Abstract
Orofacial clefts are one of the most common congenital anomalies worldwide; however, morphopathogenesis of the clefts is not yet completely understood. Taking the importance of innate immunity into account, the aim of this work was to examine the appearance and distribution of macrophages (M) 1, M2, and TNF-α, as well as to deduce any possible intercorrelations between the three factors in cleft affected lip tissue samples. Twenty samples of soft tissue were collected from children during plastic surgery. Fourteen control tissue samples were obtained during labial frenectomy. Tissues were immunohistochemically stained, analysed by light microscopy using a semi-quantitative method, and the Mann–Whitney U and Spearman’s tests were used to evaluate statistical differences and correlations. A statistically significant difference in the distribution was observed only in regard to M1. A weak correlation was observed between M2 and TNF-α but a moderate one between M1 and M2 as well as M1 and TNF-α. However, only the correlation between M1 and M2 was statistically important. The rise in M1, alongside the positive correlation between M1 and TNF-α, suggested a more pro-inflammatory/inflammatory environment in the cleft affected lip tissue. The moderate positive correlation between M1 and M2 indicated an intensification of the protective mechanisms.
1. Introduction
Facial prominences appear by the end of the fourth week; however, during the seventh week, the secondary palate is formed and fused with the primary palate and nasal septum, forming a newly formed palate. At first glance, it may seem a simple process; however, the formation of the facial structures is a complex cascade of events during which cells proliferate, differentiate, adhere, and go through apoptosis. An error during this intricate process can result in orofacial clefts or other abnormalities [,]. One of the most common congenital anomalies worldwide is the orofacial cleft. Its incidence is approximately 1 in 700 to 1000 births []. It has been observed that a cleft lip with or without a cleft palate occurs in males more frequently (~65%) than in females, and its incidence varies between populations. Furthermore, morphogenesis and pathogenesis of the cleft lip are not yet completely understood. Some cases are syndromic, others caused by exposure to teratogenic compounds []. Moreover, one of the possibilities to be considered is inflammation and inflammatory cytokines. Although children with and without a cleft lip have the same oral microbiota, children with a cleft lip have greater oral tissue inflammation [].
Most studies have established macrophages as a vital part of both innate and adaptive immunity. By now it is known that these cells, which are abundant in almost all tissues, play a pivotal role in the resolution of inflammation, tissue repair, homeostasis, and antigen presentation [,]. Moreover, their presence in various places is necessary for foetal development []. During the last two decades, the concept of macrophage polarization and its influence on inflammation have been explored in more detail. Polarisation is understood as a complex time and tissue-dependant process that entails internal, external, and tissue environment stimuli, including growth factors, cytokines, and pathogen-derived molecules. At first, type 1 macrophages (M1) were classified as having a pro-inflammatory phenotype and type 2 macrophages (M2) as anti-inflammatory macrophages. However, further studies showed that both their induction routes and regulated biological processes are more complicated than thought, and upon environmental changes, macrophages can undergo functional re-differentiation [,].
M1 are a part of the first line of defence against intracellular pathogens and promote the T helper 1 (Th1) polarization of cluster of differentiation (CD) 4+ cells. It has been observed that if an inflammatory environment is dominated by Toll-like receptor and interferon (IFN) signalling, M1 will be present []. Markers which best characterize this phenotype were identified as CD64+ and CD80+ by flow cytometry []. In terms of transcriptional markers, there are many, such as interleukin (IL)-12p35, CXC chemokine ligand (CXCL)-10, CC chemokine ligand (CCL)-5. M1 can produce pro-inflammatory cytokines, such as IL-1β, IL-6, tumour necrosis factor-alpha (TNF-α), type I IFN, and several chemokines; for instance, CXCL1, CCL5, fractalkine (CX3CL1). These biologically active substances induce Th1 response activation, promote complement-mediated phagocytosis and type I inflammation. Therefore, it is clear that M1 have the ability to guide acute inflammatory responses. Last but not least, their antigen presentation capacity is high, and in the early stages of healing, they actively phagocytize, for example, microorganisms or debris [].
M2 phenotype is activated in response to T helper 2 (Th2). Macrophage colony-stimulating factor, IL-4, IL-10, IL-13, or a mix of them can induce M2-like phenotype []. Usually, this phenotype is identified based on the expression of CD11b+ and CD209+ []. M2 are able to produce a variety of biologically active substances, for instance, IL-13, CCL1, IL-1R, IL-8, monocyte chemoattractant protein-1 (MCP-1/CCL2), macrophages inflammatory protein-1β (MIP-1β), regulated on activation, normal T cell expressed and secreted (RANTES, also known as CCL5). Therefore, they can recruit different leukocytes in an anti-inflammatory or regulatory response []. Depending on the stimuli, different subsets have been identified: M2a, M2b, M2c, and M2d [,]. M2 phenotype negatively regulates pro-inflammatory cytokines and induces production of anti-inflammatory mediators, for instance, transforming growth factor-beta (TGF-β). They participate in homeostasis, various metabolic processes, as well as repair mechanisms and pathogenesis []. M2 in a healthy tissue under homeostatic conditions is thought to be the “default” phenotype in resident macrophages [].
It is believed that for the maintenance of homeostasis, there must be an adequate balance between the two types of macrophages. A disequilibrium may lead to an unbalanced inflammation []. Based on their proved functions, it is clear that macrophages are involved in resolving inflammation at different stages of the inflammatory cascade. Unfortunately, when the stimuli that caused the onset of the inflammation is persistent or cannot be destroyed, it will lead to a certain degree of tissue damage, and chronic inflammation could develop because of the prolonged inflammatory response or insufficient production of resolution mediators []. Data from different studies show that an imbalance between M1 and M2 contributes to different diseases, such as asthma [], atherosclerosis [], endometriosis [], and osteoclastogenesis in rheumatoid arthritis patients [].
