Abstract
Traditional hand rehabilitation devices present a challenge in providing personalized training that can lead to finger movements exceeding the safe range, resulting in secondary injuries. To address this issue, we introduce a soft rehabilitation training glove with the function of safety and personalization, which can allow patients to select training modes based on rehabilitation and provide real-time monitoring, as well as feedback on finger movement data. The inner glove is equipped with bending sensors to access the maximum/minimum angle of finger movement and to provide data for the safety of rehabilitation training. The outer glove contains flexible drivers, which can drive fingers for different modes of rehabilitation training. As a result, the rehabilitation glove can drive five fingers to achieve maximum extension/flexion angles of 15.65°/85.97°, 15.34°/89.53°, 16.78°/94.27°, 15.59°/88.82°, and 16.73°/88.65°, from thumb to little finger, respectively, and the rehabilitation training frequency can reach six times per minute. The safety evaluation result indicated an error within ±6.5° of the target-motion threshold. The reliability assessment yielded a high-intra-class correlation coefficient value (0.7763–0.9996). Hence, the rehabilitation glove can achieve targeted improvement in hand function while ensuring safety.
1. Introduction
A number of diseases or injuries can lead to hand damage, such as stroke [1], Parkinson’s disease [2], incomplete spinal cord injury [3], or traumatic fractures [4]. It is reported that up to 60% to 70% of stroke patients have unilateral hand motor impairment [5,6]. Specifically, hand movement disorders mainly include joint movement disorders, hand coordination disorders, or sensory abnormalities [7,8], which will significantly limit the independence of patients, reduce their quality of life and hinder their livelihoods, as well as the entire society [9]. Clinical research has shown that repeated passive movement of the affected hand can reversely stimulate brain reorganization (neural plasticity) and improve hand-motor function [10,11]. Therefore, rehabilitation training is essential for patients with hand injuries, which aims to help patients recover to a normal state [12,13]. However, due to the complexity of finger movements, hand-function rehabilitation is a challenging and lengthy process [14].
Traditional rehabilitation mainly relies on manual methods with patients undergoing exercises under the guidance of a therapist, one-on-one or multi-on-one. However, the effectiveness of rehabilitation training can significantly vary depending on the therapists’ experiences and skill levels [15]. It is not only carrying much uncertainty, but also consuming considerable manpower and financial resources for patients and society as a whole [16,17,18,19]. The latest development in wearable hand robot devices can provide more accurate, objective, reliable and automated solutions for limb-function rehabilitation treatment [20,21]. These electronic systems have played an important role in the rehabilitation training process, offering numerous benefits over traditional methods [22,23,24,25,26,27]. Currently, rigid hand exoskeletons and wearable soft rehabilitation gloves are key points of rehabilitation equipment [28,29,30]. Rigid systems [31,32,33,34,35] aid in the rehabilitation treatment of affected hands by generating linkage forces that connect the finger segments through servo motors [14]. Normally, the mechanical structure of rigid system is complex, heavy, and not highly flexible, which can easily cause joint fatigue in long-term patients. Compared with the rigid system, flexible rehabilitation gloves provide several advantages, such as strong compliance, low cost, lightweight, and safety during interaction with unknown environments and the human body, which have been widely used in rehabilitation treatment research [36,37,38,39]. The inherent characteristics of elastic materials [40,41] and unique geometric designs [42] can be used to achieve the bending of the driver. In addition, combining the flexible driver with fabrics [43,44,45], plastics [46,47], and reinforced fibers [48] can provide good conditions for finger movement. Existing flexible rehabilitation gloves can assist patients in rehabilitation training (Table S1), but there are still challenges to be addressed. As most studies are more interested in achieving rehabilitation outcomes, they overlook the differences in patients’ hand movement abilities. This is unsafe for patients at different stages of rehabilitation and with varying degrees of illness [19,27,49,50,51]. Thus, it is necessary to combine wearable sensor technology [52,53,54] with rehabilitation training systems, in order to achieve a more accurate and safe rehabilitation diagnosis and treatment.
Here, we report a rehabilitation training soft glove that is not limited by clinical environments, assisting patients with impaired hand function to achieve home-based rehabilitation training. Specifically, we have made contributions to hand rehabilitation training in three areas. Firstly, the glove can drive the affected hand to undergo fine training, functional training and gesture training, thereby, respectively, improving the separate movement function of individual fingers, hand-group flexion and extension, and the range of pinch activities, as well as finger coordination. Secondly, the glove is designed as a two-layer structure. The outer layer integrates flexible drivers on the back of the fingers using pneumatic control technology to enable rehabilitation training for finger movement ability. The inner layer incorporates bending sensors to monitor the changes in the bending angle produced during training. It can also provide bending feedback control to prevent exceeding the current user’s motion threshold and ensure the safety of rehabilitation training. Meanwhile, a human-computer interaction interface has been developed to provide a user interface and data visualization. Our system fulfills comfortable experience and comprehensive functionality, which provides a unique and universal approach to address challenges in hand function rehabilitation for patients with hand injuries.
2. Materials and Methods
The rehabilitation glove system proposed in this article mainly consists of a pneumatic actuator module, sensor module (bending sensor and air-pressure sensor), main control module, rehabilitation training mode, and human-computer interaction interface. In order to achieve the integration of rehabilitation training and functional evaluation data, the rehabilitation glove adopts an inner and outer two-layer structure, as shown in Figure 1a. The component layout of the design is based on the anatomical and physiological structure of the patient’s hand, and the glove material is selected to have good force transmission and flexibility to improve hand-glove contact. The outer layer of the glove provides support for the flexible actuators which are pneumatically actuated to assist fingers in rehabilitation training. The bending sensor in the inner glove fits the hand and can track subtle changes in the motion ranges of the patient’s fingers. At the same time, the bending angle information is monitored in real-time based on the feedback technology to achieve safe and reliable rehabilitation training. In addition, the microcontroller, with a rich interface and excellent processing performance, communicates with the human–computer interaction interface, which facilitates patients to make their own rehabilitation training plan and monitor the progress of rehabilitation, creating data, as shown in Figure 1b.
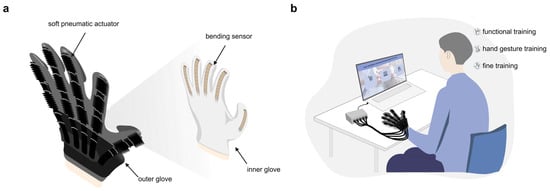
Figure 1.
Personalized safety rehabilitation training soft glove. (a) glove structure; (b) glove application scenarios.
