Abstract
Personal Emergency Response Systems (PERSs) are fall-detection devices supporting users in any situation. No previous studies have investigated the differences in events and the use of PERS between users financially supported by public authorities (public users) and those who privately afford the PERS cost (private users). More than two years of data collected by the Telemergency Operation Centre (TOC) were downloaded. All users who sent at least one real alert to request support were included. No differences were found for falls (37, 16.7% vs. 95, 13.4%) and medical problems (46, 20.7% vs. 122, 17.2%). The dispatch of an ambulance was necessary for all medical problems, while for falls, this was only in half of cases. Public users significantly asked more for service demand, while private users asked for support calls. The TOC staff directly managed most of the service demands (398, 97.3%) and support calls. PERS could be a valid instrument for promoting independent living and helping manage chronic conditions in older adults. The results suggest that PERSs might improve in-home care services, facilitating the connection to in-home services.
1. Introduction
Personal Emergency Response Systems (PERSs) are fall-detection devices born at the end of the 1970s. These devices can be worn around the neck or wrist and, besides distinguishing falls from the activities of daily living, they can activate rescue systems that can quickly intervene in case of falls [1,2,3]. In this study, PERSs are characterised by three essential elements: (a) a red button to call to, (b) a 24 h emergency response centre, and (c) a home communication system [2,3]. The alert can also be directly sent to a nominated contact, such as a caregiver [2,3]. PERSs can be purchased, leased, or rented; in many cases, the costs of the service are not covered by health insurance [2,3].
Over the years, these devices have been integrated with numerous features, including vital signs detection or machine learning systems, making it possible to detect information on gait, gait speed, and acceleration, which are all predictors of falling [4]. Compared with other technologies, PERS remains the most marketed fall detection device due to its reliability, ease of use, ease of control, and affordability [5,6]. Some evidence has reported that PERSs increase older adults’ confidence [7], feelings of safety [5,6,7], and independence [5,8], which contributes to the well-accepted use of this technology [5,6]. One possible explanation for their use is the balance they provide between maintaining the person’s freedom and the early identification of falls. In fact, according to the guidelines of the Ontario Registered Nurses Association [1], family members, caregivers, and health care providers can inadvertently limit the person’s independence when focusing on fall-prevention measures [9].
Few studies have underlined the capacity of PERS to provide a rapid rescue, with positive outcomes on ED admissions, hospitalisations, and hospital stay [10,11,12]. Moreover, PERS contributes to avoiding ambulance intervention, with a potential annual cost of AUD 76.8 per person per year [13]. Two cost-saving mechanisms exist: an intermediate assessment by the operations centre of the user’s conditions and the possibility of contacting a reference person. Thus, the operation centre may quickly identify minor events, activating the caregiver or, whether not present, district services to treat the person at home, also avoiding an ambulance intervention [13].
Technology in the real world is often used differently and for different purposes than originally intended [14]. Even if PERSs were initially developed for the rapid detection of falls, observational studies showed that almost half of the alerts involved physical or psychological symptoms (medical alerts), such as dyspnoea, severe pain, or heart problems [12,15,16]. Medical alerts ranged from 41% to 45.7% of the total alerts sent by users, requiring, more often than falls, an ambulance [12,15,16,17]. PERSs are also used by older adults for requests of transportation, medications, and nursing care (non-medical alerts) [7,16]. However, published studies often do not report on these alerts [7,12,15,16,17,18,19].
The analysis of non-medical alerts would allow a more in-depth understanding of the needs of users and their caregivers, fostering a reflection upon the best future strategies to further develop PERSs and integrate them into community care [14]. The necessity to integrate technologies in home-care services, allowing distance monitoring and care, was well underlined during the COVID-19 pandemic. After an initial use of telemedicine or telenursing systems primarily to minimise the transmission of the virus during the pandemic [20], the role of telecare was exploited in the care and treatment of people in rural areas and those with limited access to health facilities [20,21]. Evidence was produced of a reduction in resources used in health facilities, yet with improved access to care, especially in older adults, through electronic devices [20,22,23].
A better shaping of users’ profiles is another important aspect for PERSs’ improved use in home-care services. PERS users may not share the same characteristics, as we may identify those who receive the service from a public authority or financial support to partially or fully cover its costs (public users) or those who privately sustained the cost of the PERS (private users) or those who do not use the PERS (non-purchasers) [7,12,15,16]. Most studies focus only on one of these groups of users.