Essentially, macrophages are cells that “sample” the environment, often by phagocytosing material. As soon as this material, for example, a pathogen or damaged tissue, is recognized, the most appropriate response is triggered. Usually, the macrophage decides to either kill it or repair it. During the killing process, macrophages preferentially produce NO, however during the repair, they produce ornithine (a non-proteinogenic amino acid). Even though both substances arise from the same amino acid (arginine) being cleaved in slightly different ways, their functions are opposite. Whilst NO has the ability to inhibit cell proliferation, ornithine promotes proliferation and repair through polyamines and collagen. It is known that intermediates in each enzyme pathway inhibit the opposing path. Furthermore, based on the substance formed, additional changes could be observed, such as what kind of interleukins and other factors will be produced. Depending on molecules released, different types of immune response arise. In addition, macrophages express other cytokines, for example, TNF-α, IL-1β, and IL-6 that have important physiological effects; however, no direct correlation between the production of these cytokines and NO or ornithine production has been observed [].
Even though primary TNF-α is synthesized by the cells of monocytic linage (for example, macrophages, astroglia, microglia, Kupffer cells) and T cells, other types of cells can also produce it. TNF-α is a powerful pro-inflammatory agent. Moreover, studies show that it plays a vital role in regulating the cytokine cascade in inflamed tissue []. Tumour necrosis factor receptor 1 (TNFR1) and tumour necrosis factor receptor 2 (TNFR2) are transmembrane receptors through which TNF-α signals []. Moreover, this pro-inflammatory agent participates in the regulation of cell survival, proliferation, differentiation, and apoptosis. Interestingly, macrophages are not only one of the main sources of TNF-α, but they also are quite sensitive to it. This unusual process contributes to the pathogenesis of various diseases, for instance, Crohn’s disease, sepsis, and atherosclerosis []. Furthermore, TNF-α has been observed in macrophages and neutrophils in the facial tissue of children with a cleft lip and palate. Taken the functions of TNF-α into account, its role in the pathogenesis of cleft lip and cleft palate has not been excluded []. Data from different publications indicate that the autocrine signalling by TNF-α is essential for the long-term survival of macrophages. In addition, results suggest that TNF-α possesses macrophage differentiation capabilities [].
Despite the already mentioned significance of M1 to M2 ratio in different diseases, there has been limited research regarding macrophages in cleft affected tissue. Furthermore, whilst the presence of most common pro- and anti-inflammatory cytokines in cleft affected tissue has been studied, their effect is still unclear [,]. Overall, the inflammation in a cleft affected tissue is regarded as chronic and, due to their functions, macrophages are associated with chronic inflammation. Based on the above mentioned, the aim of this work was to examine the appearance and distribution of type 1 and 2 macrophages and tumour necrosis factor-alpha, as well as deduce any possible correlation between M1, M2, and TNF-α in cleft affected lip tissue samples.
2. Materials and Methods
2.1. Information about the Patients
The study was performed in accordance with the 1964 Declaration of Helsinki. The study was approved by the Ethical Committee of Riga Stradins University (22 May 2003; 17 January 2013; 5/25 June 2018), Project 5-1/384/2020 from 10 September 2020. After the nature of the study had been fully explained, written informed consent was obtained from all the parents.
In the study, 20 children (14 boys and 6 girls), aged 3 to 18 months, diagnosed with Cheilognathouranoschisis (dextra, sinistra, or bilateralis) participated. The recruitment for participation in the study happened between 2010 and 2019 at the Riga Stradins University Institute of Stomatology, Latvia. The inclusion criteria were: patients diagnosed with cleft lip, alveolar ridge and palate (unilateral or bilateral), aged before primary dentition (from 3 to 18 months), without periodontal disease or other illnesses preventing the patient from receiving cleft lip and palate repair surgery. The 19th and 20th child were included in the research as borderline cases (Table 1). The samples of soft tissues from the cleft lip region were collected during surgical procedures on unilateral (18) or bilateral (2) clefts. In 5 out of 20 cases, no additional remarks were made by the physician; however, in one case, no information about the family history was available. In two cases, ultrasonography revealed the presence of a facial cleft formed during child development. In six cases, during pregnancy, the mother had taken medication, such as antibiotics and/or paracetamol. One or more facial clefts in family history were noted in four cases and the presence of Down syndrome in one. Two children had other anomalies in addition to the facial cleft. Information about the patients is summarized in detail in Table 1.

Table 1.
Information about the patients.
The control group was also recruited at Riga Stradins University Institute of Stomatology, Latvia, from 2010 to 2019. In total, 14 control tissue samples were obtained from the upper lip mucosa during superior labial frenectomy due to hypertrophic upper lip frenulum. The inclusion criteria for the control group were: patients diagnosed with hypertrophic upper lip frenulum, no orofacial cleft in anamnesis or family history, no inflammation or any other pathology present. The control group consisted of eight boys and six girls (5–14 years of age).
For at least one month before the surgery, all the participating children were healthy, without any complications, and able to undergo surgery.
