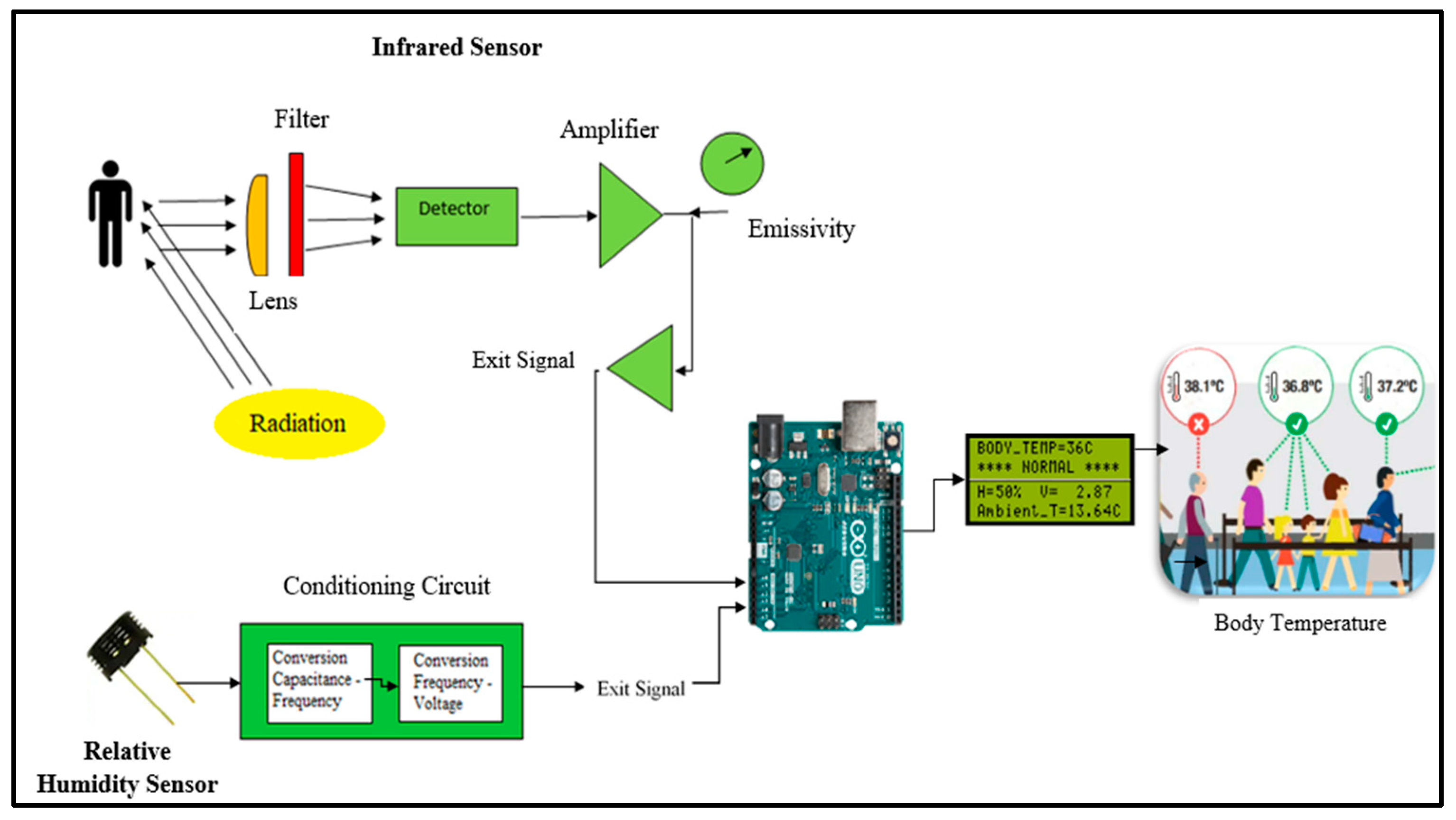
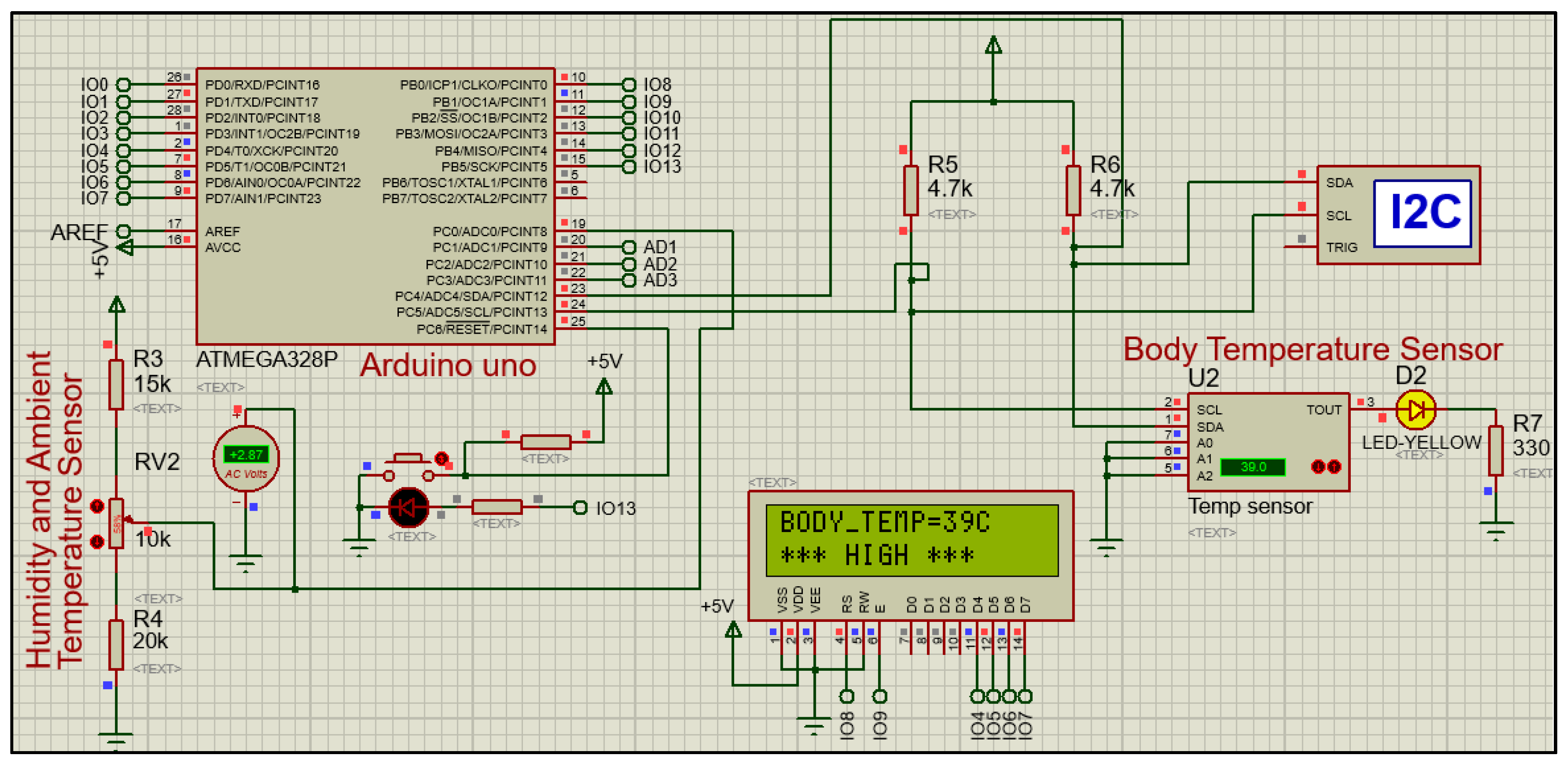
2. A Non-Contact Sensors Platform for Remote Ambient-Body Temperature Monitoring
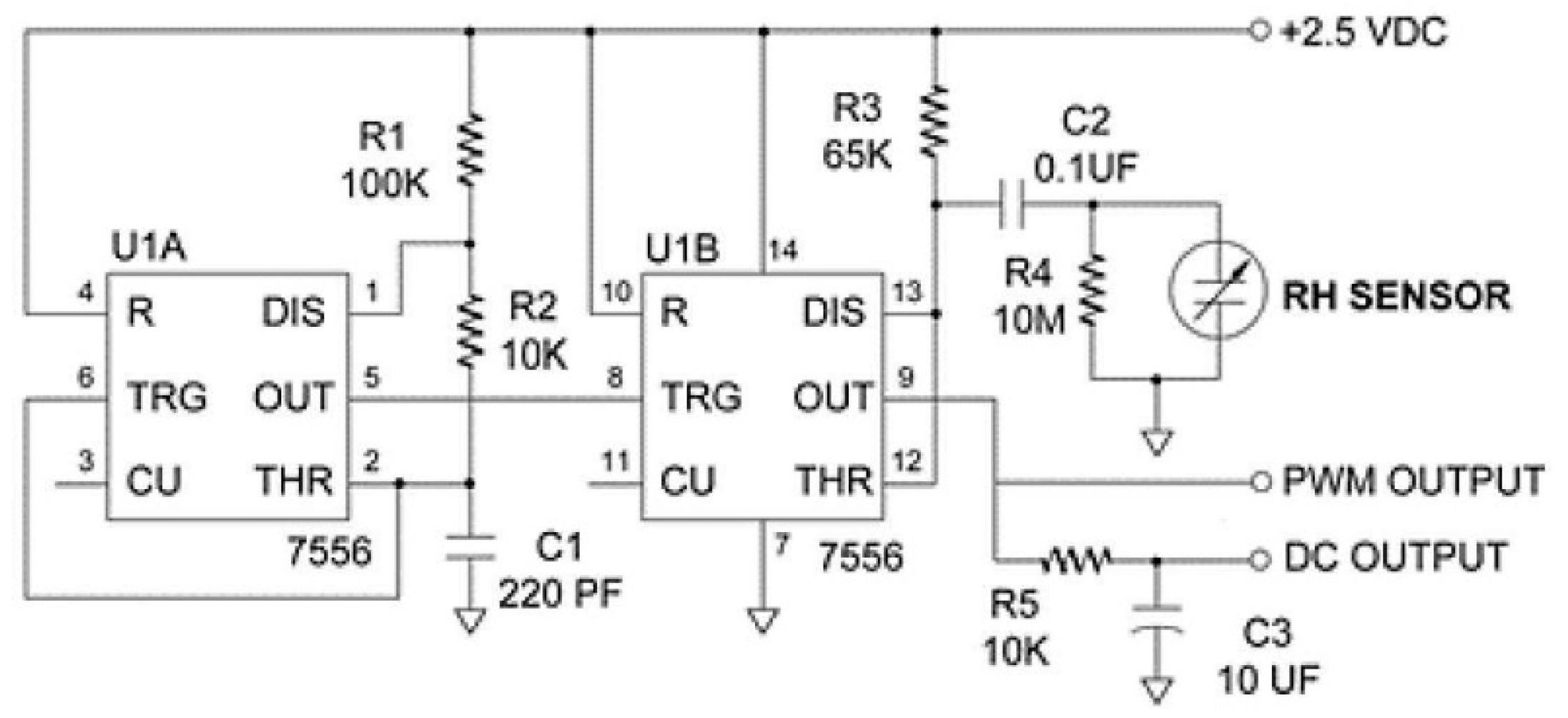
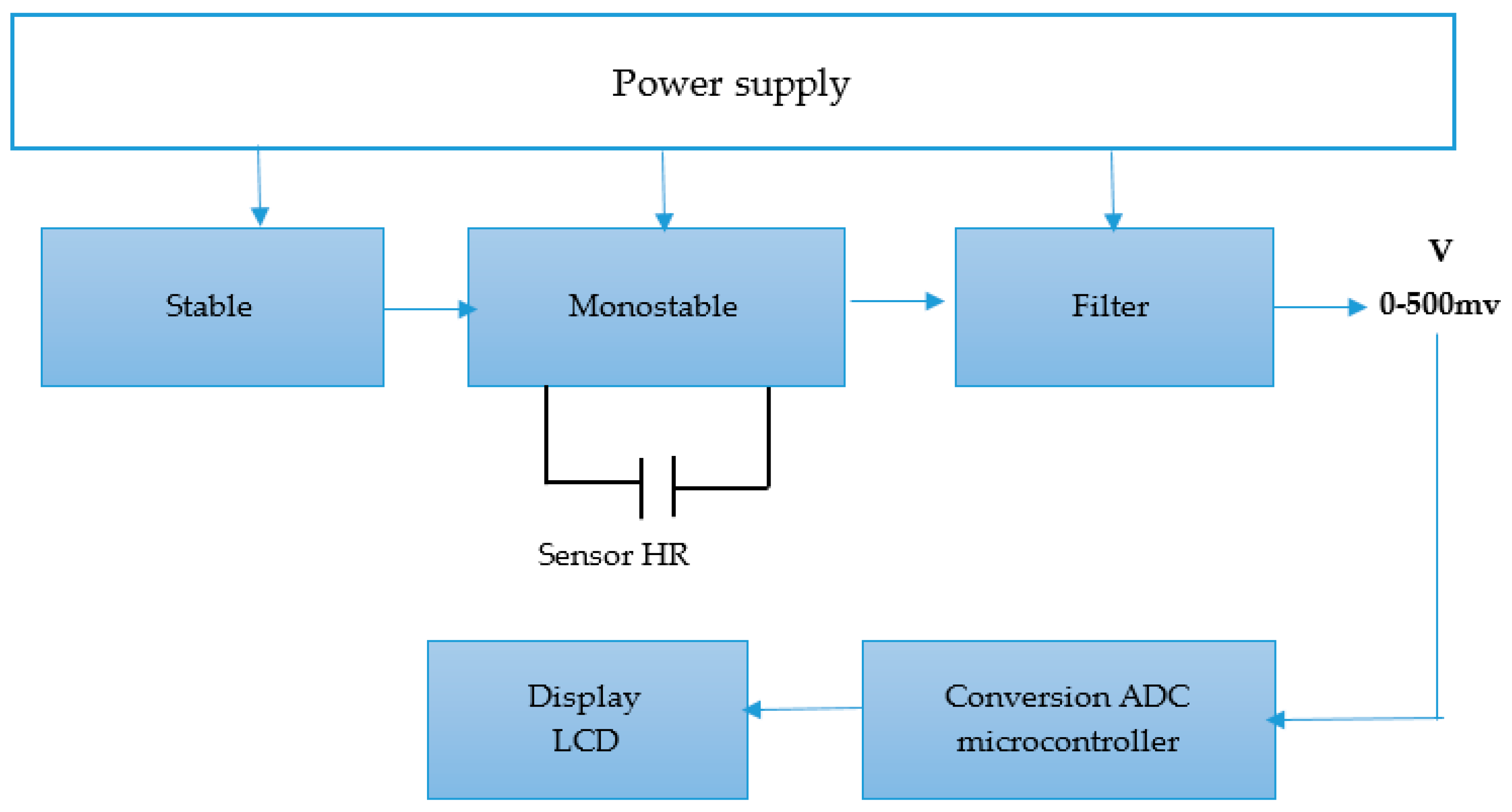
