The Role of Machine Learning in AR/VR-Based Cognitive Therapies: A Systematic Review for Mental Health Disorders
Abstract
1. Introduction
2. Recent Advancements in Machine Learning for Digital Health Solutions
2.1. Research Questions
2.1.1. The Role of AR/VR in Cognitive Therapies
2.1.2. ML for Personalization in Cognitive Therapy
2.1.3. Predictive Analytics in Mental Health Outcomes
2.1.4. Comparative Studies of AR/VR and Traditional Cognitive Therapies
2.1.5. RL and Adaptation in AR/VR Therapy
2.1.6. Technological Innovations in ML-AR/VR Cognitive Therapies
3. Materials and Methods
3.1. Search Sources and Databases
- PubMed (for biomedical and psychological studies).
- Scopus (multidisciplinary coverage).
- Web of Science (broad citation index).
- IEEE Xplore (for technological advancements in AR/VR and ML).
- PsycINFO (for mental health-focused interventions).
- Google Scholar (for Supplementary Articles and the gray literature).
- A total of 258 duplicate records.
- A total of 23 records due to language restrictions.
- A total of 14 records published before 2014.
- A total of 21 records with non-relevant titles.
- A total of 61 records for being irrelevant to the topic.
- A total of 49 non-empirical articles, such as commentaries, opinion pieces, and reviews.
- Two were excluded for insufficient methodological detail.
- Nine were excluded for lacking direct relevance to the research question.
3.2. Search Strategy
3.3. Inclusion and Exclusion Criteria
3.4. Risk of Bias Assessment
- 1.
- Selection Bias (Random sequence generation and allocation concealment)
- Low Risk: Studies that described adequate randomization methods and allocation concealment.
- Unclear Risk: Studies that lacked detailed descriptions of randomization or allocation procedures.
- 2.
- Performance Bias (Blinding of participants and personnel)
- Moderate-to-High-Risk: Blinding was inconsistently reported, particularly in AR/VR systems studies where blinding is inherently challenging.
- 3.
- Detection Bias (Blinding of outcome assessors)
- Low Risk: Most studies employed objective outcome measures (e.g., validated clinical scales for PTSD, anxiety, or cognitive performance), reducing detection bias.
- Moderate Risk: A subset of studies did not explicitly report the blinding of assessors.
- 4.
- Attrition Bias (Incomplete outcome data)
- Moderate Risk: Studies involving long-term AR/VR interventions or follow-up periods observed high dropout rates. Many mitigated this issue using intention-to-treat analyses.
- 5.
- Reporting Bias (Selective reporting)
- Low Risk: Most studies reported primary and secondary outcomes as outlined in their protocols.
- Moderate Risk: Some studies omitted exploratory analyses or lacked transparency regarding secondary outcomes.
- 6.
- Other Bias (Funding and conflicts of interest)
- Moderate Risk: A subset of studies involving ML-driven AR/VR platforms, particularly those funded by industry stakeholders, lacked transparency regarding potential conflicts of interest.
- 1.
- Selection Bias
- Low Risk: Studies with clearly defined inclusion/exclusion criteria, well-documented participant selection processes, and appropriate comparison groups.
- High Risk: Studies with unclear eligibility criteria, convenience sampling, or selection processes prone to confounding bias.
- 2.
- Comparability of Groups
- Low Risk: Studies controlled for confounding variables using statistical adjustments (e.g., propensity score matching, regression models).
- Moderate-to-High Risk: Studies that lacked appropriate matching or adjustment techniques.
- 3.
- Measurement Bias (Outcome Assessment and Blinding)
- Low Risk: Studies using validated instruments for outcome measurement with trained assessors.
- Moderate Risk: Studies with self-reported measures or without the assessor blinding.
- 4.
- Attrition and Follow-Up Bias
- Low Risk: Studies with high retention rates and thorough handling of missing data.
- High Risk: Studies with high dropout rates and insufficient handling of missing data.
- 5.
- Reporting Bias
- Low Risk: Studies that transparently reported all planned outcomes.
- Moderate Risk: Studies where outcome reporting was selective or inconsistent.
4. Results
4.1. [RQ1] How Effective Are Augmented and Virtual Reality Technologies in Enhancing Traditional Cognitive Therapies for Treating Mental Health Disorders Such as PTSD, Anxiety Disorders, and Phobias?
- Symptom Reduction: VRET demonstrates superior effectiveness in reducing symptoms of PTSD, anxiety, and phobias compared to traditional methods.
- Engagement: Higher levels of patient engagement are observed in VRET due to immersive and interactive virtual environments.
- Accessibility: VR-based therapy significantly outperforms traditional treatment in terms of accessibility, allowing patients in remote locations or those with mobility constraints to receive treatment.
- Cost-Effectiveness: VRET provides a more scalable and cost-effective treatment option, reducing the need for in-person sessions and infrastructure.
- Adherence: Patient adherence is slightly higher in VRET, as the immersive nature of VR therapy increases motivation and reduces dropout rates.
4.2. [RQ2] How Can Machine Learning Algorithms Enhance the Personalization of AR/VR-Based Cognitive Therapies to Address Individual Patients’ Needs Better?
- Personalized feedback mechanisms exhibit the highest ML integration (92%), with an impact score of 96%, underscoring the effectiveness of AI-driven response adjustments based on user interactions.
- Real-time adaptation, which dynamically modifies therapy based on physiological and behavioral responses, has an ML integration of 88% and an impact score of 94%, confirming the clinical relevance of adaptive environments.
- Outcome prediction models, responsible for forecasting treatment success using neural networks and decision trees, have an ML integration rate of 89% and an impact score of 92%, highlighting the growing importance of predictive analytics in therapy optimization.
- Physiological data utilization, incorporating real-time heart rate variability (HRV), EEG signals, and galvanic skin response (GSR), shows an ML integration score of 90% and an impact score of 93%, indicating strong AI-driven adaptability.
- Treatment success prediction relies on ML models to determine therapy effectiveness based on prior patient responses. It has an ML integration of 85% and an impact score of 91%, solidifying its role in precision medicine applications.
- Early non-responder detection, using ML classifiers such as random forests, support vector machines, and neural networks, is integrated into 84% of therapy models, with an impact score of 88%, reflecting its significance in reducing dropout rates and improving treatment efficacy.
- A 12% increase in treatment adherence when therapy modalities are optimized via AI-driven patient profiling.
- A 10–15% improvement in response rates for AR/VR-based cognitive therapies when ML is used for adaptive difficulty scaling.
- An 86% prediction accuracy in ML models that determine individualized therapy difficulty levels based on prefrontal cortex activity and behavioral markers.
- A 77% success rate in predicting therapy outcomes in iCBT, surpassing traditional therapist-led predictions.
- Artificial neural networks (ANNs) remain pivotal in predictive modeling and treatment success prediction. They leverage large-scale patient datasets to forecast therapy outcomes with up to 77% accuracy, thereby refining intervention strategies dynamically.
- Reinforcement learning (RL) is a core driver of real-time adaptation and custom difficulty adjustment. It enables dynamic modifications of VR therapy based on real-time patient responses, biometric feedback, and behavioral performance metrics.
- Supervised learning significantly enhances predictive modeling and treatment success forecasting, achieving up to 86% accuracy in therapy difficulty scaling by training models on labeled datasets of patient behaviors and treatment responses.
- Unsupervised learning is crucial in personalized feedback and monitoring, identifying hidden patterns in patient interaction data, and optimizing therapy parameters in AR/VR interventions.
- Natural language processing (NLP) augments real-time adaptation and personalized feedback monitoring, particularly within VR-based therapy environments, where automated sentiment analysis and conversational AI enhance patient-therapist interactions.
- Physiological data utilization further refines ML-driven real-time adaptation, integrating heart rate variability (HRV), EEG signals, and galvanic skin responses (GSRs) to adjust virtual environments dynamically based on emotional and physiological states.
- Reinforcement learning (RL) exhibits the highest dominance in real-time adaptation (92%) and custom difficulty adjustment (89%), making it exceptionally effective in dynamically modifying therapy sessions based on patient responses, biometric data, and performance metrics.
- Neural networks (NNs) play a leading role in predictive modeling (85%) and treatment success prediction (88%), leveraging large-scale patient datasets to forecast therapy outcomes and optimizing intervention strategies.
- Supervised learning strongly contributes to predictive modeling (80%) and treatment success prediction (86%), benefiting from highly structured datasets that enhance therapy customization and predictive accuracy.
- Unsupervised learning is integral to custom difficulty adjustment (70%) and personalized feedback monitoring (82%). It detects hidden patient behavior patterns that allow real-time therapy optimization.
- Natural language processing (NLP) ranks highest in personalized feedback monitoring (91%) and real-time adaptation (75%), supporting virtual therapist interactions, sentiment analysis, and automated response generation in VR-based therapeutic environments.
4.3. [RQ3] How Can Machine Learning Models Be Leveraged to Predict Patient Outcomes and Therapy Effectiveness in AR/VR-Based Cognitive Therapies?
- 1.
- Outcome Prediction and Accuracy
- ○
- ML models demonstrated an 84% integration rate in predictive analytics for treatment outcomes, impacting predictive accuracy at 92%.
- ○
- This suggests that ML-based predictive models significantly improve the ability to forecast treatment success, personalize interventions, and adapt therapy dynamically.
- 2.
- Real-Time Data Utilization
- ○
- In total, 88% of the studies incorporated real-time data utilization, with a 92% impact on predictive accuracy.
- ○
- This supports the hypothesis that physiological signals, behavioral responses, and patient engagement metrics collected in real-time significantly refine therapy adjustments and enhance patient responsiveness.
- 3.
- Key Predictive Factors and Therapy Adjustment
- ○
- Studies utilizing feature selection techniques and dynamic exposure models had an 85–87% integration rate, with impact accuracy ranging between 88% and 91%.
- ○
- This confirms the effectiveness of ML in adapting virtual environments, tailoring exposure therapy for phobias, and modifying intervention difficulty based on patient progress.
- 4.
- Longitudinal Data and Prognostic Accuracy
- ○
- The use of longitudinal data integration in predictive modeling had an 80% adoption rate, with a 92% impact on long-term prognosis accuracy.
- ○
- These findings suggest that ML-driven predictive analytics can improve long-term patient outcomes by identifying response patterns over multiple therapy sessions.
- 5.
- Session-by-Session Monitoring and Physiological Insights
- ○
- ML-based session monitoring techniques had an 81% integration rate, with a 86% accuracy impact, highlighting their importance in tracking patient engagement and response.
- ○
- Similarly, physiological data-driven models (e.g., heart rate variability, galvanic skin response) showed an 86% integration rate and a 90% impact on predictive accuracy, reinforcing their role in adaptive intervention strategies.
- 1.
- Expanded ML Approaches
- ○
- Supervised learning contributes significantly to outcome prediction and long-term prognosis, ensuring data-driven therapy success forecasting.
- ○
- Unsupervised learning is integrated into real-time data utilization and session monitoring, identifying hidden patterns in patient responses.
- ○
- Semi-supervised learning refined predictive factors and physiological data insights, improving patient-specific therapy adjustments.
- ○
- Reinforcement learning enables adaptive therapy adjustment and dynamic exposure levels, adapting therapy difficulty based on patient performance.
- ○
- Transfer learning enhances outcome prediction and predictive factors, leveraging pre-trained models to improve therapy accuracy.
- ○
- Federated learning strengthens real-time data integration and longitudinal tracking, ensuring privacy-preserving, and decentralized model improvements.
- 2.
- Predictive Analytics and Personalized Therapy Adjustments
- ○
- Predictive modeling, feature selection, and longitudinal data integration highlight ML’s ability to refine therapy dynamically.
- ○
- Real-time data utilization and adaptive therapy adjustment are central nodes, demonstrating their strong influence on ML-driven therapy modifications.
- ○
- Key ML models such as random forest, support vector machines, deep neural networks, and elastic net contribute to the predictive capabilities of ML in AR/VR-based therapies.
- 3.
- Interconnected Data-Driven Decision Making
- ○
- The connections between nodes illustrate how ML enables therapy process optimization, including the following:
- ▪
- Predictive factors influencing outcome prediction.
- ▪
- Real-time data utilization enhancing dynamic exposure adjustments.
- ▪
- Longitudinal data integration supporting therapy progress tracking.
- ○
- This integration fosters continuous learning models, adapting intervention strategies based on real-time patient responses.
- Incorporating additional physiological and behavioral metrics (e.g., biometric data, EEG, and facial emotion recognition).
- Enhancing adaptive models with reinforcement learning for more responsive therapy sessions.
- Exploring decentralized ML techniques, such as federated learning, to maintain privacy while improving model generalization.
4.4. [RQ4] How Does the Effectiveness of AR/VR-Based Cognitive Therapies Compare to Traditional Cognitive Therapies for the Treatment of Mental Health Disorders?
- 1.
- Exposure Therapy and Symptom Management
- AR/VR-based exposure therapy demonstrated an 85% effectiveness rate, compared to 75% in traditional exposure therapy. Creating controlled, immersive environments for exposure tasks contributes to this advantage.
- In symptom management, VR-based interventions achieved 82% effectiveness, slightly exceeding the 78% effectiveness of traditional cognitive therapies.
- 2.
- Cognitive Enhancement and Long-Term Stability
- Cognitive enhancement interventions utilizing AR/VR technologies showed 84% effectiveness, outperforming traditional methods (77%). This aligns with studies showing that VR-based cognitive training enhances memory retention, executive function, and problem-solving abilities.
- Long-term stability of treatment effects was comparable, with AR/VR at 80% and traditional therapies at 78%, indicating that both modalities sustain therapeutic benefits over time.
- 3.
- Engagement, Retention, and Adaptability
- Engagement and retention rates were significantly higher for AR/VR-based therapies (87%) than traditional therapies (73%), demonstrating the motivational advantage of immersive environments.
- Immersion and adaptability were also significantly higher in AR/VR-based interventions, with an 88% effectiveness rate, compared to 70% in traditional therapies.
- 4.
- Dynamic Adjustments and Personalization
- AR/VR-enabled real-time adjustments in therapy sessions resulted in an 86% effectiveness rate, compared to 72% in conventional therapies.
- Personalization, where treatment is tailored based on machine learning (ML) models and patient biometrics, showed 90% effectiveness in VR-based therapies, significantly exceeding the 75% rate observed in traditional therapies.
- 5.
- Safety, Control, and Dropout Rates
- Safety and control in AR/VR-based therapies were rated at 89% effectiveness, compared to 80% in traditional methods. This is attributed to the ability to provide controlled, low-risk exposure environments for patients undergoing anxiety and phobia treatment.
- Dropout rates were significantly lower in VR-based interventions, with 83% adherence, compared to 68% in traditional therapies, emphasizing immersive treatment modalities’ increased engagement and acceptability.
4.5. [RQ5] How Can RL and Adaptive Algorithms Optimize the Therapeutic Experience in AR/VR-Based Cognitive Therapies?
- Personalization: RL-driven systems tailor therapy sessions by adjusting content, intensity, and pace according to each patient’s unique needs and cognitive profile.
- Real-Time Adaptation: Adaptive models modify treatment scenarios dynamically based on biometric signals and patient performance (e.g., heart rate, neural activity, or response accuracy).
- Engagement and Motivation: Gamification techniques integrated with RL boost patient interaction, ensuring that therapy remains challenging yet achievable to maintain adherence.
- Dynamic Feedback: Real-time feedback mechanisms provide instant response adjustments, reinforcing positive therapeutic behaviors and improving intervention efficacy.
- Long-Term Optimization: By continuously learning from patient data, RL refines treatment pathways over time, ensuring sustained cognitive improvements and minimizing therapy dropout rates.
- Dynamic Difficulty Adjustment: Therapy difficulty scales dynamically, ensuring patients remain in an optimal challenge zone to maximize engagement.
- Predictive Modeling: Machine learning models forecast treatment responses, allowing proactive modifications to intervention strategies.
- Physiological Signal Processing: Real-time analysis of biometric indicators (e.g., galvanic skin response, EEG) enables adaptive interventions based on emotional and cognitive states.
- Therapeutic Gamification: RL introduces personalized reward systems, making AR/VR therapies more immersive and enjoyable.
- Real-Time Feedback Integration: Interactive mechanisms modify therapy components in real time, ensuring continuous adaptation to patient needs.
4.6. [RQ6] What Are the Latest Technological Innovations in Machine Learning and AR/VR That Are Transforming the FIELD of Cognitive Therapy?
5. Discussion
- RL substantially impacts real-time adaptation and cognitive improvements, supporting its role in dynamically adjusting therapy scenarios to user behaviors.
- ANNs and DL are shown to be highly effective in predictive analytics and cognitive therapy enhancements, suggesting their utility in pattern recognition for patient progress tracking.
- NLP contributes substantially to emotional engagement, reinforcing its effectiveness in virtual therapeutic conversations and AI-driven interventions.
- ML-based personalization and RL support individualized therapy experiences, ensuring that interventions dynamically adjust to patient needs.
- Conversely, predictive analytics and ANNs contribute to structured outcome assessments, ensuring that treatment protocols remain scientifically rigorous and scalable across diverse patient populations.
- AI-Driven Predictive Analytics: The results suggest increasing reliance on ML models for outcome forecasting, enabling clinicians to modify therapy regimens preemptively based on predicted patient trajectories.
- Ethical and Transparency Considerations: The decisive role of deep learning and NLP in cognitive therapy suggests that issues related to data transparency, bias in ML models, and interpretability of AI-driven recommendations should be further investigated.
- Hybrid AI-Therapist Models: Given that specific ML techniques (e.g., RL) show stronger associations with therapy adaptation, future research should explore the potential of AI–human hybrid therapy models, where ML systems assist but do not replace human clinical expertise.
- Optimizing Real-Time Adaptation: Enhancing RL frameworks for real-time therapeutic adjustments based on biometric and behavioral feedback.
- Fine-Tuning Predictive Accuracy: Integrating ANNs with larger multimodal datasets to improve the precision of patient progress tracking and therapy effectiveness forecasting.
- Expanding NLP Applications in Cognitive Therapy: Further refining AI-driven virtual therapists to enhance patient engagement and ensure ethical conversational boundaries.
5.1. Ethical Considerations
- 1.
- Compliance with GDPR and HIPAA:
- ▪
- General Data Protection Regulation (GDPR): This regulation ensures that data minimization, informed consent, and the right to be forgotten are upheld in ML-driven therapy applications. Patients must have complete transparency over how their data is used and stored.
- ▪
- Health Insurance Portability and Accountability Act (HIPAA): This act mandates strict encryption, access controls, and audit trails for healthcare-related patient data, which must be adhered to in ML-AR/VR mental health platforms.
- ▪
- Privacy-Preserving AI Techniques: Applying homomorphic encryption, federated learning, and differential privacy can reduce data leakage risks while ensuring model effectiveness.
- 2.
- Institutional Responsibility and Transparency:
- ▪
- Healthcare providers and developers must establish clear policies on data access, anonymization, and storage to prevent unauthorized use of sensitive patient information.
- ▪
- Patients should receive accessible consent mechanisms to opt in or out of AI-driven therapy models.
- 1.
- Addressing Algorithmic Bias:
- ▪
- Bias may emerge from skewed training data, inconsistent model validation, or preconceived assumptions embedded in algorithm design. Ensuring demographically diverse datasets is critical to avoiding biases in therapy recommendations.
- ▪
- The application of bias mitigation techniques, such as re-weighted sampling, fairness-aware learning, and adversarial debiasing, can enhance equity in AI-driven cognitive therapies.
- 2.
- Domain Bias and Context Adaptation:
- ▪
- ML models trained in one setting (e.g., a Western clinical trial) may not generalize well to different cultural, linguistic, or socioeconomic backgrounds.
- ▪
- Adaptive AI frameworks should be designed to dynamically adjust models to individual patient profiles without reinforcing systemic disparities.
- 3.
- Ethical Implications of AI Decision-Making in Mental Health:
- ▪
- While AI-enhanced AR/VR therapy can personalize mental health treatments, reliance on automated decision-making raises concerns about human oversight and clinical accountability.
- ▪
- It is crucial that therapists remain actively involved in evaluating AI-generated therapy recommendations to prevent over-reliance on opaque algorithms that may not fully capture complex patient conditions.
- 1.
- Informed Consent in AI-Augmented Therapy:
- ▪
- Patients must be explicitly informed about AI’s role in their treatment, including potential risks, limitations, and benefits of ML-driven therapy personalization.
- ▪
- Explainable AI (XAI) techniques should be integrated into AR/VR mental health platforms, allowing patients and clinicians to understand how ML models generate recommendations.
- 2.
- Therapeutic Responsibility and AI Transparency:
- ▪
- AI should not replace human clinical judgment, and systems should be auditable, interpretable, and subject to independent oversight.
- ▪
- Continuous ethical monitoring and evaluation of ML-integrated AR/VR therapy platforms are necessary to detect biases, security vulnerabilities, and unintended consequences.
- 3.
- Accessibility and Digital Divide Considerations:
- ▪
- Ethical concerns also extend to fair access—ensuring AI-driven mental health interventions do not exacerbate disparities between technologically advantaged and disadvantaged populations.
- ▪
- Solutions such as affordable AR/VR hardware, low-bandwidth AI models, and multilingual support can enhance equitable access to digital cognitive therapies.
