Comparative Assessment of Health Systems Resilience: A Cross-Country Analysis Using Key Performance Indicators
Abstract
1. Introduction
1.1. Current Pressures and the “Black Swan Era” on Healthcare Systems
1.2. Defining and Conceptualizing Health Systems Resilience (HSR)
1.3. Methodologies for Assessing HSR
1.4. Key Determinants of HSR
2. Materials and Methods
2.1. Understanding HSR Through Efficiency Analysis
2.2. Dataset
2.3. Statistical Analysis
3. Results
3.1. Descriptive Statistics
3.2. Correlation Coefficients
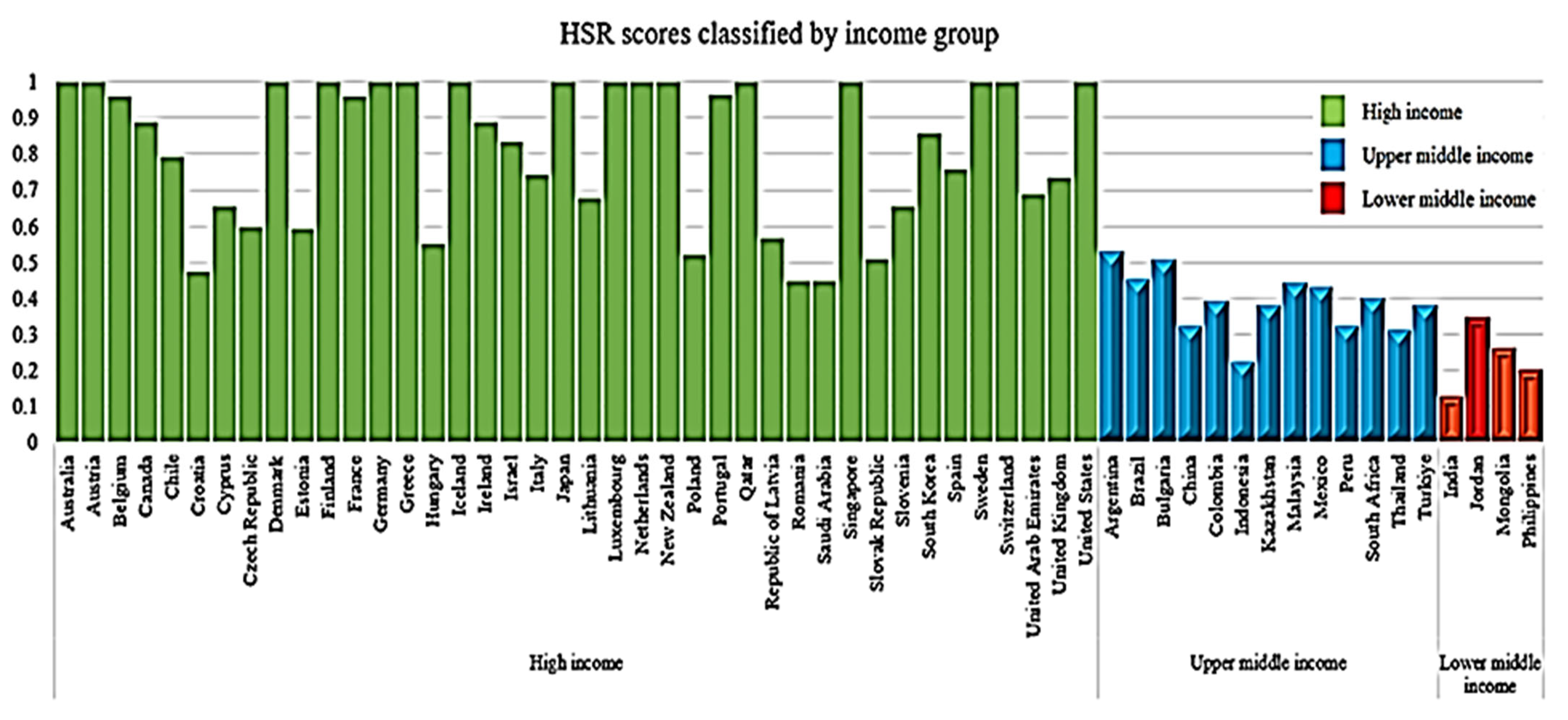
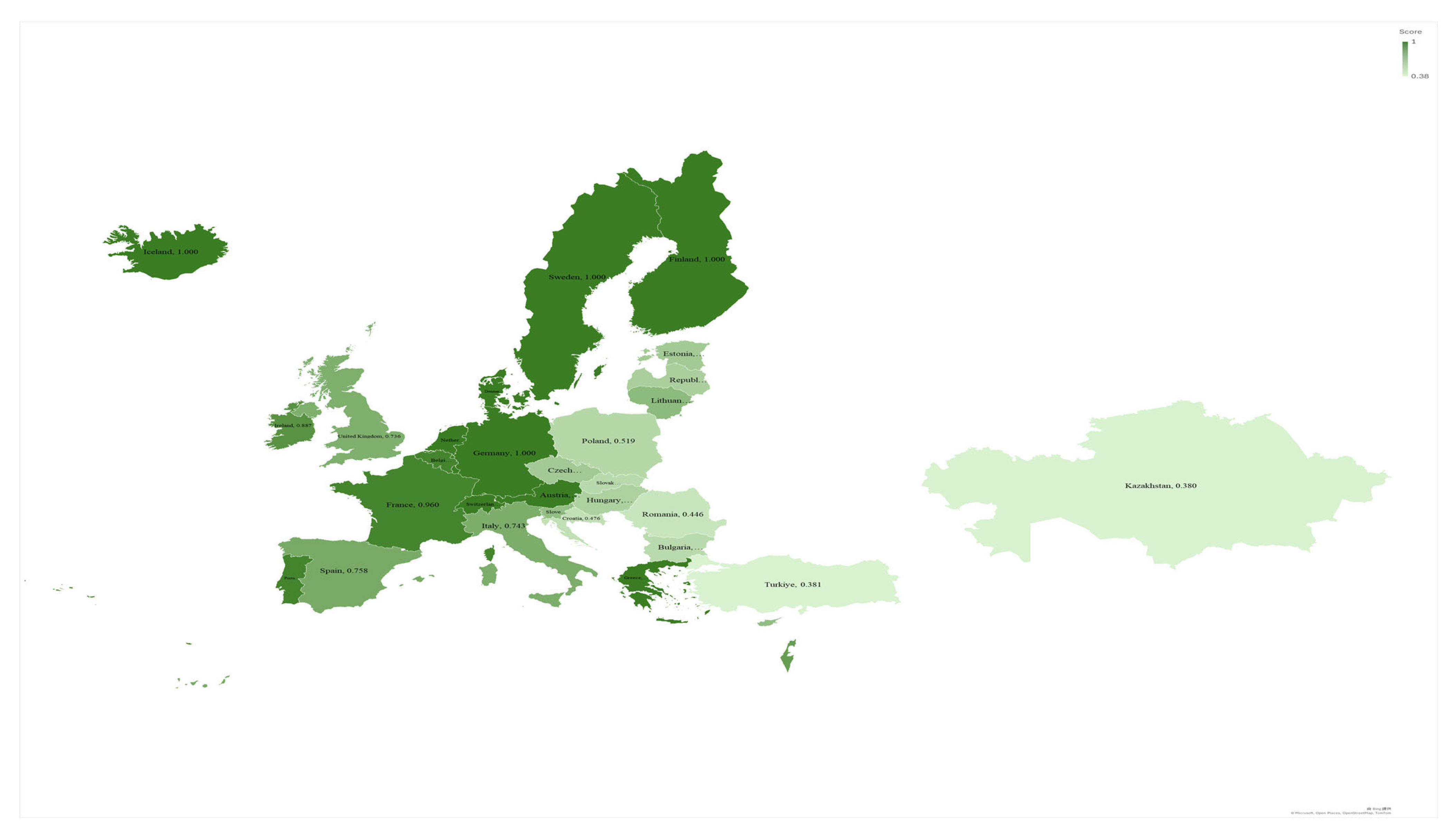
3.3. Efficiency Scores of HSR
3.4. Testing of Hypotheses
4. Discussion
4.1. Diverging HSR: Key National Drivers
4.2. Wealth, Equity, and Global HSR
4.3. Exploring the Applications and Limitations of Slack-Based Measure (SBM) Models
4.4. Reimagining Governance, Health Systems, and Economic Indices with WHO’s HSR Toolkits
5. Conclusions, Research Limitations, and Future Suggestions
5.1. Conclusions
5.2. Research Limitations and Future Suggestions
Author Contributions
Funding
Data Availability Statement
Acknowledgments
Conflicts of Interest
Appendix A
| Aspects | Indicators | Data | Source |
|---|---|---|---|
| Governance | Basic sanitation services | Population using at least basic sanitation services (%) | WHO |
| Basic drinking water services | Population using at least basic drinking water services (%) | WHO | |
| Clean fuels and tech. cooking | Access to clean fuels and technologies for cooking (% of population) | World Bank | |
| Government effectiveness | Government effectiveness: percentile rank | World Bank | |
| Regulatory quality | Regulatory quality: percentile rank | World Bank | |
| Voice and accountability | Voice and accountability: percentile rank | World Bank | |
| Health system | Number of inhabitants per physician | Number of inhabitants per physician | PRIDE/IMD |
| Number of inhabitants per nurse | Number of inhabitants per nurse | PRIDE/IMD | |
| Life expectancy at birth | Life expectancy at birth | WHO | |
| Health infra. meets society needs | Health infrastructure meet society needs presented on a scale of 0 to 10 | PRIDE/IMD | |
| UHC service coverage | Universal health coverage index for essential health services presented on a scale of 0 to 100 | World Bank | |
| Economic | GDP per capita | GDP per capita based on purchasing power parity, PPP | World Bank |
| Current health expenditure per capita | Current health expenditure per capita, PPP | World Bank | |
| Government health expenditure per capita | Domestic general government health expenditure per capita, PPP | World Bank | |
| Private health expenditure per capita | Domestic private health expenditure per capita, PPP | World Bank | |
| Pension funding | WCY executive survey pension fund adequacy rating based on an index from 0 to 10 | PRIDE/IMD | |
| Labor force participation | The labor force divided by the total working-age population aged 15 to 64 | World Bank |
Appendix B
| Year | U-Value | p-Value |
|---|---|---|
| 2016 | 9.00 *** | <0.0001 |
| 2017 | 10.00 *** | <0.0001 |
| 2018 | 9.00 *** | <0.0001 |
| 2019 | 2.00 *** | <0.0001 |
| 2020 | 2.00 ** | <0.0001 |
Appendix C
| Year | U-Value | p-Value |
|---|---|---|
| 2016 | 211.00 *** | 0.0033 |
| 2017 | 249.00 ** | 0.0116 |
| 2018 | 230.50 *** | 0.0049 |
| 2019 | 235.50 ** | 0.0174 |
| 2020 | 230.00 ** | 0.0139 |
Appendix D
| Year | U-Value | p-Value |
|---|---|---|
| 2016 | 54.00 *** | <0.0001 |
| 2017 | 28.00 *** | <0.0001 |
| 2018 | 60.00 *** | <0.0001 |
| 2019 | 43.00 *** | <0.0001 |
| 2020 | 134.00 *** | 0.001 |
Appendix E
| Year | U-Value | p-Value |
|---|---|---|
| 2016 | 3.00 *** | <0.0001 |
| 2017 | 3.00 *** | <0.0001 |
| 2018 | 9.00 *** | <0.0001 |
| 2019 | 2.00 *** | <0.0001 |
| 2020 | 23.00 *** | <0.0001 |
Appendix F
| Year | U-Value | p-Value |
|---|---|---|
| 2016 | 8.00 *** | <0.0001 |
| 2017 | 9.00 *** | <0.0001 |
| 2018 | 17.00 *** | <0.0001 |
| 2019 | 13.00 *** | <0.0001 |
| 2020 | 26.00 *** | <0.0001 |
