Abstract
This article focuses on an eHealth application, CogniViTra, to support cognitive and physical training (i.e., dual-task training), which can be done at home with supervision of a health care provider. CogniViTra was designed and implemented to take advantage of an existing Platform of Services supporting a Cognitive Health Ecosystem and comprises several components, including the CogniViTra Box (i.e., the patient terminal equipment), the Virtual Coach to provide assistance, the Game Presentation for the rehabilitation exercises, and the Pose and Gesture Recognition to quantify responses during dual-task training. In terms of validation, a functional prototype was exposed in a highly specialized event related to healthy and active ageing, and key stakeholders were invited to test it and share their insights. Fifty-seven specialists in information-technology-based applications to support healthy and active ageing were involved and the results and indicated that the functional prototype presents good performance in recognizing poses and gestures such as moving the trunk to the left or to the right, and that most of the participants would use or suggest the utilization of CogniViTra. In general, participants considered that CogniViTra is a useful tool and may represent an added value for remote dual-task training.
1. Introduction
Cognitive training is a non-pharmacological therapeutic aiming at the maintenance (e.g., older adults with neurological diseases) or the improvement (e.g., children in the school setting, to ameliorate problems associated with learning difficulties) of particular aspects of cognitive domains [1], such as attention, memory and learning, language, executive functions and calculation, and constructional and perceptive abilities [2].
A cognitive training program is usually made up of a set of different types of exercises, such as word searches, letters and numbers, or the recognition of patterns and geometric figures. The exercises can be performed individually or in groups, although their selection should comply with an individualized intervention explicitly focusing on a person’s needs, with the difficulty level of activities adapted to the individual functioning, and must be executed under the control of a clinician (e.g., psychologist, neuropsychologist, speech therapist, occupational therapist, neurologist, or psychiatrist).
Traditionally, cognitive training was based on paper-and-pencil exercises, but with technological development a diverse set of computerized tools are being used.
The simultaneous performance of cognitive and motor tasks can be difficult and can lead to worse performance in one of the domains (i.e., the cognitive or the motor domain) or in both domains. This is known as cognitive-motor interference, which is usually experienced by individuals with physical and cognitive deficits, such as patients with stroke, Parkinson’s disease, or Alzheimer’s disease [3]. Cognitive-motor interference may prevent individuals from allocating appropriate attentional resources, which impacts their daily living activities, namely in terms of mobility due to the increase of fall risk [3].
Dual-task training comprises the realization of exercises that require the simultaneous performance of two independent (i.e., with different goals and that can be performed independently) cognitive and physical tasks, which is different from a single task requiring cognitive and physical resources [4,5]. Examples of dual-task exercises include the repetition of a digit string while walking or performing different movements in response to visual, auditory, or olfactory stimuli [6].
Based on the cumulative evidence of cognitive and physical training effectiveness in enhancing cognitive functions of older adults with mild cognitive impairment [7,8,9], the combination of physical and cognitive training is assuming an increasing importance [10,11,12,13,14,15,16]. This is known as dual-task training [17,18].
Moreover, the extension of cognitive training from the clinical setup to the home environment represents a reduction of the burden for caregivers (i.e., formal and informal caregivers), and might increase the number and the duration of training sessions as well as overcome restrictions imposed by the availability of care resources, which are exacerbated by the current global pandemic. Therefore, innovative approaches (e.g., using information technologies [3,18,19]) are required to surpass the current health care system’s lack of resources (i.e., human and physical infrastructures) and address the growing number of patients with neurological disorders requiring interventions.
Although there are technological solutions able to provide multisensory feedback and modulate exercise complexity according to the patients’ capacity, they rarely provide exercises validated for neurological rehabilitative interventions [3] as well as appropriate interoperability mechanisms to support collaborative networks and the integration of clinical care and home care [20]. For these reasons, a European funded project, Cognitive Vitality Training (CogniViTra), seeks to develop and validate an eHealth application to support dual-task training, both in clinical settings and at home.
This article presents the design and development of the CogniViTra application, based on an already clinically validated set of cognitive training exercises that take the form of games, which is part of a Cognitive Health Ecosystem [21,22] supported by a Platform of Services. Furthermore, the article also presents the results of the first stage of the validation process, which consisted of a conceptual validation based on a peer review, involving a group of specialists (i.e., health care providers, social care providers, information technologies developers, and decision-makers) with experience and competence in the development of eHealth applications to support healthy and active ageing. This was considered fundamental for the preparation of a future multicenter clinical trial to assess the adherence, efficacy, and efficiency of a dual-task rehabilitation program supported by CogniViTra.
Some authors of this article are clinicians experienced in the treatments of neurological diseases, including cognitive rehabilitation, either face-to-face or remotely, namely using the Cognitive Health Ecosystem. These clinicians lead the design and development of CogniViTra, and their main motivation was to develop a scalable digital solution to optimize dual-task training intervention in the daily clinical practice.
CogniViTra presents important advantages when compared with related state-of-the-art solutions, namely the availability of clinical management tools and the integration with clinical care workflow.
Another significant advance over state-of-the-art solutions is CogniViTra’s capacity to automatically quantify and register the cognitive performance of the patients when performing dual-task training. For instance, since a dual-task training exercise require the realization of a physical activity together with a cognitive task such as the repetition of digit string in reverse order, in the current clinical approach the correctness of the repeated string must be permanently verified by the practitioner, which is neither practical nor efficient. Therefore, the automatic quantification and registration of the patients’ cognitive performance is fundamental to optimize practitioner efficiency and to scale dual-task cognitive interventions.
This article has the following structure: Section 2 reviews the research work that influenced this study and presents a summary of the state of the art regarding dual-task cognitive training. Section 3 introduces the Cognitive Health Ecosystem and the Platform of Services that supported the development of the CogniViTra application. Section 4 describes the design and development of the fundamental components of CogniViTra. Section 5 presents the results of the conceptual validation of CogniViTra. Finally, Section 6 details the conclusions of the study and points out possible future work.
2. Related Work
The individuality of each human being results, to a large extent, from the public expression of the brain, through cognitive and behavioral functioning. The skills to learn, evolve and manage all aspects of daily life are dependent on normal brain functioning. As we get older, the importance of the brain and cognitive health status becomes the determining factor for quality of life [23].
However, the brain is continuously exposed to all types of damage and disease (e.g., trauma, depression, cancer, hypertension, diabetes, smoking, stroke, and Parkinson’s and Alzheimer’s diseases), each of which has a cumulative effect on the probability to develop a cognitive problem. Throughout an individual’s life, the cognitive risk due to brain disease is 1:3 [24]. At the population level, this risk translates into 15–30 new years of life lost due to disability for every 1000 inhabitants/year [23]. Thus, considering all major groups of diseases, those of the nervous system represent the greatest contribution to the global impact on the health of populations worldwide (i.e., 6.3%) and are responsible for the highest disability rates and global burden of disease [23].
Consequently, neurological diseases are responsible for an increasing demand for health care services [23]. Regardless of their original causes (e.g., stroke, brain damage, neurodegenerative diseases), cognitive deficits rarely recover spontaneously or completely [25,26]. Brain damage, once established, is difficult to reverse; in fact, there are no pharmacological interventions with a confirmed significant positive effect [27,28,29]. Currently, cognitive care is largely dependent on traditional methods centered in institutions, only feasible in the presence of a health care practitioner. These are typically slow processes, based on the plasticity of the remaining brain tissue, and depend entirely on the implementation of rehabilitation programs, which are usually complex and intensive [30,31].
Rehabilitation programs have proven to be effective in compensating, improving, and stabilizing deficits in various diseases and nosological models. Like other rehabilitation processes, the results obtained always depend on the early start of the rehabilitation program, its intensity, and the specificity of the therapies used [26,29,32,33,34]. However, although neurological rehabilitation programs are accepted as fundamental components in current treatment models, there are strong restrictions on patient access [10,23,35,36,37], since such programs require multidisciplinary teams and are usually carried out in a hospital context, away from the patient’s home and implying the presence of family members. This translates into an enormous effort for patients, families, and institutions [33] and generates great economic burdens, both for families and health care systems [11,12]. In addition, there are limits to the effectiveness of treatment programs, given the difficulty that health care systems have in providing rehabilitation sessions in due time (i.e., right after the injury or the onset of the disease) and with the intensity, quality, and duration appropriate for the stimulation of brain tissue plasticity [38].
Bearing in mind the enormous impact associated with neurological diseases, it is now widely recognized that the services and resources available at the level of health care systems are disproportionately scarce in this area [23,39]. Moreover, these systems are unable to cope with the pressure imposed by the increased prevalence of these diseases associated with the increased average life expectancy and population aging.
Despite the serious problems verified, there have been successive scientific advances that have resulted in the production of new knowledge in terms of genetic, molecular, cellular, physiological and behavioral processes, and neural networks that support brain plasticity and recovery [40,41]. This new knowledge has given rise to new types of therapies, namely therapies centered on the promotion and modulation of neuroplasticity, on learning and memory mechanisms or on neurogenesis and axonal regeneration, whether through pharmacological or non-pharmacological strategies [42,43,44]. In this context, neurorehabilitation is also changing as a result of the practical applicability of research in neurosciences and, consequently, is largely dependent on the development of more effective technologies that facilitate the extensive application of all the knowledge produced [45,46]. Training-based rehabilitation programs, regardless of their modality (e.g., cognitive, behavioral, or motor), the place of application (e.g., at the patient’s home or at the institution), the mode of application (e.g., alone or in combination with pharmacological strategies), or the type of disease to be treated, require specific and controlled interventions, monitoring of patients, as well as clinical trials supported by direct measures of cognitive and motor functioning [46,47,48].
Dual-task training is being included in training-based rehabilitation programs, not only because the scientific literature reports positive effects [10,11,12,13,14,15,16,17,18], but also because daily living requires the ability to perform multiple cognitive and physical tasks simultaneously. In this respect, dual-task training is seen as an approach to prepare patients for adequately returning to community living (e.g., household, family, work, or leisure) [18,49]. Moreover, dual-task training has been proposed as a potentially effective strategy for reducing the risk of falling in the elderly population [50].
Although dual-task training can be supported in use of paper-and-pencil exercises, the high intensity required for physical and mental adaptations must be modifiable and personalized according to the functional status of each patient. In this respect, information technologies have brought a broad range of possibilities for smart and adapted exercises [19]. Different solutions such as virtual reality [18] and mobile apps [3] are being used to support dual-task training.
Table 1 presents relevant studies [3,51,52,53,54,55,56,57,58,59,60,61,62,63,64,65] related to the use of digital solutions to support physical activities or cognitive and physical activities with different purposes (i.e., postural control and prevention of falls [51,53,54,58,59,65], assistance in physical exercises [52,56,61], physical activity adherence [55], improvement of physical performance [58,59,60,63,64], and improvement of cognitive performance [3,57,60,62,64]). The studies are supported in various types of technologies, namely exergames and virtual reality [51,53,54,57,58,59,60,61,62,63,65], robotics [52,56,61], and mobile devices [3]. In turn, some of these articles report interactions mechanisms based on the recognition of body movements (e.g., using Kinect [51,52,57,58,65], Nintendo Wii Fit [53], or wearable devices [59,60]), feet movements using step training platforms [54,63], or leg movements on a training bicycle [55].

Table 1.
Features of relevant studies related to the use of digital solutions to support physical activities or cognitive and physical activities.
When compared with stat-of-the-art technological solutions, the study reported by this article presents two important advantages: (i) support tools and clinical information integration and (ii) automatic quantification of patient’s cognitive performance during dual-task training.
