Improving Balance and Functional Status in Spinal Cord Injury Patients: A Systematic Review Comparing Virtual Reality-Based Therapy and Conventional Therapeutic Exercises
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Protocol and Register
2.2. Literature Search
2.3. Study Selection: Inclusion and Exclusion Criteria
2.4. Data Extraction
2.5. Variables
2.6. Methodological Quality Assessment
3. Results
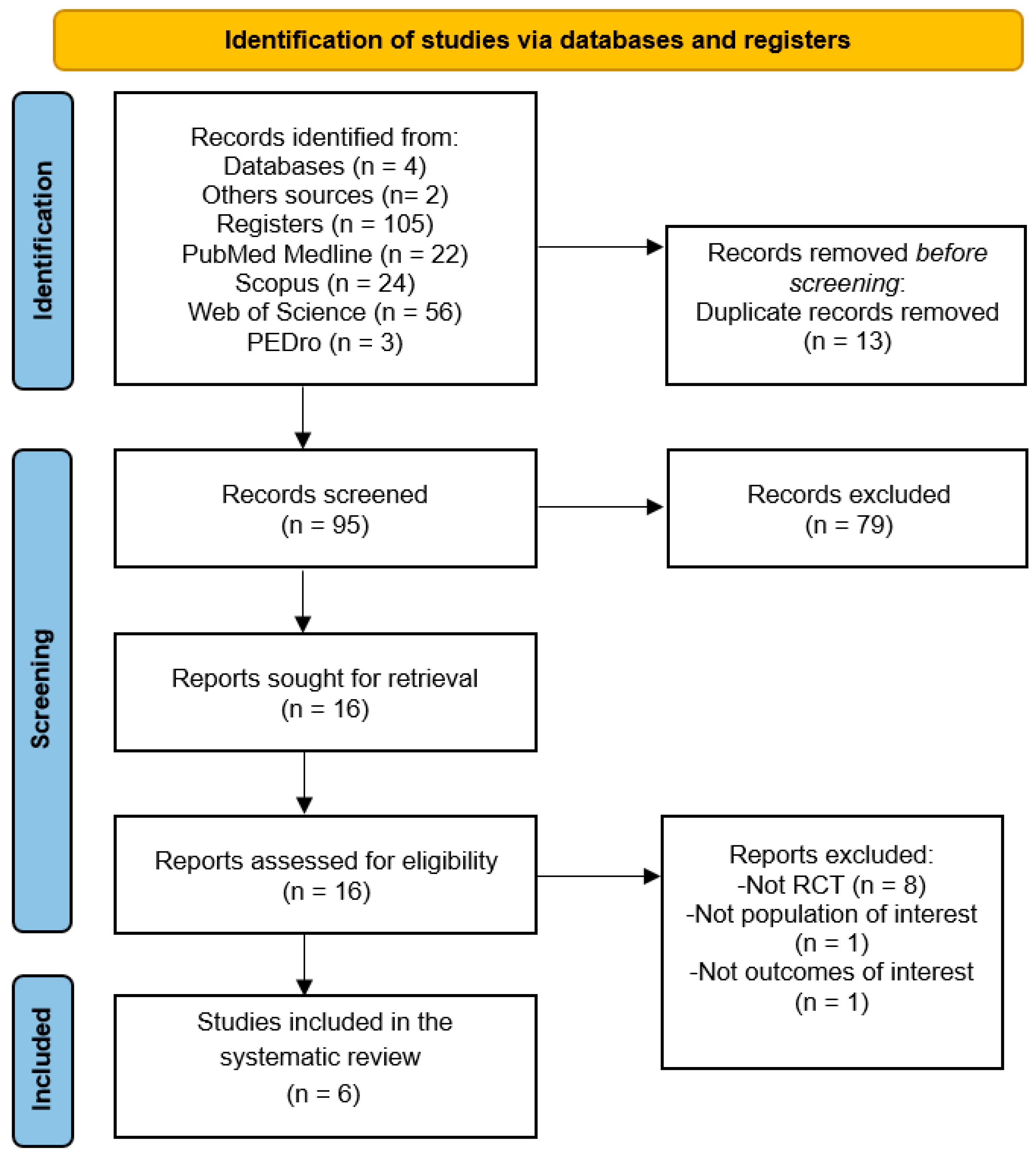
3.1. Study Selection
3.2. Characteristics of the Studies Included
3.3. Methodological Quality and Risk of Bias Assessment
3.4. Qualitative Findings
3.4.1. Postural Balance
3.4.2. Functional Status
3.4.3. Quality of Life
4. Discussion
5. Conclusions
Author Contributions
Funding
Data Availability Statement
Conflicts of Interest
References
- Anjum, A.; Yazid, M.D.; Daud, M.F.; Idris, J.; Hwei Ng, A.M.; Naicker, A.S.; Rashidah Ismail, O.H.; Kumar, R.K.A.; Lokanathan, Y. Spinal Cord Injury: Pathophysiology, Multimolecular Interactions, and Underlying Recovery Mechanisms. Int. J. Mol. Sci. 2020, 21, 7533. [Google Scholar] [CrossRef] [PubMed]
- Bennett, J.; Das, J.M.; Emmady, P.D. Spinal Cord Injuries; StatPearls Publishing: Treasure Island, FL, USA, 2022. [Google Scholar]
- Roberts, T.T.; Leonard, G.R.; Cepela, D.J. Classifications in Brief: American Spinal Injury Association (ASIA) Impairment Scale. Clin. Orthop. Relat. Res. 2017, 475, 1499. [Google Scholar] [CrossRef] [PubMed]
- Khan, F.I.; Ahmed, Z. Experimental Treatments for Spinal Cord Injury: A Systematic Review and Meta-Analysis. Cells 2022, 11, 3409. [Google Scholar] [CrossRef] [PubMed]
- Varma, A.K.; Das, A.; Wallace, G.; Barry, J.; Vertegel, A.A.; Ray, S.K.; Banik, N.L. Spinal Cord Injury: A Review of Current Therapy, Future Treatments, and Basic Science Frontiers. Neurochem. Res. 2013, 38, 895. [Google Scholar] [CrossRef] [PubMed]
- Fehlings, M.G.; Tetreault, L.A.; Wilson, J.R.; Kwon, B.K.; Burns, A.S.; Martin, A.R.; Hawryluk, G.; Harrop, J.S. A Clinical Practice Guideline for the Management of Acute Spinal Cord Injury: Introduction, Rationale, and Scope. Glob. Spine J. 2017, 7, 84S–94S. [Google Scholar] [CrossRef] [PubMed]
- Rouanet, C.; Reges, D.; Rocha, E.; Gagliardi, V.; Silva, G.S. Traumatic spinal cord injury: Current concepts and treatment update. Arq. NeuroPsiquiatria 2017, 75, 387–393. [Google Scholar] [CrossRef]
- Wirz, M.; van Hedel, H.J.A. Balance, gait, and falls in spinal cord injury. Handb. Clin. Neurol. 2018, 159, 367–384. [Google Scholar] [CrossRef] [PubMed]
- Krassioukov, A.; Elliott, S. Neural Control and Physiology of Sexual Function: Effect of Spinal Cord Injury. Top. Spinal Cord Inj. Rehabil. 2017, 23, 1–10. [Google Scholar] [CrossRef] [PubMed]
- Craggs, M.D. Pelvic somato-visceral reflexes after spinal cord injury: Measures of functional loss and partial preservation. Prog. Brain Res. 2006, 152, 205–219. [Google Scholar] [CrossRef]
- Sankari, A.; Vaughan, S.; Bascom, A.; Martin, J.L.; Badr, M.S. Sleep-Disordered Breathing and Spinal Cord Injury: A State-of-the-Art Review. Chest 2019, 155, 438–445. [Google Scholar] [CrossRef]
- Fitzpatrick, M.A.; Nwafo, N. Urinary Tract Infection Diagnostic and Management Considerations in People with Spinal Cord Injury and Neurogenic Bladder. Infect. Dis. Clin. N. Am. 2024, 38, 381–393. [Google Scholar] [CrossRef] [PubMed]