5.2. Future Directions and Emerging Trends
6. Conclusions
Supplementary Materials
Author Contributions
Funding
Conflicts of Interest
Abbreviations
| General and Technology-Related Terms | |
| AI | Artificial intelligence |
| AR | Augmented reality |
| CBT | Cognitive behavioral therapy |
| HMD | Head-Mounted Display |
| ML | Machine learning |
| MR | Mixed reality |
| NLP | Natural language processing |
| VR | Virtual reality |
| Medical and Psychological Terms | |
| ABI | Acquired brain injury |
| ADHD | Attention deficit hyperactivity disorder |
| AM | Autobiographical memory |
| AVH | Auditory verbal hallucinations |
| CBTp | Cognitive Behavioral Therapy for Psychosis |
| EEG | Electroencephalography |
| FMA | Fugl–Meyer Assessment |
| GD | Gambling disorder |
| MCI | Mild cognitive impairment |
| MDD | Major depressive disorder |
| MoCA | Montreal Cognitive Assessment |
| NIHSS | National Institutes of Health Stroke Scale |
| NSI | Neurobehavioral Symptom Inventory |
| PCL-C | PTSD Checklist—Civilian Version |
| PTSD | Post-traumatic stress disorder |
| QIDS-SR | Quick Inventory of Depressive Symptomatology—Self-Report |
| SAD | Social anxiety disorder |
| SUD | Substance use disorder |
| TAU | Treatment as usual |
| Machine Learning and Statistical Terms | |
| AUC | Area Under the Curve |
| ANN | Artificial neural network |
| CNN | Convolutional Neural Network |
| DL | Deep learning |
| FM | Full model |
| FM-UE | Fugl–Meyer Upper Extremity Assessment |
| LSTM | Long Short-Term Memory |
| MARL | Multi-Agent Reinforcement Learning |
| QEEG | Quantitative electroencephalography |
| RNN | Recurrent neural network |
| rTMS | Repetitive transcranial magnetic stimulation |
| RMSE | Root mean square error |
| RL | Reinforcement learning |
| SM | Simplified model |
| SVM | Support vector machine |
| Therapy and Research Methodology Terms | |
| ANAMs | Automated Neuropsychological Assessment Metrics |
| BOT-2 | Bruininks–Oseretsky Test of Motor Proficiency, Second Edition |
| CT | Critical thinking |
| DTVP-2 | Developmental Test of Visual Perception, Second Edition |
| FIM | Functional Independence Measure |
| IPQ | Presence Questionnaire |
| PRISMA | Preferred Reporting Items for Systematic Reviews and Meta-Analyses |
| RCT | Randomized controlled trial |
| TG | Task Generator |
| Virtual Reality Therapy and Rehabilitation | |
| BBVR | Brain-Based Virtual Reality Therapy |
| CB-VR | Cognitive Behavioral Virtual Reality Therapy |
| Reh@City | Virtual Reality-Based Rehabilitation System |
| VRCE | Virtual Reality Cue Exposure |
| VRGT | Virtual Reality Group Therapy |
References
- Georgiev, D.D.; Georgieva, I.; Gong, Z.; Nanjappan, V.; Georgiev, G.V. Virtual Reality for Neurorehabilitation and Cognitive Enhancement. Brain Sci. 2021, 11, 221. [Google Scholar] [CrossRef] [PubMed]
- Shukla, A.; Srivastava, A. Immersive Healing: Examining the Effectiveness of Cognitive Behavioral Therapy Using Virtual Reality to Reduce Cognitive Distortions. Augment. Hum. Res. 2024, 9, 2. [Google Scholar] [CrossRef]
- Gkintoni, E.; Skokou, M.; Gourzis, P. Integrating Clinical Neuropsychology and Psychotic Spectrum Disorders: A Systematic Analysis of Cognitive Dynamics, Interventions, and Underlying Mechanisms. Medicina 2024, 60, 645. [Google Scholar] [CrossRef]
- Carroll, J.; Hopper, L.; Farrelly, A.M.; Lombard-Vance, R.; Bamidis, P.D.; Konstantinidis, E.I. A Scoping Review of Augmented/Virtual Reality Health and Wellbeing Interventions for Older Adults: Redefining Immersive Virtual Reality. Front. Virtual Real. 2021, 2, 655338. [Google Scholar] [CrossRef]
- Nath, N.; Kalatzis, A.; Stanley, L. Measuring user engagement in virtual, augmented, and mixed reality interventions for stress reduction. In International Conference on Human-Computer Interaction; Springer Nature: Cham, Switzerland, 2023; pp. 570–583. [Google Scholar]
- Carlson, C.G. Virtual and Augmented Simulations in Mental Health. Curr. Psychiatry Rep. 2023, 25, 365–371. [Google Scholar] [CrossRef]
- Samuel, S. Immersive technologies in the healthcare space. In Augmented Intelligence in Healthcare: A Pragmatic and Integrated Analysis; Springer Nature: Singapore, 2022; pp. 433–451. [Google Scholar]
- Šlosar, L.; Voelcker-Rehage, C.; Paravlić, A.H.; Abazovic, E.; de Bruin, E.D.; Marusic, U. Combining physical and virtual worlds for motor-cognitive training interventions: Position paper with guidelines on technology classification in movement-related research. Front. Psychol. 2022, 13, 1009052. [Google Scholar] [CrossRef] [PubMed]
- Gkintoni, E.; Nikolaou, G. The Cross-Cultural Validation of Neuropsychological Assessments and Their Clinical Applications in Cognitive Behavioral Therapy: A Scoping Analysis. Int. J. Environ. Res. Public Health 2024, 21, 1110. [Google Scholar] [CrossRef]
- Lan, L.; Sikov, J.; Lejeune, J.; Ji, C.; Brown, H.; Bullock, K.; Spencer, A.E. A systematic review of using virtual and augmented reality for the diagnosis and treatment of psychotic disorders. Curr. Treat. Options Psychiatry 2023, 10, 87–107. [Google Scholar] [CrossRef]
- Li, W.; Liu, X.; Zhang, Q.; Zhou, B.; Wang, B. VR-Enhanced Cognitive Learning: Method, Framework, and Application. Appl. Sci. 2023, 13, 4756. [Google Scholar] [CrossRef]
- Tay, J.L.; Xie, H.; Sim, K. Effectiveness of Augmented and Virtual Reality-Based Interventions in Improving Knowledge, Attitudes, Empathy and Stigma Regarding People with Mental Illnesses—A Scoping Review. J. Pers. Med. 2023, 13, 112. [Google Scholar] [CrossRef]
- Gkintoni, E. Clinical neuropsychological characteristics of bipolar disorder, with a focus on cognitive and linguistic pattern: A conceptual analysis. F1000Research 2023, 12, 1235. [Google Scholar] [CrossRef] [PubMed]
- Qu, Z.; Lau, C.W.; Simoff, S.J.; Kennedy, P.J.; Nguyen, Q.V.; Catchpoole, D.R. Review of Innovative Immersive Technologies for Healthcare Applications. Innov. Digit. Health Diagn. Biomark. 2022, 2, 27–39. [Google Scholar] [CrossRef]
- De Luca, V.; Gatto, C.; Liaci, S.; Corchia, L.; Chiarello, S.; Faggiano, F.; Sumerano, G.; De Paolis, L.T. Virtual Reality and Spatial Augmented Reality for Social Inclusion: The “Includiamoci” Project. Information 2023, 14, 38. [Google Scholar] [CrossRef]
- Park, M.J.; Kim, D.J.; Lee, U.; Na, E.J.; Jeon, H.J. A literature overview of virtual reality (VR) in the treatment of psychiatric disorders: Recent advances and limitations. J. Med. Internet Res. 2019, 10, 505. [Google Scholar] [CrossRef] [PubMed]
- Gkintoni, E.; Vassilopoulos, S.P.; Nikolaou, G. Next-Generation Cognitive-Behavioral Therapy for Depression: Integrating Digital Tools, Teletherapy, and Personalization for Enhanced Mental Health Outcomes. Medicina 2025, 61, 431. [Google Scholar] [CrossRef]
- Higgins, O.; Short, B.L.; Chalup, S.K.; Wilson, R.L. Artificial intelligence (AI) and machine learning (ML) based decision support systems in mental health: An integrative review. Int. J. Ment. Health Nurs. 2023, 32, 966–978. [Google Scholar] [CrossRef]
- Graham, S.A.; Lee, E.E.; Jeste, D.V.; Van Patten, R.; Twamley, E.W.; Nebeker, C.; Yamada, Y.; Kim, H.-C.; Depp, C.A. Artificial intelligence approaches to predicting and detecting cognitive decline in older adults: A conceptual review. Psychiatry Res. 2020, 284, 112732. [Google Scholar] [CrossRef]
- Milne-Ives, M.; Selby, E.; Inkster, B.; Lam, C.; Meinert, E. Artificial intelligence and machine learning in mobile apps for mental health: A scoping review. PLoS Digit. Health 2022, 1, e0000079. [Google Scholar] [CrossRef]
- Zhou, S.; Zhao, J.; Zhang, L. Application of Artificial Intelligence on Psychological Interventions and Diagnosis: An Overview. Front. Psychiatry 2022, 13, 811665. [Google Scholar] [CrossRef]
- Lin, E.; Lin, C.H.; Lane, H.Y. Precision psychiatry applications with pharmacogenomics: Artificial intelligence and machine learning approaches. Int. J. Mol. Sci. 2020, 21, 969. [Google Scholar] [CrossRef]
- Gkintoni, E.; Antonopoulou, H.; Sortwell, A.; Halkiopoulos, C. Challenging Cognitive Load Theory: The Role of Educational Neuroscience and Artificial Intelligence in Redefining Learning Efficacy. Brain Sci. 2025, 15, 203. [Google Scholar] [CrossRef] [PubMed]
- Olawade, D.B.; Wada, O.Z.; Odetayo, A.; David-Olawade, A.C.; Asaolu, F.; Eberhardt, J. Enhancing mental health with Artificial Intelligence: Current trends and future prospects. J. Med. Surg. Public Health 2024, 3, 100099. [Google Scholar] [CrossRef]
- Lee, E.E.; Torous, J.; De Choudhury, M.; Depp, C.A.; Graham, S.A.; Kim, H.C.; Paulus, M.P.; Krystal, J.H.; Jeste, D.V. Arti-ficial intelligence for mental health care: Clinical applications, barriers, facilitators, and artificial wisdom. Biol. Psychiatry Cogn. Neurosci. Neuroimaging 2021, 6, 856–864. [Google Scholar] [CrossRef] [PubMed]
- Bisso, E.; Signorelli, M.S.; Milazzo, M.; Maglia, M.; Polosa, R.; Aguglia, E.; Caponnetto, P. Immersive Virtual Reality Applications in Schizophrenia Spectrum Therapy: A Systematic Review. Int. J. Environ. Res. Public Health 2020, 17, 6111. [Google Scholar] [CrossRef]
- Janiesch, C.; Zschech, P.; Heinrich, K. Machine learning and deep learning. Electron. Mark. 2021, 31, 685–695. [Google Scholar] [CrossRef]
- Punia, A.; Bhakuni, P.; Sharma, N. Development of AI-and NLP-Driven Chatbots and Virtual Assistants for Mental Health Support. In Transforming Neuropsychology and Cognitive Psychology with AI and Machine Learning; IGI Global Scientific Publishing: Pennsylvania, PA, USA, 2025; pp. 229–262. [Google Scholar] [CrossRef]
- Taiwo, O.; Al-Bander, B. Emotion-aware psychological first aid: Integrating BERT-based emotional distress detection with Psychological First Aid-Generative Pre-Trained Transformer chatbot for mental health support. Cogn. Comput. Syst. 2025, 7, e12116. [Google Scholar] [CrossRef]
- Rudnicka, Z.; Proniewska, K.; Perkins, M.; Pregowska, A. Cardiac Healthcare Digital Twins Supported by Artificial Intelligence-Based Algorithms and Extended Reality—A Systematic Review. Electronics 2024, 13, 866. [Google Scholar] [CrossRef]
- Khalaf, O.I.; Srinivasan, D.; Algburi, S.; Vellaichamy, J.; Selvaraj, D.; Sharif, M.S.; Elmedany, W. Elevating metaverse virtual reality experiences through network-integrated neuro-fuzzy emotion recognition and adaptive content generation algorithms. Eng. Rep. 2024, 6, e12894. [Google Scholar] [CrossRef]
- Naithani, K.; Raiwani, Y.P.; Tiwari, S.; Chauhan, A.S. Artificial Intelligence Techniques Based on Federated Learning in Smart Healthcare. In Federated Learning for Smart Communication Using IoT Application; Chapman and Hall/CRC: Boca Raton, FL, USA, 2024; pp. 81–108. [Google Scholar] [CrossRef]
- Mittal, H. Virtual Reality Applications in Healthcare. In Immersive Virtual and Augmented Reality in Healthcare; CRC Press: Boca Raton, FL, USA, 2023; pp. 50–62. [Google Scholar] [CrossRef]
- Vatansever, S.; Schlessinger, A.; Wacker, D.; Kaniskan, H.Ü.; Jin, J.; Zhou, M.; Zhang, B. Artificial intelligence and machine learning-aided drug discovery in central nervous system diseases: State-of-the-arts and future directions. Med. Res. Rev. 2021, 41, 1427–1473. [Google Scholar] [CrossRef]
- Kastoris, D.; Giotopoulos, K.; Papadopoulos, D. Neural Network-Based Parameter Estimation in Dynamical Systems. Information 2024, 15, 809. [Google Scholar] [CrossRef]
- Sarker, I.H. AI-Based Modeling: Techniques, Applications and Research Issues Towards Automation, Intelligent and Smart Systems. SN Comput. Sci. 2022, 3, 158. [Google Scholar] [CrossRef]
- Meena, T.; Roy, S. Bone Fracture Detection Using Deep Supervised Learning from Radiological Images: A Paradigm Shift. Diagnostics 2022, 12, 2420. [Google Scholar] [CrossRef] [PubMed]
- Zhou, Z.H.; Zhou, Z.H. Semi-supervised learning. Mach. Learn. 2021, 315–341. [Google Scholar] [CrossRef]
- Bao, Y.; Li, H. Machine learning paradigm for structural health monitoring. Struct. Health Monit. 2020, 20, 1353–1372. [Google Scholar] [CrossRef]
- Van Engelen, J.E.; Hoos, H.H. A survey on semi-supervised learning. Mach. Learn. 2020, 109, 373–440. [Google Scholar] [CrossRef]
- Zhang, L.; Wen, J.; Li, Y.; Chen, J.; Ye, Y.; Fu, Y.; Livingood, W. A review of machine learning in building load prediction. Appl. Energy 2021, 285, 116452. [Google Scholar] [CrossRef]
- Waring, J.; Lindvall, C.; Umeton, R. Automated machine learning: Review of the state-of-the-art and opportunities for healthcare. Artif. Intell. Med. 2020, 104, 101822. [Google Scholar] [CrossRef]
- Khalil, M.; McGough, A.S.; Pourmirza, Z.; Pazhoohesh, M.; Walker, S. Machine Learning, Deep Learning and Statistical Analysis for forecasting building energy consumption—A systematic review. Eng. Appl. Artif. Intell. 2022, 115, 105287. [Google Scholar] [CrossRef]
- Chauhan, K.; Jani, S.; Thakkar, D.; Dave, R.; Bhatia, J.; Tanwar, S.; Obaidat, M.S. Automated machine learning: The new wave of machine learning. In Proceedings of the 2020 2nd International Conference on Innovative Mechanisms for Industry Applications (ICIMIA), Bangalore, India, 5–7 March 2020; IEEE: Bangalore, India, 2020; pp. 327–334. [Google Scholar]
- Himeur, Y.; Elnour, M.; Fadli, F.; Meskin, N.; Petri, I.; Rezgui, Y.; Bensaali, F.; Amira, A. AI-big data analytics for building automation and management systems: A survey, actual challenges and future perspectives. Artif. Intell. Rev. 2022, 56, 4929–5021. [Google Scholar] [CrossRef]
- Halkiopoulos, C.; Gkintoni, E. Leveraging AI in E-Learning: Personalized Learning and Adaptive Assessment through Cognitive Neuropsychology—A Systematic Analysis. Electronics 2024, 13, 3762. [Google Scholar] [CrossRef]
- Wang, Z.; Hong, T.; Piette, M.A. Building thermal load prediction through shallow machine learning and deep learning. Appl. Energy 2020, 263, 114683. [Google Scholar] [CrossRef]
- Pham, B.T.; Luu, C.; Van Phong, T.; Trinh, P.T.; Shirzadi, A.; Renoud, S.; Asadi, S.; Van Le, H.; von Meding, J.; Clague, J.J. Can deep learning algorithms outperform benchmark machine learning algorithms in flood susceptibility modeling? J. Hydrol. 2021, 592, 125615. [Google Scholar] [CrossRef]
- Bui, D.T.; Tsangaratos, P.; Nguyen, V.-T.; Van Liem, N.; Trinh, P.T. Comparing the prediction performance of a Deep Learning Neural Network model with conventional machine learning models in landslide susceptibility assessment. Catena 2020, 188, 104426. [Google Scholar] [CrossRef]
- Theodorakopoulos, L.; Theodoropoulou, A.; Stamatiou, Y. A State-of-the-Art Review in Big Data Management Engineering: Real-Life Case Studies, Challenges, and Future Research Directions. Eng 2024, 5, 1266–1297. [Google Scholar] [CrossRef]
- Tiwari, A. Supervised learning: From theory to applications. In Artificial Intelligence and Machine Learning for EDGE Computing; Academic Press: Cambridge, MA, USA, 2022; pp. 23–32. [Google Scholar]
- Gomes, H.M.; Grzenda, M.; Mello, R.; Read, J.; Le Nguyen, M.H.; Bifet, A. A Survey on Semi-supervised Learning for Delayed Partially Labelled Data Streams. ACM Comput. Surv. 2022, 55, 1–42. [Google Scholar] [CrossRef]
- El Mrabet, M.A.; El Makkaoui, K.; Faize, A. Supervised machine learning: A survey. In Proceedings of the 2021 4th International Conference on Advanced Communication Technologies and Networking (CommNet), Rabat, Morocco, 3–5 December 2021; IEEE: Rabat, Morocco, 2021; pp. 1–10. [Google Scholar]
- Raikar, M.M.; Meena, S.M.; Mulla, M.M.; Shetti, N.S.; Karanandi, M. Data traffic classification in software defined networks (SDN) using supervised-learning. Procedia Comput. Sci. 2020, 171, 2740–2749. [Google Scholar] [CrossRef]
- Theodorakopoulos, L.; Karras, A.; Theodoropoulou, A.; Kampiotis, G. Benchmarking Big Data Systems: Performance and Decision-Making Implications in Emerging Technologies. Technologies 2024, 12, 217. [Google Scholar] [CrossRef]
- Hiran, K.K.; Jain, R.K.; Lakhwani, K.; Doshi, R. Machine learning: Master supervised and unsupervised learning algorithms with real examples. Int. J. Intell. Syst. Appl. 2021, 13, 72–79. [Google Scholar]
- Theodorakopoulos, L.; Karras, A.; Krimpas, G.A. Optimizing Apache Spark MLlib: Predictive Performance of Large-Scale Models for Big Data Analytics. Algorithms 2025, 18, 74. [Google Scholar] [CrossRef]
- Katsouda, M.; Kollias, K.; Halkiopoulos, C.; Boutsinas, B. Mining Association of Outliers in Time Series. In Proceedings of the International Conference of the International Association of Cultural and Digital Tourism, Mohali, India, 14–16 March 2024; Springer Proceedings in Business and Economics: Cham, Switzerland, 2024; pp. 433–444. [Google Scholar] [CrossRef]
- Ebrahimi, P.; Basirat, M.; Yousefi, A.; Nekmahmud, M.; Gholampour, A.; Fekete-Farkas, M. Social Networks Marketing and Consumer Purchase Behavior: The Combination of SEM and Unsupervised Machine Learning Approaches. Big Data Cogn. Comput. 2022, 6, 35. [Google Scholar] [CrossRef]
- Vlachou, E.; Karras, A.; Karras, C.; Theodorakopoulos, L.; Halkiopoulos, C.; Sioutas, S. Distributed Bayesian Inference for Large-Scale IoT Systems. Big Data Cogn. Comput. 2023, 8, 1. [Google Scholar] [CrossRef]
- Li, W.; Meng, W.; Au, M.H. Enhancing collaborative intrusion detection via disagreement-based semi-supervised learning in IoT environments. J. Netw. Comput. Appl. 2020, 161, 102631. [Google Scholar] [CrossRef]
- Madhuri, A.; Jyothi, V.E.; Praveen, S.P.; Sindhura, S.; Srinivas, V.S.; Kumar, D.L.S. A New Multi-Level Semi-Supervised Learning Approach for Network Intrusion Detection System Based on the ‘GOA’. J. Interconnect. Netw. 2022, 24, 2143047. [Google Scholar] [CrossRef]
- Zhang, T.; Zhu, T.; Li, J.; Han, M.; Zhou, W.; Yu, P.S. Fairness in Semi-Supervised Learning: Unlabeled Data Help to Reduce Discrimination. IEEE Trans. Knowl. Data Eng. 2020, 34, 1763–1774. [Google Scholar] [CrossRef]
- Karras, C.; Theodorakopoulos, L.; Karras, A.; Krimpas, G.A. Efficient Algorithms for Range Mode Queries in the Big Data Era. Information 2024, 15, 450. [Google Scholar] [CrossRef]
- Eckstein, M.K.; Wilbrecht, L.; Collins, A.G. What do reinforcement learning models measure? Interpreting model parameters in cognition and neuroscience. Curr. Opin. Behav. Sci. 2021, 41, 128–137. [Google Scholar] [CrossRef]
