An Agent-Based Social Impact Theory Model to Study the Impact of In-Person School Closures on Nonmedical Prescription Opioid Use among Youth
Abstract
:1. Introduction
2. Materials and Methods
2.1. Agent-Based Modeling
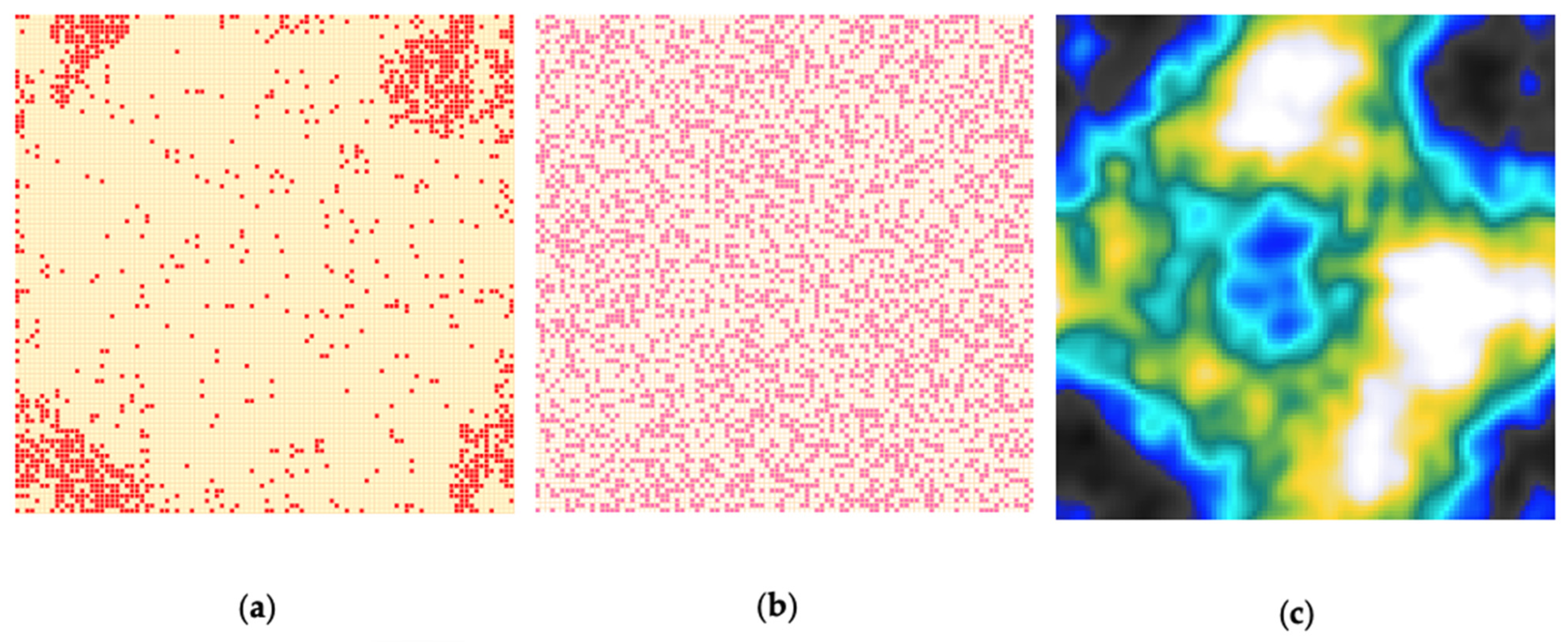
2.2. Cellular Automata for Spatially Localized Networks
2.3. Social Impact Model of Opinion Formation
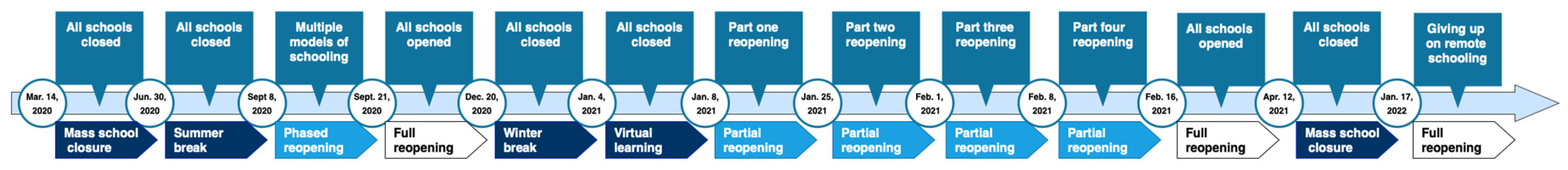
2.4. In-Person School Closures Implementation Due to the COVID-19 Pandemic
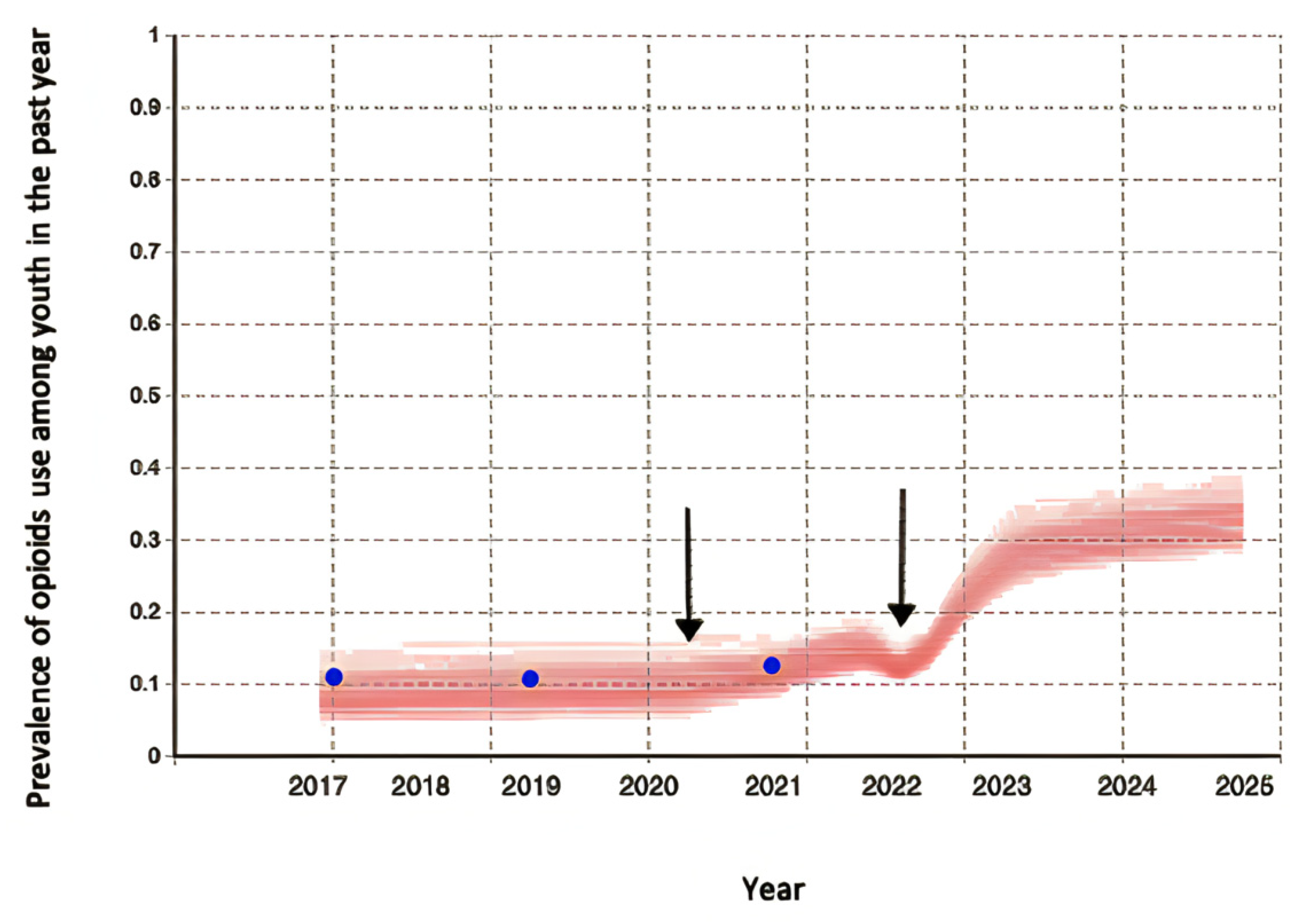
2.5. Parametrization, Calibration, and Validation
2.6. Scenarios
3. Results
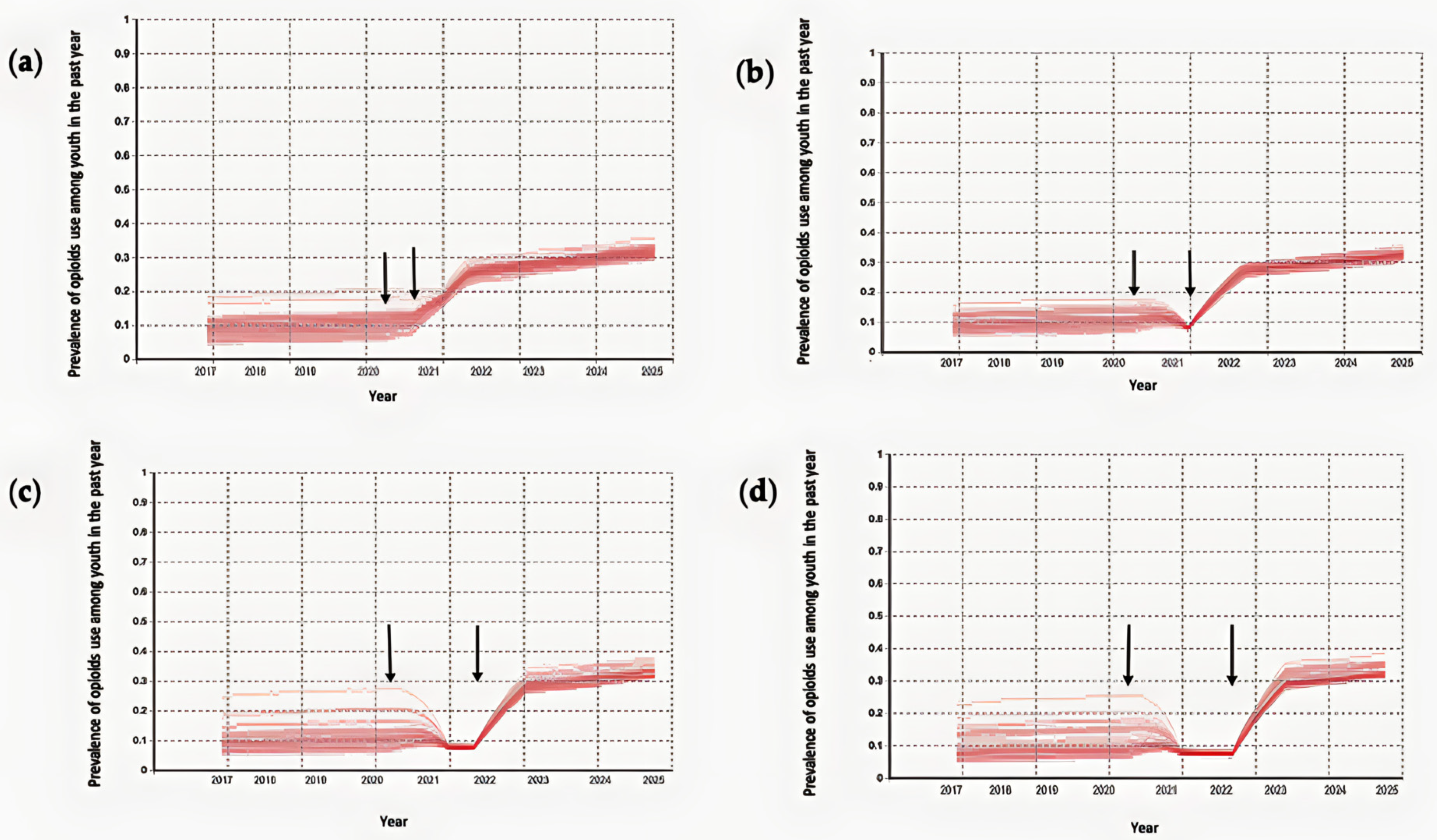
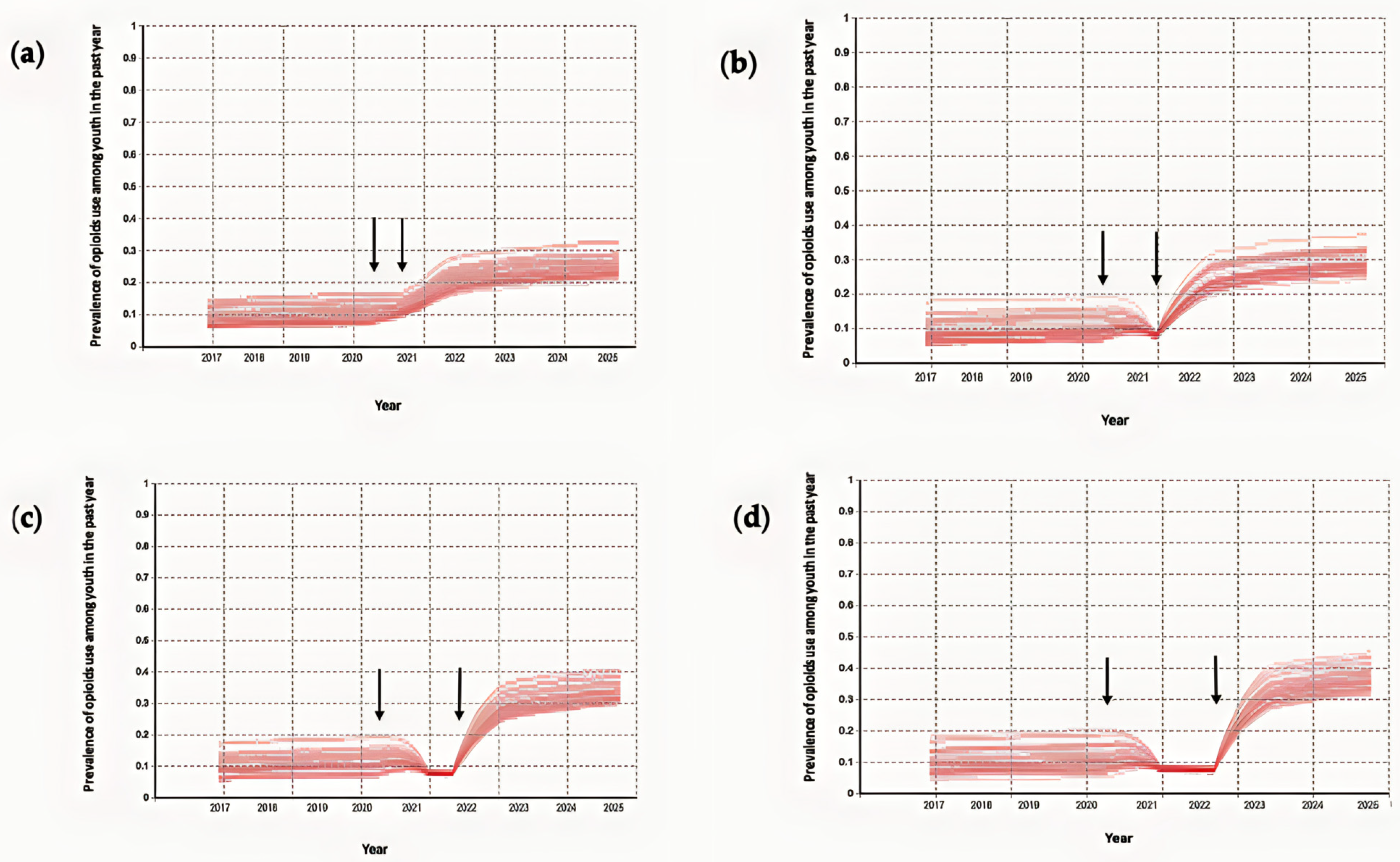
3.1. Results of the Simulation for the Prevalence of Youth with Nonmedical Prescription Opioid Use in the Past Year for Different In-Person School Closure Durations
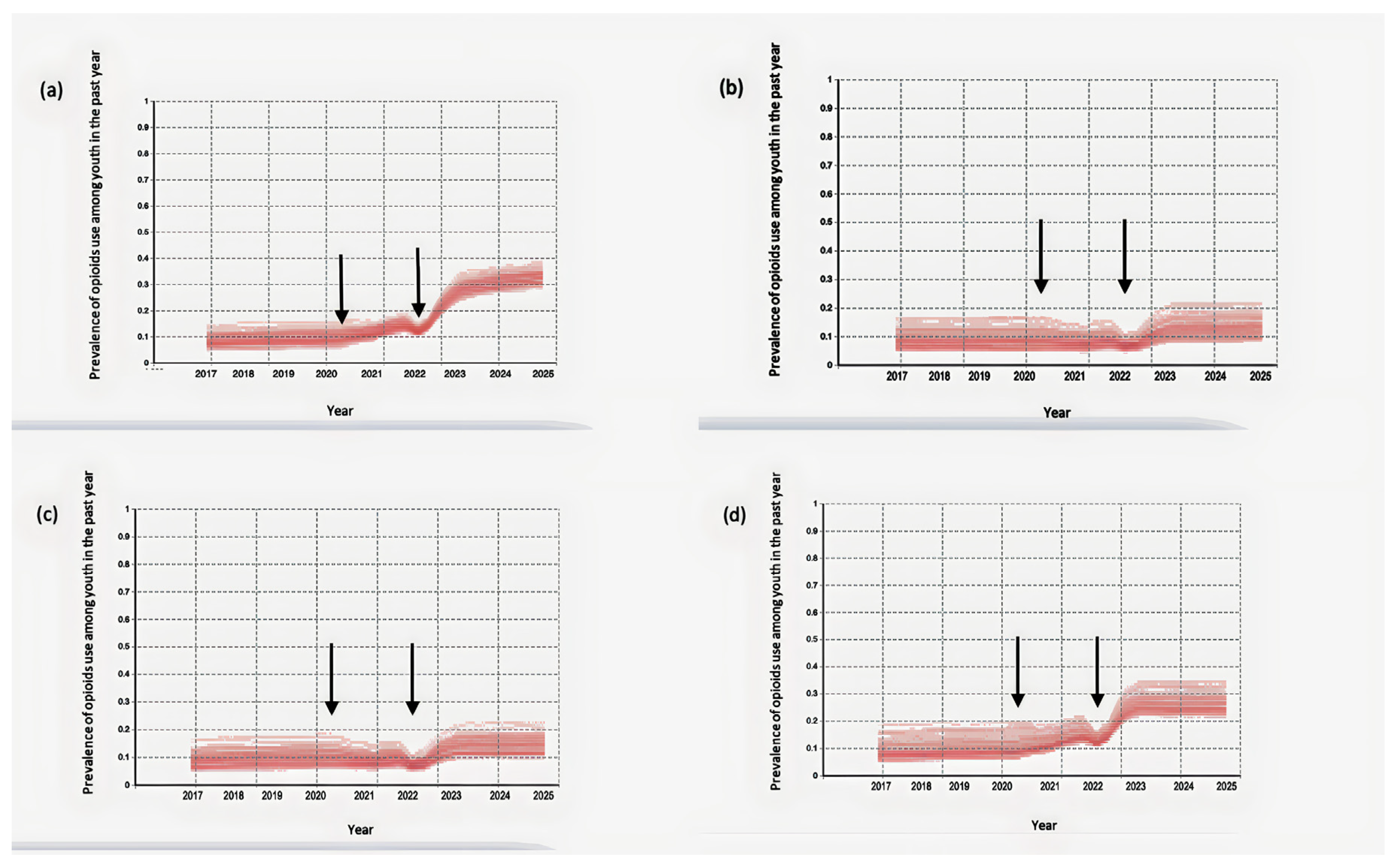
3.2. Simulation of the Model Using Ontario School Closure Timeline
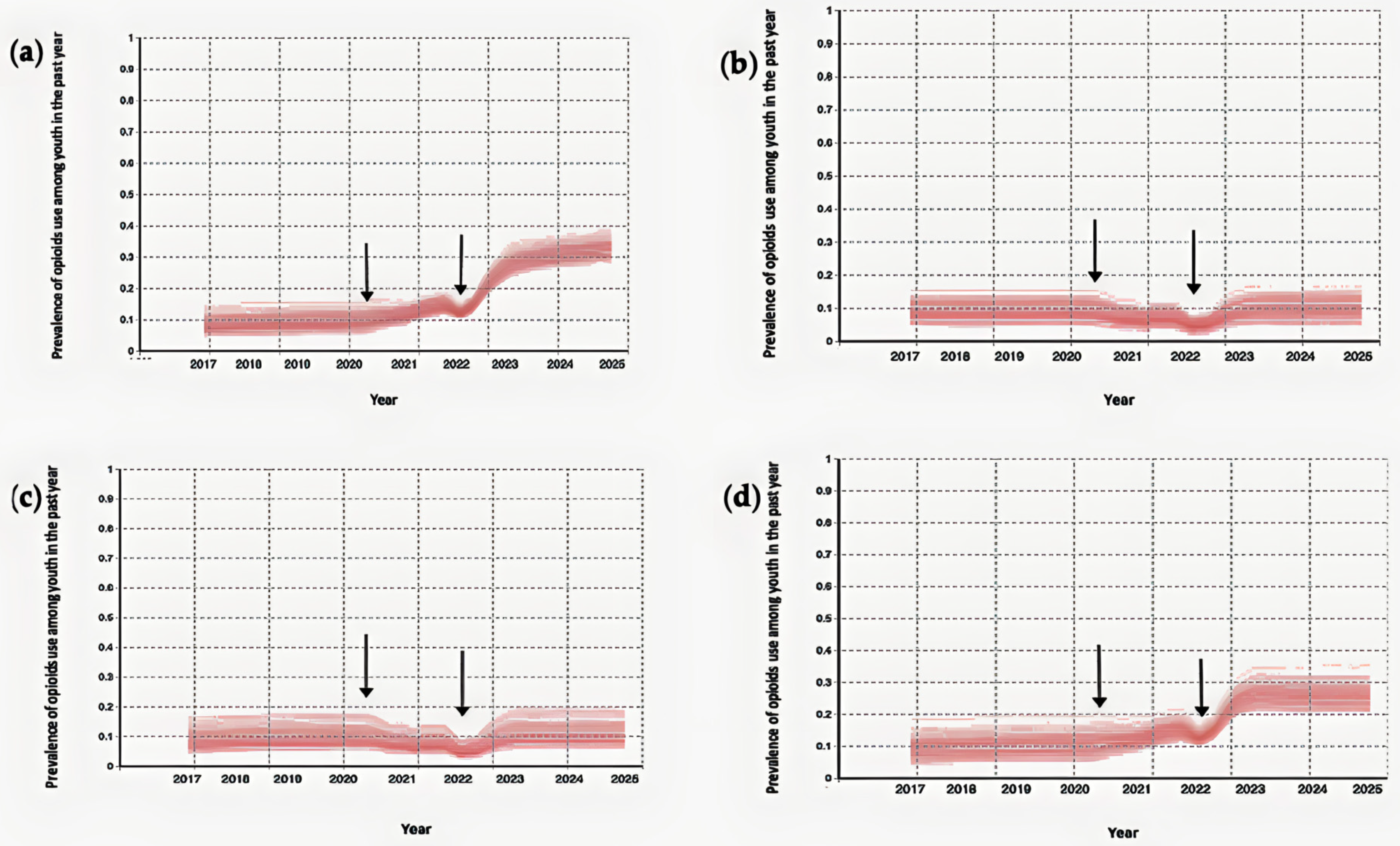
3.3. Impact of Safely Storing Prescription Opioids at Home on the Result of the Model Using the Ontario School Closure Timeline