- DeVivo, M.J.; Chen, Y.; Wen, H. Cause of Death Trends Among Persons with Spinal Cord Injury in the United States: 1960–2017. Arch. Phys. Med. Rehabil. 2022, 103, 634–641. [Google Scholar] [CrossRef] [PubMed]
- Jendelova, P. Therapeutic Strategies for Spinal Cord Injury. Int. J. Mol. Sci. 2018, 19, 3200. [Google Scholar] [CrossRef] [PubMed]
- Lam, T.; Eng, J.J.; Wolfe, D.L.; Hsieh, J.T.C.; Whittaker, M. A systematic review of the efficacy of gait rehabilitation strategies for spinal cord injury. Top. Spinal Cord Inj. Rehabil. 2007, 13, 32–57. [Google Scholar] [CrossRef] [PubMed]
- Hachem, L.D.; Ahuja, C.S.; Fehlings, M.G. Assessment and management of acute spinal cord injury: From point of injury to rehabilitation. J. Spinal Cord Med. 2017, 40, 665. [Google Scholar] [CrossRef]
- Akkurt, H.; Karapolat, H.U.; Kirazli, Y.; Kose, T. The effects of upper extremity aerobic exercise in patients with spinal cord injury: A randomized controlled study. Eur. J. Phys. Rehabil. Med. 2017, 53, 219–227. [Google Scholar] [CrossRef] [PubMed]
- Mulroy, S.J.; Thompson, L.; Kemp, B.; Hatchett, P.P.; Newsam, C.J.; Lupold, D.G.; Haubert, L.L.; Eberly, V.; Ge, T.T.; Azen, S.P.; et al. Strengthening and optimal movements for painful shoulders (STOMPS) in chronic spinal cord injury: A randomized controlled trial. Phys. Ther. 2011, 91, 305–324. [Google Scholar] [CrossRef]
- He, D.; Cao, S.; Le, Y.; Wang, M.; Chen, Y.; Qian, B. Virtual Reality Technology in Cognitive Rehabilitation Application: Bibliometric Analysis. JMIR Serious Games 2022, 10, e38315. [Google Scholar] [CrossRef]
- Jack, D.; Boian, R.; Merians, A.S.; Tremaine, M.; Burdea, G.C.; Adamovich, S.V.; Recce, M.; Poizner, H. Virtual reality-enhanced stroke rehabilitation. IEEE Trans. Neural Syst. Rehabil. Eng. 2001, 9, 308–318. [Google Scholar] [CrossRef]
- Baus, O.; Bouchard, S. Moving from Virtual Reality Exposure-Based Therapy to Augmented Reality Exposure-Based Therapy: A Review. Front. Hum. Neurosci. 2014, 8, 112. [Google Scholar] [CrossRef]
- Maples-Keller, J.L.; Bunnell, B.E.; Kim, S.J.; Rothbaum, B.O. The use of virtual reality technology in the treatment of anxiety and other psychiatric disorders. Harv. Rev. Psychiatry 2017, 25, 103. [Google Scholar] [CrossRef] [PubMed]
- Sveistrup, H. Motor rehabilitation using virtual reality. J. Neuroeng. Rehabil. 2004, 1, 10. [Google Scholar] [CrossRef] [PubMed]
- De Araújo, A.V.L.; Neiva, J.F.D.O.; Monteiro, C.B.D.M.; Magalhães, F.H. Efficacy of Virtual Reality Rehabilitation after Spinal Cord Injury: A Systematic Review. BioMed Res. Int. 2019, 2019, 7106951. [Google Scholar] [CrossRef] [PubMed]
- De Miguel-Rubio, A.; Rubio, M.D.; Alba-Rueda, A.; Salazar, A.; Moral-Munoz, J.A.; Lucena-Anton, D. Virtual Reality Systems for Upper Limb Motor Function Recovery in Patients with Spinal Cord Injury: Systematic Review and Meta-Analysis. JMIR mhealth uhealth 2020, 8, e22537. [Google Scholar] [CrossRef] [PubMed]
- Yeo, E.; Chau, B.; Chi, B.; Ruckle, D.E.; Ta, P. Virtual Reality Neurorehabilitation for Mobility in Spinal Cord Injury: A Structured Review. Innov. Clin. Neurosci. 2019, 16, 13. [Google Scholar] [PubMed]