Figure 2 outlines the workflow of the rehabilitation glove. The distinctive feature of this rehabilitation glove lies in the integration of sensing and rehabilitation control. Firstly, the inner glove captures the five-finger bending signal, and after amplification and AD conversion, it is transmitted to the human-computer interaction interface, automatically entering the program setting, and displays the training threshold. The patient sets the training parameters according to the needs of hand rehabilitation, and controls the rehabilitation process autonomously. After the system officially starts, the controller controls the pneumatic actuator module to enter the working state, according to the instructions sent by the human-computer interaction interface. By changing the air pressure inside the rehabilitation glove chamber, finger flexion or extension movement can be realized. It is worth noting that during the entire rehabilitation training process, the air pressure and bending-sensor module continuously monitors the pressure and bending-change data generated by the training in real-time, and graphs it so that patients can clearly understand the actual rehabilitation training situation. At the same time, the controller continuously judges whether the current bending angle reaches the set motion threshold, so as to achieve accurate feedback control.
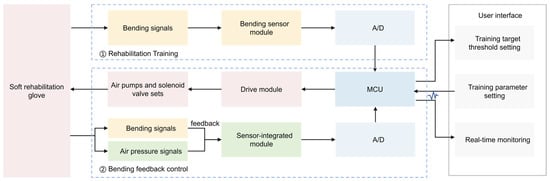
Figure 2.
Rehabilitation training process.
2.1. Pneumatic Actuator Module
The main components of the pneumatic actuator module are pneumatic actuators, air pumps and solenoid valves. Our proposed rehabilitation glove, which mainly focuses on providing a simple, safe, personalized, lightweight and portable solution, therefore chooses commercially available curved-bellows pneumatic actuators, micro air pumps, and direct-acting solenoid valves. Among them, a soft-bellows pneumatic actuator with a chamber can provide smooth and flexible bending motion [55], which meets the design requirements of this paper. The flexible pneumatic actuator is fixed on the outer glove by using fasteners, such as buckles, bases, and springs, which can convert the airflow into a mechanical motion, and then drive the fingers to achieve the target control effect. It is worth noting that the controller cannot provide the working current or voltage required by the load due to its own output voltage, power and other factors. We use a 13-way output PNP power-amplifier module to isolate and amplify the output voltage of the controller, so that it can output a voltage of 0–12 V to realize the drive control of the pneumatic actuator module.
A pneumatic circuit consisting of air pumps and solenoid valves is essential to ensure that the module performs its intended tasks precisely and reliably. For the coordination and dexterity of the patient’s fingers, the pneumatic circuit in this paper includes five pneumatic branches with the same working principle, and are independent of each other, which sequentially control the flexible pneumatic actuators corresponding to the five fingers. Each pneumatic branch is realized by a combination of a two-position, two-way solenoid valve and a two-position, three-way solenoid valve. The micro air pump provides sufficient positive pressure or negative pressure air-source power for the pneumatic circuit, as shown in Figure 3. We take a single pneumatic branch as an example to provide an overview of the workflow. The flow direction of the gas in the circuit can be changed by changing the position of the valve body when the solenoid valve coil is energized and de-energized. The different on-off combinations of the solenoid valve and the air pump determine the different deformations (swell, static, and systolic) of the flexible pneumatic actuator, corresponding to the different states of the pneumatic circuit (inflation, holding, and exhaust), and can drive the fingers to flex, hold, and perform stretching exercises; the corresponding relationship is shown in Table S2. The connection between the air pump and the solenoid valve group uses PVC pipes, and the connection positions of each branch are connected with hose connectors that match the inner diameter of the PVC pipes. In order to improve the airtightness of the pneumatic circuit, stainless steel clamps are used to fasten each interface. In addition, in the hold and exhaust state, excessive air pressure will be accumulated between the air pump and the two-position, two-way solenoid valve, threatening the life of the air pump and the solenoid valve. In order to solve this problem, we design a pressure relief branch composed of a pressure relief valve (normally closed, two-position, two-way solenoid valve). When the pneumatic circuit is in the hold or exhaust state, the pressure relief valve is turned on to release excess air pressure. When one or more branches are in an inflated state, the pressure relief valve is powered off to prevent the air pressure in the cavity of the flexible actuator from being connected to the atmospheric environment to avoid partial pressure leakage.
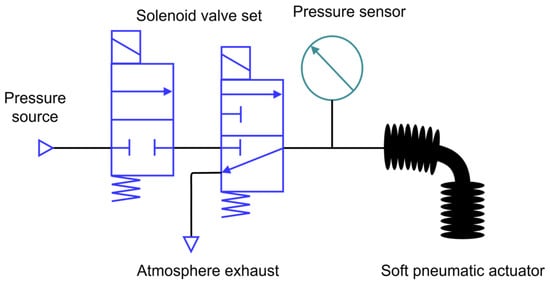
Figure 3.
Pneumatic actuator module.
2.2. Sensor Module
This article aims to achieve accurate and safe rehabilitation control by using a sensing module to monitor, in real-time, the changes in the finger bending angle and pressure inside the flexible actuator during rehabilitation training. The flexible bending sensor consists of a thin and flexible membrane that can provide one million complete bending lifecycles. It is easy to cover the observed fingers, allowing for repeated measurement of the bending angle. The pressure sensor module has small-sized characteristics, easy installation, high sensitivity, and good stability, which meet the requirements of the system. Five sets of bending sensors are fixed in sequence on the back of the inner glove of the five fingers to ensure data stability and finger-movement freedom. The five sets of pressure sensor modules are installed in sequence between each pneumatic branch of the rehabilitation glove, objectively reflecting changes in air pressure during training.
In the process of connecting the bending sensor and the controller, since the input impedance of the controller will change the input resistance of the sensor, it will affect the accuracy of the sensor. In order to solve this problem, we use a dual operational amplifier for regulation. The amplifier includes two independent, high-gain, internal frequency-compensated operational amplifiers, which can effectively reduce the error caused by the source impedance on the measurement results by using the characteristics of low-bias-current (Figure S1). Figure 4 shows the signal processing process of the sensor module. The analog signal collected by the module is first amplified by the operational amplifier, then through signal processing, ADC conditioning, serial communication and other steps, and finally received by the customized human-computer interaction interface.
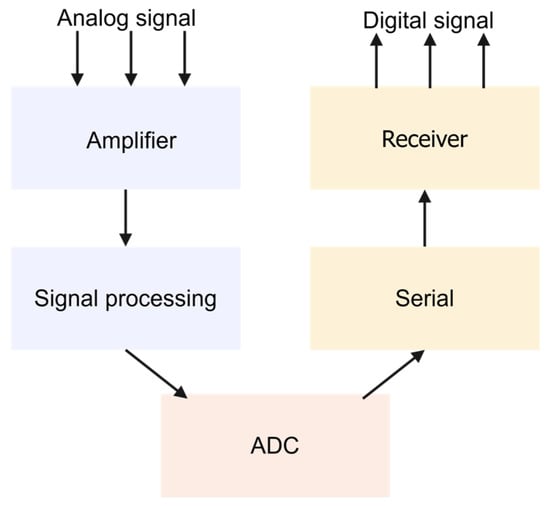
Figure 4.
