Could Avatar Therapy Enhance Mental Health in Chronic Patients? A Systematic Review
Abstract
:1. Introduction
2. Materials and Methods
2.1. General Description
2.2. Scientific Literature Review
2.3. Data
2.4. Risk of Methodological Bias
3. Results
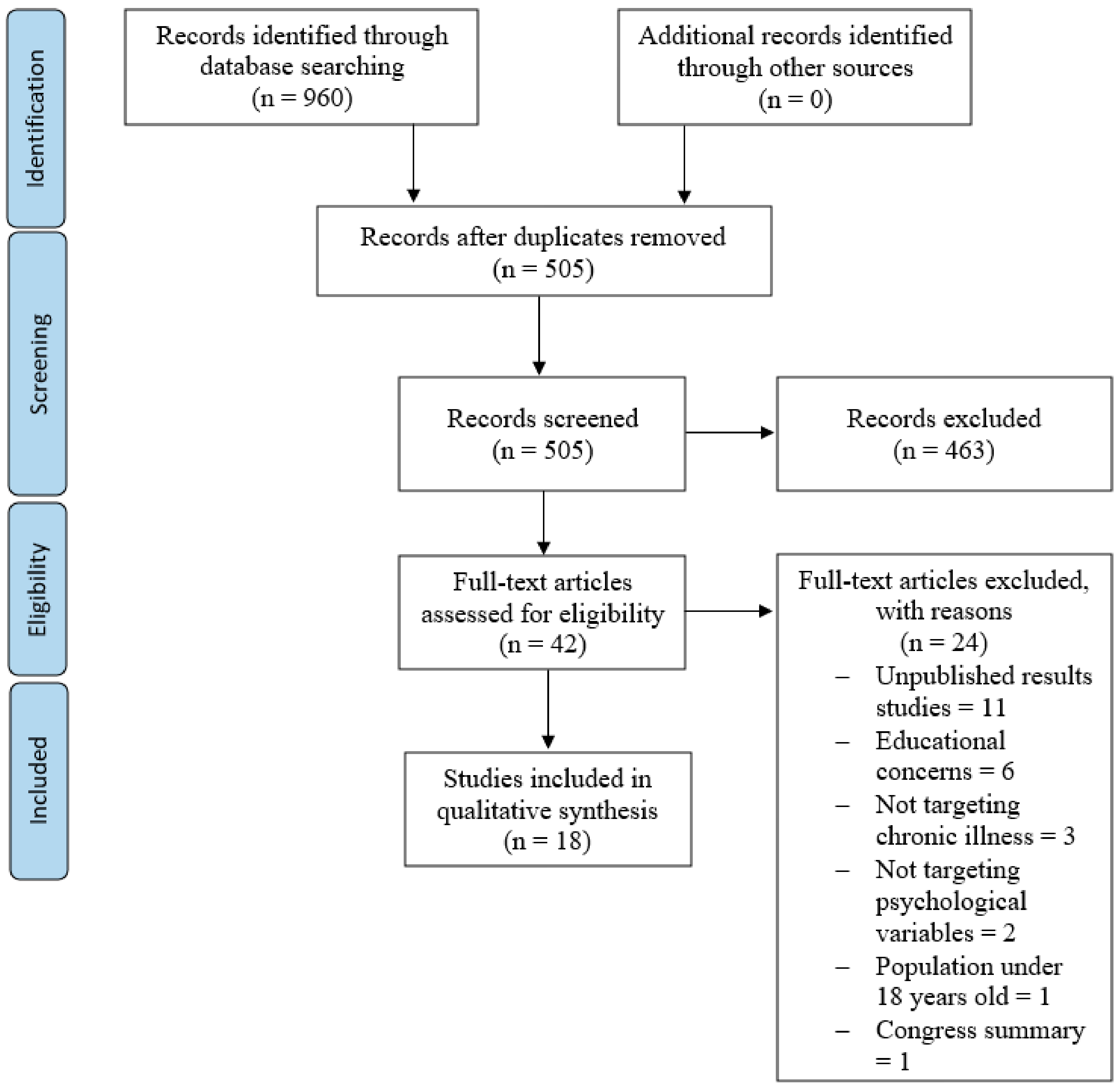
3.1. Study Selection and Inclusion
3.2. Characteristics of the Studies Included
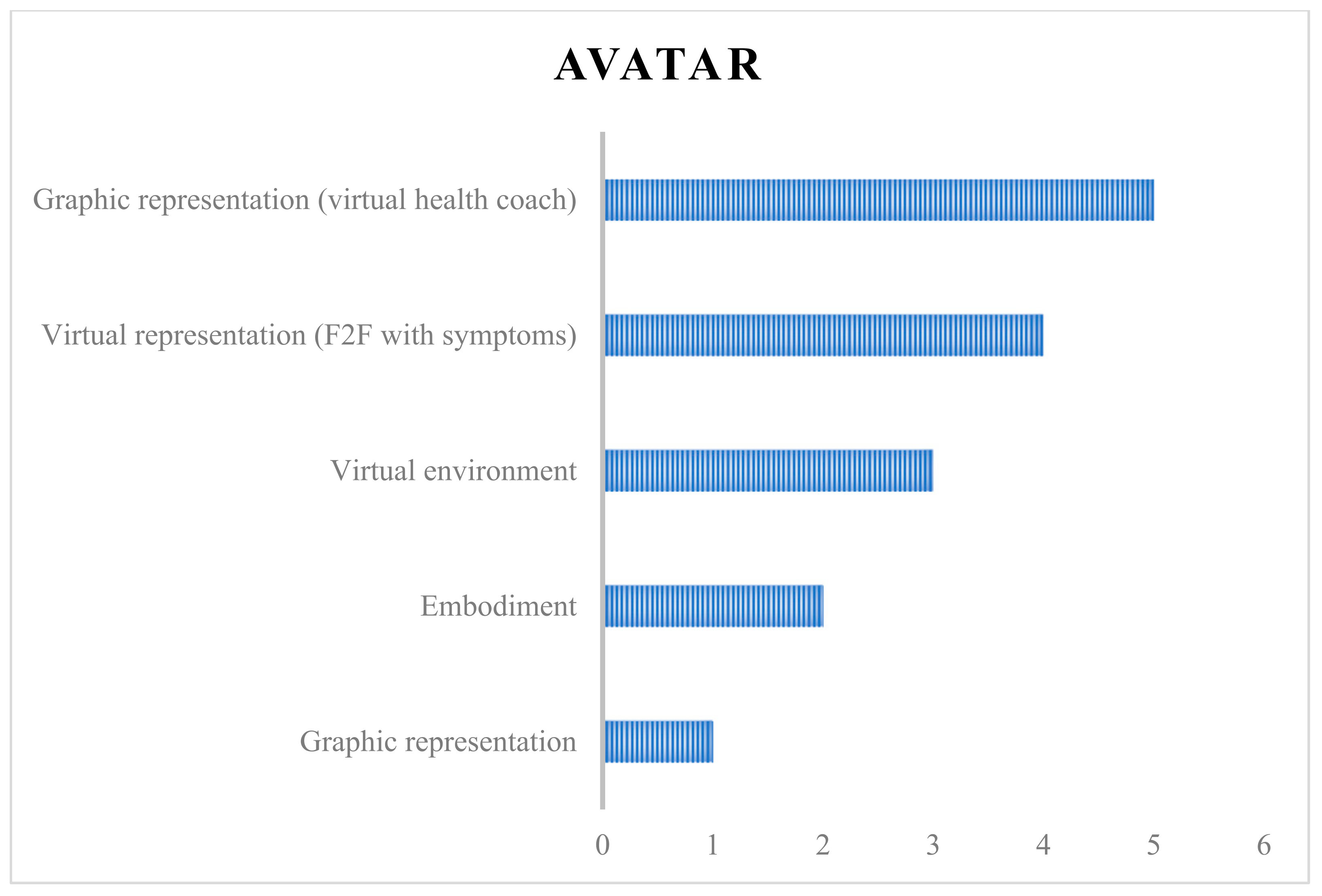
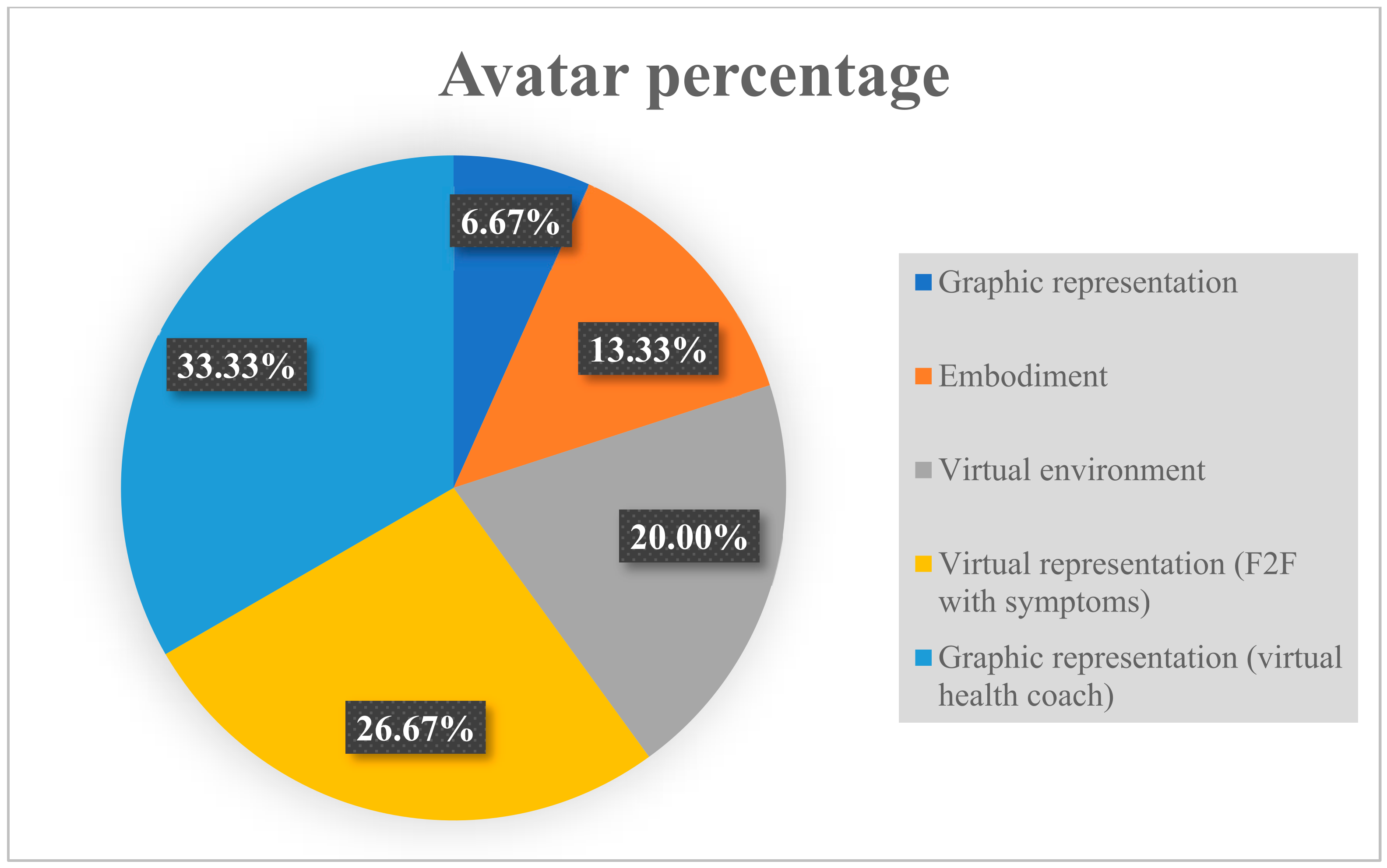
- Modality 1 (Graphic representation)—The avatar as a “virtual twin” without interaction with the patient. The simplest modality, from a technological point of view, this involved a two-dimensional graphic representation produced on a mobile or tablet screen, with the avatar representing the user. In the study in which this modality was used (n = 1) [56], the patients with breast cancer experienced a higher degree of identification with the avatar, given that they were able to personalize it to have a greater level of physical similarity to them.