- Villiger, M.; Bohli, D.; Kiper, D.; Pyk, P.; Spillmann, J.; Meilick, B.; Curt, A.; Hepp-Reymond, M.C.; Hotz-Boendermaker, S.; Eng, K. Virtual reality-augmented neurorehabilitation improves motor function and reduces neuropathic pain in patients with incomplete spinal cord injury. Neurorehabilit. Neural Repair 2013, 27, 675–683. [Google Scholar] [CrossRef] [PubMed]
- Sayenko, D.G.; Alekhina, M.I.; Masani, K.; Vette, A.H.; Obata, H.; Popovic, M.R.; Nakazawa, K. Positive effect of balance training with visual feedback on standing balance abilities in people with incomplete spinal cord injury. Spinal Cord 2010, 48, 886–893. [Google Scholar] [CrossRef] [PubMed]
- Roosink, M.; Robitaille, N.; Jackson, P.L.; Bouyer, L.J.; Mercier, C. Interactive virtual feedback improves gait motor imagery after spinal cord injury: An exploratory study. Restor. Neurol. Neurosci. 2016, 34, 227–235. [Google Scholar] [CrossRef] [PubMed]
- Jordan, M.; Richardson, E.J. Effects of Virtual Walking Treatment on Spinal Cord Injury-Related Neuropathic Pain: Pilot Results and Trends Related to Location of Pain and at-level Neuronal Hypersensitivity. Am. J. Phys. Med. Rehabil. 2016, 95, 390–396. [Google Scholar] [CrossRef]
- Gaffurini, P.; Bissolotti, L.; Calza, S.; Calabretto, C.; Orizio, C.; Gobbo, M. Energy metabolism during activity-promoting video games practice in subjects with spinal cord injury: Evidences for health promotion. Eur. J. Phys. Rehabil. Med. 2013, 49, 23–29. [Google Scholar]
- Hasnan, N.; Engkasan, J.P.; Husain, R.; Davis, G.M. High-Intensity Virtual-reality Arm plus FES-leg Interval Training in Individuals with Spinal Cord Injury. Biomed. Tech. 2013, 58 (Suppl. S1), 000010151520134028. [Google Scholar] [CrossRef]
- Hodgkiss, D.D.; Bhangu, G.S.; Lunny, C.; Jutzeler, C.R.; Chiou, S.-Y.; Walter, M.; Lucas, S.J.E.; Krassioukov, A.V.; Nightingale, T.E. Exercise and aerobic capacity in individuals with spinal cord injury: A systematic review with meta-analysis and meta-regression. PLoS Med. 2023, 20, e1004082. [Google Scholar] [CrossRef]
- Nepomuceno, P.; Souza, W.H.; Pakosh, M.; Musselman, K.E.; Craven, B.C. Exoskeleton-based exercises for overground gait and balance rehabilitation in spinal cord injury: A systematic review of dose and dosage parameters. J. Neuroeng. Rehabil. 2024, 21, 73. [Google Scholar] [CrossRef]
- Park, J.; Kim, J.; Eun, S.-D.; Kang, D. Effectiveness of Exercise Programs for Alleviation of Upper Body Pain in Patients with Spinal Cord Injury: A Systematic Review. J. Clin. Med. 2024, 13, 3066. [Google Scholar] [CrossRef] [PubMed]
- Ponzano, M.; Buren, R.; Adams, N.T.; Jun, J.; Jetha, A.; Mack, D.E.; Ginis, K.A.M. Effect of Exercise on Mental Health and Health-related Quality of Life in Adults with Spinal Cord Injury: A Systematic Review and Meta-Analysis. Arch. Phys. Med. Rehabil. 2024. ahead of print. [Google Scholar] [CrossRef]
- Abou, L.; Malala, V.D.; Yarnot, R.; Alluri, A.; Rice, L.A. Effects of Virtual Reality Therapy on Gait and Balance Among Individuals with Spinal Cord Injury: A Systematic Review and Meta-analysis. Neurorehabilit. Neural Repair 2020, 34, 375–388. [Google Scholar] [CrossRef]