Sensor module signal acquisition flow chart.
2.3. Main Control Module
We developed a battery-powered main control circuit board for data processing and control, as shown in Figure 5. The main control circuit board consists of MCU, power management module, bending-sensor conditioning circuit, and I/O interfaces (Figure S2), which are integrated on a fast-prototyping PCB board patterned using a UV laser system (LPKF; Protolaser U4). The power management module is composed of a 12 V lithium battery combined with a voltage regulator chip, which provides 12 V, 5 V, and 3.3 V power supply for different modules of the rehabilitation training system. The ingenious design of the voltage regulator circuit can prevent voltage inversion after power failure and suppress self-excited oscillation, ensuring the stability of the entire system. In order to take into account the weight, integration, and circuit design requirements and cost of the flexible rehabilitation glove system, using reflow soldering technology will solder the bending-sensor conditioning circuit on the main control circuit board. The external interfaces bring convenience to the overall system construction. Both the bending-sensor and the air-pressure sensor module are connected to the relevant pins of the main control circuit board through wires to continuously monitor the bending and air pressure signals, respectively.
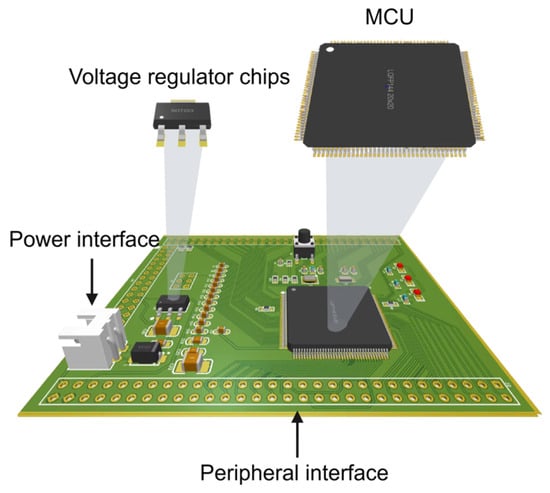
Figure 5.
Main control module circuit board.
The main control module uses the USART serial port to communicate with the PC. The rehabilitation training control process is shown in Figure S3. In the initialization state, the air pressure inside the rehabilitation glove is connected to the atmosphere, presenting a natural bending state. The extent of rehabilitation training depends on the determination of the patient’s finger movement threshold. During the training process, the controller will continuously receive the bending signal generated by the trained finger and compare it with the set motion threshold. If it exceeds significantly, the system is forced to return to the initialization state to avoid causing secondary damage to the affected hand due to the excessive training range. On the contrary, the system operates normally until the set training times are reached. The control module we designed can solve the safety problem during the training process and achieve the expected rehabilitation training effect.
2.4. Rehabilitation Training Modes
We designed three rehabilitation training modes (fine training, functional training, and gesture training) and a total of 13 different hand gestures (Table S3) to meet the rehabilitation requirements of patients with different types of hand functional impairments. A complete rehabilitation training session includes flexion, hold, extension, and hold, with a training frequency of 6 times per minute. It’s worth noting that all gestures can assist patients in performing different degrees of bending and stretching movements in their fingers, significantly improving the range of movement in their hands and alleviating joint movement disorders. In addition, different training modes can also improve the coordination of hand movements in patients. Fine training (“FT”, “FI”, “FM”, “FR”, “FL”) focuses on training individual fingers to perform bending and stretching movements to improve finger separation and movement function. Functional training includes whole-finger training (“CH”) and two-finger pinch training (“FTI”, “FTM”, “FTR”, “FTL”), which can improve patients’ hand-grouping movement, as well as pinch strength, and prevent hand atrophy. Gesture training modes include “OK”, “VICTOR”, and “Orchid finger” to train the coordination ability of each finger to complete more challenging actions together.
2.5. Human-Computer Interaction Interface
The designed human-computer interaction interface includes login management, user information, rehabilitation training, and history record functions. When the patient clicks on the corresponding button to trigger the system’s specific function, the target interface will automatically display the next step of operation prompts, assisting the patient in quickly mastering the use of the system. In this study, the rehabilitation training interface and history record interface were selected for demonstration. Before starting the formal rehabilitation training, the patient puts on the flexible rehabilitation glove and completes the fist and flat hand actions after clicking the “movement threshold” button. The software interface will display the maximum and minimum movement thresholds for the five fingers (as shown in Figure 6a). After the patient clicks the “training parameters” button to enter the corresponding interface, they can choose the rehabilitation training mode according to their own status, set the rehabilitation training times, duration, and intensity (as shown in Figure 6b). The intensity setting range is from 0% to 50% (0% intensity is the maximum). After clicking the “data monitoring” button, the bending and air pressure changes of each finger during the rehabilitation training process will be presented via a waveform in the interface (as shown in Figure 6c), which is convenient for the patient to observe the actual training status more intuitively and clearly. In addition, clicking the “return” button can return to the previous interface. The history record interface can continuously and truthfully record the patient’s daily rehabilitation training progress (as shown in Figure 6d), which helps the patient understand the rehabilitation trend and adjust the rehabilitation plan in advance. It is worth noting that we have designed an “emergency stop” button on all interfaces of the system to deal with external emergencies and urgent situations, further ensuring the safety of patient rehabilitation training.
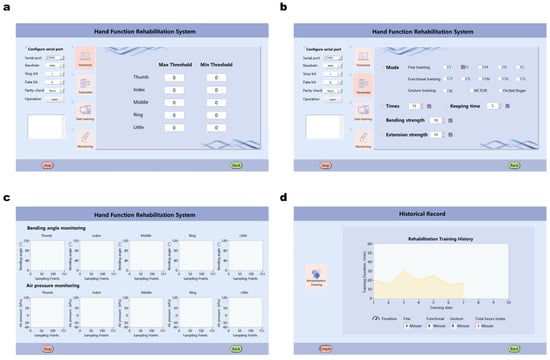
Figure 6.
Rehabilitation glove human-computer interaction interface. (a) finger movement threshold acquisition; (b) training parameter settings; (c) visualization of rehabilitation exercise data; (d) historical records.