4. Discussion
Author Contributions
Funding
Data Availability Statement
Conflicts of Interest
Appendix A


| Parameter | Values | References |
|---|---|---|
| Youth population size | 10,000 | Assumed |
| Total number of family | 10,000 | Assumed |
| Family size | Poisson probability distribution | Assumed [66] |
| Moore neighborhood range | 0–3 | Assumed |
| Rate of opioid prescription for each family member without prescription opioids (1/week) | 0.003 | Calibrated [67] |
| Probability that the duration of the opioid prescription ends for each family member (1/week) | 0.02 | Calibrated [67] |
| Level of youth exposure to prescription opioids at home | Uniform distribution between 450 and 900 | Calibrated [61,62] |
| Percentage of the socio-cultural environment with a positive drug use view | 14% | Calibrated [61,62] |
| Level of drug promotion inside the drug-positive socio-cultural environment | Uniform distribution between 1 and 1500 | Calibrated [61,62] |
| Initial amount of encountering drug use situations for youth | Lognormal distribution | Calibrated [61,62] |
| Encountering drug use situations coefficient for different level of socialization among youth | Lognormal distribution | Calibrated [61,62] |
| Level of supportiveness for peers | Uniform distribution between 0 and 100 | Assumed [23,58] |
| Level of persuasiveness for peers | Uniform distribution between 0 and 100 | Assumed [23,58] |
| Severity of acute withdrawal from nonmedical opioid use | Lognormal distribution | Calibrated [71] |
| Probability that peers share drugs with peers who request it | 0.075 | Calibrated [61,62] |
References
- Dash, G.F.; Holt, L.; Kenyon, E.A.; Carter, E.K.; Ho, D.; Hudson, K.A.; Ewing, S.W.F. Detection of Vaping, Cannabis Use, and Hazardous Prescription Opioid Use among Adolescents. Lancet Child Adolesc. Health 2022, 6, 820–828. [Google Scholar] [CrossRef] [PubMed]
- Degenhardt, L.; Stockings, E.; Patton, G.; Hall, W.D.; Lynskey, M. The Increasing Global Health Priority of Substance Use in Young People. Lancet Psychiatry 2016, 3, 251–264. [Google Scholar] [CrossRef] [PubMed]