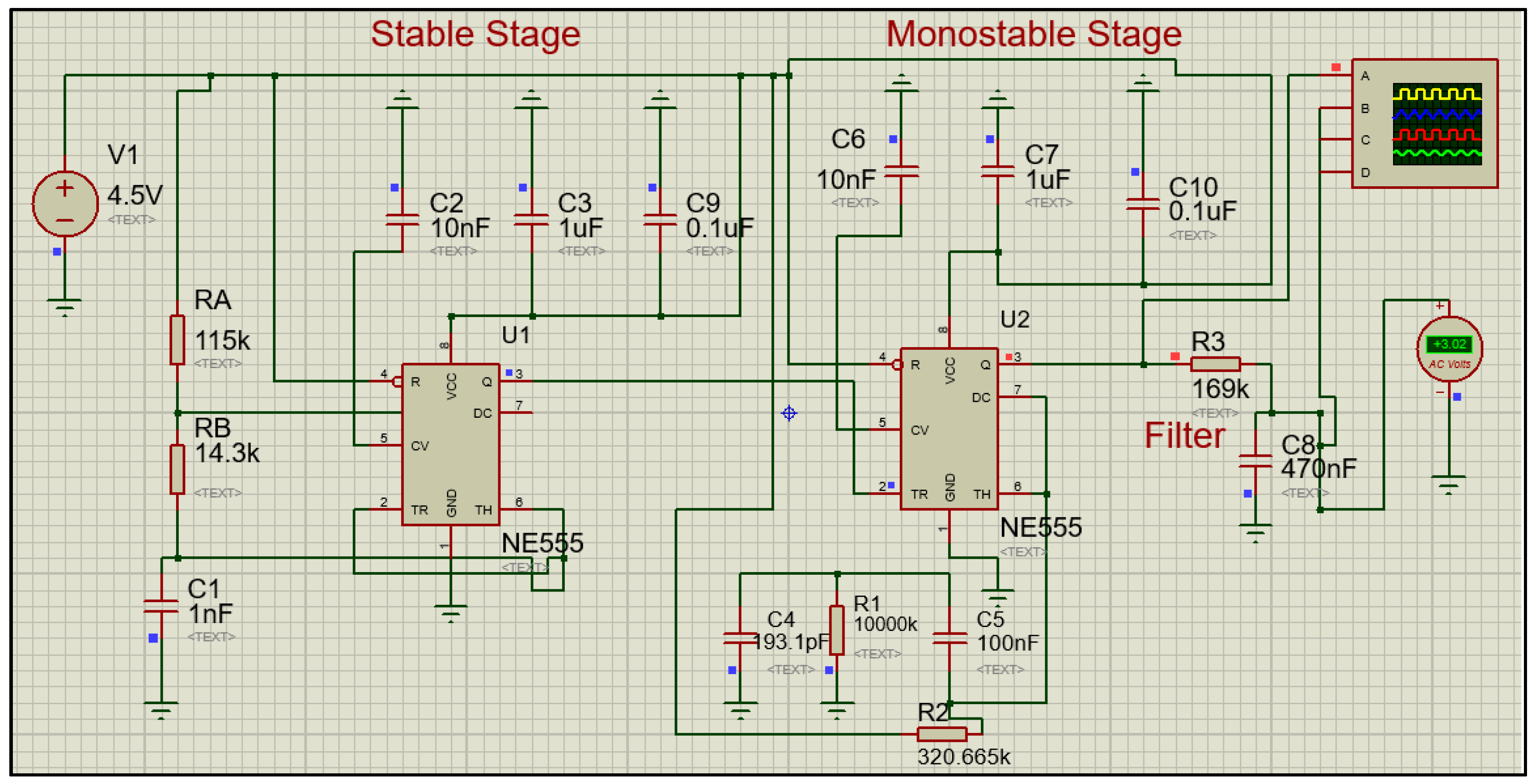
2.1. Relative Humidity Computation
- A = the area of the plates;
- d = the distance between the two conductors;
- ε = the electrical permittivity of the non-conductor material.