- Shuvaev, S.A.; Tran, N.B.; Stephenson-Jones, M.; Li, B.; Koulakov, A.A. Neural Networks with Motivation. Front. Syst. Neurosci. 2021, 14, 609316. [Google Scholar] [CrossRef]
- Sugiyama, T.; Schweighofer, N.; Izawa, J. Reinforcement learning establishes a minimal metacog-nitive process to monitor and control motor learning performance. Nat. Commun. 2023, 14, 3352. [Google Scholar] [CrossRef]
- Anwar, H.; Caby, S.; Dura-Bernal, S.; D’onofrio, D.; Hasegan, D.; Deible, M.; Grunblatt, S.; Chadderdon, G.L.; Kerr, C.C.; Lakatos, P.; et al. Training a spiking neuronal network model of visual-motor cortex to play a virtual racket-ball game using reinforcement learning. PLoS ONE 2022, 17, e0265808. [Google Scholar] [CrossRef]
- Véronneau-Veilleux, F.; Robaey, P.; Ursino, M.; Nekka, F. A mechanistic model of ADHD as resulting from dopamine phasic/tonic imbalance during reinforcement learning. Front. Comput. Neurosci. 2022, 16, 849323. [Google Scholar] [CrossRef]
- Bălan, O.; Moldoveanu, A.; Leordeanu, M. A machine learning approach to automatic phobia therapy with virtual reality. In Modern Approaches to Augmentation of Brain Function; Springer: Berlin/Heidelberg, Germany, 2021; pp. 607–636. [Google Scholar]
- Lindner, P. Better, Virtually: The Past, Present, and Future of Virtual Reality Cognitive Behavior Therapy. Int. J. Cogn. Ther. 2020, 14, 23–46. [Google Scholar] [CrossRef]
- Torous, J.; Bucci, S.; Bell, I.H.; Kessing, L.V.; Faurholt-Jepsen, M.; Whelan, P.; Carvalho, A.F.; Keshavan, M.; Linardon, J.; Firth, J. The growing field of digital psychiatry: Current evidence and the future of apps, social media, chatbots, and virtual reality. World Psychiatry 2021, 20, 318–335. [Google Scholar] [CrossRef]
- Bălan, O.; Moise, G.; Moldoveanu, A.; Leordeanu, M.; Moldoveanu, F. An Investigation of Various Machine and Deep Learning Techniques Applied in Automatic Fear Level Detection and Acrophobia Virtual Therapy. Sensors 2020, 20, 496. [Google Scholar] [CrossRef] [PubMed]
- Jung, D.; Kim, D.I.; Kim, N. Bringing nature into hospital architecture: Machine learning-based EEG analysis of the biophilia effect in virtual reality. J. Environ. Psychol. 2023, 89, 102033. [Google Scholar] [CrossRef]
- Rahman, M.A.; Brown, D.J.; Mahmud, M.; Harris, M.; Shopland, N.; Heym, N.; Sumich, A.; Turabee, Z.B.; Standen, B.; Downes, D.; et al. Enhancing biofeedback-driven self-guided virtual reality exposure therapy through arousal detection from multimodal data using machine learning. Brain Inform. 2023, 10, 14. [Google Scholar] [CrossRef] [PubMed]
- Kritikos, J.; Alevizopoulos, G.; Koutsouris, D. Personalized Virtual Reality Human-Computer Interaction for Psychiatric and Neurological Illnesses: A Dynamically Adaptive Virtual Reality Environment That Changes According to Real-Time Feedback From Electrophysiological Signal Responses. Front. Hum. Neurosci. 2021, 15, 596980. [Google Scholar] [CrossRef]
- Komatsu, H.; Watanabe, E.; Fukuchi, M. Psychiatric neural networks and precision therapeutics by machine learning. Biomedicines 2021, 9, 403. [Google Scholar] [CrossRef]
- Chekroud, A.M.; Bondar, J.; Delgadillo, J.; Doherty, G.; Wasil, A.; Fokkema, M.; Cohen, Z.; Belgrave, D.; DeRubeis, R.; Iniesta, R.; et al. The promise of machine learning in predicting treatment outcomes in psychiatry. World Psychiatry 2021, 20, 154–170. [Google Scholar] [CrossRef]
- Schwartz, B.; Cohen, Z.D.; Rubel, J.A.; Zimmermann, D.; Wittmann, W.W.; Lutz, W. Personalized treatment selection in routine care: Integrating machine learning and statistical algorithms to recommend cognitive behavioral or psychodynamic therapy. Psychother. Res. 2021, 31, 33–51. [Google Scholar] [CrossRef]
- Injadat, M.; Moubayed, A.; Nassif, A.B.; Shami, A. Machine learning towards intelligent systems: Applications, challenges, and opportunities. Artif. Intell. Rev. 2021, 54, 3299–3348. [Google Scholar] [CrossRef]
- Ryum, T.; Kazantzis, N. Elucidating the process-based emphasis in cognitive behavioral therapy. J. Context. Behav. Sci. 2024, 33, 100819. [Google Scholar] [CrossRef]
- Blackwell, S.E.; Heidenreich, T. Cognitive Behavior Therapy at the Crossroads. Int. J. Cogn. Ther. 2021, 14, 1–22. [Google Scholar] [CrossRef] [PubMed]
- Romanowska, M.; Dobroczyński, B. The unconscious in a new guise: Latent processes in two theories of the third wave of cognitive behavioral therapy. Theory Psychol. 2021, 31, 867–886. [Google Scholar] [CrossRef]
- Gkintoni, E.; Vassilopoulos, S.P.; Nikolaou, G. Mindfulness-Based Cognitive Therapy in Clinical Practice: A Systematic Review of Neurocognitive Outcomes and Applications for Mental Health and Well-Being. J. Clin. Med. 2025, 14, 1703. [Google Scholar] [CrossRef]
- Khan, S. Augmented and virtual reality-based interventions for learning disabilities: Current practices and future prospects. In Handbook on Augmenting Telehealth Services; CRC Press: Boca Raton, FL, USA, 2024. [Google Scholar] [CrossRef]
- Szabó, P.; Ara, J.; Halmosi, B.; Sik-Lanyi, C.; Guzsvinecz, T. Technologies designed to assist indi-viduals with cognitive impairments. Sustainability 2023, 15, 13490. [Google Scholar] [CrossRef]
- Calderon-Sastre, E.; Renganathan, G.; Palani, P.; Ramasamy, P.; Kurita, Y.; Ćuković, S. Accelerating rehabilitation through AR/VR solutions. In Smart VR/AR/MR Systems for Professionals; CRC Press: Boca Raton, FL, USA, 2024; pp. 137–166. [Google Scholar] [CrossRef]
- Wilson, J.C.; Nair, S.; Scielzo, S.; Larson, E.C. Objective measures of cognitive load using deep multi-modal learning: A use-case in aviation. Proc. ACM Interact. Mob. Wearable Ubiquitous Technol. 2021, 5, 1–35. [Google Scholar] [CrossRef]
- Bermejo, C.; Lee, L.H.; Chojecki, P.; Przewozny, D.; Hui, P. Exploring Button Designs for Mid-air Interaction in Virtual Reality: A Hexa-metric Evaluation of Key Representations and Multi-modal Cues. Proc. ACM Hum.-Comput. Interact. 2021, 5, 1–26. [Google Scholar] [CrossRef]
- Chandrashekar, N.D. [DC] Understanding the Impact of the Fidelity of Multimodal Interactions in XR based Training Simulators on Cognitive Load. In Proceedings of the 2024 IEEE Conference on Virtual Reality and 3D User Interfaces Abstracts and Workshops (VRW), Orlando, FL, USA, 16–21 March 2024; IEEE: Orlando, FL, USA, 2024; pp. 1116–1117. [Google Scholar]
- Xin, X.; Wang, Y.; Xiang, G.; Yang, W.; Liu, W. Effectiveness of multimodal display in navigation situations. In Proceedings of the Ninth International Symposium of Chinese CHI, Online Event, 16–17 October 2021; pp. 50–62. [Google Scholar]
- Rizzo, A.; Ermini, S.; Zanca, D.; Bernabini, D.; Rossi, A. A Machine Learning Approach for Detecting Cognitive Interference Based on Eye-Tracking Data. Front. Hum. Neurosci. 2022, 16, 806330. [Google Scholar] [CrossRef]
- Greener, J.G.; Kandathil, S.M.; Moffat, L.; Jones, D.T. A guide to machine learning for biologists. Nat. Rev. Mol. Cell Biol. 2021, 23, 40–55. [Google Scholar] [CrossRef]
- Mahmud, M.; Kaiser, M.S.; McGinnity, T.M.; Hussain, A. Deep Learning in Mining Biological Data. Cogn. Comput. 2021, 13, 1–33. [Google Scholar] [CrossRef]
- Reel, P.S.; Reel, S.; Pearson, E.; Trucco, E.; Jefferson, E. Using machine learning approaches for multi-omics data analysis: A review. Biotechnol. Adv. 2021, 49, 107739. [Google Scholar] [CrossRef] [PubMed]
- Lopatkin, A.J.; Collins, J.J. Predictive biology: Modelling, understanding and harnessing microbial complexity. Nat. Rev. Microbiol. 2020, 18, 507–520. [Google Scholar] [CrossRef] [PubMed]
- Muzio, G.; O’Bray, L.; Borgwardt, K. Biological network analysis with deep learning. Brief. Bioinform. 2021, 22, 1515–1530. [Google Scholar] [CrossRef]
- Cipresso, P.; Giglioli, I.A.C.; Raya, M.A.; Riva, G. The Past, Present, and Future of Virtual and Augmented Reality Research: A Network and Cluster Analysis of the Literature. Front. Psychol. 2018, 9, 2086. [Google Scholar] [CrossRef]
- Haddaway, N.R.; Page, M.J.; Pritchard, C.C.; McGuinness, L.A. PRISMA2020: An R package and Shiny app for producing PRISMA 2020-compliant flow diagrams, with interactivity for optimised digital transparency and Open Synthesis. Campbell Syst. Rev. 2022, 18, e1230. [Google Scholar] [CrossRef] [PubMed]
- Van den Akker, O.R.; Peters, G.Y.; Bakker, C.; Carlsson, R.; Coles, N.A.; Corker, K.S.; Feldman, G.; Moreau, D.; Nordström, T.; Pickering, J.S.; et al. Increasing the transparency of systematic reviews: Presenting a generalized registration form. Syst. Rev. 2023, 12, 170. [Google Scholar] [CrossRef] [PubMed]
- Ahn, S. Combined Effects of Virtual Reality and Computer Game-Based Cognitive Therapy on the Development of Visual-Motor Integration in Children with Intellectual Disabilities: A Pilot Study. Occup. Ther. Int. 2021, 2021, 1–8. [Google Scholar] [CrossRef]
- Albizu, A.; Fang, R.; Indahlastari, A.; O’shea, A.; Stolte, S.E.; See, K.B.; Boutzoukas, E.M.; Kraft, J.N.; Nissim, N.R.; Woods, A.J. Machine learning and individual variability in electric field characteristics predict tDCS treatment response. Brain Stimul. 2020, 13, 1753–1764. [Google Scholar] [CrossRef]
- Alkhabra, Y.A.; Ibrahem, U.M.; Alkhabra, S.A. Augmented reality technology in enhancing learning retention and critical thinking according to STEAM program. Humanit. Soc. Sci. Commun. 2023, 10, 1–10. [Google Scholar] [CrossRef]
- Allcoat, D.; von Mühlenen, A. Learning in virtual reality: Effects on performance, emotion and engagement. Res. Learn. Technol. 2018, 26. [Google Scholar] [CrossRef]
- Alsem, S.C.; van Dijk, A.; Verhulp, E.E.; Dekkers, T.J.; de Castro, B.O. Treating children’s aggressive behavior problems using cognitive behavior therapy with virtual reality: A multicenter randomized controlled trial. Child Dev. 2023, 94, E344–E361. [Google Scholar] [CrossRef]
- Alwashmi, K.; Meyer, G.; Rowe, F.; Ward, R. Enhancing learning outcomes through multisensory integration: A fMRI study of audio-visual training in virtual reality. NeuroImage 2023, 285, 120483. [Google Scholar] [CrossRef] [PubMed]
- Andersen, S.A.W.; Konge, L.; Sørensen, M.S. The effect of distributed virtual reality simulation training on cognitive load during subsequent dissection training. Med. Teach. 2018, 40, 684–689. [Google Scholar] [CrossRef] [PubMed]
- Aran, O.T.; Şahin, S.; Köse, B.; Ağce, Z.B.; Kayihan, H. Effectiveness of the virtual reality on cognitive function of children with hemiplegic cerebral palsy: A single-blind randomized controlled trial. Int. J. Rehabil. Res. 2020, 43, 12–19. [Google Scholar] [CrossRef]
- Arquissandas, P.; Lamas, D.R.; Oliveira, J. Moving from VR into AR using bio-cybernetic loops and physiological sensory devices for intervention on anxiety disorders. Virtual Real. 2021, 27, 233–243. [Google Scholar] [CrossRef]
- Aziz, F.A.; Alsaeed, A.S.; Sulaiman, S.; Ariffin, M.K.A.M.; Al-Hakim, M.F. Mixed Reality Improves Education and Training in Assembly Processes. J. Eng. Technol. Sci. 2020, 52, 598. [Google Scholar] [CrossRef]
- Bond, J.; Kenny, A.; Pinfold, V.; Couperthwaite, L.; Kabir, T.; Larkin, M.; Beckley, A.; Rosebrock, L.; Lambe, S.; Freeman, D.; et al. A Safe Place to Learn: Peer Research Qualitative Investigation of gameChange Virtual Reality Therapy. JMIR Serious Games 2023, 11, e38065. [Google Scholar] [CrossRef]
- Bouchard, S.; Robillard, G.; Giroux, I.; Jacques, C.; Loranger, C.; St-Pierre, M.; Chrétien, M.; Goulet, A. Using Virtual Reality in the Treatment of Gambling Disorder: The Development of a New Tool for Cognitive Behavior Therapy. Front. Psychiatry 2017, 8, 27. [Google Scholar] [CrossRef]
- Bruschetta, R.; Maggio, M.G.; Naro, A.; Ciancarelli, I.; Morone, G.; Arcuri, F.; Tonin, P.; Tartarisco, G.; Pioggia, G.; Cerasa, A.; et al. Gender Influences Virtual Reality-Based Recovery of Cognitive Functions in Patients with Traumatic Brain Injury: A Secondary Analysis of a Randomized Clinical Trial. Brain Sci. 2022, 12, 491. [Google Scholar] [CrossRef]
- Buccellato, K.H.; Nordstrom, M.; Murphy, J.M.; Burdea, G.C.; Polistico, K.; House, G.; Kim, N.; Grampurohit, N.; Sorensen, J.; Isaacson, B.M.; et al. A Randomized Feasibility Trial of a Novel, Integrative, and Intensive Virtual Rehabilitation Program for Service Members Post-Acquired Brain Injury. Mil. Med. 2019, 185, E203–E211. [Google Scholar] [CrossRef]
- Butti, N.; Biffi, E.; Genova, C.; Romaniello, R.; Redaelli, D.F.; Reni, G.; Borgatti, R.; Urgesi, C. Virtual Reality Social Prediction Improvement and Rehabilitation Intensive Training (VR-SPIRIT) for paediatric patients with congenital cerebellar diseases: Study protocol of a randomised controlled trial. Trials 2019, 21, 1–12. [Google Scholar] [CrossRef] [PubMed]
- Câmara, J.; Ferreira, R.; Teixeira, L.; Nóbrega, J.; Romeira, C.; i Badia, S.B.; Faria, A.L. Efficacy of adaptive cognitive training through desktop virtual reality and paper-and-pencil in the treatment of mental and behavioral disorders. Virtual Real. 2021, 27, 291–306. [Google Scholar] [CrossRef]
- Chen, L.; Chen, Y.; Bin Fu, W.; Huang, D.F.; Lo, W.L.A. The Effect of Virtual Reality on Motor Anticipation and Hand Function in Patients with Subacute Stroke: A Randomized Trial on Movement-Related Potential. Neural Plast. 2020, 2022, 1–14. [Google Scholar] [CrossRef]
- Chen, X.J.; Wang, D.M.; Zhou, L.D.; Winkler, M.; Pauli, P.; Sui, N.; Li, Y.H. Mindfulness-based relapse prevention combined with virtual reality cue exposure for methamphetamine use disorder: Study protocol for a randomized controlled trial. Contemp. Clin. Trials 2018, 70, 99–105. [Google Scholar] [CrossRef] [PubMed]
- Cheng, T.-C.; Huang, S.-F.; Wu, S.-Y.; Lin, F.-G.; Lin, W.-S.; Tsai, P.-Y. Integration of Virtual Reality into Transcranial Magnetic Stimulation Improves Cognitive Function in Patients with Parkinson’s Disease with Cognitive Impairment: A Proof-of-Concept Study. J. Park. Dis. 2021, 12, 723–736. [Google Scholar] [CrossRef]
- Choi, D.; Seo, S.; Park, H.; Hong, T.; Koo, C. Forecasting personal learning performance in virtual reality-based construction safety training using biometric responses. Autom. Constr. 2023, 156, 105115. [Google Scholar] [CrossRef]
- Chun, J.Y.; Kim, H.-J.; Hur, J.-W.; Jung, D.; Lee, H.-J.; Pack, S.P.; Lee, S.; Kim, G.; Cho, C.-Y.; Lee, S.-M.; et al. Prediction of Specific Anxiety Symptoms and Virtual Reality Sickness Using In Situ Autonomic Physiological Signals During Virtual Reality Treatment in Patients with Social Anxiety Disorder: Mixed Methods Study. JMIR Serious Games 2022, 10, e38284. [Google Scholar] [CrossRef]
- Collaço, E.; Kira, E.; Sallaberry, L.H.; Queiroz, A.C.M.; Machado, M.A.A.M.; Jr, O.C.; Tori, R. Immersion and haptic feedback impacts on dental anesthesia technical skills virtual reality training. J. Dent. Educ. 2020, 85, 589–598. [Google Scholar] [CrossRef]
- D’Alfonso, S.; Santesteban-Echarri, O.; Rice, S.; Wadley, G.; Lederman, R.; Miles, C.; Gleeson, J.; Alvarez-Jimenez, M. Artificial Intelligence-Assisted Online Social Therapy for Youth Mental Health. Front. Psychol. 2017, 8, 796. [Google Scholar] [CrossRef]
- Dahdah, M.N.; Bennett, M.; Prajapati, P.; Parsons, T.D.; Sullivan, E.; Driver, S. Application of virtual environments in a multi-disciplinary day neurorehabilitation program to improve executive functioning using the Stroop task. Neurorehabilitation 2017, 41, 721–734. [Google Scholar] [CrossRef]
- Dellazizzo, L.; Potvin, S.; Phraxayavong, K.; Dumais, A. Exploring the Benefits of Virtual Reality-Assisted Therapy Following Cognitive-Behavioral Therapy for Auditory Hallucinations in Patients with Treatment-Resistant Schizophrenia: A Proof of Concept. J. Clin. Med. 2020, 9, 3169. [Google Scholar] [CrossRef]
- Dercon, Q.; Mehrhof, S.Z.; Sandhu, T.R.; Hitchcock, C.; Lawson, R.P.; Pizzagalli, D.A.; Dalgleish, T.; Nord, C.L. A core component of psychological therapy causes adaptive changes in computational learning mechanisms. Psychol. Med. 2023, 54, 327–337. [Google Scholar] [CrossRef]
- Dilgul, M.; Hickling, L.M.; Antonie, D.; Priebe, S.; Bird, V.J. Virtual Reality Group Therapy for the Treatment of Depression: A Qualitative Study on Stakeholder Perspectives. Front. Virtual Real. 2021, 1, 609545. [Google Scholar] [CrossRef]
- Donker, T.; Fehribach, J.; van Klaveren, C.; Cornelisz, I.; Toffolo, M.B.J.; van Straten, A.; van Gelder, J.-L. Automated mobile virtual reality cognitive behavior therapy for aviophobia in a natural setting: A randomized controlled trial. Psychol. Med. 2022, 53, 6232–6241. [Google Scholar] [CrossRef]
- Donker, T.; van Klaveren, C.; Cornelisz, I.; Kok, R.N.; van Gelder, J.-L. Analysis of Usage Data from a Self-Guided App-Based Virtual Reality Cognitive Behavior Therapy for Acrophobia: A Randomized Controlled Trial. J. Clin. Med. 2020, 9, 1614. [Google Scholar] [CrossRef]
- Duhne, P.G.S.; Delgadillo, J.; Lutz, W. Predicting early dropout in online versus face-to-face guided self-help: A machine learning approach. Behav. Res. Ther. 2022, 159, 104200. [Google Scholar] [CrossRef] [PubMed]
- Ekstrand, C.; Jamal, A.; Nguyen, R.; Kudryk, A.; Mann, J.; Mendez, I. Immersive and interactive virtual reality to improve learning and retention of neuroanatomy in medical students: A randomized controlled study. CMAJ Open 2018, 6, E103–E109. [Google Scholar] [CrossRef] [PubMed]
- Erguzel, T.; Tarhan, N. Machine Learning Approaches to Predict Repetitive Transcranial Magnetic Stimulation Treatment Response in Major Depressive Disorder. In Proceedings of the SAI Intelligent Systems Conference, London, UK, 21–22 September 2016. [Google Scholar] [CrossRef]
- Faria, A.L.; Cameirão, M.S.; Couras, J.F.; Aguiar, J.R.O.; Costa, G.M.; i Badia, S.B. Combined Cognitive-Motor Rehabilitation in Virtual Reality Improves Motor Outcomes in Chronic Stroke—A Pilot Study. Front. Psychol. 2018, 9, 854. [Google Scholar] [CrossRef]
- Faria, A.L.; Pinho, M.S.; i Badia, S.B. A comparison of two personalization and adaptive cognitive rehabilitation approaches: A randomized controlled trial with chronic stroke patients. J. Neuroeng. Rehabil. 2020, 17, 1–15. [Google Scholar] [CrossRef] [PubMed]
