Experimental Analysis to Detect Corona COVID-19 Virus Symptoms in Male Patients through Breath Pattern Using Machine Learning Algorithms
Abstract
1. Introduction
2. Background
3. Human Breathe Pattern and Virus Detection
Corona COVID-19 Virus Dataset Challenge
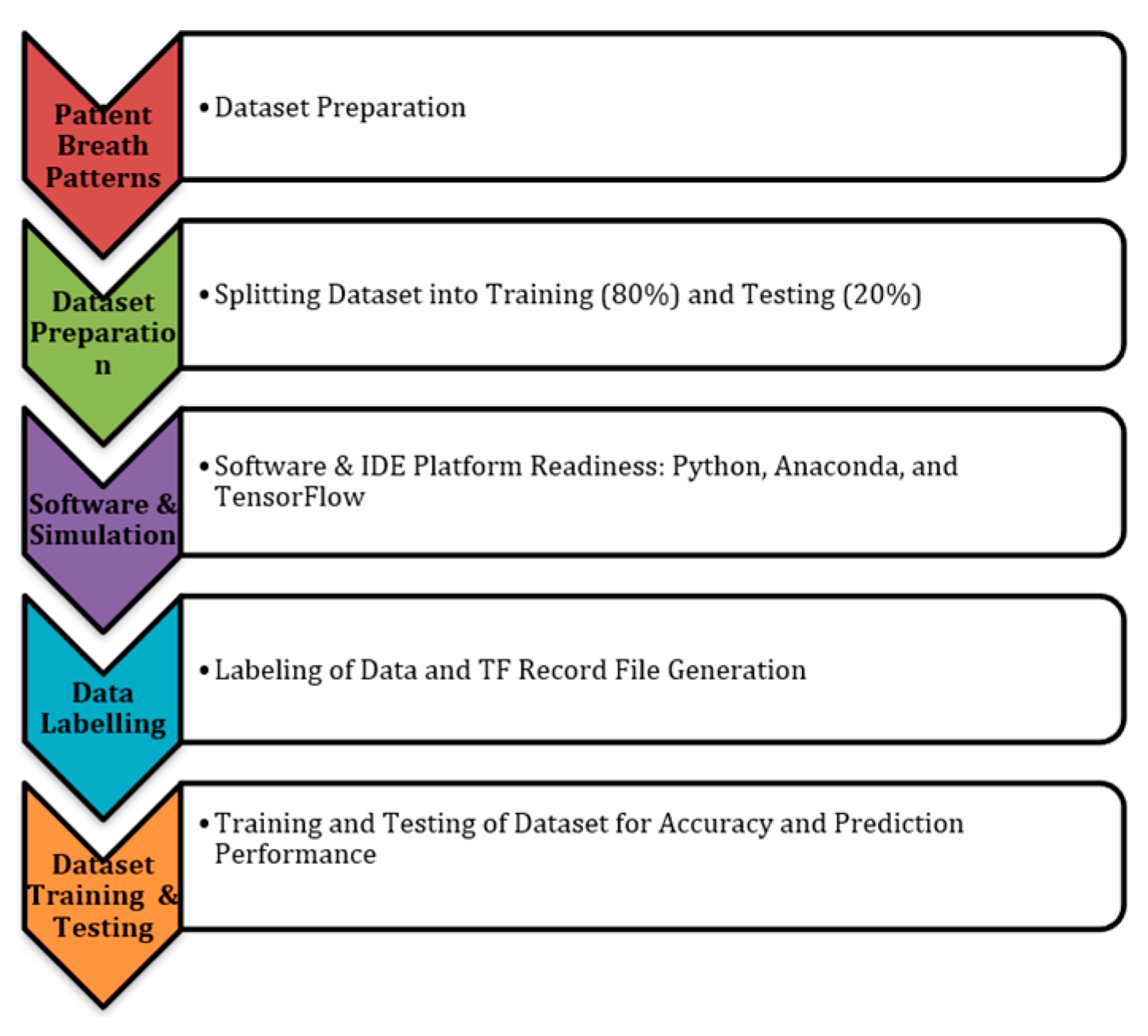
4. Breath Parameter and Dataset Preparation—The Implementation Strategy