- Maximum supply voltage equal to 10 V;
- Unrestricted frequency range between 5 kHz and 300 kHz;
- Ability to measure between 0% (RH) and 100% (RH), which correspond, respectively, to the minimum (161.6 pF) and maximum (193.1 pF) capacitance values.
- f = the frequency (Hz);
- D = the duty cycle (%);
- RA, RB = the resistors (Ω);
- C = the capacitor (F).
- t = time (s);
- R = the resistor ;
- Cs = the variable capacitor of the HS1101LF sensor (F).
- Vout = the output voltage (V);
- Vcc = 4.5, the supply voltage (V);
- = time (s);
- f = the frequency (Hz).
- y = the relative humidity (%);
- x = the voltage (V);
- p1 = 55.43;
- p2 = −114.6;
- p3 = −76.87.
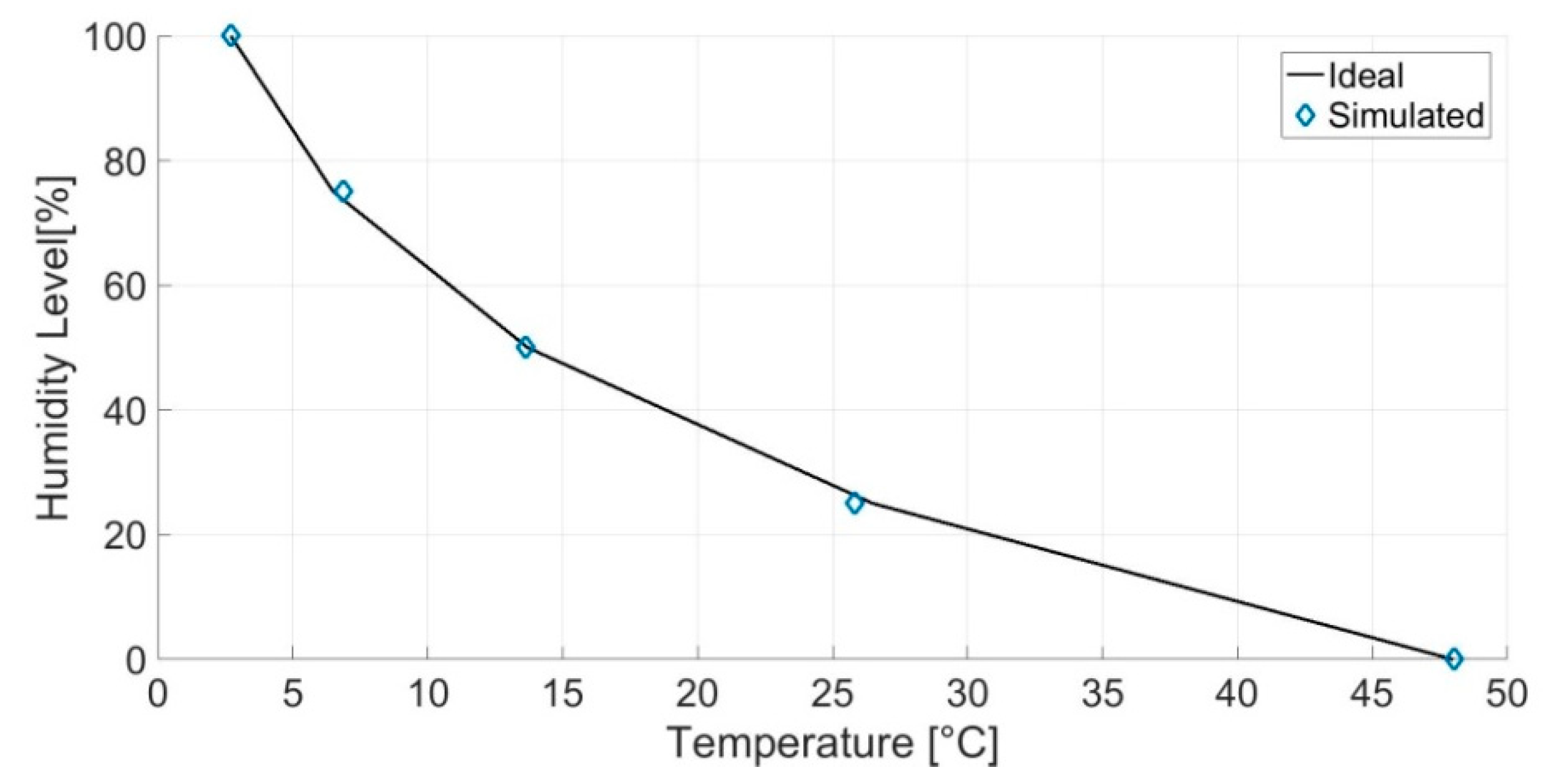
2.2. Ambient Temperature Computation
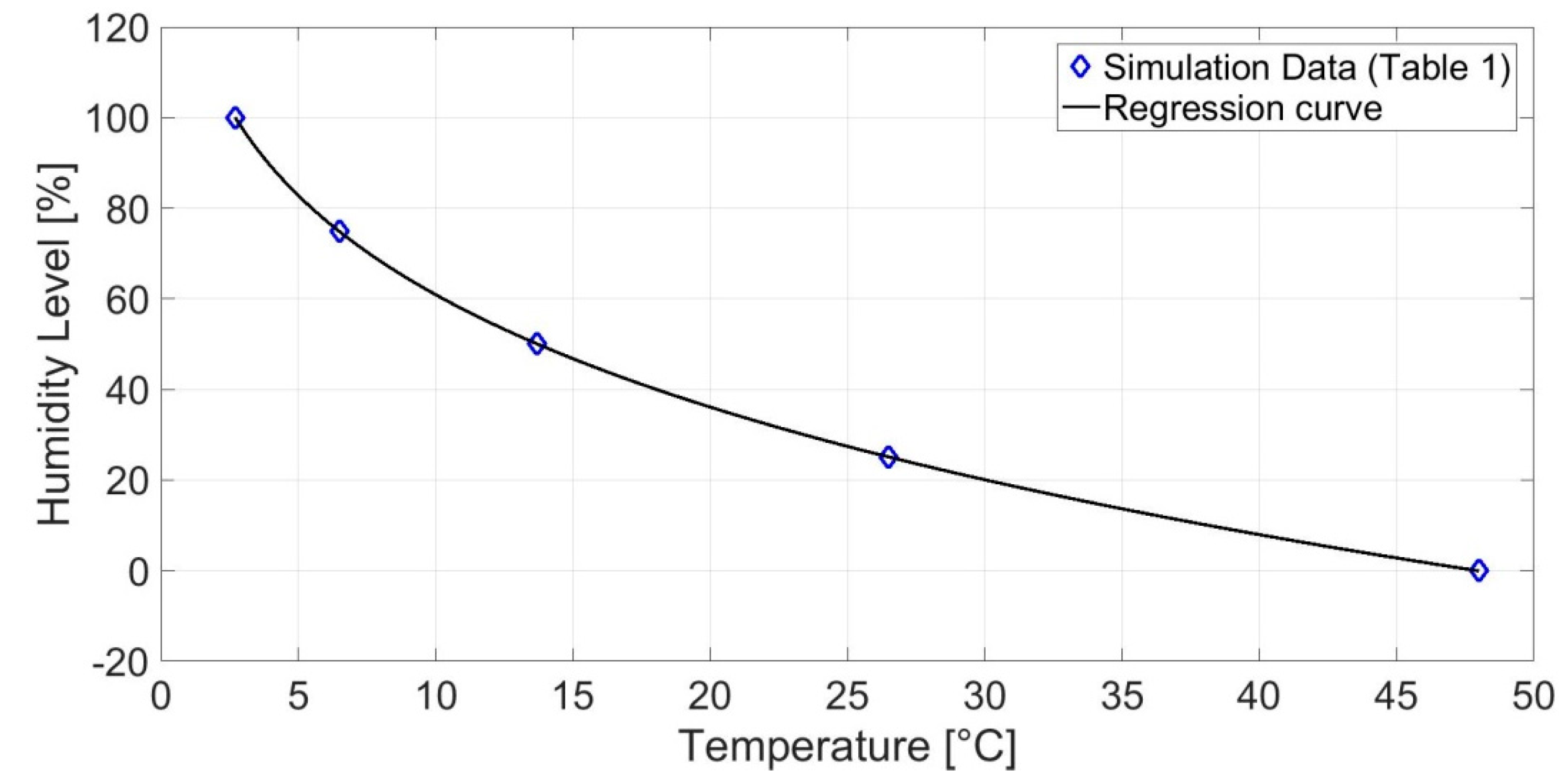
- y = the relative humidity (%);
- x = the temperature °C;
- a = −121.3;
- b = 0.18;
- c = 245.5.