- Walia, S.; Kumar, P.; Kataria, C. Interventions to Improve Standing Balance in Individuals with Incomplete Spinal Cord Injury: A Systematic Review and Meta-Analysis. Top. Spinal Cord Inj. Rehabil. 2023, 29, 56–83. [Google Scholar] [CrossRef]
- De Miguel-Rubio, A.; Rubio, M.D.; Salazar, A.; Moral-Munoz, J.A.; Requena, F.; Camacho, R.; Lucena-Anton, D. Is Virtual Reality Effective for Balance Recovery in Patients with Spinal Cord Injury? A Systematic Review and Meta-Analysis. J. Clin. Med. 2020, 9, 2861. [Google Scholar] [CrossRef] [PubMed]
- Page, M.J.; McKenzie, J.E.; Bossuyt, P.M.; Boutron, I.; Hoffmann, T.C.; Mulrow, C.D.; Shamseer, L.; Tetzlaff, J.M.; Akl, E.A.; Brennan, S.E.; et al. The PRISMA 2020 statement: An updated guideline for reporting systematic reviews. BMJ 2021, 372, n71. [Google Scholar] [CrossRef] [PubMed]
- Higgins, J.P.T.; Green, S. Cochrane Handbook for Systematic Reviews of Intervention Version 5.1.0 [Updated March 2011]; The Cochrane Collaboration: London, UK, 2011. [Google Scholar]
- Amir-Behghadami, M.; Janati, A. Population, Intervention, Comparison, Outcomes and Study (PICOS) design as a framework to formulate eligibility criteria in systematic reviews. Emerg. Med. J. 2020, 37, 387. [Google Scholar] [CrossRef]
- Horak, F.B. Postural orientation and equilibrium: What do we need to know about neural control of balance to prevent falls? Age Ageing 2006, 35 (Suppl. S2), ii7–ii11. [Google Scholar] [CrossRef]
- Ustün, T.B.; Chatterji, S.; Kostansjek, N.; Bickenbach, J. WHO’s ICF and functional status information in health records. Health Care Financ. Rev. 2003, 24, 77–88. [Google Scholar]
- Maher, C.G.; Sherrington, C.; Herbert, R.D.; Moseley, A.M.; Elkins, M. Reliability of the PEDro scale for rating quality of randomized controlled trials. Phys. Ther. 2003, 83, 713–721. [Google Scholar] [CrossRef]
- Moseley, A.M.; Herbert, R.D.; Sherrington, C.; Maher, C.G. Evidence for physiotherapy practice: A survey of the Physiotherapy Evidence Database (PEDro). Aust. J. Physiother. 2002, 48, 43–49. [Google Scholar] [CrossRef]
- Macedo, L.G.; Elkins, M.R.; Maher, C.G.; Moseley, A.M.; Herbert, R.D.; Sherrington, C. There was evidence of convergent and construct validity of Physiotherapy Evidence Database quality scale for physiotherapy trials. J. Clin. Epidemiol. 2010, 63, 920–925. [Google Scholar] [CrossRef]
- Lee, M.J.; Lee, S.M. The Effect of Virtual Reality Exercise Program on Sitting Balance Ability of Spinal Cord Injury Patients. Healthcare 2021, 9, 183. [Google Scholar] [CrossRef]
- Manzanares, A.; Camblor, Á.; Romero-Arenas, S.; Segado, F.; Gil-Arias, A. Effect of a semi-immersive virtual reality navigation therapy on quality of life in persons with spinal cord injury. Disabil. Rehabil. Assist. Technol. 2023, 18, 730–735. [Google Scholar] [CrossRef]
- Dimbwadyo-Terrer, I.; Trincado-Alonso, F.; de los Reyes-Guzmán, A.; Aznar, M.A.; Alcubilla, C.; Pérez-Nombela, S.; del Ama-Espinosa, A.; Polonio-López, B.; Gil-Agudo, Á. Upper limb rehabilitation after spinal cord injury: A treatment based on a data glove and an immersive virtual reality environment. Disabil. Rehabil. Assist. Technol. 2016, 11, 462–467. [Google Scholar] [CrossRef]