Despite the numerous benefits, the main reasons not to purchase a PERS are the cost and the lack of a caregiver for contact in case of emergencies. The cost of the device is rarely reported but amounts to approximately AUD 600 for equipment and installation, with a monthly fee of AUD 19 [15]. Health insurance often does not cover these costs. The main users of PERS are women older than 85, living alone but with family support, with one or more comorbidities [12,18,24]. Offering the device only to those who live alone or lack health insurance coverage excludes a portion of the population that could benefit from this device but who either cannot afford the cost or, although frail, do not live alone.
To our knowledge, no article highlighted the differences in the need and use of the device between public and private users. These elements would help policymakers develop policies to promote equitable access to obtaining a PERS for older adults, or those with difficulties in accessing health services. The acknowledgement of the benefits of PERS could promote a revision of the criteria for the subsidy of these devices, possibly expanding their provision and broadening the coverage of the costs of the service [15].
The present study aims to highlight the differences in the use of PERSs (type and number of user requests, supportive calls, and medical alerts) between those who privately afford the cost of the telemergency system offered by Ass.I.S.Te Cooperative (Ass.I.S.Te from now on) (private users) and those who are financially supported by a public authority (public users).
2. Materials and Methods
This is a cross-sectional study conducted at the Telemergency Operation Centre (TOC), located at Ville Roddolo Nursing Home (Moncalieri, Northern Italy), between 1 December 2020 and 31 March 2023.
2.1. Setting of the Study
The telemergency service offered by for-profit agency Ass.I.S.Te aims to promote independent living at home to aged or frail people using PERSs. Users can be monitored in and out of the house, and the service is active for over twenty-four hours.
The service can be purchased by single users or public authorities, such as social services.
The public authority sustains the cost of device installation and the monthly fee for users with special health and non-health conditions (i.e., depression, loneliness, grief, etc.) with an income not exceeding EUR 850 per month or may ask for a partial contribution if the income is up to EUR 1100 per month. For private purchasers, the cost of the Telemergency service includes a monthly fee of EUR 25, plus the cost of activation and installation of the PERS (EUR 50 to 100 according to indoor-only monitoring, outdoor monitoring, or both) and a deposit (EUR 100). The user purchases the SIM card.
The user may choose between two types of PERS: indoor devices equipped with radio transmitters and connected to wearable devices around the neck or wrist; an outdoor device equipped with a Global Positioning System (GPS), which can be clipped to the belt or watch. All the PERSs are of the third generation: they are embedded with sensors (i.e., an accelerometer and a gyroscope) designed to automatically identify a fall or a high impact with a hard surface. Following an impact, the fall detection system evaluates the change in height and rotation of the device, as well as if the user is on the ground. The remote control, wearable on the wrist or neck, has a survival control function and a micro-movement sensor. It can send an automatic alert in cases of no motion for a pre-defined time (in days or hours), allowing the system to know whether the user is wearing it.
An alert can be automatically generated by the device (i.e., in case of a fall) or by the user by pressing a button. Each PERS is equipped with a small radio transmitter that allows easy communication with the TOC staff after activating an alert: if the user is on the floor after a fall, the PERS allows the user to talk with the staff. In cases of false alerts, the automatic call forwarding system can be turned off in indoor devices by pressing the green button within 15 s, while in outdoor devices, this occurs if the fallen person rises within 15 s from the impact.
All alerts are managed by the lay staff of the TOC (Figure 1).
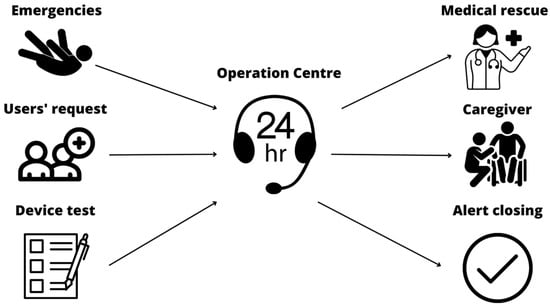
Figure 1.
Alert management of the Telemergency Operation Centre.
The staff can display the user’s data on the screen (including the type of device), the date and time of alert dispatch, and the PERS code. The device can assign up to 31 codes (i.e., general alert, fall, medical alert, etc.). The TOC lay staff conducts a brief interview to assess the user’s health conditions and to confirm or re-code the alert. Any other relevant information is reported in the software’s free field ‘Notes’. In the “closing code”, the staff reports if the public safety answering point (112), the first aid station, the General Practitioner (GP), or the caregiver were contacted or if no action was needed.
