Abstract
Eyebrow elevation and reshaping are common concerns that we handle in everyday practice, and we have noticed that the trend is shifting from a medical concern to a cosmetic one. Several eyebrow lift methods are available, both invasive and non-surgical. The method of choice depends on several factors, such as patient expectations and beliefs, financial budget, acceptance of downtime and the available tools in the practice. In this article, we review the recent literature on non-surgical eyebrow lift methods to provide an overview of the current state of this field. We discuss seven different methods for eyebrow lift and reshaping, including botulinum toxin, dermal fillers, fractional radiofrequency, high-intensity focused ultrasound, thermo-mechanical ablation, lasers, and threads. Moreover, we provide practical insight into the procedure, injection techniques, expected results, and patient satisfaction rate.
1. Introduction
The brow region is one of the major aesthetic features visible on the face and plays a significant role in facial and mood expressions. The brow is a complex and dynamic structure influenced by an individual’s gender and age. The male brow is broader and heavier than the female brow and lies over the superior orbital rim with little arch on a horizontal plane, whereas the female brow begins medially at or below the rim and ascends laterally with an arch, peaking in the lateral third as it tapers laterally.
Aging causes a decrease in bone, fat, collagen, and muscle volume in the supraorbital compartment, giving the face a sunken aspect. Furthermore, textural inconsistencies and a loss in tissue quality and elasticity reduce the superior orbital rim’s scaffolding ability, resulting in downward sagging of the brow, which not only gives an individual a fatigued, sad, or sunken appearance but may also impede vision. The lateral brow segment is more vulnerable because it receives less support from deeper structures than the medial brow. Although both men’s and women’s brows can descend with age, men’s brows are usually more resistant to such descent until they are 50 or older. However, current research indicates that the influence of aging on brow position is a complex process [1].
Moreover, temporary eyebrow shaping has become more frequent and is under higher demand among the younger population due to fast-evolving and changing beauty standards [2]. The ideal aesthetic look of the brows varies by gender, with women preferring higher and more arched brows than men. Patients frequently contemplate brow lifting to correct extra skin; however, this procedure requires a major and sometimes expensive surgical procedure, with significant downtime and possible consequences such as deformity or scarring. As a result, non-surgical and minimally invasive rejuvenation procedures have grown in popularity over the last decade, with benefits such as reduced downtime, a higher cosmetic return, and a lower risk of side effects. This article provides a brief overview of recent publications on non-surgical brow lifting and reshaping procedures, and our feedback and practical experience on best practices in this field.
1.1. The Ideal Eyebrow Shapes
Eyebrow shapes have changed over the years, with different eras and cultures favoring different looks [3,4,5,6,7]. In recent years, there has been a trend towards more natural-looking eyebrows, as opposed to the heavily arched brows that were popular in the 1990s [8,9,10]. There are differences in gender and ethnicity in the upper face features, including the eyebrow shape and elevation [11,12,13].
In the era of the metaphase, social media influencers and make-up artists significantly influence the norms and definitions of physical beauty and ideal facial features, including eyebrow shape and height [14,15,16].
The influence of make-up artists started decades earlier, as Westmore contributed to modern notions of the perfect female brow in the 1970s [17]. Most of the debates were on the position of the eyebrow apex (EA) between the lateral limbus (LL) and lateral canthus (LC), as reviewed in 2014 [18] and 2021 [19]. The individual’s age determines the attractiveness of the female eyebrow shape and position. The 2007 statistics indicated that the desire for a certain eyebrow shape varied with age. Young participants up to 30 years old favored lowered and rejected arched eyebrows. Respondents older than 50 had the opposite preference [20].
The position of the eyebrow apex is the main factor that affects the shape of the eyebrow, as shown in Figure 1. Regardless of the position of the EA, there is a consensus on the height of the eyebrow. The ideal height is 2.5 cm between the mid-pupil and the top edge of the eyebrow and 5 cm from the upper edge of the eyebrow to the female hairline [21].
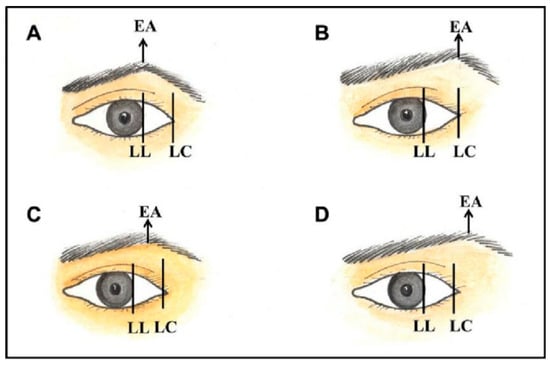
Figure 1.
Different eyebrow apex positions: (A) above the lateral limbus, (B) halfway between the lateral limbus and lateral canthus, (C) above the lateral canthus, and (D) later almost brow. EA, the apex of the eyebrow; LC, lateral canthus; LL, lateral limbus [22].
1.2. Ethnicity and Gender
Beauty is a cultural concept. Historically, beauty standards have had a strong connection with cultural and ethnic backgrounds. Globalization has diminished the cultural differences between different nations and ethnic groups in the last two decades, including beauty standards. However, there are still distinctive facial and anatomical features. For example, the Chinese actress Fan Bingbing is considered the epitome of female beauty. She has childlike facial features; a round face; thin, rather straight eyebrows; comparatively large eyes with a lower eyelid roll; an oval face with a round and narrow chin; and sexually dimorphic traits, such as full, prominent lips. In contrast, the Western ideal of feminine beauty, Angelina Jolie, has prominent cheeks and jawline, submalar hollowing, and full lips, as shown in Figure 2 [4].

Figure 2.
Images of Fan Bingbing (left) and Angelina Jolie (right) [4].
Asians, including those with Fitzpatrick skin phototypes III and above, show fewer age-related rhytids than Caucasians. This has been attributed to a thicker dermis, increased fat above and deep within the superficial muscular aponeurotic system, and dense fat and fibrous connections between the superficial muscular aponeurotic system and deep parotid masseteric fascia, based on anecdotal evidence from cadaver dissections [23].
Some muscles, such as the corrugator supercilii, have a lesser mass in Asians than Caucasians; the corrugator supercilii are also often shorter, thinner, and less hyperdynamic. Variations in the frequency of certain facial expressions, such as frowning, are believed to provide a genetic and cultural foundation for these distinctions [24]. In contrast, Asians have masseter muscles that are typically more developed than most Caucasians [25,26].
In an interesting study, photographs were taken of the faces of two Asian women and two Caucasian women of varying ages. The images of each model were altered to generate different eyebrow shapes. Subsequently, the author recruited and gathered demographic information from volunteers from the general public to evaluate the altered photographs according to their aesthetic preferences. The authors found that neither the ethnicity of the models nor the ethnicity of the volunteers who judged them significantly influenced the optimal location of the eyebrow arch. However, a more medial brow apex is generally preferred in older faces, whereas a more lateral brow apex is preferred in younger faces [27].
Nevertheless, Asian brows feature a slightly straighter bow than Caucasians’ angular arch, and their brow lines are gentler [4,28]. Asian faces with highly arched brows might appear particularly artificial, due in part to their relatively wider width. The optimal brow shape for Asian women is flatter and lower in the lateral two thirds than Caucasians, historically. Asians avoid the lateral arching of the brow, often known as the “Samurai eyebrow,” which is regarded as a less desirable “angry look” [29].
Other cultures might have different beauty standards, including, but not limited to, eyebrow shape and elevation [6,12,30].
Gender has always played an important role in beauty standards and natural eyebrows [31,32]. Caucasian females of all age groups have much higher eyebrows than their male counterparts. In a study with younger and middle-aged cohorts, African American females had a considerably higher eyebrow height than males. In nearly all Caucasian and Afro-American males, the distance between the brow apex and the lateral corneal limbus was higher than in females. In contrast, women had a larger brow apex angle than men [33].
1.3. Forehead Anatomy
An eight-layer configuration has been identified in the forehead, as shown in Figure 3. These layers, from superficial to deep, are as follows:
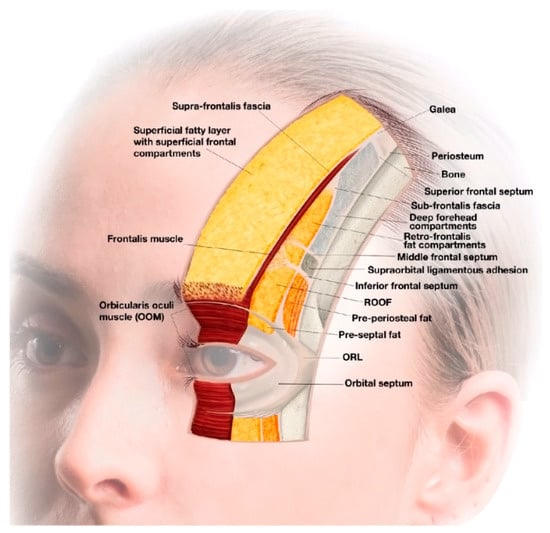
Figure 3.
The eight-layer forehead configuration system. The fascial layers are exposed in a progressive fashion, beginning at the skin (medially) and progressing deeper till they reach the bone (laterally, temporal crest). The hue of the neighboring fat can also be used to determine the depth of each structure. The superficial fatty layer is the lightest (yellow), the retrofrontalis fat is slightly darker (bright orange), and the preperiosteal fat is the darkest (dark orange). Note how the orbicularis retaining ligament and the supraorbital ligamentous adhesion transition into more superficial layers and provide boundaries for cranial and caudal compartments [34].