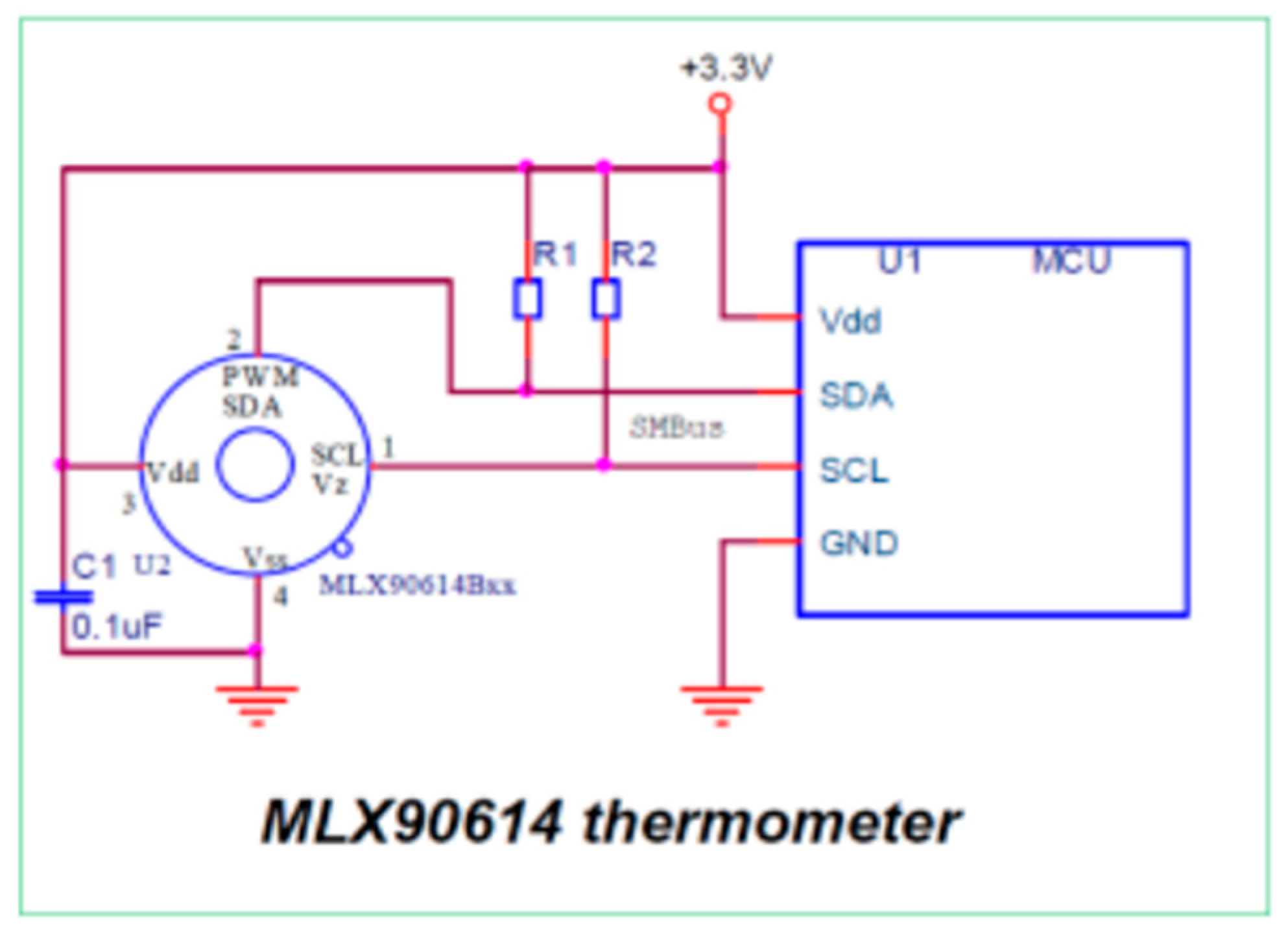
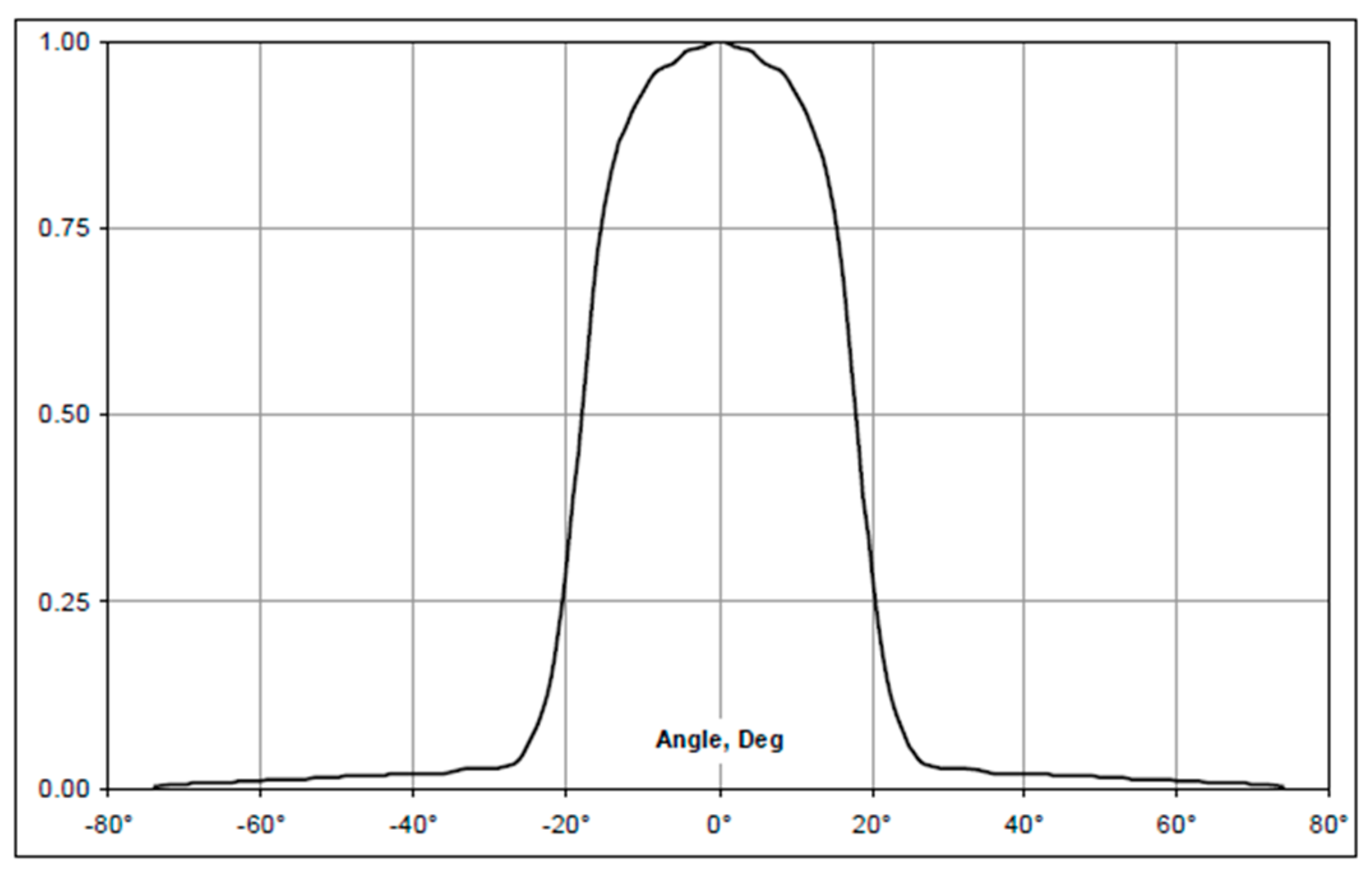
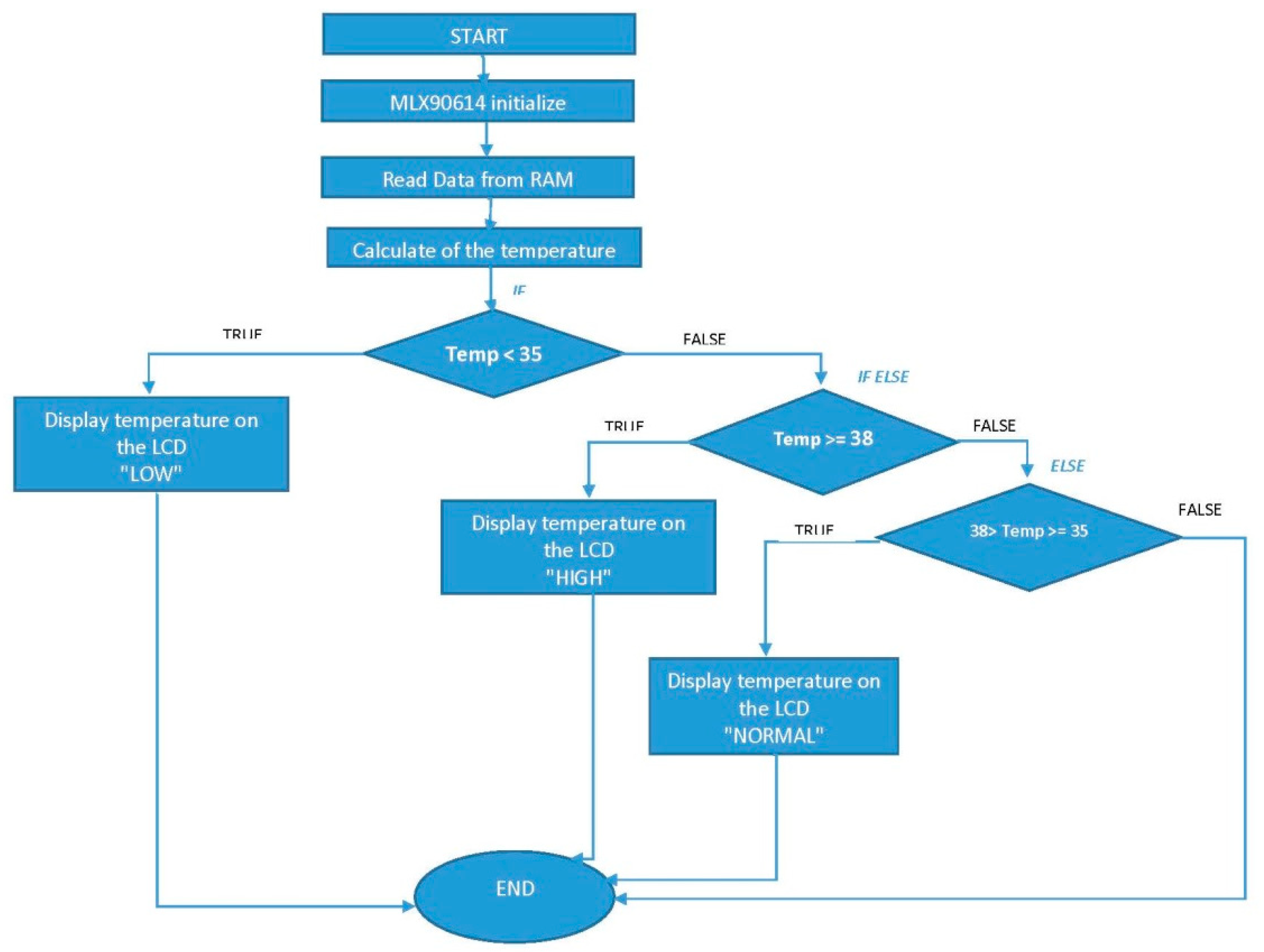
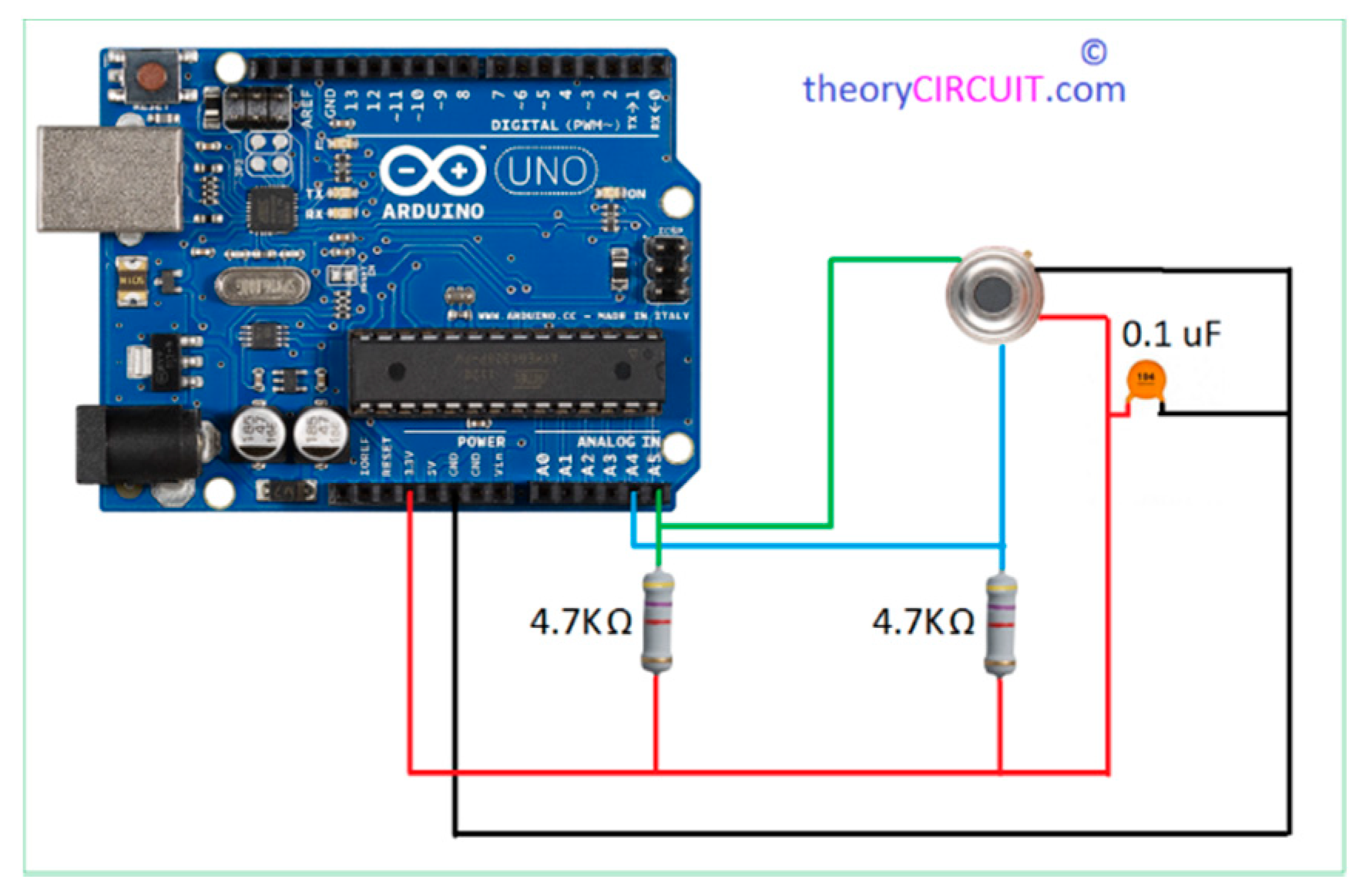
2.3. Body Temperature Computation
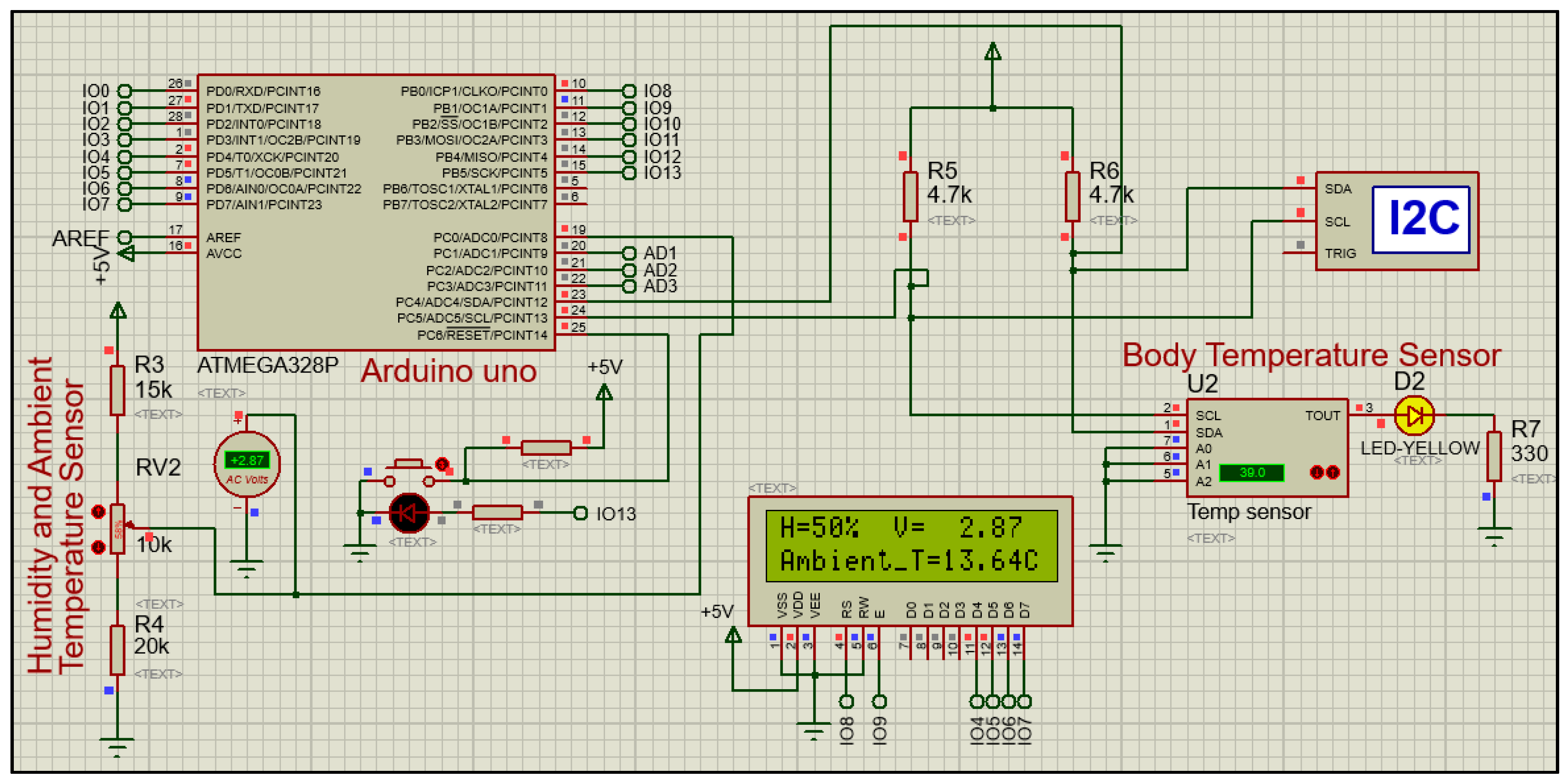
3. Simulation Results
4. Experimental Results
- Tb = the correct body temperature;
- TS = the measured system temperature;
- Ta = the ambient temperature.
5. Conclusions
Author Contributions
Funding
Conflicts of Interest
References
- Di Gennaro, F.; Pizzol, D.; Marotta, C.; Antunes, M.; Racalbuto, V.; Veronese, N.; Smith, L. Coronavirus Diseases (COVID-19) Current Status and Future Perspectives: A Narrative Review. Int. J. Environ. Res. Public Health 2020, 17, 2690. [Google Scholar] [CrossRef] [PubMed]
- Xie, J.; Zhu, Y. Association between ambient temperature and COVID-19 infection in 122 cities from China. Sci. Total Environ. 2020, 724, 1–5. [Google Scholar] [CrossRef] [PubMed]
- Xu, H.; Yan, C.; Fu, Q.; Xiao, K.; Yu, Y.; Han, D.; Wang, W.; Cheng, J. Possible environmental effects on the spread of COVID-19 in China. Sci. Total Environ. 2020, 731, 1–7. [Google Scholar] [CrossRef] [PubMed]
- RadiantWatch IoT Platform. Available online: https://radiantwatch.com/ (accessed on 5 September 2020).