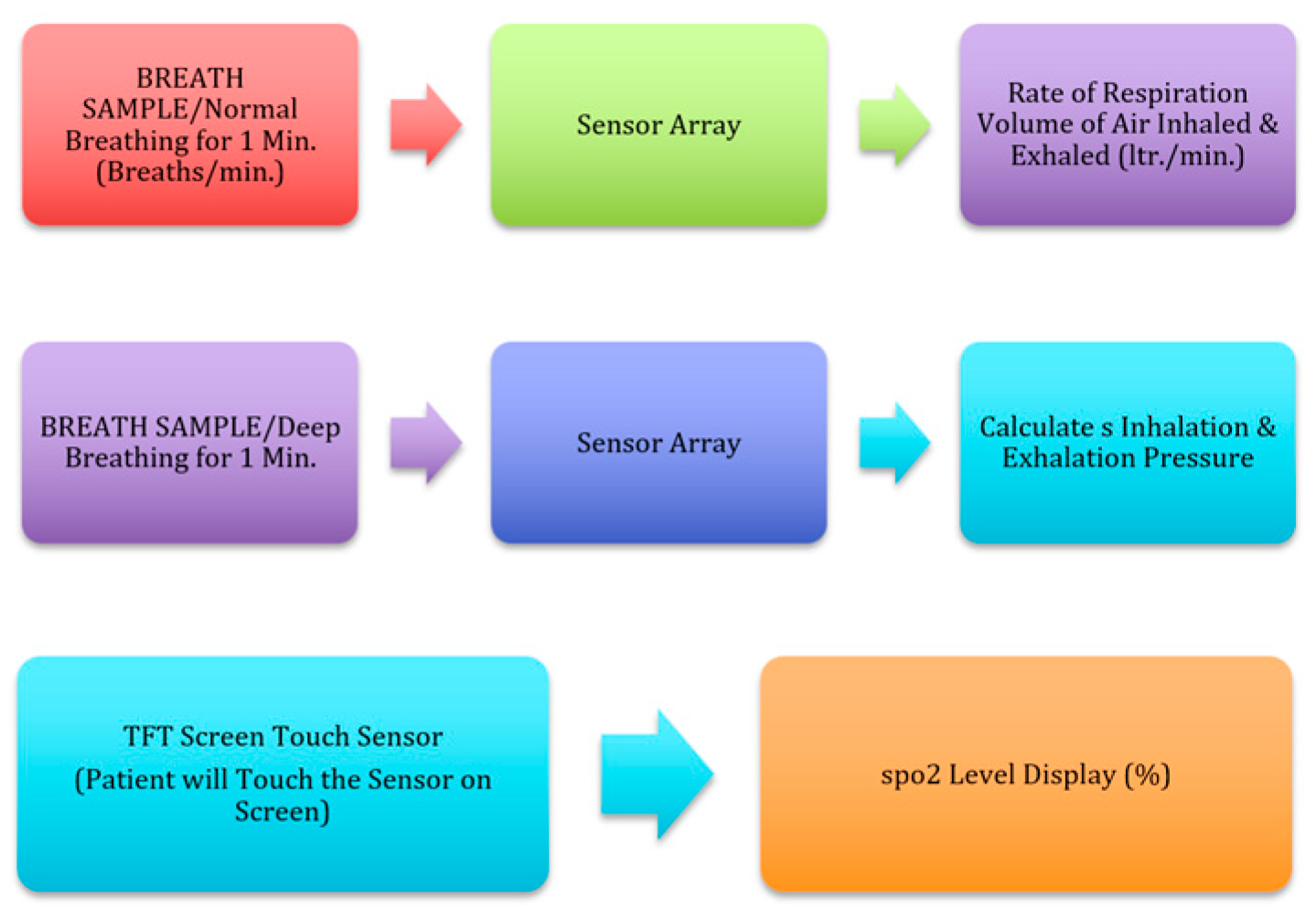
4.1. Electronic Spirometry (E-Spirometry) Analysis (Data Is Collected through the Mobile App)
- FEV1—forced expiratory volume in one second: the volume of air exhaled in the first second under force after a maximal inhalation (normal range FEV1 ≥ 80%).
- FEV1/FVC ratio: the percentage of the FVC expired in one second (normal range FEV1/FVC ≥ 70%).