CogniViTra presents backend applications that are fundamental to helping practitioners with the management of clinical interventions, including the preparation of individualized intervention plans (e.g., definition of objectives, areas of cognitive intervention, individual composition of training sessions, and duration and intensity of treatment) and the monitoring of the intervention results. These features are not present in the identified studies and are impossible in some of them (e.g., the solution reported by [56] is a single-exercise solution, and the solution reported by [51] uses four commercial adventure games). Moreover, CogniViTra is supported in a clinical validated exercise battery, and its clinical data structures together with security mechanisms promote the integration of the corresponding interventions with the clinical care workflows. This means, for instance, that CogniViTra clinical assessments of specific patients might be available, when required, to the authorized multidisciplinary care team, safeguarding the privacy, integrity, and confidentiality of the information.
Furthermore, one of the most relevant features of the CogniViTra application is the automatic quantification and registration of the cognitive performance of the patients. This is fundamental for the practitioner assessment of the clinical intervention and surpasses difficulties associated with usual clinical cognitive interventions.
The aforementioned CogniViTra features result from the approach followed for the definition of its functional requirements. Contrary to other solutions, a major concern to consider for the development of CogniViTra was to contribute to bridging the gap between technological advancement and clinical relevance, a problem associated with dual-task rehabilitation programs, as indicated by [19].
3. Cognitive Health Ecosystem
To respond to the challenges of cognitive rehabilitation, some of the authors of this article were involved in the development of several eHealth applications that, taken together, constitute a Cognitive Health Ecosystem [21,22]. This development started in 2005 in a memory clinic that organized and delivered care to a 400,000 inhabitant population and was anchored in a hospital with clinical and research obligations.
An important contribution of this ecosystem is the minimization of critical sustainability issues for the cognitive health management of the population by increasing the capacity to identify early and monitor all individuals at risk for cognitive decline and providing early cognitive interventions with the adequate quality, intensity, and duration to obtain relevant functional effects. For this purpose, the Cognitive Health Ecosystem aims to disseminate innovative technological solutions to support different clinical domains:
- Screening—sustainable population-based cognitive screening strategies to allow the population at risk to be tracked, without requiring physical travel to specialized clinical centers or expensive radiology, nuclear, or molecular medicine exams;
- Diagnosis—solutions to optimize the global neuropsychological assessment process of patients and to improve the collection of data on cognitive functioning to reduce patient fatigue and the duration of assessments;
- Rehabilitation—strategies to allow individual or group cognitive training programs, using cognitive tasks and others that involve exercises and movement, ideally at home or in community-based institutions;
- Research—multicentric scientific studies facilitated by a translational network environment that promotes large sample sizes, while simultaneously shortening the time needed to recruit patients and complete the study. These studies carried out within the ecosystem aim to facilitate the rapid implementation of innovative processes and the mobility of the knowledge produced;
- Impact—articulation between the various domains described above to have a significant impact in terms of the cognitive health of the population served, measured by the levels of intellectual performance, social participation, and quality of life of the citizens.
In strategical terms, Cogweb [21] is the ultimate exponent of the available services, and approximately 10,000 patients had access to Cogweb-mediated remote cognitive rehabilitation.
3.1. Platform of Services
The key element of the Cognitive Health Ecosystem is a Platform of Services that supports different eHealth applications [21,22] and was based on two important requirements: (i) to increase the productivity and intervention capacity of the professionals and (ii) to move the clinical decision to the community, to ensure increased adherence and quality of the services.
Without a common and shared architectural standard for software, data formats, storage systems, modules, and information resources, development and integration are difficult and often promote replicated data in diverse data formats and storage systems. To overcome these difficulties, a service oriented architecture (SOA) [66] was considered. This architecture presents several advantages since it can optimize flexibility and interoperability of the components over the longer term. Furthermore, the use of an n-tier SOA allows the separation of business rules from the applications and the technologies that interpret them, which maximizes flexibility and minimizes the cost of accommodating changes in business rules and therefore allows the development of specific applications without significant development effort.
The generic architecture of the Platform of Services is divided into three layers (Figure 1): (i) the User Application Layer comprises a set of applications to fulfil the needs of all those involved in the Cognitive Health Ecosystem; (ii) the Backend Services Layer is responsible for all logic related to the interactions between the different applications and the data being persisted; and (iii) the Data Layer ensures the persistence of all information used in the remaining layers, and it is divided into a set of databases, each housing specific data about a given goal.
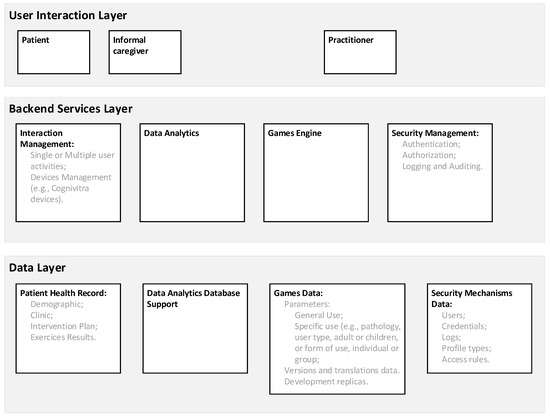
Figure 1.
Generic architecture of the Platform of Services.
3.2. User Application Layer
All information collection and communication procedures are processed through the components of the User Application Layer. This layer is understood in a bidirectional sense in terms of information communication and admits specialization according to the characteristics of the users’ profiles and the hardware used for access (e.g., a desktop or a tablet computer). Concerning users’ profiles, beside the patients and the specialized practitioners (e.g., neuropsychologists), other types of users include informal caregivers, physicians, researchers (e.g., data analysts or biostatistics), or those that are responsible for the ecosystem management. The specificities of the various types of users are omitted for clarity.
The cognitive interventional approaches are conducted by practitioners that play a central role in defining the degree of supervision and the type of patient exposure to the treatment, namely the definition of objectives, areas of cognitive intervention, individual composition of training sessions, or duration and intensity of treatment. Although the presence of practitioners is not continuously necessary for the training, they can actively direct all activities via online interaction and periodic (e.g., daily, weekly, or monthly) meetings.
Concerning the patients, the User Application Layer, in addition to allowing access to the online training area, contains educational content targeting the general population and a blog. The aim of the site is to provide scientific and pedagogical information about cognitive functioning and its changes, and the possibilities and indications for cognitive training.
3.3. Backend Services Layer
The main element of the Backend Services Layer is the Cognitive Games Engine that comprehends a pool of more than 100 original exercises (i.e., games) that are grouped according to major cognitive function stimulated (i.e., attention, memory and learning, language, executive functions and calculation, constructional and perceptive abilities); cover different degrees of impairment, from normal function to moderate deficits; have sequential levels of difficulty, the progression through levels being automatic and determined by patients’ performance; and are prepared not only for sessions with single patients, but also for group sessions.
A typical cognitive exercise is the digit span backwards [67], a mental tracking task that requires sustained attention, working memory, and information processing speed. A string of digits (e.g., 5-7-1-6-3) is presented at a fixed rate (e.g., one per second), and the patients are requested to repeat the string in reverse order. Each patient’s digit span length is determined by the largest sequence length for which the patient scores at least 75%.
Figure 2 presents other four possible exercises: faces and names, match the color, changing letters, and arrange the words. In the first exercise, faces and names, photos of several individuals with their corresponding names are presented in the beginning of the exercise; then, the different photos are individually presented, and the participants should indicate whether the given name is correct or not, considering the set of photos initially presented. In the second exercise, match the color, a sequence of two words sets is presented, and the participants should indicate whether the words have the same color or not. Concerning the concrete example presented in Figure 2 of the changing the letters exercise, the participants should replace the letter R with the letter N when the traffic light is green and, when the traffic light turns red, the participants should replace the letter Q with the letter P. Finally, in the arrange the words exercise, a sequence of words is presented, and the participants should classify them. For instance, considering the specific instance of a sequence of words presented in the arrange the words exercise of Figure 2, the participants should indicate that the dolphin is a marine animal and not an insect or a vegetable.
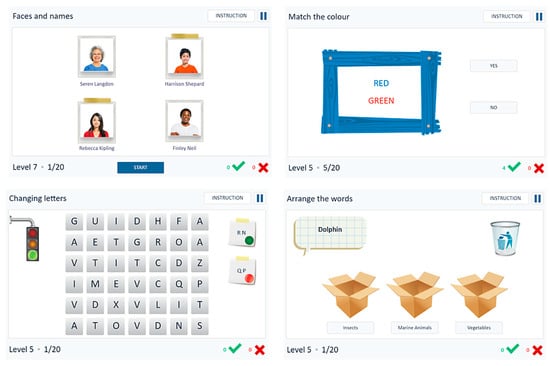
Figure 2.
Examples of cognitive exercises.
Some of these exercises are computerized versions of existing paper-and-pencil exercises, and others were created to meet specific requirements expressed by the practitioners and to exploit computer functionalities that would be particularly difficult to reproduce with a paper-and-pencil approach. During the dynamic generation of the exercises, the individual patients’ performance data (e.g., accuracy and number of clues required) are analyzed to set the appropriate difficulty level. For each exercise and each level, thresholds are defined to allow difficulty levels to be progressively increased. Therefore, for each training section different parameters are retrieved, such as type of exercise, difficulty level, accuracy, and response time, which are used to assess both the overall outcome of a session and the global trend of the rehabilitation.
Since the Platform of Services supports a collaborative network and can be accessed by a broad range of users that are distributed, both in geographical terms and in the administrative terms, privacy, integrity, and confidentiality of the information need to be ensured in a transparent easy-to-maintain way and supported on a strong granularity in terms of the definition of different authorization levels. For this purpose, the Backend Services Layer presents the following services:
- Authentication, to provide the identification of the users;
- Authorization, to regulate access to the information, including the establishment of access controls to limit personnel access, which is challenged by a diverse set of policies, complexity of workflows, and high risk of denying access to key information;
- Logging and Auditing, to trace which users look at which records so an auditor can use this information to detect abuses.
Concerning Authentication, users’ credentials are analyzed, and notifications are stored by the Logging and Auditing service. Furthermore, for each authentication process, a JavaScript Object Notation (JSON) Token (JWT) is generated with several identifying elements of the entity trying to access the Platform of Services to be analyzed by the Authorization service.
The main purpose of the Authorization service is to provide general mechanisms to control data access. In terms of the implementation, both role-based access control (RBAC) and attribute-based access control (ABAC) mechanisms were considered for the access to the data resources [68]. Each member of the cognitive intervention team has access to the clinical information of their patients. However, different types of practitioners (e.g., psychologists, neuropsychologists, speech therapists, and neurologists) have different roles according to their competencies and responsibilities, which is translated into different privileges (i.e., RBAC mechanisms), mainly in terms of information writing. However, when required in terms of integration with clinical workflows, subsets of the clinical information of specific patients should be shared with clinicians that are not members of the cognitive intervention team, according to established protocols. Conceptually, although it was not implemented, the patients themselves could authorize the access of parts of their clinical information to their caregivers (e.g., their general practitioners). Consequently, in addition to the RBAC mechanisms, ABAC mechanisms were also implemented.
The application of the RBAC and ABAC mechanisms requires the definition of information access policies, so that requests related to specific patients, information, or actions are analyzed through a set of pre-established rules (of a certain policy). In this respect, the eXtensible Access Control Markup Language (XACML) [69] was used since it is a standard for handling requests for actions, regarding information access, using ABAC policies, and with additional application logic it can also be used to implement RBAC mechanisms. With XACML, policies and their corresponding rules can have different levels of detail, according to the different number of attributes needed before reaching a decision.