- Dembo, R.; Blount, W.R.; Schmeidler, J.; Burgos, W. Perceived Environmental Drug Use Risk and the Correlates of Early Drug Use or Nonuse among Inner-City Youths: The Motivated Actor. Int. J. Addict. 1986, 21, 977–1000. [Google Scholar] [CrossRef] [PubMed]
- Rhodes, T.; Lilly, R.; Fernández, C.; Giorgino, E.; Kemmesis, U.E.; Ossebaard, H.C.; Lalam, N.; Faasen, I.; Spannow, K.E. Risk Factors Associated with Drug Use: The Importance of ‘Risk Environment’. Drugs Educ. Prev. Policy 2003, 10, 303–329. [Google Scholar] [CrossRef]
- Bauman, K.E.; Ennett, S.T. On the Importance of Peer Influence for Adolescent Drug Use: Commonly Neglected Considerations. Addiction 1996, 91, 185–198. [Google Scholar] [CrossRef]
- Kobus, K. Peers and Adolescent Smoking. Addiction 2003, 98, 37–55. [Google Scholar] [CrossRef]
- Montgomery, S.C.; Donnelly, M.; Bhatnagar, P.; Carlin, A.; Kee, F.; Hunter, R.F. Peer Social Network Processes and Adolescent Health Behaviors: A Systematic Review. Prev. Med. 2020, 130, 105900. [Google Scholar] [CrossRef]
- Salmanzadeh, H.; Ahmadi-Soleimani, S.M.; Pachenari, N.; Azadi, M.; Halliwell, R.F.; Rubino, T.; Azizi, H. Adolescent Drug Exposure: A Review of Evidence for the Development of Persistent Changes in Brain Function. Brain Res. Bull. 2020, 156, 105–117. [Google Scholar] [CrossRef]