- The Fight Against Novel Coronavirus: Automated Temperature Monitoring for COVID-19 Patients. Available online: http://www.vivalnk.com/covid-19 (accessed on 5 September 2020).
- Thermal Cameras Are Being Outfitted to Detect Fever and Conduct Contact Tracing for COVID-19. Available online: https://spectrum.ieee.org/news-from-around-ieee/the-institute/ieee-member-news/thermal-cameras-are-being-outfitted-to-detect-fever-and-conduct-contact-tracing-for-covid19 (accessed on 5 September 2020).
- With Safety in Phase 3 of the COVID-19 Pandemic. Available online: https://www.wikifriend.net/smart-health-coronavirus-thermal-scanner.html (accessed on 5 September 2020).
- This Temperature-Screening System for COVID-19 Can Check Up to 9 People at Once. Available online: https://spectrum.ieee.org/news-from-around-ieee/the-institute/ieee-member-news/this-temperaturescreening-system-for-covid19-can-check-up-to-9-people-at-once (accessed on 5 September 2020).
- Non-Contact Temperature Assessment Devices during the COVID-19 Pandemic. Available online: https://www.fda.gov/medical-devices/coronavirus-covid-19-and-medical-devices/non-contact-temperature-assessment-devices-during-covid-19-pandemic (accessed on 5 September 2020).
- Zheng, K.; Dong, R.; Wang, H.; Granick, S. Infrared assessment of human facial temperature in the presence and absence of common cosmetics. medRxiv 2020. [Google Scholar] [CrossRef]