Appendix G
| Country | Basic Sanitation Services | Basic Drinking Water Services | Clean Fuels and Tech. Cooking | Government Effectiveness | Regulatory Quality | Voice and Accountability |
|---|---|---|---|---|---|---|
| Argentina | 0.971 | 0.998 | 1.000 | 0.538 | 0.412 | 0.663 |
| Australia | 1.000 | 1.000 | 1.000 | 1.000 | 1.000 | 1.000 |
| Austria | 1.000 | 1.000 | 1.000 | 1.000 | 1.000 | 1.000 |
| Belgium | 1.000 | 1.000 | 1.000 | 0.982 | 0.990 | 0.989 |
| Brazil | 0.898 | 1.000 | 0.971 | 0.396 | 0.488 | 0.612 |
| Bulgaria | 0.867 | 1.000 | 0.893 | 0.569 | 0.763 | 0.611 |
| Canada | 0.996 | 0.995 | 1.000 | 0.989 | 0.994 | 0.994 |
| Chile | 1.000 | 0.999 | 1.000 | 0.875 | 0.913 | 0.932 |
| China | 0.948 | 1.000 | 0.795 | 0.739 | 0.476 | 0.078 |
| Colombia | 0.945 | 1.000 | 0.951 | 0.529 | 0.677 | 0.544 |
| Croatia | 0.962 | 1.000 | 1.000 | 0.700 | 0.691 | 0.637 |
| Cyprus | 0.995 | 0.998 | 1.000 | 0.783 | 0.836 | 0.815 |
| Czech Republic | 0.992 | 0.999 | 1.000 | 0.799 | 0.891 | 0.788 |
| Denmark | 1.000 | 1.000 | 1.000 | 1.000 | 1.000 | 1.000 |
| Estonia | 0.992 | 1.000 | 1.000 | 0.847 | 0.966 | 0.903 |
| Finland | 1.000 | 1.000 | 1.000 | 1.000 | 1.000 | 1.000 |
| France | 0.998 | 1.000 | 1.000 | 0.982 | 0.981 | 0.969 |
| Germany | 1.000 | 1.000 | 1.000 | 1.000 | 1.000 | 1.000 |
| Greece | 1.000 | 1.000 | 1.000 | 1.000 | 1.000 | 1.000 |
| Hungary | 0.981 | 1.000 | 1.000 | 0.691 | 0.733 | 0.621 |
| Iceland | 1.000 | 1.000 | 1.000 | 1.000 | 1.000 | 1.000 |
| India | 0.669 | 0.912 | 0.598 | 0.657 | 0.490 | 0.707 |
| Indonesia | 0.844 | 0.964 | 0.826 | 0.636 | 0.621 | 0.615 |
| Ireland | 0.923 | 0.969 | 1.000 | 0.930 | 0.980 | 0.960 |
| Israel | 1.000 | 1.000 | 1.000 | 0.930 | 0.954 | 0.842 |
| Italy | 1.000 | 1.000 | 1.000 | 0.755 | 0.806 | 0.856 |
| Japan | 1.000 | 1.000 | 1.000 | 1.000 | 1.000 | 1.000 |
| Jordan | 0.976 | 0.992 | 1.000 | 0.588 | 0.616 | 0.307 |
| Kazakhstan | 1.000 | 0.974 | 0.949 | 0.531 | 0.604 | 0.152 |
| Lithuania | 0.933 | 0.977 | 1.000 | 0.828 | 0.877 | 0.812 |
| Luxembourg | 1.000 | 1.000 | 1.000 | 1.000 | 1.000 | 1.000 |
| Malaysia | 0.987 | 1.000 | 0.989 | 0.827 | 0.781 | 0.416 |
| Mexico | 0.914 | 1.000 | 0.859 | 0.479 | 0.615 | 0.492 |
| Mongolia | 0.778 | 0.943 | 0.568 | 0.507 | 0.621 | 0.694 |
| The Netherlands | 1.000 | 1.000 | 1.000 | 1.000 | 1.000 | 1.000 |
| New Zealand | 1.000 | 1.000 | 1.000 | 1.000 | 1.000 | 1.000 |
| Peru | 0.800 | 0.970 | 0.855 | 0.461 | 0.746 | 0.610 |
| Philippines | 0.849 | 0.988 | 0.480 | 0.623 | 0.673 | 0.609 |
| Poland | 0.989 | 0.926 | 1.000 | 0.707 | 0.813 | 0.720 |
| Portugal | 0.999 | 0.998 | 1.000 | 0.983 | 0.964 | 0.983 |
| Qatar | 1.000 | 1.000 | 1.000 | 1.000 | 1.000 | 1.000 |
| Republic of Latvia | 0.924 | 0.987 | 1.000 | 0.794 | 0.867 | 0.751 |
| Romania | 0.858 | 1.000 | 0.872 | 0.463 | 0.694 | 0.668 |
| Saudi Arabia | 0.954 | 0.987 | 1.000 | 0.631 | 0.525 | 0.057 |
| Singapore | 1.000 | 1.000 | 1.000 | 1.000 | 1.000 | 1.000 |
| Slovak Republic | 0.976 | 0.998 | 1.000 | 0.727 | 0.801 | 0.769 |
| Slovenia | 0.986 | 0.995 | 1.000 | 0.838 | 0.776 | 0.808 |
| South Africa | 0.798 | 1.000 | 0.919 | 0.616 | 0.623 | 0.762 |
| South Korea | 1.000 | 0.998 | 1.000 | 0.928 | 0.941 | 0.890 |
| Spain | 1.000 | 0.999 | 1.000 | 0.855 | 0.852 | 0.870 |
| Sweden | 1.000 | 1.000 | 1.000 | 1.000 | 1.000 | 1.000 |
| Switzerland | 1.000 | 1.000 | 1.000 | 1.000 | 1.000 | 1.000 |
| Thailand | 0.985 | 1.000 | 0.820 | 0.658 | 0.568 | 0.246 |
| Turkiye | 1.000 | 0.985 | 0.969 | 0.524 | 0.583 | 0.271 |
| United Arab Emirates | 0.994 | 1.000 | 1.000 | 0.921 | 0.871 | 0.349 |
| United Kingdom | 0.996 | 1.000 | 1.000 | 0.948 | 0.985 | 0.955 |
| United States | 1.000 | 1.000 | 1.000 | 1.000 | 1.000 | 1.000 |
| Indicator’s average output efficiency | 0.959 | 0.992 | 0.953 | 0.803 | 0.826 | 0.760 |
| Total average output efficiency of the governance | 0.882 | |||||
Appendix H
| Country | Number of Inhabitants per Physician | Number of Inhabitants per Nurse | Life Expectancy at Birth | Health Infrastructure Meets Society Needs | UHC Service Coverage |