- Layer 1: skin;
- Layer 2: superficial fatty layer;
- Layer 3: suprafrontalis fascia;
- Layer 4: orbicularis oculi and frontalis muscle (same plane);
- Layer 5: a homogenous layer of fat (preseptal fat (in the upper eyelid), retro-orbicularis oculi fat (deep to the orbicularis oculi muscle), and retrofrontalis fat (deep in the occipitofrontalis muscle));
- Layer 6: subfrontalis fascia;
- Layer 7: preperiosteal fat within the prefrontal space in the lower forehead and deep compartments in the upper forehead;
- Layer 8: periosteum bone.
The depth of different layers, obtained using ultrasound imaging, is shown in Figure 4.
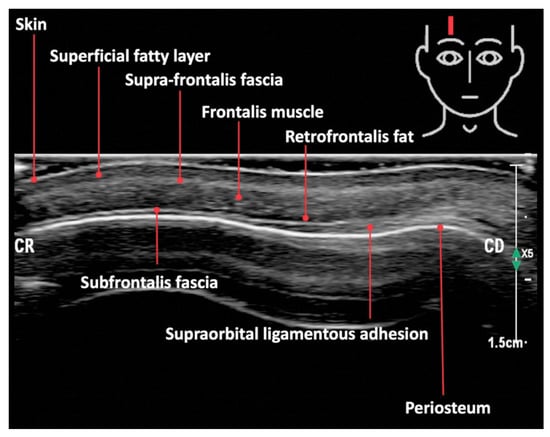
Figure 4.
Ultrasound image depicting the layered forehead anatomy in a 45-year-old female Caucasian patient [34].
1.4. Changes in Eyebrow Shape and Elevation with Age
There is growing evidence in the literature that paradoxical medial brow elevation with age may be seen in a subset of individuals [35,36,37]. A recent photographic study of brow position and shape changes with aging, undertaken by comparing cohorts of women aged 20 to 30 years with an elderly cohort of women aged 50 to 60, indicated the elevation of the medial and central brows compared to the lateral brow, as shown in Figure 5. One potential explanation for this observation is the persistent activation of the occipitofrontalis muscle in situations of visually significant dermatochalasis or ptosis to widen the superior visual field. Again, the results of this muscular-driven elevation would be most visible medial to the temporal fusion line of the skull, perhaps leading to lateral ptosis [1,35,38,39,40].

Figure 5.
The difference in the tilt of the brow changes from apex lateral (left) to apex neutral (right). Typical outcomes for patients aged 20 to 30 (left) and 50 to 60 (right) are displayed. Younger individuals have a low medial brow with an apex lateral configuration. Older individuals’ higher medial and middle brows lead to a flattened look. For each position measured, measurements to the top of the brow edge are shown [35].
1.5. The Need for Non-Surgical Eyebrow Lifting
A 2019 systematic review and meta-analysis showed that while the eyebrow height at the LC remains constant, the medial eyebrow position becomes higher as we age [40]. Moreover, some medical conditions may significantly change the eyebrow shape and position [41]. Non-surgical eyebrow lift treatments have been developed to meet the demand brought on by the rapid evolution of the aesthetics industry and the proliferation of non-surgical techniques.
2. Non-Surgical Eyebrow Lift Treatments
2.1. Botulinum Toxin
Although there is no direct attachment of the brow to the underlying bone, it is sensitive to the interaction of the numerous periorbital muscles, which, when functioning together, allow key nonverbal cues to be delivered. Understanding the balance and interplay of these muscles is critical when using neuromodulators to target the periorbital area. The 3D movement of the brows is controlled by four muscles, as shown in Table 1.

Table 1.
An overview of the three axes of eyebrow movement and the function of each periorbital muscle.
Botulinum toxin (BTX) is the most common non-surgical eyebrow lift treatment [42,43,44]. Frankel and Kamer were the first to investigate this indication and referred to it as a chemical browlift [45]. They noticed that their patients experienced eyebrow lifts after receiving BTX injections in the glabellar and crow’s feet areas. They concluded that the botulinum toxin allows the occipitofrontalis muscles to act without resistance from the depressor supercilii muscles (orbital orbicularis oculi, procerus, corrugator superciliis, and depressor supercilii) to provide a lateral eyebrow lift. However, no treatment protocol was proposed. Following this, various protocols with varying degrees of simplicity and injection points have been proposed, as shown in Figure 6, Figure 7, Figure 8 and Figure 9 [46,47,48,49,50,51]. A recent review summarized the different techniques using BTX for brow elevation and shaping [52]. In addition to the traditional hypodermic needle for BTX delivery, recent research has suggested microbotox, which combines topical delivery with increased skin permeability via thermal injury [53]. The location and the depths of the BTX injection should be relative to the muscles’ function and placement in individuals, as shown in Figure 10, Figure 11 and Figure 12.
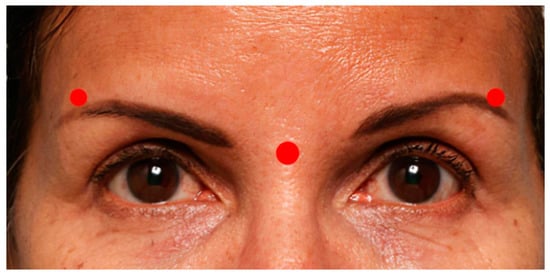
Figure 6.
The red dots approximate the placement of botulinum toxin injections [49].

Figure 7.
The red dots approximate the placement of botulinum toxin injections [52].
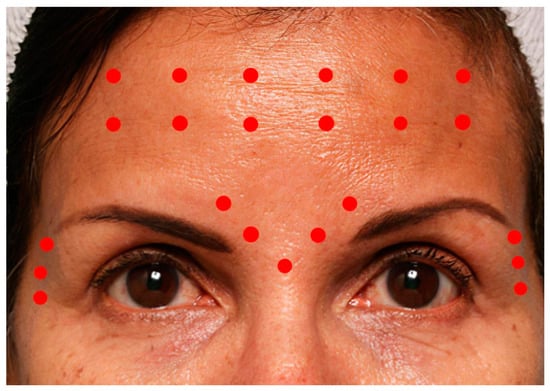
Figure 8.
The red dots approximate the placement of botulinum toxin injections [46].
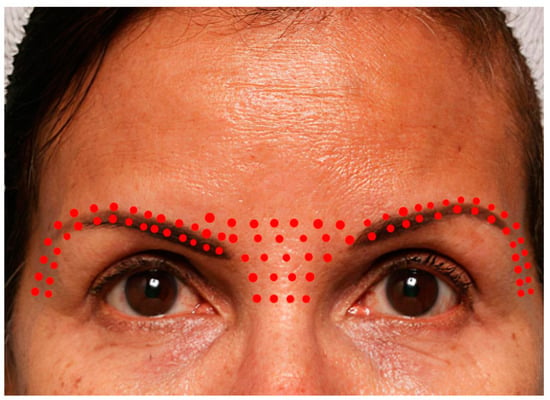
Figure 9.
The red dots approximate the placement of botulinum toxin injections for the microdroplet lift [54].
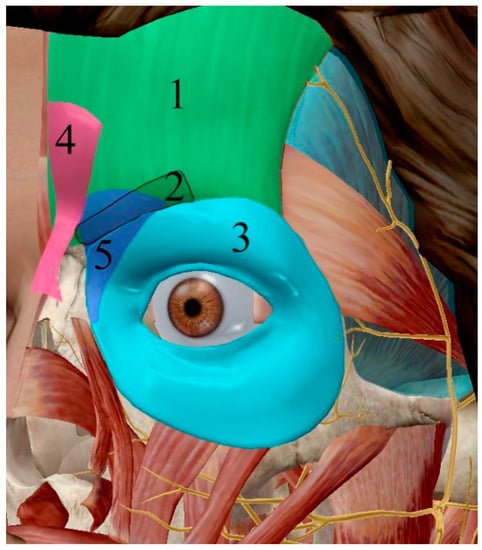
Figure 10.
Illustration of (1) frontalis muscles, (2) corrugator supercilia, (3) lateral part of the orbital orbicularis oculi, (4) procerus, and (5) depressor supercilii from a frontal and 45-degree position.
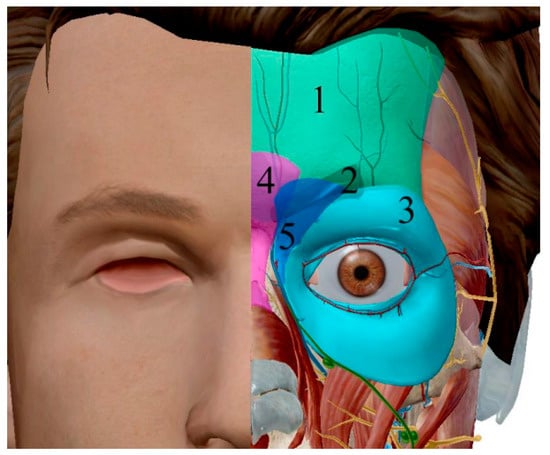
Figure 11.