- Zheng, J.; Menghan, H.; Zhongpai, G.; Fan, L.; Ranran, D.; Pan, Y.; Tang, W.; Guangtao, Z.; Yong, L. Detection of Respiratory Infections using RGB-infrared sensors on Portable Device. IEEE Sens. J. 2020. [Google Scholar] [CrossRef]
- Relative Humidity Sensor. HS1101LF Meets RoHS Regulations. Available online: https://www.alldatasheet.es/datasheet-pdf/pdf/241417/HUMIREL/HS1101LF.html (accessed on 5 September 2020).
- Sajadi, M.M.; Habibzadeh, P.; Vintzileos, A.; Shokouhi, S.; Miralles-Wilhelm, F.; Amoroso, A. Temperature, Humidity, and Latitude Analysis to Estimate Potential Spread and Seasonality of Coronavirus Disease 2019 (COVID-19). JAMA Netw. 2020, 3, 1–11. [Google Scholar] [CrossRef] [PubMed]
- Usamentiaga, R.; Venegas, P.; Guerediaga, J.; Vega, L.; Molleda, L.; Bulnes, F.G. Infrared Thermography for Temperature Measurement and Non-Destructive Testing. Open Access Sens. 2014, 1, 12308–12310. [Google Scholar] [CrossRef] [PubMed]
- Wang, D. FDC1004: Basics of Capacitive Sensing and Applications. Tex. Instrum. 2014, 1, 2. [Google Scholar]
- Zdankiewicz, E.M.; A Comparison of Relative Humidity Sensing Technologies. HIGOMETRIX Applications Note 2004-2, Volume 1, p. 3. Available online: https://docplayer.net/22214027-A-comparison-of-relative-humidity-sensing-technologies.html (accessed on 5 September 2020).