2.2. Immunohistochemical Analysis
Tissues were fixed for a day in a mixture of 2% formaldehyde and 0.2% picric acid in 0.1 M phosphate buffer with pH 7.2. Subsequently, the tissue material was rinsed in Tyrode buffer (content: NaCl, KCl, CaCl2·2H2O, MgCl2·6H2O, NaHCO3, NaH2PO4·H2O, glucose), containing 10% saccharose, for 12 h and then embedded into paraffin. The tissue samples were cut three micrometres thick and, afterwards, stained with haematoxylin and eosin for routine morphological evaluation.
Biotin–streptavidin biochemical method was used for immunohistochemistry to detect following primary antibodies: anti-tumour necrosis factor alpha (TNF-α, ab6671, rabbit, working dilution 1:200, Abcam, Cambridge, UK), anti-macrophage inflammatory protein 1 beta (anti-MIP-1β, ab9675, rabbit, working dilution 1:100, Abcam, Cambridge, UK), and anti-CD163 (ab87099, rabbit, working dilution 1:200, Abcam, Cambridge, UK). The antibodies used in this study were diluted with antibody diluent (code 938B-05, Cell MarqueTM, Rocklin, CA, USA). The tissue samples were deparaffinized, washed in alcohol and water, placed in a holder, rinsed twice for five minutes with TRIS buffer (code 2017X12508, Diapath S.p.A., Martinengo, Italy), then boiled in EDTA buffer (code 2017X02239, Diapath S.p.A., Martinengo, Italy) in a microwave for approximately 20 minutes. After cooling down, the tissue samples were washed in TRIS wash buffer twice for five minutes. The blocking was performed for 10 min, using 3% peroxide solution, followed by repeated washing in TRIS wash buffer. The tissue samples were then incubated for an hour with primary antibodies. Subsequently, after incubation and rinsing with TRIS wash buffer three times, the HiDef DetectionTM (code 954D-31, Cell MarqueTM, Rocklin, CA, USA) reaction amplificator was applied for 10 min at room temperature. This was followed by repeated washing for 5 min in TRIS wash buffer and then a second incubation for 10 min, also at room temperature, using the HiDef DetectionTM HRP Polymer Detector (code 954D-32, Cell MarqueTM, Rocklin, CA, USA). After another rinsing with TRIS buffer 3 times for 5 min and then tissue coating with the DAB+ chromogenic liquid DAB Substrate Kit (code 957D-60, Cell MarqueTM, Rocklin, CA, USA) up to 10 min at room temperature was performed, which resulted in positive structures staining in brown colour. After incubation with the chromogenic substrate system, the samples were rinsed with water and counterstained with haematoxylin (code 05-M06002, Mayer’s Bio Optica Milano S.p.A., Milano, Italy). Further, the tissue samples were dehydrated with 70–90 °C ethanol solutions and clarified with carboxylic acid and xylol. A drop of Pertex glue was applied to the tissue section and a coverslip was glued.
In sections parallel to the investigated ones, the primary antibody was replaced with the antibody diluent. These sections were used as negative controls. For each series of tissue sections, positive controls indicated by the manufacturer were also prepared.
Two independent morphologists, who analysed the tissue samples of the oral mucosa by light microscopy using a semi-quantitative scoring system [], were blinded to the sample identification. The results were assessed by grading the appearance of positively stained cells in five randomly selected fields of view at x400 magnification. Structures were labelled as follows: 0, negative staining (0%); 0/+, occasional positive structures (12.5%); +, few positive structures (25%); +/++, few to moderate immunoreactive structures (37.5%); ++, moderate number of positive structures (50%); ++/+++, moderate to numerous positive structures (62.5%); +++, numerous positive structures in the visual field (75%) [].
For visual illustration, we used a Leica LEITZ DM RB microscope, Euromex Scientific Camera DC.20000i, and the image processing and analysis software ImageFocusAlpha (Euromex Microscopen bv, Arnhem, The Netherlands).
2.3. Statistical Analysis
The data processing was performed using IBM SPSS Statistics Version 26 (IBM Company, Armonk, New York, NY, USA). The results from semi-quantitative evaluation were transformed into numerical form as follows: 0 equals to 0, 0/+ equals to 0.5, + equals to 1, +/++ equals to 1.5, ++ equals to 2, ++/+++ equals to 2.5, +++ equals to 3. Spearman’s rank correlation coefficient was used, and the R-value was judged as follows: R = 0.0–0.2, a very weak correlation; R = 0.2–0.4, a weak correlation; R = 0.4–0.6, a moderate correlation; R = 0.6–0.8, a strong correlation; and R = 0.8–1.0, a very strong correlation. To analyse the data from patients versus control groups, Mann–Whitney U test was used. The significance level for both tests was 5% (p-value < 0.05).
3. Results
Routine haematoxylin and eosin staining showed patchy vacuolization of the lip epithelial cells (seborrheic keratosis) in 16 out of 20 cases, varying degrees of inflammation in 14 tissue samples, and basal cell hyperplasia in the epithelium of 9 tissue samples (Table 2, Figure 1a,b). Only one tissue sample and the controls did not show any of the above-mentioned signs (Table 2, Figure 1c).

Table 2.
The relative number of M1-, M2-, and TNF-α-positive structures and the degree of seborrheic keratosis, inflammation, and basal cell hyperplasia present in the cleft affected tissue samples as well as in the control group.
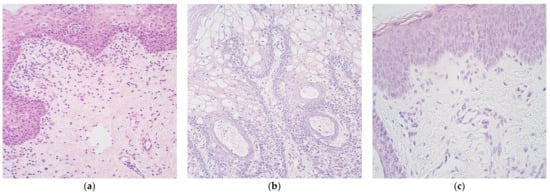
Figure 1.