2.6. Ethical Information
This study was approved by the Ethics Committees of China-Japan Union Hospital of Jilin University (Clinical Research Review No. 20221124002). Written informed consent was obtained from all participants. Inclusion criteria were as follows: (1) diagnosed with stroke, Parkinson’s disease, or hand trauma; (2) sufficient cognitive and language expression ability to understand the experiment and follow instructions; (3) stable vital signs, well-controlled underlying diseases, and able to participate in various rehabilitation training exercises; and (4) patients and their families were informed about this study and voluntarily signed an informed consent form. Exclusion criteria were: (1) behaviors and cognitive impairment that interfere with active treatment; (2) low compliance; and (3) hand structural and functional abnormalities, such as finger defects, fractures, and joint deformities. Eight patients with hand functional disorders of different severity were recruited for our study. Their symptoms included, but were not limited to, stiffness, spasms, and tendon adhesions. Their detailed information is shown in Table S4.
3. Results and Discussion
3.1. Bending Driver Experiment
In order to obtain an accurate characteristic relationship between the resistance value and the bending angle of each bending sensor, we conducted a calibration experiment on the bending sensor. The bending sensors fixed on the back of the thumbs, index fingers, middle fingers, ring fingers, and little fingers are labeled as 01–05, respectively. During the calibration process, the internal resistance value of the bending sensor is measured using a multimeter, and the angle change is measured by an angle-measuring ruler. The experiment recorded the changes in the internal resistance values of the five bending sensors corresponding to bending angles from 0° to 90° (with intervals of 10°), and the resistance values for each bending angle of each sensor were the average of three calibrations (Table S5). The calibration results were curve-fitted using the least squares method to obtain Figure 7. From the figure, it can be seen that the resistance value of the bending sensor depends on the deformation of the sensor, and the two are proportional, with the resistance value increasing with the increase of the bending angle.
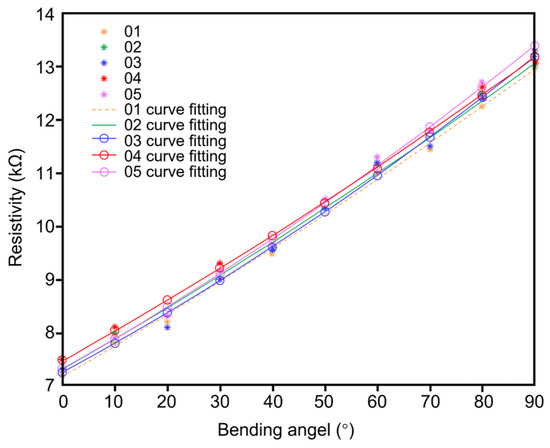
Figure 7.
Bending sensor resistance value-bending angle characteristic curve.
The bending angles and corresponding pressure values of the rehabilitation glove in a natural state, maximum bending state, and maximum extension state are shown in Table S6. In order to verify the relationship between the bending performance of the flexible actuator and the air pressure, the experiment was conducted under −30–100 kPa air pressure, with a negative pressure step of 5 kPa and a positive pressure step of 20 kPa. During the experiment, the bending angle of the flexible actuator at different pressures was recorded (Tables S7 and S8). The experimental data reveals that the error between the actual pressure measured by the pressure sensor module and the theoretical pressure is within ±1.5 kPa. During the inflation (positive pressure) or deflation (negative pressure) process of the flexible actuator, the uneven pressure distribution may cause a certain amount of motion error and bending-angle error. To mitigate accidental data, each group of experiments was repeated five times and the average value was taken to draw the bending-pressure characteristic curve (Figure 8). It can be concluded from the figure that the bending angle of the flexible actuator is positively correlated with the air pressure. The flexible actuator exhibits a slight bending shape in the natural state. Under negative pressure, the flexible actuator undergoes compression deformation, driving the fingers to perform extension movements. Conversely, under positive pressure, it undergoes expansion deformation, driving the fingers to perform flexion movements.
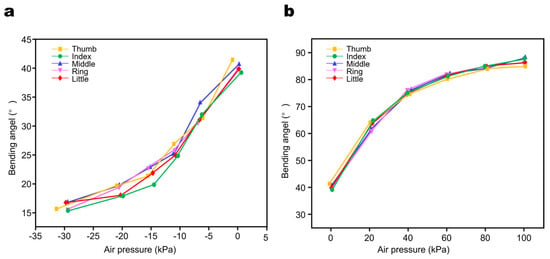
Figure 8.
Air pressure and bending characteristics of the five finger actuators. (a) Bending angle and air pressure characteristic curve of actuator under negative pressure condition; (b) Bending angle and air pressure characteristic curve of actuator under positive pressure condition.
3.2. Rehabilitation Training Experiment
All participants participated in the rehabilitation training experiment to verify the actual training effect of the rehabilitation glove. After wearing the proposed flexible rehabilitation gloves, participants underwent a 60 s calibration stage to reduce sensor changes and variations in hand size. Then, participants were guided to click the rehabilitation training function button on the human-machine interface to enter the rehabilitation training parameter-setting interface. Participants were allowed to choose any rehabilitation training gesture according to their needs and set the number of training sessions, duration, and intensity. After completing each gesture, participants were instructed to relax for 5 s to prepare for the next gesture and to reduce measurement errors caused by finger fatigue. During the experiment, the system monitored the bending angle of the participants’ fingers in real-time. We analyzed the data of one participant, and the maximum/minimum bending-movement thresholds of the participant’s five fingers are shown in Table S9. Figure 9a–c and Figures S4–S6 show the execution effect of the participant’s rehabilitation training and the changes in bending angle during training. The results show that in the “FL” and “FTR” training (Figure 9a,b), the adjacent fingers of the trained finger will move in the same trend as the bending angle of the trained finger changes. This is due to the coupling relationship between finger joints, and finger movement will be constrained by ligaments and muscle tendons. In addition, both fine training and functional training involve a cycle of bending, holding, stretching, and holding. In one cycle of the “VICTOR” training (Figure 9c), the thumb, ring finger, and little finger have the same movement state (bending, holding, stretching, holding), while the index finger and middle finger have the same movement state (stretching), and the actual rehabilitation training effect is consistent with the expected movement. During all training processes, the five fingers did not exceed the subject’s own safe movement threshold, and the system exhibited good performance in the rehabilitation training process, achieving the expected rehabilitation training effect.
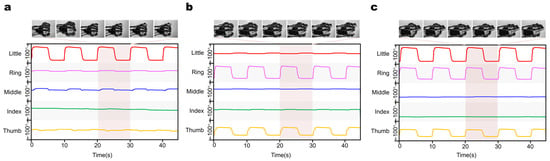
Figure 9.
(a) training effect of “FL” gesture and change of finger bending angle; (b) training effect of “FTR” gesture and change of finger bending angle; (c) training effect of “VICTOR” gesture and change of finger bending angle.