- FEV6—forced expiratory volume in six seconds: the amount of air exhaled after full inhalation within the first six seconds under force (normal range FEV6 ≥ 80%). FEF25–75%—forced expiratory flow: the FEP over the middle one half of the FVC; the average flow from the point at which 25% of the FVC has been exhaled to the point at which 75% of the FVC has been exhaled.
- MVV—maximal voluntary ventilation: the volume of air expired in a specified period during repetitive maximal effort (normal range is 15–20 times and the resting minute volume average values for males and females are 140–180 and 80–120 L per minute, respectively).
- PEF—peak expiratory flow: the highest forced expiratory flow is measured with a peak flow meter (normal range is 400–700 L/min).
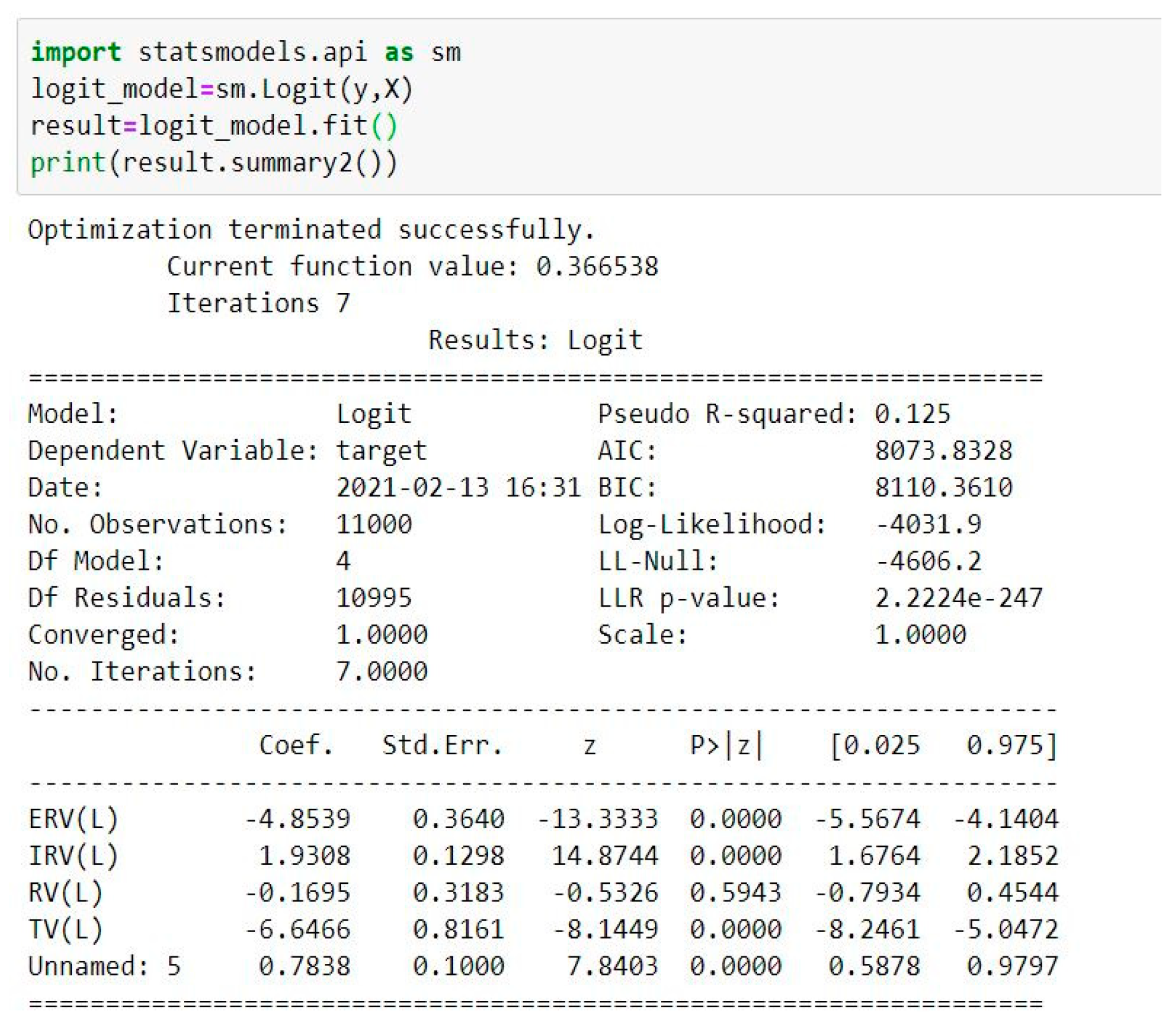
4.2. Lung Volumes Analysis
- ERV—expiratory reserve volume: at the end of each exhalation, the maximum amount of air exhaled (normal range = 1.1 L (males) and 0.7 L (females));
- IRV—inspiratory reserve volume: the maximum amount of air inhaled as a result of end-inspiration [40] (normal range = 3.3 L (males) and 1.9 L (females));
- RV—residual volume: after a maximal exhale, the amount of air left in the lungs [40] (normal range = 1.2 L (males) and 1.1 L (females));
- TV—tidal volume: during each respiratory cycle, the amount of air inhaled or exhaled (normal range = 0.5 L).