2.2. Participants and Data Collection
All public and private users who sent a service demand, a support call, or a medical alert during the study period and consented to the processing of the information collected by the telemergency system for research purposes were included. The following baseline information from those regularly collected by the TOC are reported: service information (ID code, private/public user, date of start and end of the service use, reason for service interruption, and device type), demographics (sex, age, marital status, living condition, caregiver presence, dependence level), and health information (comorbidities, use of a walking aid, visual and hearing impairment, lower limb disabilities, alcohol or drugs abuse, and medications). Information on the number and type of drugs was collected, and on drugs that increase the risk of falling (anticoagulants, antihypertensives, diuretics, analgesics, antidepressants, anxiolytics, hypnotics, antiparkinsonians, and neuroleptics) [25,26]. The study was approved by the Ethics Committee of the University of Torino (Prot. n. 0339442).
Alerts sent for 28 months were downloaded from the software in use in the TOC, and between April and May 2023, and researchers created the dataset (the system did not allow for the downloading of longer periods). All the alerts received by the TOC were considered, whether sent by the user or automatically generated by the device. Each alert included the date and hour of dispatch, the date and hour of alert closure by the TOC staff, the PERS code, the TOC lay staff code, the free field note, and the closing code. Two researchers (E.C. and A.C.) independently reviewed all the alerts, comparing the PERS code and the TOC code (Table 1).

Table 1.
Process of re-coding performed by researchers.
All the medical alerts identified by the TOC were re-coded as falls or medical problems based on the information reported in the free field notes and any fall or event that required a medical rescue, even if not coded as a medical alert. Researchers also reviewed the closing code, classifying the alert outcome into four categories: no action needed (if the TOC lay staff managed the alert), ambulance (if the TOC lay staff called a public safety answering point and an ambulance attended the scene), GP (if the TOC contacted the General Practitioner), first aid station (if the TOC reached the emergency medical service), and caregiver (if a relative or a friend was called by the TOC). Since users may send multiple alerts for the same event, alerts reporting the same activation and closure date and the same description in the free field were considered one event. Only support calls, service demands, and emergencies (falls and medical problems) were considered real events and included in the final analysis. Each event was associated with the user through the ID code. Only users who sent at least one real alert were included in the analyses.
2.3. Statistical Analyses
Descriptive data are reported as absolute frequencies and percentages for categorical variables. The normality of the distribution of continuous variables was assessed with the Shapiro–Wilk normality test. Continuous variables with a normal distribution were presented as mean and standard deviation (SD), otherwise median and interquartile range (IQR) were used. Differences between groups (private vs. public users) were assessed using the Chi-squared test for categorical variables and t-test or the non-parametric Wilcoxon rank-sum test, as appropriate, for continuous variables.
Statistical analyses were performed using Jamovi Version 2.3.26.0 [27,28,29,30].
3. Results
Out of the 720 users who sent at least one alert (total number of alerts = 48,874) from December 2020 to March 2023, 315 were included in the final analysis. At the end of March 2023, 308 patients (42.7%) had suspended the service for notice of termination (109, 35.4%), death (103, 33.4%), admission to a nursing home (73, 23.4%), cohabitation with a caregiver (16, 5.5%), and moving home (2, 0.6%); five (1.6%) did not specify the reason. Users who experienced real events were more dependent (p = 0.049) and presented a higher period of overall service use (p < 0.001) and of service use during the study period (p < 0.001). Moreover, they suffered more from respiratory diseases (p = 0.009) and visual impairment (p < 0.001). However, people who had not experienced a real event took more fall-risk-increasing drugs than those who experienced one (p < 0.001).
3.1. Users’ Characteristics
Users’ characteristics are shown in Table 2. Most were widowed women who lived alone with a family network. Private users were significantly older than public users but were comparable for gender, living condition, marital status, and time of service use during the study period (28 months). However, only seven (2.2%) private users lived alone and without a family network, compared with forty public users (12.6%). Private users were significantly more independent and more supported by a caregiver.

Table 2.
Demographic characteristics of participants.
Overall, the median time of use of the telemergency service was 4.6 years, 4.4 years for private users and 4.8 years for public ones. Nearly 50% of the participants used the service for between one and five years, with longer use by public users. However, the two groups were comparable for length of use during the study period: the median time of service use was 2.3 years for both groups.