|---|---|---|---|---|---|
| Argentina | 0.922 | 0.203 | 0.920 | 0.515 | 0.914 |
| Australia | 1.000 | 1.000 | 1.000 | 1.000 | 1.000 |
| Austria | 1.000 | 1.000 | 1.000 | 1.000 | 1.000 |
| Belgium | 0.944 | 0.952 | 0.998 | 1.000 | 1.000 |
| Brazil | 0.507 | 0.560 | 0.907 | 0.244 | 0.960 |
| Bulgaria | 0.949 | 0.251 | 0.911 | 0.340 | - |
| Canada | 0.763 | 0.839 | 0.998 | 0.925 | 1.000 |
| Chile | 0.851 | 0.500 | 0.976 | 0.743 | 0.981 |
| China | 0.563 | 0.157 | 0.983 | 0.643 | 0.982 |
| Colombia | 0.495 | 0.075 | 0.950 | 0.306 | 0.962 |
| Croatia | 0.789 | 0.376 | 0.938 | 0.517 | 0.924 |
| Cyprus | 0.948 | 0.304 | 0.970 | 0.537 | 0.942 |
| Czech Republic | 0.959 | 0.487 | 0.949 | 0.772 | 0.971 |
| Denmark | 1.000 | 1.000 | 1.000 | 1.000 | 1.000 |
| Estonia | 0.799 | 0.353 | 0.938 | 0.643 | 0.913 |
| Finland | 1.000 | 1.000 | 1.000 | 1.000 | 1.000 |
| France | 0.944 | 0.950 | 1.000 | 0.973 | 1.000 |
| Germany | 1.000 | 1.000 | 1.000 | 1.000 | 1.000 |
| Greece | 1.000 | 1.000 | 1.000 | 1.000 | 1.000 |
| Hungary | 0.779 | 0.372 | 0.914 | 0.329 | 0.919 |
| Iceland | 1.000 | 1.000 | 1.000 | 1.000 | 1.000 |
| India | 0.287 | 0.152 | 0.895 | 0.695 | 0.727 |
| Indonesia | 0.122 | 0.123 | 0.913 | 0.740 | 0.674 |
| Ireland | 0.907 | 0.899 | 0.997 | 0.592 | 0.950 |
| Israel | 0.849 | 0.714 | 0.998 | 0.825 | 1.000 |
| Italy | 0.961 | 0.477 | 0.996 | 0.813 | 0.988 |
| Japan | 1.000 | 1.000 | 1.000 | 1.000 | 1.000 |
| Jordan | 0.729 | 0.205 | 0.931 | 0.785 | 0.799 |
| Kazakhstan | 0.915 | 0.360 | 0.872 | 0.527 | 0.955 |
| Lithuania | 1.000 | 0.625 | 0.908 | 0.643 | 0.860 |
| Luxembourg | 1.000 | 1.000 | 1.000 | 1.000 | 1.000 |
| Malaysia | 0.472 | 0.203 | 0.943 | 0.879 | 0.928 |
| Mexico | 0.627 | 0.181 | 0.902 | 0.442 | 0.871 |
| Mongolia | 0.744 | 0.193 | 1.000 | 0.333 | 0.916 |
| The Netherlands | 1.000 | 1.000 | 1.000 | 1.000 | 1.000 |
| New Zealand | 1.000 | 1.000 | 1.000 | 1.000 | 1.000 |
| Peru | 0.585 | 0.159 | 0.960 | 0.286 | 0.907 |
| Philippines | 0.088 | 0.055 | 0.959 | 0.713 | 0.750 |
| Poland | 0.547 | 0.284 | 0.933 | 0.371 | 0.953 |
| Portugal | 1.000 | 0.971 | 0.997 | 0.958 | 1.000 |
| Qatar | 1.000 | 1.000 | 1.000 | 1.000 | 1.000 |
| Republic of Latvia | 0.751 | 0.252 | 0.904 | 0.444 | 0.878 |
| Romania | 0.690 | 0.408 | 0.909 | 0.308 | 0.913 |
| Saudi Arabia | 0.595 | 0.307 | 0.922 | 0.673 | 0.849 |
| Singapore | 1.000 | 1.000 | 1.000 | 1.000 | 1.000 |
| Slovak Republic | 0.809 | 0.324 | 0.926 | 0.356 | 0.965 |
| Slovenia | 0.721 | 0.571 | 0.971 | 0.565 | 0.977 |
| South Africa | 0.166 | 0.202 | 0.847 | 0.415 | 0.891 |
| South Korea | 0.817 | 0.762 | 0.998 | 0.924 | 1.000 |
| Spain | 0.963 | 0.497 | 0.996 | 0.938 | 0.999 |
| Sweden | 1.000 | 1.000 | 1.000 | 1.000 | 1.000 |
| Switzerland | 1.000 | 1.000 | 1.000 | 1.000 | 1.000 |
| Thailand | 0.136 | 0.215 | 0.964 | 0.837 | 0.950 |
| Turkiye | 0.426 | 0.124 | 0.942 | 0.757 | 0.911 |
| United Arab Emirates | 0.690 | 0.490 | 0.964 | 0.898 | 0.925 |
| United Kingdom | 0.665 | 0.535 | 0.985 | 0.698 | 0.994 |
| United States | 1.000 | 1.000 | 1.000 | 1.000 | 1.000 |
| Indicator’s average output efficiency | 0.780 | 0.573 | 0.963 | 0.735 | 0.946 |
| Total average output efficiency of the health systems | 0.799 | ||||
Appendix I
| Country | GDP per Capita | Current Health Expenditure per Capita | Government Health Expenditure per Capita | Private Health Expenditure per Capita | Pension Funding Adequacy Rating | Labor Force Participation |
|---|---|---|---|---|---|---|
| Argentina | 0.325 | 0.266 | 0.526 | 0.142 | 0.276 | 0.793 |
| Australia | 1.000 | 1.000 | 1.000 | 1.000 | 1.000 | 1.000 |
| Austria | 1.000 | 1.000 | 1.000 | 1.000 | 1.000 | 1.000 |
| Belgium | 0.970 | 0.957 | 1.000 | 0.887 | 0.912 | 0.972 |
| Brazil | 0.213 | 0.177 | 0.232 | 0.151 | 0.302 | 0.834 |
| Bulgaria | 0.308 | 0.194 | 0.345 | 0.126 | 0.344 | 0.831 |
| Canada | 0.832 | 0.871 | 1.000 | 0.707 | 1.000 | 0.987 |
| Chile | 0.653 | 0.659 | 0.641 | 0.771 | 0.901 | 0.875 |