Pre-established rules are divided into different categories. The decision for the access request is obtained after comparing all the values of the attributes of the appropriate categories, between the request and the previously defined rules. Depending on how a specific decision rule was defined, the result of a request might be a denial or a permit. Once a decision is achieved, it is communicated by the Authorization service to the Logging and Auditing services, to the entity that requested the information access, and to the logic that supports the Patient Health Record (Figure 1).
For the Logging and Auditing service, based on a previous work [70], a cryptographic secure blockchain was proposed to store the events and the blocks (of the blockchain) in a specific database, which can be assessed for auditing. The implementation of this blockchain mechanism was not supported in available frameworks such as Hyperledger due to the intention to avoid external dependency in the long run on a commercial product. Instead, a custom solution was implemented.
The communication of any ecosystem entity with the Logging and Auditing service is first initiated with a process that aims to establish a security association. This process consists of the exchange of public keys, which are stored for the remainder of the time. The Logging and Auditing service may authorize or reject the association, as configured by the system administration, so that only authentic entities belonging to the infrastructure may generate log entries. For an authentic entity, the process culminates in the attribution of a unique shared cryptographic key, generated by the Logging and Auditing service for the purposes of encrypting the logs sent for storage. Each log entry is then encrypted and signed by the entity private key. The keys can be refreshed periodically, and a wide range of ciphers can be used. In the current implementation we resorted to Advanced Encryption Standard (AES) in the Galois/Counter Mode (GCM), as it provides encryption and integrity control. In addition, Hypertext Transfer Protocol Secure may also be used between the entities, but the cryptographic material will only be used for the establishment of a secure communication tunnel and will have no impact on the log entries.
Log insertion is triggered when an event occurs, usually as a consequence of an action executed by a user. The data describing the event are sent as a Hypertext Transfer Protocol Post to the Logging and Auditing service, where they are inserted in its request body as a JSON object. Since requests must also have a JWT, the verification of signatures is made using the algorithm specified in the JWT together with a secret key, which allows the validation of the requested events. Moreover, the Logging and Auditing service decrypts the object and processes its contents, indexing different elements involved in the event (e.g., date, user identifier, application/service identifier) to construct an appropriate document and the corresponding metadata. Log integrity is validated locally on block insertion at fixed intervals as stated by a timer. Inserting a block requires both validating previous blocks in the chain, which can be done by the Logging and Auditing service or by an offloaded service, and then registering pending log entries. This creates an interdependence between log entries from multiple sources, limiting single source spoofing.
Each block contains the set of event entries that were received since the insertion of the last block. If there is a period without activity, a block will be also created, but its contents will be a random nonce, concatenated with the current timestamp. This way, nobody external to the ecosystem will know if there really was activity or not, since only the block’s metadata are shown. The block effectively seals the chain, asserting its state at a given instant. If there are data, a cryptographic hash of the block is calculated, which also considers the content of the previous block, through its hash value. The block is then inserted into document-based storage, with multiple indexes, using the ElasticSearch indexer.
Auditing of log entries is the final process and can be conducted either automatically or by human observers. Existing tools such as Kibana can be used, and the integrity of the data observed can be ensured. The integrity of the chain can be verified at any time to check for any inconsistencies. Since every block of the chain has a clear identification, with fingerprints of the log data as well as time stamps of the first and last event during that time period, the hash of all the events that occurred between two checkpoints can be recalculated to check if it matches the one stored in the block. The next and previous hash fields on every block can also be used to verify that the block itself has not been tampered with.
The Backend Services Layer also includes a data analytics framework of unidentified data generated by the users of the platform. Its main purpose is to analyze the quality of processes according to the standards established by a board of consulting clinicians. Long-term monitoring tools were incorporated into the data analytics to supervise clinical evolution and adjust programs according to the patients’ progression (e.g., alerts, reports, benchmarking instruments, longitudinal analysis of evolution, prognostic and predictive models). Moreover, management algorithms were also implemented to guarantee scalability, so that some changes occur automatically, according to the results of the data analytics algorithms, such as evidence for the substitution of a useless exercise, the changing of system features that lead to errors, setting new automatisms such as alert signs for some clinical situations, or the preparation of specific educational campaigns for practitioners.
3.4. Data Layer
The Data Layer is divided into a set of databases, each housing specific data about a given goal. This division is intended to: (i) separate different types of information; (ii) ensure the autonomy of information that is persisted; (iii) increase security levels; and (iv) allow different technologies to be adopted for the implementation of different databases.
The main database is the Patient Health Record, where the practitioners may add patients’ information to the system and manage it later. It includes the medical form (e.g., identification data, data on the duration of the license to use the system and patients’ credentials to access it, and clinical data), the neuropsychological assessment (e.g., the general descriptive data of the evaluation and quantitative results obtained in each neuropsychological test, with the possibility to record several evaluations over time), and the intervention plan (e.g., treatment plan, including duration, main cognitive domains, and the expected intensity of training, which can be used for the detailed evaluation of the quality of the tasks prescribed to the patient in the next session).
In addition to the Patient Health Record, the Data Layer also includes all the databases required by the ecosystem, namely the users’ database (including the practitioners), the games database (i.e., information on rehabilitation activities including complementary information, such as indication of a general-purpose exercise or specific use exercise, type of pathology, type of user, form of use, versioning, and translations) and the security database (e.g., credential, profiles, access policies or Logging and Auditing).
4. CogniViTra
The CogniViTra project seeks to develop and validate an eHealth application to support dual-task training both in clinical settings and at home. For the CogniViTra implementation, the flexibility of an SOA architecture of the Platform of Services supporting the Cognitive Health Ecosystem was utilized.
Therefore, as can be seen in Figure 3, the CogniViTra implementation was based on the resources already available in the Platform of Services, including the components of the Backend Services (e.g., the security services, or the Cognitive Games Engine, which is responsible for the management of the various games, as well as the subsequent storage of the patients’ results) and the Data Layer (e.g., patient, game, and security mechanism data). In terms of User Application Layer, the practitioners’ interface is based on the already existing interface.
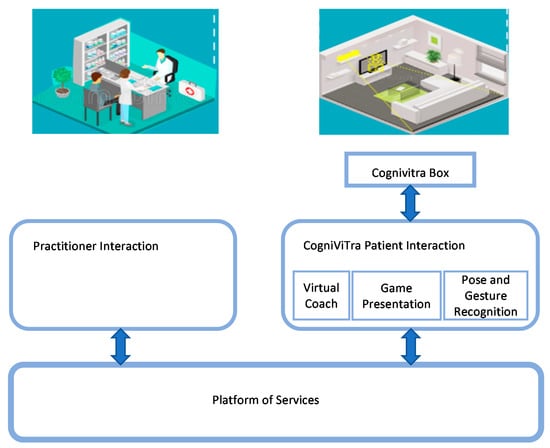
Figure 3.
Conceptual model of CogniViTra.
However, concerning the patients, new developments were made for the User Application Layer, including the CogniViTra Box, a hardware component to quantify individual and group responses and interactions during dual-task training (i.e., Pose and Gesture Recognition).
To take advantage of the CogniViTra Box, the CogniViTra Patient Interaction was also developed, which is responsible for the management of the data received from the CogniViTra Box and the presentation of the rehabilitation exercises. Additionally, given that the inclusion of physical exercises necessarily implies a greater physical distance from the patient in relation to the terminal equipment, an attempt was made to make the interaction mechanisms more flexible, namely in terms of availability of multimodal strategies and of an embodied conversational agent, which aims to provide a unified, accessible, and easy-to-use interface to ensure that the patients have a seamless interaction with the CogniViTra application.
Figure 4 presents a simplified diagram of the CogniViTra Patient Interaction application with some of the components of the Platform of Services, the generic architecture of which is introduced in Figure 1.
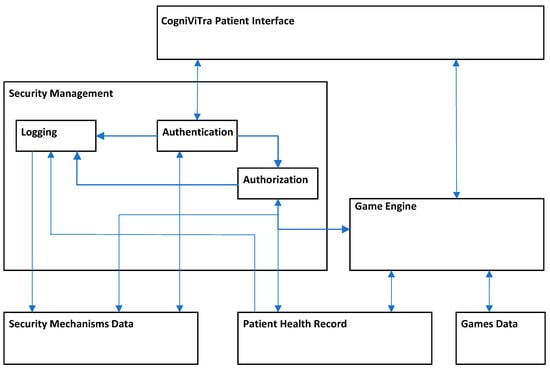
Figure 4.
Interaction between the patient’s interface and some of the components of the Platform of Services.
4.1. CogniViTra Box
The concept that supported the design of the CogniViTra Box was the creation of an aesthetic and functional hub, serving as interface between the user and the CogniViTra application, without the need for a bulky computer.
As presented in Figure 5, the CogniViTra Box is connected to a TV. Moreover, a Universal Serial Bus (USB) keyboard and mouse, a Wi-Fi network, and an external speaker can be added. However, if the TV is connected through High-Definition Multimedia Interface (HDMI), the speaker will not be necessary.
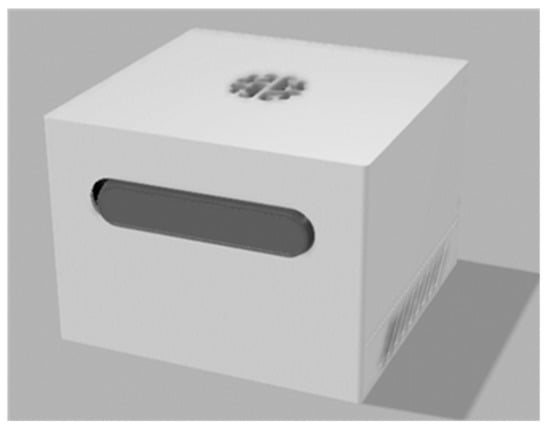
Figure 5.
CogniViTra Box and peripheral devices at home.
Figure 6 and Figure 7 represent the CogniViTra Box in a higher level of detail, with the components that are encased, specifically the single board computer (SBC) (i.e., Intel/Aaeon Up Squared), the vision processing unit (VPU) (i.e., Intel Movidius Myriad X), the uninterruptible power supply (UPS) and perception devices (i.e., video and audio).
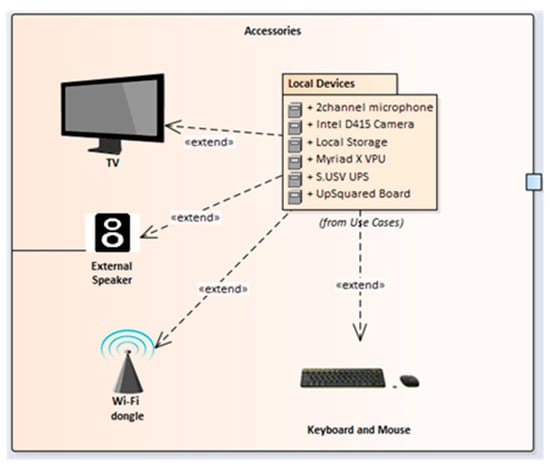
Figure 6.
CogniViTra Box enclosure, 3D render.
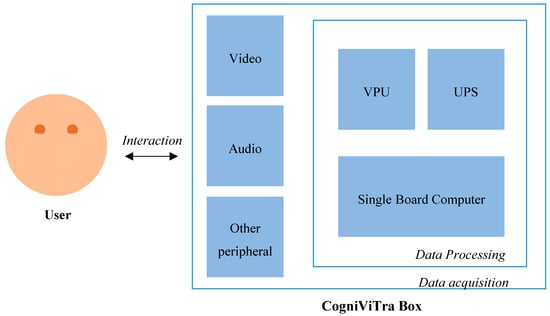
Figure 7.