- Nair, M.S.; Kulkarni, V.N.; Shyam, A.K. Combined Effect of Virtual Reality Training (VRT) and Conventional Therapy on Sitting Balance in Patients with Spinal Cord Injury (SCI): Randomized Control Trial. Neurol. India 2022, 70, S245–S250. [Google Scholar] [CrossRef]
- Khurana, M.; Walia, S.; Noohu, M.M. Study on the effectiveness of virtual reality game-based training on balance and functional performance in individuals with paraplegia. Top. Spinal Cord Inj. Rehabil. 2017, 23, 263–270. [Google Scholar] [CrossRef]
- An, Y.; Park, C. The effects of virtual soccer game on balance, gait function, and kick speed in chronic incomplete spinal cord injury: A randomized controlled trial. Spinal Cord 2022, 60, 504–509. [Google Scholar] [CrossRef]
- Sandrow-Feinberg, H.R.; Houlé, J.D. Exercise after Spinal Cord Injury as an Agent for Neuroprotection, Regeneration and Rehabilitation. Brain Res. 2015, 1619, 12. [Google Scholar] [CrossRef]
- Wouda, M.F.; Løtveit, M.F.; Bengtson, E.I.; Strøm, V. The relationship between balance control and thigh muscle strength and muscle activity in persons with incomplete spinal cord injury. Spinal Cord Ser. Cases 2024, 10, 7. [Google Scholar] [CrossRef]
- Edgerton, V.R.; Courtine, G.; Gerasimenko, Y.P.; Lavrov, I.; Ichiyama, R.M.; Fong, A.J.; Cai, L.L.; Otoshi, C.K.; Tillakaratne, N.J.K.; Burdick, J.W.; et al. Training Locomotor Networks. Brain Res. Rev. 2008, 57, 241. [Google Scholar] [CrossRef]
- Fouad, K.; Pedersen, V.; Schwab, M.E.; Brösamle, C. Cervical sprouting of corticospinal fibers after thoracic spinal cord injury accompanies shifts in evoked motor responses. Curr. Biol. 2001, 11, 1766–1770. [Google Scholar] [CrossRef]
- Lee, J.K.; Johnson, C.S.; Wrathall, J.R. Up-regulation of 5-HT2 receptors is involved in the increased H-reflex amplitude after contusive spinal cord injury. Exp. Neurol. 2007, 203, 502. [Google Scholar] [CrossRef]
- Santos, L.V.; Pereira, E.T.; Reguera-García, M.M.; de Oliveira, C.E.P.; Moreira, O.C. Resistance Training and Muscle Strength in people with Spinal cord injury: A systematic review and meta-analysis. J. Bodyw. Mov. Ther. 2022, 29, 154–160. [Google Scholar] [CrossRef]
- Leemhuis, E.; Esposito, R.M.; De Gennaro, L.; Pazzaglia, M. Go Virtual to Get Real: Virtual Reality as a Resource for Spinal Cord Treatment. Int. J. Environ. Res. Public Health 2021, 18, 1819. [Google Scholar] [CrossRef]
- Noamani, A.; Lemay, J.-F.; Musselman, K.E.; Rouhani, H. Characterization of standing balance after incomplete spinal cord injury: Alteration in integration of sensory information in ambulatory individuals. Gait Posture 2021, 83, 152–159. [Google Scholar] [CrossRef]
- Alashram, A.R.; Padua, E.; Hammash, A.K.; Lombardo, M.; Annino, G. Effectiveness of virtual reality on balance ability in individuals with incomplete spinal cord injury: A systematic review. J. Clin. Neurosci. 2020, 72, 322–327. [Google Scholar] [CrossRef]
- De Miguel-Rubio, A.; Muñoz-Pérez, L.; Alba-Rueda, A.; Arias-Avila, M.; Rodrigues-de-Souza, D.P. A Therapeutic Approach Using the Combined Application of Virtual Reality with Robotics for the Treatment of Patients with Spinal Cord Injury: A Systematic Review. Int. J. Environ. Res. Public Health 2022, 19, 8772. [Google Scholar] [CrossRef]