- Faria, A.L.; Andrade, A.; Soares, L.; i Badia, S.B. Benefits of virtual reality based cognitive rehabilitation through simulated activities of daily living: A randomized controlled trial with stroke patients. J. Neuroeng. Rehabil. 2016, 13, 1–12. [Google Scholar] [CrossRef]
- Fernandez-Alvarez, J.; Colombo, D.; Suso-Ribera, C.; Chirico, A.; Serino, S.; Di Lernia, D.; Palacios, A.G.; Riva, G.; Botella, C. Using virtual reality to target positive autobiographical memory in individuals with moderate-to-moderately severe depressive symptoms: A single case experimental design. Internet Interv. 2021, 25, 100407. [Google Scholar] [CrossRef] [PubMed]
- Freeman, D.; Yu, L.-M.; Kabir, T.; Martin, J.; Craven, M.; Leal, J.; Lambe, S.; Brown, S.; Morrison, A.; Chapman, K.; et al. Automated virtual reality (VR) cognitive therapy for patients with psychosis: Study protocol for a single-blind parallel group randomised controlled trial (gameChange). BMJ Open 2019, 9, e031606. [Google Scholar] [CrossRef] [PubMed]
- Freeman, D.; Freeman, J.; Ahmed, M.; Haynes, P.; Beckwith, H.; Rovira, A.; Miguel, A.L.; Ward, R.; Bousfield, M.; Riffiod, L.; et al. Automated VR therapy for improving positive self-beliefs and psychological well-being in young patients with psychosis: A proof of concept evaluation of Phoenix VR self-confidence therapy. Behav. Cogn. Psychother. 2023, 52, 277–287. [Google Scholar] [CrossRef]
- Frewen, P.; Mistry, D.; Zhu, J.; Kielt, T.; Wekerle, C.; Lanius, R.A.; Jetly, R. Proof of Concept of an Eclectic, Integrative Therapeutic Approach to Mental Health and Well-Being Through Virtual Reality Technology. Front. Psychol. 2020, 11, 858. [Google Scholar] [CrossRef]
- Fusco, A.; Giovannini, S.; Castelli, L.; Coraci, D.; Gatto, D.M.; Reale, G.; Pastorino, R.; Padua, L. Virtual Reality and Lower Limb Rehabilitation: Effects on Motor and Cognitive Outcome—A Crossover Pilot Study. J. Clin. Med. 2022, 11, 2300. [Google Scholar] [CrossRef] [PubMed]
- Gamito, P.; Oliveira, J.; Coelho, C.; Morais, D.; Lopes, P.; Pacheco, J.; Brito, R.; Soares, F.; Santos, N.; Barata, A.F. Cognitive training on stroke patients via virtual reality-based serious games. Disabil. Rehabil. 2017, 39, 385–388. [Google Scholar] [CrossRef] [PubMed]
- Gamito, P.; Oliveira, J.; Matias, M.; Cunha, E.; Brito, R.; Lopes, P.F.; Deus, A. Virtual Reality Cognitive Training Among Individuals with Alcohol Use Disorder Undergoing Residential Treatment: Pilot Randomized Controlled Trial. J. Med. Internet Res. 2020, 23, e18482. [Google Scholar] [CrossRef] [PubMed]
- Gangemi, A.; De Luca, R.; Fabio, R.A.; Lauria, P.; Rifici, C.; Pollicino, P.; Marra, A.; Olivo, A.; Quartarone, A.; Calabrò, R.S. Effects of Virtual Reality Cognitive Training on Neuroplasticity: A Quasi-Randomized Clinical Trial in Patients with Stroke. Biomedicines 2023, 11, 3225. [Google Scholar] [CrossRef] [PubMed]
- Gavish, N.; Gutiérrez, T.; Webel, S.; Rodríguez, J.; Peveri, M.; Bockholt, U.; Tecchia, F. Evaluating virtual reality and augmented reality training for industrial maintenance and assembly tasks. Interact. Learn. Environ. 2015, 23, 778–798. [Google Scholar] [CrossRef]
- Ghiţă, A.; Hernández-Serrano, O.; Fernández-Ruiz, J.; Moreno, M.; Monras, M.; Ortega, L.; Mondon, S.; Teixidor, L.; Gual, A.; Gacto-Sanchez, M.; et al. Attentional Bias, Alcohol Craving, and Anxiety Implications of the Virtual Reality Cue-Exposure Therapy in Severe Alcohol Use Disorder: A Case Report. Front. Psychol. 2021, 12, 543586. [Google Scholar] [CrossRef]
- Gomez, J.; Hoffman, H.G.; Bistricky, S.L.; Gonzalez, M.; Rosenberg, L.; Sampaio, M.; Garcia-Palacios, A.; Navarro-Haro, M.V.; Alhalabi, W.; Rosenberg, M.; et al. The Use of Virtual Reality Facilitates Dialectical Behavior Therapy® “Observing Sounds and Visuals” Mindfulness Skills Training Exercises for a Latino Patient with Severe Burns: A Case Study. Front. Psychol. 2017, 8, 1611. [Google Scholar] [CrossRef] [PubMed]
- Gueye, T.; Dedkova, M.; Rogalewicz, V.; Grunerova-Lippertova, M.; Angerova, Y. Early post-stroke rehabilitation for upper limb motor function using virtual reality and exoskeleton: Equally efficient in older patients. Neurol. Neurochir. Pol. 2020, 55, 91–96. [Google Scholar] [CrossRef] [PubMed]
- Hadley, W.; Houck, C.; Brown, L.K.; Spitalnick, J.S.; Ferrer, M.; Barker, D. Moving Beyond Role-Play: Evaluating the Use of Virtual Reality to Teach Emotion Regulation for the Prevention of Adolescent Risk Behavior Within a Randomized Pilot Trial. J. Pediatr. Psychol. 2018, 44, 425–435. [Google Scholar] [CrossRef]
- Heinrich, C.; Morkisch, N.; Langlotz, T.; Regenbrecht, H.; Dohle, C. Feasibility and psychophysical effects of immersive virtual reality-based mirror therapy. J. Neuroeng. Rehabil. 2022, 19, 1–20. [Google Scholar] [CrossRef]
- Hisler, G.C.; Young, K.S.; Cumpanasoiu, D.C.; Palacios, J.E.; Duffy, D.; Enrique, A.; Keegan, D.; Richards, D. Incorporating a deep-learning client outcome prediction tool as feedback in supported internet-delivered cognitive behavioural therapy for depression and anxiety: A randomised controlled trial within routine clinical practice. Couns. Psychother. Res. 2024, 25, e12771. [Google Scholar] [CrossRef]
- Hong, J.C.; Eclov, N.C.W.; Stephens, S.J.; Mowery, Y.M.; Palta, M. Implementation of machine learning in the clinic: Challenges and lessons in prospective deployment from the System for High Intensity EvaLuation During Radiation Therapy (SHIELD-RT) randomized controlled study. BMC Bioinform. 2022, 23, 1–7. [Google Scholar] [CrossRef]
- Hornstein, S.; Forman-Hoffman, V.; Nazander, A.; Ranta, K.; Hilbert, K. Predicting therapy outcome in a digital mental health intervention for depression and anxiety: A machine learning approach. Digit. Health 2020, 7, 20552076211060659. [Google Scholar] [CrossRef] [PubMed]
- Hung, S.C.-W.; Ho, A.Y.-N.; Lai, I.H.-W.; Lee, C.S.-W.; Pong, A.S.-K.; Lai, F.H.-Y. Meta-Analysis on the Effectiveness of Virtual Reality Cognitive Training (VRCT) and Computer-Based Cognitive Training (CBCT) for Individuals with Mild Cognitive Impairment (MCI). Electronics 2020, 9, 2185. [Google Scholar] [CrossRef]
- Javanbakht, A.; Madaboosi, S.; Grasser, L. Augmented Reality and Telemedicine: Real Life Contextualization of Safety Learning in Exposure Therapy. Biol. Psychiatry 2020, 87, S256. [Google Scholar] [CrossRef]
- Jeun, Y.J.; Nam, Y.; A Lee, S.; Park, J.-H. Effects of Personalized Cognitive Training with the Machine Learning Algorithm on Neural Efficiency in Healthy Younger Adults. Int. J. Environ. Res. Public Health 2022, 19, 13044. [Google Scholar] [CrossRef]
- Jiménez, S.; Angeles-Valdez, D.; Rodríguez-Delgado, A.; Fresán, A.; Miranda, E.; Alcalá-Lozano, R.; Duque-Alarcón, X.; de Montis, I.A.; Garza-Villarreal, E.A. Machine learning detects predictors of symptom severity and impulsivity after dialectical behavior therapy skills training group in borderline personality disorder. J. Psychiatr. Res. 2022, 151, 42–49. [Google Scholar] [CrossRef]
- Jóźwik, S.; Cieślik, B.; Gajda, R.; Szczepańska-Gieracha, J. Evaluation of the Impact of Virtual Reality-Enhanced Cardiac Rehabilitation on Depressive and Anxiety Symptoms in Patients with Coronary Artery Disease: A Randomised Controlled Trial. J. Clin. Med. 2021, 10, 2148. [Google Scholar] [CrossRef] [PubMed]
- Jung, H.W.; Jang, K.W.; Nam, S.; Ahn, M.E.; Lee, S.-K.; Kim, Y.J.; Shin, J.-K.; Park, J.H.; Roh, D. Personalized virtual reality exposure for panic disorder and agoraphobia: A preliminary neurophysiological study. Compr. Psychiatry 2023, 129, 152447. [Google Scholar] [CrossRef] [PubMed]
- Kaldo, V.; Isacsson, N.; Forsell, E.; Bjurner, P.; Ben Abdesslem, F.; Boman, M. AI-driven adaptive treatment strategies in internet-delivered CBT. Eur. Psychiatry 2021, 64, S20. [Google Scholar] [CrossRef]
- Kaminska, D.; Smolka, K.; Zwolinski, G.; Wiak, S.; Merecz-Kot, D.; Anbarjafari, G. Stress Reduction Using Bilateral Stimulation in Virtual Reality. IEEE Access 2020, 8, 200351–200366. [Google Scholar] [CrossRef]
- Kannampallil, T.; Dai, R.; Lv, N.; Xiao, L.; Lu, C.; Ajilore, O.A.; Snowden, M.B.; Venditti, E.M.; Williams, L.M.; Kringle, E.A.; et al. Cross-trial prediction of depression remission using problem-solving therapy: A machine learning approach. J. Affect. Disord. 2022, 308, 89–97. [Google Scholar] [CrossRef]
- Kawakami, N.; Imamura, K.; Watanabe, K.; Sekiya, Y.; Sasaki, N.; Sato, N.; SMART-CBT Project Team. Effectiveness of an Internet-Based Machine-Guided Stress Management Program Based on Cognitive Behavioral Therapy for Improving Depression Among Workers: Protocol for a Randomized Controlled Trial. JMIR Res. Protoc. 2021, 10, e30305. [Google Scholar] [CrossRef]
- Kennedy, G.A.; Pedram, S.; Sanzone, S. Improving safety outcomes through medical error reduction via virtual reality-based clinical skills training. Saf. Sci. 2023, 165, 106200. [Google Scholar] [CrossRef]
- King, S.; Boyer, J.; Bell, T.; Estapa, A. An Automated Virtual Reality Training System for Teacher-Student Interaction: A Randomized Controlled Trial. JMIR Serious Games 2022, 10, e41097. [Google Scholar] [CrossRef]
- Kitapcioglu, D.; Aksoy, M.E.; Ozkan, A.E.; Usseli, T. Comparing Learning Outcomes of Machine-Guided Virtual Reality–Based Training with Educator-Guided Training in a Metaverse Environment: Randomized Controlled Trial. JMIR Serious Games 2024, 12, e58654. [Google Scholar] [CrossRef]
- Kohli, M.; Kar, A.K.; Bangalore, A.; AP, P. Machine learning-based ABA treatment recommendation and personalization for autism spectrum disorder: An exploratory study. Brain Inform. 2022, 9, 1–25. [Google Scholar] [CrossRef]
- Koo, K.-I.; Park, D.K.; Youm, Y.S.; Cho, S.D.; Hwang, C.H. Enhanced Reality Showing Long-Lasting Analgesia after Total Knee Arthroplasty: Prospective, Randomized Clinical Trial. Sci. Rep. 2018, 8, 1–9. [Google Scholar] [CrossRef] [PubMed]
- Kovar, I. Virtual Reality as Support of Cognitive Behavioral Therapy in Social Anxiety Disorder. Int. J. Adv. Sci. Eng. Inf. Technol. 2018, 8, 1343–1349. [Google Scholar] [CrossRef][Green Version]
- Ledwos, N.; Mirchi, N.; Yilmaz, R.; Winkler-Schwartz, A.; Sawni, A.; Fazlollahi, A.M.; Bissonnette, V.; Bajunaid, K.; Sabbagh, A.J.; Del Maestro, R.F. Assessment of learning curves on a simulated neurosurgical task using metrics selected by artificial intelligence. J. Neurosurg. 2022, 137, 1160–1171. [Google Scholar] [CrossRef] [PubMed]
- Lee, M.; Tang, N.; Ahluwalia, M.; Fonkem, E.; Fink, K.; Dhruv, H.; Berens, M.; Peng, S. BIOM-24. Identifying vulnerability signatures through machine learning in an umbrella trial for glioblastoma. Neuro-Oncology 2020, 22, ii6–ii7. [Google Scholar] [CrossRef]
- Leehr, E.J.; Roesmann, K.; Böhnlein, J.; Dannlowski, U.; Gathmann, B.; Herrmann, M.J.; Junghöfer, M.; Schwarzmeier, H.; Seeger, F.R.; Siminski, N.; et al. Clinical predictors of treatment response towards exposure therapy in virtuo in spider phobia: A machine learning and external cross-validation approach. J. Anxiety Disord. 2021, 83, 102448. [Google Scholar] [CrossRef]
- Leonardi, S.; Maggio, M.G.; Russo, M.; Bramanti, A.; Arcadi, F.A.; Naro, A.; Calabrò, R.S.; De Luca, R. Cognitive recovery in people with relapsing/remitting multiple sclerosis: A randomized clinical trial on virtual reality-based neurorehabilitation. Clin. Neurol. Neurosurg. 2021, 208, 106828. [Google Scholar] [CrossRef]
- Li, F.; Jörg, F.; Merkx, M.; Feenstra, T. RWD43 Early Symptom-Change Contributes to the Outcome Prediction of Cognitive Behavioral Therapy for Depression Patients: A Machine Learning Approach. Value Health 2022, 25, S456. [Google Scholar] [CrossRef]
- Liao, S.; Shao, S.; Gao, S.; Lai, E.C. Augmented reality enhances medical education and improves efficiency. Med. Educ. 2024, 58, 586–587. [Google Scholar] [CrossRef]
- Liao, Y.-Y.; Tseng, H.-Y.; Lin, Y.-J.; Wang, C.-J.; Hsu, W.-C. Using virtual reality-based training to improve cognitive function, instrumental activities of daily living and neural efficiency in older adults with mild cognitive impairment. Eur. J. Phys. Rehabil. Med. 2020, 56, 47–57. [Google Scholar] [CrossRef]
- Lin, P.-H.; Chen, S.-Y. Design and Evaluation of a Deep Learning Recommendation Based Augmented Reality System for Teaching Programming and Computational Thinking. IEEE Access 2020, 8, 45689–45699. [Google Scholar] [CrossRef]
- De Luca, R.; Bonanno, M.; Marra, A.; Rifici, C.; Pollicino, P.; Caminiti, A.; Castorina, M.V.; Santamato, A.; Quartarone, A.; Calabrò, R.S. Can Virtual Reality Cognitive Rehabilitation Improve Executive Functioning and Coping Strategies in Traumatic Brain Injury? A Pilot Study. Brain Sci. 2023, 13, 578. [Google Scholar] [CrossRef] [PubMed]
- De Luca, R.; Maggio, M.G.; Maresca, G.; Latella, D.; Cannavò, A.; Sciarrone, F.; Voi, E.L.; Accorinti, M.; Bramanti, P.; Calabrò, R.S. Improving Cognitive Function after Traumatic Brain Injury: A Clinical Trial on the Potential Use of the Semi-Immersive Virtual Reality. Behav. Neurol. 2019, 2019, 1–7. [Google Scholar] [CrossRef] [PubMed]
- Maciołek, J.; Wąsek, W.; Kamiński, B.; Piotrowicz, K.; Krzesiński, P. The impact of mobile virtual reality–enhanced relaxation training on anxiety levels in patients undergoing cardiac rehabilitation. Kardiol. Pol. 2020, 78, 1032–1034. [Google Scholar] [CrossRef]
- Maggio, M.G.; Cannavò, A.; Quartarone, A.; Manuli, A.; Tonin, P.; Calabrò, R.S. Enhancing the Quality of Life of Patients with Multiple Sclerosis: Promising Results on the Role of Cognitive Tele-Rehabilitation Plus Virtual Reality. Brain Sci. 2023, 13, 1636. [Google Scholar] [CrossRef]
- Maggio, M.G.; De Cola, M.C.; Latella, D.; Maresca, G.; Finocchiaro, C.; La Rosa, G.; Cimino, V.; Sorbera, C.; Bramanti, P.; De Luca, R.; et al. What About the Role of Virtual Reality in Parkinson Disease’s Cognitive Rehabilitation? Preliminary Findings From a Randomized Clinical Trial. J. Geriatr. Psychiatry Neurol. 2018, 31, 312–318. [Google Scholar] [CrossRef]
- Maggio, M.G.; Torrisi, M.; Buda, A.; De Luca, R.; Piazzitta, D.; Cannavò, A.; Leo, A.; Milardi, D.; Manuli, A.; Calabro, R.S. Effects of robotic neurorehabilitation through lokomat plus virtual reality on cognitive function in patients with traumatic brain injury: A retrospective case-control study. Int. J. Neurosci. 2019, 130, 117–123. [Google Scholar] [CrossRef]
- Manenti, R.; Gobbi, E.; Baglio, F.; Macis, A.; Ferrari, C.; Pagnoni, I.; Rossetto, F.; Di Tella, S.; Alemanno, F.; Cimino, V.; et al. Effectiveness of an Innovative Cognitive Treatment and Telerehabilitation on Subjects with Mild Cognitive Impairment: A Multicenter, Randomized, Active-Controlled Study. Front. Aging Neurosci. 2020, 12, 585988. [Google Scholar] [CrossRef]
- Maresca, G.; Leonardi, S.; De Cola, M.C.; Giliberto, S.; Di Cara, M.; Corallo, F.; Quartarone, A.; Pidalà, A. Use of Virtual Reality in Children with Dyslexia. Children 2022, 9, 1621. [Google Scholar] [CrossRef]
- Navarrete, J.; Martínez-Sanchis, M.; Bellosta-Batalla, M.; Baños, R.; Cebolla, A.; Herrero, R. Compassionate Embodied Virtual Experience Increases the Adherence to Meditation Practice. Appl. Sci. 2021, 11, 1276. [Google Scholar] [CrossRef]
- Maskey, M.; Rodgers, J.; Ingham, B.; Freeston, M.; Evans, G.; Labus, M.; Parr, J.R. Using Virtual Reality Environments to Augment Cognitive Behavioral Therapy for Fears and Phobias in Autistic Adults. Autism Adulthood 2019, 1, 134–145. [Google Scholar] [CrossRef]
- Massetti, T.; Crocetta, T.B.; da Silva, T.D.; Trevizan, I.L.; Arab, C.; Caromano, F.A.; Monteiro, C.B.d.M. Application and outcomes of therapy combining transcranial direct current stimulation and virtual reality: A systematic review. Disabil. Rehabil. Assist. Technol. 2017, 12, 551–559. [Google Scholar] [CrossRef] [PubMed]
- Mazurek, J.; Cieślik, B.; Wrzeciono, A.; Gajda, R.; Szczepańska-Gieracha, J. Immersive Virtual Reality Therapy Is Supportive for Orthopedic Rehabilitation among the Elderly: A Randomized Controlled Trial. J. Clin. Med. 2023, 12, 7681. [Google Scholar] [CrossRef] [PubMed]
- Meinlschmidt, G.; Tegethoff, M.; Belardi, A.; Stalujanis, E.; Oh, M.; Jung, E.K.; Kim, H.-C.; Yoo, S.-S.; Lee, J.-H. Personalized prediction of smartphone-based psychotherapeutic micro-intervention success using machine learning. J. Affect. Disord. 2020, 264, 430–437. [Google Scholar] [CrossRef]
- Miloff, A.; Lindner, P.; Dafgård, P.; Deak, S.; Garke, M.; Hamilton, W.; Heinsoo, J.; Kristoffersson, G.; Rafi, J.; Sindemark, K.; et al. Automated virtual reality exposure therapy for spider phobia vs. in-vivo one-session treatment: A randomized non-inferiority trial. Behav. Res. Ther. 2019, 118, 130–140. [Google Scholar] [CrossRef]
- Miloff, A.; Lindner, P.; Hamilton, W.; Reuterskiöld, L.; Andersson, G.; Carlbring, P. Single-session gamified virtual reality exposure therapy for spider phobia vs. traditional exposure therapy: Study protocol for a randomized controlled non-inferiority trial. Trials 2016, 17, 1–8. [Google Scholar] [CrossRef] [PubMed]
- Montesano, A.; Medina, J.C.; Paz, C.; García-Mieres, H.; Niño-Robles, N.; García-Grau, E.; Crespillo, J.C.; García-Gutiérrez, A.; Alabèrnia-Segura, M.; Feixas, G. Does virtual reality increase the efficacy of psychotherapy for young adults with mild-to-moderate depression? A study protocol for a multicenter randomized clinical trial. Trials 2021, 22, 1–14. [Google Scholar] [CrossRef]
- Navarra-Ventura, G.; Gomà, G.; de Haro, C.; Jodar, M.; Sarlabous, L.; Hernando, D.; Bailón, R.; Ochagavía, A.; Blanch, L.; López-Aguilar, J.; et al. Virtual Reality-Based Early Neurocognitive Stimulation in Critically Ill Patients: A Pilot Randomized Clinical Trial. J. Pers. Med. 2021, 11, 1260. [Google Scholar] [CrossRef]
- Nekar, D.M.; Lee, D.-Y.; Hong, J.-H.; Kim, J.-S.; Kim, S.-G.; Seo, Y.-G.; Yu, J.-H. Effects of Augmented Reality Game-Based Cognitive–Motor Training on Restricted and Repetitive Behaviors and Executive Function in Patients with Autism Spectrum Disorder. Healthcare 2022, 10, 1981. [Google Scholar] [CrossRef]
- Norouzi, E.; Gerber, M.; Pühse, U.; Vaezmosavi, M.; Brand, S. Combined virtual reality and physical training improved the bimanual coordination of women with multiple sclerosis. Neuropsychol. Rehabil. 2020, 31, 552–569. [Google Scholar] [CrossRef]