- Kandel, D.B.; Yamaguchi, K.; Chen, K. Stages of Progression in Drug Involvement from Adolescence to Adulthood: Further Evidence for the Gateway Theory. J. Stud. Alcohol 1992, 53, 447–457. [Google Scholar] [CrossRef]
- Probst, C.; Elton-Marshall, T.; Imtiaz, S.; Patte, K.A.; Rehm, J.; Sornpaisarn, B.; Leatherdale, S.T. A Supportive School Environment May Reduce the Risk of Non-Medical Prescription Opioid Use Due to Impaired Mental Health among Students. Eur. Child Adolesc. Psychiatry 2021, 30, 293–301. [Google Scholar] [CrossRef]
- Silverman, M.; Sibbald, R.; Stranges, S. Ethics of COVID-19-Related School Closures. Can. J. Public Health 2020, 111, 462–465. [Google Scholar] [CrossRef] [PubMed]
- Gallagher-Mackay, K.; Srivastava, P.; Underwood, K.; Dhuey, E.; McCready, L.; Born, K.; Maltsev, A.; Perkhun, A.; Steiner, R.; Barrett, K. COVID-19 and Education Disruption in Ontario: Emerging Evidence on Impacts. Available online: https://scholars.wlu.ca/laso_faculty/1 (accessed on 22 January 2023).