Details of the CogniViTra Box.
The hardware components require specific drivers or operating system versions and kernels. Therefore, a specific configuration is required in order to achieve a complete synergy between the components:
- With the UPS requiring the latest version of the Ubuntu operating system (18.04 Long Term Support) and the VPU requiring at least version 16, the first step is to install and activate the Ubuntu operating system on the main board;
- Having the operating system and kernel installed, all peripheral ports will be available, and the remaining drivers can be installed in any order, namely the latest version of OpenVINO, OpenCV 3.4.4, Python 3.7, Virtualenv, and also Intel RealSense Software Development Kit 2.0.
For the patient side of the system, it is preferable to have the software start-up as automatic as possible, with minimal human interaction or patient training required. To achieve this, because the CogniViTra Box is Ubuntu-based, the boot process was simplified to the minimum, and the only interaction required is the user login.
The start-up script includes initialization, the use of the correct workspace, the launching of the required software as a background task, and the activation of a browser with the CogniViTra website already open.
4.2. Interaction Management
CogniViTra Patient Interaction (Figure 8) comprises three parts: (i) Digital Coach; (ii) Games Presentation; and (iii) Pose and Gesture Recognition. The first two components are presented in two iframes, one with fixed content (i) and the other dynamic (ii). The dynamic content iframe presents all the games as well the web pages from which exercises can be selected, working as normal of Hypertext Markup Language (HTML) documents. The third component, Pose and Gesture Recognition, aims to gather feedback from the patients by recognizing predefined static poses and gestures and is configurable for use in a home or a clinical setting.
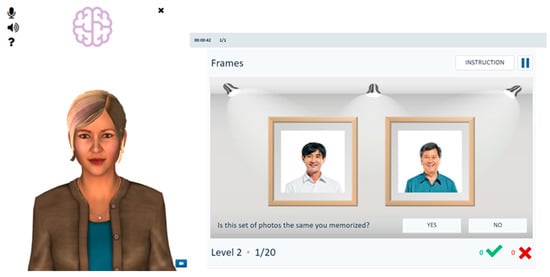
Figure 8.
Layout of the patient interface.
4.2.1. Digital Coach
The Digital Coach is based on a 3D human embodied conversational agent (named Rachel) designed to transmit a comfortable feeling and able to communicate using natural language, with which the patients can interact using a multimodal interface, including automatic speech recognition and a graphical touch-based user interface. To closely simulate the human conversational behavior, the Digital Coach includes components for speech recognition, synthesis of speech, sound and movement, synchronized non-verbal behaviors such as head nods and facial expressions, and dialogue management. To enable speech interaction, the microphone and high-definition speakers of the CogniViTra Box are used.
The Digital Coach was developed using SmartBodyJS.js (a JavaScript compiled Library based on SmartBody [71] that allows quick development of virtual agents). The behavior and locomotion are manipulated using Behavioral Markup Language (BML) tags. Achieving poses and gestures is important to strengthen the interaction between the user and the Digital Coach as this is a form of non-verbal communication. In this respect, SmartBody has a set of pre-compiled character behaviors such as posture, animations (e.g., jogging, walking, or playing guitar) and gazes (e.g., staring at an object). Moreover, in terms of speech synthesis, the SmartBody allows the synchronization of the audio input with the movements of the embodied conversational agent, namely in terms of mouth movements, which contributes to the naturalness of the interaction.
4.2.2. Games Presentation
The Games Presentation was developed primarily with web technology, using a combination of HTML, Hypertext Preprocessor (PHP), and JavaScript. All pages are rendered on the Platform of Services side to guarantee that all sensitive and private information remains safe on the backend. For this reason, PHP is used extensively to communicate with the Platform of Services, and, in turn, from the Platform of Services side, JavaScript was used for the implementation of the Cognitive Games Engine, being in charge of the most dynamic details of the pages and also responsible for control and operation of all cognitive games available in the system (Figure 9).
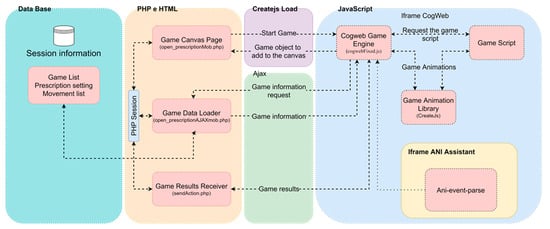
Figure 9.
Architecture of the Cognitive Game Engine.
The client-side elements, implemented in HTML and PHP, are:
- Game Canvas Page, where the game is presented on the client side;
- Game Data Loader, the point of access to information related to the game (e.g., game Id, name, or language);
- Game Results Receiver, the point of reception and storage of game results.
- These three elements are internments united by the PHP session system, which retains all information regarding client authentication and identification during the operation period.
- Looking at the Cognitive Game Engine from the Platform of Services side, the JavaScript elements are:
- Game Animation Library, which uses a set of modular libraries and tools that work together or independently to allow interactive web content called CreateJS;
- Cognitive Game Engine, the central point in our system, being responsible for managing several important exercise system elements, such as game loading and subsequent presentation on the canvas;
- Game Script, the file with specific logical instructions (e.g., operation or winning conditions) from the game, developed and generated in Adobe Animate.
The Cognitive Game Engine provides classes and methods responsible for various tasks related to the game presentation process, graphic interface around the game (inside the canvas), and communication with the Platform of Services. These tasks vary over the different phases of the games’ operation as presented in Figure 10.
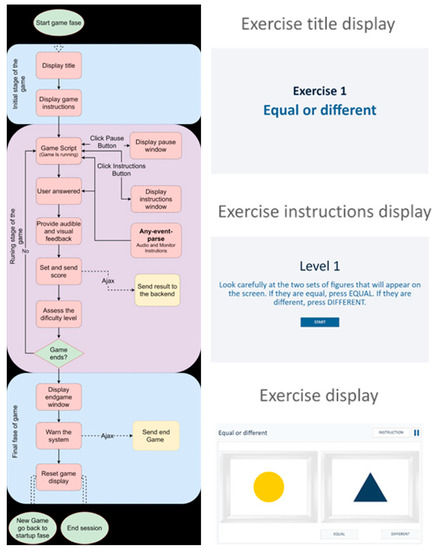
Figure 10.
Flowchart of the Cognitive Game Engine during the various phases of the rehabilitation exercise.
During the initial stage, the game canvas is loaded on the page, and the Cognitive Game Engine commences. Then, the basic game information and the necessary resources for the game such as images, sounds, and message texts are loaded as well as the game script.
The game starts with the presentation of the title in the display for a few seconds (e.g., exercise title screen of Figure 10), which is followed by the presentation of the game instructions on the screen (e.g., exercise instruction screen of Figure 10). Then, the game enters a standby mode and only starts when user input occurs.
After the user input occurs, the game script becomes responsible for the game, while the engine in the background manages the click events of pause and instructive buttons and responds as expected, displaying a window with a pause or some instructions (e.g., Figure 10), monitors the responses given by patients to update the results to define and adjust game difficulty level between attempts, and determines whether the game will end. When this occurs, the Cognitive Games Engine is responsible for evaluating whether the exercise session has ended or not, and, if not, the cycle starts over again for the next game. Otherwise, the session ends, the backend receives the end of session information, and the user is sent to the portal of the patient.
4.2.3. Pose and Gesture Recognition
Pose and gesture language such as head nodding, body postures, and hand gestures are effective communication channels in human–human collaboration and can be categorized into three types with respect to which part of the body is engaged [72]:
- Body―full body poses, actions or motions;
- Hand and arm―arm pose and hand gestures;
- Head and face―nodding or shaking head, winkling lips.
According to the requirements of CogniViTra, the Pose and Gesture Recognition module was designed to recognize the three types of gesture and poses: full body poses, actions, or motions (e.g., ‘trunk displacement to the left’ or ‘trunk displacement to the right’), arm poses and hand gestures (e.g., ‘arms raised’, singular or both) and nodding or shaking head (e.g., ‘head tilt to the left’ or ‘head tilt to the right’).
The process of Pose and Gesture Recognition can be divided into four essential sections as follows:
- Sensor data collection―the raw data of poses and gestures are captured by sensors;
- Pose and gesture identification—in each frame, a pose or a gesture is identified from raw data;
- Pose and gesture tracking―the located skeleton is tracked during body movement;
- Pose and gesture classification―tracked pose or gesture is classified according to predefined pose and gesture types.
The sensors that can be utilized in Pose and Gesture Recognition can be classified into two main groups, image-based and non-image-based [73]. In turn, the image-based technologies can be further categorized into four different classes, depending on the type of sensor being used. Hence, we can find approaches using markers [72], a single camera [74], stereo cameras [75], and depth sensors [76,77,78]. Although image-based methods have been dominant in recognizing poses and gestures for several decades, recently, the developments related to sensors have opened new possibilities in terms of non-image-based Pose and Gesture Recognition methods. Several approaches include wearable sensors such as glove-based gestural interfaces [79] and band-based sensors relying on a wristband or a similar wearable device [80,81,82,83]. Furthermore, a third type of non-image-based technologies adopts non-wearable sensors. Non-wearable sensors can detect poses and gestures without contacting the human body, for example using radio frequency sensors or radar [84,85,86,87,88]. Considering the CogniViTra implementation, the CogniViTra Box provides a single camera and depth sensors to perform the required data collection.
Identification is the first stage in Pose and Gesture Recognition, after the raw data acquisition by sensors. In the present implementation, a skeleton model approach was applied that employs a human skeleton to distinguish human body poses and simplify pose and gesture classification, as shown in Figure 11 [89].

Figure 11.
Example of skeleton model identification.
Pose and gesture tracking as the process of finding temporal correspondences between frames and continuous tracking of an identified pose and gesture in the previous frames with current frame is not required in the current implementation of CogniViTra, since the focus is static poses and gestures that can be represented by only one frame.
Pose and gesture classification is the last but somehow most determining step in recognition. It can be resolved by many popular artificial intelligence and machine learning algorithms including K-nearest neighbors [90,91], hidden Markov model [92,93], support vector machines [94,95,96,97], artificial neural networks [98,99,100], and deep learning algorithms, from which currently two methods are popular, namely convolutional neural networks and recurrent neural networks [101].
In CogniViTra, our approach was to adopt existing open-source frameworks and tools, in particular, the available implementations based on convolutional neural networks, for which OpenPose lay the foundations for the part affinity field (PAF) algorithm proposed by the authors of this tool [102]. In Figure 12, we depict the classes that are used in the software in order to analyze the patients’ poses and gestures.
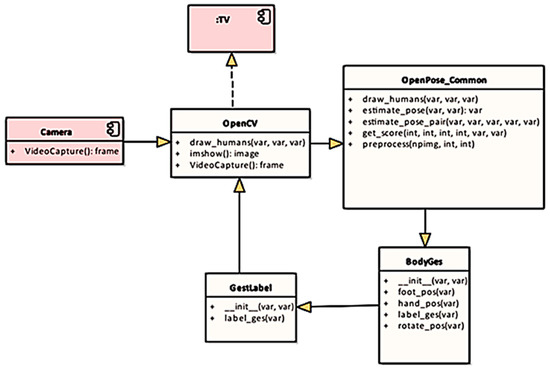
Figure 12.
Pose and Gesture Recognition classes.
The algorithm behind the skeleton output to pose estimation is based on the relative position of the 18 skeleton key points between each other.
This approach gives the patients more mobility to answer to the cognitive challenges without restricting them to a very rigid position, since there is an area where each specific pose is considered valid. For example, by having the wrist key point above the eye key point at a certain threshold distance, there is a large area to recognize the ‘arm up’ answers. This minimizes incorrect answers due to the patient’s physical difficulties (e.g., shoulder impingements).