- Modality 2 (Virtual representation: F2F with symptoms)—The avatar as “another virtual patient that interacts only with the patient”. This was a two-dimensional virtual representation of an avatar that embodied the symptoms of the user and with which they could communicate face to face. It was the second most used modality (n = 4) [42,46,53,55], and the objective of the studies that applied this kind of avatar was to make subjects confront their own auditory hallucinations in a face-to-face conversation, so that, with help from the therapist, who also guided the avatar, they could gradually take control of these hallucinations.
- Modality 3 (Virtual environment)—The avatar as a “virtual twin that interacts with the avatars of other patients”. This modality involved a digital self-representation in a non-immersive, two-dimensional virtual environment (n = 3) [25,45,52]. Here, the users could interact with other people, also represented by avatars, on a screen through a written and/or audio messaging platform. The fact that it was not immersive meant that the virtual environment was two-dimensional rather than three-dimensional and users did not receive sensory stimuli, which does occur in immersive experiences. Two of the studies that used this modality [25,45] used the Second Life© platform (SL), and, while one [25] allowed users to personalize the avatar, the other [45] did not specify whether the users adapted the avatars to resemble themselves. The other study [52] used the ProReal© platform, and the degree of identification with the avatar was low, as the representations consisted of colorless silhouettes with neither facial nor bodily elements.
- Modality 4 (Embodiment)—The avatar as a “virtual incarnation that interacts with the avatars of other patients”. This modality entailed the incarnation of an avatar from a first-person perspective using a virtual reality device called a head-mounted display (HMD) (n = 2), which creates a three-dimensional, non-immersive virtual environment that reduced the users’ feeling of pain [47] or improved their verbal communication via the movements and gestures involved in operating the avatar [44];
- Modality 5 (Graphic representation: virtual health coach)—The avatar as “coach” that only interacts with the patient. The graphic representation here could also comprise an avatar that represented a person other than the user. This was the modality most frequently used (n = 5), [3,6,43,48,50]. Here, the avatar was used as a virtual health coach that guided and instructed the user in managing their illness. In one study using this modality [6], two types of avatars were used: one with a high degree of physical resemblance to the patient, a self-avatar “peer” mentor (SAP) that produced an increased sense of identification; and another that had no physical resemblance to the user, a generic avatar coach (GAC), the sense of identification with which was consequentially lower.