3.2. Users’ Health Status
Overall, the users had a median of two comorbidities (IQR 2; 3), with a statistically significant difference, between public (median three, IQR 2; 4) and private (median two, IQR 1; 3) users (p = 0.02). The two groups were comparable for hearing and visual impairment, number of drugs, and fall-risk-increasing drugs (Table 3). More than 60% (n = 237) of all users took at least one drug that may increase the risk of falling. The public users suffered significantly more from mental diseases.

Table 3.
Users’ health conditions and medication.
3.3. PERS Activation
A significantly higher number of public users sent a request for service demand, but no differences were observed for the proportion of users that asked for a support call, or sent an alert for health emergencies (medical problems and falls) (Table 4). Moreover, during the study period, users experienced a median of two events, with a significant difference between private and public users (Table 4).

Table 4.
Number of users with at least one real event (service demand, support call, medical problem or fall).
Over the observation time, 300 health emergencies were reported, 168 medical problems (i.e., cardiovascular symptoms, malaise, and tremors, etc.), and 132 falls (Table 5).

Table 5.
Number and types of real events experienced by users.
No significant differences were observed between private and public users for falls, medical problems, and the dispatch of an ambulance. Health emergencies (falls and medical problems) were managed by the caregiver more in private than in public users, and by the first-aid station, significantly more in public than in private users.
Public users experienced more traumatic falls, mainly resulting in head trauma and hip fracture (Table 5). In two cases, the fall caused the death of the user. In the majority of cases, falls occurred when the user was alone (89, 67.4%) and only in in 1/3 of cases, the caregiver activated the alert (43, 32.6%), without differences between the two groups (p = 0.983). Only in six cases was the alert automatically activated by the device.
Of the 168 medical problems, the majority were due to cardiovascular symptoms (i.e., hypotension, heart attack, heart failure, etc.) and malaise and tremors (Table 5). As for falls, most medical problems were directly communicated by the user (141, 83.9%), while only in a small percentage of cases was the alert sent by a caregiver (27, 16.1%), without any differences between the two groups (p = 0.101).
Almost all medical problems (118, 70%) required the dispatch of an ambulance, while only half of the fall cases did so (71, 53.8%). Hospital admission was required in eight cases for medical problems (four in both groups) and two for falls; however, hospitalisations were not always reported, with possible underestimation.
Public users significantly asked for more service demands, while private users significantly sent more support calls (Table 5). Among those who used the service, private users sent, on average, 2.3 calls vs. 1.8 of public users. The main reason for service demands was the need for transportation for medical examinations. The majority of service demands were directly managed by the TOC staff (398, 97.3%), except for 11 cases where the staff asked for the support of a caregiver. The totality of support calls was managed by the TOC staff.
4. Discussion
To our knowledge, this is the first study which aimed at underlining the differences in the use of a PERS and at describing the reasons for alert activation between two different groups of users of a telemergency service. Previous studies focused on describing the characteristics and factors associated with using the PERS [24], focusing on a specific population [12,16,17], or comparing health outcomes (i.e., number of falls, emergency department admissions, or hospitalizations, etc.) between purchasers and non-purchasers [7,15,18,19]. Extending the analysis of alarms to include non-medical alarms may obtain a broader overview of how PERSs are actually used.
Even if PERSs were developed as a fall detection device, our real-world data show a broader use for medical and non-medical needs. Most activations during the study period regarded demands for services and the need to talk to someone (support calls). Only a small part of the alerts involved medical problems and falls, in contrast with previous studies [12,16,17]. A possible explanation for these discrepancies is related to the differences in the number of alerts and real events. In fact, more than one alert can be sent to manage a single fall or an event [12]. Analysing only the events may offer a clearer picture of reasons for using PERS, thereby avoiding overestimations, particularly those related to emergencies (falls and medical problems).
A significantly larger number of public users requested more assistance and sent demands for services compared with private users. A possible explanation for this difference is related to the possibility for public users to request additional services, such as transportation for health exams or health and social workers (i.e., nurses, nurse assistants, etc.) as part of an agreement with public authorities. In contrast, the same services are directly billed to private users. A second explanation was reported by Nyman et al. [24]: frail older people living alone and without the support of a caregiver declared a higher use of a PERS than those who cohabit. These results are consistent with ours, as public users, who were frailer, less independent, and less supported by a caregiver, sent a larger number of requests. These people may have unmet health and non-health needs due to the lack of a caregiver who can identify or solve them promptly [24].