Micrographs of a cleft affected lip tissue. (a) Notable inflammation (+++) in the connective tissue and moderate degree of basal cell hyperplasia (++) in the epithelium of a 13 months old child with a cleft lip and palate. Haematoxylin and eosin, ×250; (b) Vacuolated cells of seborrheic keratosis of the lip epithelium in a three months old child with a cleft lip and palate. Haematoxylin and eosin, ×250. (c) Tissue sample without seborrheic keratosis, inflammation, and basal cell hyperplasia in a four months old child with a cleft lip and palate. Haematoxylin and eosin, ×400.
M1-positive structures were found in the range from a few (+) to numerous (+++) (Table 2, Figure 2). However, half of the cases had a moderate number of positive structures (++), five had a few (+), whilst only one tissue sample could have been graded as having numerous positive structures (+++) (Figure 3a). In terms of controls, one had negative staining, but the other overall had a small number of positive structures (Figure 3b).
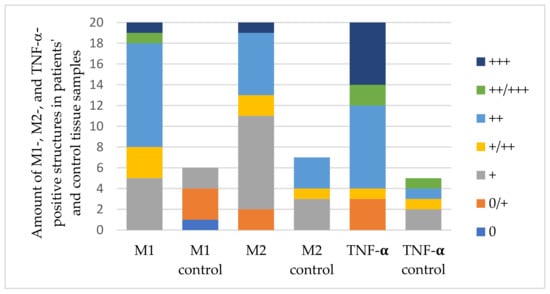
Figure 2.
The distribution of M1-, M2-, and TNF-α-positive structures in patients’ group and control group tissue samples. Abbreviations: M1—phenotype 1 macrophages, M2—phenotype 2 macrophages, TNF-α—tumour necrosis factor alpha, 0—negative staining, 0/+—occasional positive structures, +—few positive structures, +/++—few to moderate immunoreactive structures, ++—moderate number of positive structures, ++/+++—moderate to numerous positive structures, +++—numerous positive structures in the visual field.
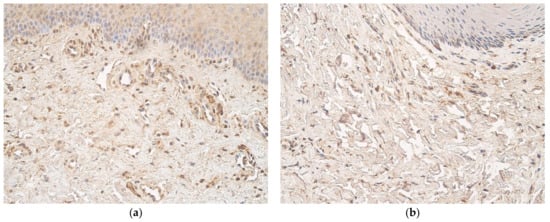
Figure 3.
Immunohistochemical micrographs of M1 in a cleft affected lip tissue and in a control subject. (a) Moderate positive M1 cells (++) in the connective tissue of the cleft lip tissue sample in a three months old child with a cleft lip and palate. M1 IMH, ×250; (b) Occasional positive M1 cells (0/+) in the control group tissue sample of a six years old child. M1 IMH, ×250.
M2-positive structures were found in the range from occasional (0/+) to numerous (+++) (Table 2, Figure 2). Many of the tissue samples (9 out of 20 cases) had a few positive structures (+), followed by a moderate number (++) in 6 cases (Figure 4a). The numbers of positive cells in the control group tissue samples were similar to those in patients’ samples (Figure 4b).
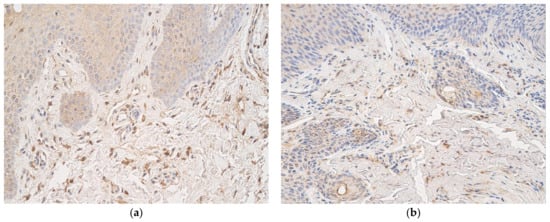
Figure 4.
Immunohistochemical micrographs of M2 in a cleft affected lip tissue and in a control subject. (a) Moderate M2 cells (++) in the connective tissue of the cleft lip tissue sample in an eight months old child with a cleft lip and palate. M2 IMH, x250; (b) Occasional positive M2 cells (0/+) in the control group tissue sample of a six years old child. M2 IMH, ×250.
Although many of the cases (8 out of 20 tissue samples) had a moderate number of TNF-α-positive structures (++), 6 of the tissue samples had numerous (+++), and 2 of them had moderate to numerous positive structures (++/+++) (Table 2, Figure 2 and Figure 5a). Control tissue samples had different numbers of TNF-α-containing cells (Figure 5b).
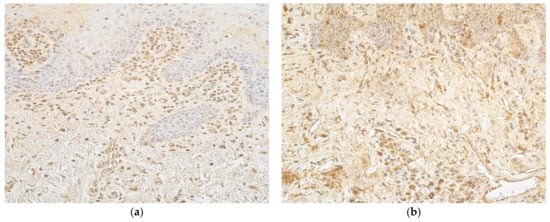
Figure 5.
Immunohistochemical micrographs of TNF-α in a cleft affected lip tissue and in control subjects. (a) Numerous positive cells (+++) of TNF-α in the connective tissue of a 13 months old child with a cleft lip and palate. TNF-α IMH, ×250; (b) Moderate positive cells (++) of TNF-α in the control group tissue sample of a five years old child. TNF-α IMH, ×250.
A statistically important difference in the distribution of a particular factor between the patients’ group and control group was observed only in regard to type 1 macrophages (p = 0.0002) (Table 3).

Table 3.
The statistical significance of the distribution of factors between the patients’ group and control.
In terms of correlations, a weak correlation was observed between M2 and TNF-α (R = 0.261), a moderate correlation between M1 and M2 (R = 0.503) as well as M1 and TNF-α (R = 0.433). However, the only statistically significant one was between M1 and M2 (p = 0.024) (Table 4).