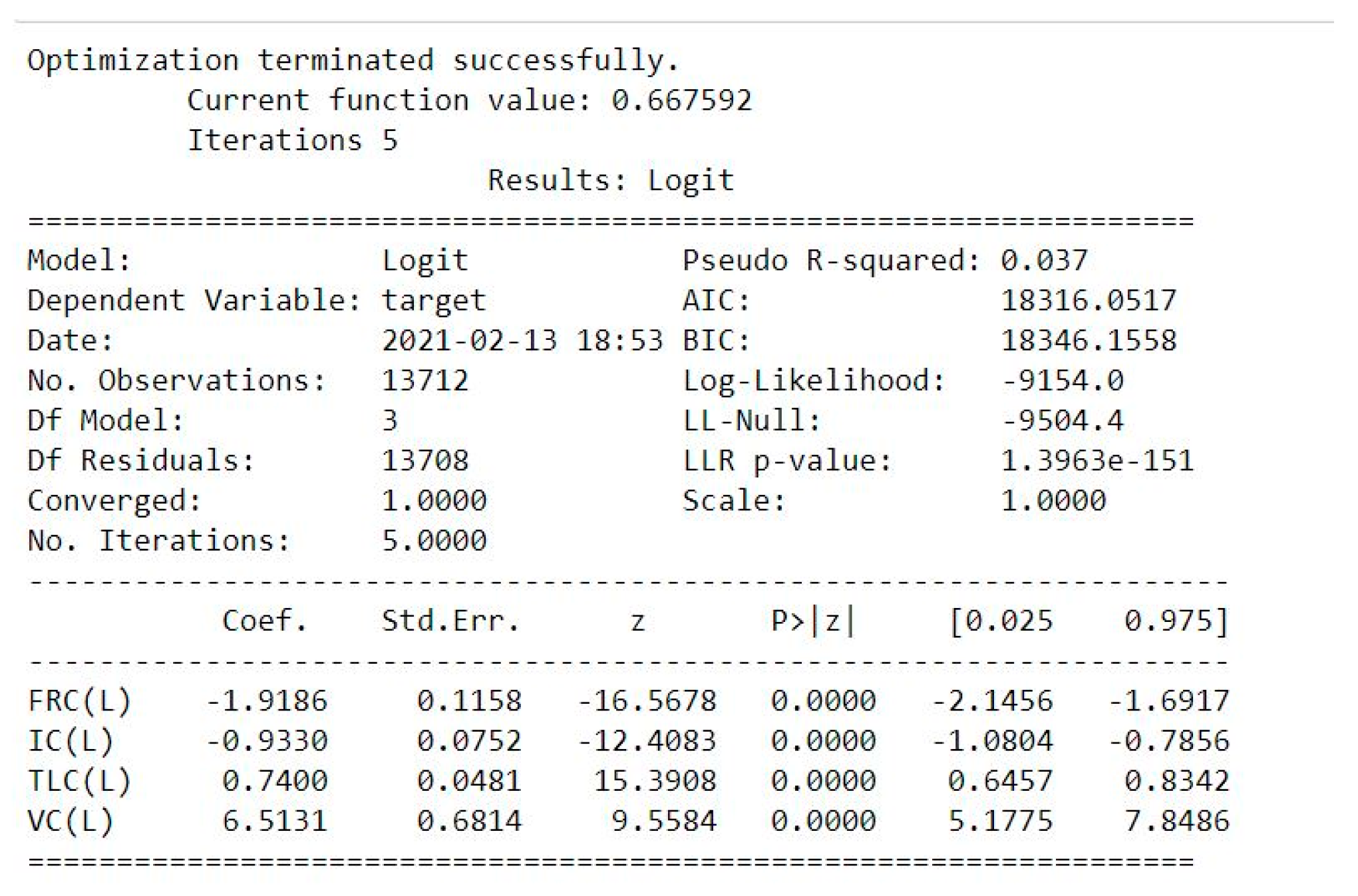
4.3. Lung Capacities Analysis
- FRC—functional residual capacity: at resting end-expiration, the volume of air in the lungs [41] (normal range = 2.4 L (males) and 1.8 L (females));
- IC—inspiratory capacity: from the resting expiratory level, the maximum volume of air that can be inhaled [41] (normal range = 3.8 L (males) and 2.4 L (females));
- TLC—total lung capacity: the amount of air in the lungs when fully inflated (normal range = 6.0 L (males) and 4.2 L (females));
- VC—vital capacity: after full inspiration, the highest volume is measured on complete exhale [40] (normal range = 4.8 L (males) and 3.1 L (females)).