Illustration of (1) frontalis muscles, (2) corrugator supercilia, (3) lateral part of the orbital orbicularis oculi, (4) procerus, and (5) depressor supercilii from a frontal and 45-degree position.

Figure 12.
Five glabellar complex sites; eight crow’s feet line sites are injected (four on each side). Note that the various symbols used here represent different injection depths: squares indicate full-needle depth, Xs indicate one-half needle depth, and asterisks indicate one-third needle depth [55].
The depressor supercilii is superficial and lowers the eyebrow. Therefore, the BTX injection should be shallow (approximately one third of the needle).
The procerus draws down the eyebrow and is positioned under the depressor supercilii. Therefore, the BTX injection should be of medium depth (around one half of the needle). The corrugator supercilii draws the eyebrow downwards and medially and is positioned under a group of muscles. Therefore, the BTX injection should be deep (approximately the whole needle length), as shown in Figure 12.
The lateral part of the orbital orbicularis oculi is superficial and draws the eyebrow downwards and medially. Therefore, the BTX injection should be shallow (approximately one third of the needle).
The eyebrows are a relatively inaccurate cutaneous landmark, particularly in females, due to their inclination to alter eyebrow shapes, such as tweezing or plucking. The treatment technique should be determined by the subject’s muscle mass, muscle shape, muscle activity pattern, and what is cosmetically acceptable in the context of the entire facial structure. Examining the overlaying soft tissues, such as fat and skin, is a useful adjuvant. Dosages are adjusted based on muscle activity and mass, while injection site placement is influenced by muscle shape [29]. Practitioners should individualize the number of BTX units for each patient; for example, Asian people may need a lower BTX amount compared to Caucasian ones [25].
Because the substance metabolizes within 3–4 months, major long-term effects of BTX therapy are uncommon [56]. As a result, small problems are more likely and might be troublesome in the short term. Botulinum toxin difficulties fall into three categories: (1) injection-related complications, (2) complications inherent to the toxin’s pharmacologic qualities, and (3) the practitioner’s injection method in particular anatomical regions. Pain, swelling, bruising, a heavy feeling, and headache are common injection-related consequences. However, practitioners may consider applying particular approaches to alleviate these issues [57,58,59].
2.2. Dermal Fillers
In addition to BTX injections, there is also the dermal filler approach. Fillers are often utilized with BTX or when BTX fails to raise the eyebrows sufficiently [60]. In addition to the eyebrow lift, fillers may increase the volume and shape of the eyebrows. The most common filler base is hyaluronic acid (HA). An upper-face-focused facial assessment and injection guide for BTX and HA fillers was published in 2017 [55]. The guide demonstrated a consensus for BTX injection positioning and low- and high-density HA filler density to enhance and elevate brows, and it was adapted in 2019 [61]. HA fillers are not the only ones reported for this purpose, as calcium hydroxylapatite fillers have also been used for the cosmetic enhancement of the brow [62,63].
There are three main factors to consider when injecting HA filler for eyebrow reshaping and elevation:
- The entry points;
- The depth and extension;
- Injection techniques.
2.2.1. The Entry Points
Determining the entry point is critical to minimize the risk of bruising and other vascular adverse events. Furthermore, when using a cannula, a well-planned entry point may make the treatment more comfortable by reducing the number of entry points. The recommended entry points are shown as green circles in Figure 13.
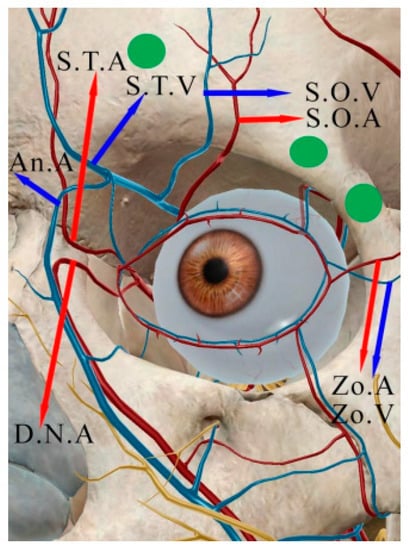
Figure 13.
The typical branching pattern of the supraorbital artery and vein (S.O.A. and S.O.V.), the supratrochlear artery and vein (S.T.A. and S.T.V.), the dorsal nasal artery (D.N.A.), the angular vein (An.V.), and the zygomaticoorbital artery and vein (Zo.A. and Zo.V.), as well as the cannula entrance positions (green circles).
The ocular arteries are blood vessels in the circulatory system that supply oxygenated blood to the eyes. They arise from the internal carotid artery and pass into the orbit, or eye socket, through the orbital canal. The branches of the ophthalmic artery supply the orbit, the muscles, and the bulb of the eye, including the sclera, retina, and choroid. There 11 branches of the ophthalmic artery, including the
- Supratrochlear artery (A. supratrochelaris—S.T.A.);
- Supraorbital artery (A. supraorbitalis—S.O.A.).
The other two major arteries in the periorbital areas are an external carotid artery branch:
- Zygomaticoorbital artery (A. zygomaticoorbitalis—Zo.A.);
- Dorsal nasal artery (A. dorsalis nasi—D.N.A.).
We recommend one of three entry points to avoid filler injections in the supraorbital artery and supratrochlear artery:
- On the zygomaticofrontal suture to elevate the area lateral to the LC line;
- Lateral to the zygomaticofrontal suture, to elevate the area between the LL and LC lines;
- Medial to the mid-pupillary line to elevate the area medial to the LL lines.
2.2.2. The Depth and Extension of the Injections
There have been several recommendations about filler injection depth. It also has been demonstrated that placing the fillers at the pre-periosteal plane requires a smaller volume of filler and is associated with reproducible results. Others suggest injecting into the subcutaneous plane rather than the sub-orbicularis and subcutaneous fat.
We recommend injecting into the retro-orbicularis oculi fat (ROOF) pad as it has suitable depth, thickness, and dimensions for filler implementation. The ROOF fat compartment is approximately 1.2 cm in depth, with a mean thickness of 1.40 ± 0.2/1.30 ± 0.2 mm (mid-pupillary/lateral canthus), respectively. The mean length of this fat compartment (i.e., the distance between the orbicularis retaining ligament and the supraorbital ligamentous adhesion) is 13.68 ± 0.8/13.64 ± 0.9 mm, respectively, as shown in Table 2 [34].

Table 2.
ROOF distances and thicknesses using ultrasound.
2.2.3. The Injection Technique
The periorbital area is heavily vascularized. Therefore, soft tissue necrosis and visual impairment are examples of ischemic problems associated with filler injections that should be mentioned to patients undergoing filler injections [64]. The incidence of vascular occlusion with face HA injections may be slightly lower at 3-9/10,000 injections [65,66,67]. The glabellae and nasal region are the most at risk, although they can occur everywhere in which an artery runs, including the lip, nasolabial fold, and temple.
There are precautions that can be taken to avoid accidental intra-arterial product injection. However, no strategy is 100% efficient in preventing ischemic consequences. Utilizing local anesthetics with epinephrine to vasoconstrict arteries before injection, injecting tiny quantities at each pass, aspiration before injection, using a low injection pressure, avoiding scarred regions, and contemplating using blunt cannulas are some strategies that might be effective. Blunt cannulas, on the other hand, can reduce the risk but may behave similarly to needles, especially when used in scarred areas, where vessels are more prone to being tethered [68]. Hyaluronidase injection into the vitreous cavity has been used in the past safely. Table 3 provides practitioners with some valuable tips to reduce the risk of ischemic events.

Table 3.
Injection techniques to help avoid ischemic complications.
We highly recommend using a blunt cannula to minimize the risk of bruising and vascular occlusion [69]. We also recommend a multi-level technique with several retrograde linear paths. The filler should be first injected into the ROOF and then could be augmented by a deeper layer at the pre-periosteal plane. The volume of the filler depends on the expected results. Each eyebrow should receive a modest aliquot (0.2–0.5 mL) of filler until the clinical impact is obvious.
A combination of BTX and dermal fillers is common to achieve stronger eyebrow-lifting results, as shown in Figure 14.
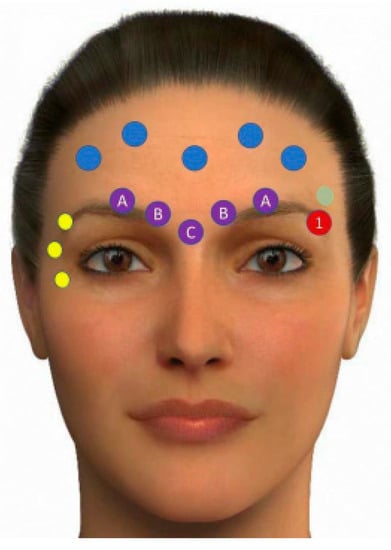
Figure 14.
Different upper-face treatment points. The yellow circles show botulinum toxin A therapy for crow’s feet lines. Blue circles represent BTX therapy for forehead lines. The purple circles represent the treatment locations for glabellar lines with botulinum toxin A. The red circle denotes spot (1) for implanting low-density hyaluronic acid to raise the brow’s tail. The green circle represents the temporal area, which will be treated with a high-density hyaluronic acid implant (T1). A denotes one third of the needle depth to target depressor supercilii. B denotes full needle depth to target the corrugator supercilii. C represents one-half needle depth to target the procerus [61].