| Study | Avatar | Identification | Device |
|---|---|---|---|
| Aali et al. [42] | F2F with symptoms | No | Computerized system |
| Andrade et al. [6] | Virtual health coach | Both | Online platform |
| Cho et al. [43] | Virtual health coach | Yes | Not applicable |
| Clarke et al. [55] | F2F with symptoms | No | Computerized system |
| Dang et al. [44] | Embodiment | Yes | Headset |
| du Sert et al. [54] | Embodiment and F2F with symptoms | Both | Headset |
| Falconer et al. [52] | Virtual environment | No | VR software |
| Leff et al. [53] | F2F with symptoms | No | Computerized system |
| Pinto et al. [48] | Virtual health coach | No | Screen-based |
| Robinson-Whelen et al. [45] | Virtual environment | Not applicable | Online platform |
| Rus-Calafell et al. [46] | F2F with symptoms | No | Not applicable |
| Stewart et al. [25] | Virtual environment | Not applicable | Online platform |
| Thomas et al. [49] | Several types of avatars | Not applicable | Not applicable |
| Tong et al. [47] | Embodiment | Yes | Headset |
| Tongpeth et al. [50] | Virtual health coach | No | App |
| Triberti et al. [56] | Graphic representation | Yes | App |
| Wonggom et al. [51] | Several types of avatars | Not applicable | Not applicable |
| Wonggom et al. [3] | Virtual health coach | No | App |
| Study | Effectiveness | Patient Satisfaction Measured |
|---|---|---|
| Aali et al. [42] | No | Unknown |
| Andrade et al. [6] | Yes | Unknown |
| Cho et al. [43] | Yes | Yes |
| Clarke et al. [55] | No | Unknown |
| Dang et al. [44] | No | Yes |
| du Sert et al. [54] | Yes | Unknown |
| Falconer et al. [52] | No | Yes |
| Leff et al. [53] | Yes | Unknown |
| Pinto et al. [48] | Yes | Unknown |
| Robinson-Whelen et al. [45] | Yes | Yes |
| Rus-Calafell et al. [46] | Yes | Unknown |
| Stewart et al. [25] | Unknown | Yes |
| Thomas et al. [49] | Unknown | Unknown |
| Tong et al. [47] | Yes | Unknown |
| Tongpeth et al. [50] | Yes | Yes |
| Triberti et al. [56] | Unknown | Unknown |
| Wonggom et al. [51] | Yes | Yes |
| Wonggom et al. [3] | Yes | Yes |
4. Discussion
5. Conclusions
5.1. Clinical and Researcher Implications
5.2. Limitations
Supplementary Materials
Author Contributions
Funding
Data Availability Statement
Conflicts of Interest
References
- World Health Organization. Global Status Report on Noncommunicable Diseases 2014; World Health Organization: Geneva, Switzerland, 2015. [Google Scholar]
- Kang, E.; Kim, S.; Rhee, Y.E.; Lee, J.; Yun, Y.H. Self-management strategies and comorbidities in chronic disease patients: Associations with quality of life and depression. Psychol. Health Med. 2021, 26, 1031–1043. [Google Scholar] [CrossRef] [PubMed]
- Wonggom, P.; Nolan, P.; Clark, R.A.; Barry, T.; Burdeniuk, C.; Nesbitt, K.; O’Toole, K.; Du, H. Effectiveness of an avatar educational application for improving heart failure patients’ knowledge and self-care behaviors: A pragmatic randomized controlled trial. J. Adv. Nurs. 2020, 76, 2401–2415. [Google Scholar] [CrossRef]
- Fehily, C.; Hodder, R.; Bartlem, K.; Wiggers, J.; Wolfenden, L.; Dray, J.; Bailey, J.; Wilczynska, M.; Stockings, E.; Clinton-McHarg, T.; et al. The effectiveness of interventions to increase preventive care provision for chronic disease risk behaviours in mental health settings: A systematic review and meta-analysis. Prev. Med. Rep. 2020, 19, 101–108. [Google Scholar] [CrossRef] [PubMed]
- Golubić, M.; Schneeberger, D.; Kirkpatrick, K.; Bar, J.; Bernstein, A.; Weems, F.; Ehrman, J.; Perko, J.; Doyle, J.; Roizen, M. Comprehensive Lifestyle Modification Intervention to Improve Chronic Disease Risk Factors and Quality of Life in Cancer Survivors. J. Altern. Complement. Med. 2018, 24, 1085–1091. [Google Scholar] [CrossRef] [PubMed]
- Andrade, A.D.; Anam, R.; Karanam, C.; Downey, P.; Ruiz, J.G. An Overactive Bladder Online Self-management Program with Embedded Avatars: A Randomized Controlled Trial of Efficacy. Urology 2015, 85, 561–567. [Google Scholar] [CrossRef]
- Rehm, I.C.; Foenander, E.; Wallace, K.; Abbott, J.-A.M.; Kyrios, M.; Thomas, N. What Role Can Avatars Play in e-Mental Health Interventions? Exploring New Models of Client–Therapist Interaction. Front. Psychiatry 2016, 7, 186. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Liu, Y.; Liu, Y.; Xu, S.; Cheng, K.; Masuko, S.; Tanaka, J. Comparing VR- and AR-Based Try-On Systems Using Personalized Avatars. Electronics 2020, 9, 1814. [Google Scholar] [CrossRef]
- Knoblock-Hahn, A.L.; Wray, R.; LeRouge, C.M. Perceptions of adolescents with overweight and obesity for the development of user-centered design self-management tools within the context of the chronic care model: A qualitative study. J. Acad. Nutr. Diet. 2016, 116, 957–967. [Google Scholar] [CrossRef] [PubMed]