Table 4.
The correlations between the factors in patients’ tissue samples based on the Spearman’s correlation analyses.
4. Discussion
M1-, M2-, and TNF-α-positive cells were present in both the cleft affected tissues and controls. However, the amount of M1 in patients’ material was greater than in the control, suggesting a more pro-inflammatory environment in the cleft affected lip tissue. This was in agreement with other studies, in which more pronounced oral tissue inflammation in children with clefts had been reported [,,]. Interestingly, no notable inflammation with inflammatory cells was detected in 6 out of 20 haematoxylin and eosin stained tissue samples, whilst cells weakly stained with antibodies against M1, M2, and TNF-α antigens were observed there. This suggested a role of specific targeting of inflammatory cells, which otherwise could not be visualised.
A study demonstrated moderate to numerous TNF-α containing macrophages and neutrophils in the cleft affected tissue [], another reported that other cells, such as keratinocytes, which maintain normal homeostatic mechanisms, can also produce TNF-α []. Furthermore, in another research, ELISA (enzyme-linked immunosorbent assay) showed a consistent expression of TNF-α in cleft affected tissue with the second highest mean concentration of all the examined cytokines. However, the coefficient of variation was >50% and the study did not have a control group []. The number of M2- and TNF-α-immunoreactive cells did not differ between the controls and patients in our study. In our opinion, it suggests a possible balance between the cells expressing the two factors and also between the intensity of inflammation and anti-inflammation regulation.
We revealed a statistically significant moderate positive correlation between M1 and M2 in our patients’ tissues. Therefore, it can be deduced that when M1 increased, M2 did as well. In general, an adequate and dynamic balance between pro- and anti-inflammatory factors must exist, otherwise an overzealous inflammatory response could occur, causing extensive tissue damage. Thus, the rise in M2 alongside M1 could be interpreted as a protective mechanism, which helps prevent unbalanced inflammation. A study on the presence of some of the most common interleukins revealed a strong and moderate correlation between IL-1, IL-4, IL-8, IL-10, but not IL-6, in the epithelium of a cleft affected tissue. The authors suggested a compensatory mechanism of self-defence to enhance the local inflammatory immune response without involving all pro-inflammatory cytokines []. This further supports the concept of a protective mechanism. Another research examined the changes in the M1/M2 ratio in isolated microglia after a four-day alcohol exposure in male rats. An increase in both phenotypes in the hippocampus and entorhinal cortex was observed. The authors noted that some TNF-α induction was required to elicit protective M2 responses in the brain; however, the rise in M1 was attributed to the pathology itself []. Furthermore, a significant rise in mRNA expression levels of M1 and M2 markers were observed in the retinal pigment epithelium–choroid (RPE–choroid) and retina following laser photocoagulation in a mouse model of choroidal neovascularization. The M1 phenotype was detected to a greater extent in the RPE–choroid, whilst the one of M2 mainly in the retina []. Even though we observed a simultaneous increase in both factors, many studies have proven that different M1 and M2 appearance patterns also exist. For instance, M1 dominance has been observed not only in periodontitis [] but also at advanced peri-implantitis sites []. In a COPD mouse model, alveolar macrophages favoured the M2 phenotype, thus skewing the macrophage ratio in favour of M2 []. However, in atherosclerosis, the M1/M2 ratio changed depending on the morphological compartment of the vessel wall. For example, M1 macrophages were predominantly at the rupture-prone shoulder regions [].
Nowadays, increasing evidence suggests that macrophages exist on a continuous spectrum rather than the simplistic dichotomous distinction of activation. It appears that these subpopulations express varying numbers of M1 and M2 markers and activities. Some previous studies have identified populations of macrophages expressing both M1 and M2 markers in their research [,,]. In this study, it was not examined whether the macrophages present could express M1 and M2 markers simultaneously. Therefore, the possibility of the intermediate forms in the studied cleft affected lip tissues could not be excluded. Furthermore, perhaps the observed concurrent rise in both M1 and M2 phenotypes could, at least partially, be due to cells expressing both M1 and M2 markers.
In addition, our results also revealed a moderate positive correlation between M1 and TNF-α. This relationship between the two factors in cleft affected tissue seems possible, taking into account that both factors are by nature associated with inflammation, the cells of monocytic linage are the primary TNF-α producers, and TNF-α is vital for the long-term survival of macrophages. Usually, M1 activation is induced by very different factors, including TNF-α [,]. Other studies have also reported a positive correlation between TNF-α and M1 macrophages. For instance, in psoriatic patients, the research data indicated a preferential M1 polarization. On the other hand, after administration of a TNF-α inhibitor (adalimumab), the research team observed a restored M1/M2 ratio []. Similarly, in a study, in which authors evaluated the capacity of the Androctonus australis hector venom to induce the expression of M1 or M2 markers in adipose tissue, TNF-α modulated macrophage polarization towards the M1 phenotype []. In steroid-induced osteonecrosis, a high TNF-α activity alongside M1 dominance in the necrotic zone led to disease progression [].