Practitioners who use the “pinch and pull” procedure should understand the anatomical changes associated with this technique [70,71]. The “pinch and pull” technique separates the surface mobile tissue layers from the deeper layers [72]. Because the blood arteries in the top two thirds of the forehead are being dragged up using a “pinch and pull” approach, injecting the filler at a deeper layer would be much safer. Because the blood vessels in the lower one third of the forehead and brow region, namely the SO artery and ST artery, are not pulled up with the “pinch and pull” maneuver, injecting the filler at a deeper layer in the lower third would be dangerous, and a superficial filler injection plane is preferred, particularly in the brow region, as shown in Figure 15, Figure 16 and Figure 17 [73].
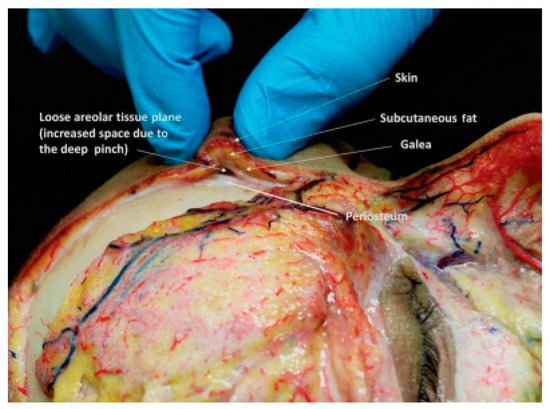
Figure 15.
The cadaver dissection demonstrates the “pinch anatomy” of the forehead, with the superficial mobile layers sliding across the periosteum to bunch up, allowing greater room for a needle bevel during filler injection in the loose areolar tissue layer [73].
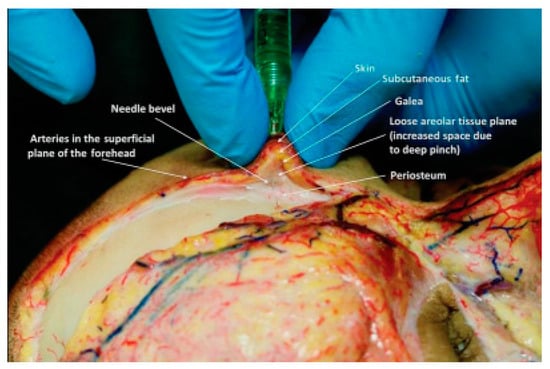
Figure 16.
During filler injection, the cadaver dissection shows “pinch anatomy” of the forehead during a deep pinch, generating additional space so that the needle’s whole bevel is evident in the comparatively avascular, loose areolar tissue layer [73].
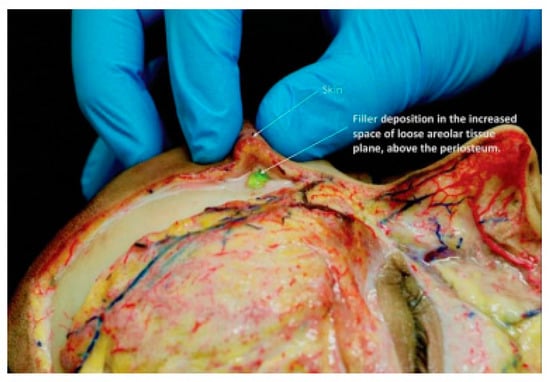
Figure 17.
The forehead cadaver dissection and filler material’s position (green color) in the relatively avascular, loose areolar tissue layer [73].
2.3. Fractional Radiofrequency and Radiofrequencyfractional Microneedling
As recently reviewed, radiofrequency (RF) devices produce controlled heating to encourage tissue regeneration and tightness [74]. The proof of concept for the use of volumetric heating by radiofrequency (RF) was performed in 2004 [75]. Since then, the technology has evolved into bipolar, fractional delivery for RF [74]. The ideal temperature for constant collagen, elastin, and hyaluronic acid production in the reticular dermis is 67 degrees Celsius, sustained for three seconds [76].
In addition to the traditional method of performing RF microneedling, a study found that if both the reticular dermis and the mimetic muscles were treated with microneedle penetration and fractional RF radiation, more benefits could be realized. The muscle and skin are closely connected and move as a unit in the lower eyelid, crow’s feet, upper lip, and commissure, making the intramuscular administration of RF energy possible [77].
A 2021 case reported the results of using a bipolar RF fractional microneedling device to achieve a non-surgical brow lift on two patients; the patients exhibited between 2 and 2.5 mm of brow elevation at their follow-up appointments [78].
2.4. High-Intensity Focused Ultrasound (HIFU)
The Food and Drug Administration (FDA) approved the high-intensity focused ultrasound (HIFU) brow-lifting technique in 2009 [79]. Acoustic energy creates heat in the range of 60 °C to 70 °C, targeting the deep dermis and superficial musculoaponeurotic system (SMAS), causing collagen denouement, new collagen synthesis, skin tightness, and elevation. The thicknesses of the facial skin layers vary somewhat anatomically; hence, the depths of the targeted therapy layers must be modified correspondingly [80]. Multiple studies have shown significant improvements in facial ptosis, specifically of the brows, nasolabial folds, mandibular angle, and platysma, after HIFU treatment. Histologic examination revealed increased collagen regeneration following treatment [80,81,82,83]. One study reported an elevation of the eyebrow by 1.7 mm after 90 days of treatment [79].
Moreover, a multimodal approach combined botulinum toxin, fillers, and micro-focused ultrasound to rejuvenate the periocular region. First, the supra-brow, lateral canthus, and infraorbital areas were treated with micro-focused ultrasound MFU. The filler was injected into the sunken upper eyelid, lateral brow, and infraorbital region. Finally, on the same day, botulinum toxin was injected into the forehead, glabella, crow’s feet, and lateral orbital margin behind the brow [84].
In a pilot study, a hybrid device that combined HIFU and fractional RF technology was effective in facial and neck rejuvenation, including eyebrow lifting [85]. The efficacy of the hybrid device was not compared with the efficacy of standalone HIFU or fractional RF devices.
2.5. Thermo-Mechanical Ablation
Thermo-mechanical ablation technology has been used for medical and, more recently, cosmetic purposes. The FDA cleared the technology in 2021, and it is intended for dermatological procedures that require skin ablation and resurfacing [86].
For correcting peri-orbital wrinkles, the efficacy of this technology was comparable to that of fractional laser [87,88]. The most successful application of this technology is to increase skin permeability and enhance the local delivery of topical medication, as discussed in the microbotox [89].
2.6. Lasers
Laser therapy is one of the most popular options for skin rejuvenation [90,91,92]. It can target various concerns, including wrinkles, fine lines, age spots and more—including laser therapy through ablation, coagulation, or a combination of them [93,94,95]. Histochemical research revealed that the eyelids have greater levels of collagen 30 days after a single CO2 treatment [96]. However, ablative (such as CO2 and Er:YAG) and non-ablative fiberglass fractional lasers are primarily used for upper eyelid dermatochalasis and periorbital rejuvenation rather than brow elevation [88,97,98,99]. A recent case report discussed an eyebrow lift using Er:YAG in smooth mode, which relies merely on the coagulation effect of the laser [100].
2.7. Thread Lifting
Eyebrow thread lifting is a minimally invasive technique that may correct mild-to-moderate ptosis while providing good cosmetic outcomes. In the absence of ptosis, thread lifting is an excellent option for repositioning the brow and improving the gaze [101]. Threads provide actual mechanical suspension, which is a significant advantage over previous methods of eyebrow elevation [102]. The first report on using threads in a cosmetic suture suspension procedure was in 1993 [103]. Since then, threads have significantly improved in material, shape, and procedure [104].
Threads are characterized by their composition, shape, thickness, and implementation methods. Currently, most of the commonly used threads are either absorbable (polylactic acid, caprolactone threads, polydioxanone) or semi-absorbable (polypropylene-polylactic acid) threads [105,106,107].
In terms of shape, threads are classified into mono, spring, twin, uni-direction cogged, bi-direction cogged, and multi-direction cogged threads. Each of these threads has a unique indication and implementation process. Cogged (barbed) threads are primarily used in the brow lift procedure. Moreover, barbs can be substituted with cones in bi-directional threads, such as Silhouette Soft.
Threads are loaded on a sharp needle, into a cannula, or attached to a single or double needle, which determines the implementation procedure [108,109,110]. The UPS system commonly denotes the size to number their thickness relative to their diameter. The numbering system revolves around the “0” suture, and the number preceding the “-0” denotes the number of zeros in the UPS size [111,112]. The strand’s diameter decreases as the number of zeros in the suture size increases. Suture size thus increases from USP 0 to 1.2 and upwards, while it decreases from 0 to 2-0 (00), 3-0 (000), and downwards [113]. Moreover, the manufacturing of cogged threads has recently improved from laser cutting to pressing and molding, enhancing the thread resistance [114].
One of the most common techniques uses cogged threads loaded into the cannula to raise the eyebrows by inserting two to four cogged threads at the insertion point (A), 1 cm below the hairline, for a medial and lateral brow lift, as shown in Figure 18. To avoid trauma to the temporal branch of the facial nerve, one should insert the first cog thread through the sub-dermis and end at point B, 1 cm above the brow. After anchoring the cog thread, one can then slowly retract the cannula and clamp the cog thread. Then, one should sub-dermally insert the second cog thread towards end-point C, 1 cm above the brow and parallel to the lateral canthus line, and then clamp together both cog threads and trim them close to the skin [115].