- Bialystok, L. Education after COVID. Philos. Inq. Educ. 2022, 29, 1–4. [Google Scholar] [CrossRef]
- Halsall, T.; Mahmoud, K.; Iyer, S.N.; Orpana, H.; Zeni, M.; Matheson, K. Implications of Time and Space Factors Related with Youth Substance Use Prevention: A Conceptual Review and Case Study of the Icelandic Prevention Model Being Implemented in the Context of the COVID-19 Pandemic. Int. J. Qual. Stud. Health Well-Being 2023, 18, 2149097. [Google Scholar] [CrossRef]
- Jayasinha, R.; Nairn, S.; Conrod, P. A Dangerous “Cocktail”: The COVID-19 Pandemic and the Youth Opioid Crisis in North America: A Response to Vigo et al.(2020). Can. J. Psychiatry 2020, 65, 692–694. [Google Scholar] [CrossRef] [PubMed]
- de Vaan, M.; Stuart, T. Does Intra-Household Contagion Cause an Increase in Prescription Opioid Use? Am. Sociol. Rev. 2019, 84, 577–608. [Google Scholar] [CrossRef]
- Nguyen, A.P.; Glanz, J.M.; Narwaney, K.J.; Binswanger, I.A. Association of Opioids Prescribed to Family Members with Opioid Overdose among Adolescents and Young Adults. JAMA Netw. Open 2020, 3, e201018. [Google Scholar] [CrossRef] [PubMed]
- Binswanger, I.A.; Glanz, J.M. Pharmaceutical Opioids in the Home and Youth: Implications for Adult Medical Practice. Subst. Abus. 2015, 36, 141–143. [Google Scholar] [CrossRef] [PubMed]
- Griesler, P.C.; Hu, M.-C.; Wall, M.M.; Kandel, D.B. Nonmedical Prescription Opioid Use by Parents and Adolescents in the US. Pediatrics 2019, 143, e20182354. [Google Scholar] [CrossRef]
- Calina, D.; Hartung, T.; Mardare, I.; Mitroi, M.; Poulas, K.; Tsatsakis, A.; Rogoveanu, I.; Docea, A.O. COVID-19 Pandemic and Alcohol Consumption: Impacts and Interconnections. Toxicol. Rep. 2021, 8, 529–535. [Google Scholar] [CrossRef]
- Gohari, M.R.; Varatharajan, T.; MacKillop, J.; Leatherdale, S.T. Examining the Impact of the COVID-19 Pandemic on Youth Alcohol Consumption: Longitudinal Changes from Pre-to Intra-Pandemic Drinking in the COMPASS Study. J. Adolesc. Health 2022, 71, 665–672. [Google Scholar] [CrossRef]
- Osborne, V.; Serdarevic, M.; Crooke, H.; Striley, C.; Cottler, L.B. Non-Medical Opioid Use in Youth: Gender Differences in Risk Factors and Prevalence. Addict. Behav. 2017, 72, 114–119. [Google Scholar] [CrossRef] [PubMed]
- Valente, T.W.; Hoffman, B.R.; Ritt-Olson, A.; Lichtman, K.; Johnson, C.A. Effects of a Social-Network Method for Group Assignment Strategies on Peer-Led Tobacco Prevention Programs in Schools. Am. J. Public Health 2003, 93, 1837–1843. [Google Scholar] [CrossRef] [PubMed]
- Valente, T.W.; Gallaher, P.; Mouttapa, M. Using Social Networks to Understand and Prevent Substance Use: A Transdisciplinary Perspective. Subst. Use Misuse 2004, 39, 1685–1712. [Google Scholar] [CrossRef] [PubMed]
- Ennett, S.T.; Bauman, K.E.; Hussong, A.; Faris, R.; Foshee, V.A.; Cai, L.; DuRant, R.H. The Peer Context of Adolescent Substance Use: Findings from Social Network Analysis. J. Res. Adolesc. 2006, 16, 159–186. [Google Scholar] [CrossRef]
- Michell, M.P. Smoke Rings: Social Network Analysis of Friendship Groups, Smoking and Drug-Taking. Drugs Educ. Prev. Policy 2000, 7, 21–37. [Google Scholar] [CrossRef]
- Jackson, J.C.; Rand, D.; Lewis, K.; Norton, M.I.; Gray, K. Agent-Based Modeling: A Guide for Social Psychologists. Soc. Psychol. Personal. Sci. 2017, 8, 387–395. [Google Scholar] [CrossRef]
- Macy, M.W.; Willer, R. From Factors to Actors: Computational Sociology and Agent-Based Modeling. Annu. Rev. Sociol. 2002, 28, 143–166. [Google Scholar] [CrossRef]
- Agar, M. My Kingdom for a Function: Modeling Misadventures of the Innumerate. J. Artif. Soc. Soc. Simul. 2003, 6, 1–8. [Google Scholar]
- Agar, M. Agents in Living Color: Towards Emic Agent-Based Models. J. Artif. Soc. Soc. Simul. 2005, 8, 4. [Google Scholar]
- Garrison, L.A.; Babcock, D.S. Alcohol Consumption among College Students: An Agent-based Computational Simulation. Complexity 2009, 14, 35–44. [Google Scholar] [CrossRef]
- Lamy, F.; Bossomaier, T.; Perez, P. An Ontologic Agent-Based Model of Recreational Polydrug Use: SimUse. Int. J. Simul. Process Model. 2015, 10, 207–222. [Google Scholar] [CrossRef]
- Agar, M.H.; Wilson, D. Drugmart: Heroin Epidemics as Complex Adaptive Systems. Complexity 2002, 7, 44–52. [Google Scholar] [CrossRef]
- Perez, P.; Dray, A.; Moore, D.; Dietze, P.; Bammer, G.; Jenkinson, R.; Siokou, C.; Green, R.; Hudson, S.L.; Maher, L. SimAmph: An Agent-Based Simulation Model for Exploring the Use of Psychostimulants and Related Harm amongst Young Australians. Int. J. Drug Policy 2012, 23, 62–71. [Google Scholar] [CrossRef]
- Agar, M.; Reisinger, H.S. Using Trend Theory to Explain Heroin Use Trends. J. Psychoact. Drugs 2001, 33, 203–211. [Google Scholar] [CrossRef]
- Di Clemente, R.; Pietronero, L. Statistical Agent Based Modelization of the Phenomenon of Drug Abuse. Sci. Rep. 2012, 2, 532. [Google Scholar] [CrossRef]