- Edgerton, V.R.; Tillakaratne, N.J.K.; Bigbee, A.J.; De Leon, R.D.; Roy, R.R. Plasticity of the spinal neural circuitry after injury. Annu. Rev. Neurosci. 2004, 27, 145–167. [Google Scholar] [CrossRef]
- Murakami, F.; Song, W.J.; Katsumaru, H. Plasticity of neuronal connections in developing brains of mammals. Neurosci. Res. 1992, 15, 235–253. [Google Scholar] [CrossRef]
- Fouad, K.; Tetzlaff, W. Rehabilitative training and plasticity following spinal cord injury. Exp. Neurol. 2012, 235, 91–99. [Google Scholar] [CrossRef]
- Vaynman, S.; Ying, Z.; Gomez-Pinilla, F. Interplay between brain-derived neurotrophic factor and signal transduction modulators in the regulation of the effects of exercise on synaptic-plasticity. Neuroscience 2003, 122, 647–657. [Google Scholar] [CrossRef]
- Gray, N.; Shaikh, J.; Cowley, A.; Goosey-Tolfrey, V.; Logan, P.; Quraishi, N.; Booth, V. The effect of early mobilisation (<14 days) on pathophysiological and functional outcomes in animals with induced spinal cord injury: A systematic review with meta-analysis. BMC Neurosci. 2024, 25, 20. [Google Scholar] [CrossRef]
- Bargeri, S.; Scalea, S.; Agosta, F.; Banfi, G.; Corbetta, D.; Filippi, M.; Sarasso, E.; Turolla, A.; Castellini, G.; Gianola, S. Effectiveness and safety of virtual reality rehabilitation after stroke: An overview of systematic reviews. eClinicalMedicine 2023, 64, 102220. [Google Scholar] [CrossRef]
- Anneken, V.; Hanssen-Doose, A.; Hirschfeld, S.; Scheuer, T.; Thietje, R. Influence of physical exercise on quality of life in individuals with spinal cord injury. Spinal Cord 2010, 48, 393–399. [Google Scholar] [CrossRef]
| Database | Search Strategy |
|---|---|
| PubMed Medline | (spinal cord injuries[mh] OR spinal cord injur*[tiab]) AND (virtual reality[mh] OR virtual reality[tiab] OR virtual reality exposure therapy[mh] OR virtual reality exposure therapy[tiab] OR non-immersive virtual reality[tiab] OR immersive virtual reality[tiab] OR semi-immersive virtual reality[tiab] OR video games[mh] OR video game*[tiab] OR serious gam*[tiab] OR exergam*[tiab]) AND (exercise therapy[mh] or exercise therapy[tiab]) |
| SCOPUS | (TITLE-ABS-KEY ((“spinal cord injuries”)) AND TITLE-ABS-KEY ((“virtual reality” OR “virtual reality exposure therapy” OR “non-immersive virtual reality” OR “immersive virtual reality” OR “semi-immersive virtual reality” OR “video games” OR “serious games” OR “exercises”)) AND TITLE-ABS-KEY ((“exercise therapy”))) |
| Web of Science | (*spinal cord injury*) AND (*virtual reality* OR *virtual reality exposure therapy* OR *non-immersive virtual reality* OR *immersive virtual reality* OR *semi-immersive virtual reality* OR *video games* OR *serious games* OR *exergames*) AND (*exercise therapy*) |
| PEDro | Spinal Cord Injury AND Virtual Reality |
| Study | Study Design | Sample | VRBT Group | Control Group | Variables | Qualitative Findings |
|---|---|---|---|---|---|---|
| Lee and Lee, 2021 [48] (South Korea) | Single-blind RCT | Twenty patients (13M:7F) 54.4 ± 8 years old Thoracic and lumbar SCI (ASIA: C, D) 16.9 months since diagnosis | Ten patients (55.1 years old) VR balance training for 30 min (five sessions per week for 8 weeks) using Bio Rescue, plus 30 min of occupational therapy exercises | Ten patients (53.7 years old) Balance therapeutic exercise in sitting position and unstable surfaces (30 min, five sessions per week for 8 weeks) | Sitting balance for left side (FSA) | Significant intragroup improvement for VRBT and control groups (p = 0.011). Statistically significant improvements favor VRBT (p = 0.036) |