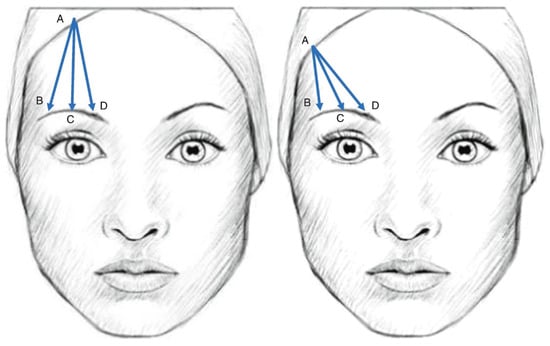
Figure 18.
The use of unidirectional cogged threads for eyebrow central elevation (left) and lateral elevation (right). (A) de-note the entry point and (B–D) denote the anchoring points. Reprinted with permission from Ref. [116].
The two most common techniques for eyebrow elevation when using bi-directional threads attached to two needles are the L-shape and U-shape techniques, as shown in Figure 19. The U shape provides more lifting along the medial line, while the L shape enhances the lateral elevation [116]. Other less common insertion models are the N-shape and O-shape techniques, as shown in Figure 20 [117].
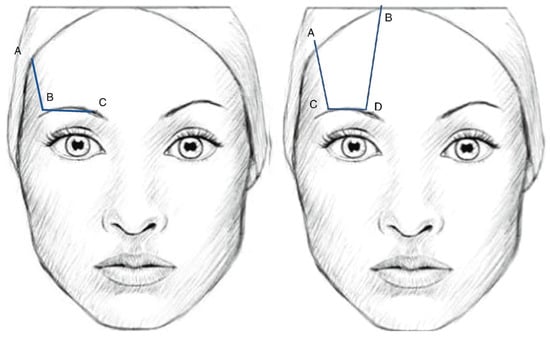
Figure 19.
The use two-needle thread in L Shape (left) and U shape (right). For the L shape, (A) denote the entry point, (B) the anchoring point and (C) the exit point. For the U shape, (A,B) denote the entry and exit point respectively. (C,D) denote the anchoring points. Reprinted with permission from Ref. [116].
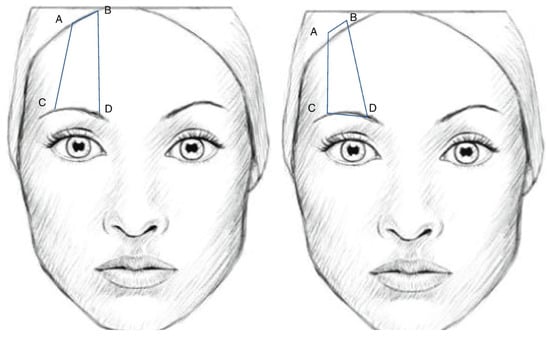
Figure 20.
The use two-needle thread in N Shape (left) and O shape (right). For the N shape, (C,D) denote the entry and exit point respectively. (A,B) denote the anchoring points. For the (O) shape, (D) denotes both the entry and exit point. (A–C) denote the anchoring points. Reprinted with permission from Ref. [116].
3. Opinion
BTX injections are the most popular and least expensive non-surgical brow lifting technique. The procedure is relatively simple, and there is plenty of educational material to support its use. However, new practitioners should avoid injecting BTX to elevate and reshape the brow until they have mastered the necessary hand skills and injection techniques. Most patients have considered the procedure affordable and effective in the last three months. Dermal fillers can significantly improve the outcomes of BTX injections. Injecting fillers in the brow and periorbital area, on the other hand, requires advanced training to avoid occlusion. We strongly advise using a blunt cannula rather than a sharp hypodermic needle. Practitioners should satisfy a 10-point planning system to improve the safety of filler injection procedures [71]. The 10 points include the following:
- Patient history and selection;
- Patient assessment;
- Patient informed consent;
- Filler reversibility;
- Product characteristics;
- Product layering;
- Before and after photography;
- Procedural planning and aseptic technique;
- Injection anatomy;
- Technical knowledge.
The use of threads for brow lifting has grown in popularity in recent years. While the procedure is more invasive than the injection of BTX and fillers, the results are more impressive and last longer. It is simpler to use barbed threads loaded on a cannula than bi-directional threads equipped with two needles.
Except for HIFU technology, there is a lack of strong evidence in favor of using energy-based machines for brow lifting. Although some studies found statistically significant differences in eyebrow elevation, patient satisfaction remained low. Patients are required to receive multiple treatments, which can be costly and time-consuming. Furthermore, these methods are costly and necessitate practitioners’ purchase of expensive machines.
Author Contributions
Conceptualization, D.O., A.A., S.T. and K.A; methodology, not applicable; software, not applicable; validation, A.A. and S.T.; formal analysis, D.O. and K.A; investigation, D.O. and K.A.; resources, K.A.; data curation, D.O., A.A., S.T. and K.A.; Writing—original draft preparation, D.O. and K.A.; writing—review and editing, D.O. and K.A.; visualization, D.O. and K.A.; supervision, K.A.; project administration, D.O. and K.A.; funding acquisition, not applicable. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Conflicts of Interest
The authors declare no conflict of interest.
Abbreviations
BTX: Botulinum toxin, HIFU: High-intensity focused ultrasound, HA: Hyaluronic acid, RF: Radiofrequency, ROOF: Retro-orbicularis oculi fat, S.O.A.: Supraorbital artery, S.O.V.: Supraorbital artery, S.T.A.: Supratrochlear artery, S.T.V.: Supratrochlear vein, D.N.A.: Dorsal nasal artery, An.V.: Angular vein, Zo.A.: Zygomaticoorbital artery, Zo.V.: Zygomaticoorbital artery.
References
- Park, J.; Yun, S.; Son, D. Changes in Eyebrow Position and Movement with Aging. Arch. Plast. Surg. 2017, 44, 65–71. [Google Scholar] [CrossRef] [PubMed]
- Cerrati, E.W.; Thomas, J.R. The Multicultural Evolution of Beauty in Facial Surgery; SciELO Brasil: Sao Paolo, Brasil, 2017; pp. 373–374. [Google Scholar]
- Li, G.; Liu, Z.; Su, L.; Ji, X. (Eds.) Research on 3D facial assessment for facial plastic surgery. In Proceedings of the 4th International Conference on Information Science, Electrical, and Automation Engineering (ISEAE 2022), Guangzhou, China, 25–27 March 2022. [Google Scholar]
- Samizadeh, S. Beauty Standards in Asia. In Non-Surgical Rejuvenation of Asian Faces; Springer: Berlin, Germany, 2022; pp. 21–32. [Google Scholar]
- Miralles, C.; Ragpala, L.; Aliwa, M.; Parohinog, A.; Arciaga, J.; Bandral, K.; Galang, R. Barbie Dolls: People’s Body Standards. Res. J. 2020, 3, 137. [Google Scholar]
- Metlej, J. Fitting in and/or Standing out: Lebanese-Canadian Women’s Experiences of Beauty Culture. Master’s Thesis, Saint Mary’s University, Halifax, NS, Canada, 2022. [Google Scholar]
- Batniji, R.K.; Perkins, S.W. Upper and Midfacial Rejuvenation in the Non-Caucasian Face. Facial Plast. Surg. Clin. N. Am. 2010, 18, 19–33. [Google Scholar] [CrossRef] [PubMed]
- Falk, S. The Made-up Woman: Women’s Daily Use of Makeup in Rome. Bachelor’s Thesis, Uppsala University, Uppsala, Sweden, 2022. [Google Scholar]
- Parker, M. Fundamentals for Cosmetic Practice: Toxins, Fillers, Skin, and Patients; CRC Press: Boca Raton, FL, USA, 2022. [Google Scholar]
- Kashmar, M.; Alsufyani, M.A.; Ghalamkarpour, F.; Chalouhi, M.; Alomer, G.; Ghannam, S.; El Minawi, H.; Saedi, B.; Hunter, N.; Alkobaisi, A.; et al. Consensus Opinions on Facial Beauty and Implications for Aesthetic Treatment in Middle Eastern Women. Plast. Reconstr. Surg.—Glob. Open 2019, 7, e2220. [Google Scholar] [CrossRef]
- de Maio, M. Ethnic and gender considerations in the use of facial injectables: Male patients. Plast. Reconstr. Surg. 2015, 136, 40S–43S. [Google Scholar] [CrossRef]
- Karlin, J.; Farajzadeh, J.; Azhdam, A.; Hirji, S.; Baugh, S.; Esfandiari, M.; Goldberg, R.; Rootman, D. Analysis of eyelid and eyebrow metrics in Iranian American adults. J. Plast. Reconstr. Aesthet. Surg. 2022; in press. [Google Scholar] [CrossRef]
- Jindawattanaphum, S. Travelers, merchants, and foreigners appeared in facial stucco sculptures in Dvaravati humans in Nakhon Pathom Province. Interdiscip. Res. Rev. 2022, 17, 20–24. [Google Scholar]
- Maharani, B.M.; Hawa, B.C.N.; Devita, P.T. The Role of Photo Editing in Instagram Towards the Body Image Among Female Teenagers. Asian J. Media Commun. 2020, 4, 1. [Google Scholar]
- Henriques, M.; Patnaik, D. Social Media and Its Effects on Beauty. In Beauty-Cosmetic Science, Cultural Issues and Creative Developments; IntechOpen: London, UK, 2020. [Google Scholar]