- Otkhmezuri, B.; Boffo, M.; Siriaraya, P.; Matsangidou, M.; Wiers, R.W.; Mackintosh, B.; Ang, C.S.; Salemink, E. Believing Is Seeing: A Proof-of-Concept Semiexperimental Study on Using Mobile Virtual Reality to Boost the Effects of Interpretation Bias Modification for Anxiety. JMIR Ment. Health 2019, 6, e11517. [Google Scholar] [CrossRef]
- Park, J.-S.; Jung, Y.-J.; Lee, G. Virtual Reality-Based Cognitive–Motor Rehabilitation in Older Adults with Mild Cognitive Impairment: A Randomized Controlled Study on Motivation and Cognitive Function. Healthcare 2020, 8, 335. [Google Scholar] [CrossRef] [PubMed]
- Park, M.; Ha, Y. Effects of Virtual Reality-Based Cognitive Rehabilitation in Stroke Patients: A Randomized Controlled Trial. Healthcare 2023, 11, 2846. [Google Scholar] [CrossRef] [PubMed]
- Pau, M.; Porta, M.; Bertoni, R.; Mattos, F.G.M.; Cocco, E.; Cattaneo, D. Effect of immersive virtual reality training on hand-to-mouth task performance in people with Multiple Sclerosis: A quantitative kinematic study. Mult. Scler. Relat. Disord. 2022, 69, 104455. [Google Scholar] [CrossRef]
- Paul, M.; Bullock, K.; Bailenson, J. Virtual Reality Behavioral Activation for Adults with Major Depressive Disorder: Feasibility Randomized Controlled Trial. JMIR Ment. Health 2021, 9, e35526. [Google Scholar] [CrossRef]
- Paul, M.; Bullock, K.; Bailenson, J.; Burns, D. Examining the Efficacy of Extended Reality–Enhanced Behavioral Activation for Adults with Major Depressive Disorder: Randomized Controlled Trial. JMIR Ment. Health 2023, 11, e52326. [Google Scholar] [CrossRef] [PubMed]
- Pearson, R.; Pisner, D.; Meyer, B.; Shumake, J.; Beevers, C.G. A machine learning ensemble to predict treatment outcomes following an Internet intervention for depression. Psychol. Med. 2018, 49, 2330–2341. [Google Scholar] [CrossRef]
- Piette, J.D.; Newman, S.; Krein, S.L.; Marinec, N.; Chen, J.; Williams, D.A.; Edmond, S.N.; Driscoll, M.; LaChappelle, K.M.; Maly, M.; et al. Artificial Intelligence (AI) to improve chronic pain care: Evidence of AI learning. Intell. Med. 2022, 6, 100064. [Google Scholar] [CrossRef]
- Plencler, I.; Kruk, D.; Daren, A.; Stankiewicz, P.; Nowak, A.; Radoń, S.; Chrobak, A.; Cechnicki, A.; Siwek, M. The effects of mindfulness-based training in virtual reality on psychotic symptoms, mood and cognitive functioning—A pilot study. Psychiatr. Polska 2024, 58, 289–302. [Google Scholar] [CrossRef]
- Porras-Garcia, B.; Ferrer-Garcia, M.; Serrano-Troncoso, E.; Carulla-Roig, M.; Soto-Usera, P.; Miquel-Nabau, H.; Olivares, L.F.-D.C.; Marnet-Fiol, R.; Santos-Carrasco, I.d.l.M.; Borszewski, B.; et al. AN-VR-BE. A Randomized Controlled Trial for Reducing Fear of Gaining Weight and Other Eating Disorder Symptoms in Anorexia Nervosa through Virtual Reality-Based Body Exposure. J. Clin. Med. 2021, 10, 682. [Google Scholar] [CrossRef]
- Price, G.D.; Heinz, M.V.; Nemesure, M.D.; McFadden, J.; Jacobson, N.C. Predicting symptom response and engagement in a digital intervention among individuals with schizophrenia and related psychoses. Front. Psychiatry 2022, 13, 807116. [Google Scholar] [CrossRef] [PubMed]
- Raglio, A.; Imbriani, M.; Imbriani, C.; Baiardi, P.; Manzoni, S.; Gianotti, M.; Castelli, M.; Vanneschi, L.; Vico, F.; Manzoni, L. Machine learning techniques to predict the effectiveness of music therapy: A randomized controlled trial. Comput. Methods Programs Biomed. 2019, 185, 105160. [Google Scholar] [CrossRef] [PubMed]
- Raikwar, A.; Mifsud, D.; Wickens, C.D.; Batmaz, A.U.; Warden, A.C.; Kelley, B.; Clegg, B.A.; Ortega, F.R. Beyond the Wizard of Oz: Negative Effects of Imperfect Machine Learning to Examine the Impact of Reliability of Augmented Reality Cues on Visual Search Performance. IEEE Trans. Vis. Comput. Graph. 2024, 30, 2662–2670. [Google Scholar] [CrossRef] [PubMed]
- Rao, A.K.; Chandra, S.; Dutt, V. Learning from feedback: Evaluation of dynamic decision-making in virtual reality under various repetitive training frameworks. Front. Psychol. 2022, 13, 872061. [Google Scholar] [CrossRef]
- Real, F.J.; Whitehead, M.; Ollberding, N.J.; Rosen, B.L.; Meisman, A.; Crosby, L.E.; Klein, M.D.; Herbst, R. A Virtual Reality Curriculum to Enhance Residents’ Behavioral Health Anticipatory Guidance Skills: A Pilot Trial. Acad. Pediatr. 2022, 23, 185–192. [Google Scholar] [CrossRef]
- Richter, T.; Fishbain, B.; Fruchter, E.; Richter-Levin, G.; Okon-Singer, H. Machine learning-based diagnosis support system for differentiating between clinical anxiety and depression disorders. J. Psychiatr. Res. 2021, 141, 199–205. [Google Scholar] [CrossRef]
- Rutkowski, S.; Szczegielniak, J.; Szczepańska-Gieracha, J. Evaluation of the Efficacy of Immersive Virtual Reality Therapy as a Method Supporting Pulmonary Rehabilitation: A Randomized Controlled Trial. J. Clin. Med. 2021, 10, 352. [Google Scholar] [CrossRef]
- Serino, S.; Pedroli, E.; Tuena, C.; De Leo, G.; Stramba-Badiale, M.; Goulene, K.; Mariotti, N.G.; Riva, G. A Novel Virtual Reality-Based Training Protocol for the Enhancement of the “Mental Frame Syncing” in Individuals with Alzheimer’s Disease: A Development-of-Concept Trial. Front. Aging Neurosci. 2017, 9, 240. [Google Scholar] [CrossRef]
- Serrano-Vergel, R.; Morillo, P.; Casas-Yrurzum, S.; Cruz-Neira, C. Exploring the Suitability of Using Virtual Reality and Augmented Reality for Anatomy Training. IEEE Trans. Hum.-Mach. Syst. 2023, 53, 378–389. [Google Scholar] [CrossRef]
- Shaw, M.; Palmeri, M.; Krupp, L.; Charvet, L. Acute and Lasting Benefits of a Virtual Reality in Multiple Sclerosis (P1.7-010). Neurology 2019, 92 (Suppl. 15), P1-7. [Google Scholar] [CrossRef]
- Shiels, S.-A.; Fadipe, A.; Hundle, A.; Williams, J.; Warren, R.; Higham, H. O21 Real learning in a virtual emergency: Comparing teaching methods for medical students. In Proceedings of the Abstracts of the Association of Simulated Practice in Healthcare, 10th Annual Conference, Belfast, UK, 4–6 November 2019. [Google Scholar] [CrossRef]
- Singh, G.; Mantri, A.; Sharma, O.; Kaur, R. Virtual reality learning environment for enhancing electronics engineering laboratory experience. Comput. Appl. Eng. Educ. 2020, 29, 229–243. [Google Scholar] [CrossRef]
- Smith, M.J.; Humm, L.B.; Fleming, M.F.; Jordan, N.; Wright, M.A.; Ginger, E.J.; Wright, K.; Olsen, D.; Bell, M.D. Virtual reality job interview training for veterans with posttraumatic stress disorder. J. Vocat. Rehabil. 2015, 42, 271–279. [Google Scholar] [CrossRef]
- Soboczenski, F.; Trikalinos, T.A.; Kuiper, J.; Bias, R.G.; Wallace, B.C.; Marshall, I.J. Machine learning to help researchers evaluate biases in clinical trials: A prospective, randomized user study. BMC Med. Inform. Decis. Mak. 2019, 19, 96. [Google Scholar] [CrossRef] [PubMed]
- Sokołowska, B.; Świderski, W.; Smolis-Bąk, E.; Sokołowska, E.; Sadura-Sieklucka, T. A machine learning approach to evaluate the impact of virtual balance/cognitive training on fall risk in older women. Front. Comput. Neurosci. 2024, 18, 1390208. [Google Scholar] [CrossRef] [PubMed]
- Solcà, M.; Ronchi, R.; Bello-Ruiz, J.; Schmidlin, T.; Herbelin, B.; Luthi, F.; Konzelmann, M.; Beaulieu, J.-Y.; Delaquaize, F.; Schnider, A.; et al. Heartbeat-enhanced immersive virtual reality to treat complex regional pain syndrome. Neurology 2018, 91, e479–e489. [Google Scholar] [CrossRef]
- Specht, J.; Stegmann, B.; Gross, H.; Krakow, K. Cognitive Training with Head-Mounted Display Virtual Reality in Neurorehabilitation: Pilot Randomized Controlled Trial. JMIR Serious Games 2023, 11, e45816. [Google Scholar] [CrossRef] [PubMed]
- Stamou, G.; Garcia-Palacios, A.; Woodford, B.J.; Suso-Ribera, C.; Botella, C. The Combination of Cognitive-Behavioural Therapy with Virtual Reality for the Treatment of Postnatal Depression in a Brief Intervention Context: A Single-Case Study Trial. J. Health Eng. 2021, 2021, 1–20. [Google Scholar] [CrossRef]
- Stephenson, C.; Jagayat, J.; Kumar, A.; Khamooshi, P.; Eadie, J.; Pannu, A.; Meartsi, D.; Danaee, E.; Gutierrez, G.; Khan, F.; et al. Comparing clinical decision-making of AI technology to a multi-professional care team in an electronic cognitive behavioural therapy program for depression: Protocol. Front. Psychiatry 2023, 14, 1220607. [Google Scholar] [CrossRef]
- Syed, U.E.; Kamal, A. Video game-based and conventional therapies in patients of neurological deficits: An experimental study. Disabil. Rehabil. Assist. Technol. 2019, 16, 332–339. [Google Scholar] [CrossRef]
- Symons, M.; Feeney, G.F.; Gallagher, M.R.; Young, R.M.; Connor, J.P. Machine learning vs addiction therapists: A pilot study predicting alcohol dependence treatment outcome from patient data in behavior therapy with adjunctive medication. J. Subst. Abus. Treat. 2019, 99, 156–162. [Google Scholar] [CrossRef]
- Tacca, C.; Kerr, B.A.; McLamb, C.; Ridgway, K.L.; Friis, E.A. Efficacy of a remote virtual reality and EEG enabled psychotherapy system for the treatment of depressive symptoms. Front. Virtual Real. 2024, 5, 1281017. [Google Scholar] [CrossRef]
- Tan, M.; Xiao, Y.; Jing, F.; Xie, Y.; Lu, S.; Xiang, M.; Ren, H. Evaluating machine learning-enabled and multimodal data-driven exercise prescriptions for mental health: A randomized controlled trial protocol. Front. Psychiatry 2024, 15, 1352420. [Google Scholar] [CrossRef]
- Thapa, N.; Park, H.J.; Yang, J.-G.; Son, H.; Jang, M.; Lee, J.; Kang, S.W.; Park, K.W.; Park, H. The Effect of a Virtual Reality-Based Intervention Program on Cognition in Older Adults with Mild Cognitive Impairment: A Randomized Control Trial. J. Clin. Med. 2020, 9, 1283. [Google Scholar] [CrossRef] [PubMed]
- Thomas, J.; McDonald, S.; Noel-Storr, A.; Shemilt, I.; Elliott, J.; Mavergames, C.; Marshall, I.J. Machine learning reduced workload with minimal risk of missing studies: Development and evaluation of a randomized controlled trial classifier for Cochrane Reviews. J. Clin. Epidemiol. 2020, 133, 140–151. [Google Scholar] [CrossRef] [PubMed]
- Tonacci, A.; Dellabate, A.; Dieni, A.; Bachi, L.; Sansone, F.; Conte, R.; Billeci, L. Can Machine Learning Predict Stress Reduction Based on Wearable Sensors’ Data Following Relaxation at Workplace? A Pilot Study. Processes 2020, 8, 448. [Google Scholar] [CrossRef]
- Torpil, B.; Şahin, S.; Pekçetin, S.; Uyanık, M. The Effectiveness of a Virtual Reality-Based Intervention on Cognitive Functions in Older Adults with Mild Cognitive Impairment: A Single-Blind, Randomized Controlled Trial. Games Health J. 2021, 10, 109–114. [Google Scholar] [CrossRef]
- Tsai, C.-F.; Yeh, S.-C.; Huang, Y.; Wu, Z.; Cui, J.; Zheng, L. The Effect of Augmented Reality and Virtual Reality on Inducing Anxiety for Exposure Therapy: A Comparison Using Heart Rate Variability. J. Health Eng. 2018, 2018, 1–8. [Google Scholar] [CrossRef]
- Viczko, J.; Tarrant, J.; Jackson, R. Effects on Mood and EEG States After Meditation in Augmented Reality with and Without Adjunctive Neurofeedback. Front. Virtual Real. 2021, 2, 618381. [Google Scholar] [CrossRef]
- Weerasinghe, M.; Quigley, A.; Pucihar, K.C.; Toniolo, A.; Miguel, A.; Kljun, M. Arigatō: Effects of Adaptive Guidance on Engagement and Performance in Augmented Reality Learning Environments. IEEE Trans. Vis. Comput. Graph. 2022, 28, 3737–3747. [Google Scholar] [CrossRef]
- Winslow, B.D.; Kwasinski, R.; Hullfish, J.; Ruble, M.; Lynch, A.; Rogers, T.; Nofziger, D.; Brim, W.; Woodworth, C. Automated stress detection using mobile application and wearable sensors improves symptoms of mental health disorders in military personnel. Front. Digit. Health 2022, 4, 919626. [Google Scholar] [CrossRef]
- Wuang, Y.-P.; Chen, Y.J.; Chiu, Y.-H.; Wang, C.-C.; Chen, C.-P.; Huang, C.-L.; Wu, T.-M.; Hsieh, T.-H.; Ho, W.-H. Effectiveness of Kinesthetic Game-Based Training System in Children with Visual-Perceptual Dysfunction. IEEE Access 2021, 9, 153838–153849. [Google Scholar] [CrossRef]
- Yang, J.-G.; Thapa, N.; Park, H.-J.; Bae, S.; Park, K.W.; Park, J.-H.; Park, H. Virtual Reality and Exercise Training Enhance Brain, Cognitive, and Physical Health in Older Adults with Mild Cognitive Impairment. Int. J. Environ. Res. Public Health 2022, 19, 13300. [Google Scholar] [CrossRef]
- Yang, S.; Chun, M.H.; Son, Y.R. Effect of Virtual Reality on Cognitive Dysfunction in Patients with Brain Tumor. Ann. Rehabil. Med. 2014, 38, 726–733. [Google Scholar] [CrossRef] [PubMed]
- Yang, W.; Wang, X. Why do Generative Learning Strategy Improve Memory in VR? Based on ICALM. Int. J. Inf. Educ. Technol. 2021, 11, 646–650. [Google Scholar] [CrossRef]
- Antonopoulou, H.; Halkiopoulos, C.; Gkintoni, E.; Katsimpelis, A. Application of Gamification Tools for Identification of Neurocognitive and Social Function in Distance Learning Education. Int. J. Learn. Teach. Educ. Res. 2022, 21, 367–400. [Google Scholar] [CrossRef]
- Gkintoni, E.; Vantaraki, F.; Skoulidi, C.; Anastassopoulos, P.; Vantarakis, A. Promoting Physical and Mental Health among Children and Adolescents via Gamification—A Conceptual Systematic Review. Behav. Sci. 2024, 14, 102. [Google Scholar] [CrossRef]
- Lv, Z.; Qiao, L.; Wang, Q.; Piccialli, F. Advanced machine-learning methods for brain-computer interfacing. IEEE/ACM Trans. Comput. Biol. Bioinform. 2020, 18, 1688–1698. [Google Scholar] [CrossRef]
- Moss, J.; Wong, A.Y.; Durriseau, J.A.; Bradshaw, G.L. Tracking strategy changes using machine learning classifiers. Behav. Res. Methods 2021, 54, 1818–1840. [Google Scholar] [CrossRef]
- Punamiya, Z.; Gupta, N.; Patil, S.A. Exploring augmented reality, virtual reality, and machine learning for delivering better value in the healthcare sector. In Revolutionizing the Healthcare Sector with AI; IGI Global: Hershey, PA, USA, 2024; pp. 111–130. [Google Scholar]
- Gkintoni, E.; Aroutzidis, A.; Antonopoulou, H.; Halkiopoulos, C. From Neural Networks to Emotional Networks: A Systematic Review of EEG-Based Emotion Recognition in Cognitive Neuroscience and Real-World Applications. Brain Sci. 2025, 15, 220. [Google Scholar] [CrossRef]
- Ford, T.; Buchanan, D.M.; Azeez, A.; Benrimoh, D.A.; Kaloiani, I.; Bandeira, I.D.; Hunegnaw, S.; Lan, L.; Gholmieh, M.; Buch, V.; et al. Taking modern psychiatry into the metaverse: Integrating augmented, virtual, and mixed reality technologies into psychiatric care. Front. Digit. Health 2023, 5, 1146806. [Google Scholar] [CrossRef]
- Halbig, A.; Babu, S.K.; Gatter, S.; Latoschik, M.E.; Brukamp, K.; von Mammen, S. Opportunities and Challenges of Virtual Reality in Healthcare—A Domain Experts Inquiry. Front. Virtual Real. 2022, 3, 837616. [Google Scholar] [CrossRef]
- Halkiopoulos, C.; Gkintoni, E.; Aroutzidis, A.; Antonopoulou, H. Advances in Neuroimaging and Deep Learning for Emotion Detection: A Systematic Review of Cognitive Neuroscience and Algorithmic Innovations. Diagnostics 2025, 15, 456. [Google Scholar] [CrossRef] [PubMed]
- Alkaeed, M.; Qayyum, A.; Qadir, J. Privacy preservation in Artificial Intelligence and Extended Reality (AI-XR) metaverses: A survey. J. Netw. Comput. Appl. 2024, 231, 103989. [Google Scholar] [CrossRef]
- Letafati, M.; Otoum, S. On the privacy and security for e-health services in the metaverse: An overview. Ad Hoc Netw. 2023, 150, 103262. [Google Scholar] [CrossRef]
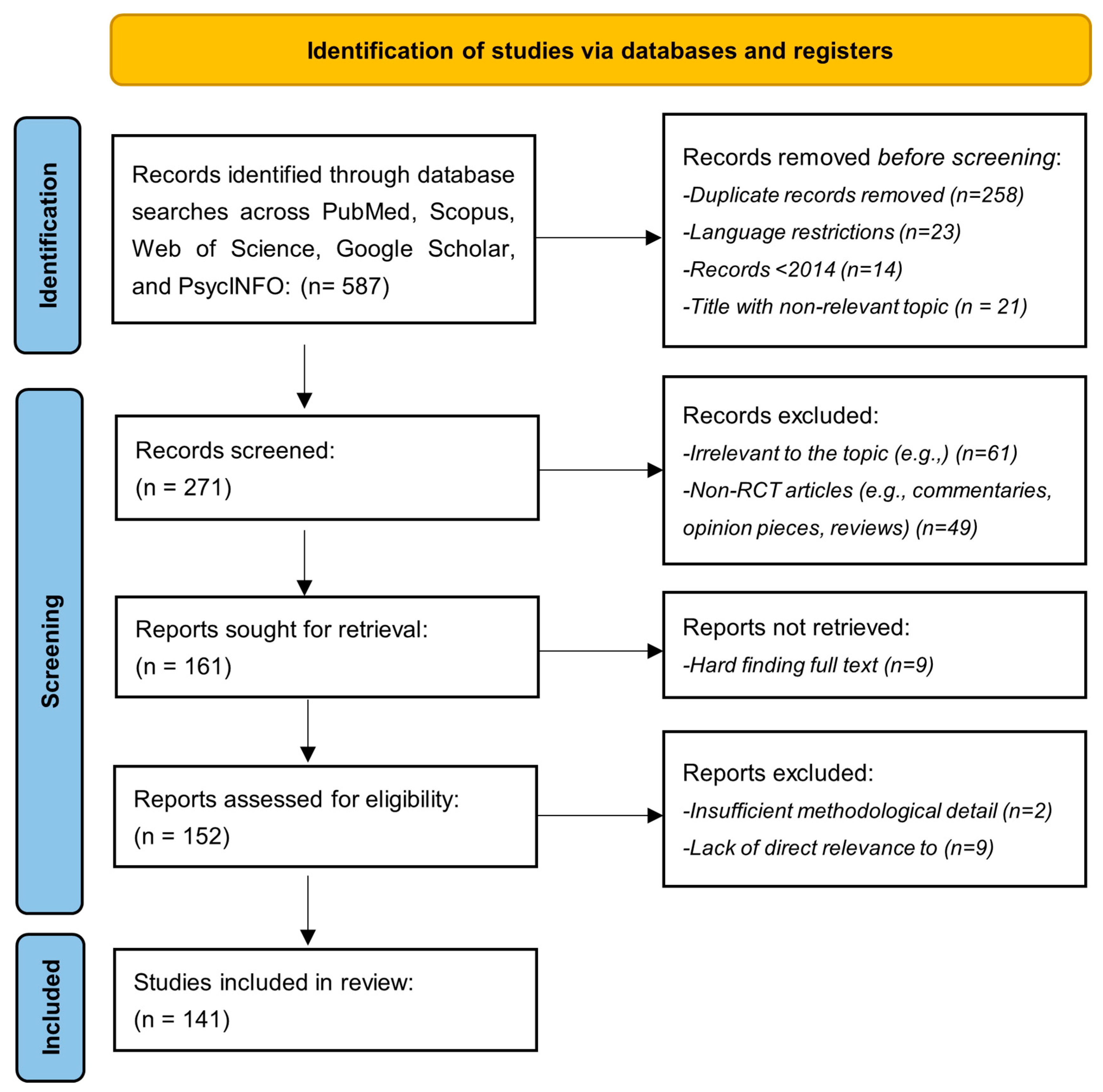



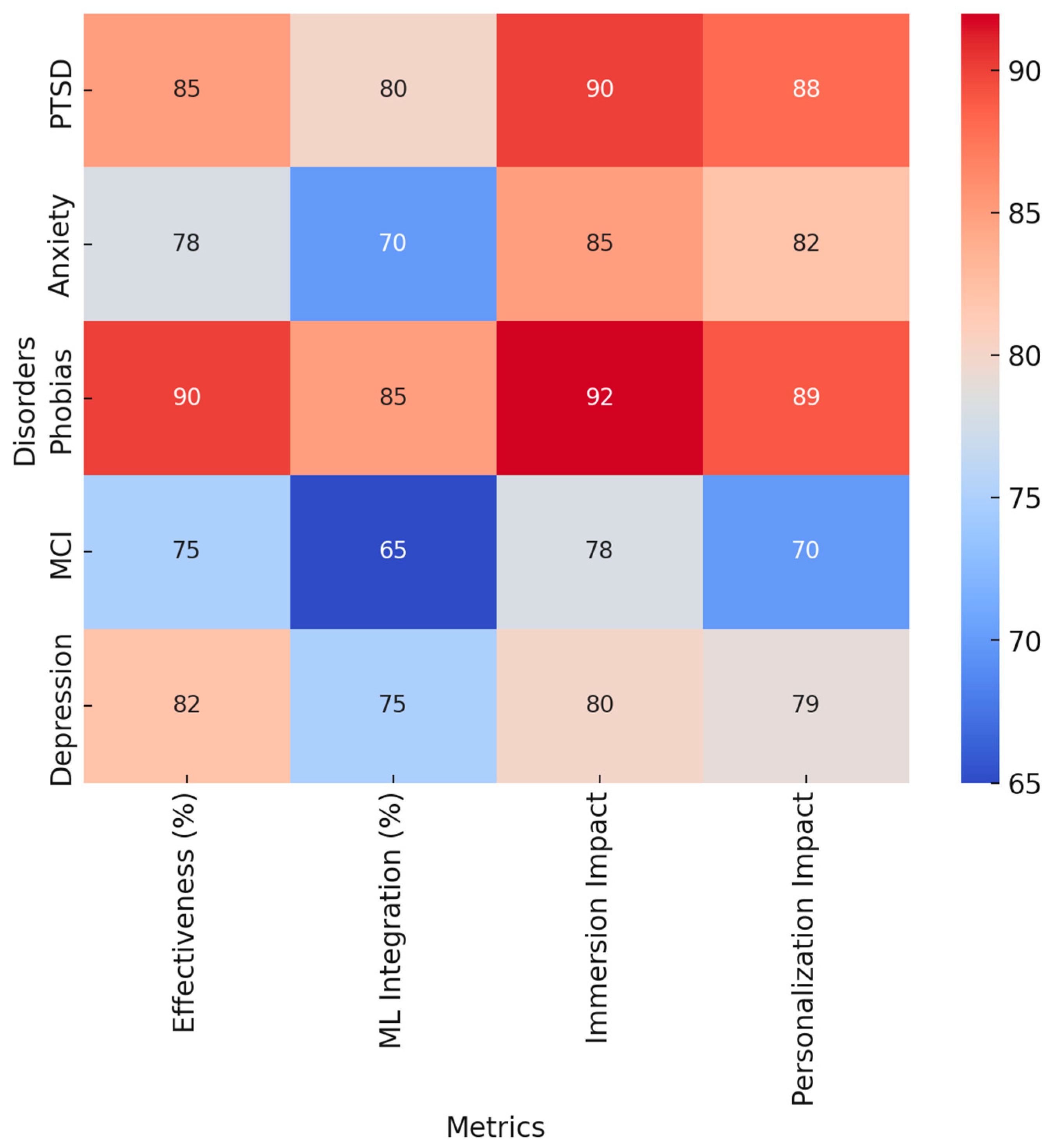

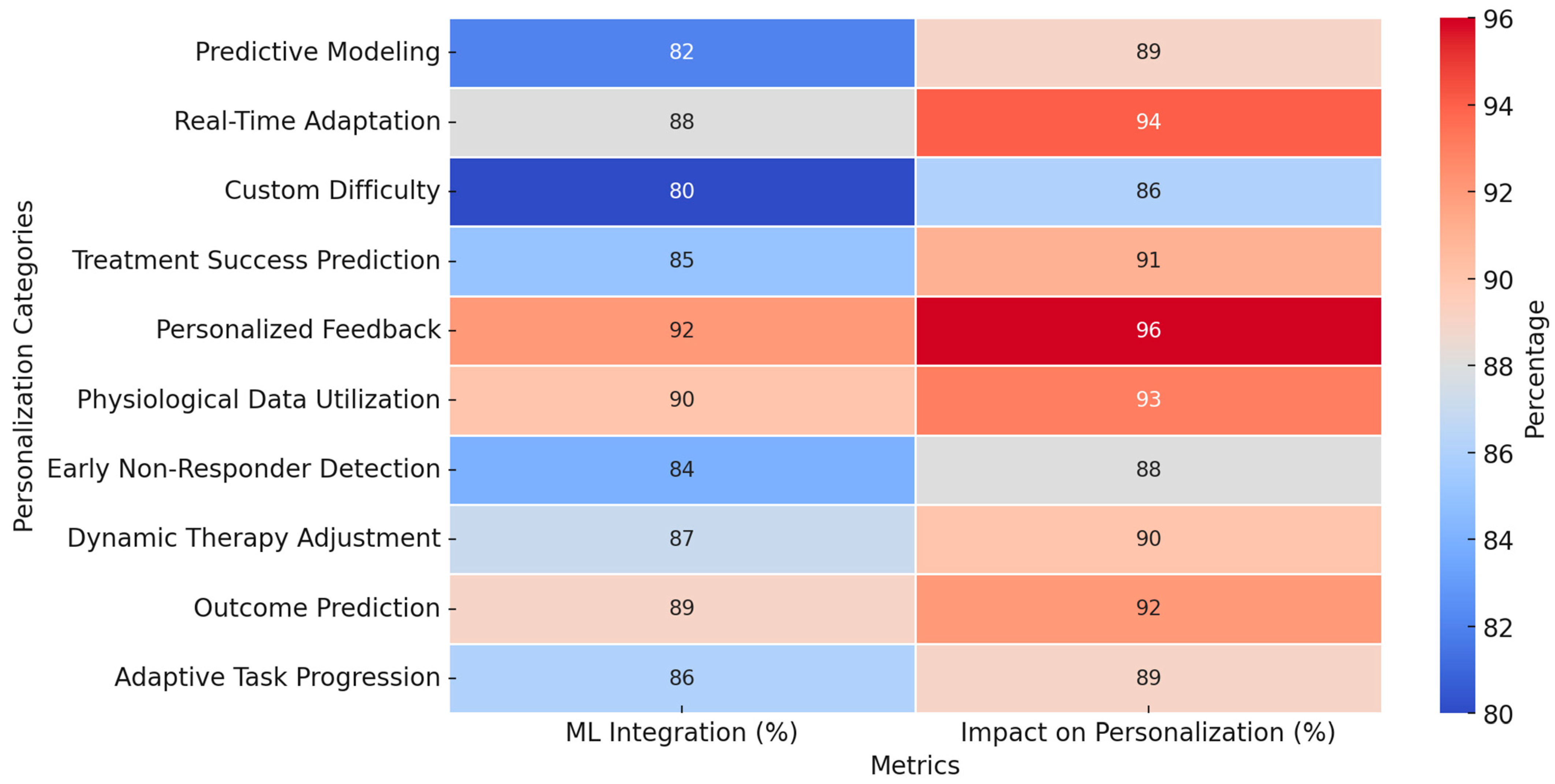
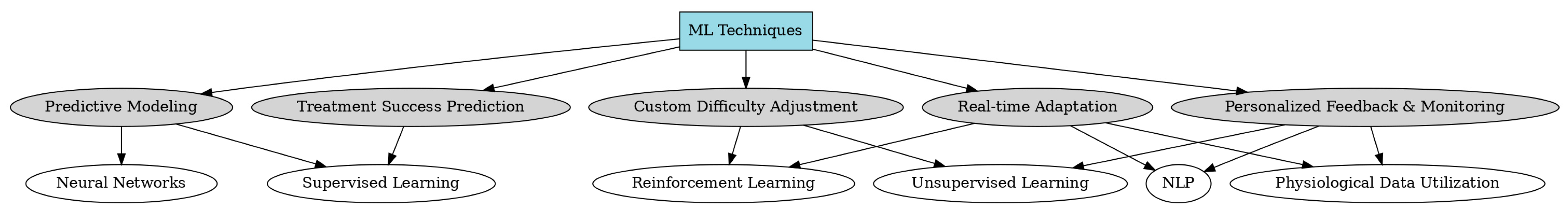
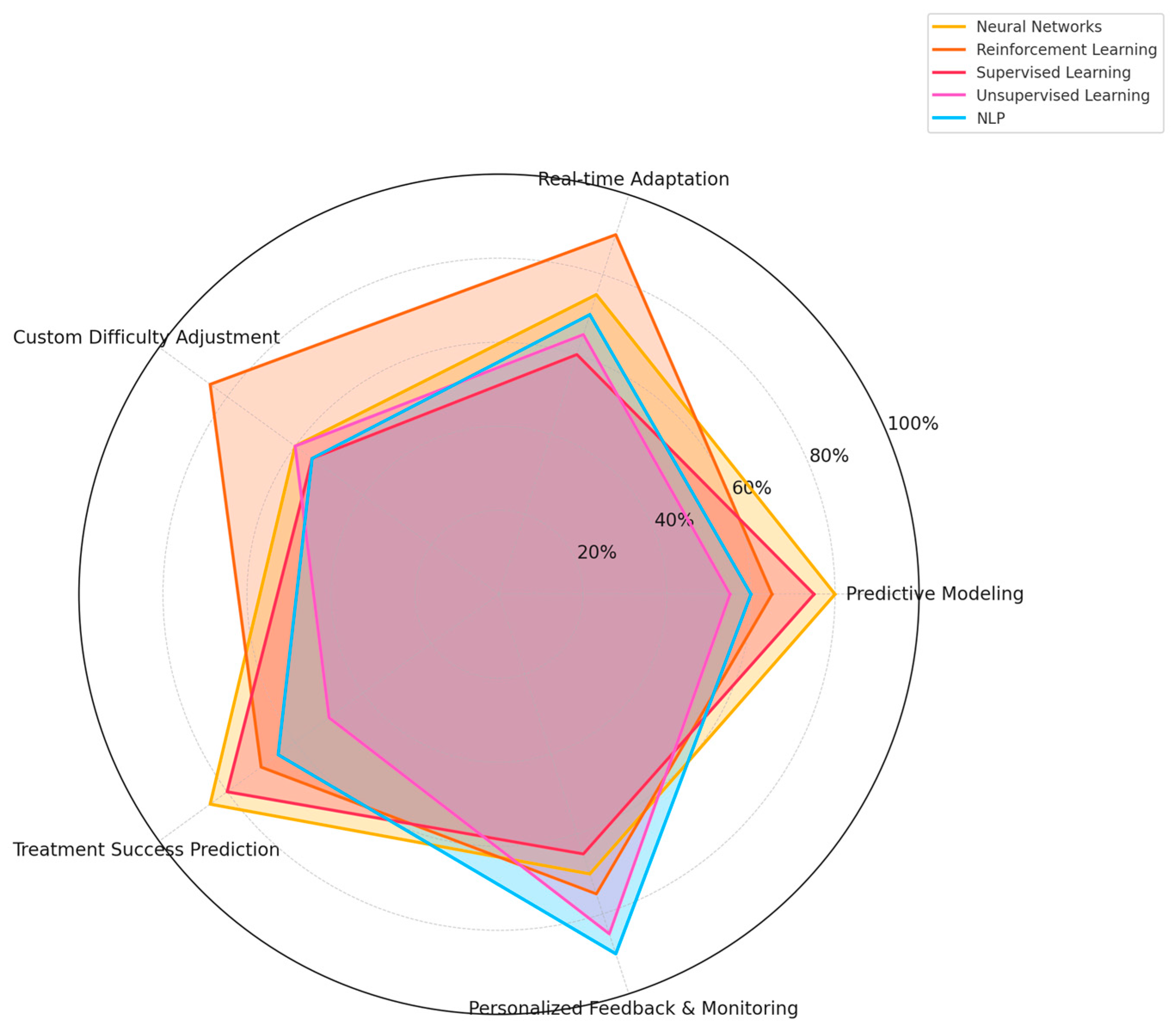


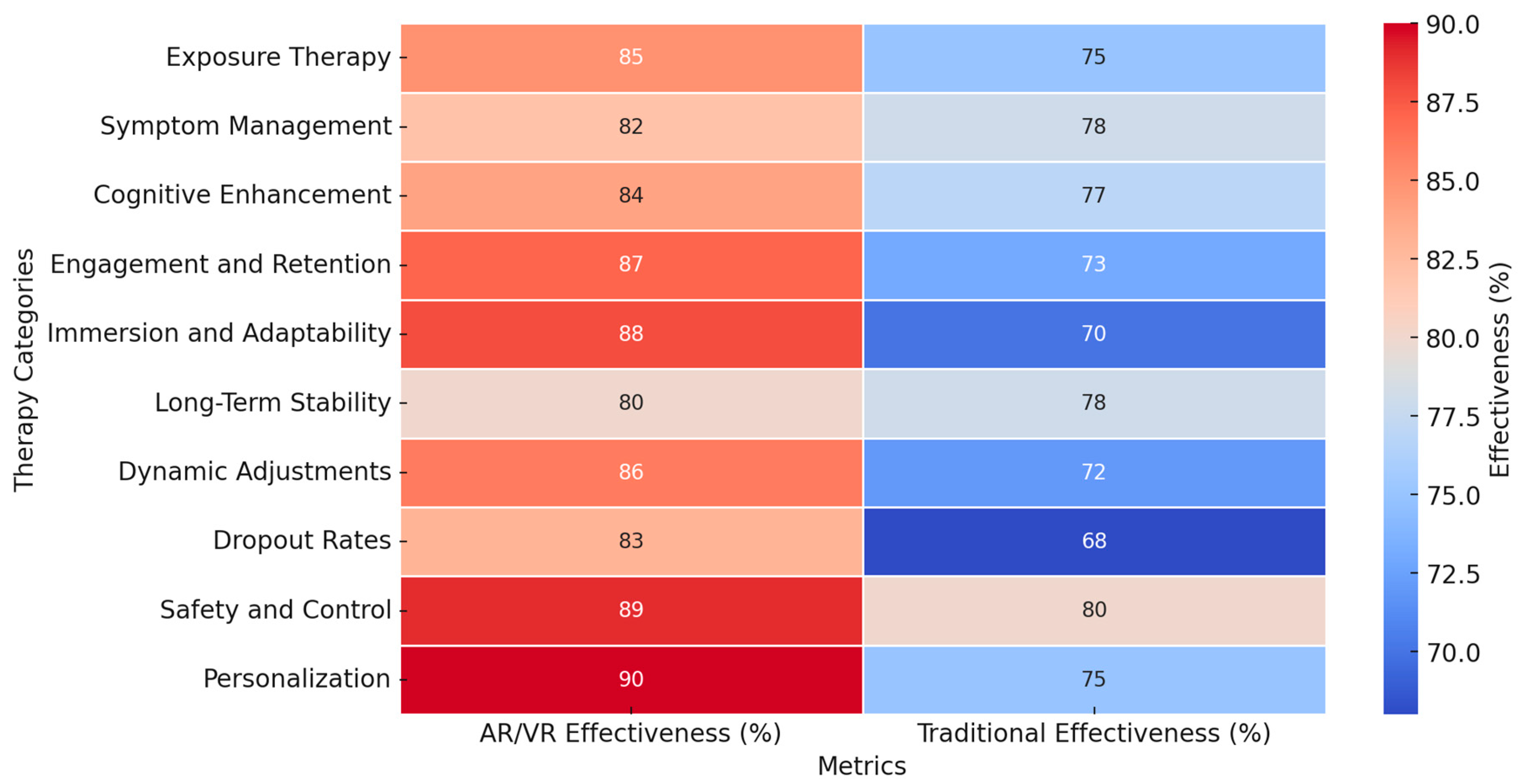
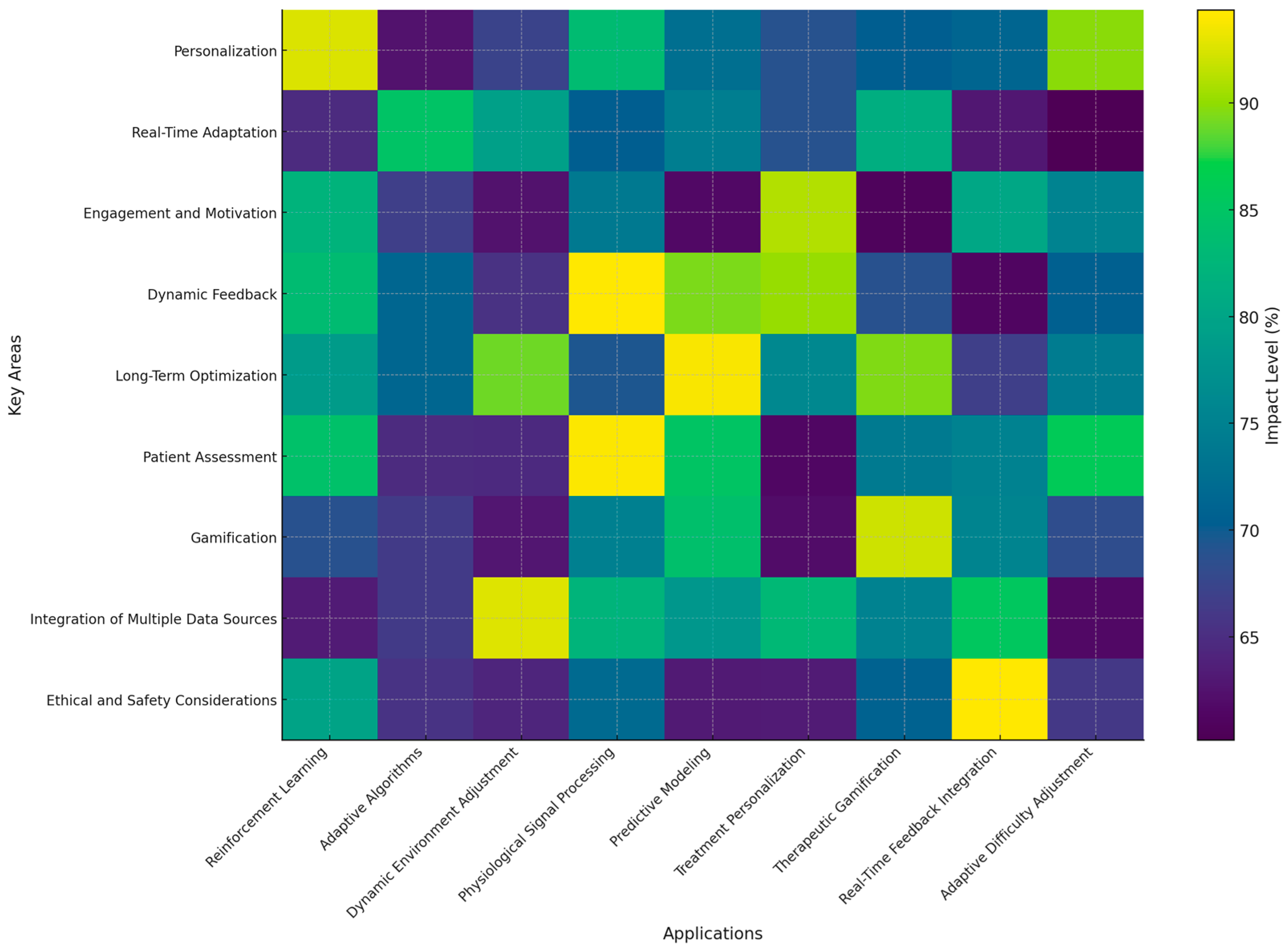

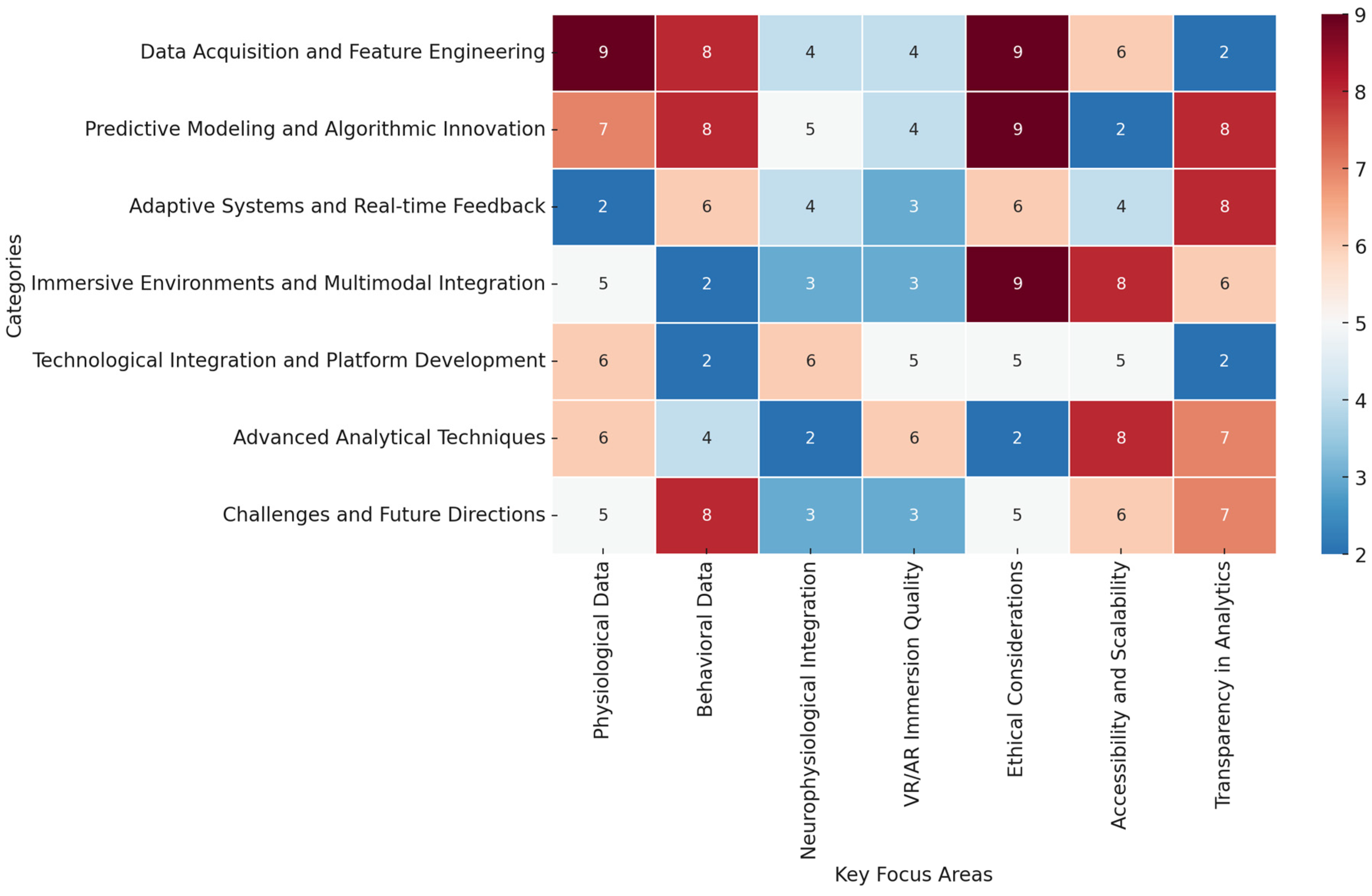
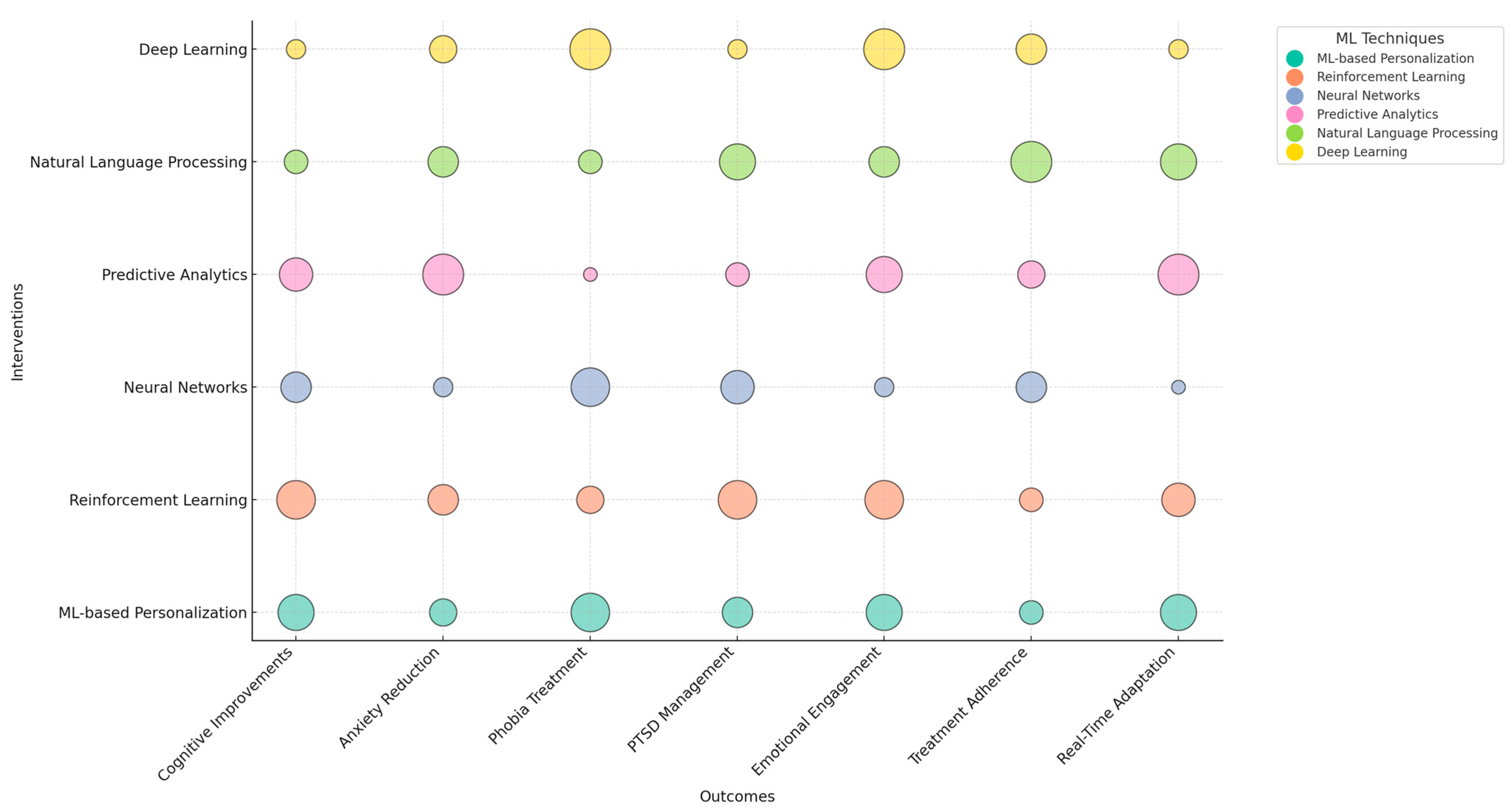
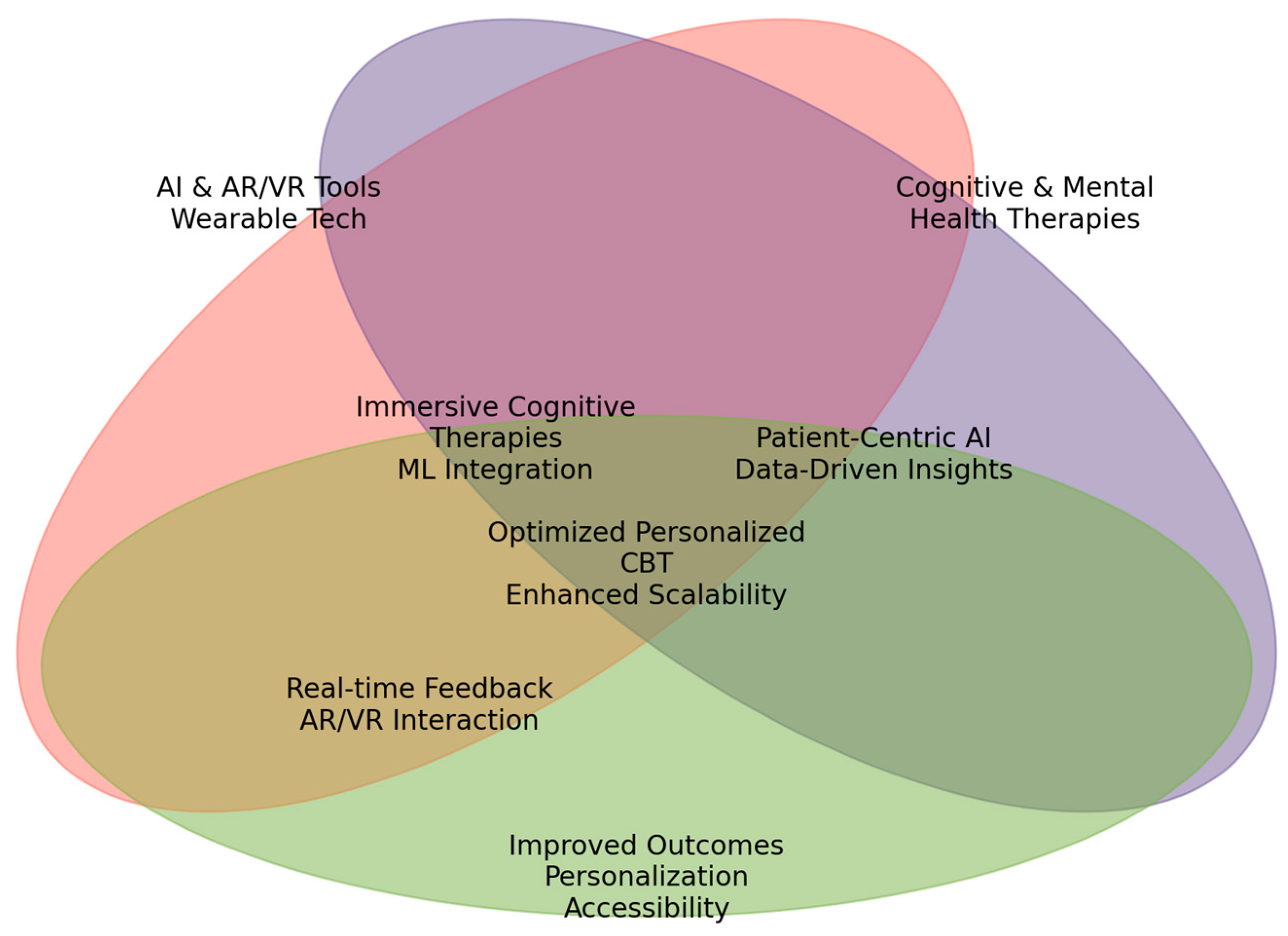
| Machine Learning | Description | Examples in Cognitive Therapy | Common Algorithms/Approaches |
|---|---|---|---|
| Supervised Learning [53,54,55,56,57] | Utilizes labeled datasets to train models for predictive tasks. | Patient progress prediction, emotion detection, diagnosis of mental health conditions. | Linear Regression, Decision Trees, SVM, Random Forests, Neural Networks. |
| Unsupervised Learning [58,59,60,61,62] | Finds hidden patterns in unlabeled datasets by clustering similar data points or reducing dimensional complexity. | Patient clustering, anomaly detection, feature extraction for VR therapy. | K-Means Clustering, Hierarchical Clustering, PCA, Autoencoders, SOM. |
| Semi-Supervised Learning [63,64,65,66,67] | Combines small amounts of labeled data with large volumes of unlabeled data. | AI-powered mental health assessments, personalized AR/VR exposure therapy. | Self-Training Models, Graph-Based Learning, GANs, Label Propagation. |
| Reinforcement Learning [68,69,70] | Learns optimal decision making by interacting with an environment and maximizing cumulative rewards. | Real-time therapy adjustment, gamification in cognitive therapy, adaptive treatment planning. | Q-Learning, Deep Q-Networks, Proximal Policy Optimization, Actor–Critic Models. |
| Deep Learning [71,72,73,74] | Uses multilayer artificial neural networks to automate feature extraction and handle complex patterns. | Virtual counselors and chatbots, speech and emotion recognition, EEG-based mental health monitoring. | CNNs, RNNs, LSTM, Transformers (BERT, GPT). |
| Transfer Learning [28,29,30] | Enables pre-trained ML models to be fine-tuned for specific applications. | Customizing VR therapy models, emotion analysis from pre-trained models. | Fine-tuned CNNs, BERT, GPT, ResNet, U-Net. |
| Federated Learning [31,32,33] | Allows ML models to be trained across multiple decentralized data sources without sharing raw patient data. | Secure multi-center VR therapy training, real-time AI adaptation for mental health. | Google’s Federated Averaging, Differential Privacy, Secure Aggregation Protocols. |
| Inclusion Criteria | Details |
|---|---|
| Research Focus | Investigates the efficacy, feasibility, or applicability of ML-enhanced AR/VR cognitive therapies for mental health treatment. |
| Study Design | Randomized controlled trials (RCTs), quasi-experimental studies, or other empirical research using validated methodologies. |