| China | 0.231 | 0.104 | 0.181 | 0.067 | 0.660 | 0.946 |
| Colombia | 0.214 | 0.151 | 0.333 | 0.064 | 0.554 | 0.885 |
| Croatia | 0.401 | 0.240 | 0.610 | 0.063 | 0.286 | 0.793 |
| Cyprus | 0.580 | 0.351 | 0.584 | 0.230 | 0.574 | 0.869 |
| Czech Republic | 0.571 | 0.380 | 0.967 | 0.087 | 0.403 | 0.911 |
| Denmark | 1.000 | 1.000 | 1.000 | 1.000 | 1.000 | 1.000 |
| Estonia | 0.503 | 0.302 | 0.697 | 0.113 | 0.519 | 0.932 |
| Finland | 1.000 | 1.000 | 1.000 | 1.000 | 1.000 | 1.000 |
| France | 0.942 | 0.951 | 1.000 | 0.884 | 0.931 | 0.977 |
| Germany | 1.000 | 1.000 | 1.000 | 1.000 | 1.000 | 1.000 |
| Greece | 1.000 | 1.000 | 1.000 | 1.000 | 1.000 | 1.000 |
| Hungary | 0.445 | 0.260 | 0.555 | 0.119 | 0.480 | 0.854 |
| Iceland | 1.000 | 1.000 | 1.000 | 1.000 | 1.000 | 1.000 |
| India | 0.103 | 0.019 | 0.012 | 0.028 | 1.000 | 0.703 |
| Indonesia | 0.184 | 0.040 | 0.045 | 0.036 | 1.000 | 0.945 |
| Ireland | 0.998 | 0.873 | 1.000 | 0.672 | 0.692 | 0.947 |
| Israel | 0.784 | 0.678 | 0.760 | 0.582 | 0.960 | 0.931 |
| Italy | 0.689 | 0.573 | 1.000 | 0.345 | 0.689 | 0.828 |
| Japan | 1.000 | 1.000 | 1.000 | 1.000 | 1.000 | 1.000 |
| Jordan | 0.147 | 0.080 | 0.092 | 0.065 | 1.000 | 0.527 |
| Kazakhstan | 0.375 | 0.101 | 0.194 | 0.057 | 0.691 | 0.945 |
| Lithuania | 0.542 | 0.324 | 0.519 | 0.185 | 0.466 | 0.943 |
| Luxembourg | 1.000 | 1.000 | 1.000 | 1.000 | 1.000 | 1.000 |
| Malaysia | 0.400 | 0.126 | 0.184 | 0.094 | 1.000 | 0.860 |
| Mexico | 0.297 | 0.132 | 0.196 | 0.103 | 0.497 | 0.792 |
| Mongolia | 0.201 | 0.070 | 0.127 | 0.036 | 0.389 | 0.892 |
| The Netherlands | 1.000 | 1.000 | 1.000 | 1.000 | 1.000 | 1.000 |
| New Zealand | 1.000 | 1.000 | 1.000 | 1.000 | 1.000 | 1.000 |
| Peru | 0.190 | 0.084 | 0.156 | 0.047 | 0.711 | 1.000 |
| Philippines | 0.139 | 0.036 | 0.029 | 0.043 | 0.997 | 0.878 |
| Poland | 0.454 | 0.253 | 0.551 | 0.110 | 0.340 | 0.836 |
| Portugal | 0.914 | 0.901 | 0.899 | 0.903 | 0.919 | 0.989 |
| Qatar | 1.000 | 1.000 | 1.000 | 1.000 | 1.000 | 1.000 |
| Republic of Latvia | 0.430 | 0.238 | 0.436 | 0.142 | 0.610 | 0.928 |
| Romania | 0.406 | 0.198 | 0.486 | 0.060 | 0.400 | 0.804 |
| Saudi Arabia | 0.691 | 0.345 | 0.781 | 0.145 | 0.904 | 0.683 |
| Singapore | 1.000 | 1.000 | 1.000 | 1.000 | 1.000 | 1.000 |
| Slovak Republic | 0.448 | 0.265 | 0.653 | 0.080 | 0.339 | 0.864 |
| Slovenia | 0.540 | 0.402 | 0.900 | 0.165 | 0.538 | 0.880 |
| South Africa | 0.219 | 0.153 | 0.278 | 0.092 | 0.650 | 0.801 |
| South Korea | 0.838 | 0.750 | 0.879 | 0.691 | 0.845 | 0.929 |
| Spain | 0.679 | 0.587 | 0.922 | 0.379 | 0.541 | 0.913 |
| Sweden | 1.000 | 1.000 | 1.000 | 1.000 | 1.000 | 1.000 |
| Switzerland | 1.000 | 1.000 | 1.000 | 1.000 | 1.000 | 1.000 |
| Thailand | 0.264 | 0.079 | 0.142 | 0.038 | 0.885 | 0.950 |
| Turkiye | 0.410 | 0.147 | 0.355 | 0.048 | 0.630 | 0.686 |
| United Arab Emirates | 1.000 | 0.504 | 0.731 | 0.387 | 0.943 | 0.992 |
| United Kingdom | 0.756 | 0.667 | 1.000 | 0.276 | 0.691 | 0.959 |
| United States | 1.000 | 1.000 | 1.000 | 1.000 | 1.000 | 1.000 |
| Indicator’s average output efficiency | 0.637 | 0.535 | 0.667 | 0.460 | 0.763 | 0.910 |
| Total average output efficiency of the economic aspect | 0.662 | |||||
Appendix J
| Country | HSR Score Ranking | WCY Ranking 2020 | HAQ Index Ranking 2019 | Country | HSR Score Ranking | WCY Ranking 2020 | HAQ Index Ranking 2019 | Country | HSR Score Ranking | WCY Ranking 2020 | HAQ Index Ranking 2019 |
|---|---|---|---|---|---|---|---|---|---|---|---|
| Argentina | 36 | 62 | 47 | Hungary | 35 | 47 | 31 | Poland | 37 | 39 | 34 |
| Australia | 1 | 18 | 6 | Iceland | 1 | 21 | 1 | Portugal | 17 | 37 | 23 |
| Austria | 1 | 16 | 11 | India | 57 | 43 | 57 | Qatar | 1 | 14 | 32 |
| Belgium | 18 | 25 | 17 | Indonesia | 55 | 40 | 55 | Republic of Latvia | 34 | 41 | 38 |
| Brazil | 41 | 56 | 51 | Ireland | 20 | 12 | 7 | Romania | 43 | 51 | 37 |
| Bulgaria | 39 | 48 | 41 | Israel | 23 | 26 | 26 | Saudi Arabia | 42 | 24 | 43 |
| Canada | 21 | 8 | 4 | Italy | 26 | 44 | 9 | Singapore | 1 | 1 | 20 |