| Sitting balance for right side (FSA) | Significant intragroup improvement for VRBT (p = 0.037). Statistically significant improvements favor VRBT (p = 0.027) | |||||
| Dynamic balance (LOS) | Significant intragroup improvement for VRBT (p < 0.001) and control (p = 0.001) group. Statistically significant improvements favor VRBT (p = 0.048) | |||||
| Manzanares et al., 2023 [49] (Spain) | Not blind RCT | Eleven patients (7M:4F) 42.3 ± 13 years old <T1 SCI (ASIA: A, C, D) 5.2 months since diagnosis | Six patients (42.3 years old) Semi-immersive VR-based exercises (30–40 min, three times per week for 6 weeks), plus strength and mobility exercise program (five days per week) | Ten patients (42.4 years old) Strength and mobility therapeutic exercises (five days per week) | Functional status (SCIM) | No statistically significant differences in VRBT (p = 0.278) and control group (p = 0.376). No statistically significant differences between groups (p > 0.05) |
| Balance (MFRT) | Statistically significant differences in VRBT (p = 0.011). No statistically significant differences between groups (p > 0.05) | |||||
| Quality of life (SCI QL-23) | No statistically significant differences pre–post in VRBT (p = 0.092) and control group (p = 0.619). No statistically significant differences between groups (p > 0.05) | |||||
| Dimbwadyo-Terrer et al., 2016 [50] (Spain) | Not blind RCT | Nine patients (7M:2F) 49.2 ± 7.2 years old Cervical and thoracic SCI (ASIA: A, D) >12 months | Six patients (54.3 years old) Immersive VR-based exercises in the upper limb using CyberGlove® (twice per week for 2 weeks), plus conventional rehabilitation | Three patients (44.2 years old) Balance exercises and mobilizations (twice per week for 2 weeks). | Functional status (SCIM) | No statistically significant differences between groups (p = 0.71) |
| Nair et al., 2022 [51] (India) | Double-blind RCT | Twenty-one patients (13M:8F) 31.3 ± 7.5 years old ≤T10 SCI (ASIA: A, B) | Eleven patients (32.5 years old) Non-immersive VR-based balance exercises with Xbox plus Kinect (30 min, three times per week for 4 weeks), plus conventional rehabilitation program | Ten patients (30.1 years old) Physiotherapy plus balance training exercises (30 min, three times per week for 4 weeks) | Balance (MFRT and t-shirt test) | Statistically significant intragroup improvement for VRBT (p < 0.001) and control (p < 0.05) group. No statistically significant differences between groups (p = 0.085) |
| Khurana et al., 2017 [52] (India) | Not blind RCT | Thirty patients (28M:2F) 29.6 ± 7.3 years old, complete T6-T12 SCI (ASIA: A, B) >6 months | Fifteen patients (29.5 years old) Non-immersive VR-based exercises using PlayStation 2 and Eye Toy (45 min, five times per week for 4 weeks), plus conventional balance exercises | Fifteen patients (29.8 years old) Physiotherapy plus balance exercises (45 min, five times per week for 4 weeks) | Balance (MFRT and t-shirt test) | Significant intragroup improvement for VRBT (p = 0.05). Statistically significant differences between groups favor VRBT (p = 0.001) |