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- World Health Organization. Middle East Respiratory Syndrome Coronavirus (MERS-CoV); WHO: Geneva, Switzerland, 2019; Available online: http://www.who.int/emergencies/mers-cov/en/ (accessed on 16 September 2022).
- Crawford, D.H. Viruses: A Very Short Introduction, 2nd ed.; Oxford University Press Print: Oxford, UK, 2018; ISBN 13 9780198811718. [Google Scholar] [CrossRef]
- European Centre for Disease Control and Prevention Rapid Risk Assessment. Outbreak of Severe Acute Respiratory Syndrome Coronavirus 2 (SARS-CoV-2): Increased Transmission beyond China—Fourth Update; ECDC: Stockholm, Sweden, 2020. [Google Scholar]
- Zaki, A.M.; van Boheemen, S.; Bestebroer, T.M.; Osterhaus, A.D.M.E.; Fouchier, R.A.M. Isolation of a novel coronavirus from a man with pneumonia in Saudi Arabia. N. Engl. J. Med. 2012, 367, 1814–1820. [Google Scholar] [CrossRef] [PubMed]
- Bhargava, A.; Shewade, H.D. The potential impact of the COVID-19 response-related lockdown on TB incidence and mortality in India. Indian J. Tuberc. 2020, 67, S139–S146. [Google Scholar] [CrossRef] [PubMed]
- Coronavirus disease (COVID-19) Pandemic. World Health Organization (WHO). 7 July 2020. Available online: https://www.who.int/emergencies/diseases/novel-coronavirus-2019 (accessed on 16 September 2022).
- Diamond, F. Asymptomatic Carriers May Play a Huge Part in COVID-19 Surge. 12 January 2021. Available online: https://www.infectioncontroltoday.com/view/asymptomatic-carriers-may-play-a-huge-part-in-covid-19-surge (accessed on 16 September 2022).