| Chile | 24 | 38 | 35 | Japan | 1 | 34 | 14 | Slovak Republic | 38 | 57 | 33 |
| China | 51 | 20 | 36 | Jordan | 50 | 58 | 40 | Slovenia | 31 | 35 | 12 |
| Colombia | 47 | 54 | 45 | Kazakhstan | 49 | 42 | 48 | South Africa | 46 | 59 | 54 |
| Croatia | 40 | 60 | 28 | Lithuania | 29 | 31 | 39 | South Korea | 22 | 23 | 18 |
| Cyprus | 30 | 30 | 19 | Luxembourg | 1 | 15 | 15 | Spain | 25 | 36 | 8 |
| Czech Republic | 32 | 33 | 27 | Malaysia | 44 | 27 | 50 | Sweden | 1 | 6 | 5 |
| Denmark | 1 | 2 | 22 | Mexico | 45 | 53 | 52 | Switzerland | 1 | 3 | 2 |
| Estonia | 33 | 28 | 30 | Mongolia | 54 | 61 | 53 | Thailand | 53 | 29 | 44 |
| Finland | 1 | 13 | 13 | The Netherlands | 1 | 4 | 3 | Turkiye | 48 | 46 | 42 |
| France | 19 | 32 | 10 | New Zealand | 1 | 22 | 21 | United Arab Emirates | 28 | 9 | 49 |
| Germany | 1 | 17 | 16 | Peru | 52 | 52 | 46 | United Kingdom | 27 | 19 | 25 |
| Greece | 1 | 49 | 24 | Philippines | 56 | 45 | 56 | United States | 1 | 10 | 29 |
Appendix K
| Output-Oriented Super SBM with Undesirable Items as Inputs | ||
|---|---|---|
| Country | Aggregate HSR Score | Rank |
| Greece | 1.048 | 1 |
| Finland | 1.038 | 2 |
| Switzerland | 1.016 | 3 |
| Austria | 1.008 | 4 |
| Luxembourg | 1.007 | 5 |
| Germany | 1.005 | 6 |
| Denmark | 1.004 | 7 |
| Sweden | 1.001 | 8 |
| Iceland | 0.898 | 10 |
| The Netherlands | 0.751 | 11 |
| Australia | 0.720 | 12 |
| United States | 0.651 | 14 |
| New Zealand | 0.516 | 21 |
| Singapore | 0.434 | 26 |
| Japan | 0.397 | 30 |
| Qatar | 0.294 | 38 |
| Portugal | 0.962 | 9 |
| Belgium | 0.550 | 19 |
| France | 0.530 | 20 |
| Ireland | 0.673 | 13 |
| Canada | 0.461 | 23 |
| South Korea | 0.363 | 33 |
| Israel | 0.480 | 22 |
| Chile | 0.319 | 37 |
| Spain | 0.596 | 15 |
| Italy | 0.572 | 16 |
| United Kingdom | 0.436 | 25 |
| United Arab Emirates | 0.338 | 35 |
| Lithuania | 0.568 | 17 |
| Cyprus | 0.555 | 18 |
| Slovenia | 0.424 | 27 |
| Czech Republic | 0.451 | 24 |
| Estonia | 0.410 | 28 |
| Republic of Latvia | 0.369 | 32 |
| Hungary | 0.354 | 34 |
| Argentina | 0.398 | 29 |
| Poland | 0.241 | 41 |
| Slovak Republic | 0.326 | 36 |
| Bulgaria | 0.376 | 31 |
| Croatia | 0.284 | 39 |
| Brazil | 0.194 | 44 |
| Saudi Arabia | 0.203 | 43 |
| Romania | 0.229 | 42 |
| Malaysia | 0.161 | 46 |
| Mexico | 0.188 | 45 |
| South Africa | 0.074 | 53 |
| Colombia | 0.155 | 47 |
| Türkiye | 0.124 | 52 |
| Kazakhstan | 0.241 | 40 |
| Jordan | 0.139 | 49 |
| China | 0.134 | 50 |
| Peru | 0.129 | 51 |
| Thailand | 0.039 | 54 |
| Mongolia | 0.140 | 48 |
| Indonesia | 0.016 | 56 |
| Philippines | 0.009 | 57 |
| India | 0.016 | 55 |
References
- Hadian, M.; Mozafari, M.; Mazaheri, E.; Jabbari, A. Challenges of the Health System in Preventing Non-Communicable Diseases; Systematized Review. Int. J. Prev. Med. 2021, 12, 71. [Google Scholar] [CrossRef] [PubMed]
- Bodor, K.; Micheu, M.M.; Keresztesi, Á.; Birsan, M.-V.; Nita, I.-A.; Bodor, Z.; Petres, S.; Korodi, A.; Szép, R. Effects of PM10 and Weather on Respiratory and Cardiovascular Diseases in the Ciuc Basin (Romanian Carpathians). Atmosphere 2021, 12, 289. [Google Scholar] [CrossRef]
- Ebi, K.L.; Bowen, K. Extreme events as sources of health vulnerability: Drought as an example. Weather Clim. Extrem. 2016, 11, 95–102. [Google Scholar] [CrossRef]
- Weilnhammer, V.; Schmid, J.; Mittermeier, I.; Schreiber, F.; Jiang, L.; Pastuhovic, V.; Herr, C.; Heinze, S. Extreme weather events in Europe and their health consequences—A systematic review. Int. J. Hyg. Environ. Health 2021, 233, 113688. [Google Scholar] [CrossRef]
- World Health Organization (WHO). Health Systems Resilience Toolkit: A WHO Global Public Health Good to Support Building and Strengthening of Sustainable Health Systems Resilience in Countries with Various Contexts; World Health Organization: Geneva, Switzerland, 2022. [Google Scholar]
- World Health Organization (WHO). Key Facts: Coronavirus Disease (COVID-19). 2023. Available online: https://www.who.int/news-room/fact-sheets/detail/coronavirus-disease-(covid-19) (accessed on 1 October 2023).