While only 1/3 of users in both groups asked for support, private users needed it more (2.3 vs. 1.8 calls on average). The main reason for support calls was the need to talk to someone to alleviate the sense of loneliness, not mitigated by the two-week routine calls made by the TOC staff to check users’ health status. Though a higher proportion of private users may rely on a caregiver, this may not alleviate the sense of loneliness. The availability of a caregiver does not imply a greater presence at home nor a reduced need for support calls [31]. When scheduling support calls, the sense of loneliness experienced should be considered.
Our findings regarding the characteristics of public and private users and the number of emergencies are consistent with the literature. The characteristics of our participants were very similar to other published studies: most users were women, living alone, and almost one in five users had no family support [18,24]. Similarities were found, particularly, between public users and non-purchasers, except for the independence level. Non-purchasers were younger, less functionally dependent, with less support from family members and they had a personal referred health lower than purchasers [15,19]. Moreover, even though they were younger and more independent, they had a higher risk of in-home emergencies than purchasers, underlining the advantages of using a PERS. Since, as reported by De San Miguel et al. [15], the main barriers in not purchasing a PERS are social isolation and the cost, the availability of all-inclusive services that include a PERS, could provide more equitable access for people at risk for home emergencies [15]. In our study, public authorities sustained the cost of the device (installation and monthly fee) for users with special health and non-health conditions. Compared with previous studies [12,17], the criteria for access to funding are broader. In fact, not only frail people who lived alone, had disabilities, and were at higher risk of falling or already falling were considered but so were those frail people (i.e., with cognitive impairment, lower limb disabilities, which highly limit the movements, etc.) who lived with a caregiver (child, elder spouse, etc.).
As in other studies [7,15,19], despite public users being more dependent and with a larger use of walking aids, no significant differences were observed in the number of falls and medical problems. One possible explanation for this lack of difference could be related to the additional services public users receive. The telemergency service is offered on top of home care services; thus, some health needs may have been detected in advance and treated promptly (i.e., home assessment and environmental hazard modification for fall prevention) [32]. Since data on hospitalisations for emergencies were possibly underestimated, differently from other studies [10,33], any differences between public and private users were not observed.
The presence of a single centralised point of contact which managed all the alerts made response faster, particularly in emergencies [17], and also performed a filter function, with the advantages of managing false alerts, thus alleviating the caregiver’s stress [8,16,18]. In our study, in most cases, the minor health emergencies were managed by a caregiver more in private than public users, and conversely, by the first-aid station, significantly more in public users, who were almost entirely responsible for minor health events. The user was, therefore, treated at home, assuming a reduction not only in costs but also in the stress associated with avoidable transportation to the emergency department [13,18].
Compared with other published studies [7,12,15,16,17], it was possible to also highlight the use of the PERS by the caregiver. In fact, in 32.6% of falls and 16.1% of medical problems, a caregiver sent the alert, requesting the support of the TOC, instead of directly calling an ambulance. This is in contrast to other two other two studies, which reported that the main reason reported by users for not activating the alert is the presence of a caregiver when the emergency occurs, who directly manage the situation or call for rescue [7,18]. Thus, it seems that the PERS is useful not only for the user but also for the caregiver. Moreover, the notification to the TOC allowed the staff to assess the situation and activate the most relevant rescue service.
Moreover, the TOC is particularly relevant for people who live alone, representing the majority of our sample, without any family support, or for those living in rural areas with greater difficulty accessing health or social services. The TOC could further expand its intervention area by connecting the user to other services for health and social needs. A potential further expansion of the service may include the provision of health promotion, education, prevention, and disease management services or information [21]. The integration between telemergency and home care management services has already been described [12,17,24]. However, details on how the two services were integrated and interact are sometimes lacking.
In conclusion, our study presents some limitations. Firstly, data were analysed cross-sectionally, not allowing for the highlighting of the characteristics which may influence the alert sending. More prospective studies are necessary to understand these factors (i.e., age, living conditions, level of ADL/IADL, etc.). Another limit is related to health information, such as the number and type of comorbidities and drugs, as they were only sometimes fully collected at the start of the service; the hospitalisations were not regularly reported. This may have underestimated the number of medical conditions and medications taken by users and the possible benefits of the service in preventing hospitalisations by having a clearer picture of the severity of the events dealt with by the TOC.
5. Conclusions
Compared with other marketed and the newest technologies, PERSs still remain widely used due to their ease of use and affordable cost. Integrating a PERS in a telemergency service, with a single centralised point of contact, allows users to receive broader support, not only for health but also for social needs. Where the telemergency service is integrated into home care services, a broader population who may benefit from the service can be reached, i.e., persons living alone and without a caregiver or a social network. The support from public authorities allows us to overcome one of the principal barriers to adopting PERS, which is the cost of the service. The PERS represents a valid instrument to promote independent living, help manage chronic conditions, and facilitate access to other social and health services.