In the case of the 3D movements such as the punches, the approach is similar; however, both frames (i.e., red, green, and blue—RGB―and depth frames) are aligned with the data merged in order to determine the depth of the key point, making it possible to detect, for instance, a wrist with a depth lower than the neck.
Hence, the accuracy of the exercises is not measured in terms of very specific pose patterns but rather is evaluated within an area or a volume in a broader space referenced in the sensor’s frames. This approach was considered adequate for the specific application scenario of CogniViTra, since it is acceptable to compromise precision while ensuring accuracy: It is preferable to identify the pose, even if deviates from the ideal form, instead of discarding it and breaking the intended aim of the rehabilitation exercise being performed.
5. Assessment
5.1. Methods
A peer review assessment [103] was conducted to gather the opinion of peers about CogniViTra. A prototype was prepared to be exposed in a highly specialized event related to healthy and active ageing, and key stakeholders were invited to test it and to share their opinion. The event chosen was the AAL FORUM 2019 [104], which took place in the city of Aarhus in Denmark in September 2019. The audience included technological developers with an interest in healthy and active ageing, health care and social care providers, investors looking for new solutions and innovations, individuals participating in research projects, and European, national, and regional decision-makers in the fields of health care, social issues, and technological innovations [20].
Participants comprised a convenience sample of individuals recruited using the hallway technique (i.e., the participants that walked by the CogniViTra stand were invited to participate). The defined inclusion criteria were being a participant in the AAL Forum and consequently being a stakeholder for the development of applications based on information technologies to support healthy and active ageing, understanding the study, accepting to voluntarily participate in the study, and giving informed consent.
All steps were taken to protect participants’ privacy, and all relevant rules on data privacy were followed. Information allowing identification of participants was not captured. The participants were distinguished in the study documents by a unique running number. The researchers involved in conducting and reporting the study were obliged to professional secrecy. The principal investigator was responsible for making sure that all members of the team were aware they must not reveal information obtained by granting access to research data to anyone outside the scientific research team.
Prior to the interaction with the application, the participants received all information about CogniViTra, the assessment objectives, duration, and methods. A member of the research team explained that participants could request additional information about the study at any moment and abandon the study at any time without any explanation or personal prejudice. Moreover, all participants completed and signed informed consent.
Each test followed three stages: (i) pre-test: the participants received all the information about CogniViTra and clarified all the questions they had; (ii) test: the participants interacted freely with CogniViTra for as long as they wanted and performed a dual-task exercise (i.e., answering to a cognitive set of tasks with a physical movements); and (iii) post-test: the participants were asked to fill in an opinion questionnaire on a tablet and to share their insights regarding the CogniViTra prototype.
The questionnaire used to gather the data was specifically created for this study and included sociodemographic information, namely country, age and gender, opinions about CogniViTra, expectation of use, perception of its market value, suggestions for improvement, and other comments.
5.2. Prototype Setup
Different living room configurations were considered for the two testing setups, resulting in a ‘high setup’ and a ‘low setup’ (Figure 13 and Figure 14). Both configurations only differ in the height at which the CogniViTra Box is placed in front of the user. In the ‘high setup’ the height of the box is of about 0.9 m, while in the ‘low setup’ it stands at 0.45 m, measured from the ground plane. A location of two meters from the CogniViTra Box is recommended to optimize pose and gesture detection.
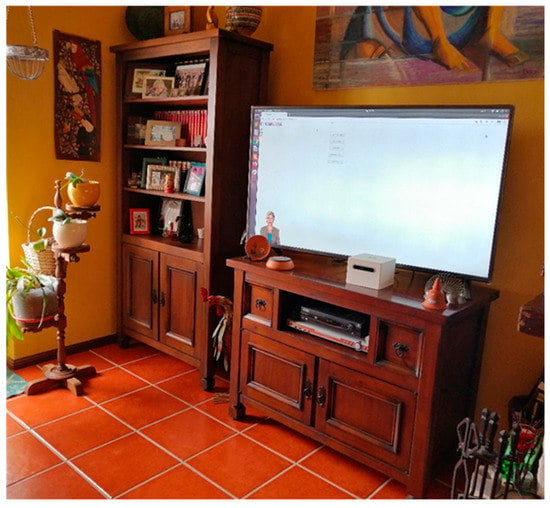
Figure 13.
Prototype deployed in a living room―‘high setup’.
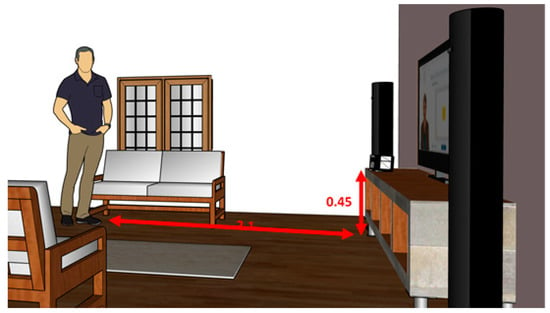
Figure 14.
Prototype deployed in a living room―‘low setup’.
In the exercise selected for the experiment (Figure 15), the participants had to perform an attention task, comparing the figures in the left and right boards, and choosing between the ‘equal’ or ‘different’ options by performing two different movements.
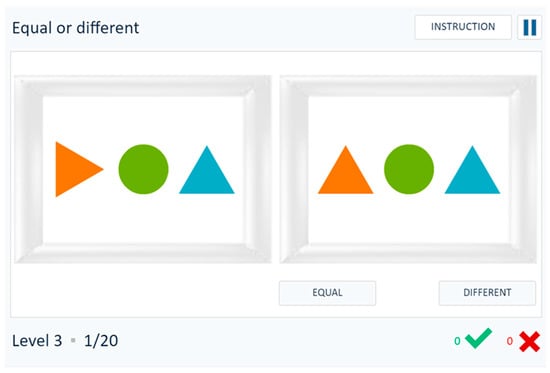
Figure 15.
Exercise selected for the experiment.
To prepare the experimental set-up, a set of nine different poses and gestures were considered: ‘arms raised’ (singular or both), ‘head tilt/twist’ (both sides), ‘punch movement’ (both arms), and ‘trunk displacement’ (to the left and to the right). As an example, Figure 16 presents the pose and gesture ‘arm raised’ (singular and both), where the images represent the inference output from a pre-trained model with depth expansion, over the RGB stream with a depth-based background subtraction.
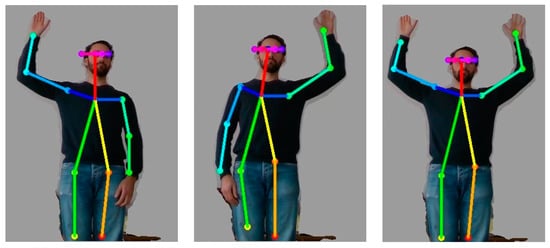
Figure 16.
Right hand up, left hand up and both hands up.
As a testing procedure, we conducted trials with five different subjects performing a sequence of pose and gesture combinations. Each pose and gesture combination was repeated 20 times each in the two different box installation setups. The conditions of the test sites simulated different living room environments (e.g., cluttered background, different lighting conditions, or different furniture layout). To consider a positive recognition of a pose and gesture, the same classification result had to be maintained over five frames, which a clear result to be identified by the system.
Additionally, as a pre-condition to the testing, the users were instructed on how to correctly perform a pose and gesture, and they had available a feedback mechanism (e.g., visual feedback of their skeleton model as perceived by the system) to avoid errors due to human factor. We accordingly conducted the trials always being sure that the user was performing the sequences, holding still for one second (i.e., corresponding to grabbing five frames) and not being influenced by uncertainty that could be caused by incorrect skeleton detection).The testing results were different in the two set-ups. While in the ‘low setup’, CogniViTra was 100% successful for all trials of all participants, for the ‘high setup’ the same performance was achieved for the poses and gestures ‘arm raised’ (singular and both), ‘look left’, and ‘look right’. For the remaining poses and gestures, the success rate was also high, being above 90%. According to these results, a comprehensive set of postures and gestures could be used for the peer review. After brainstorming, it was decided that the participants in the peer review should move the trunk to the left if they wanted to select the ‘equal’ option or to the right if they wanted to select the ‘different’ option.
5.3. Results of the Conceptual Validation
In the conceptual validation, the methodological approach of which is presented in [20], a sample of 57 peers from 16 different countries participated (Figure 17). The average age was 41.5 years (Standard Deviation = 11.4); the oldest participant was 66 years old, and the youngest was 24 years old. Regarding the gender, 32 participants (56%) were male, and 25 (43%) were female.
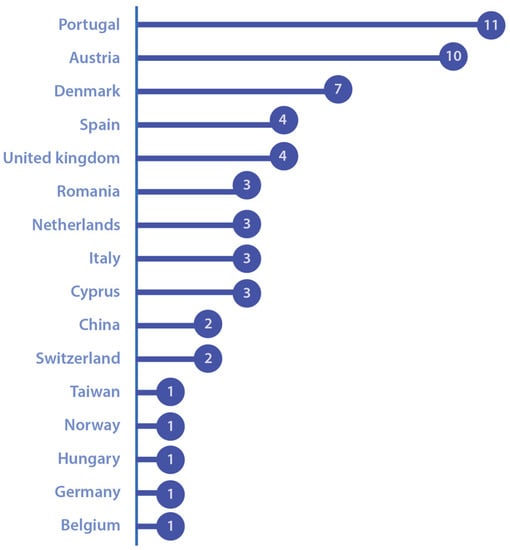
Figure 17.
Nationality of the participants.
Most of the participants (n = 53) expressed that they would use or suggest the utilization of CogniViTra. Of those, six participants (10%) stated that they would use it themselves for cognitive and physical training, while 23 (40%) mentioned that they would suggest this to a family member or a friend. Furthermore, 14 participants (25%) mentioned the intention to use it in their professional activities, and 10 (18%) would adopt CogniViTra in their organization so other staff members could use it (Figure 18).

Figure 18.
Expectation of use.
Regarding the aspects that the participants considered to be the topics that CogniViTra helps to solve (Figure 19), the most valued was the possibility of remote follow-up by health care providers (27%), followed by the possibility to extend the clinical setting to the home (24%) and increasing the number of training sessions (22%). The less valued aspects were the reduction of the costs with transportation to clinical settings (12%) and the closer follow-up from family and other informal careers (15%).
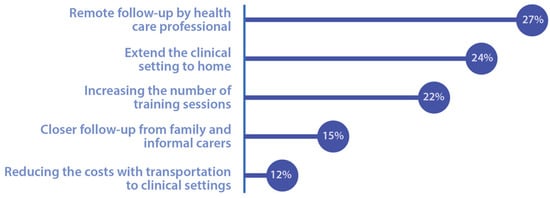
Figure 19.
CogniViTra valued aspects.
Finally, concerning the price that each participant would be willing to pay to use the system, most participants answered up to EUR 25, followed by the range of EUR 25 to EUR 50.
Participants made relevant comments and suggestions about the prototype: (i) inclusion of different levels of difficulties to accompany the entire performance spectrum, from very easy levels so that people with cognitive or physical limitations can use it, to levels with great difficulty, so that people with high performance are challenged to better themselves; (ii) improvement of the performance of the system response; (iii) revision of the icons and instructions, making them more appealing and intuitive; (iv) improvement of the exercise duration by including the option of doing shorter exercises, with 10 or 20 trials; and (v) improvement of the user interaction, namely the interaction with the Digital Coach, which should be further developed to greet, suggest drinking water, and indicate instructions.