3.3. System Security Evaluation Experiment
The goal of this experiment is to verify whether the proposed flexible rehabilitation glove system can ensure the safety of patients. To avoid introducing human intention noise or other interference during the experiment, a flexible glove was placed on a flat table and the experiment was carried out without load. Prior to the experiment, a participant was randomly selected and their finger movement threshold was recorded as the safety assessment experiment threshold and entered into the rehabilitation training system, as shown in Table S10. As the safety performance experiment involved five fingers, the “CH” function training mode was selected. The number of training sessions was set to six (i.e., a duration of 1 min), with a hold time of 5 s, a bending intensity of 10%, and an extension intensity of 10%. The bending angles of each finger during the training process were monitored in real-time, and the minimum/maximum bending angles of the five fingers were recorded for each session (Tables S11 and S12). The distribution characteristics of the bending-angle data of each finger for each training session were analyzed by drawing box plots, as shown in Figure 10 and Figure S7. The box plot directly reflects the maximum, minimum, mean, and outlier values of finger movement. It can be seen that no abnormal values were observed in the bending data of each finger during any of the training sessions.
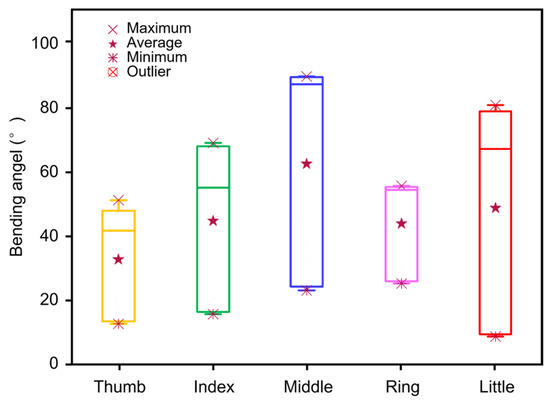
Figure 10.
System safety evaluation single training box graph.
Furthermore, this study conducted a calculation of the deviation between the actual motion threshold and the prescribed-motion range, and then statistically analyzed the mean, standard deviation, and 95% confidence interval of the difference, as shown in Tables S13 and S14. The results showed that the standard deviation of the five-finger motion range of the rehabilitation glove was less than 3°, and the 95% confidence interval was limited within ±6.5°. These results provide evidence that the rehabilitation glove is safe to use during actual rehabilitation training. The existing errors are not likely to compromise the effectiveness of the rehabilitation training, nor do they pose any secondary harm to the participant’s hand.
3.4. System Reliability Evaluation Experiment
To avoid the possibility of chance results, we comprehensively verified the performance and stability of the personalized and safe soft glove for rehabilitation training through three repeated tests. Eight subjects were required to complete 13 sets of test movements, with each set requiring the subject to complete the movements five times, and a test frequency of 10 s per time. To prevent fatigue caused by multiple experiments, a rest time of 30 s was reserved between each group of movements. Figure 11 shows the actual situation of the subjects undergoing the three repeated tests.
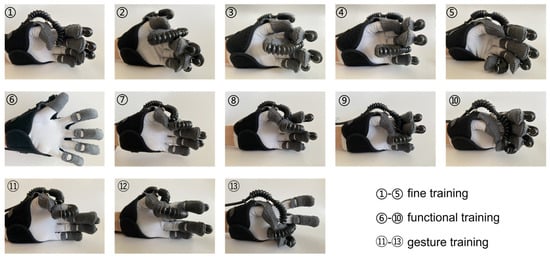
Figure 11.
Implementation effect of rehabilitation glove reliability evaluation.
In this study, the ICC, two-way mixed effects, and consistency model were used to determine the reliability of the measured values in each test. ICC is a statistical indicator used to evaluate the consistency, reliability, and test-retest reliability of quantitative data. The ICC value ranges from 0 to 1, with higher values indicating higher reliability, and lower values indicating unreliable results. Specifically, reliability is classified as excellent (ICC > 0.9), good (0.75 < ICC ≤ 0.9), moderate (0.5 < ICC ≤ 0.75), or poor [56]. By statistically analyzing the five measurement values in each group of movements, the average of the ICC values of all training fingers in each movement was used as the reliability coefficient of that movement (Table 1). The reliability coefficient of each training mode was determined by taking the average of the reliability coefficients of the movements within each mode (Table 2). It can be seen from the tables that fine training and functional training showed strong consistency (with ICC values of 0.9996 and 0.9983, respectively). Gesture training was affected by the coordination between the fingers, resulting in a lower ICC value (0.7763) compared to the other two modes, but still demonstrated strong consistency. Finally, due to the high-ICC values obtained (ranging from 0.7763 to 0.9996), it can be concluded that the system is reliable and can be used for rehabilitation training of hand-function disorders.

Table 1.
Reliability coefficient of 13 gestures.

Table 2.
Reliability coefficient of 3 training modes.
4. Conclusions
This article proposes a feedback-based rehabilitation glove for patients with hand function disabilities (Table S15 and Figure S8). This glove achieves multi-mode hand rehabilitation training while being comfortable and lightweight. The glove can successfully capture the patient’s threshold for voluntary finger movement, enabling personalized, home-based rehabilitation training and ensuring the safety of the rehabilitation training process. The article validates the characteristic relationship between the bending angle of the flexible actuator and the air pressure, and uses the bending-angle signal as an indicator of the rehabilitation progress. Multiple mode rehabilitation training experiments are conducted to verify the system’s performance. The results show that the rehabilitation glove can achieve separate finger movements, hand flexion and extension movements, and coordination between fingers. Furthermore, no-load experiments are conducted to validate the safety of the system, which is found to effectively prevent secondary injuries during continuous and repetitive training. The high-reliability coefficient obtained from the three repeat tests validates the reliability of the rehabilitation glove. In addition, the design of the human-computer interaction interface facilitates patients’ rehabilitation training and visualizes the rehabilitation process. The glove is successfully demonstrated to have hand rehabilitation training capabilities in practical scenarios, and its compatibility with current clinical-rehabilitation requirements solves the problems of safety and personalization in hand rehabilitation training, displaying broad prospects in various fields such as assistive technology and the Internet of Things. Future work includes increasing the freedom of adduction or abduction to promote more comprehensive hand rehabilitation training.