In our patients, a weak correlation between M2 and TNF-α in cleft affected lip tissue was observed. Even though M2 macrophages are usually associated with the secretion of anti-inflammatory cytokines, studies show that they are also able to produce pro-inflammatory cytokines—for instance, TNF-α—hence a weak positive correlation []. This type of correlation is further supported by other authors, who suggested that some TNF-α induction is necessary for the elicitation of protective M2 responses in the brain []. Interestingly, a positive correlation between TNF-α and M2 was also observed in a study concerning a possible treatment option for periodontitis. Preconditioning of gingival tissue-derived mesenchymal stem cells with TNF-α increased the number of exosomes secreted as well as improved the exosomal expression of CD73; thus, it induced M2 polarization. Moreover, the results suggested that due to TNF-α preconditioning, the secreted exosomes were capable of converting M1 to M2, hence improving the wound healing capacity []. Although TNF-α is a potent pro-inflammatory agent and M2 an anti-inflammatory macrophage, a negative correlation between the two factors is more likely to exist. In addition to all the above-mentioned studies, in which TNF-α and M1positively correlated, a decrease in M2 but a rise in TNF-α was observed in sepsis-induces acute kidney injury in male rats [].
Overall, the data we presented indicate that in cleft affected tissue, not only the M1 levels are altered but the M1/M2 ratio also changes. However, the correlation between M1 and M2 could indicate a protective mechanism that helps to avoid an overzealous inflammation.
Our study had some limitations. Even though the macrophage ratio has been studied in other pathologies, to our knowledge, this was the first study in which the M1/M2 ratio in orofacial cleft affected tissue, particularly cleft lip tissue samples, was examined. Therefore, for instance, a comparison of results is not possible. Moreover, the relatively small sample size of the study and control groups may interfere with the general applicability of our findings. Furthermore, in our study, we only used one method, immunohistochemistry. Perhaps if we had combined different methods, such as immunohistochemistry with ELISA or flow cytometry (depending on the factor of interest), the results would have been more meaningful. In our case, the amount of tissue received for the study depended on how much of the tissue had not been used to correct the cleft. Therefore, unfortunately, the usage of two or more methods was not possible due to an insufficient amount of tissue sample.
Moving further, for future studies, we recommend including and examining not only M1 and M2 appearance and distribution in cleft affected tissue but also their intermediate forms. Moreover, we believe that identifying genes and transcription factors involved in cleft morphopathogenesis and analysing the results together with our observations could reveal potential tissue endotypes.
5. Conclusions
An increase in M1 and their difference in the distribution between the patients’ group and control alongside the positive correlation between M1 and TNF-α suggested a more pro-inflammatory/inflammatory environment in the cleft affected lip tissue.
The moderate positive correlation between M1 and M2 as well as M1 and TNF-α proved a persistent elevation of the protective mechanisms parallel to the increasing tissue inflammation.
Author Contributions
Conceptualization, M.P.; methodology, M.P.; software, J.G.; validation, M.P.; formal analysis, J.G.; investigation, J.G.; resources, M.P.; data curation, M.P.; writing—original draft preparation, J.G.; writing—review and editing, M.P., J.G.; visualization, J.G.; supervision, M.P.; project administration, M.P.; funding acquisition, M.P. All authors have read and agreed to the published version of the manuscript.
Funding
This research was funded by Riga Stradins University, Project 5-1/384/2020 “The complex research on the interrelation between tissue remodelling, tissue phenotype, and inflammation in most common craniofacial anomalies in Latvia”. Tissue samples were provided by Professor Ilze Akota.
Institutional Review Board Statement
The study was conducted according to the guidelines of the Declaration of Helsinki and approved by the Ethical Committee of Riga Stradins University (22 May 2003; 17 January 2013; 5/25 June 2018).
Informed Consent Statement
Informed consent was obtained from all subjects involved in the study.
Data Availability Statement
The data used and/or analysed in this study are presented in the results section of the present research.
Acknowledgments