- BSI. BS 65000—Guidance on Organizational Resilience; B.s. Institution: London, UK, 2014. [Google Scholar]
- OECD. Ready for the Next Crisis? Investing in Health System Resilience; OECD: Paris, France, 2023. [Google Scholar] [CrossRef]
- Haldane, V.; De Foo, C.; Abdalla, S.M.; Jung, A.-S.; Tan, M.; Wu, S.; Chua, A.; Verma, M.; Shrestha, P.; Singh, S.; et al. Health systems resilience in managing the COVID-19 pandemic: Lessons from 28 countries. Nat. Med. 2021, 27, 964–980. [Google Scholar] [CrossRef]
- Thomas, S.; Sagan, A.; Larkin, J.; Cylus, J.; Figueras, J.; Karanikolos, M. Strengthening health systems resilience: Key concepts and strategies. In Policy Brief 36; European Observatory on Health Systems and Policies: Copenhagen, Denmark, 2020; p. 33. [Google Scholar]
- Turenne, C.P.; Gautier, L.; Degroote, S.; Guillard, E.; Chabrol, F.; Ridde, V. Conceptual analysis of health systems resilience: A scoping review. Soc. Sci. Med. 2019, 232, 168–180. [Google Scholar] [CrossRef]
- Hanefeld, J.; Mayhew, S.; Legido-Quigley, H.; Martineau, F.; Karanikolos, M.; Blanchet, K.; Liverani, M.; Yei Mokuwa, E.; McKay, G.; Balabanova, D. Towards an understanding of resilience: Responding to health systems shocks. Health Policy Plan. 2018, 33, 355–367. [Google Scholar] [CrossRef]
- Tone, K.; Tsutsui, M. Dynamic DEA: A slacks-based measure approach. Omega 2010, 38, 145–156. [Google Scholar] [CrossRef]
- Hu, J.-L.; Chang, T.-P. Total-factor energy efficiency and its extensions: Introduction, computation and application. Int. Ser. Oper. Res. Manag. Sci. 2016, 238, 45–69. [Google Scholar]
- Tone, K. A slacks-based measure of efficiency in data envelopment analysis. Eur. J. Oper. Res. 2001, 130, 498–509. [Google Scholar] [CrossRef]
- Huda, T.M.; Hayes, A.; Dibley, M.J. Examining horizontal inequity and social determinants of inequality in facility delivery services in three South Asian countries. J. Glob. Health 2018, 8, 010416. [Google Scholar] [CrossRef]
- Alamilla, S.G.; Cano, M.Á. COVID-19 and Adverse Social Determinants of Health. Behav. Med. 2022, 48, 67–71. [Google Scholar] [CrossRef]
- Stevens, G.W.J.M.; Buyukcan-Tetik, A.; Maes, M.; Weinberg, D.; Vermeulen, S.; Visser, K.; Finkenauer, C. Examining socioeconomic disparities in changes in adolescent mental health before and during different phases of the coronavirus disease 2019 pandemic. Stress Health J. Int. Soc. Investig. Stress 2022, 39, 169–181. [Google Scholar] [CrossRef]
- World Health Organization (WHO). Health Inequities and Their Causes. [Who.int/news-room/facts-in-pictures/detail]. 2018. Available online: https://www.who.int/news-room/facts-in-pictures/detail/health-inequities-and-their-causes (accessed on 17 March 2023).
- Saulnier, D.D.; Blanchet, K.; Canila, C.; Muñoz, D.C.; Zennaro, L.D.; de Savigny, D.; Durski, K.N.; Garcia, F.; Grimm, P.Y.; Kwamie, A.; et al. A health systems resilience research agenda: Moving from concept to practice. BMJ Glob. Health 2021, 6, e006779. [Google Scholar] [CrossRef] [PubMed]
- Fleming, P.; O’DOnoghue, C.; Almirall-Sanchez, A.; Mockler, D.; Keegan, C.; Cylus, J.; Sagan, A.; Thomas, S. Metrics and indicators used to assess health system resilience in response to shocks to health systems in high income countries—A systematic review. Health Policy 2022, 126, 1195–1205. [Google Scholar] [CrossRef] [PubMed]
- Peters, F.; Nusselder, W.J.; Reibling, N.; Wegner-Siegmundt, C.; Mackenbach, J.P. Quantifying the contribution of changes in healthcare expenditures and smoking to the reversal of the trend in life expectancy in the Netherlands. BMC Public Health 2015, 15, 1024. [Google Scholar] [CrossRef] [PubMed]
- Reynolds, M.M.; Avendano, M. Social policy expenditures and life expectancy in high-income countries. Am. J. Prev. Med. 2018, 54, 72–79. [Google Scholar] [CrossRef]
- Wu, K.-F.; Hu, J.-L.; Chiou, H. Degrees of shortage and uncovered ratios for long-term care in Taiwan’s regions: Evidence from dynamic dea. Int. J. Environ. Res. Public Health 2021, 18, 605. [Google Scholar] [CrossRef]
- Van Doorslaer, E.; Masseria, C.; Koolman, X. Inequalities in access to medical care by income in developed countries. Can. Med. Assoc. J. 2006, 174, 177–183. [Google Scholar] [CrossRef]
- Bíró, A.; Hajdu, T.; Kertesi, G.; Prinz, D. The Role of Place and Income in Life Expectancy Inequality: Evidence from Hungary; CERS-IE Working Papers; Hungarian Academy of Sciences: Budapest, Hungary, 2020. [Google Scholar]
- Bloom, D.E.; Canning, D. Commentary: The Preston Curve 30 years on: Still sparking fires. Int. J. Epidemiol. 2007, 36, 498–499. [Google Scholar] [CrossRef]
- Mackenbach, J.P.; Looman, C.W. Life expectancy and national income in Europe, 1900–2008: An update of Preston’s analysis. Int. J. Epidemiol. 2013, 42, 1100–1110. [Google Scholar] [CrossRef]
- Ho, J.Y.; Hendi, A.S. Recent trends in life expectancy across high income countries: Retrospective observational study. BMJ 2018, 362, k2562. [Google Scholar] [CrossRef]
- Stewart, F. Horizontal inequalities as a cause of conflict: A review of CRISE findings. In World Development Report; Word Bank: Washington, DC, USA, 2010. [Google Scholar]
- Khang, Y.-H.; Bahk, J.; Lim, D.; Kang, H.-Y.; Lim, H.-K.; Kim, Y.-Y.; Park, J.H. Trends in inequality in life expectancy at birth between 2004 and 2017 and projections for 2030 in Korea: Multiyear cross-sectional differences by income from national health insurance data. BMJ Open 2019, 9, e030683. [Google Scholar] [CrossRef]
- Preston, S.H. The changing relation between mortality and level of economic development. Popul. Stud. 1975, 29, 231–248. [Google Scholar] [CrossRef]
- Wu, T.Y.; Majeed, A.; Kuo, K.N. An overview of the healthcare system in Taiwan. Lond. J. Prim. Care 2010, 3, 115–119. [Google Scholar] [CrossRef] [PubMed]
- Wears, R.L.; Hollnagel, E.; Braithwaite, J. Resilient Health Care, Volume 2: The Resilience of Everyday Clinical Work; Ashgate Publishing, Ltd.: Farnham, UK, 2015; pp. 39–40. [Google Scholar]
- Tan, M.Z.Y.; Prager, G.; McClelland, A.; Dark, P. Healthcare resilience: A meta-narrative systematic review and synthesis of reviews. BMJ Open 2023, 13, e072136. [Google Scholar] [CrossRef] [PubMed]
- Waitzberg, R.; Pfundstein, I.; Maresso, A.; Rechel, B.; van Ginneken, E.; Quentin, W. Health system description and assessment: A scoping review of templates for systematic analyses. Health Res. Policy Syst. 2024, 22, 82. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization (WHO). Maternal, Newborn, Child and Adolescent Health and Aging Data; World Health Organization: Geneva, Switzerland, 2023. [Google Scholar]
- PRIDE. 2023, Science and Technology Policy Research and Information Center, National Applied Research Laboratories. Available online: https://pride.stpi.narl.org.tw/index/dashboard?type=INT_COMP&cdmId=15 (accessed on 17 October 2023).