Supplementary Materials
The following supporting information can be downloaded at https://www.mdpi.com/article/10.3390/electronics12112531/s1, Table S1: Comparison of the proposed rehabilitation gloves with those mentioned in previous literature; Table S2: Implementation of different states in a single branch; Table S3: 13 gestures in three modes, adapted from [20]; Table S4: Characteristics of subjects; Table S5: Bending sensor calibration results; Table S6: Bending angle and its corresponding air pressure change in different states of the actuator; Table S7: The relationship between air pressure and bending angle during the extension movement of the actuator; Table S8: The relationship between air pressure and bending angle during the flexion movement of the actuator; Table S9: Subject’s movement thresholds in the rehabilitation training experiment; Table S10: Movement thresholds for randomly selected subject in safety assessment experiment; Table S11: Minimum movement threshold of each finger during 6 sessions of “CH”; Table S12: Maximum movement threshold of each finger during 6 sessions of “CH”; Table S13: Consistency analysis of the actual minimum movement threshold and the target minimum movement threshold of the five fingers; Table S14: Consistency analysis of the actual maximum movement thresholds of the five fingers and the target maximum movement thresholds. Table S15: Technical specifications of the glove. Figure S1: Bending sensors conditioning circuit; Figure S2: The circuit schematic of the main control module; Figure S3: The process of rehabilitation training control; Figure S4: The effect of “fine training” and the change of bending angle of five fingers. (a) “FT”; (b) “FI”; (c) “FM”; (d) “FR”; Figure S5: The effect of “functional training” and the change of bending angle of five fingers. (a) “CH”; (b) “FTI”; (c) “FTM”; (d) “FTL”; Figure S6: The effect of “hand gesture training” and the change of bending angle of five fingers. (a) “OK”; (b) “Orchid finger”; Figure S7: The five-training box line figure for system security assessment; Figure S8: Flexible rehabilitation gloves physical picture.
Author Contributions
X.J. and X.X. are the corresponding authors, supervised the whole project, presented the whole idea, and revised the paper. F.M., Y.L., X.J. and X.X. designed and conducted the research. Q.L. and C.L. (Chenyi Lyu) analyzed the subjects’ data. G.G. and J.Y. designed the program. F.M. and C.L. (Chang Liu) wrote the first draft of the manuscript and all authors contributed to writing the report. C.L. (Chang Liu), H.H., Q.L., C.L. (Chenyi Lyu) and Z.W. organized and checked the manuscript. All authors have read and agreed to the published version of the manuscript.
Funding
This research was funded by Science and Technology Development Plan Project of Jilin Province (No. 20230401088YY). National Research Foundation, Singapore, and A*STAR under its RIE2020 Industry Alignment Fund—Industry Collaboration Projects (IAF-ICP) grant call (Grant No. I2001E0059).
Data Availability Statement
All data generated or analyzed during this study are included in this published article and its supplementary information files.
Acknowledgments
Xiaoqiang Ji thanks support from Science and Technology Development Plan Project of Jilin Province (No. 20230401088YY). Xiao Xiao acknowledges support from the SIA-NUS Digital Aviation Corporate Laboratory Corporate Laboratory, the N.1 Institute for Health, and the Institute for Health Innovation and Technology, NUS.
Conflicts of Interest
The authors declare no conflict of interest.
References
- Huang, Y.; Nam, C.; Li, W.; Rong, W.; Xie, Y.; Liu, Y.; Qian, Q.; Hu, X. A Comparison of the Rehabilitation Effectiveness of Neuromuscular Electrical Stimulation Robotic Hand Training and Pure Robotic Hand Training after Stroke: A Randomized Controlled Trial. Biomed Signal Proces. 2020, 56, 101723. [Google Scholar] [CrossRef]
- Zach, H.; Dirkx, M.; Bloem, B.R.; Helmich, R.C. The Clinical Evaluation of Parkinson’s Tremor. J. Park Dis. 2015, 5, 471–474. [Google Scholar] [CrossRef]
- Cappello, L.; Meyer, J.T.; Galloway, K.C.; Peisner, J.D.; Granberry, R.; Wagner, D.A.; Engelhardt, S.; Paganoni, S.; Walsh, C.J. Assisting Hand Function after Spinal Cord Injury with a Fabric-Based Soft Robotic Glove. J. Neuroeng. Rehabil. 2018, 15, 59. [Google Scholar] [CrossRef]
- Rashid, A.; Hasan, O. Wearable Technologies for Hand Joints Monitoring for Rehabilitation: A Survey. Microelectron J. 2019, 88, 173–183. [Google Scholar] [CrossRef]
- Virani, S.S.; Alonso, A.; Aparicio, H.J.; Benjamin, E.J.; Bittencourt, M.S.; Callaway, C.W.; Carson, A.P.; Chamberlain, A.M.; Cheng, S.; Delling, F.N.; et al. Heart Disease and Stroke Statistics—2021 Update: A Report from the American Heart Association. Circulation 2021, 143, e254–e743. [Google Scholar] [CrossRef] [PubMed]
- Veldema, J.; Nowak, D.A.; Gharabaghi, A. Resting Motor Threshold in the Course of Hand Motor Recovery after Stroke: A Systematic Review. J. Neuroeng. Rehabil. 2021, 18, 158. [Google Scholar] [CrossRef]
- Smith, Z.A.; Barry, A.J.; Paliwal, M.; Hopkins, B.S.; Cantrell, D.; Dhaher, Y. Assessing hand dysfunction in cervical spondylotic myelopathy. PLoS ONE 2019, 14, e0223009. [Google Scholar] [CrossRef] [PubMed]
- Wijemanne, S.; Jankovic, J. Hand, Foot, and Spine Deformities in Parkinsonian Disorders. J. Neural Transm. 2019, 126, 253–264. [Google Scholar] [CrossRef]