- Jalba, R. If and How are Instagram’s Top Male Makeup Influencers Shifting the Beauty Norms & Beauty Representations in a Female Oriented Industry. Master’s Thesis, Malmö University, Malmö, Sweden, 2018. [Google Scholar]
- Westmore, M. Facial Cosmetics in Conjunction with Surgery. In Proceedings of the Course Presented at the Aesthetic Plastic Surgery Society Meeting, Vancouver, BC, Canada, May 1975. [Google Scholar]
- Yalçınkaya, E.; Cingi, C.; Söken, H.; Ulusoy, S.; Muluk, N.B. Aesthetic analysis of the ideal eyebrow shape and position. Eur. Arch. Oto-Rhino-Laryngol. 2016, 273, 305–310. [Google Scholar] [CrossRef]
- Ding, A. The Ideal Eyebrow: Lessons Learnt from the Literature. Aesthet. Plast. Surg. 2021, 45, 536–543. [Google Scholar] [CrossRef]
- Feser, D.K.; Gründl, M.; Eisenmann-Klein, M.; Prantl, L. Attractiveness of Eyebrow Position and Shape in Females Depends on the Age of the Beholder. Aesthet. Plast. Surg. 2007, 31, 154–160. [Google Scholar] [CrossRef]
- McKinney, P.; Mossie, R.D.; Zukowski, M.L. Criteria for the forehead lift. Aesthet. Plast. Surg. 1991, 15, 141–147. [Google Scholar] [CrossRef] [PubMed]
- Packiriswamy, V.; Kumar, P.; Bashour, M. Photogrammetric Analysis of Eyebrow and Upper Eyelid Dimensions in South Indians and Malaysian South Indians. Aesthet. Surg. J. 2013, 33, 975–982. [Google Scholar] [CrossRef] [PubMed]
- Sykes, J.M. Management of the Aging Face in the Asian Patient. Facial Plast. Surg. Clin. N. Am. 2007, 15, 353–360. [Google Scholar] [CrossRef]
- Yang, H.-M.; Kim, H.-J. Anatomical study of the corrugator supercilii muscle and its clinical implication with botulinum toxin A injection. Surg. Radiol. Anat. 2013, 35, 817–821. [Google Scholar] [CrossRef] [PubMed]
- Tzou, C.; Giovanoli, P.; Ploner, M.; Frey, M. Are there ethnic differences of facial movements between Europeans and Asians? Br. J. Plast. Surg. 2005, 58, 183–195. [Google Scholar] [CrossRef] [PubMed]
- Baohua, P.; Samizadeh, S. Non-Surgical Aesthetics-Injection Strategy of East Asian Faces. In Non-Surgical Rejuvenation of Asian Faces; Springer: Berlin, Germany, 2022; pp. 297–319. [Google Scholar]
- Biller, J.A.; Kim, D.W. A contemporary assessment of facial aesthetic preferences. Arch. Facial Plast. Surg. 2009, 11, 91–97. [Google Scholar] [CrossRef]
- Arzadon, J.A.A.; Santorelli, A.; Braganza, L.J. Eyebrow Reshaping (ER) with DefinisseTM Threads. Int. J. Clin. Ski. 2022, 16, 241. [Google Scholar]
- Sundaram, H.; Huang, P.-H.; Hsu, N.-J.; Huh, C.H.; Wu, W.T.; Wu, Y.; Cassuto, D.; Kerscher, M.J.; Koo-Il Seo, K. Aesthetic applications of botulinum toxin A in Asians: An international, multidisciplinary, pan-Asian consensus. Plast. Reconstr. Surg. Glob. Open 2016, 4, e872. [Google Scholar] [CrossRef]
- Ricarte, F.; Singh, D.; Wong-Putnam, P.; Vickery, S.A. Eye Cosmetics. In Cosmetic Dermatology: Products and Procedures, 3rd ed.; John Wiley & Sons: Hoboken, NJ, USA, 2022; pp. 259–268. [Google Scholar]
- Khellat-Kihel, S.; Muhammad, J.; Sun, Z.; Tistarelli, M. Gender and ethnicity recognition based on visual attention-driven deep architectures. J. Vis. Commun. Image Represent. 2022, 88, 103627. [Google Scholar] [CrossRef]
- Somenek, M.; Romero, N.J. Brow Lift and Brow Position for Gender Affirmation. Otolaryngol. Clin. N. Am. 2022, 55, 797–808. [Google Scholar] [CrossRef]
- Price, K.M.; Gupta, P.K.; Woodward, J.A.; Stinnett, S.S.; Murchison, A.P. Eyebrow and Eyelid Dimensions: An Anthropometric Analysis of African Americans and Caucasians. Plast. Reconstr. Surg. 2009, 124, 615–623. [Google Scholar] [CrossRef] [PubMed]
- Ingallina, F.; Frank, K.; Mardini, S.; Gavril, D.L.; Hernandez, C.A.; Benslimane, F.; Gotkin, R.H.; Davidovic, K.; Moellhoff, N.; Cotofana, S. Reevaluation of the Layered Anatomy of the Forehead: Introducing the Subfrontalis Fascia and the Retrofrontalis Fat Compartments. Plast. Reconstr. Surg. 2022, 149, 587–595. [Google Scholar] [CrossRef] [PubMed]
- Matros, E.; Garcia, J.A.; Yaremchuk, M.J. Changes in Eyebrow Position and Shape with Aging. Plast. Reconstr. Surg. 2009, 124, 1296–1301. [Google Scholar] [CrossRef] [PubMed]
- Panda, A.K.; Nilesh, K.; Patil, M. Cosmetic applications of botulinum toxin in eyebrow lift. In The Application of Botulinum Toxin in Oral and Maxillofacial Surgery; Cambridge Scholars Publishing: Newcastle upon Tyne, UK, 2022; p. 40. [Google Scholar]
- Papageorgiou, K.I.; Mancini, R.; Garneau, M.H.C.; Chang, S.-H.; Jarullazada, I.; King, A.; Forster-Perlini, E.; Hwang, C.; Douglas, R.; Goldberg, R.A. A Three-Dimensional Construct of the Aging Eyebrow: The Illusion of Volume Loss. Aesthet. Surg. J. 2012, 32, 46–57. [Google Scholar] [CrossRef]
- Lambros, V. Changes in Eyebrow Position and Shape with Aging. Plast. Reconstr. Surg. 2009, 124, 1302–1303. [Google Scholar] [CrossRef] [PubMed]
- Yun, S.; Son, D.; Yeo, H.; Kim, S.; Kim, J.; Han, K.; Lee, S.; Lee, J. Changes of eyebrow muscle activity with aging: Functional analysis revealed by electromyography. Plast. Reconstr. Surg. 2014, 133, 455e–463e. [Google Scholar] [CrossRef]
- Asaad, M.; Kelarji, A.B.; Jawhar, C.S.; Banuelos, J.; Taslakian, E.; Wahood, W.; Vyas, K.S.; Sharaf, B. Eyebrow height changes with aging: A systematic review and meta-analysis. Plast. Reconstr. Surg Global Open 2019, 7, e2433. [Google Scholar] [CrossRef]
- Tran, A.Q.; Yang, C.; Tooley, A.A.; Mahan, M.; Jamerson, E.C.; Kazim, M.; Glass, L.R.D. The Arched Rainbow Brow in Thyroid Eye Disease. Ophthalmic Plast. Reconstr. Surg. 2022, 10, 1097. [Google Scholar] [CrossRef]
- Favre, N.; Sherris, D. Botulinum toxin in facial plastic surgery. Plast. Aesthet. Res. 2020, 7, 71. [Google Scholar] [CrossRef]
- Driessen, C.; Tzou, C.-H.J.; Rodríguez-Lorenzo, A. Principles of Symmetrisation Techniques in Facial Palsy. In Facial Palsy; Springer: Berlin, Germany, 2021; pp. 285–293. [Google Scholar]
- Lee, W.W.; Levitt, A.E. Periocular rejuvenation with neurotoxin and dermal filler. Plast. Aesthet. Res. 2018, 5, 43. [Google Scholar] [CrossRef][Green Version]
- Frankel, A.S.; Kamer, F.M. Chemical browlift. Arch. Otolaryngol.-Head Neck Surg. 1998, 124, 321–323. [Google Scholar] [CrossRef] [PubMed]
- Rohrich, R.J.; Janis, J.E.; Fagien, S.; Stuzin, J.M. The Cosmetic Use of Botulinum Toxin. Plast. Reconstr. Surg. 2003, 112, 177S–188S. [Google Scholar] [CrossRef] [PubMed]
- Steinsapir, K.D. Reply re: “Cosmetic Microdroplet Botulinum Toxin A Forehead Lift: A New Treatment Paradigm”. Ophthalmic Plast. Reconstr. Surg. 2015, 31, 491. [Google Scholar] [CrossRef] [PubMed]
- Carruthers, A.; Carruthers, J. (Eds.) Botulinum toxin type A: History and current cosmetic use in the upper face. In Seminars in Cutaneous Medicine and Surgery; WB Saunders: Philadelphia, PA, USA, 2001. [Google Scholar]
- Huilgol, S.C.; Carruthers, A.; Carruthers, J.D.A. Raising Eyebrows with Botulinum Toxin. Dermatol. Surg. 1999, 25, 373–376. [Google Scholar] [CrossRef]
- Steinsapir, K.D. Cosmetic Use of Botulinum Toxin for the Treatment of Eyebrow and Forehead Ptosis, and Unwanted Eyebrow Expression. U.S. Patent US7846457B2, 7 December 2010. [Google Scholar]
- Huang, W.; Rogachefsky, A.S.; Foster, J.A. Browlift with Botulinum Toxin. Dermatol. Surg. 2000, 26, 55–60. [Google Scholar] [CrossRef]
- Steinsapir, K.D.; Steinsapir, S. Botulinum Toxin Brow Elevation and Shaping. Adv. Cosmet. Surg. 2022, 5, 137–144. [Google Scholar] [CrossRef]