- Edwards, R.; Davidson, E.; Jamieson, L.; Weller, S. Theory and the breadth-and-depth method of analyzing large amounts of qualitative data: A research note. Qual. Quant. 2021, 55, 1275–1280. [Google Scholar] [CrossRef]
- Adiguzel, Y.; Kulah, H. Breath sensors for lung cancer diagnosis. Biosens. Bioelectron. 2015, 65, 121–138. [Google Scholar] [CrossRef]
- Kononov, A.; Korotetsky, B.; Jahatspanian, I.; Gubal, A.; Vasiliev, A.; Arsenjev, A.; Nefedov, A.; Barchuk, A.; Gorbunov, I.; Kozyrev, K.; et al. Online breath analysis using metal oxide semiconductor sensors (electronic nose) for diagnosis of lung cancer. J. Breath Res. 2019, 14, 016004. [Google Scholar] [CrossRef]
- Rehman, A.U.; Jiang, A.; Rehman, A.; Paul, A.; Din, S.; Sadiq, M.T. Identification and role of opinion leaders in information diffusion for online discussion network. J. Ambient. Intell. Humaniz. Comput. 2020, 1–13. [Google Scholar] [CrossRef]
- Rehman, A.U.; Tariq, R.; Rehman, A.; Paul, A. Collapse of Online Social Networks: Structural Evaluation, Open Challenges, and Proposed Solutions. In Proceedings of the 2020 IEEE Globecom Workshops (GC Wkshps), Taipei, Taiwan, 7–11 December 2020; pp. 1–6. [Google Scholar] [CrossRef]
- Davidson, E.; Edwards, R.; Jamieson, L.; Weller, S. Big data, qualitative style: A breadth-and-depth method for working with large amounts of secondary qualitative data. Qual. Quant. 2018, 53, 363–376. [Google Scholar] [CrossRef]
- Priftis, K.N.; Hadjileontiadis, L.J.; Everard, M.L. Breath Sounds. In From Basic Science to Clinical Practice, 1st ed.; Springer: Cham, Switzerland, 2018. [Google Scholar] [CrossRef]
- Valenti, M.; Tonelli, D.; Vesperini, F.; Principi, E.; Squartini, S. A Neural Network Approach for Sound Event Detection in Real Life Audio. In Proceedings of the 2017 25th European Signal Processing Conference (EUSIPCO), Kos, Greece, 28 August–2 September 2017. [Google Scholar] [CrossRef]
- Nakhleh, M.K.; Amal, H.; Jeries, R.; Broza, Y.Y.; Aboud, M.; Gharra, A.; Ivgi, H.; Khatib, S.; Badarneh, S.; Har-Shai, L.; et al. Diagnosis and classification of 17 diseases from 1404 subjects via pattern analysis of exhaled molecules. ACS Nano 2017, 11, 112–125. [Google Scholar] [CrossRef]
- Lee, S.J.; Motai, Y.; Weiss, E.; Sun, S.S. Irregular Breathing Classification From Multiple Patient Datasets Using Neural Networks. IEEE Trans. Inf. Technol. Biomed. 2012, 16, 1253–1264. [Google Scholar]
- Ardabili, S.; Mosavi, A.; Ghamisi, P.; Ferdinand, F.; Varkonyi-Koczy, A.; Reuter, U.; Rabczuk, T.; Atkinson, P. COVID-19 Outbreak Prediction with Machine Learning. Algorithms 2020, 13, 249. [Google Scholar] [CrossRef]
- Mok, K. Scientists’ Artificially Intelligent Nanoarray Can Diagnose Disease Using Your Breath. 8 January 2017. Available online: https://thenewstack.io/scientists-artificially-intelligent-nanoarray-can-diagnose-disease-using-breath/ (accessed on 16 September 2022).
- UNICEF for Every Child. What Is the Difference between Home Self-Isolation and Quarantine? Ministry of Health, Romania. Available online: https://www.unicef.org/romania/documents/what-difference-between-home-self-isolation-and-quarantine (accessed on 16 September 2022).
- Ahmed, M.A.; Colebunders, R.; Fodjo, J.N.S. Evidence for significant COVID-19 community transmission in Somalia using a clinical case definition. Int. J. Infect. Dis. 2020, 98, 206–207. [Google Scholar] [CrossRef] [PubMed]
- Pitol, A.K.; Julian, T.R. Community Transmission of SARS-CoV-2 by Surfaces: Risks and Risk Reduction Strategies. Environ. Sci. Technol. Lett. 2021, 8, 263–269. [Google Scholar] [CrossRef]