| Target Population | Individuals diagnosed with PTSD, anxiety disorders, phobias, or other clinically relevant mental health conditions are treated with AR/VR-based cognitive therapies. |
| ML Techniques | Studies applying RL, neural networks, supervised learning, predictive analytics, or adaptive algorithms within AR/VR-based cognitive interventions. |
| Publication Source | Peer-reviewed journal articles and conference proceedings published between 2014 and 2024. |
| Language | Published in English to ensure accessibility for systematic analysis. |
| Full-Text Access | Studies with full-text availability for comprehensive data extraction and analysis. |
| Exclusion Criteria | Details |
|---|---|
| Non-Relevant Focus | Studies that do not explicitly explore ML, AR/VR, or cognitive therapy interventions for mental health disorders. |
| Study Type | Non-empirical papers include systematic reviews, meta-analyses, commentaries, editorials, theoretical papers, and opinion pieces. |
| Language Restriction | Articles published in languages other than English. |
| Unrelated Population | Research focuses on populations outside PTSD, anxiety disorders, and phobias, such as neurological disorders or cognitive impairments unrelated to mental health. |
| Methodological Limitations | Studies with small sample sizes, inadequate statistical analysis, lack of control groups, or insufficient methodological transparency. |
| Publication Date | Studies published before 2014 consider advancements in ML and AR/VR therapy applications in the past decade. |
| Authors | Hypotheses |
|---|---|
| Ahn, 2021 [101] | -Cognitive therapy improvements: Combined VR and computer game-based cognitive therapy enhance visual perception aspects, including spatial relations, visual-motor speed, motor-reduced visual perception, and general visual perception, in children with intellectual disabilities. |
| Albizu et al., 2020 [102] | -Classification of treatment responders: ML combined with MRI-derived electric field models can effectively classify reatment responders versus non-responders. |
| Alkhabra et al., 2023 [103] | -AR technology: Enhances retention of learning and critical thinking. -Effectiveness of AR: Varies in critical thinking and practical skills based on learners’ mental capacity. |
| Allcoat and Mühlenen, 2018 [104] | -VR technology enhances learning, leading to better outcomes, improved memory retention, and higher engagement than traditional and video methods. -VR positively influences emotions, increasing positive feelings and reducing negative ones during the learning process. |
| Alsem et al., 2023 [105] | -Aggression decreases: Expected to be larger in both YourSkills groups (VR and roleplay) compared to the care-as-usual group, with more significant reductions in the VR group. -Perceived efficacy: The VR group is expected to rate the treatment as more effective than the role-play group. |
| Alwashmi et al., 2023 [106] | -Functional brain changes: Support behavioral performance improvements during an audiovisual (AV) learning task. -AV training: Leads to better performance outcomes compared to visual-only training. -Increased functional activation: In multisensory brain regions, it is associated with performance gains. -Multisensory integration: Enhances cognitive function. |
| Andersen et al., 2018 [107] | -Repeated and distributed VR simulation practice: Induces a lower cognitive load during subsequent cadaveric dissection training. |
| Aran et al., 2020 [108] | -Virtual reality-based rehabilitation: Improves cognitive functions in children with hemiplegic cerebral palsy and is more effective than traditional occupational therapy in enhancing cognitive functions in children with hemiplegic cerebral palsy. |
| Arquissandas et al., 2021 [109] | -AR-based system: Effectively elicits and measures physiological responses during exposure therapy for anxiety disorders. -Personalization: The system can adapt to individual profiles using ML algorithms to tailor exposure therapy. |
| Aziz et al., 2020 [110] | -AR technique: The AR technique improves education and training outcomes in assembly processes. |
| Bond et al., 2023 [111] | -gameChange VR cognitive therapy reduces agoraphobic avoidance and distress in people with psychosis. -The therapy is especially effective for individuals with severe avoidance. -Improvements in persecutory ideation, quality of life, and perceived recovery are expected. |
| Bouchard et al., 2017 [112] | -Study 1: VR induces cravings in gamblers comparable to real gambling and more substantial than control games. -Study 2: VR, when integrated with CBT, helps identify high-risk situations, and cravings are linked to improved treatment outcomes. -Study 3: VR is as safe as imaginal exposure, not causing stronger or more uncontrollable urges. |
| Bruschetta et al., 2022 [113] | -Gender and clinical factors: Gender significantly influences cognitive recovery in TBI patients undergoing VR rehabilitation. -Other factors: Anxiety levels and FIM scores also affect recovery outcomes. |
| Buccellato et al., 2019 [114] | -Feasibility: Implementation of the BBVR system in an outpatient clinic. -Effectiveness: Impact on motor function, cognitive performance, and emotional symptoms. -Dose–response: Exploring the effects of therapy duration or intensity. -Performance correlation: Linking BBVR game performance to long-term clinical outcomes. |
| Butti et al., 2019 [115] | -VR-Spirit will enhance social prediction ability in patients with congenital cerebellar malformations. -VR-Spirit will indirectly improve cognitive performance across various domains. -VR-Spirit is more effective than standard VR training in improving social perception skills. |
| Câmara et al., 2021 [116] | -Both Reh@City v2.0 and Task Generator will improve cognitive and emotional outcomes. -Reh@City v2.0 will show greater gains in visual memory and depressive symptoms. -Task Generator will lead to greater improvements in processing speed, verbal memory, and quality of life. -Effects will be maintained at follow-up, with additional improvements in specific cognitive domains for each intervention. |
| Chen et al., 2020 [117] | -VR training will significantly reduce CNV latency and improve upper limb function. -VR intervention will lead to more significant improvements than conventional treatment. |
| Chen et al., 2018 [118] | -Effectiveness of MBRP with VRCE: Mindfulness-Based Relapse Prevention (MBRP) combined with Virtual Reality Cue Exposure (VRCE) will be more effective than MBRP alone and treatment as usual in reducing cravings and emotional responses in individuals with methamphetamine use disorders. |
| Cheng et al., 2021 [119] | -Combining VR training with rTMS will enhance cognitive improvement, especially in memory and visuospatial functions, in patients with Parkinson’s disease and mild cognitive impairment compared to rTMS alone. |
| Choi et al., 2023 [120] | -Biometric responses can effectively forecast personal learning performance in VR-based construction safety training. -A simplified forecast model using principal features can outperform a complete model in prediction accuracy and reduce overfitting. |
| Chun et al., 2022 [121] | -ML models can predict anxiety severity and VR sickness in SAD patients using autonomic signals like heart rate and skin response. -Prediction performance varies across models for different anxiety and VR sickness subdomains. |
| Collaço et al., 2020 [122] | -Immersive technologies enhance skill training in dental anesthesia. -Immersive preceptorship and training improve accuracy and confidence in anesthesia administration. |
| D’Alfonso et al., 2017 [123] | -Online therapy improves long-term outcomes: online psychosocial interventions extend the clinical benefits of specialized face-to-face youth mental health programs into sustained, long-term improvements. -AI supplements clinical support: advanced computational and AI methods effectively supplement the support provided by moderators and clinicians, enabling scalable and personalized user-tailored therapy. |
| Dahdah et al., 2017 [124] | -Immersive VR interventions improve executive function: immersive virtual reality treatment interventions enhance recovery from executive dysfunction in patients with brain injury. -VR Stroop task outperforms traditional formats: performance on a virtual reality version of the Stroop test is more substantial than conventional Stroop test formats. |
| Dellazizzo et al., 2020 [125] | -CBT and VRT combination improves outcomes: combining cognitive behavioral therapy (CBT) and virtual reality therapy (VRT) will be beneficial for treatment-resistant schizophrenia patients. -Synergistic effect of CBT and VRT: Combining CBT and VRT will produce a synergistic effect, enhancing both primary and secondary treatment outcomes. -Greater efficacy on hallucinations: CBT combined with VRT will achieve greater efficacy in reducing auditory verbal hallucinations compared to generic CBT for psychosis (CBTp). |
| Dercon et al., 2023 [126] | -Clearer representations of option values: Cognitive distancing results in more precise representations of option values, reflected by higher inverse temperatures. -Increased sensitivity to negative feedback: Cognitive distancing enhances sensitivity to negative feedback, demonstrated by higher loss learning rates. -Strategic shift over time: Cognitive distancing leads to a strategic change, increasing sensitivity to negative feedback as the task progresses. |
| Dilgul et al., 2021 [127] | -VR group therapy acceptability: The study explores the hypothesis that VR group therapy (VRGT) is an acceptable form of therapy for depression. -Stakeholder perspectives on VR therapy: The study investigates stakeholders’ views on cognitive behavioral group therapy delivered via virtual reality. -Adaptation of CBT for VR delivery: The study examines how cognitive behavioral group therapy can be adapted for effective delivery via virtual reality. |
| Donker et al., 2022 [128] | -Aviophobia symptom reduction: The VR-CBT app treatment is expected to reduce aviophobia symptoms compared to a wait-list control group significantly. -Long-term effectiveness: The reduction in aviophobia symptoms is predicted to be maintained at both 3-month and 12-month follow-up assessments. |
| Donker et al., 2020 [129] | -VR activity and acrophobia symptoms: Higher VR activity (number of completed VR sessions, practice time in VR) is associated with reduced post-test acrophobia symptoms. -Presence and anxiety reduction: Higher presence scores on the IPQ are correlated with more substantial decreases in anxiety ratings directly after practicing with exposure in the VR environment. -Acrophobia and VR response: Higher acrophobia symptoms at pre-test correlate positively with VR anxiety ratings and VR activity and negatively with a reduction in acrophobia symptoms at post-test. -Anxiety reduction over repeated sessions: Post-session anxiety levels consistently decrease compared to pre-session anxiety levels after repeated practice in the VR environment. |
| Duhne et al., 2022 [130] | -Improved attendance: Matching patients to either face-to-face or computerized low-intensity psychological interventions can enhance attendance rates. -Better treatment outcomes: Appropriately matching patients to suitable treatment modalities can improve depression treatment outcomes. |
| Ekstrand et al., 2018 [131] | -Learning outcomes: Virtual reality neuroanatomy training results in equivalent or superior learning outcomes compared to traditional paper-based methods. -Reduced neurophobia and increased motivation: VR training decreases neurophobia and boosts motivation among medical students. |
| Erguzel and Tarhan, 2016 [132] | -rTMS efficacy: Pre-treatment quantitative electroencephalography (QEEG) data can predict the effectiveness of repetitive transcranial magnetic stimulation (rTMS) in treating major depressive disorder (MDD). -ML classification: Various ML techniques, including artificial neural networks (ANNs), support vector machines (SVMs), and decision trees (DTs), can classify MDD patients as responders to rTMS treatment. |
| Faria et al., 2018 [133] | -Improved outcomes: Rehabilitation with the Reh@Task system will result in superior motor and cognitive outcomes compared to standard rehabilitation. -Ecological validity: Integrating motor and cognitive components in VR training enhances its ecological validity, potentially leading to more effective rehabilitation outcomes. |
| Faria et al., 2020 [134] | -Cognitive improvements: The VR-based ADL simulation (Reh@City v2.0) is more effective than paper-and-pencil training (Task Generator) in enhancing general cognitive functioning, visuospatial ability, and executive functions. -Ecological validity: The VR-based approach leads to more significant improvements in cognitive domains and self-perceived cognitive deficits compared to the paper-and-pencil approach. |
| Faria et al., 2016 [135] | -Global cognitive functioning: VR-based cognitive rehabilitation results in more significant global cognitive functioning improvements than conventional rehabilitation. -Attention: VR-based cognitive rehabilitation shows superior improvements in attention compared to conventional methods. -Executive functions: VR-based cognitive rehabilitation leads to more significant enhancements in executive functions than conventional rehabilitation. |
| Fernández-Álvarez et al., 2021 [136] | -Improved recall: The VR-enhanced autobiographical memory (AM) task can enhance the recall of positive memories in individuals with moderate-to-moderately severe depressive symptoms. -Standalone effectiveness: The VR-based AM recall treatment is effective as a standalone intervention. |
| Freeman et al., 2019 [137] | -Reduction in avoidance and distress: VR cognitive therapy, when combined with treatment as usual, will reduce avoidance and distress in real-world situations post-treatment compared to treatment as usual alone. -Reduction in psychiatric symptoms: VR cognitive therapy added to treatment as usual will reduce psychiatric symptoms (paranoia, anxious avoidance, depression, suicidal ideation), increase activity, and improve quality of life post-treatment. -Sustained effects: Treatment effects are expected to be maintained at the 6-month follow-up. -Mediators of treatment: Changes in safety beliefs, threat cognitions, and defense behaviors will mediate VR treatment efficacy. |
| Freeman et al., 2023 [138] | -Increased positive self-beliefs: The VR self-confidence therapy (Phoenix) will enhance positive self-beliefs in participants. -Improved psychological well-being: The VR self-confidence therapy (Phoenix) will improve psychological well-being. |
| Frewen et al., 2020 [139] | -Stronger emotional responses: Direct perception of virtual reality (VR) stimuli is expected to evoke stronger emotional reactions than mental imagery and episodic recall. -Increased vividness and presence: VR may enhance vividness and presence, resulting in more excellent absorption, which mediates the effects on positive affect and psychological well-being. |
| Fusco et al., 2022 [140] | -Enhanced cognitive and motor function: The visual feedback provided by virtual reality (VR), in conjunction with robotic therapy, is hypothesized to improve patients’ cognitive and motor functions more effectively than conventional robotic therapy alone. -Lower limb recovery: A semi-immersive, video-enriched robotic system is expected to enhance the recovery of lower limb function and reduce overall disability in patients with severe acquired brain injury (ABI). |
| Gamito et al., 2017 [141] | -Cognitive improvements: The virtual reality-based cognitive training program effectively enhances stroke patients’ attention and memory functions. |
| Gamito et al., 2020 [142] | -Feasibility: VR-based cognitive training is feasible for improving mental function in patients with alcohol use disorder (AUD) undergoing residential treatment. -Impact on cognitive functions: VR-based cognitive training is expected to positively impact attention and executive functions in individuals with AUD. -Measurable effect: The intervention will demonstrate a measurable effect size to guide future definitive randomized controlled trials (RCTs). |
| Gangemi et al., 2023 [143] | -Neurophysiological changes: VR-based cognitive rehabilitation induces neurophysiological changes in patients with chronic ischemic stroke. -Enhanced cognitive recovery: VR technology enhances cognitive recovery through measurable EEG changes. -Neuroplasticity: VR-based rehabilitation promotes neuroplastic changes in stroke patients. -EEG activity: VR training increases alpha and beta EEG band activity. |
| Gavish et al., 2015 [144] | -Effectiveness in industrial tasks: VR and AR platforms are hypothesized to be effective for training in industrial maintenance and assembly tasks. -Comparison with traditional methods: VR and AR platforms are hypothesized to differ in efficiency and effectiveness from traditional training methods. -AR training: AR training is expected to result in fewer unsolved errors than traditional methods. -VR training: VR training is hypothesized not to significantly improve performance over traditional methods due to a ceiling effect. |
| Ghiţă et al., 2021 [145] | -Reduction in alcohol craving: VR-based cue exposure therapy (VR-CET) is expected to reduce levels of alcohol craving. -Anxiety reduction: VR-CET will lead to a reduction in anxiety levels. -Attentional bias: VR-CET will prompt changes in attentional bias (AB) toward alcohol-related content. -Feasibility: The VR-CET protocol is feasible for implementation within a clinical trial setting. |
| Gómez et al., 2017 [146] | -Emotional impact: After each VR-based DBT-R mindfulness skill training session, the patient is expected to experience a decrease in negative and positive emotions. -Acceptance of VR: The patient is anticipated to accept VR as a method for learning DBT-R mindfulness skills. |