- Iranmanesh, B.; Khalili, M.; Mohammadi, S.; Amiri, R.; Aflatoonian, M. Employing microbotox technique for facial rejuvenation and face-lift. J. Cosmet. Dermatol. 2022, 21, 4160–4170. [Google Scholar] [CrossRef]
- Steinsapir, K.D.; Rootman, D.; Wulc, A.; Hwang, C. Cosmetic microdroplet botulinum toxin A forehead lift: A new treatment paradigm. Ophthalmic Plast. Reconstr. Surg. 2015, 31, 263–268. [Google Scholar] [CrossRef]
- De Maio, M.; DeBoulle, K.; Braz, A.; Rohrich, R.J. Facial assessment and injection guide for botulinum toxin and injectable hyaluronic acid fillers: Focus on the midface. Plast. Reconstr. Surg. 2017, 140, 540e–550e. [Google Scholar] [CrossRef]
- Li, K.; Meng, F.; Li, Y.R.; Tian, Y.; Chen, H.; Jia, Q.; Cai, H.; Jiang, H.B. Application of Nonsurgical Modalities in Improving Facial Aging. Int. J. Dent. 2022, 2022, 8332631. [Google Scholar] [CrossRef]
- Brown, A.; Teller, C. Identifying and managing complications caused by cosmetic neurotoxin treatment. Dermatol. Rev. 2022, 3, 247–256. [Google Scholar] [CrossRef]
- Martina, E.; Diotallevi, F.; Radi, G.; Campanati, A.; Offidani, A. Therapeutic Use of Botulinum Neurotoxins in Dermatology: Systematic Review. Toxins 2021, 13, 120. [Google Scholar] [CrossRef] [PubMed]
- Domínguez-Duarte, A. Aesthetic implications of depressor supercilii muscle block with botulinum toxin type A. J. Cosmet. Dermatol. 2022, 21, 1374–1378. [Google Scholar] [CrossRef] [PubMed]
- de Maio, M. The minimal approach: An innovation in facial cosmetic procedures. Aesthet. Plast. Surg. 2004, 28, 295–300. [Google Scholar] [CrossRef] [PubMed]
- Farolch-Prats, L.; Nome-Chamorro, C. Facial Contouring by Using Dermal Fillers and Botulinum Toxin A: A Practical Approach. Aesthet. Plast. Surg. 2019, 43, 793–802. [Google Scholar] [CrossRef]
- Minelli, L.; Richa, J.; Mendelson, B.C. Aesthetic Enhancement of the Brow using Hydroxyapatite. Aesthet. Plast. Surg. 2022, 46, 1201–1210. [Google Scholar] [CrossRef]
- Van Loghem, J.; Yutskovskaya, Y.A.; Werschler, W.P. Calcium hydroxylapatite: Over a decade of clinical experience. J. Clin. Aesthet. Dermatol. 2015, 8, 38. [Google Scholar]
- Hwang, C.J. Periorbital injectables: Understanding and avoiding complications. J. Cutan. Aesthet. Surg. 2016, 9, 73–79. [Google Scholar] [CrossRef]
- Beleznay, K.; Carruthers, J.D.; Humphrey, S.; Jones, D. Avoiding and Treating Blindness from Fillers: A Recent Review of the World Literature. Dermatol. Surg. 2015, 41, 1097–1117. [Google Scholar] [CrossRef]
- Beleznay, K.; Humphrey, S.; Carruthers, J.D.; Carruthers, A. Vascular compromise from soft tissue augmentation: Experience with 12 cases and recommendations for optimal outcomes. J. Clin. Aesthet. Dermatol. 2014, 7, 37–43. [Google Scholar]
- Ozturk, C.N.; Li, Y.; Tung, R.; Parker, L.; Piliang, M.P.; Zins, J.E. Complications Following Injection of Soft-Tissue Fillers. Aesthet. Surg. J. 2013, 33, 862–877. [Google Scholar] [CrossRef] [PubMed]
- Rzany, B.; Delorenzi, C. Understanding, Avoiding, and Managing Severe Filler Complications. Plast. Reconstr. Surg. 2015, 136, 196S–203S. [Google Scholar] [CrossRef] [PubMed]
- Mella, J.; Oyer, S. Nonsurgical rhinoplasty: Prevention and management of associated complications. Curr. Opin. Otolaryngol. Head Neck Surg. 2022, 30, 241–248. [Google Scholar] [CrossRef] [PubMed]
- Kapoor, K.M.; Chatrath, V.; Li, C.Q.; Bertossi, D. Pinch anatomy: An injection guide for temple filler injections. Dermatol. Ther. 2020, 33, e13983. [Google Scholar] [CrossRef]
- Heydenrych, I.; De Boulle, K.; Kapoor, K.M.; Bertossi, D. The 10-Point Plan 2021: Updated concepts for improved procedural safety during facial filler treatments. Clin. Cosmet. Investig. Dermatol. 2021, 14, 779, Corrected in Clin. Cosmetic Investig. Dermatol. 2021, 14, 1601–1602. [Google Scholar] [CrossRef]
- De Maio, M.; Swift, A.; Signorini, M.; Fagien, S. Facial assessment and injection guide for botulinum toxin and injectable hyaluronic acid fillers: Focus on the upper face. Plast. Reconstr. Surg. 2017, 140, 265e–276e. [Google Scholar] [CrossRef]
- Kapoor, K.M.; Chatrath, V.; Li, C.Q.; Bertossi, D. Pinch Anatomy of Forehead: An Injection Guide for Forehead Filler Treatment. Facial Plast. Surg. 2022, 38, 156–162. [Google Scholar] [CrossRef]
- Austin, G.K.; Struble, S.L.; Quatela, V.C. Evaluating the effectiveness and safety of radiofrequency for face and neck rejuvenation: A systematic review. Lasers Surg. Med. 2022, 54, 27–45. [Google Scholar] [CrossRef]
- Nahm, W.K.; Su, T.T.; Rotunda, A.M.; Moy, R.L. Objective changes in brow position, superior palpebral crease, peak angle of the eyebrow, and jowl surface area after volumetric radiofrequency treatments to half of the face. Dermatol. Surg. 2004, 30, 922–928. [Google Scholar]
- Alexiades, M.; Berube, D. Randomized, blinded, 3-arm clinical trial assessing optimal temperature and duration for treatment with minimally invasive fractional radiofrequency. Dermatol. Surg. 2015, 41, 623–632. [Google Scholar] [CrossRef]
- Kornstein, A.N. (Ed.) Intramuscular Insertion of a Radiofrequency Microneedling Device for Facial Rejuvenation: A New Technique and Case Reports. In Aesthetic Surgery Journal Open Forum; Oxford University Press US: Cary, NC, USA, 2020. [Google Scholar]
- Ukoha, U.; Malone, C.H.; Munavalli, G. Nonsurgical Brow Lift with a Temperature-Controlled, Fractionated Radiofrequency Needle Device. Dermatol. Surg. 2021, 47, 296–298. [Google Scholar] [CrossRef] [PubMed]
- Alam, M.; White, L.E.; Martin, N.; Witherspoon, J.; Yoo, S.; West, D.P. Ultrasound tightening of facial and neck skin: A rater-blinded prospective cohort study. J. Am. Acad. Dermatol. 2010, 62, 262–269. [Google Scholar] [CrossRef] [PubMed]
- Lio, M.-L.; Chang, C.-C.; Chuang, A.D.-C.; Tsai, L.-C.; Chen, C.-C. Quantified Facial Rejuvenation Utilizing High Intense Focus Ultrasound with Multiple Penetrative Depths. Clin. Cosmet. Investig. Dermatol. 2022, 15, 489–496. [Google Scholar] [CrossRef] [PubMed]
- Wanitphakdeedecha, R.; Yan, C.; Ng, J.N.C.; Ya-Nin Nokdhes, D.P.D.S.; Tantrapornpong, P.; Techapichetvanich, T.; Eimpunth, S.; Manuskiatti, W. The efficacy of macro-focused ultrasound in the treatment of upper facial laxity: A pilot study. J. Cosmet. Dermatol. 2020, 19, 1955–1961. [Google Scholar] [CrossRef] [PubMed]
- Alam, M.; Dover, J.S. Ultrasound Tightening of Facial and Neck Skin. In Non-Surgical Skin Tightening and Lifting; Elsevier: Amsterdam, The Netherlands, 2008; pp. 33–39. [Google Scholar]
- Witherspoon, J.; White, L.; West, D.; Ortiz, S.; Yoo, S.; Havey, J.; Agha, R.; Martin, N.; Alam, M. (Eds.) Procedure for evaluating change in eyebrow position induced by ultrasound skin tightening. J. Investig. Dermatol. 2008, S78. [Google Scholar]
- Park, J.Y.; Byun, E.J.; Kim, H.S. Rejuvenation of periocular region in Koreans: A multimodal approach combining botulinum toxin, fillers, and micro-focused ultrasound with visualization for optimal results. Dermatol. Ther. 2020, 33, e13159. [Google Scholar] [CrossRef]
- Hugul, H.; Oba, M.C.; Kirisci, M.; Kutlubay, Z. Focused radiofrequency and ultrasound for face and neck rejuvenation: A retrospective evaluation of 158 patients. J. Cosmet. Dermatol. 2022, 21, 290–295. [Google Scholar] [CrossRef]
- FDA. Tixel® System; Department of Health and Human Services, FDA: Silver Springs, MD, USA, 2021.