- Bhattacharya, Y.; Milne, M. Psychrometric Chart Tutorial: A Tool for Understanding Human Thermal Comfort Conditions; University of California: Los Angeles, CA, USA, 2009. [Google Scholar]
- Giddings, S.B. Hawking radiation, the Stefan–Boltzmann law, and unitarization. Phys. Lett. B 2016, 1, 40–42. [Google Scholar] [CrossRef]
- Lahiri, B.B.; Bagavathiappan, S.; Jayakumar, T.; Philip, J. Medical applications of infrared thermography: A review. Infrared Phys. Technol. 2012, 1, 226. [Google Scholar] [CrossRef] [PubMed]
- Karakostopulos, K. MLX90614 family Single and Dual Zone Infra Red Thermometer in TO-39. Melexis Microelectron. Integr. Syst. 2008, 1, 1–42. [Google Scholar]
- IR Thermometer Sensor MLX90614 SKU: SEN0206. Available online: https://wiki.dfrobot.com/IR_Thermometer_Sensor_MLX90614_SKU__SEN0206 (accessed on 5 September 2020).
- Infrared Thermometer Arduino. Available online: http://www.theorycircuit.com/infrared-thermometer-arduino/ (accessed on 5 September 2020).
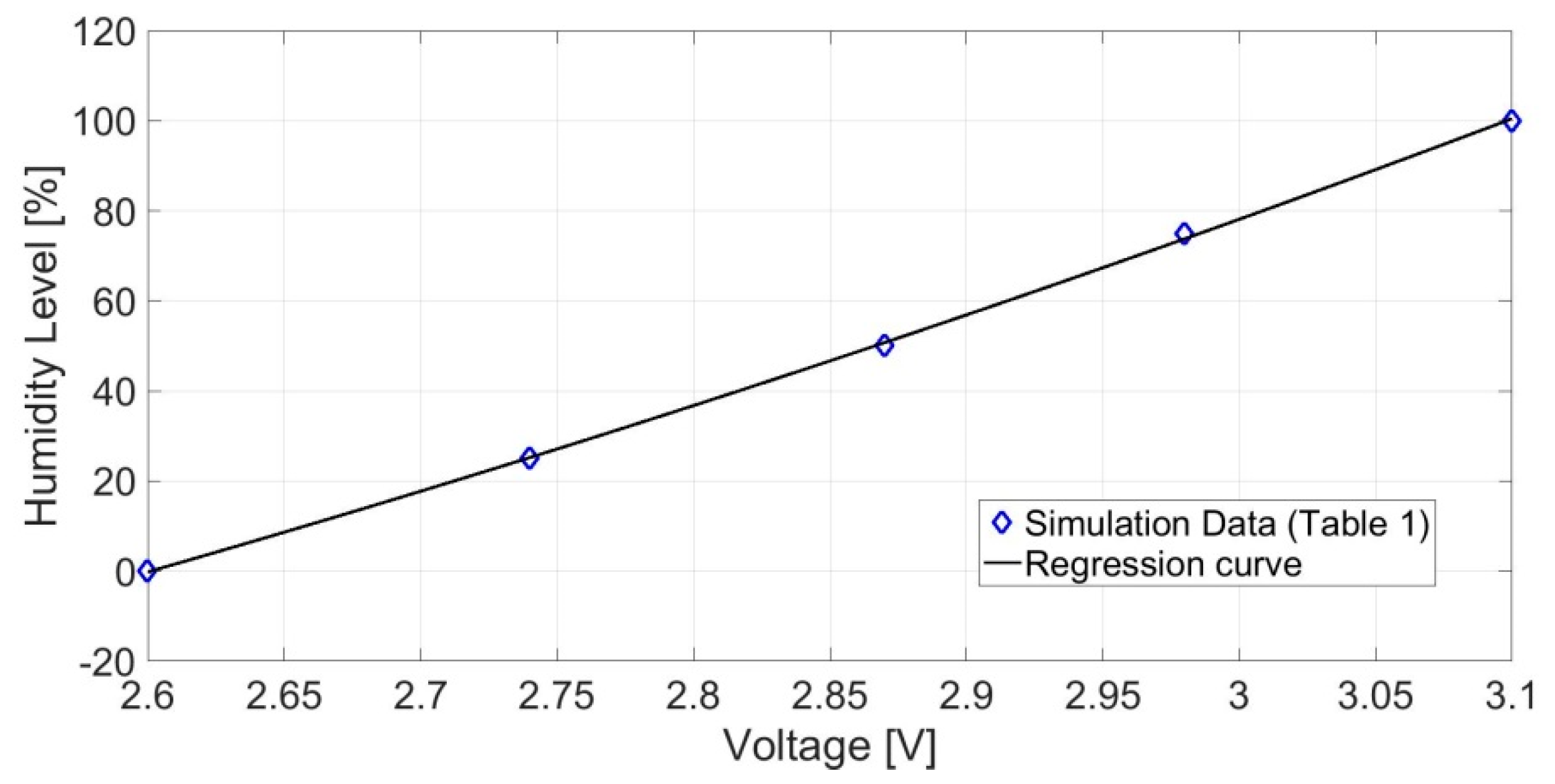

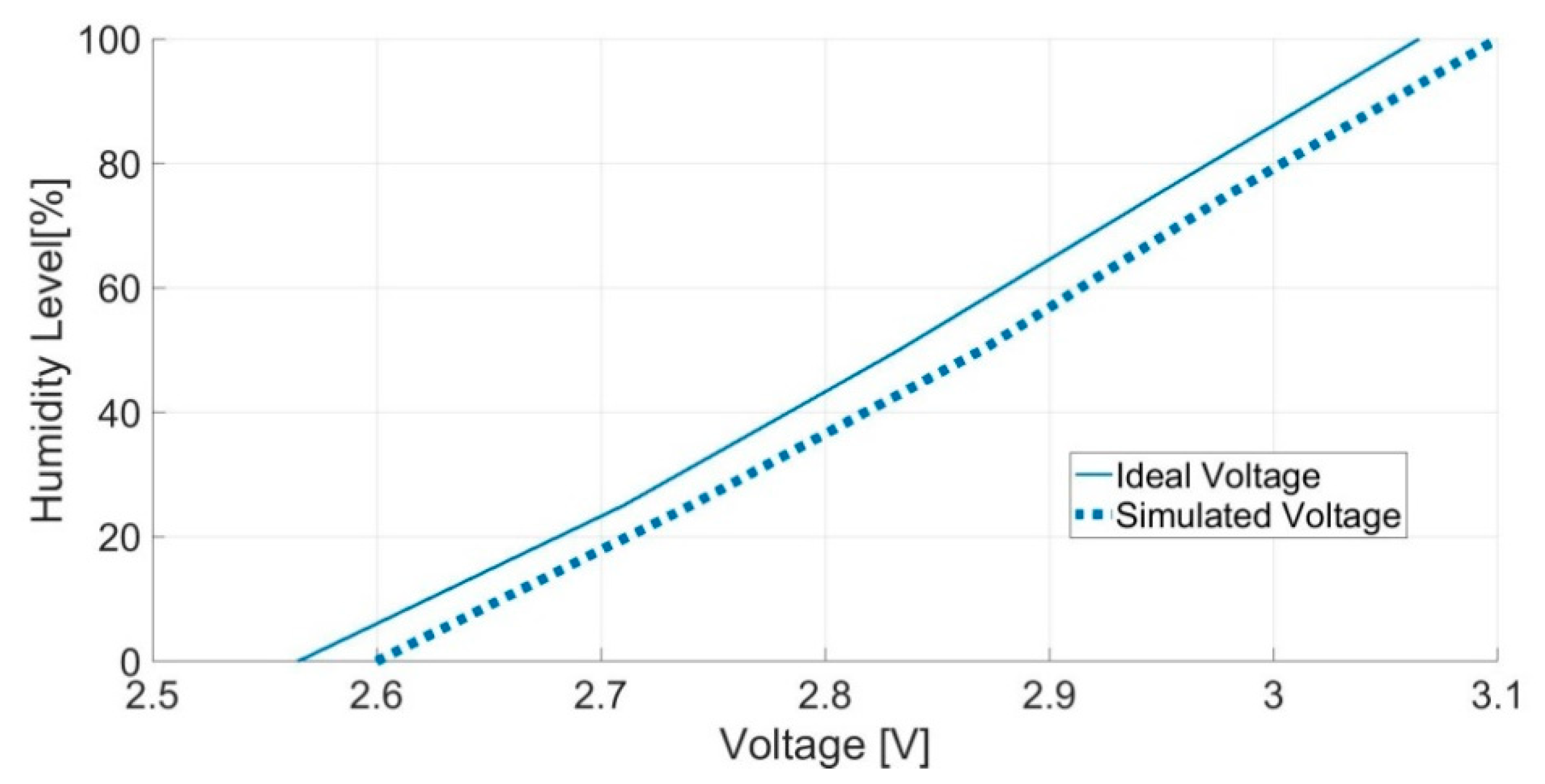



| RH% | C(pf) | Vout (V) Ideal | Vout (V) Simulation |
|---|---|---|---|
| 0 | 161.6 | 2.565 | 2.6 |
| 25 | 170.7 | 2.710 | 2.74 |
| 50 | 178.5 | 2.833 | 2.87 |
| 75 | 185.7 | 2.948 | 2.98 |
| 100 | 193.1 | 3.065 | 3.10 |
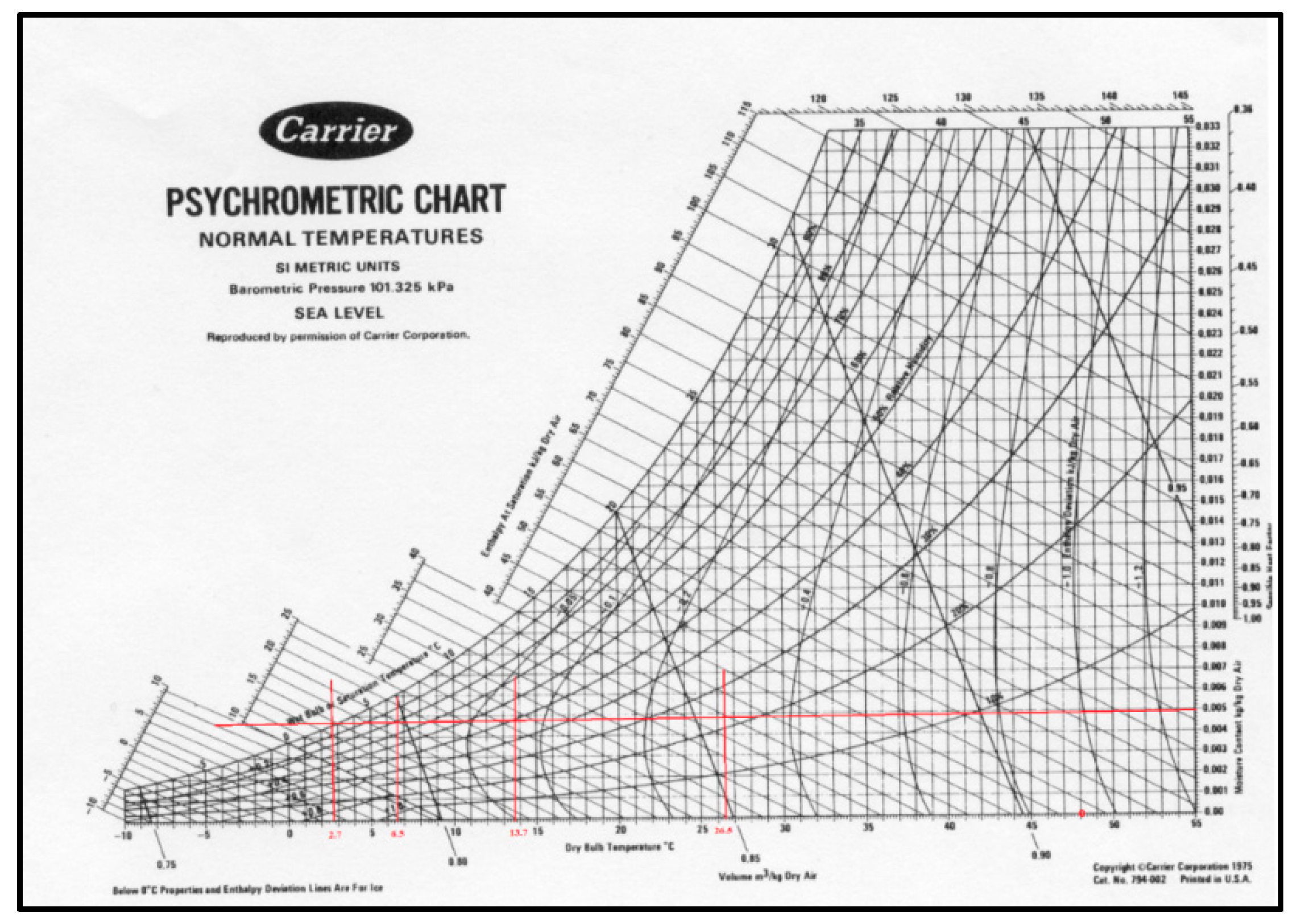
| Relativity Humidity (%) | Dry Bulb Temperature (°C) |
|---|---|
| 0 | 48 |
| 25 | 26.5 |
| 50 | 13.7 |
| 75 | 6.5 |
| 100 | 2.7 |
| C(pf) | Ideal RH% | Simulated RH% | Ideal Vout (V) | Simulated Vout (V) | Ideal Temperature (°C) | Simulated Temperature (°C) |
|---|---|---|---|---|---|---|
| 161.6 | 0 | 0 | 2.565 | 2.6 | 48 | 48.03 |
| 170.7 | 25 | 26 | 2.710 | 2.74 | 26.5 | 25.83 |
| 178.5 | 50 | 50 | 2.833 | 2.87 | 13.7 | 13.64 |
| 185.7 | 75 | 73 | 2.948 | 2.98 | 6.5 | 6.86 |
| 193.1 | 100 | 100 | 3.065 | 3.10 | 2.7 | 2.71 |
| Simulated body Temperature (°C) | State | Body Temperature (°K) | Power Radiation W/m^2 | |
|---|---|---|---|---|
| 30 | LOW | 303.15 | - | 95.71 |
| 34 | LOW | 307.15 | - | 100.9 |
| 36 | NORMAL | 309.15 | 0.2 | 103.5 |
| 38 | HIGH | 311.15 | - | 106.2 |
| 40 | HIGH | 313.15 | - | 109.1 |