- Rheu, M.; Jang, Y.; Peng, W. Enhancing Healthy Behaviors through Virtual Self: A Systematic Review of Health Interventions Using Avatars. Games Health J. 2020, 9, 85–94. [Google Scholar] [CrossRef] [PubMed]
- Yoshida-Montezuma, Y.; Ahmed, M.; Ezezika, O. Does gamification improve fruit and vegetable intake in adolescents? A systematic review. Nutr. Health 2020, 26, 347–366. [Google Scholar] [CrossRef] [PubMed]
- Burton, C.; Tatar, A.S.; McKinstry, B.; Matheson, C.; Matu, S.; Moldovan, R.; Macnab, M.; Farrow, E.; David, D.; Pagliari, C.; et al. Pilot randomised controlled trial of Help4Mood, an embodied virtual agent-based system to support treatment of depression. J. Telemed. Telecare 2016, 22, 348–355. [Google Scholar] [CrossRef] [Green Version]
- Porras-Garcia, B.; Serrano-Troncoso, E.; Carulla-Roig, M.; Soto-Usera, P.; Ferrer-Garcia, M.; Figueras-Puigderrajols, N.; Yilmaz, L.; Sen, Y.O.; Shojaeian, N.; Gutiérrez-Maldonado, J. Virtual Reality Body Exposure Therapy for Anorexia Nervosa. A Case Report with Follow-Up Results. Front. Psychol. 2020, 11, 956. [Google Scholar] [CrossRef]
- Ralph-Nearman, C.; Arevian, A.C.; Moseman, S.; Sinik, M.; Chappelle, S.; Feusner, J.D.; Khalsa, S.S. Visual mapping of body image disturbance in anorexia nervosa reveals objective markers of illness severity. Sci. Rep. 2021, 11, 1–12. [Google Scholar] [CrossRef] [PubMed]
- Hone-Blanchet, A.; Wensing, T.; Fecteau, S. The Use of Virtual Reality in Craving Assessment and Cue-Exposure Therapy in Substance Use Disorders. Front. Hum. Neurosci. 2014, 8, 844. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Skeva, R.; Gregg, L.; Jay, C.; Pettifer, S. Views of Practitioners and Researchers on the Use of Virtual Reality in Treatments for Substance Use Disorders. Front. Psychol. 2021, 12, 1852. [Google Scholar] [CrossRef] [PubMed]
- Hartanto, D.W.; Kang, N.; Brinkman, W.-P.; Kampmann, I.L.; Morina, N.; Emmelkamp, P.G.M.; Neerincx, M.A. Automatic mechanisms for measuring subjective unit of discomfort. Stud. Health Technol. Inform. 2012, 181, 192–196. [Google Scholar] [PubMed]
- Holmberg, T.T.; Eriksen, T.L.; Petersen, R.; Frederiksen, N.N.; Damgaard-Sørensen, U.; Lichtenstein, M.B. Social Anxiety Can Be Triggered by 360-Degree Videos in Virtual Reality: A Pilot Study Exploring Fear of Shopping. Cyberpsychol. Behav. Soc. Netw. 2020, 23, 495–499. [Google Scholar] [CrossRef] [PubMed]
- James, L.K.; Lin, C.-Y.; Steed, A.; Swapp, D.; Slater, M. Social Anxiety in Virtual Environments: Results of a Pilot Study. Cyberpsychol. Behav. 2003, 6, 237–243. [Google Scholar] [CrossRef]
- Peñate, W.; Pitti, C.T.; Bethencourt, J.M.; de la Fuente, J.; Gracia, R. The effects of a treatment based on the use of virtual reality exposure and cognitive-behavioral therapy applied to patients with agoraphobia. Int. J. Clin. Health Psychol. 2008, 8, 5–22. [Google Scholar]
- Foronda, C.; Gattamorta, K.; Snowden, K.; Bauman, E.B. Use of virtual clinical simulation to improve communication skills of baccalaureate nursing students: A pilot study. Nurse Educ. Today 2014, 34, e53–e57. [Google Scholar] [CrossRef] [PubMed]
- Hay, L.; Pymm, B. Real learning in a virtual world: A case study of the school of information studies’ learning centre in Second Life. Educ. Inf. 2011, 28, 187–202. [Google Scholar] [CrossRef]
- Lange, E.J. Teachlive: A Qualitative Study on Pre-Services Teachers’ Perspectives. Ph.D. Thesis, Lamar University, Beaumont, TX, USA, 2019. [Google Scholar]
- Lowell, V.L.; Alshammari, A. Experiential learning experiences in an online 3D virtual environment for mental health interviewing and diagnosis role-playing: A comparison of perceived learning across learning activities. Educ. Technol. Res. Dev. 2019, 67, 825–854. [Google Scholar] [CrossRef]
- Stewart, S.; Pope, D.; Duncan, D. Using Second Life to enhance ACCEL an online accelerated nursing BSN program. In Connecting Health and Humans; IOS Press: Amsterdam, The Netherlands, 2009; Volume 146, pp. 636–640. [Google Scholar] [CrossRef]
- del Aguila, J.; González-Gualda, L.M.; Játiva, M.A.; Fernández-Sotos, P.; Fernández-Caballero, A.; García, A.S. How interpersonal distance between avatar and human influences facial affect recognition in immersive virtual reality. Front. Psychol. 2021, 12, 675515. [Google Scholar] [CrossRef] [PubMed]
- Fernández-Sotos, P.; García, A.S.; Vicente-Querol, M.A.; Lahera, G.; Rodriguez-Jimenez, R.; Fernández-Caballero, A. Validation of dynamic virtual faces for facial affect recognition. PLoS ONE 2021, 16, e0246001. [Google Scholar] [CrossRef] [PubMed]