The TOC also plays a fundamental role during emergencies. The trained lay staff triages the person and activates the most appropriate service acting as a filter between users and health services, thus potentially reducing inappropriate transportation to emergency rooms and promoting the person’s treatment at home.
The future integration of PERS with the newest forms of AI, such as Chat-GPT, in telemergency services may promote interesting developments, such as the refinement of algorithms to guide the phone interview by TOC staff, to better identify and answer to patients requests for help, and also by integrating medical patient history, symptoms, triage, and conditions [34]. The integration of requests for help with the health and social characteristics of users could better shape the characteristics of subgroups with the same needs for surveillance [34,35].
Further studies are needed to better understand how PERS could further promote the management of chronic conditions and to improve strategies adopted by public authorities to integrate private telemergency and homecare services.
Author Contributions
Conceptualization, data curation, methodology, supervision, validation, visualization, and writing original and editing draft of the manuscript E.C. and P.D.G.; data analysis, formal analysis E.C. and L.C.; conceptualization, formal analysis, validation, and visualization A.C.; validation, supervision, writing—review and editing L.C., D.V., S.C. and V.D. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
This study was approved by the Ethical Committee of the University of Torino, on 23 May 2023 with protocol number 0339442-[UOR: SI000045-Classif. III/11]. When signing the contract with Ass.I.S.Te scs company, users also provided their consent for data processing for research purposes. To further protect users’ privacy, the data were provided to the researchers totally anonymized.
Data Availability Statement
Data that support the finding of our study are available from Ass.I.S.Te scs company, but restrictions are applied to the availability of these data, which were used thanks to an agreement with the company. The data are not available to the public without the consent of the PI Elena Casabona and the Ass.I.S.Te.
Acknowledgments
We would thank the staff of the Telemergency Operation Centre of the Ass.I.S.Te scs company for their support in the research and for providing anonymized data. We would thank the Ministry of University and Research for the founding of the doctoral programs on Innovation and Green topic. We also thank the REACtion research Group (Interreg Project 2014–2020) for their contribution.
Conflicts of Interest
Dante Viotti (D.V.) is the Director of Ville Roddolo Nursing Home (Ass.I.S.Te company), where the telemergency service is located. The remaining authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
References
- Registered Nurses’ Association of Ontario. Preventing Falls and Reducing Injury from Falls, 4th ed.; Registered Nurses’ Association of Ontario: Toronto, ON, USA, 2017. [Google Scholar]
- Hessels, V.; Le Prell, G.S.; Mann, W.C. Advances in Personal Emergency Response and Detection Systems. Assist. Technol. 2011, 23, 152–161. [Google Scholar] [CrossRef]
- Mann, W.C.; Belchior, P.; Tomita, M.R.; Kemp, B.J. Use of Personal Emergency Response Systems by Older Individuals with Disabilities. Assist. Technol. 2005, 17, 82–88. [Google Scholar] [CrossRef] [PubMed]
- Yu, L.; Wang, H.; Zhao, Y.; Sun, T.; Murphy, T.E.; Tsui, K. Assessing Elderly’s Functional Balance and Mobility via Analyzing Data from Waist-Mounted Tri-Axial Wearable Accelerometers in Timed up and Go Tests. BMC Med. Inform. Decis. Mak. 2021, 21, 108. [Google Scholar] [CrossRef] [PubMed]