- Hwang, Y.-T.; Lu, W.-A.; Lin, B.-S. Use of Functional Data to Model the Trajectory of an Inertial Measurement Unit and Classify Levels of Motor Impairment for Stroke Patients. IEEE Trans. Neural Syst. Rehabil. Eng. 2022, 30, 925–935. [Google Scholar] [CrossRef]
- Heung, K.H.L.; Tong, R.K.Y.; Lau, A.T.H.; Li, Z. Robotic Glove with Soft-Elastic Composite Actuators for Assisting Activities of Daily Living. Soft. Robot. 2019, 6, 289–304. [Google Scholar] [CrossRef]
- Sawabe, M.; Momosaki, R.; Hasebe, K.; Sawaguchi, A.; Kasuga, S.; Asanuma, D.; Suzuki, S.; Miyauchi, N.; Abo, M. Rehabilitation Characteristics in High-Performance Hospitals after Acute Stroke. J. Stroke Cerebrovasc. Dis. 2018, 27, 2431–2435. [Google Scholar] [CrossRef]
- Wang, Y.; Xu, Q. Design and Testing of a Soft Parallel Robot Based on Pneumatic Artificial Muscles for Wrist Rehabilitation. Sci. Rep. 2021, 11, 1273. [Google Scholar] [CrossRef]
- Sheng, B.; Zhang, Y.; Meng, W.; Deng, C.; Xie, S. Bilateral Robots for Upper-Limb Stroke Rehabilitation: State of the Art and Future Prospects. Med. Eng. Phys. 2016, 38, 587–606. [Google Scholar] [CrossRef]
- Wang, Y.; Kokubu, S.; Zhou, Z.; Guo, X.; Hsueh, Y.-H.; Yu, W.; Yu, W. Designing Soft Pneumatic Actuators for Thumb Movements. IEEE Robot. Autom. Lett. 2021, 6, 8450–8457. [Google Scholar] [CrossRef]
- Yap, H.K.; Lim, J.H.; Nasrallah, F.; Yeow, C.-H. Design and Preliminary Feasibility Study of a Soft Robotic Glove for Hand Function Assistance in Stroke Survivors. Front. Neurosci. 2017, 11, 547. [Google Scholar] [CrossRef]
- Polygerinos, P.; Wang, Z.; Galloway, K.C.; Wood, R.J.; Walsh, C.J. Soft Robotic Glove for Combined Assistance and At-Home Rehabilitation. Robot Auton. Syst. 2015, 73, 135–143. [Google Scholar] [CrossRef]
- Ji, X.; Rao, Z.; Zhang, W.; Liu, C.; Wang, Z.; Zhang, S.; Zhang, B.; Hu, M.; Servati, P.; Xiao, X. Airline Point-of-Care System on Seat Belt for Hybrid Physiological Signal Monitoring. Micromachines 2022, 13, 1880. [Google Scholar] [CrossRef]
- Chen, G.; Xiao, X.; Zhao, X.; Tat, T.; Bick, M.; Chen, J. Electronic Textiles for Wearable Point-of-Care Systems. Chem. Rev. 2022, 122, 3259–3291. [Google Scholar] [CrossRef]
- Zhang, S.; Bick, M.; Xiao, X.; Chen, G.; Nashalian, A.; Chen, J. Leveraging Triboelectric Nanogenerators for Bioengineering. Matter 2021, 4, 845–887. [Google Scholar] [CrossRef]
- Chen, X.; Gong, L.; Wei, L.; Yeh, S.-C.; Xu, L.D.; Zheng, L.; Zou, Z. A Wearable Hand Rehabilitation System with Soft Gloves. IEEE Trans. Ind. Inf. 2019, 17, 943–952. [Google Scholar] [CrossRef]
- Popov, D.; Gaponov, I.; Ryu, J.-H. Portable Exoskeleton Glove with Soft Structure for Hand Assistance in Activities of Daily Living. IEEE ASME Trans. Mechatron. 2015, 22, 865–875. [Google Scholar] [CrossRef]
- Polygerinos, P.; Correll, N.; Morin, S.A.; Mosadegh, B.; Onal, C.D.; Petersen, K.; Cianchetti, M.; Tolley, M.T.; Shepherd, R.F. Soft Robotics: Review of Fluid-Driven Intrinsically Soft Devices; Manufacturing, Sensing, Control, and Applications in Human-Robot Interaction. Adv. Eng. Mater. 2017, 19, 1700016. [Google Scholar] [CrossRef]
- Mayer, M.; Xiao, X.; Yin, J.; Chen, G.; Xu, J.; Chen, J. Advances in Bioinspired Triboelectric Nanogenerators. Adv. Electron. Mater. 2022, 8, 2200782. [Google Scholar] [CrossRef]
- Xiao, X.; Yin, J.; Chen, J. Triboelectric Nanogenerator for Healthcare. In Handbook of Triboelectric Nanogenerators; Wang, Z.L., Yang, Y., Zhai, J., Wang, J., Eds.; Springer International Publishing: Cham, Switzerland, 2023; pp. 1–50. [Google Scholar]
- Peng, Z.; Huang, J. Soft Rehabilitation and Nursing-Care Robots: A Review and Future Outlook. Appl. Sci. 2019, 9, 3102. [Google Scholar] [CrossRef]
- Al-Fahaam, H.; Davis, S.; Nefti-Meziani, S. The Design and Mathematical Modelling of Novel Extensor Bending Pneumatic Artificial Muscles (EBPAMs) for Soft Exoskeletons. Robot Auton. Syst. 2018, 99, 63–74. [Google Scholar] [CrossRef]
- Jin, L.; Xiao, X.; Deng, W.; Nashalian, A.; He, D.; Raveendran, V.; Yan, C.; Su, H.; Chu, X.; Yang, T.; et al. Manipulating Relative Permittivity for High-Performance Wearable Triboelectric Nanogenerators. Nano Lett. 2020, 20, 6404–6411. [Google Scholar] [CrossRef]
- Zhu, Y.; Gong, W.; Chu, K.; Wang, X.; Hu, Z.; Su, H. A Novel Wearable Soft Glove for Hand Rehabilitation and Assistive Grasping. Sensors 2022, 22, 6294. [Google Scholar] [CrossRef]
- Luo, Y.; Wang, Z.; Wang, J.; Xiao, X.; Li, Q.; Ding, W.; Fu, H.Y. Triboelectric Bending Sensor Based Smart Glove towards Intuitive Multi-Dimensional Human-Machine Interfaces. Nano Energy 2021, 89, 106330. [Google Scholar] [CrossRef]
- Shen, S.; Xiao, X.; Yin, J.; Xiao, X.; Chen, J. Self-Powered Smart Gloves Based on Triboelectric Nanogenerators. Small Methods 2022, 6, 2200830. [Google Scholar] [CrossRef]
- Fischer, H.C.; Triandafilou, K.M.; Thielbar, K.O.; Ochoa, J.M.; Lazzaro, E.D.C.; Pacholski, K.A.; Kamper, D.G. Use of a Portable Assistive Glove to Facilitate Rehabilitation in Stroke Survivors with Severe Hand Impairment. IEEE Trans. Neural Syst. Rehabil. Eng. 2016, 24, 344–351. [Google Scholar] [CrossRef]
- Lee, S.W.; Landers, K.A.; Park, H.-S. Development of a Biomimetic Hand Exotendon Device (BiomHED) for Restoration of Functional Hand Movement Post-Stroke. IEEE Trans. Neural Syst. Rehabil. Eng. 2014, 22, 886–898. [Google Scholar] [CrossRef]