- Coates, A.; Han, L.; Kleerekoper, A. A Unified Framework for Opinion Dynamics. In Proceedings of the 17th International Conference on Autonomous Agents and Multiagent Systems, International Foundation for Autonomous Agents and Multiagent Systems, Stockholm, Sweden, 10–15 July 2018. [Google Scholar]
- Grabisch, M.; Rusinowska, A. A Survey on Nonstrategic Models of Opinion Dynamics. Games 2020, 11, 65. [Google Scholar] [CrossRef]
- Anderson, B.D.; Ye, M. Recent Advances in the Modelling and Analysis of Opinion Dynamics on Influence Networks. Int. J. Autom. Comput. 2019, 16, 129–149. [Google Scholar] [CrossRef]
- Sun, R.; Mendez, D. An Application of the Continuous Opinions and Discrete Actions (CODA) Model to Adolescent Smoking Initiation. PLoS ONE 2017, 12, e0186163. [Google Scholar] [CrossRef]
- Moore, T.W.; Finley, P.D.; Apelberg, B.J.; Ambrose, B.K.; Brodsky, N.S.; Brown, T.J.; Husten, C.; Glass, R.J. An Opinion-Driven Behavioral Dynamics Model for Addictive Behaviors. Eur. Phys. J. B 2015, 88, 1–28. [Google Scholar] [CrossRef]
- Clifford, P.; Sudbury, A. A Model for Spatial Conflict. Biometrika 1973, 60, 581. [Google Scholar] [CrossRef]
- Castellano, C.; Muñoz, M.A.; Pastor-Satorras, R. Nonlinear Q-Voter Model. Phys. Rev. E 2009, 80, 041129. [Google Scholar] [CrossRef] [PubMed]
- Castellano, C.; Loreto, V.; Barrat, A.; Cecconi, F.; Parisi, D. Comparison of Voter and Glauber Ordering Dynamics on Networks. Phys. Rev. E 2005, 71, 066107. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Mobilia, M. Does a Single Zealot Affect an Infinite Group of Voters? Phys. Rev. Lett. 2003, 91, 028701. [Google Scholar] [CrossRef]
- Malik, N.; Mucha, P.J. Role of Social Environment and Social Clustering in Spread of Opinions in Coevolving Networks. Chaos Interdiscip. J. Nonlinear Sci. 2013, 23, 043123. [Google Scholar] [CrossRef] [PubMed]
- Krapivsky, P.L.; Redner, S. Dynamics of Majority Rule in Two-State Interacting Spin Systems. Phys. Rev. Lett. 2003, 90, 238701. [Google Scholar] [CrossRef]
- Galam, S. Minority Opinion Spreading in Random Geometry. Eur. Phys. J. B-Condens. Matter Complex Syst. 2002, 25, 403–406. [Google Scholar] [CrossRef]
- Sznajd-Weron, K.; Sznajd, J. Opinion Evolution in Closed Community. Int. J. Mod. Phys. C 2000, 11, 1157–1165. [Google Scholar] [CrossRef]
- Sznajd-Weron, K.; Sznajd, J.; Weron, T. A Review on the Sznajd Model—20 Years After. Phys. A: Stat. Mech. Its Appl. 2021, 565, 125537. [Google Scholar] [CrossRef]
- Sznajd-Weron, K. Sznajd Model and Its Applications. arXiv 2005, arXiv:physics/0503239. [Google Scholar]
- Deffuant, G.; Amblard, F.; Weisbuch, G.; Faure, T. How Can Extremism Prevail? A Study Based on the Relative Agreement Interaction Model. J. Artif. Soc. Soc. Simul. 2002, 5, 4. [Google Scholar]
- Deffuant, G.; Neau, D.; Amblard, F.; Weisbuch, G. Mixing Beliefs among Interacting Agents. Adv. Complex Syst. 2001, 3, 87–98. [Google Scholar] [CrossRef]
- Martins, A.C. Continuous Opinions and Discrete Actions in Opinion Dynamics Problems. Int. J. Mod. Phys. C 2008, 19, 617–624. [Google Scholar] [CrossRef]
- Fan, K.; Pedrycz, W. Emergence and Spread of Extremist Opinions. Phys. A Stat. Mech. Its Appl. 2015, 436, 87–97. [Google Scholar] [CrossRef]
- Martins, A.C.; Kuba, C.D. The Importance of Disagreeing: Contrarians and Extremism in the Coda Model. Adv. Complex Syst. 2010, 13, 621–634. [Google Scholar] [CrossRef] [Green Version]
- Latané, B. The Psychology of Social Impact. Am. Psychol. 1981, 36, 343. [Google Scholar] [CrossRef]
- Nowak, A.; Szamrej, J.; Latané, B. From Private Attitude to Public Opinion: A Dynamic Theory of Social Impact. Psychol. Rev. 1990, 97, 362. [Google Scholar] [CrossRef]
- Castellano, C.; Fortunato, S.; Loreto, V. Statistical Physics of Social Dynamics. Rev. Mod. Phys. 2009, 81, 591. [Google Scholar] [CrossRef]
- Hołyst, J.A.; Kacperski, K.; Schweitzer, F. Social Impact Models of Opinion Dynamics. Annu. Rev. Comput. Phys. 2001, 253–273. [Google Scholar] [CrossRef]
- Boak, A.; Elton-Marshall, T.; Mann, R.E.; Hamilton, H.A. Drug Use among Ontario Students, 1977–2019: Detailed Findings from the Ontario Student Drug Use and Health Survey (OSDUHS); Centre for Addiction and Mental Health: Toronto, ON, Canada, 2020. [Google Scholar]
- Boak, A.; Elton-Marshall, T.; Hamilton, H.A. The Well-Being of Ontario Students: Findings from the 2021 Ontario Student Drug Use and Health Survey (OSDUHS); Centre for Addiction and Mental Health: Toronto, ON, Canada, 2022. [Google Scholar]
- Berryman, M. Review of Software Platforms for Agent Based Models. Available online: https://citeseerx.ist.psu.edu/document?repid=rep1&type=pdf&doi=f3acb55df14e3e83f60bb14f067f5fcb5afc97d1 (accessed on 22 January 2023).