- Hawley-Hague, H.; Boulton, E.; Hall, A.; Pfeiffer, K.; Todd, C. Older Adults’ Perceptions of Technologies Aimed at Falls Prevention, Detection or Monitoring: A Systematic Review. Int. J. Med. Inf. 2014, 83, 416–426. [Google Scholar] [CrossRef] [PubMed]
- Pietrzak, E.; Cotea, C.; Pullman, S. Does Smart Home Technology Prevent Falls in Community-Dwelling Older Adults: A Literature Review. J. Innov. Health Inform. 2014, 21, 105–112. [Google Scholar] [CrossRef]
- De San Miguel, K.; Lewin, G.; Burton, E.L.; Howat, P.; Boldy, D.; Toye, C. Personal Emergency Alarms: Do Health Outcomes Differ for Purchasers and Nonpurchasers? Home Health Care Serv. Q. 2017, 36, 164–177. [Google Scholar] [CrossRef]
- Moore, K.; O’Shea, E.; Kenny, L.; Barton, J.; Tedesco, S.; Sica, M.; Crowe, C.; Alamäki, A.; Condell, J.; Nordström, A.; et al. Older Adults’ Experiences With Using Wearable Devices: Qualitative Systematic Review and Meta-Synthesis. JMIR MHealth UHealth 2021, 9, 204–211. [Google Scholar] [CrossRef]
- Miake-Lye, I.M.; Hempel, S.; Ganz, D.A.; Shekelle, P.G. Inpatient Fall Prevention Programs as a Patient Safety Strategy: A Systematic Review. Ann. Intern. Med. 2013, 158, 390–396. [Google Scholar] [CrossRef]
- Ong, N.W.R.; Ho, A.F.W.; Chakraborty, B.; Fook-Chong, S.; Yogeswary, P.; Lian, S.; Xin, X.; Poh, J.; Chiew, K.K.Y.; Ong, M.E.H. Utility of a Medical Alert Protection System Compared to Telephone Follow-up Only for Home-Alone Elderly Presenting to the ED—A Randomized Controlled Trial. Am. J. Emerg. Med. 2018, 36, 594–601. [Google Scholar] [CrossRef]
- Roush, R.; Teasdale, T.A.; Murphy, J.N.; Kirk, S.M. Impact of a Personal Emergency Response System on Hospital Utilization by Community-Residing Elders. South Med. J. 1995, 88, 917–922. [Google Scholar] [CrossRef]
- Soh, S.-E.; Ayton, D.; Morello, R.; Natora, A.; Yallop, S.; Barker, A. Understanding the Profile of Personal Alert Victoria Clients Who Fall. Health Soc. Care Community 2018, 26, 759–767. [Google Scholar] [CrossRef] [PubMed]
- Wang, Y.; Srikanth, V.; Snowdon, D.A.; Ellmers, S.; Beare, R.; Moran, C.; Richardson, D.; Lotz, P.; Andrew, N.E. Quantifying the Economic Benefit of the Personal Alarm and Emergency Response System in Australia: A Cost Analysis of the Reduction in Ambulance Attendances. Aust. Health Rev. 2020, 45, 51–58. [Google Scholar] [CrossRef] [PubMed]
- Stokke, R. The Personal Emergency Response System as a Technology Innovation in Primary Health Care Services: An Integrative Review. J. Med. Internet Res. 2016, 18, e187. [Google Scholar] [CrossRef] [PubMed]
- De San Miguel, K.; Lewin, G.; Burton, E.; Toye, C.; Boldy, D.; Howat, P. Exploring Risk Profiles and Emergency Frequency of Purchasers and Non-Purchasers of Personal Emergency Alarms: A Prospective Cohort Study. BMC Geriatr. 2015, 15, 140. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Agboola, S.; Golas, S.; Fischer, N.; Nikolova-Simons, M.; Op Den Buijs, J.; Schertzer, L.; Kvedar, J.; Jethwani, K. Healthcare Utilization in Older Patients Using Personal Emergency Response Systems: An Analysis of Electronic Health Records and Medical Alert Data: Brief Description: A Longitudinal Retrospective Analyses of Healthcare Utilization Rates in Older Patients Using Personal Emergency Response Systems from 2011 to 2015. BMC Health Serv. Res. 2017, 17, 282. [Google Scholar] [CrossRef]
- Andrew, N.E.; Wang, Y.; Teo, K.; Callisaya, M.L.; Moran, C.; Snowdon, D.A.; Ellmers, S.; Beare, R.; Richardson, D.; Srikanth, V. Exploring Patterns of Personal Alarm System Use and Impacts on Outcomes. Australas. J. Ageing 2021, 40, 252–260. [Google Scholar] [CrossRef] [PubMed]
- Johnston, K.; Worley, A.; Grimmer-Somers, K.; Sutherland, M.; Amos, L. Personal Alarm Use to Call the Ambulance after a Fall in Older People: Characteristics of Clients and Falls. Australas. J. Paramed. 2010, 8, 1–9. [Google Scholar] [CrossRef]