- World Bank. Search & Share Development Data; World Bank: Washington, DC, USA, 2023. [Google Scholar]
- IMD. IMD World Competitiveness Ranking 2020: Showing Strength of Small Economies; IMD: Lausanne, Switzerland, 2020. [Google Scholar]
- Li, Y.; Cheng, W.; Wei, X. Measuring national economic resilience to the SARS and COVID-19 pandemics. Appl. Econ. 2023, 56, 6467–6482. [Google Scholar] [CrossRef]
- Lee, C.-T.; Hu, J.-L.; Kung, M.-H. Economic Resilience in the Early Stage of the COVID-19 Pandemic: An Across-Economy Comparison. Sustainability 2022, 14, 4609. [Google Scholar] [CrossRef]
- Chang, P.-L.; Hwang, S.-N.; Cheng, W.-Y. Using data envelopment analysis to measure the achievement and change of regional development in Taiwan. J. Environ. Manag. 1995, 43, 49–66. [Google Scholar] [CrossRef]
- Seiford, L.M.; Zhu, J. Context-dependent data envelopment analysis—Measuring attractiveness and progress. Omega 2003, 31, 397–408. [Google Scholar] [CrossRef]
- Mann, H.B.; Whitney, D.R. On a test of whether one of two random variables is stochastically larger than the other. Ann. Math. Stat. 1947, 18, 50–60. [Google Scholar] [CrossRef]
- Paschoalotto, M.A.C.; Lazzari, E.A.; Rocha, R.; Massuda, A.; Castro, M.C. Health systems resilience: Is it time to revisit resilience after COVID-19? Soc. Sci. Med. 2023, 320, 115716. [Google Scholar] [CrossRef] [PubMed]
- IHME. Global Burden of Disease Collaborative Network. Global Burden of Disease Study 2019 (GBD 2019) Healthcare Access and Quality Index 1990–2019; Institute for Health Metrics and Evaluation Seattle: Seattle, WA, USA, 2022. [Google Scholar]
- Nuzzo, J.B.; Bell, J.A.; Cameron, E.E. Suboptimal US Response to COVID-19 Despite Robust Capabilities and Resources. JAMA 2020, 324, 1391–1392. [Google Scholar] [CrossRef] [PubMed]
- George, J.D.; Fragkou, P.C.; Gkirmpa, A.M.; Tsangaris, G.; Hoffman, R.M.; Anagnostopoulos, A.K. The Experience of Greece as a Model to Contain COVID-19 Infection Spread. In Vivo 2021, 35, 1285. [Google Scholar] [CrossRef]
- Chang, M.C.; Baek, J.H.; Park, D. Lessons from South Korea Regarding the Early Stage of the COVID-19 Outbreak. Healthcare 2020, 8, 229. [Google Scholar] [CrossRef]
- Zanaa, A.; Paramita, S.A.; Erdenee, O.; Tsolmon, B.; Purevdagva, A.; Yamazaki, C.; Uchida, M.; Hamazaki, K. Childhood Tuberculosis in Mongolia: Trends and Estimates, 2010–2030. Tohoku J. Exp. Med. 2022, 257, 193–203. [Google Scholar] [CrossRef]
- Ghosh, A.; Nundy, S.; Mallick, T.K. How India is dealing with COVID-19 pandemic. Sens. Int. 2020, 1, 100021. [Google Scholar] [CrossRef]
- UNDESA. Transforming our World: The 2030 Agenda for Sustainable Development. In General Assembly Resolution A/RES/70/1; United Nations Department of Economic and Social Affairs (UNDESA): New York, NY, USA, 2015. [Google Scholar]
- Chen, C.-M. Super efficiencies or super inefficiencies? Insights from a joint computation model for slacks-based measures in DEA. Eur. J. Oper. Res. 2013, 226, 258–267. [Google Scholar] [CrossRef]
- Tone, K. A slacks-based measure of super-efficiency in data envelopment analysis. Eur. J. Oper. Res. 2002, 143, 32–41. [Google Scholar] [CrossRef]
- World Health Organization (WHO). Health system resilience indicators: An integrated package for measuring and monitoring health system resilience in countries. In Special Programme on Primary Health Care (PHC); World Health Organization: Geneva, Switzerland, 2024; ISBN 978-92-4-008898-6. [Google Scholar]

| Aspects | Index | Type | Mean | S.D. | Max. | Min. |
|---|---|---|---|---|---|---|
| Governance | Basic sanitation services | Desirable | 94.98 | 8.17 | 100.00 | 60.84 |
| Basic drinking water services | Desirable | 98.17 | 3.46 | 100.00 | 79.40 | |
| Clean fuels and tech. cooking | Desirable | 94.60 | 12.23 | 100.00 | 43.30 | |
| Government effectiveness | Desirable | 75.59 | 17.66 | 100.00 | 33.33 | |
| Regulatory quality | Desirable | 76.80 | 17.19 | 100.00 | 33.33 | |
| Voice and accountability | Desirable | 68.60 | 25.95 | 99.52 | 4.83 | |
| Health systems | Number of inhabitants per physician | Undesirable | 487.22 | 633.56 | 4394.09 | 161.62 |
| Number of inhabitants per nurse | Undesirable | 227.39 | 234.47 | 1671.14 | 47.06 | |
| Life expectancy at birth | Desirable | 78.80 | 4.06 | 85.00 | 65.00 | |
| Health infra. meets society needs | Desirable | 5.90 | 2.00 | 9.25 | 1.72 | |
| UHC service coverage | Desirable | 80.27 | 7.31 | 91.00 | 54.00 | |
| Economic | GDP per capita | Desirable | 39,148.72 | 22,557.76 | 116,283.70 | 5789.68 |
| Current health expenditure per capita | Desirable | 3236.36 | 2203.05 | 11,702.41 | 179.45 | |
| Government health expenditure per capita | Desirable | 2238.86 | 1580.44 | 6643.36 | 54.34 | |
| Private health expenditure per capita | Desirable | 992.76 | 952.01 | 5631.53 | 118.95 | |
| Pension funding adequacy rating | Desirable | 4.18 | 1.60 | 8.32 | 0.84 | |