- Nguyen, G.; Dlugolinsky, S.; Bobák, M.; Tran, V.; García, L.; Heredia, I.; Malík, P.; Hluchý, L. Machine Learning and Deep Learning frameworks and libraries for large-scale data mining: A survey. Artif. Intell. Rev. 2019, 52, 77–124. [Google Scholar] [CrossRef]
- Nazemi, E.; Roshani, G.H.; Feghhi, S.A.H.; Setayeshi, S.; Zadeh, E.E.; Fatehi, A. Optimization of a method for identifying the flow regime and measuring void fraction in a broad beam gamma-ray attenuation technique. Int. J. Hydrogen Energy 2016, 41, 7438–7444. [Google Scholar] [CrossRef]
- Shukla, N.K.; Mayet, A.M.; Vats, A.; Aggarwal, M.; Raja, R.K.; Verma, R.; Muqeet, M.A. High speed integrated RF–VLC data communication system: Performance constraints and capacity considerations. Phys. Commun. 2021, 50, 101492. [Google Scholar] [CrossRef]
- Roshani, G.H.; Nazemi, E.; Feghhi, S.A.; Setayeshi, S. Flow regime identification and void fraction prediction in two-phase flows based on gamma ray attenuation. Measurment 2015, 62, 25–32. [Google Scholar] [CrossRef]
- Mayet, A.; Hussain, M. Amorphous WNx Metal for Accelerometers and Gyroscope. In Proceedings of the MRS Fall Meeting, Boston, MA, USA, 30 November–5 December 2014. [Google Scholar]
- Karami, A.; Roshani, G.H.; Khazaei, A.; Nazemi, E.; Fallahi, M. Investigation of different sources in order to optimize the nuclear metering system of gas–oil–water annular flows. Neural Comput. Appl. 2018, 32, 3619–3631. [Google Scholar] [CrossRef]
- Mayet, A.; Smith, C.; Hussain, M.M. Amorphous metal based nanoelectromechanical switch. In Proceedings of the 2013 Saudi International Electronics, Communications and Photonics Conference (SIECPC), Riyadh, Saudi Arabia, 27–30 April 2013; pp. 1–5. [Google Scholar]
- Nazemi, E.; Feghhi, S.A.H.; Roshani, G.H.; Peyvandi, R.G.; Setayeshi, S. Precise Void Fraction Measurement in Two-phase Flows Independent of the Flow Regime Using Gamma-ray Attenuation. Nucl. Eng. Technol. 2016, 48, 64–71. [Google Scholar] [CrossRef]
- Mayet, A.M.; Alizadeh, S.M.; Kakarash, Z.A.; Al-Qahtani, A.A.; Alanazi, A.K.; Alhashimi, H.H.; Eftekhari-Zadeh, E.; Nazemi, E. Introducing a Precise System for Determining Volume Percentages Independent of Scale Thickness and Type of Flow Regime. Mathematics 2022, 10, 1770. [Google Scholar] [CrossRef]
- Alanazi, A.K.; Alizadeh, S.M.; Nurgalieva, K.S.; Nesic, S.; Guerrero, J.W.G.; Abo-Dief, H.M.; Eftekhari-Zadeh, E.; Nazemi, E.; Narozhnyy, I.M. Application of Neural Network and Time-Domain Feature Extraction Techniques for Determining Volumetric Percentages and the Type of Two Phase Flow Regimes Independent of Scale Layer Thickness. Appl. Sci. 2022, 12, 1336. [Google Scholar] [CrossRef]
- Mayet, A.M.; Alizadeh, S.M.; Nurgalieva, K.S.; Hanus, R.; Nazemi, E.; Narozhnyy, I.M. Extraction of Time-Domain Characteristics and Selection of Effective Features Using Correlation Analysis to Increase the Accuracy of Petroleum Fluid Monitoring Systems. Energies 2022, 15, 1986. [Google Scholar] [CrossRef]
- Hosseini, S.; Taylan, O.; Abusurrah, M.; Akilan, T.; Nazemi, E.; Eftekhari-Zadeh, E.; Bano, F.; Roshani, G.H. Application of Wavelet Feature Extraction and Artificial Neural Networks for Improving the Performance of Gas–Liquid Two-Phase Flow Meters Used in Oil and Petrochemical Industries. Polymers 2021, 13, 3647. [Google Scholar] [CrossRef]
- Mayet, A.; Smith, C.E.; Hussain, M.M. Energy reversible switching from amorphous metal based nanoelectromechanical switch. In Proceedings of the 2013 13th IEEE Conference on Nanotechnology (IEEE-NANO), Beijing, China, 5–8 August 2013; pp. 366–369. [Google Scholar]