- Muros, N.; García, A.; Forner, C.; López-Arcas, P.; Lahera, G.; Rodriguez-Jimenez, R.; Nieto, K.; Latorre, J.; Fernández-Caballero, A.; Fernández-Sotos, P. Facial Affect Recognition by Patients with Schizophrenia Using Human Avatars. J. Clin. Med. 2021, 10, 1904. [Google Scholar] [CrossRef] [PubMed]
- Hirosawa, T.; Kontani, K.; Fukai, M.; Kameya, M.; Soma, D.; Hino, S.; Kitamura, T.; Hasegawa, C.; An, K.-M.; Takahashi, T.; et al. Different associations between intelligence and social cognition in children with and without autism spectrum disorders. PLoS ONE 2020, 15, e0235380. [Google Scholar] [CrossRef]
- Bourke, C.; Douglas, K.; Porter, R. Processing of Facial Emotion Expression in Major Depression: A Review. Aust. N. Z. J. Psychiatry 2010, 44, 681–696. [Google Scholar] [CrossRef] [PubMed]
- Kumazaki, H.; Warren, Z.; Swanson, A.; Yoshikawa, Y.; Matsumoto, Y.; Yoshimura, Y.; Shimaya, J.; Ishiguro, H.; Sarkar, N.; Wade, J.; et al. Brief report: Evaluating the utility of varied technological agents to elicit social attention from children with autism spectrum disorders. J. Autism Dev. Disord. 2019, 49, 1700–1708. [Google Scholar] [CrossRef] [Green Version]
- Forbes, P.A.G.; Pan, X.; Hamilton, A.F.D.C. Reduced Mimicry to Virtual Reality Avatars in Autism Spectrum Disorder. J. Autism Dev. Disord. 2016, 46, 3788–3797. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Lecciso, F.; Levante, A.; Fabio, R.A.; Caprì, T.; Leo, M.; Carcagnì, P.; Distante, C.; Mazzeo, P.L.; Spagnolo, P.; Petrocchi, S. Emotional Expression in Children With ASD: A Pre-Study on a Two-Group Pre-Post-Test Design Comparing Robot-Based and Computer-Based Training. Front. Psychol. 2021, 12, 678052. [Google Scholar] [CrossRef] [PubMed]
- Wang, X.; Xing, W.; Laffey, J.M. Autistic youth in 3D game-based collaborative virtual learning: Associating avatar interaction patterns with embodied social presence. Br. J. Educ. Technol. 2018, 49, 742–760. [Google Scholar] [CrossRef]
- Lindner, P. Better, Virtually: The Past, Present, and Future of Virtual Reality Cognitive Behavior Therapy. Int. J. Cogn. Ther. 2020, 14, 23–46. [Google Scholar] [CrossRef]
- Boboc, R.G.; Chiriac, R.-L.; Antonya, C. How Augmented Reality Could Improve the Student’s Attraction to Learn Mechanisms. Electronics 2021, 10, 175. [Google Scholar] [CrossRef]
- Andrews, C.; Southworth, M.K.; Silva, J.N.A.; Silva, J.R. Extended Reality in Medical Practice. Curr. Treat. Opt. Cardiovasc. Med. 2019, 21, 18. [Google Scholar] [CrossRef]
- Bérubé, C.; Schachner, T.; Keller, R.; Fleisch, E.; Wangenheim, F.V.; Barata, F.; Kowatsch, T. Voice-Based Conversational Agents for the Prevention and Management of Chronic and Mental Health Conditions: Systematic Literature Review. J. Med. Internet Res. 2021, 23, e25933. [Google Scholar] [CrossRef] [PubMed]
- Altman, D.G. Practical Statistics for Medical Research; Chapman and Hall: London, UK, 1990; pp. 1–624. [Google Scholar]
- Cohen, J. A Coefficient of Agreement for Nominal Scales. Educ. Psychol. Meas. 1960, 20, 37–46. [Google Scholar] [CrossRef]
- Schulz, K.F.; Altman, D.G.; Moher, D.; CONSORT Group. CONSORT 2010 statement: Updated guidelines for reporting parallel group randomised trials. PLoS Med. 2010, 7, e1000251. [Google Scholar] [CrossRef] [PubMed]
- Aali, G.; Kariotis, T.; Shokraneh, F. Avatar Therapy for people with schizophrenia or related disorders. Cochrane Database Syst. Rev. 2020, 5, CD011898. [Google Scholar] [CrossRef] [PubMed]
- Kato-Lin, Y.-C.; Strotbaum, V.; Cho, H.; Porras, T.; Flynn, G.; Schnall, R. Usability of a Consumer Health Informatics Tool Following Completion of a Clinical Trial: Focus Group Study. J. Med. Internet Res. 2020, 22, e17708. [Google Scholar] [CrossRef]
- Dang, M.; Noreika, D.; Ryu, S.; Sima, A.; Ashton, H.; Ondris, B.; Coley, F.; Nestler, J.; del Fabbro, E. Feasibility of delivering an avatar-facilitated life review intervention for patients with cancer. J. Palliat. Med. 2021, 24, 520–526. [Google Scholar] [CrossRef]
- Robinson-Whelen, S.; Hughes, R.B.; Taylor, H.B.; Markley, R.; Vega, J.C.; Nosek, T.M.; Nosek, M.A. Promoting psychological health in women with SCI: Development of an online self-esteem intervention. Disabil. Health J. 2020, 13, 100867. [Google Scholar] [CrossRef]
- Calafell, M.D.M.R.; Ward, T.; Zhang, X.C.; Edwards, C.J.; Garety, P.; Craig, T. The Role of Sense of Voice Presence and Anxiety Reduction in AVATAR Therapy. J. Clin. Med. 2020, 9, 2748. [Google Scholar] [CrossRef] [PubMed]