| Functional status (SCIM) | Statistically significant differences between groups favor VRBT (p = 0.001) | |||||
| An and Park, 2022 [53] (South Korea) | Single-blind RCT | Forty patients (23M:17F) 42.6 ± 6.1 years old C5-C6 SCI (ASIA: C, D) >12 months | Twenty patients (42.3 years old) Immersive VR-based lower limb (30 min, three times per week for 4 weeks) | Twenty patients (43 years old) Lower limb extension exercises (30 min, three times per week for 4 weeks) | Balance (CST and TUG) | Significant intragroup improvement for VRBT (p = 0.01) and control (p = 0.02) group. Statistically significant differences between groups favor VRBT group (p = 0.03 and p = 0.04) |
| Functional status (10 MWT) | Significant intragroup improvement for VRBT (p = 0.01) and control (p = 0.02) group. Statistically significant differences between groups favor VRBT group (p = 0.03) |
| Study | I1 | I2 | I3 | I4 | I5 | I6 | I7 | I8 | I9 | I10 | I11 | Total Score | Quality |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Lee and Lee, 2021 [48] | Y | Y | N | Y | N | N | Y | Y | Y | Y | Y | 7/10 | Good |
| Manzanares et al., 2023 [49] | Y | Y | N | Y | N | N | N | N | N | Y | Y | 4/10 | Moderate |
| Dimbwadyo-Terrer et al., 2016 [50] | Y | Y | N | N | N | N | N | N | N | Y | Y | 3/10 | Low |
| Nair et al., 2022 [51] | Y | Y | N | Y | Y | N | Y | Y | N | Y | Y | 7/10 | Good |
| Khurana et al., 2017 [52] | Y | Y | N | Y | N | N | N | Y | Y | Y | Y | 6/10 | Good |
| An and Park, 2022 [53] | Y | Y | N | Y | N | N | N | N | N | Y | Y | 4/10 | Low |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Obrero-Gaitán, E.; López-Nájera, L.; Piñar-Lara, M.; Ibancos-Losada, M.d.R.; Cortés-Pérez, I.; García-López, H. Improving Balance and Functional Status in Spinal Cord Injury Patients: A Systematic Review Comparing Virtual Reality-Based Therapy and Conventional Therapeutic Exercises. Electronics 2024, 13, 2594. https://doi.org/10.3390/electronics13132594
Obrero-Gaitán E, López-Nájera L, Piñar-Lara M, Ibancos-Losada MdR, Cortés-Pérez I, García-López H. Improving Balance and Functional Status in Spinal Cord Injury Patients: A Systematic Review Comparing Virtual Reality-Based Therapy and Conventional Therapeutic Exercises. Electronics. 2024; 13(13):2594. https://doi.org/10.3390/electronics13132594
Chicago/Turabian StyleObrero-Gaitán, Esteban, Luis López-Nájera, Marina Piñar-Lara, María del Rocío Ibancos-Losada, Irene Cortés-Pérez, and Héctor García-López. 2024. "Improving Balance and Functional Status in Spinal Cord Injury Patients: A Systematic Review Comparing Virtual Reality-Based Therapy and Conventional Therapeutic Exercises" Electronics 13, no. 13: 2594. https://doi.org/10.3390/electronics13132594
APA StyleObrero-Gaitán, E., López-Nájera, L., Piñar-Lara, M., Ibancos-Losada, M. d. R., Cortés-Pérez, I., & García-López, H. (2024). Improving Balance and Functional Status in Spinal Cord Injury Patients: A Systematic Review Comparing Virtual Reality-Based Therapy and Conventional Therapeutic Exercises. Electronics, 13(13), 2594. https://doi.org/10.3390/electronics13132594