- Bloch, F.; Lundy, J.-E.; Rigaud, A.-S. Profile Differences of Purchasers, Non-Purchasers, and Users and Non-Users of Personal Emergency Response Systems: Results of a Prospective Cohort Study. Disabil. Health J. 2017, 10, 607–610. [Google Scholar] [CrossRef]
- Bouabida, K.; Lebouché, B.; Pomey, M.-P. Telehealth and COVID-19 Pandemic: An Overview of the Telehealth Use, Advantages, Challenges, and Opportunities during COVID-19 Pandemic. Healthcare 2022, 2293, 10. [Google Scholar] [CrossRef]
- Rush, K.L.; Singh, S.; Seaton, C.L.; Burton, L.; Li, E.; Jones, C.; Davis, J.C.; Hasan, K.; Kern, B.; Janke, R. Telehealth Use for Enhancing the Health of Rural Older Adults: A Systematic Mixed Studies Review. Gerontologist 2022, 62, e564–e577. [Google Scholar] [CrossRef]
- Khoshrounejad, F.; Hamednia, M.; Mehrjerd, A.; Pichaghsaz, S.; Jamalirad, H.; Sargolzaei, M.; Hoseini, B.; Aalaei, S. Telehealth-Based Services During the COVID-19 Pandemic: A Systematic Review of Features and Challenges. Front. Public Health 2021, 9, 711762. [Google Scholar] [CrossRef] [PubMed]
- Monaghesh, E.; Hajizadeh, A. The Role of Telehealth during COVID-19 Outbreak: A Systematic Review Based on Current Evidence. BMC Public Health 2020, 20, 1193. [Google Scholar] [CrossRef] [PubMed]
- Nyman, S.R.; Victor, C.R. Use of Personal Call Alarms among Community-Dwelling Older People. Ageing Soc. 2014, 34, 67–89. [Google Scholar] [CrossRef]
- De Vries, M.; Seppala, L.J.; Daams, J.G.; Van De Glind, E.M.M.; Masud, T.; Van Der Velde, N.; Blain, H.; Bousquet, J.; Bucht, G.; Caballero-Mora, M.A.; et al. Fall-Risk-Increasing Drugs: A Systematic Review and Meta-Analysis: I. Cardiovascular Drugs. J. Am. Med. Dir. Assoc. 2018, 19, 371.e1–371.e9. [Google Scholar] [CrossRef] [PubMed]
- Woolcott, J.C. Meta-Analysis of the Impact of 9 Medication Classes on Falls in Elderly Persons. Arch. Intern. Med. 2009, 169, 1952–1960. [Google Scholar] [CrossRef] [PubMed]
- Jamovi The Jamovi Project 2022. Available online: https://www.jamovi.org/ (accessed on 1 September 2023).
- R Core Team. R: A Language and Environment for Statistical Computing; R Core Team: Vienna, Austria, 2021. [Google Scholar]
- Heinzen, E.; Sinnwell, J.; Atkinson, E.; Gunderson, T.; Dougherty, G. An Arsenal of “R” Functions for Large-Scale Statistical Summaries. [Computer Software]. 2018.
- Serdar, B. ClinicoPath Jamovi Module, Version 0.0.2.0038, [R Package]; Zenodo: Genève, Switzerland, 2022. [Google Scholar] [CrossRef]
- Johnston, K. Perspectives on Use of Personal Alarms by Older Fallers. Int. J. Gen. Med. 2010, 2010, 231–237. [Google Scholar] [CrossRef]
- Stevens, M.; Holman, C.D.J.; Bennett, N. Preventing Falls in Older People: Impact of an Intervention to Reduce Environmental Hazards in the Home. J. Am. Geriatr. Soc. 2001, 49, 1442–1447. [Google Scholar] [CrossRef]
- Lee, J.S.; Hurley, M.J.; Carew, D.; Fisher, R.; Kiss, A.; Drummond, N. A Randomized Clinical Trial to Assess the Impact on an Emergency Response System on Anxiety and Health Care Use among Older Emergency Patients after a Fall. Acad. Emerg. Med. 2007, 14, 301–308. [Google Scholar] [CrossRef]
- Bugaj, M.; Kliestik, T.; Lizaroiu, G. Generative Artificial Intelligence-Based Diagnostic Algorithms in Disease Risk Detection, in Personalized and Targeted Healthcare Procedures, and in Patient Care Safety and Quality. Contemp. Read. Law Soc. Justice 2023, 15, 9. [Google Scholar] [CrossRef]
- Grupa, M.; Zauskova, A.; Nica, E. Generative Artificial Intelligence-Based Treatment Planning in Clinical Decision-Making, in Precision Medicine, and in Personalized Healthcare. Contemp. Read. Law Soc. Justice 2023, 15, 45. [Google Scholar] [CrossRef]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).