| Gueye et al., 2020 [147] | -Upper limb motor function improvement: Virtual reality therapy (VRT) using the Armeo Spring® exoskeleton effectively enhances upper limb motor function in early post-stroke rehabilitation. -Comparison with conventional physiotherapy: VRT improves upper limb motor function more effectively. |
| Hadley et al., 2018 [148] | -Greater satisfaction: Adolescents randomized to emotion regulation (ER) combined with immersive virtual reality exposure (IVRE) are expected to report greater satisfaction with the intervention. -Higher attendance: Adolescents randomized to ER + IVRE are anticipated to demonstrate higher attendance rates. -Improvement in ER skills: Adolescents randomized to ER + IVRE are expected to significantly improve emotion regulation (ER) skills. -Increased self-efficacy: At the 3-month follow-up, adolescents randomized to ER + IVRE are expected to report greater self-efficacy in engaging in safer behaviors. |
| Heinrich et al., 2022 [149] | -Feasibility: Assessing the feasibility of using an immersive virtual reality (VR) system for mirror therapy in a clinical setting. -Effectiveness: Evaluating the effectiveness of immersive VR-based mirror therapy compared to conventional mirror therapy. |
| Hisler et al., 2024 [150] | -Therapist feedback effects: Assessing the impact of implementing therapist feedback via a deep learning model tool on client treatment response in iCBT. -Therapist acceptability: Evaluating therapists’ acceptability of the deep learning model prediction tool. |
| Hong et al., 2022 [151] | -Mitigating acute care risk: ML can mitigate the increased risk for acute care during outpatient cancer therapy. -Reducing acute care rates: ML models based on electronic health record (EHR) data can guide supplemental clinical evaluations and reduce the rate of acute care during cancer radiotherapy. |
| Hornstein et al., 2020 [152] | -Predicting treatment outcomes: ML can effectively predict treatment outcomes in digital mental health interventions for depression and anxiety. -Contributing variables: Specific clinical and sociodemographic variables contribute significantly to the accuracy of these predictions. |
| Hung et al., 2020 [153] | -Cognitive improvement: Virtual Reality Cognitive Training (VRCT) and Computer-Based Cognitive Training (CBCT) are effective in improving cognitive domains with mild cognitive impairment (MCI). -VRCT benefits: VRCT is more beneficial than CBCT in improving global cognitive function (GCF), executive function (EF), language (Lang), and visuospatial abilities (VSs). -CBCT benefits: CBCT is more beneficial than VRCT in improving memory (Mem). |
| Javanbakht et al., 2020 [154] | -Effectiveness in exposure therapy: Augmented reality combined with telemedicine effectively treats fear of spiders in exposure therapy. |
| Jeun et al., 2022 [155] | -Neural efficiency: Personalized cognitive training with the algorithm has the potential to induce neural efficiency in healthy subjects. |
| Jiménez et al., 2022 [156] | -Baseline predictors: Baseline predictors can be identified to improve the response rate to Dialectical Behavior Therapy (DBT) in patients with borderline personality disorder (BPD). -ML prediction: ML can detect clinical features that predict improvement or worsening in symptom severity and impulsivity. -Key predictors: Specific baseline characteristics, such as “non-judging” mindfulness ability and “non-planning” impulsiveness, are significant predictors of clinical change. -Personalized treatment: Utilizing ML to identify essential variables can enhance personalized treatment and improve disease prognosis. |
| Józwik et al., 2021 [157] | -Effectiveness in reducing depression and anxiety: VR-enhanced cardiac rehabilitation is more effective than standard cardiac rehabilitation in reducing depression and anxiety symptoms. |
| Jung et al., 2023 [158] | -Increased anxiety: Personalized VR exposure can provoke heightened anxiety in patients with panic disorder and agoraphobia. -Stronger anxiogenic effects: Personalized VR exposure elicits more substantial anxiogenic effects, as self-reported measures and neurophysiological data indicate. |
| Kaldo et al., 2021 [159] | -Improved prediction accuracy: ML algorithms can predict a single patient’s outcome with accuracy better than chance. |
| Kamińska et al., 2020 [160] | -Stress relief through VR and EMDR: Integrating virtual reality (VR) with bilateral stimulation used in Eye Movement Desensitization and Reprocessing (EMDR) can effectively relieve stress. -Measurable effects: The VR relaxation training program will have a measurable impact on stress indicators. -Physiological changes: Observable changes in stress levels and physiological indicators will occur before, during, and after the VR sessions. |
| Kannampallil et al., 2022 [161] | -Prediction of depression remission: ML algorithms can be developed to predict depression remission for patients undergoing problem-solving therapy. -Generalization across datasets: These ML models can effectively generalize across different datasets, such as ENGAGE-2 and RAINBOW. -Prediction accuracy: The ML models can predict depression remission with accuracy significantly greater than chance. |
| Kawakami et al., 2021 [162] | -Improvement in depression symptoms: The fully automated machine-guided iCBT program is expected to improve symptoms of depression compared to the control group. -Effect on subthreshold depression: The program is anticipated to have a positive effect on depression among participants with subthreshold depression. |
| Kennedy et al., 2023 [163] | -Reduction in human error: VR-based clinical skill training reduces human error compared to traditional training alone. -Improved learner outcomes: VR-based clinical skill training is a viable approach that provides improved outcomes for learners. |
| King et al., 2022 [164] | -Improvement in mathematical questioning strategy: Compared to individuals who did not receive VR training, the simulation aims to improve participants’ acquisition of steps in a mathematical questioning strategy. -Perceived confidence: The VR simulation is expected to increase participants’ perceived confidence in using the procedure relative to the control group. |
| Kitapcioglu et al., 2024 [165] | -Learning outcome comparison: There is no significant difference in learning outcomes between VR-based, machine-guided training and educator-guided, VR-based training in the metaverse environment for adult advanced cardiac life support (ACLS) training. |
| Kohli et al., 2022 [166] | -Personalized ABA treatment goals: ML algorithms can effectively recommend and personalize applied behavior analysis (ABA) treatment goals for individuals with Autism Spectrum Disorder (ASD). -Mastery of treatment goals: The study participants are expected to master the ABA treatment goals recommended by the ML models effectively. |
| Koo et al., 2018 [167] | -Longer-lasting pain relief: Enhanced reality (ER) analgesia provides longer-lasting pain relief than traditional virtual reality (VR). -Impact of therapy duration: The duration of ER therapy influences the longevity and effectiveness of pain relief and improvements in range of motion (ROM). |
| Kovár, 2018 [168] | -Faster therapy outcomes: Incorporating virtual reality into cognitive behavioral therapy (CBT) can speed up treatment for social anxiety disorder. -Reduced pharmaceutical use: Virtual reality can help reduce the reliance on pharmaceuticals in treating social anxiety disorder. -Greater effectiveness: Virtual reality sessions are more effective than traditional therapeutic sessions in treating social anxiety disorder. |
| Kritikos et al., 2021 [76] | -Personalized VR scenarios: Investigating whether it is possible to create VR scenarios that adapt in real time to each patient’s unique personality during the simulation. -Dynamic adaptation: Exploring whether the proposed VR system can dynamically adapt during the session, in real time, to each participant’s unique behavioral patterns and align with the treatment’s goals. |
| Ledwos et al., 2022 [169] | -AI-derived learning curve metrics: AI-derived metrics can effectively measure learning curves across different expertise levels. -Differences in expertise levels: There are measurable differences in learning curves between groups with varying levels of expertise. -Impact of repeated practice: Repeated practice leads to measurable improvements in performance on VR-simulated tasks. |
| Lee et al., 2020 [170] | -Predictive biomarker signatures: Different biomarker signatures can predict which treatment arm is most beneficial for glioblastoma patients. -Patient classification: Gene Set Variation Analysis (GSVA) and semi-supervised ML can effectively classify patients based on their likelihood of response to specific treatments. |
| Leehr et al., 2021 [171] | -Predictive factors for treatment response: Certain sociodemographic and clinical pre-treatment factors can predict treatment response in individuals with spider phobia. -Effectiveness of VRET: Virtual reality exposure therapy (VRET) is effective at the group level for treating spider phobia. -ML for individual predictions: ML can predict individual treatment responses based on pre-treatment factors. |
| Leonardi et al., 2021 [172] | -Cognitive improvement in MS: VR-based rehabilitation improves cognitive outcomes in multiple sclerosis (MS) patients. -Mood and visuospatial skills: Both conventional and VR cognitive rehabilitation improve mood and visuospatial skills in MS patients. -Greater cognitive gains with VR: VR-based rehabilitation improves specific cognitive domains and quality of life compared to conventional methods. |
| Li et al., 2022 [173] | -Predicting treatment outcomes: ML algorithms can predict treatment outcomes in depression. -Use of predictors: Pre-treatment predictors and early symptom changes can be used to forecast treatment outcomes. |
| Liao et al., 2024 [174] | -Skill acquisition: Augmented reality (AR) enhances trainee skill acquisition by easing spatial orientation challenges and reducing cognitive overload. -Procedural efficiency: AR improves procedural efficiency in ultrasound-guided procedures. -Reduced cognitive workload: AR reduces cognitive workload during training. -Decreased instructional dependence: AR decreases trainees’ dependence on instructional guidance. |
| Liao et al., 2020 [175] | -Cognitive and physical improvements: VR-based physical and cognitive training improves cognitive function, brain activation, and instrumental activities of daily living (IADLs). -Greater effectiveness: VR training is more effective than combined physical and cognitive training in improving these outcomes. -Neural efficiency: VR training leads to increased neural efficiency, as indicated by decreased activation in prefrontal areas. |
| Lin and Chen, 2020 [176] | -Improved learning achievement: The deep learning recommendation system improves learning achievement compared to a non-deep learning recommendation system. -Enhanced computational thinking: The deep learning recommendation system enhances computational thinking ability compared to a non-deep learning recommendation system. -Specific skill improvements: The deep learning recommendation system improves specific dimensions of computational thinking, including creativity, logical computing, critical thinking, and problem-solving skills. |
| Luca et al., 2023 [177] | -Improved executive abilities: Non-immersive virtual reality-based training enhances executive skills in patients with traumatic brain injury (TBI). -Reduced anxiety and depression: Non-immersive virtual reality-based training reduces symptoms of anxiety and depression in TBI patients. -Improved coping and mood: Non-immersive virtual reality-based training improves coping strategies and mood in individuals with chronic TBI. |
| Luca et al., 2019 [178] | -Cognitive function improvement: Virtual reality training with BTS Nirvana is expected to improve cognitive functions in subjects with traumatic brain injury (TBI). -Behavioral function improvement: Virtual reality training with BTS Nirvana will enhance behavioral functions in TBI subjects. |
| Maciolek et al., 2020 [179] | -Reduced anxiety: VR-enhanced relaxation training effectively reduces anxiety levels in patients undergoing cardiac rehabilitation. |
| Maggio et al., 2023 [180] | -Feasibility of cognitive telerehabilitation: Cognitive telerehabilitation is feasible for patients with multiple sclerosis (MS). -Positive influence on quality of life: A home-based personalized exercise program using the Virtual Reality Rehabilitation System (VRRS) can positively impact quality of life scores in MS patients. |
| Maggio et al., 2018 [181] | -Cognitive and behavioral recovery: Virtual reality training with the BTS Nirvana system enhances cognitive and behavioral recovery in patients with Parkinson’s disease. -Improved executive and visuospatial abilities: Virtual reality training improves executive and visuospatial abilities more effectively than traditional cognitive training. |
| Maggio et al., 2020 [182] | -Improved attention and executive functions: Robotic neurorehabilitation using Lokomat with VR enhances attention processes and executive functions in traumatic brain injury (TBI) patients. -Greater cognitive improvements: The integration of VR with Lokomat leads to greater improvements in cognitive, executive, and attention functions compared to using Lokomat without VR. -Enhanced quality of life: The use of Lokomat with VR significantly improves quality of life, particularly in mental and physical well-being, more than Lokomat without VR. |
| Manenti et al., 2020 [183] | -Enhanced memory and attention: The face-to-face Virtual Reality Rehabilitation System (VRRS) is expected to improve memory and attentional abilities more effectively. -Long-term benefits of home-based treatment: Implementing home-based treatment through the cognitive VRRS could induce long-term benefits, extending the positive effects of face-to-face treatment. |
| Maresca et al., 2022 [184] | -Cognitive improvement in dyslexia: The use of a Virtual Reality Rehabilitation System (VRRS) in children with dyslexia is expected to result in additional cognitive improvements. |
| Marti et al., 2021 [185] | -Increased adherence: The embodied VR system is expected to increase adherence to meditation practice. -Improved meditation quality: The embodied VR system will enhance the quality of meditation practice. -Compassionate response: The embodied VR system will generate a compassionate response in participants. |
| Maskey et al., 2019 [186] | -Engagement with VRE scenes: Explore whether autistic adults engage with computer-generated virtual reality exposure (VRE) scenes in a way that allows them to approach and remain in anxiety-provoking situations. -Participation and retention: Investigate participation rates and retention throughout the study. -Session structure appropriateness: Assess whether the four-session treatment structure is suitable for autistic adults by using the same number of sessions and monitoring attendance and outcomes. |
| Massetti et al., 2017 [187] | -Combined tDCS and VR therapy benefits: The combination of transcranial direct current stimulation (tDCS) and virtual reality (VR) therapy leads to beneficial outcomes in multiple health aspects, including improved body sway, gait, stroke recovery, pain management, and vegetative reactions. |
| Mazurek et al., 2023 [188] | -Mental and functional benefits: VR therapy has a beneficial effect on the mental and functional state of individuals undergoing rehabilitation after lower limb arthroplasty. -Reduction in depression, anxiety, and stress: VR therapy effectively alleviates symptoms of depression and anxiety and reduces perceived stress levels in older adults who have undergone arthroplasty surgery. |
| Meinlschmidt et al., 2019 [189] | -Predicting success with ML: ML can predict the success of smartphone-based psychotherapeutic micro-interventions in eliciting mood changes. -Mood changes: Smartphone-based psychotherapeutic micro-interventions can effectively lead to mood changes. |
| Miloff et al., 2019 [190] | -Non-inferiority of VRET: Virtual reality exposure therapy (VRET) is non-inferior to one-session therapy (OST) in reducing symptoms of spider phobia. |
| Miloff et al., 2016 [191] | -Comparable effectiveness: Gamified VR exposure therapy is not inferior to traditional one-session exposure therapy (OST) for treating spider phobia. |
| Montesano et al., 2021 [192] | -Effectiveness of PCT-VR over PCT: Person-Centered Therapy combined with virtual reality (PCT-VR) is more effective than PCT alone in treating mild-to-moderate depression in young adults. -Effectiveness of PCT-VR over CBT: PCT-VR is more effective than cognitive behavioral therapy (CBT) in treating mild-to-moderate depression in young adults. |
| Navarra-Ventura et al., 2021 [193] | -Cognitive and emotional improvements: ENRIC therapy is expected to improve cognitive functioning and emotional state one month after ICU discharge. -Long-term maintenance: The cognitive and emotional improvements from ENRIC therapy will be maintained over a 12-month period. |
| Nekar et al., 2022 [194] | -Improvement in RRBs: AR game-based cognitive-motor training will improve restricted and repetitive behaviors (RRBs) in patients with Autism Spectrum Disorder (ASD). -Enhancement of executive function: AR game-based cognitive-motor training will improve executive function (EF) in patients with ASD. -Attention improvement: AR game-based cognitive-motor training will enhance attention in patients with ASD. |
| Norouzi et al., 2020 [195] | -Bimanual coordination improvement: Each intervention (virtual reality training (VRT), Conventional Physical Therapy (CPT), and their combination (COMB)) will improve bimanual coordination over time. -Greater improvement with combined therapy: The combination of VRT and CPT (COMB) will improve coordination accuracy and consistency compared to VRT or CPT alone. |