- Roshani, G.; Hanus, R.; Khazaei, A.; Zych, M.; Nazemi, E.; Mosorov, V. Density and velocity determination for single-phase flow based on radiotracer technique and neural networks. Flow Meas. Instrum. 2018, 61, 9–14. [Google Scholar] [CrossRef]
- Mayet, A.M.; Salama, A.S.; Alizadeh, S.M.; Nesic, S.; Guerrero, J.W.G.; Eftekhari-Zadeh, E.; Nazemi, E.; Iliyasu, A.M. Applying Data Mining and Artificial Intelligence Techniques for High Precision Measuring of the Two-Phase Flow’s Characteristics Independent of the Pipe’s Scale Layer. Electronics 2022, 11, 459. [Google Scholar] [CrossRef]
- Iliyasu, A.M.; Alizadeh, S.M.; Salama, A.S.; Nazemi, E.; Hirota, K. Application of artificial intelligence to calculate the volume percentages of a stratified regime three-phase flow regardless of the pipe’s scale thickness. Appl. Sci. 2022, 10, 1996. [Google Scholar] [CrossRef]
- Mayet, A.; Hussain, A.; Hussain, M. Three-terminal nanoelectromechanical switch based on tungsten nitride, an amorphous metallic material. Nanotechnology 2016, 27. [Google Scholar] [CrossRef] [PubMed]
- Thafasal Ijyas, V.P.; Mayet, A.M. Electronic circuit implementation of the compartmental models for population dynamics of COVID-19 like epidemics. Sādhanā 2022, 47, 1–6. [Google Scholar] [CrossRef]
- Barreiro, T.J.; Perillo, I. An approach to interpreting spirometry. Am. Fam. Physician 2004, 69, 1107–1114. [Google Scholar] [PubMed]




| Parameter | FVC | FEV1 | RATIO FEV1/FVC | FEV6 | FEF | MVV | PEF |
|---|---|---|---|---|---|---|---|
| Normal | 80% or more | 80% or more/second | 70% or more | 80%/6 s or more | 25–75% | 140–180 per liter per minute (Male)80–120 per liter per minute (Female) | 400–700 L/min |
| Parameter | ERV | IRV | RV | TV |
|---|---|---|---|---|
| Normal | 1.2 L (Male) 0.7 L (Female) | 3.3 L (Male) 1.9 L (Female) | 1.2 L (Male) 1.1 L (Female) | 0.5 L |
| Parameter | FRC | IC | TLC | VC |
|---|---|---|---|---|
| Normal | 2.4 L (Male) 1.8 L (Female) | 3.8 L (Male) 2.4 L (Female) | 6.0 L (Male) 4.2 L (Female) | 4.8 L (Male) 3.1 L (Female) |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Mayet, A.M.; Shukla, N.K.; Raja, M.R.; Ahmad, I.; Aiesh Qaisi, R.M.; Al-Qahtani, A.A.; Taparwal, A.; Tirth, V.; AL-Dossary, R. Experimental Analysis to Detect Corona COVID-19 Virus Symptoms in Male Patients through Breath Pattern Using Machine Learning Algorithms. Electronics 2023, 12, 10. https://doi.org/10.3390/electronics12010010
Mayet AM, Shukla NK, Raja MR, Ahmad I, Aiesh Qaisi RM, Al-Qahtani AA, Taparwal A, Tirth V, AL-Dossary R. Experimental Analysis to Detect Corona COVID-19 Virus Symptoms in Male Patients through Breath Pattern Using Machine Learning Algorithms. Electronics. 2023; 12(1):10. https://doi.org/10.3390/electronics12010010
Chicago/Turabian StyleMayet, Abdulilah Mohammad, Neeraj Kumar Shukla, M. Ramkumar Raja, Ijaz Ahmad, Ramy Mohammed Aiesh Qaisi, Ali Awadh Al-Qahtani, Anita Taparwal, Vineet Tirth, and Reem AL-Dossary. 2023. "Experimental Analysis to Detect Corona COVID-19 Virus Symptoms in Male Patients through Breath Pattern Using Machine Learning Algorithms" Electronics 12, no. 1: 10. https://doi.org/10.3390/electronics12010010
APA StyleMayet, A. M., Shukla, N. K., Raja, M. R., Ahmad, I., Aiesh Qaisi, R. M., Al-Qahtani, A. A., Taparwal, A., Tirth, V., & AL-Dossary, R. (2023). Experimental Analysis to Detect Corona COVID-19 Virus Symptoms in Male Patients through Breath Pattern Using Machine Learning Algorithms. Electronics, 12(1), 10. https://doi.org/10.3390/electronics12010010