- Hilerowicz, Y.; Friedman, O.; Zur, E.; Ziv, R.; Koren, A.; Salameh, F.; Mehrabi, J.N.; Artzi, O. Thermomechanical ablation-assisted photodynamic therapy for the treatment of acne vulgaris. A retrospective chart review of 30 patients. Lasers Surg. Med. 2020, 52, 966–970. [Google Scholar] [CrossRef]
- Salameh, F.; Daniely, D.; Kauvar, A.; Carasso, R.L.; Mehrabi, J.N.; Artzi, O. Treatment of periorbital wrinkles using thermo-mechanical fractional injury therapy versus fractional non-ablative 1565 nm laser: A comparative prospective, randomized, double-arm, controlled study. Lasers Surg. Med. 2022, 54, 46–53. [Google Scholar] [CrossRef]
- Parhi, R.; Mandru, A. Enhancement of skin permeability with thermal ablation techniques: Concept to commercial products. Drug Deliv. Transl. Res. 2021, 11, 817–841. [Google Scholar] [CrossRef]
- Grewal, S.K.; Ortiz, A. Perioral Rejuvenation in Aesthetics: Review and Debate. Clin. Dermatol. 2022, 40, 265–273. [Google Scholar] [CrossRef] [PubMed]
- Gray, M.L.; Boahene, K.D.O. Facial Rejuvenation in Patients of Color. Curr. Otorhinolaryngol. Rep. 2022, 10, 303–309. [Google Scholar] [CrossRef]
- Nunez, J.H.; Strong, A.L.; Comish, P.; Hespe, G.E.; Harvey, J.; Sorkin, M.; Levi, B. A Review of Laser Therapies for the Treatment of Scarring and Vascular Anomalies. Adv. Wound Care, 2022; ahead of print. [Google Scholar] [CrossRef]
- Kołodziejczak, A.; Rotsztejn, H. Efficacy of fractional laser, radiofrequency and IPL rejuvenation of periorbital region. Lasers Med. Sci. 2022, 37, 895–903. [Google Scholar] [CrossRef] [PubMed]
- Alhallak, K.; Abdulhafid, A.; Tomi, S.; Omran, D. Pigmentation and Scaring Management after Hypodermoclysis, a Case Report. Cosmetics 2022, 9, 10. [Google Scholar] [CrossRef]
- Al Hallak, K.; Tomi, S.; Omran, D. Q-switch nanosecond laser as innovative and instant management for bruises discoloration, a case report. J. Cosmet. Laser Ther. 2021, 23, 19–23. [Google Scholar] [CrossRef] [PubMed]
- de Filippi Sartori, J.; Osaki, T.H.; Osaki, M.H.; de Souza, R.B.; Allemann, N. “Split-Face” Evaluation of Collagen Changes Induced by Periorbital Fractional CO2 Laser Resurfacing. Aesthet. Surg. J. 2022, 42, 239–248. [Google Scholar] [CrossRef]
- Balzani, A.; Chilgar, R.M.; Nicoli, M.; Sapountzis, S.; Lazzeri, D.; Cervelli, V.; Nicoli, F. Novel approach with fractional ultrapulse CO2 laser for the treatment of upper eyelid dermatochalasis and periorbital rejuvenation. Lasers Med. Sci. 2013, 28, 1483–1487. [Google Scholar] [CrossRef]
- Malik, A.; Denisova, K.; Barmettler, A. Contemporary Management of the Periocular Area. Curr. Otorhinolaryngol. Rep. 2021, 9, 448–456. [Google Scholar] [CrossRef]
- Badawi, A.; Sobeih, T.; Jasmina, V. Periocular rejuvenation using a unique non-ablative long-pulse 2940 nm Er:YAG laser. Lasers Med. Sci. 2022, 37, 1111–1118. [Google Scholar] [CrossRef]
- Gaspar, A. Er:YAG Treatment for Eyebrow Tail Elevation and Eyelid Rejuvenation using the Fotona VectorLift Technique with SMOOTH Mode Hyperstacking. J. Laser Health Acad. 2021, 2021, CN23. [Google Scholar]
- Santorelli, A.; Cirillo, P.; Fundarò, S.; Cavallini, M.; Salti, G.; Avvedimento, S. Eyebrow lifting with barbed threads: A simple, safe and effective ambulatory procedure. J. Cosmet. Dermatol. 2022; ahead of print. [Google Scholar] [CrossRef]
- Halepas, S.; Chen, X.J.; Ferneini, E.M. Thread-lift sutures: Anatomy, technique, and review of current literature. J. Oral Maxillofac. Surg. 2020, 78, 813–820. [Google Scholar] [CrossRef] [PubMed]
- Sulamanidze, M.; Sulamanidze, G. APTOS Suture Lifting Methods: 10 Years of Experience. Clin. Plast. Surg. 2009, 36, 281–306. [Google Scholar] [CrossRef] [PubMed]
- Silvino, T.S.T.; Souza Weimann, E.T.; Matos, L.S. Introduction: Threads in Cosmetic Procedures. In Minimally Invasive Aesthetic Procedures; Springer: Berling, Germany, 2020; pp. 393–402. [Google Scholar]
- Borzykh, O.B.; Karpova, E.I.; Shnayder, N.A.; Demina, O.M. Contemporary View on Thread Lifting: Histological And Anatomical Approaches. Russ. Open Med. J. 2022, 11, 107. [Google Scholar] [CrossRef]
- Wong, V. The science of absorbable poly (L-Lactide-Co-ε-Caprolactone) threads for soft tissue repositioning of the face: An evidence-based evaluation of their physical properties and clinical application. Clin. Cosmet. Investig. Dermatol. 2021, 14, 45. [Google Scholar] [CrossRef]
- De Masi, E.C.; De Masi, F.D.; De Masi, R.D. Suspension threads. Facial Plast. Surg. 2016, 32, 662–663. [Google Scholar] [CrossRef] [PubMed]
- Kochhar, A.; Kumar, P.; Karimi, K. Minimally Invasive Techniques for Facial Rejuvenation Utilizing Polydioxanone Threads. Facial Plast. Surg. Clin. N. Am. 2022, 30, 375–387. [Google Scholar] [CrossRef]
- Atiyeh, B.S.; Chahine, F.; Ghanem, O.A. Percutaneous Thread Lift Facial Rejuvenation: Literature Review and Evidence-Based Analysis. Aesthet. Plast. Surg. 2021, 45, 1540–1550. [Google Scholar] [CrossRef]
- Pham, C.T.; Chu, S.; Foulad, D.P.; Mesinkovska, N.A. Safety Profile of Thread Lifts on the Face and Neck: An Evidence-Based Systematic Review. Dermatol. Surg. 2021, 47, 1460–1465. [Google Scholar] [CrossRef]
- Lekic, N.; Dodds, S.D. Suture Materials, Needles, and Methods of Skin Closure: What Every Hand Surgeon Should Know. J. Hand Surg. 2022, 47, 160–171.e1. [Google Scholar] [CrossRef]
- Greenberg, J.A. The use of barbed sutures in obstetrics and gynecology. Rev. Obstet. Gynecol. 2010, 3, 82–91. [Google Scholar]
- Byrne, M.; Aly, A. The surgical suture. Aesthet. Surg. J. 2019, 39 (Suppl. 2), S67–S72. [Google Scholar] [CrossRef] [PubMed]
- Kim, B.; Oh, S.; Jung, W. Type of Absorbable Thread Products. In The Art and Science of Thread Lifting; Springer: Berlin, Germany, 2019; pp. 73–77. [Google Scholar]
- Yongtrakul, P.; Sirithanabadeekul, P.; Siriphan, P. Thread lift: Classification, technique, and how to approach to the patient. World Acad. Sci. Eng. Technol. 2016, 10, 558–566. [Google Scholar]
- Ghasemi, S.; Stevens, M.R.; Hosn Centero, S.A. Thread Lift. In Integrated Procedures in Facial Cosmetic Surgery; Springer: Berlin, Germany, 2021; pp. 629–634. [Google Scholar]
- Felipe, I. Eyebrow Thread Lifting. In Minimally Invasive Aesthetic Procedures; Springer: Berlin, Germany, 2020; pp. 407–413. [Google Scholar]
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).