The authors would like to thank Ilze Akota for providing the material. The kind support of Riga Stradins University is highly acknowledged.
Conflicts of Interest
The authors declare no conflict of interest.
References
- Sadler, T.W. Langman’s Medical Embryology, 12th ed.; Wolters Kluwer Health; Lippincott Williams & Wilkins: Philadelphia, PA, USA, 2012; pp. 275–282. [Google Scholar]
- Chigurupati, R.; Heggie, A.; Bonanthaya, K. Cleft Lip and Palate: An Overview. In Oral and Maxillofacial Surgery, 1st ed.; Chapter 45; Kahnberg, K.E., Ed.; Wiley-Blackwell: Chichester, UK, 2010; pp. 945–948. [Google Scholar]
- Moreno, L.M.; Arcos-Burgos, M.; Marazita, M.L.; Krahn, K.; Maher, B.S.; Cooper, M.E.; Valencia-Ramirez, C.R.; Lidral, A.C. Genetic analysis of candidate loci in non-syndromic cleft lip families from antioquia-Colombia and Ohio. Am. J. Med. Genet. 2004, 125A, 135–144. [Google Scholar] [CrossRef] [PubMed]
- Costa, B.; Lima, J.E.D.; Gomide, M.R.; Rosa, O.P.D. Clinical and microbiological evaluation of the periodontal status of children with unilateral complete cleft lip and palate. Cleft Palate Craniofacial J. 2003, 40, 585–589. [Google Scholar] [CrossRef] [PubMed]
- Chen, Y.N.; Hu, M.R.; Wang, L.; Chen, W.D. Macrophage M1/M2 polarization. Eur. J. Pharmacol. 2020, 877, 173090. [Google Scholar] [CrossRef]
- Hughes, C.E.; Benson, R.A.; Bedaj, M.; Maffia, P. Antigen-Presenting Cells and Antigen Presentation in Tertiary Lymphoid Organs. Front. Immunol. 2016, 7, 481. [Google Scholar] [CrossRef] [PubMed]
- Mills, C.D. M1 and M2 Macrophages: Oracles of Health and Disease. Crit. Rev. Immunol. 2012, 32, 463–488. [Google Scholar] [CrossRef]
- Xu, W.; Zhao, X.W.; Daha, M.R.; van Kooten, C. Reversible differentiation of pro- and anti-inflammatory macrophages. Mol. Immunol. 2013, 53, 179–186. [Google Scholar] [CrossRef]
- Cohen, H.B.; Mosser, D.M. Extrinsic and intrinsic control of macrophage inflammatory responses. J. Leukoc. Biol. 2013, 94, 913–919. [Google Scholar] [CrossRef]
- Atri, C.; Guerfali, F.Z.; Laouini, D. Role of Human Macrophage Polarization in Inflammation during Infectious Diseases. Int. J. Mol. Sci. 2018, 19, 1801. [Google Scholar] [CrossRef]
- Tarique, A.A.; Logan, J.; Thomas, E.; Holt, P.G.; Sly, P.D.; Fantino, E. Phenotypic, Functional, and Plasticity Features of Classical and Alternatively Activated Human Macrophages. Am. J. Respir. Cell Mol. Biol. 2015, 53, 676–688. [Google Scholar] [CrossRef]
- Iqbal, S.; Kumar, A. Characterization of In vitro Generated Human Polarized Macrophages. J. Clin. Cell. Immunol. 2015, 6, 380. [Google Scholar] [CrossRef]
- Huang, X.; Li, Y.; Fu, M.G.; Xin, H.B. Polarizing Macrophages In Vitro. Methods Mol. Biol. 2018, 1784, 119–126. [Google Scholar] [CrossRef]
- Ley, K. M1 Means Kill; M2 Means Heal. J. Immunol. 2017, 199, 2191–2193. [Google Scholar] [CrossRef]
- Madore, A.M.; Perron, S.; Turmel, V.; Laviolette, M.; Bissonnette, E.Y.; Laprise, C. Alveolar macrophages in allergic asthma: An expression signature characterized by heat shock protein pathways. Hum. Immunol. 2010, 71, 144–150. [Google Scholar] [CrossRef]
- Stoger, J.L.; Gijbels, M.J.J.; van der Velden, S.; Manca, M.; van der Loos, C.M.; Biessen, E.A.L.; Daemen, M.J.A.P.; Lutgens, E.; de Winther, M.P.J. Distribution of macrophage polarization markers in human atherosclerosis. Atherosclerosis 2012, 225, 461–468. [Google Scholar] [CrossRef]
- Wu, J.J.; Xie, H.Y.; Yao, S.Z.; Liang, Y.C. Macrophage and nerve interaction in endometriosis. J. Neuroinflamm. 2017, 14, 53. [Google Scholar] [CrossRef]
- Fukui, S.; Iwamoto, N.; Takatani, A.; Igawa, T.; Shimizu, T.; Umeda, M.; Nishino, A.; Horai, Y.; Hirai, Y.; Koga, T.; et al. M1 and M2 Monocytes in Rheumatoid Arthritis: A Contribution of Imbalance of M1/M2 Monocytes to Osteoclastogenesis. Front. Immunol. 2018, 8, 1958. [Google Scholar] [CrossRef]
- Zelova, H.; Hosek, J. TNF-alpha signalling and inflammation: Interactions between old acquaintances. Inflamm. Res. 2013, 62, 641–651. [Google Scholar] [CrossRef]
- Horiuchi, T.; Mitoma, H.; Harashima, S.; Tsukamoto, H.; Shimoda, T. Transmembrane TNF-alpha: Structure, function and interaction with anti-TNF agents. Rheumatology 2010, 49, 1215–1228. [Google Scholar] [CrossRef]
- Parameswaran, N.; Patial, S. Tumor Necrosis Factor-a Signaling in Macrophages. Crit. Rev. Eukaryot. Gene Expr. 2010, 20, 87–103. [Google Scholar] [CrossRef]
- Smane, L.; Pilmane, M.; Akota, I. Local expression of inflammatory cytokines in the facial tissue of children with a cleft lip and palate. Pap. Anthropol. 2012, 21, 264–275. [Google Scholar] [CrossRef][Green Version]
- Pilmane, M.; Sidhoma, E.; Akota, I.; Kazoka, D. Characterization of Cytokines and Proliferation Marker Ki67 in Cleft Affected Lip Tissue. Med. Lith. 2019, 55, 518. [Google Scholar] [CrossRef]