| 30 | LOW | 303.15 | - | 287.2 |
| 34 | LOW | 307.15 | - | 302.5 |
| 36 | NORMAL | 309.15 | 0.6 | 310.5 |
| 38 | HIGH | 311.15 | - | 318.7 |
| 40 | HIGH | 313.15 | - | 327.1 |
| 30 | LOW | 303.15 | - | 478.5 |
| 34 | LOW | 307.15 | - | 504.3 |
| 36 | NORMAL | 309.15 | 1.0 | 517.4 |
| 38 | HIGH | 311.15 | - | 531.3 |
| 40 | HIGH | 313.15 | - | 545.3 |
| Implemented System | Traditional Thermometer | Body Temperature Difference | ||
|---|---|---|---|---|
| Ambient Temperature (°C) | Relative Humidity (%) | Body Temperature (°C) | - | - |
| 29 | 67 | 31.11 | 36.6 | 5.49 |
| 29 | 67 | 31.1 | 36.5 | 5.4 |
| 29 | 67 | 31.13 | 36.4 | 5.27 |
| 29 | 67 | 31.13 | 36.7 | 5.27 |
| 29 | 67 | 31.12 | 36.3 | 5.18 |
| Average | 31.12 | 36.5 | 5.32 | |
| Hour | Implemented System | Traditional Thermometer | Absolute Error | Relative Error % | ||
|---|---|---|---|---|---|---|
| - | Body temperature (°C) | Ambient temperature (°C) | Relative humidity (%) | - | - | - |
| 6:00 | 35.85 | 24 | 70 | 35.9 | 0.05 | 0.14 |
| 10:00 | 36.21 | 29 | 54 | 36.4 | 0.19 | 0.52 |
| 14:00 | 36.75 | 34 | 52 | 36.9 | 0.15 | 0.41 |
| 16:00 | 36.51 | 31 | 57 | 36.7 | 0.19 | 0.52 |
| 17:00 | 36.32 | 29 | 59 | 36.6 | 0.28 | 0.76 |
| 21:00 | 36.12 | 28 | 63 | 36.3 | 0.18 | 0.49 |
| Average error | 0.47 | |||||
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Costanzo, S.; Flores, A. A Non-Contact Integrated Body-Ambient Temperature Sensors Platform to Contrast COVID-19. Electronics 2020, 9, 1658. https://doi.org/10.3390/electronics9101658
Costanzo S, Flores A. A Non-Contact Integrated Body-Ambient Temperature Sensors Platform to Contrast COVID-19. Electronics. 2020; 9(10):1658. https://doi.org/10.3390/electronics9101658
Chicago/Turabian StyleCostanzo, Sandra, and Alexandra Flores. 2020. "A Non-Contact Integrated Body-Ambient Temperature Sensors Platform to Contrast COVID-19" Electronics 9, no. 10: 1658. https://doi.org/10.3390/electronics9101658
APA StyleCostanzo, S., & Flores, A. (2020). A Non-Contact Integrated Body-Ambient Temperature Sensors Platform to Contrast COVID-19. Electronics, 9(10), 1658. https://doi.org/10.3390/electronics9101658