- Tong, X.; Wang, X.; Cai, Y.; Gromala, D.; Williamson, O.; Fan, B.; Wei, K. “I Dreamed of My Hands and Arms Moving Again”: A Case Series Investigating the Effect of Immersive Virtual Reality on Phantom Limb Pain Alleviation. Front. Neurol. 2020, 11, 876. [Google Scholar] [CrossRef] [PubMed]
- Pinto, M.D.; Hickman, R.L.; Clochesy, J.; Buchner, M. Avatar-based depression self-management technology: Promising approach to improve depressive symptoms among young adults. Appl. Nurs. Res. 2013, 26, 45–48. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Thomas, N.; Bless, J.J.; Alderson-Day, B.; Bell, I.H.; Cella, M.; Craig, T.; Delespaul, P.; Hugdahl, K.; Laloyaux, J.; Larøi, F.; et al. Potential Applications of Digital Technology in Assessment, Treatment, and Self-help for Hallucinations. Schizophr. Bull. 2019, 45, S32–S42. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Tongpeth, J.; Du, H.Y.; Clark, R.A. Development and feasibility testing of an avatar-based education application for patients with acute coronary syndrome. J. Clin. Nurs. 2018, 27, 3561–3571. [Google Scholar] [CrossRef] [PubMed]
- Wonggom, P.; Kourbelis, C.; Newman, P.; Du, H.; Clark, R.A. Effectiveness of avatar-based technology in patient education for improving chronic disease knowledge and self-care behavior: A systematic review. JBI Evid. Synth. 2019, 17, 1101–1129. [Google Scholar] [CrossRef] [PubMed]
- Falconer, C.J.; Cutting, P.; Bethan-Davies, E.; Hollis, C.; Stallard, P.; Moran, P. Adjunctive avatar therapy for mentalization-based treatment of borderline personality disorder: A mixed-methods feasibility study. Evid.-Based Ment. Health 2017, 20, 123–127. [Google Scholar] [CrossRef] [PubMed]
- Leff, J.; Williams, G.; Huckvale, M.A.; Arbuthnot, M.; Leff, A.P. Computer-assisted therapy for medication-resistant auditory hallucinations: Proof-of-concept study. Br. J. Psychiatry 2013, 202, 428–433. [Google Scholar] [CrossRef] [Green Version]
- du Sert, O.P.; Potvin, S.; Lipp, O.; Dellazizzo, L.; Laurelli, M.; Breton, R.; Lalonde, P.; Phraxayavong, K.; O’Connor, K.; Pelletier, J.-F.; et al. A virtual reality therapy for refractory auditory verbal hallucinations in schizophrenia: A pilot clinical trial. Schizophr. Res. 2018, 197, 176–181. [Google Scholar] [CrossRef]
- Clarke, S.; Hanna, D.; Mulholland, C.; Shannon, C.; Urquhart, C. A systematic review and meta-analysis of digital health technologies effects on psychotic symptoms in adults with psychosis. Psychosis 2019, 11, 362–373. [Google Scholar] [CrossRef]
- Triberti, S.; Gorini, A.; Savioni, L.; Sebri, V.; Pravettoni, G. Avatars and the Disease: Digital Customization as a Resource for Self-Perception Assessment in Breast Cancer Patients. Cyberpsychol. Behav. Soc. Netw. 2019, 22, 558–564. [Google Scholar] [CrossRef]
- Haddock, G.; McCarron, J.; Tarrier, N.; Faragher, E.B. Scales to measure dimensions of hallucinations and delusions: The psychotic symptom rating scales (PSYRATS). Psychol. Med. 1999, 29, 879–889. [Google Scholar] [CrossRef]
- Chadwick, P.; Lees, S.; Birchwood, M. The revised Beliefs about Voices Questionnaire (BAVQ–R). Br. J. Psychiatry 2000, 177, 229–232. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kroenke, K.; Spitzer, R.L.; Williams, J.B. The PHQ-9: Validity of a brief depression severity measure. J. Gen. Intern. Med. 2001, 16, 606–613. [Google Scholar] [CrossRef]
- Beaudoin, M.; Potvin, S.; Machalani, A.; Dellazizzo, L.; Bourguignon, L.; Phraxayavong, K.; Dumais, A. The therapeutic processes of avatar therapy: A content analysis of the dialogue between treatment-resistant patients with schizophrenia and their avatar. Clin. Psychol. Psychother. 2021, 28, 500–518. [Google Scholar] [CrossRef] [PubMed]
- Green, R.; Delfabbro, P.H.; King, D.L. Avatar identification and problematic gaming: The role of self-concept clarity. Addict. Behav. 2021, 113, 106694. [Google Scholar] [CrossRef]
- Grogan, S.; Flett, K.; Clark-Carter, D.; Conner, M.; Davey, R.; Richardson, D.; Rajaratnam, G. A randomized controlled trial of an appearance-related smoking intervention. Health Psychol. 2011, 30, 805–809. [Google Scholar] [CrossRef] [PubMed]
- Fox, J.; Bailenson, J.N. Virtual Self-Modeling: The Effects of Vicarious Reinforcement and Identification on Exercise Behaviors. Media Psychol. 2009, 12, 1–25. [Google Scholar] [CrossRef] [Green Version]
- Baylor, A.L.; Ryu, J. The Effects of Image and Animation in Enhancing Pedagogical Agent Persona. J. Educ. Comput. Res. 2003, 28, 373–394. [Google Scholar] [CrossRef]
- Rosenberg-Kima, R.B.; Baylor, A.L.; Plant, E.A.; Doerr, C.E. The importance of interface agent visual presence: Voice alone is less effective in impacting young women’s attitudes toward engineering. In International Conference on Persuasive Technology; Springer: Heidelberg, Germany, 2007; pp. 214–222. [Google Scholar] [CrossRef]