6. Conclusions and Future Work
To achieve cognitive health benefits in the population, key clinical operations such as monitoring and assessment of cognitive functions and cognitive rehabilitation must be optimized. In this respect, the use of information technologies is seen as an opportunity to incorporate changes in operating processes of health systems. However, this incorporation currently suffers from a serious implementation problem [105], and there is an enormous difficulty for implementation and dissemination on a sufficient scale to allow the translation of value to the health level of the populations. This problem is not exclusive to cognitive health; it occurs in all fields of medicine and research, and for both pharmacological and non-pharmacological solutions or even innovations in terms of technologies, processes, and organization.
In this context, the study reported by this article aimed to take advantage of the flexibility of the existing resources of a Platform of Services, namely backend services, to optimize the implementation of an application for dual-task training, as well as to promote the integration of an existing Cognitive Health Ecosystem. This approach not only allowed the optimization of the quality of the implementation and the minimization of the associated development costs, but also the availability of a set of clinically validated cognitive exercises.
The major development efforts were concentrated in the interaction mechanism for the patients. A new user interface was developed that comprises a Digital Coach and two additional modules, Game Presentation and Pose and Gesture Recognition. The patients’ interaction is supported by specific hardware, the CogniViTra Box, which replaces the traditional computer and provides the hardware features to recognize poses and gestures.
An observational study was conducted to verify the viability of the dual-task training application. For this purpose, a functional prototype was exposed in a highly specialized event related to healthy and active ageing, and 57 participants were invited to share their opinion after testing the application. Positive feedback for the CogniViTra application was obtained From the participants. In general, participants considered that it is a useful application and may represent an added value for dual-task training, including cognitive and physical activities.
The fact that more than 90% of the participants expressed that they would use CogniViTra or suggest its utilization is an important indicator that shows a high level of acceptance and great potential of this application. Another interesting result is that some of the participants mentioned that they would use it themselves, which shows a change in mentality that results in an investment in preventive health and cognitive and physical training throughout the patient’s lifespan.
Another interesting contribution was the list of problems that CogniViTra helps to solve. The most valued aspects included the possibility for remote follow-up by health care providers and the possibility to extend the clinical setting by providing home care, to increase the number of training sessions, to reduce the costs with transportation, and to promote a closer follow-up from family and informal carers.
Although the results of this study were very positive and encouraging of further development, improvements in the system should be implemented before starting tests with real users. The participants suggestions focused on the difficulty level, the system response performance, the intuitiveness of icons and instructions, the user interaction, the exercise duration, and the inclusion of a suggestion to drink water. Most suggestions were in line with the requirements previously defined for CogniViTra and were already planned to be implemented in future versions of the prototype.
This article reports the first stage of the CogniViTra assessment to verify the viability of the application. For the second stage, a study involving users interacting with the application prototype in a controlled environment is planned to assess its usability. Finally, in the third stage, a multicentric clinical trial will be conducted in Portugal, Luxembourg, and Spain to assess the adherence, efficiency, and efficacy (i.e., lifestyles and quality of life changes) of the dual-task training supported by CogniViTra.
A total number of 180 participants (90 for the experimental group and another 90 for the control group) are estimated to be enrolled. According to the trial design, the intervention plan will have a duration of 12 weeks and include individual sessions (i.e., CogniViTra activities performed by a single participant in a clinical setting or at home) and group sessions (i.e., CogniViTra activities performed by various participants in a clinical setting). In terms of exercises, the dual-task training will encompass exercises related to different cognitive domains and the patients’ interactions will be based on physical exercises with different complexity levels (e.g., to move the arm towards the opposite hand, to move an arm towards the floor, or to crouch with hands on the knees and climb up and opening the arms).
In terms of outcomes, the clinical trial will compare the CogniViTra strategy to standard of care, in terms of (i) time spent on cognitive training and physical and social stimulation activities per participant; (ii) access to specialized activities per hour of specialized human resources; (iii) neuropsychiatric morbidity; (iv) quality of life; (iv) and compliance with behaviors that reduce the individual risk for a brain disease.
CogniViTra was conceptualized and designed prior to the emergence of the coronavirus pandemic situation, which led to the confinement of part of the world population. This situation made even more imperative the need for integrated solutions that allow continued care at home with provider support and advanced easy-to-use eHealth applications as in the case of CogniViTra.
Author Contributions
Conceptualization, J.P., J.Q.; N.P.R., V.T.C.; Methodology, A.I.M., J.P., J.Q.; L.N., N.P.R., V.T.C.; Software, H.S., S.S.; Validation, A.I.M., J.Q., L.N., S.S.; Investigation, J.P., A.I.M., A.C. (Antonio Callén), D.B., F.D., V.T.C.; Writing—original draft preparation, N.P.R.; Writing—review and editing, J.Q., J.P., A.I.M., A.C. (Antonio Callén), D.B., A.C. (António Cunha), N.P.R., V.T.C.; Project administration, J.Q. All authors have read and agreed to the published version of the manuscript.
Funding
This study has received funding from the European Union under the AAL programme through project CogniViTra (Grant No. AAL-2018-5-115-CP), with national funding support from FCT, ISCIII, and FNR. This presentation reflects the authors’ views, and neither AAL nor the National Funding Agencies are responsible for any use that may be made of the information.
Conflicts of Interest
The authors declare no conflict of interest.
Abbreviations
The following abbreviations are used in this manuscript:
| ABAC | Attribute-based access control |
| AES | Advanced Encryption Standard |
| BML | Behavioral markup language |
| CogniViTra | Cognitive Vitality Training |
| HDMI | High-Definition Multimedia Interface |
| HTML | Hypertext Markup Language |
| GCM | Galois/Counter Mode |
| JSON | JavaScript Object Notation |
| JWT | JSON Web Token |
| PAF | Part affinity field |
| PHP | Hypertext Preprocessor |
| RBAC | Role-based access control |
| RGB | Red, green, and blue |
| SBC | Single board computer |
| SOA | Service oriented architecture |
| USB | Universal Serial Bus |
| UPS | Uninterruptible power supply |
| VPU | Vision processing unit |
| XACML | eXtensible Access Control Markup Language |
References
- Irazoki, E.; Contreras-Somoza, L.M.; Toribio-Guzmán, J.M.; Jenaro-Río, C.; van der Roest, H.; Franco-Martín, M.A. Technologies for Cognitive Training and Cognitive Rehabilitation for People with Mild Cognitive Impairment and Dementia. A Systematic Review. Front. Psychol. 2020, 11, 648. [Google Scholar] [CrossRef] [PubMed]
- Lezak, M.D.; Howieson, D.B.; Loring, D.W.; Fischer, J.S. Neuropsychological Assessment; Oxford University Press: Oxford, UK, 2004. [Google Scholar]
- Tacchino, A.; Veldkamp, R.; Coninx, K.; Brulmans, J.; Palmaers, S.; Hämäläinen, P.; D’hooge, M.; Vanzeir, E.; Kalron, A.; Brichetto, G.; et al. Design, Development, and Testing of an App for Dual-Task Assessment and Training Regarding Cognitive-Motor Interference (CMI-APP) in People with Multiple Sclerosis: Multicenter Pilot Study. JMIR mHealth uHealth 2020, 8, e15344. [Google Scholar] [CrossRef] [PubMed]
- McIsaac, T.L.; Lamberg, E.M.; Muratori, L.M. Building a framework for a dual task taxonomy. BioMed Res. Int. 2015, 591475. [Google Scholar] [CrossRef]
- Plummer, P.; Osborne, M.B. What Are We Attempting to Improve When We Train Dual-Task Performance? J. Neurol. Phys. Ther. 2015, 39, 154–155. [Google Scholar] [CrossRef]
- Ansai, J.H.; de Andrade, L.P.; de Souza Buto, M.S.; de Vassimon Barroso, V.; Farche, A.C.S.; Rossi, P.G.; de Medeiros Takahashi, A.C. Effects of the addition of a dual task to a supervised physical exercise program on older adults’ cognitive performance. J. Aging Phys. Act. 2017, 25, 234–239. [Google Scholar] [CrossRef] [PubMed]
- Simon, S.S.; Yokomizo, J.E.; Bottino, C.M. Cognitive intervention in amnestic Mild Cognitive Impairment: A systematic review. Neurosci. Biobehav. Rev. 2012, 4, 1163–1178. [Google Scholar] [CrossRef] [PubMed]
- Suzuki, T.; Shimada, H.; Makizako, H.; Doi, T.; Yoshida, D.; Tsutsumimoto, K.; Anan, Y.; Uemura, K.; Lee, L.; Park, H. Effects of multicomponent exercise on cognitive function in older adults with amnestic mild cognitive impairment: A randomized controlled trial. BMC Neurol. 2012, 1, 1–9. [Google Scholar] [CrossRef] [PubMed]
- Suzuki, T.; Shimada, H.; Makizako, H.; Doi, T.; Yoshida, D.; Ito, K.; Shimokata, H.; Washimi, Y.; Endo, H.; Kato, T. A randomized controlled trial of multicomponent exercise in older adults with mild cognitive impairment. PLoS ONE 2013, 4, e61483. [Google Scholar] [CrossRef] [PubMed]
- Langhorne, P.; Bernhardt, J.; Kwakkel, G. Stroke rehabilitation. Lancet 2011, 9778, 1693–1702. [Google Scholar] [CrossRef]
- Aminoff, M.J.; Boller, F.; Swaab, D.F. Foreward. In Handbook of Clinical Neurology; Michael, P.B., David, C.G., Eds.; Elsevier: Amsterdam, The Netherlads, 2013. [Google Scholar]