| Labor force participation | Desirable | 72.48 | 8.42 | 89.21 | 40.68 |
| Variables | Basic Sanitation Services | Basic Drinking Water Services | Clean Fuels and Tech. Cooking | Government Effectiveness | Regulatory Quality | Voice and Accountability | Number of Inhabitants per Physician | Number of Inhabitants per Nurse | Life Expectancy at Birth | Health Infra. Meets Society Needs | UHC Service Coverage | GDP per Capita | Current Health Expenditure per Capita | Government Health Exp. per Capita | Private Health Exp. per Capita | Pension Funding Adequacy Rating | Labor Force Participation |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Basic sanitation services | 1 | ||||||||||||||||
| Basic drinking water services | 0.836 | 1 | |||||||||||||||
| Clean fuels and tech. cooking | 0.848 | 0.797 | 1 | ||||||||||||||
| Government effectiveness | 0.615 | 0.528 | 0.560 | 1 | |||||||||||||
| Regulatory quality | 0.567 | 0.507 | 0.580 | 0.882 | 1 | ||||||||||||
| Voice and accountability | 0.256 | 0.306 | 0.373 | 0.596 | 0.709 | 1 | |||||||||||
| Number of inhabitants per physician | −0.447 | −0.364 | −0.672 | −0.314 | −0.371 | −0.300 | 1 | ||||||||||
| Number of inhabitants per nurse | −0.496 | −0.432 | −0.697 | −0.506 | −0.494 | −0.392 | 0.800 | 1 | |||||||||
| Life expectancy at birth | 0.745 | 0.659 | 0.646 | 0.766 | 0.734 | 0.511 | −0.456 | −0.520 | 1 | ||||||||
| Health infra. meets society needs | 0.594 | 0.489 | 0.433 | 0.764 | 0.597 | 0.285 | −0.175 | −0.385 | 0.671 | 1 | |||||||
| UHC service coverage | 0.729 | 0.639 | 0.693 | 0.648 | 0.655 | 0.524 | −0.603 | −0.659 | 0.799 | 0.466 | 1 | ||||||
| GDP per capita | 0.502 | 0.453 | 0.513 | 0.718 | 0.693 | 0.317 | −0.348 | −0.513 | 0.655 | 0.614 | 0.512 | 1 | |||||
| Current health expenditure per capita | 0.527 | 0.489 | 0.524 | 0.782 | 0.773 | 0.649 | −0.372 | −0.541 | 0.697 | 0.625 | 0.657 | 0.743 | 1 | ||||
| Government health exp. per capita | 0.521 | 0.485 | 0.524 | 0.775 | 0.778 | 0.682 | −0.375 | −0.554 | 0.706 | 0.626 | 0.655 | 0.732 | 0.926 | 1 | |||
| Private health exp. per capita | 0.356 | 0.328 | 0.344 | 0.524 | 0.497 | 0.368 | −0.237 | −0.333 | 0.443 | 0.407 | 0.432 | 0.501 | 0.777 | 0.482 | 1 | ||
| Pension funding adequacy rating | 0.250 | 0.225 | 0.182 | 0.518 | 0.447 | 0.054 | −0.007 | −0.128 | 0.324 | 0.602 | 0.165 | 0.478 | 0.375 | 0.363 | 0.265 | 1 | |
| Labor force participation | 0.404 | 0.335 | 0.383 | 0.579 | 0.595 | 0.327 | −0.284 | −0.473 | 0.501 | 0.380 | 0.503 | 0.528 | 0.486 | 0.491 | 0.312 | 0.352 | 1 |
| Country | Score | Rank | Country | Score | Rank | Country | Score | Rank |
|---|---|---|---|---|---|---|---|---|
| Australia | 1 | 1 | Ireland | 0.887 | 20 | Bulgaria | 0.506 | 39 |
| Austria | 1 | 1 | Canada | 0.887 | 21 | Croatia | 0.476 | 40 |
| Denmark | 1 | 1 | South Korea | 0.858 | 22 | Brazil | 0.454 | 41 |
| Finland | 1 | 1 | Israel | 0.833 | 23 | Saudi Arabia | 0.447 | 42 |
| Germany | 1 | 1 | Chile | 0.791 | 24 | Romania | 0.446 | 43 |
| Greece | 1 | 1 | Spain | 0.758 | 25 | Malaysia | 0.442 | 44 |
| Iceland | 1 | 1 | Italy | 0.743 | 26 | Mexico | 0.432 | 45 |
| Japan | 1 | 1 | United Kingdom | 0.736 | 27 | South Africa | 0.401 | 46 |
| Luxembourg | 1 | 1 | United Arab Emirates | 0.688 | 28 | Colombia | 0.393 | 47 |
| The Netherlands | 1 | 1 | Lithuania | 0.678 | 29 | Turkiye | 0.381 | 48 |
| New Zealand | 1 | 1 | Cyprus | 0.655 | 30 | Kazakhstan | 0.380 | 49 |
| Qatar | 1 | 1 | Slovenia | 0.654 | 31 | Jordan | 0.346 | 50 |
| Singapore | 1 | 1 | Czech Republic | 0.595 | 32 | China | 0.324 | 51 |
| Sweden | 1 | 1 | Estonia | 0.593 | 33 | Peru | 0.324 | 52 |
| Switzerland | 1 | 1 | Republic of Latvia | 0.565 | 34 | Thailand | 0.312 | 53 |
| United States | 1 | 1 | Hungary | 0.552 | 35 | Mongolia | 0.261 | 54 |
| Portugal | 0.964 | 17 | Argentina | 0.531 | 36 | Indonesia | 0.224 | 55 |
| Belgium | 0.962 | 18 | Poland | 0.519 | 37 | Philippines | 0.202 | 56 |
| France | 0.960 | 19 | Slovak Republic | 0.511 | 38 | India | 0.129 | 57 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Chuang, Y.-H.; Hu, J.-L. Comparative Assessment of Health Systems Resilience: A Cross-Country Analysis Using Key Performance Indicators. Systems 2025, 13, 663. https://doi.org/10.3390/systems13080663
Chuang Y-H, Hu J-L. Comparative Assessment of Health Systems Resilience: A Cross-Country Analysis Using Key Performance Indicators. Systems. 2025; 13(8):663. https://doi.org/10.3390/systems13080663
Chicago/Turabian StyleChuang, Yu-Hsiu, and Jin-Li Hu. 2025. "Comparative Assessment of Health Systems Resilience: A Cross-Country Analysis Using Key Performance Indicators" Systems 13, no. 8: 663. https://doi.org/10.3390/systems13080663
APA StyleChuang, Y.-H., & Hu, J.-L. (2025). Comparative Assessment of Health Systems Resilience: A Cross-Country Analysis Using Key Performance Indicators. Systems, 13(8), 663. https://doi.org/10.3390/systems13080663