- T’ng, S.T.; Pau, K. Identification of Avatar Mediates the Associations between Motivations of Gaming and Internet Gaming Disorder among the Malaysian Youth. Int. J. Ment. Health Addict. 2020, 19, 1346–1361. [Google Scholar] [CrossRef]
- Ye, J. Pediatric Mental and Behavioral Health in the Period of Quarantine and Social Distancing with COVID-19. JMIR Pediatr. Parent. 2020, 3, e19867. [Google Scholar] [CrossRef] [PubMed]
- Alevizopoulos, A.; Kritikos, J.; Alevizopoulos, G. Intelligent machines and mental health in the era of COVID-19. Psychiatriki 2021, 32, 99–102. [Google Scholar] [CrossRef] [PubMed]
- Stasolla, F.; Matamala-Gomez, M.; Bernini, S.; Caffò, A.O.; Bottiroli, S. Virtual Reality as a Technological-Aided Solution to Support Communication in Persons with Neurodegenerative Diseases and Acquired Brain Injury during COVID-19 Pandemic. Front. Public Health 2021, 8, 635426. [Google Scholar] [CrossRef] [PubMed]
- Sampaio, M.; Haro, M.V.N.; De Sousa, B.; Melo, W.V.; Hoffman, H.G. Therapists Make the Switch to Telepsychology to Safely Continue Treating Their Patients During the COVID-19 Pandemic. Virtual Reality Telepsychology May Be Next. Front. Virtual Real. 2021, 1. [Google Scholar] [CrossRef] [PubMed]
| Study | Publication Year | Country | Type of Study |
|---|---|---|---|
| Aali et al. [42] | 2020 | England | Review |
| Andrade et al. [6] | 2015 | USA | RCT 1 |
| Cho et al. [43] | 2020 | USA | RCT |
| Clarke et al. [55] | 2019 | Ireland | Review |
| Dang et al. [44] | 2020 | USA | Feasibility study |
| du Sert et al. [54] | 2018 | Canada | RCT |
| Falconer et al. [52] | 2017 | England | Feasibility study |
| Leff et al. [53] | 2013 | England | RCT |
| Pinto et al. [48] | 2013 | USA | Pilot testing |
| Robinson-Whelen et al. [45] | 2020 | USA | RCT |
| Rus-Calafell et al. [46] | 2020 | England | RCT |
| Stewart et al. [25] | 2010 | USA | Narrative review |
| Thomas et al. [49] | 2019 | Australia | Narrative review |
| Tong et al. [47] | 2020 | China | Case series |
| Tongpeth et al. [50] | 2018 | Australia | Feasibility pilot testing |
| Triberti et al. [56] | 2019 | Italy | Pilot testing |
| Wonggom et al. [51] | 2019 | Australia | Review |
| Wonggom et al. [3] | 2020 | Australia | RCT |
| Study | Participant Number | Mean Age | Target Population |
|---|---|---|---|
| Aali et al. [42] | 195 | Not provided | Schizophrenia or related disorders |
| Andrade et al. [6] | 41 | 61 | Overactive bladder |
| Cho et al. [43] | 39 | 55 | HIV with HANA conditions |
| Clarke et al. [55] | 1535 | Not provided | Psychosis |
| Dang et al. [44] | 11 | Not provided | Cancer |
| du Sert et al. [54] | 19 | 42.9 | Schizophrenia |
| Falconer et al. [52] | 11 | 31.2 | Borderline personality disorder |
| Leff et al. [53] | 26 | Not provided | Schizophrenia |
| Pinto et al. [48] | 28 | Not provided | Depression |
| Robinson-Whelen et al. [45] | 21 | Not provided | Spinal cord injury |
| Rus-Calafell et al. [46] | 39 | 43.87 | Schizophrenia |
| Stewart et al. [25] | Not provided | Not provided | People with disabilities (physical, psychological, cognitive rehabilitation, chronically ill, convalescing or homebound) |
| Thomas et al. [49] | Not provided | Not provided | Schizophrenia |
| Tong et al. [47] | 5 | 50.2 | Phantom limb pain (brachial plexus avulsion injury and amputees’ outpatients) |
| Tongpeth et al. [50] | 10 | 52.2 | Acute coronary syndrome |
| Triberti et al. [56] | 22 | 49.4 | Cancer |
| Wonggom et al. [51] | 752 | Not provided | Chronic disease (cardiovascular and chronic respiratory disease, diabetes, cancer) |
| Wonggom et al. [3] | 36 | 67.5 | Heart failure |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Franco, M.; Monfort, C.; Piñas-Mesa, A.; Rincon, E. Could Avatar Therapy Enhance Mental Health in Chronic Patients? A Systematic Review. Electronics 2021, 10, 2212. https://doi.org/10.3390/electronics10182212
Franco M, Monfort C, Piñas-Mesa A, Rincon E. Could Avatar Therapy Enhance Mental Health in Chronic Patients? A Systematic Review. Electronics. 2021; 10(18):2212. https://doi.org/10.3390/electronics10182212
Chicago/Turabian StyleFranco, Marta, Carlos Monfort, Antonio Piñas-Mesa, and Esther Rincon. 2021. "Could Avatar Therapy Enhance Mental Health in Chronic Patients? A Systematic Review" Electronics 10, no. 18: 2212. https://doi.org/10.3390/electronics10182212
APA StyleFranco, M., Monfort, C., Piñas-Mesa, A., & Rincon, E. (2021). Could Avatar Therapy Enhance Mental Health in Chronic Patients? A Systematic Review. Electronics, 10(18), 2212. https://doi.org/10.3390/electronics10182212