- Barnes, M.P.; Good, D.C. Preface. In Handbook of Clinical Neurology; Michael, P.B., David, C.G., Eds.; Elsevier: Amsterdam, The Netherlads, 2013. [Google Scholar]
- Barnes, D.E.; Santos-Modesitt, W.; Poelke, G.; Kramer, A.F.; Castro, C.; Middleton, L.E.; Yaffe, K. The Mental Activity and eXercise (MAX) trial: A randomized controlled trial to enhance cognitive function in older adults. JAMA Intern. Med. 2013, 9, 797–804. [Google Scholar] [CrossRef] [PubMed]
- Anderson-Hanley, C.; Barcelos, N.M.; Zimmerman, E.A.; Gillen, R.W.; Dunnam, M.; Cohen, B.D.; Yerokhin, V.; Miller, K.; Hyes, D.; Arciero, P.; et al. The aerobic and cognitive exercise study (ACES) for community-dwelling older adults with or at-risk for mild cognitive impairment (MCI): Neuropsychological, neurobiological and neuroimaging outcomes of a randomized clinical trial. Front. Aging Neurosci. 2018, 10, 76. [Google Scholar] [CrossRef] [PubMed]
- Damirchi, A.; Hosseini, F.; Babaei, P. Mental training enhances cognitive function and BDNF more than either physical or combined training in elderly women with MCI: A small-scale study. Am. J. Alzheimer’s Dis. Other Dement. 2018, 1, 20–29. [Google Scholar] [CrossRef]
- Gallou-Guyot, M.; Mandigout, S.; Combourieu-Donnezan, L.; Bherer, L.; Perrochon, A. Cognitive and physical impact of cognitive-motor dual-task training in cognitively impaired older adults: An overview. Neurophysiol. Clinique. 2020, 6, 441–453. [Google Scholar] [CrossRef] [PubMed]
- Tay, L.; Lim, W.S.; Chan, M.; Ali, N.; Chong, M.S. A combined cognitive stimulation and physical exercise programme (MINDVital) in early dementia: Differential effects on single-and dual-task gait performance. Gerontology 2016, 6, 604–610. [Google Scholar] [CrossRef]
- Liao, Y.Y.; Chen, I.; Lin, Y.J.; Chen, Y.; Hsu, W.C. Effects of virtual reality-based physical and cognitive training on executive function and dual-task gait performance in older adults with mild cognitive impairment: A randomized control trial. Front. Aging Neurosci. 2019, 11, 162. [Google Scholar] [CrossRef]
- McCaskey, M.A.; Schättin, A.; Martin-Niedecken, A.L.; de Bruin, E.D. Making more of IT: Enabling intensive motor cognitive rehabilitation exercises in geriatrics using information technology solutions. BioMed Res. Int. 2018, 2018, 1–17. [Google Scholar] [CrossRef]
- Martins, A.I.; Quintas, J.; Neves, L.; Sousa, S.; Cruz, V.T.; Pais, J.; Benhsain, D.; Callén, A.; Rocha, N.P. Cognivitra: An Information Technology-Based Solution to Support Cognitive and Physical Training at Home. In Proceedings of the 9th International Conference on Software Development and Technologies for Enhancing Accessibility and Fighting Info-exclusion, Vila Real, Portugal, 2–4 December 2020. [Google Scholar]
- Cruz, V.T.; Pais, J.; Ruano, L.; Mateus, C.; Colunas, M.; Alves, I.; Barreto, R.; Conde, E.; Sousa, A.; Araújo, I.; et al. Implementation and Outcomes of a Collaborative Multi-Center Network Aimed at Web-Based Cognitive Training–COGWEB Network. JMIR Ment. Health 2014, 1, e2. [Google Scholar] [CrossRef] [PubMed]
- Ruano, L.; Sousa, A.; Severo, M.; Alves, I.; Colunas, M.; Barreto, R.; Mateus, C.; Moreira, S.; Conde, E.; Bento, V.; et al. Development of a self-administered web-based test for longitudinal cognitive assessment. Sci. Rep. 2016, 1, 1–10. [Google Scholar] [CrossRef]
- Cicerone, K.D.; Langenbahn, D.M.; Braden, C.; Malec, J.F.; Kalmar, K.; Fraas, M.; Felicetti, T.; Laatsch, L.; Harley, J.P.; Bergquist, T.; et al. Evidence-based cognitive rehabilitation: Updated review of the literature from 2003 through 2008. Arch. Phys. Med. Rehabil. 2011, 4, 519–530. [Google Scholar] [CrossRef]
- Seshadri, S.; Wolf, P.A. Lifetime risk of stroke and dementia: Current concepts, and estimates from the Framingham Study. Lancet Neurol. 2007, 12, 1106–1114. [Google Scholar] [CrossRef]
- Vincent, C.; Desrosiers, J.; Landreville, P.; Demers, L. Burden of caregivers of people with stroke: Evolution and predictors. Cerebrovasc. Dis. 2009, 27, 456–464. [Google Scholar] [CrossRef] [PubMed]
- Rebok, G.W.; Langbaum, J.B.; Jones, R.N.; Gross, A.L.; Parisi, J.M.; Spira, A.P.; Kueider, A.M.; Petras, H.; Brandt, J. Memory training in the active study: How much is needed and who benefits? J. Aging Health 2012, 21S–42S. [Google Scholar] [CrossRef]
- World Health Organization. Atlas: Global Resources for Persons with Intellectual Disabilities; WHO Press: Geneva, Switzerland, 2007. [Google Scholar]
- Eaton, J.; McCay, L.; Semrau, M.; Chatterjee, S.; Baingana, F.; Araya, R.; Ntulo, C.; Thornicroft, G.; Saxena, S. Scale up of services for mental health in low-income and middle-income countries. Lancet 2011, 378, 1592–1603. [Google Scholar] [CrossRef]
- Kakuma, R.; Minas, H.; van Ginneken, N.; Dal Poz, M.R.; Desiraju, K.; Morris, J.E.; Saxena, S.; Scheffler, R.M. Human resources for mental health care: Current situation and strategies for action. Lancet 2011, 378, 1654–1663. [Google Scholar] [CrossRef]
- Putman, K.; de Wit, L. European comparison of stroke rehabilitation. Top Stroke Rehabil. 2009, 16, 20–26. [Google Scholar] [CrossRef] [PubMed]
- De Wit, L.; Putman, K.; Schuback, B.; Komárek, A.; Angst, F.; Baert, I.; Berman, P.; Bogaerts, K.; Brinkmann, N.; Connell, L.; et al. Motor and functional recovery after stroke: A comparison of 4 european rehabilitation centers. Stroke 2007, 38, 2101–2107. [Google Scholar] [CrossRef]
- Zeiler, S.R.; Krakauer, J.W. The interaction between training and plasticity in the poststroke brain. Curr. Opin. Neurol. 2013, 26, 609–616. [Google Scholar] [CrossRef]
- Dobkin, B.H.; Dorsch, A. The promise of mhealth: Daily activity monitoring and outcome assessments by wearable sensors. Neurorehabil. Neural Repair 2011, 25, 788–798. [Google Scholar] [CrossRef] [PubMed]
- Hobart, J.C.; Cano, S.J.; Zajicek, J.P.; Thompson, A.J. Rating scales as outcome measures for clinical trials in neurology: Problems, solutions, and recommendations. Lancet Neurol. 2007, 6, 1094–1105. [Google Scholar] [CrossRef]
- Rosser, N.; Floel, A. Pharmacological enhancement of motor recovery in subacute and chronic stroke. Neurorehabilitation 2008, 23, 95–103. [Google Scholar] [CrossRef] [PubMed]
- Iosa, M.; Morone, G.; Fusco, A.; Bragoni, M.; Coiro, P.; Multari, M.; Venturiero, V.; de Angelis, D.; Pratesi, L.; Paolucci, S. Seven capital devices for the future of stroke rehabilitation. Stroke Res. Treat. 2012, 187965. [Google Scholar] [CrossRef]
- Selzer, M.E. Textbook of Neural Repair and Rehabilitation; Cambridge University Press: New York, NY, USA, 2006. [Google Scholar]
- Sharma, N.; Classen, J.; Cohen, L.G. Neural plasticity and its contribution to functional recovery. Handb. Clin. Neurol. 2013, 110, 3–12. [Google Scholar]
- Behrman, A.L.; Bowden, M.G.; Rose, D.K. Chapter 5—Clinical trials in neurorehabilitation. In Handbook of Clinical Neurology; Michael, P.B., David, C.G., Eds.; Elsevier: Amsterdam, The Netherlads, 2013. [Google Scholar]
- Mahncke, H.W.; Connor, B.B.; Appelman, J.; Ahsanuddin, O.N.; Hardy, J.L.; Wood, R.A.; Joyce, N.M.; Boniske, T.; Atkins, S.M.; Merzenich, M.M. Memory enhancement in healthy older adults using a brain plasticity-based training program: A randomized, controlled study. Proc. Natl. Acad. Sci. USA 2006, 103, 12523–12528. [Google Scholar] [CrossRef] [PubMed]
- La Rue, A. Healthy brain aging: Role of cognitive reserve, cognitive stimulation, and cognitive exercises. Clin. Geriatr. Med. 2010, 26, 99–111. [Google Scholar] [CrossRef]
- Nudo, R.J. Recovery after brain injury: Mechanisms and principles. Front. Hum. Neurosci. 2013, 7, 887. [Google Scholar] [CrossRef]
- Gardner, W.J.; Karnosh, L.J.; McClure, C.C., Jr.; Gardner, A.K. Residual function following hemispherectomy for tumour and for infantile hemiplegia. Brain 1955, 78, 487–502. [Google Scholar] [CrossRef]
- Chen, R.; Cohen, L.G.; Hallett, M. Nervous system reorganization following injury. Neuroscience 2002, 111, 761–773. [Google Scholar] [CrossRef]
- Staudt, M. Reorganization after pre- and perinatal brain lesions. J. Anat. 2010, 217, 469–474. [Google Scholar] [CrossRef] [PubMed]
- Cohen, L.G.; Weeks, R.A.; Sadato, N.; Celnik, P.; Ishii, K.; Hallett, M. Period of susceptibility for cross-modal plasticity in the blind. Ann. Neurol. Off. J. Am. Neurol. Assoc. Child Neurol. Soc. 1999, 4, 451–460. [Google Scholar] [CrossRef]
- Eyre, J.A. Corticospinal tract development and its plasticity after perinatal injury. Neurosci. Biobehav. Rev. 2007, 31, 1136–1149. [Google Scholar] [CrossRef] [PubMed]
- Jacobs, R.; Harvey, A.S.; Anderson, V. Executive function following focal frontal lobe lesions: Impact of timing of lesion on outcome. Cortex 2007, 43, 792–805. [Google Scholar] [CrossRef]
- He, Y.; Yang, L.; Zhou, J.; Yao, L.; Pang, M.Y. Dual-task training effects on motor and cognitive functional abilities in individuals with stroke: A systematic review. Clin. Rehabil. 2018, 7, 865–877. [Google Scholar] [CrossRef]
- Wang, X.; Pi, Y.; Chen, P.; Liu, Y.; Wang, R.; Chan, C. Cognitive motor interference for preventing falls in older adults: A systematic review and meta-analysis of randomised controlled trials. Age Ageing 2014, 44, 205–212. [Google Scholar] [CrossRef]
- Bacha, J.M.R.; Gomes, G.C.V.; de Freitas, T.B.; Viveiro, L.A.P.; da Silva, K.G.; Bueno, G.C.; Pompeu, J.E. Effects of Kinect adventures games versus conventional physical therapy on postural control in elderly people: A randomized controlled trial. Games Health J. 2018, 7, 24–36. [Google Scholar] [CrossRef]
- Lotfi, A.; Langensiepen, C.; Yahaya, S.W. Socially assistive robotics: Robot exercise trainer for older adults. Technologies 2018, 6, 32. [Google Scholar] [CrossRef]
- Kannan, L.; Vora, J.; Bhatt, T.; Hughes, S.L. Cognitive-motor exergaming for reducing fall risk in people with chronic stroke: A randomized controlled trial. Neurorehabilitation 2019, 44, 493–510. [Google Scholar] [CrossRef] [PubMed]
- Sturnieks, D.L.; Menant, J.; Valenzuela, M.; Delbaere, K.; Sherrington, C.; Herbert, R.D.; Lord, S.R. Effect of cognitive-only and cognitive-motor training on preventing falls in community-dwelling older people: Protocol for the smart±step randomised controlled trial. BMJ Open 2019, 9, e029409. [Google Scholar] [CrossRef]