- Pilmane, M.; Rumba, I.; Sundler, F.; Luts, A. Patterns of distribution and occurrence of neuroendocrine elements in lungs of humans with chronic lung disease. Proc. Latv. Acad. Sci. 1998, 52, 144–152. [Google Scholar]
- Vitenberga, Z.; Pilmane, M.; Babjoniseva, A. The evaluation of inflammatory, anti-inflammatory and regulatory factors contributing to the pathogenesis of COPD in airways. Pathol. Res. Pract. 2019, 215, 97–105. [Google Scholar] [CrossRef]
- Papathanasiou, E.; Trotman, C.A.; Scott, A.R.; Van Dyke, T.E. Current and Emerging Treatments for Postsurgical Cleft Lip Scarring: Effectiveness and Mechanisms. J. Dent. Res. 2017, 96, 1370–1377. [Google Scholar] [CrossRef]
- Bokhout, B.; Hofman, F.X.W.M.; van Limbeek, J.; Kramer, G.J.C.; PrahlAndersen, B. Incidence of dental caries in the primary dentition in children with a cleft lip and/or palate. Caries Res. 1997, 31, 8–12. [Google Scholar] [CrossRef]
- Groeger, S.; Meyle, J. Oral Mucosal Epithelial Cells. Front. Immunol. 2019, 10, 208. [Google Scholar] [CrossRef]
- Pilmane, M.; Jain, N.; Jain, S.; Akota, I.; Kroica, J. Quantification of Cytokines in Lip Tissue from Infants Affected by Congenital Cleft Lip and Palate. Children 2021, 8, 140. [Google Scholar] [CrossRef]
- Peng, H.; Nickell, C.R.G.; Chen, K.Y.; McClain, J.A.; Nixon, K. Increased expression of M1 and M2 phenotypic markers in isolated microglia after four-day binge alcohol exposure in male rats. Alcohol 2017, 62, 29–40. [Google Scholar] [CrossRef] [PubMed]
- Zhou, Y.D.; Yoshida, S.; Kubo, Y.; Yoshimura, T.; Kobayashi, Y.; Nakama, T.; Yamaguchi, M.; Ishikawa, K.; Oshima, Y.; Ishibashi, T. Different distributions of M1 and M2 macrophages in a mouse model of laser-induced choroidal neovascularization. Mol. Med. Rep. 2017, 15, 3949–3956. [Google Scholar] [CrossRef] [PubMed]
- Almubarak, A.; Tanagala, K.K.K.; Papapanou, P.N.; Lalla, E.; Momen-Heravi, F. Disruption of Monocyte and Macrophage Homeostasis in Periodontitis. Front. Immunol. 2020, 11, 330. [Google Scholar] [CrossRef] [PubMed]
- Galarraga-Vinueza, M.E.; Obreja, K.; Ramanauskaite, A.; Magini, R.; Begic, A.; Sader, R.; Schwarz, F. Macrophage polarization in peri-implantitis lesions. Clin. Oral Investig. 2021, 25, 2335–2344. [Google Scholar] [CrossRef]
- He, S.Y.; Xie, L.H.; Lu, J.J.; Sun, S.H. Characteristics and potential role of M2 macrophages in COPD. Int. J. Chronic Obstruct. Pulmon. Dis. 2017, 12, 3029–3039. [Google Scholar] [CrossRef]
- Zhou, T.; Huang, Z.J.; Sun, X.W.; Zhu, X.W.; Zhou, L.L.; Li, M.; Cheng, B.; Liu, X.L.; He, C. Microglia Polarization with M1/M2 Phenotype Changes in rd1 Mouse Model of Retinal Degeneration. Front. Neuroanat. 2017, 11, 77. [Google Scholar] [CrossRef]
- Tada, S.; Okuno, T.; Hitoshi, Y.; Yasui, T.; Honorat, J.A.; Takata, K.; Koda, T.; Shimagami, H.; Choong, C.J.; Namba, A.; et al. Partial suppression of M1 microglia by Janus kinase 2 inhibitor does not protect against neurodegeneration in animal models of amyotrophic lateral sclerosis. J. Neuroinflamm. 2014, 11, 179. [Google Scholar] [CrossRef][Green Version]
- Knudsen, N.H.; Lee, C.H. Identity Crisis: CD301b(+) Mononuclear Phagocytes Blur the M1-M2 Macrophage Line. Immunity 2016, 45, 461–463. [Google Scholar] [CrossRef]
- Roszer, T. Understanding the Mysterious M2 Macrophage through Activation Markers and Effector Mechanisms. Mediat. Inflamm. 2015, 2015, 816460. [Google Scholar] [CrossRef]
- Lin, S.H.; Chuang, H.Y.; Ho, J.C.; Lee, C.H.; Hsiao, C.C. Treatment with TNF-alpha inhibitor rectifies M1 macrophage polarization from blood CD14+monocytes in patients with psoriasis independent of STAT1 and IRF-1 activation. J. Dermatol. Sci. 2018, 91, 276–284. [Google Scholar] [CrossRef]
- Ait-Lounis, A.; Laraba-Djebari, F. TNF-alpha modulates adipose macrophage polarization to M1 phenotype in response to scorpion venom. Inflamm. Res. 2015, 64, 929–936. [Google Scholar] [CrossRef]
- Wu, X.H.; Xu, W.H.; Feng, X.B.; He, Y.; Liu, X.Z.; Gao, Y.; Yang, S.H.; Shao, Z.W.; Yang, C.; Ye, Z.W. TNF-a mediated inflammatory macrophage polarization contributes to the pathogenesis of steroid-induced osteonecrosis in mice. Int. J. Immunopathol. Pharmacol. 2015, 28, 351–361. [Google Scholar] [CrossRef]
- Nakao, Y.; Fukuda, T.; Zhang, Q.Z.; Sanui, T.; Shinjo, T.; Kou, X.X.; Chen, C.; Liu, D.W.; Watanabe, Y.; Hayashi, C.; et al. Exosomes from TNF-alpha-treated human gingiva-derived MSCs enhance M2 macrophage polarization and inhibit periodontal bone loss. Acta Biomater. 2021, 122, 306–324. [Google Scholar] [CrossRef]
- Li, X.; Mu, G.H.; Song, C.M.; Zhou, L.L.; He, L.; Jin, Q.; Lu, Z.Q. Role of M2 Macrophages in Sepsis-Induced Acute Kidney Injury. Shock 2018, 50, 233–239. [Google Scholar] [CrossRef]
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).