- Yang, J.; Xie, H.; Shi, J. A Novel Motion-Coupling Design for a Jointless Tendon-Driven Finger Exoskeleton for Rehabilitation. Mech. Mach. Theory 2016, 99, 83–102. [Google Scholar] [CrossRef]
- Wang, D.; Meng, Q.; Meng, Q.; Li, X.; Yu, H. Design and Development of a Portable Exoskeleton for Hand Rehabilitation. IEEE Trans. Neural Syst. Rehabil. Eng. 2018, 26, 2376–2386. [Google Scholar] [CrossRef]
- Jo, I.; Bae, J. Design and Control of a Wearable and Force-Controllable Hand Exoskeleton System. Mechatronics 2017, 41, 90–101. [Google Scholar] [CrossRef]
- Gorissen, B.; Reynaerts, D.; Konishi, S.; Yoshida, K.; Kim, J.; Volder, M.D. Elastic Inflatable Actuators for Soft Robotic Applications. Adv. Mater. 2017, 29, 1604977. [Google Scholar] [CrossRef]
- Boyraz, P.; Runge, G.; Raatz, A. An Overview of Novel Actuators for Soft Robotics. Actuators 2018, 7, 48. [Google Scholar] [CrossRef]
- Nguyen, P.H.; Zhang, W. Design and Computational Modeling of Fabric Soft Pneumatic Actuators for Wearable Assistive Devices. Sci. Rep. 2020, 10, 9638. [Google Scholar] [CrossRef]
- Ayodele, E.; Zaidi, S.A.R.; Scott, J.; Zhang, Z.; Hayajneh, A.; Shittu, S.; McLernon, D. A Weft Knit Data Glove. IEEE Trans. Instrum. Meas. 2021, 70, 1–12. [Google Scholar] [CrossRef]
- Polygerinos, P.; Wang, Z.; Overvelde, J.T.B.; Galloway, K.C.; Wood, R.J.; Bertoldi, K.; Walsh, C.J. Modeling of Soft Fiber-Reinforced Bending Actuators. IEEE Trans. Robot. 2015, 31, 778–789. [Google Scholar] [CrossRef]
- Ge, G.; Mandal, K.; Haghniaz, R.; Li, M.; Xiao, X.; Carlson, L.; Jucaud, V.; Dokmeci, M.R.; Ho, G.W.; Khademhosseini, A. Deep Eutectic Solvents-Based Ionogels with Ultrafast Gelation and High Adhesion in Harsh Environments. Adv. Funct. Mater. 2023, 33, 2207388. [Google Scholar] [CrossRef]
- Polygerinos, P.; Lyne, S.; Wang, Z.; Nicolini, L.F.; Mosadegh, B.; Whitesides, G.M.; Walsh, C.J. Towards a Soft Pneumatic Glove for Hand Rehabilitation. In Proceedings of the 2013 IEEE/RSJ International Conference on Intelligent Robots and Systems, Tokyo, Japan, 3–7 November 2013; pp. 1512–1517. [Google Scholar] [CrossRef]
- Yap, H.K.; Khin, P.M.; Koh, T.H.; Sun, Y.; Liang, X.; Lim, J.H.; Yeow, C.-H. A Fully Fabric-Based Bidirectional Soft Robotic Glove for Assistance and Rehabilitation of Hand Impaired Patients. IEEE Robot. Autom. Lett. 2016, 2, 1383–1390. [Google Scholar] [CrossRef]
- Cappello, L.; Galloway, K.C.; Sanan, S.; Wagner, D.A.; Granberry, R.; Engelhardt, S.; Haufe, F.L.; Peisner, J.D.; Walsh, C.J. Exploiting Textile Mechanical Anisotropy for Fabric-Based Pneumatic Actuators. Soft. Robot. 2018, 5, 662–674. [Google Scholar] [CrossRef] [PubMed]
- Ge, L.; Chen, F.; Wang, D.; Zhang, Y.; Han, D.; Wang, T.; Gu, G. Design, Modeling, and Evaluation of Fabric-Based Pneumatic Actuators for Soft Wearable Assistive Gloves. Soft. Robot. 2020, 7, 583–596. [Google Scholar] [CrossRef] [PubMed]
- Yap, H.K.; Lim, J.H.; Goh, J.C.H.; Yeow, C.-H. Design of a Soft Robotic Glove for Hand Rehabilitation of Stroke Patients With Clenched Fist Deformity Using Inflatable Plastic Actuators. J. Med. Devices 2016, 10, 044504. [Google Scholar] [CrossRef]
- Yin, J.; Zhao, Q.; Shen, Y.; He, B. P (LLA-co-PDO) copolymers with random and block architectures: Synthesis and characterizations. Appl. Polym. Sci. 2022, 139, e52410. [Google Scholar] [CrossRef]
- Tarvainen, T.V.J.; Fernandez-Vargas, J.; Yu, W. New Layouts of Fiber Reinforcements to Enable Full Finger Motion Assist with Pneumatic Multi-Chamber Elastomer Actuators. Actuators 2018, 7, 31. [Google Scholar] [CrossRef]
- Chen, Y.; Tan, X.; Yan, D.; Zhang, Z.; Gong, Y. A composite fabric-based soft rehabilitation glove with soft joint for dementia in Parkinson’s disease. IEEE J. Transl. Eng. Health Med. 2020, 8, 1–10. [Google Scholar] [CrossRef]
- Ben-Tzvi, P.; Ma, Z. Sensing and force-feedback exoskeleton (SAFE) robotic glove. IEEE Trans. Neural Syst. Rehabil. Eng. 2014, 23, 992–1002. [Google Scholar] [CrossRef]
- Yi, J.; Chen, X.; Wang, Z. A three-dimensional-printed soft robotic glove with enhanced ergonomics and force capability. IEEE Robot. Autom. Lett. 2017, 3, 242–248. [Google Scholar] [CrossRef]
- Gao, Z.; Xiao, X.; Carlo, A.D.; Yin, J.; Wang, Y.; Huang, L.; Tang, J.; Chen, J. Advances in Wearable Strain Sensors Based on Electrospun Fibers. Adv. Funct. Mater. 2023, 33, 2214265. [Google Scholar] [CrossRef]
- Xiao, X.; Yin, J.; Chen, G.; Shen, S.; Nashalian, A.; Chen, J. Bioinspired acoustic textiles with nanoscale vibrations for wearable biomonitoring. Matter 2022, 5, 1342–1345. [Google Scholar] [CrossRef]
- Meng, K.; Xiao, X.; Wei, W.; Chen, G.; Nashalian, A.; Shen, S.; Xiao, X.; Chen, J. Wearable Pressure Sensors for Pulse Wave Monitoring. Adv. Mater. 2022, 34, 2109357. [Google Scholar] [CrossRef]
- Zhao, S.; Wang, Z.; Lei, Y.; Zhang, J.; Li, Y.; Sun, Z.; Gong, Z. 3D-Printed Soft Pneumatic Robotic Digit Based on Parametric Kinematic Model for Finger Action Mimicking. Polymers 2022, 14, 2786. [Google Scholar] [CrossRef]
- Li, Y.; Yin, J.; Liu, S.; Xue, B.; Shokoohi, C.; Ge, G.; Hu, M.; Li, T.; Tao, X.; Rao, Z.; et al. Learning Hand Kinematics for Parkinson’s Disease Assessment Using a Multimodal Sensor Glove. Adv. Sci. 2023, 2206982. [Google Scholar] [CrossRef]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).