| Otkhmezuri et al., 2019 [196] | -Higher immersion and presence: Compared to standard CBM-I, participants will report higher rates of immersion and presence in the VR-Cognitive Bias Modification for Interpretation (VR-CBM-I) training scenarios. -Positive interpretations: VR-CBM-I training will significantly endorse positive interpretations and fewer negative interpretations than standard CBM-I. -Anxiety reduction: VR-CBM-I will result in a more significant decrease in state anxiety compared to standard CBM-I. |
| Park et al., 2020 [197] | -Cognitive function improvement: Virtual Reality Cognitive-Motor Rehabilitation (VRCMR) is more effective than conventional cognitive rehabilitation (CCR) in improving cognitive function. |
| Park and Ha, 2023 [198] | -Improved stroke self-efficacy: The virtual reality-based cognitive rehabilitation program will improve stroke self-efficacy in stroke patients. -Cognitive function enhancement: The program will improve cognitive function in stroke patients. -Improved visual perception: The virtual reality-based program will enhance visual perception in stroke patients. -Enhanced quality of life: The virtual reality-based cognitive rehabilitation program will improve health-related quality of life in stroke patients. |
| Pau et al., 2022 [199] | -Improved upper limb motor function: Immersive VR training improves upper limb motor function in people with Multiple Sclerosis. -Enhanced hand-to-mouth movement: Immersive VR training improves the speed and stability of hand-to-mouth movement in people with Multiple Sclerosis. |
| Paul et al., 2021 [200] | -Feasibility and acceptance: VR-enhanced behavioral activation (BA) is a feasible, acceptable, and tolerable treatment for major depressive disorder (MDD). -Clinical efficacy: VR-enhanced BA may have clinical efficacy in reducing depression severity compared to traditional BA and treatment as usual. |
| Paul et al., 2023 [201] | -Feasibility and efficacy: Extended reality behavioral activation (XR-BA) is feasible and efficacious in treating major depressive disorder (MDD). -Noninferiority to traditional BA: XR-BA is non-inferior to conventional behavioral activation (BA) in terms of efficacy. |
| Pearson et al., 2018 [202] | -Predicting treatment outcomes: ML models (elastic net and random forest) can predict treatment outcomes following an Internet intervention for depression. -Significant predictors: Certain variables, such as comorbid psychopathology and treatment credibility, are significant predictors of treatment response. |
| Piette et al., 2022 [203] | -Effectiveness through interactions: Investigating whether AI-CBT-CP (Artificial Intelligence Cognitive Behavioral Therapy—Collaborative Program) increases its effectiveness through patient interactions. -Optimization of reward function: Exploring whether AI-CBT-CP can optimize a reward function based on patient-reported outcomes. |
| Plencler et al., 2022 [204] | -Reduction in symptom severity: The VR-aided mindfulness intervention reduces symptom severity in psychotic patients. -Improved cognitive functioning: The VR-aided mindfulness intervention improves cognitive functioning in psychotic patients. |
| Porras-Garcia et al., 2021 [205] | -Enhanced treatment effectiveness: If a component of body exposure through VR (intensified by the illusion of virtual body ownership) is added to the usual treatment for anorexia nervosa (AN), the treatment will be more effective than the typical treatment alone. -Experimental group outcomes: The experimental group (AN-VR-BE + TAU) will show a significant increase in BMI values, alongside significant reductions in fear of gaining weight (FGW), other eating disorder (ED) symptomatology, and body-related attentional bias (AB), compared to the control group (TAU). |
| Price et al., 2022 [206] | -Prediction of symptom response: Unique baseline patient characteristics paired with ML would moderately predict individual symptom response to, engagement with, and sentiment toward A4i (a mental health intervention app). -Higher affective symptom response: Individuals with higher affective symptoms (e.g., depression) and lower psychotic symptoms would show the most robust use and response, resulting in more positive sentiment toward the app. -Interpersonal sensitivity impact: Persons with higher interpersonal sensitivity would demonstrate the strongest response to the intervention. |
| Raglio et al., 2019 [207] | -Predictive factors for relaxation: Certain factors, such as initial relaxation level, education and musical training, age, and frequency of music listening, can predict the relaxation effects of music listening. -ML for outcome prediction: ML techniques can effectively identify predictive factors for therapeutic music listening outcomes. |
| Raikwar et al., 2024 [208] | -Automation bias with imperfect cues: Imperfect visual cues in augmented reality systems lead to automation bias, negatively affecting search performance. -Improved performance with visual cues: Visual cues (whether perfect or imperfect) increase performance and shorten search times compared to no cues. |
| Rao et al., 2022 [209] | -Better storage and retrieval: The heterogeneous training condition will enable better storage and retrieval of salient instances compared to the difficult and sham conditions. -Performance improvement: Participants will perform better with heterogeneous and difficult training compared to the sham condition. -Long-term performance: Participants in the heterogeneous training condition will perform better on Day 8 compared to those in the sham condition. |
| Real et al., 2022 [210] | -Enhanced BHAG skills: A training curriculum using virtual reality (VR) simulations would enhance residents’ evidence-based skills related to behavioral health anticipatory guidance (BHAG). -Improved motivational interviewing skills: A VR-based training curriculum would improve residents’ skills in motivational interviewing (MI). |
| Richter et al., 2021 [211] | -Differentiation between anxiety and depression: An ML-based diagnostic support system can differentiate between anxiety and depression disorders. -Cognitive performance as a classifier: Cognitive performance patterns can be used to classify psychiatric disorders. -Classification success (anxiety/depression/mixed vs. control): The system can classify participants into anxiety, depression, mixed, or control groups with specific success rates. |
| Rutkowski et al., 2021 [212] | -Enhanced symptom reduction: The implementation of immersive virtual reality during a pulmonary rehabilitation program will lead to a more efficient reduction in symptoms of depression, anxiety, and stress levels. |
| Serino et al., 2017 [213] | -Improved mental frame syncing and spatial abilities: The VR-based training protocol will enhance “mental frame syncing” and improve general spatial abilities in patients with Alzheimer’s Disease. -Enhanced executive functioning: The VR-based training will have a significant effect on executive functioning in cognitively healthy elderly individuals. |
| Serrano-Vergel et al., 2023 [214] | -Suitability for anatomy training: The improved AR-based setup will be more suitable for anatomy training compared to the VR-based setup. |
| Shaw et al., 2019 [215] | -Symptom management and quality of life: VR can manage symptom burden and increase the quality of life for MS patients. -Feasibility and tolerability: VR is feasible and tolerable for use in MS patients. -Symptomatic benefits: VR can induce symptomatic benefits, particularly by improving positive affect and reducing negative affect. |
| Shiels et al., 2019 [216] | -Value in decision-making skills: Virtual reality simulation (VRS) is valuable for teaching decision-making skills to medical students. -Increased confidence: VRS increases students’ confidence levels more than case-based discussion (CBD). |
| Singh et al., 2020 [217] | -Knowledge development: VR improves student knowledge development. -Enhanced learning motivation: VR enhances learning motivation. -Positive cognitive impact: VR positively impacts cognition. |
| Smith et al., 2015 [218] | -Acceptability: Virtual Reality Job Interview Training (VR-JIT) is acceptable to veterans with PTSD. -Improved job interview skills: VR-JIT is efficacious for improving job interview skills in veterans with PTSD. -Increased self-confidence: VR-JIT is efficacious for improving self-confidence in veterans with PTSD. |
| Soboczenski et al., 2019 [219] | -Faster bias assessment: Semi-automation using RobotReviewer is quicker than manual assessment of bias in randomized controlled trials (RCTs). -Accurate ML suggestions: The ML system’s suggestions are accurate enough to be accepted by reviewers. -High usability: The RobotReviewer system is rated highly usable according to the System Usability Scale. |
| Sokołowska et al., 2024 [220] | -Clinical improvements with VR-based training: VR-based training will lead to beneficial improvements in clinical tests and posturographic trajectories in older women. -Effectiveness of VR balance training: Both balance–strength and balance–cognitive VR training will be effective in preventing balance loss and fall risk, potentially with different impacts. |
| Solcà et al., 2018 [221] | -Pain reduction with HEVR: HEVR reduces pain ratings in patients with CRPS. -Motor function improvement: HEVR improves motor limb function in patients with CRPS. -HRV modulation: HEVR modulates heart rate variability (HRV) as a physiologic pain marker in patients with CRPS. |
| Specht et al., 2023 [222] | -Cognitive improvement superiority: The VR serious game is hypothesized to be superior to conventional computerized cognitive training in improving cognitive abilities. -Patient-reported outcomes: The VR serious game is hypothesized to be superior in improving patient-reported outcomes, including quality of life and health state. -Transfer to daily life: The VR serious game is hypothesized to be superior in facilitating the transfer of learned abilities to daily life. |
| Stamou et al., 2021 [223] | -Clinical usefulness: The combination of CBT with VR is clinically useful for treating postnatal depression. -Effectiveness: The combination of CBT with VR is effective in treating postnatal depression. -Enhancement of awareness and decision making: VR can enhance awareness, decision making, and self-appreciation. |
| Stephenson et al., 2023 [224] | -Reduced time and cost: The AI/VR approach to e-CBT will decrease the overall time and cost commitment compared to the standard multi-professional healthcare decision-making team. |
| Syed et al., 2019 [225] | -Physical ability: Virtual reality therapy is more effective than conventional therapy in improving physical ability. -Mental health: Virtual reality therapy is more effective than conventional therapy in improving mental health by lowering depression, anxiety, and stress. -Self-esteem: Virtual reality therapy is more effective than conventional therapy in enhancing self-esteem. -Social support: Virtual reality therapy is more effective than conventional therapy in increasing social support. -Intrinsic motivation: Virtual reality therapy is more effective than conventional therapy in boosting intrinsic motivation, including task-based competence, choice, and interest. |
| Symons et al., 2019 [226] | -ML model accuracy: ML models are more accurate than clinical staff in predicting alcohol dependence treatment outcomes. -Adjunctive information: The best performing prediction models can provide useful adjunctive information to standard clinically available prognostic data. |
| Tacca et al., 2024 [227] | -VR-EEG therapy vs. Zoom counseling: The VR-EEG therapy system is as useful and functional in fostering restorativeness and a sense of presence as Zoom online counseling. -Efficacy in therapeutic alliance and mood improvement: The VR-EEG therapy system is as efficacious as Zoom online counseling in creating clients’ positive assessment of the therapeutic alliance, improving client mood-related symptoms of depression, increasing positivity, and producing positive client reactions to the counseling. |
| Tan et al., 2024 [228] | -AI-driven exercise: The AI-driven exercise prescription system will demonstrate greater effectiveness in improving mental health outcomes compared to standard exercise prescriptions. -Adherence and long-term outcomes: The AI-driven exercise prescription system will lead to better adherence and mental health outcomes over time compared to standard care. |
| Thapa et al., 2020 [229] | -Cognitive function improvement: The VR intervention program will improve cognitive function in older adults with mild cognitive impairment. -Brain function improvement: The VR intervention program will improve brain function in older adults with mild cognitive impairment. -Physical function improvement: The VR intervention program will improve physical function in older adults with mild cognitive impairment. |
| Thomas et al., 2020 [230] | -Workload reduction: The ML classifier can reduce the study identification workload for Cochrane Reviews. -Minimal risk of missing studies: The ML classifier can achieve this with minimal risk of missing relevant studies. |
| Tonacci et al., 2020 [231] | -ANS activity changes: A quick relaxation protocol using audio and video can lead to detectable changes in autonomic nervous system (ANS) activity. -ML discrimination: ML can effectively discriminate between individuals who benefit from the relaxation protocol and those who do not. -Wearable sensor detection: Wearable sensors can detect changes in ANS activity during the relaxation protocol. |
| Torpil et al., 2020 [232] | -Cognitive function improvement: A virtual reality-based rehabilitation program is effective in improving cognitive functions in older adults with mild cognitive impairment (MCI). |
| Tsai et al., 2018 [233] | -Triggering anxiety: VR and AR environments are equally capable of triggering anxiety in participants. -Claustrophobia treatment: VR and AR environments elicit fear of enclosed spaces effectively as a model for claustrophobia treatment. |
| Viczko et al., 2021 [234] | -Mood improvement with neurofeedback: Both groups will show reductions in negative mood states and increased positive mood states, with the addition of neurofeedback amplifying these effects. -Cortical activity changes: The AR + NF group will experience a larger change in cortical activity, as measured by pre-to-post resting-state EEG activity, compared to the AR-NF group. -Correlation between EEG and mood: EEG changes will correlate more strongly with mood changes for the AR + NF group compared to the AR-NF group. |
| Weerasinghe et al., 2022 [235] | -Effect of guidance amount: The fixed amount of guidance will lead to higher engagement and better learning outcomes compared to the adaptive amount of guidance. -Effect of guidance type: The adaptive-association guidance will result in greater engagement and improved learning outcomes compared to fixed-association guidance. |
| Winslow et al., 2022 [236] | -mHealth application with CBT: The combination of the mHealth application and CBT will significantly reduce anger and stress in active-duty service members. -Symptom reduction: The mHealth application will lead to significantly lower levels of anger, anxiety, depression, and PTSD symptoms following CBT treatment compared to standard CBT. |
| Wuang et al., 2021 [237] | -KBTS vs. TVPT for visual–motor integration: The kinesthetic game-based training system (KBTS) is more effective than traditional visual perceptual training (TVPT) in improving visual–motor integration. -KBTS vs. TVPT for visual perceptual functions: The KBTS is more effective than TVPT in enhancing overall visual perceptual functions in children with developmental delays. -KBTS vs. TVPT for school functions: The KBTS is more effective than TVPT in improving school functions in children with developmental delays. |
| Yang et al., 2022 [238] | -VRCT improves brain, cognitive, and physical functions in older adults with MCI. -Exercise training improves brain, cognitive, and physical functions in older adults with MCI. -There are differences in the effectiveness of VRCT and exercise training on brain, cognitive, and physical health. -Both VRCT and exercise training are more effective than no intervention (control group) in improving brain, cognitive, and physical health. |
| Yang et al., 2014 [239] | -VR training for cognitive recovery: VR training will help the recovery of cognitive function in brain tumor patients. -VR + cognitive rehabilitation vs. cognitive rehabilitation alone: The combination of VR training and computer-assisted cognitive rehabilitation is more effective than computer-assisted cognitive rehabilitation alone. |
| Yang and Wang, 2021 [240] | -The generative strategy will induce more emotions in the cognition process than viewing a continuous VR lesson. -Adding a generative strategy prompt to a VR lesson will increase positive ratings toward emotional self-regulation. -Students will have better learning outcomes when they use a generative strategy compared to viewing a VR lesson without it. |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Halkiopoulos, C.; Gkintoni, E. The Role of Machine Learning in AR/VR-Based Cognitive Therapies: A Systematic Review for Mental Health Disorders. Electronics 2025, 14, 1110. https://doi.org/10.3390/electronics14061110
Halkiopoulos C, Gkintoni E. The Role of Machine Learning in AR/VR-Based Cognitive Therapies: A Systematic Review for Mental Health Disorders. Electronics. 2025; 14(6):1110. https://doi.org/10.3390/electronics14061110
Chicago/Turabian StyleHalkiopoulos, Constantinos, and Evgenia Gkintoni. 2025. "The Role of Machine Learning in AR/VR-Based Cognitive Therapies: A Systematic Review for Mental Health Disorders" Electronics 14, no. 6: 1110. https://doi.org/10.3390/electronics14061110
APA StyleHalkiopoulos, C., & Gkintoni, E. (2025). The Role of Machine Learning in AR/VR-Based Cognitive Therapies: A Systematic Review for Mental Health Disorders. Electronics, 14(6), 1110. https://doi.org/10.3390/electronics14061110