- Arlati, S.; Colombo, V.; Spoladore, D.; Greci, L.; Pedroli, E.; Serino, S.; Sacco, M. A social virtual reality-based application for the physical and cognitive training of the elderly at home. Sensors 2019, 19, 261. [Google Scholar] [CrossRef]
- Andriella, A.; Torras, C.; Alenya, G. Cognitive system framework for brain-training exercise based on human-robot interaction. Cogn. Comput. 2020, 12, 793–810. [Google Scholar] [CrossRef]
- Yun, S.J.; Kang, M.G.; Yang, D.; Choi, Y.; Kim, H.; Oh, B.M.; Seo, H.G. Cognitive Training Using Fully Immersive, Enriched Environment Virtual Reality for Patients with Mild Cognitive Impairment and Mild Dementia: Feasibility and Usability Study. JMIR Serious Games 2020, 8, e18127. [Google Scholar] [CrossRef] [PubMed]
- Phirom, K.; Kamnardsiri, T.; Sungkarat, S. Beneficial Effects of Interactive Physical-Cognitive Game-Based Training on Fall Risk and Cognitive Performance of Older Adults. Int. J. Environ. Res. Public Health 2020, 17, 6079. [Google Scholar] [CrossRef] [PubMed]
- Peng, H.T.; Tien, C.W.; Lin, P.S.; Peng, H.Y.; Song, C.Y. Novel mat exergaming to improve the physical performance, cognitive function, and dual-task walking and decrease the fall risk of community-dwelling older adults. Front. Psychol. 2020, 11, 1620. [Google Scholar] [CrossRef]
- Adcock, M.; Fankhauser, M.; Post, J.; Lutz, K.; Zizlsperger, L.; Luft, A.R.; de Bruin, E.D. Effects of an in-home multicomponent exergame training on physical functions, cognition, and brain volume of older adults: A randomized controlled trial. Front. Med. 2020, 6, 321. [Google Scholar] [CrossRef]
- Manuli, A.; Maggio, M.G.; Latella, D.; Cannavò, A.; Balletta, T.; de Luca, R.; Calabrò, R.S. Can robotic gait rehabilitation plus Virtual Reality affect cognitive and behavioural outcomes in patients with chronic stroke? A randomized controlled trial involving three different protocols. J. Stroke Cerebrovasc. Dis. 2020, 29, 104994. [Google Scholar] [CrossRef] [PubMed]
- Zhang, H.; Shen, Z.; Liu, S.; Yuan, D.; Miao, C. Ping Pong: An Exergame for Cognitive Inhibition Training. Int. J. Hum. Comput. Interact. 2021, 1–12. [Google Scholar] [CrossRef]
- Swinnen, N.; Vandenbulcke, M.; de Bruin, E.D.; Akkerman, R.; Stubbs, B.; Firth, J.; Vancampfort, D. The efficacy of exergaming in people with major neurocognitive disorder residing in long-term care facilities: A pilot randomized controlled trial. Alzheimers Res. Ther. 2021, 13, 1–13. [Google Scholar] [CrossRef] [PubMed]
- Jardim, N.Y.V.; Bento-Torres, N.V.O.; Costa, V.O.; Carvalho, J.P.R.; Pontes, H.T.S.; Tomás, A.M.; Diniz, C.W.P. Dual-Task Exercise to Improve Cognition and Functional Capacity of Healthy Older Adults. Front. Aging Neurosci. 2021, 13, 33. [Google Scholar] [CrossRef] [PubMed]
- Molhemi, F.; Monjezi, S.; Mehravar, M.; Shaterzadeh-Yazdi, M.J.; Salehi, R.; Hesam, S.; Mohammadianinejad, E. Effects of virtual reality vs conventional balance training on balance and falls in people with multiple sclerosis: A randomized controlled trial. Arch. Phys. Med. Rehabil. 2021, 102, 290–299. [Google Scholar] [CrossRef]
- Laskey, K.B.; Laskey, K. Service oriented architecture. Wiley Interdiscip. Rev. Comput. Stat. 2009, 1, 101–105. [Google Scholar] [CrossRef]
- Wechsler, D. WAIS-III Administration and Scoring Manual; Psychological Corporation: San Antonio, TX, USA, 1997. [Google Scholar]
- Rosa, M.; Barraca, J.P.; Zuquete, A.; Rocha, N.P. A Parser to Support the Definition of Access Control Policies and Rules Using Natural Languages. J. Med. Syst. 2020, 44, 1–12. [Google Scholar] [CrossRef] [PubMed]
- OASIS, XACML (2013). Available online: http://docs.oasis-open.org/xacml/3.0/xacml-3.0-core-spec-os-en.html (accessed on 26 May 2021).
- Rosa, M.; Barraca, J.P.; Rocha, N.P. Blockchain structures to guarantee logging integrity of a digital platform to support community-dwelling older adults. Clust. Comput. 2020, 23, 1887–1898. [Google Scholar] [CrossRef]
- SmartBody. Available online: https://smartbody.ict.usc.edu/ (accessed on 7 April 2021).
- Mitra, S.; Acharya, T. Gesture recognition: A survey. IEEE Trans. Syst. Man Cybern. Part C 2007, 3, 311–324. [Google Scholar] [CrossRef]
- Liu, H.; Wang, L. Gesture recognition for human-robot collaboration: A review. Int. J. Ind. Ergon. 2018, 68, 355–367. [Google Scholar] [CrossRef]
- Starner, T.; Weaver, J.; Pentland, A. Real-time american sign language recognition using desk and wearable computer based video. IEEE Trans. Pattern Anal. Mach. Intell. 1998, 12, 1371–1375. [Google Scholar] [CrossRef]
- Wachs, J.P.; Kölsch, M.; Stern, H.; Edan, Y. Vision-based hand-gesture applications. Commun. ACM 2011, 2, 60–71. [Google Scholar] [CrossRef]
- Gokturk, S.B.; Yalcin, H.; Bamji, C. A time-of-flight depth sensor-system description, issues and solutions. In Proceedings of the 2004 Conference on Computer Vision and Pattern Recognition Workshop, Washington, DC, USA, 27 June–2 July 2004; pp. 33–35. [Google Scholar]
- Kapuściński, T.; Oszust, M.; Wysocki, M. Hand gesture recognition using time-of-flight camera and viewpoint feature histogram. In Intelligent Systems in Technical and Medical Diagnostics; Springer: Berlin/Heidelberg, Germany, 2014. [Google Scholar]
- Wang, C.; Liu, Z.; Chan, S.C. Superpixel-based hand gesture recognition with kinect depth camera. IEEE Trans. Multimed. 2014, 1, 29–39. [Google Scholar] [CrossRef]
- Erol, A.; Bebis, G.; Nicolescu, M.; Boyle, R.D. Vision-based hand pose estimation: A review. Comput. Vis. Image Underst. 2007, 1, 52–73. [Google Scholar] [CrossRef]
- Boyali, A.; Hashimoto, N.; Matsumoto, O. Hand posture and gesture recognition using MYO armband and spectral collaborative representation based classification. In Proceedings of the 2015 IEEE 4th Global Conference on Consumer Electronics (GCCE), Osaka, Japan, 27–30 October 2015; pp. 200–201. [Google Scholar]
- Zhang, Y.; Harrison, C. Wearable, low-cost electrical impedance tomography for hand gesture recognition. In Proceedings of the 28th Annual ACM Symposium on User Interface Software & Technology, Charlotte, NC, USA, 8–11 November 2015; pp. 167–173. [Google Scholar]
- Haroon, N.; Malik, A.N. Multiple hand gesture recognition using surface EMG signals. J. Biomed. Eng. Med. Imaging 2016, 1, 1. [Google Scholar] [CrossRef]
- Roy, S.; Ghosh, S.; Barat, A. Real-time implementation of electromyography for hand gesture detection using micro accelerometer. In Proceedings of the Artificial Intelligence and Evolutionary Computations in Engineering Systems 2016, Chennai, Tamilnadu, India, 19–21 May 2016; pp. 357–364. [Google Scholar]
- Google, Project Soli. 2015. Available online: atap.google.com/soli (accessed on 26 May 2021).
- Smith, J.; White, T.; Dodge, C.; Paradiso, J.; Gershenfeld, N.; Allport, D. Electric field sensing for graphical interfaces. IEEE Comput. Graph. Appl. 1998, 18, 54–60. [Google Scholar] [CrossRef]
- Adib, F.; Katabi, D. See through walls with WiFi! In Proceedings of the ACM SIGCOMM 2013 Conference, Hong Kong, China, 12–16 August 2013; pp. 75–86. [Google Scholar]
- Adib, F.; Kabelac, Z.; Katabi, D.; Miller, R.C. 3d tracking via body radio reflections. In Proceedings of the 11th USENIX Symposium on Networked Systems Design and Implementation (NSDI 14), Seattle, WA, USA, 2–4 April 2014. [Google Scholar]
- Adib, F.; Hsu, C.Y.; Mao, H.; Katabi, D.; Durand, F. Capturing the human figure through a wall. ACM Trans. Graph. 2015, 6, 1–3. [Google Scholar] [CrossRef]
- Ye, M.; Wang, X.; Yang, R.; Ren, L.; Pollefeys, M. Accurate 3d pose estimation from a single depth image. In Proceedings of the 2011 International Conference on Computer Vision, Barcelona, Spain, 6–13 November 2011; pp. 731–738. [Google Scholar]
- Peterson, L.E. K-nearest neighbor. Scholarpedia 2009, 2, 1883. [Google Scholar] [CrossRef]
- Muja, M.; Lowe, D.G. Fast approximate nearest neighbors with automatic algorithm configuration. VISAPP 2009, 2, 331–340. [Google Scholar]
- Wilson, A.D.; Bobick, A.F. Parametric hidden markov models for gesture recognition. IEEE Trans. Pattern Anal. Mach. Intell. 1999, 9, 884–900. [Google Scholar] [CrossRef]
- Wilson, A.D.; Bobick, A.F. Hidden Markov models for modeling and recognizing gesture under variation. Int. J. Pattern Recognit. Artif. Intell. 2001, 1, 123–160. [Google Scholar] [CrossRef]
- Hearst, M.A.; Dumais, S.T.; Osuna, E.; Platt, J.; Scholkopf, B. Support vector machines. IEEE Intell. Syst. Their Appl. 1998, 4, 18–28. [Google Scholar] [CrossRef]
- Patsadu, O.; Nukoolkit, C.; Watanapa, B. Human gesture recognition using Kinect camera. In Proceedings of the 2012 International Conference on Computer Science and Software Engineering (JCSSE), Bangkok, Thailand, 30 May–1 June 2012; pp. 28–32. [Google Scholar]
- Feng, K.P.; Yuan, F. Static hand gesture recognition based on HOG characters and support vector machines. In Proceedings of the 2nd International Symposium on Instrumentation and Measurement, Sensor Network and Automation (IMSNA), Toronto, ON, Canada, 23–24 December 2013; pp. 936–938. [Google Scholar]
- Ghimire, D.; Lee, J. Geometric feature-based facial expression recognition in image sequences using multi-class adaboost and support vector machines. Sensors 2013, 6, 7714–7734. [Google Scholar] [CrossRef] [PubMed]
- Haykin, S. Neural Networks and Learning Machines; Prentice Hall: New York, NY, USA, 2009. [Google Scholar]
- Maung, T.H. Real-time hand tracking and gesture recognition system using neural networks. World Acad. Sci. Eng. Technol. 2009, 50, 466–470. [Google Scholar]
- D’Orazio, T.; Attolico, G.; Cicirelli, G.; Guaragnella, C. A Neural Network Approach for Human Gesture Recognition with a Kinect Sensor. In Proceedings of the ICPRAM, Anger, France, 6–8 March 2014. [Google Scholar]
- Hinton, G.; LeCun, Y.; Bengio, Y. Deep learning. Nature 2015, 7553, 436–444. [Google Scholar]
- Cao, Z.; Hidalgo, G.; Simon, T.; Wei, S.E.; Sheikh, Y. OpenPose: Realtime multi-person 2D pose estimation using Part Affinity Fields. IEEE Trans. Pattern Anal. Mach. Intell. 2019, 43, 172–186. [Google Scholar] [CrossRef]
- Sowards, S.W. What is Peer Review, and Does it Have a Future? Bibl. Forsch. Prax. 2015, 39, 200–205. [Google Scholar] [CrossRef]
- AAL Forum—Ageing Well in the Digital World. Available online: http://www.aal-europe.eu/aal-forum/ (accessed on 7 April 2021).
- Hayden, E.C. How to beat HIV. Nat. News 2015, 7559, 146. [Google Scholar] [CrossRef] [PubMed]
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).