- Nikolai, C.; Madey, G. Tools of the Trade: A Survey of Various Agent Based Modeling Platforms. J. Artif. Soc. Soc. Simul. 2009, 12, 2. [Google Scholar]
- Borshchev, A. The Big Book of Simulation Modeling: Multimethod Modeling with AnyLogic 6; AnyLogic: New York, NY, USA, 2013; ISBN 0-9895731-7-6. [Google Scholar]
- Average Number of People per Family in Canada in 2019, by Province. Available online: https://www.statista.com/statistics/478954/average-family-size-in-canada-by-province/ (accessed on 22 January 2023).
- Carrière, G.; Garner, R.; Sanmartin, C. Significant Factors Associated with Problematic Use of Opioid Pain Relief Medications among the Household Population, Canada, 2018. Health Rep. 2021, 32, 11–26. [Google Scholar]
- Sharma, B.; Bruner, A.; Barnett, G.; Fishman, M. Opioid Use Disorders. Child Adolesc. Psychiatr. Clin. 2016, 25, 473–487. [Google Scholar] [CrossRef] [PubMed]
- Branstetter, S.A.; Low, S.; Furman, W. The Influence of Parents and Friends on Adolescent Substance Use: A Multidimensional Approach. J. Subst. Use 2011, 16, 150–160. [Google Scholar] [CrossRef] [PubMed]
- Mansouri, A.; Taghiyareh, F. Effect of Segregation on the Dynamics of Noise-Free Social Impact Model of Opinion Formation through Agent-Based Modeling. Int. J. Web Res. 2019, 2, 36–44. [Google Scholar]
- Lerner, A.; Klein, M. Dependence, Withdrawal and Rebound of CNS Drugs: An Update and Regulatory Considerations for New Drugs Development. Brain Commun. 2019, 1, fcz025. [Google Scholar] [CrossRef] [PubMed]
- Bordogna, C.M.; Albano, E.V. Dynamic Behavior of a Social Model for Opinion Formation. Phys. Rev. E 2007, 76, 061125. [Google Scholar] [CrossRef]
- Hołyst, J.A.; Kacperski, K.; Schweitzer, F. Phase Transitions in Social Impact Models of Opinion Formation. Phys. A Stat. Mech. Its Appl. 2000, 285, 199–210. [Google Scholar] [CrossRef]
- Cooley, P.; Solano, E. Agent-Based Model (ABM) Validation Considerations. In Proceedings of the Third International Conference on Advances in System Simulation (SIMUL 2011), Barcelona, Spain, 23–29 October 2011; pp. 134–139. [Google Scholar]
- Sayama, H. Introduction to the Modeling and Analysis of Complex Systems; Open SUNY Textbooks: Albany, NY, USA, 2015. [Google Scholar]
- Andrews, J.L.; Foulkes, L.; Blakemore, S.-J. Peer Influence in Adolescence: Public-Health Implications for COVID-19. Trends Cogn. Sci. 2020, 24, 585–587. [Google Scholar] [CrossRef]
- Cho, J.; Bello, M.S.; Christie, N.C.; Monterosso, J.R.; Leventhal, A.M. Adolescent Emotional Disorder Symptoms and Transdiagnostic Vulnerabilities as Predictors of Young Adult Substance Use during the COVID-19 Pandemic: Mediation by Substance-Related Coping Behaviors. Cogn. Behav. Ther. 2021, 50, 276–294. [Google Scholar] [CrossRef]
- Pelham III, W.E.; Tapert, S.F.; Gonzalez, M.R.; McCabe, C.J.; Lisdahl, K.M.; Alzueta, E.; Baker, F.C.; Breslin, F.J.; Dick, A.S.; Dowling, G.J. Early Adolescent Substance Use before and during the COVID-19 Pandemic: A Longitudinal Survey in the ABCD Study Cohort. J. Adolesc. Health 2021, 69, 390–397. [Google Scholar] [CrossRef]
- Miller, B.L.; Lowe, C.C.; Kaakinen, M.; Savolainen, I.; Sirola, A.; Stogner, J.; Ellonen, N.; Oksanen, A. Online Peers and Offline Highs: An Examination of Online Peer Groups, Social Media Homophily, and Substance Use. J. Psychoact. Drugs 2021, 53, 345–354. [Google Scholar] [CrossRef]
- Huang, G.C.; Unger, J.B.; Soto, D.; Fujimoto, K.; Pentz, M.A.; Jordan-Marsh, M.; Valente, T.W. Peer Influences: The Impact of Online and Offline Friendship Networks on Adolescent Smoking and Alcohol Use. J. Adolesc. Health 2014, 54, 508–514. [Google Scholar] [CrossRef] [PubMed]
- Nairn, S.A.; Audet, M.; Stewart, S.H.; Hawke, L.D.; Isaacs, J.Y.; Henderson, J.; Saah, R.; Knight, R.; Fast, D.; Khan, F. Interventions to Reduce Opioid Use in Youth At-Risk and in Treatment for Substance Use Disorders: A Scoping Review. Can. J. Psychiatry 2022, 07067437221089810. [Google Scholar] [CrossRef] [PubMed]



Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Shojaati, N.; Osgood, N.D. An Agent-Based Social Impact Theory Model to Study the Impact of In-Person School Closures on Nonmedical Prescription Opioid Use among Youth. Systems 2023, 11, 72. https://doi.org/10.3390/systems11020072
Shojaati N, Osgood ND. An Agent-Based Social Impact Theory Model to Study the Impact of In-Person School Closures on Nonmedical Prescription Opioid Use among Youth. Systems. 2023; 11(2):72. https://doi.org/10.3390/systems11020072
Chicago/Turabian StyleShojaati, Narjes, and Nathaniel D. Osgood. 2023. "An Agent-Based Social Impact Theory Model to Study the Impact of In-Person School Closures on Nonmedical Prescription Opioid Use among Youth" Systems 11, no. 2: 72. https://doi.org/10.3390/systems11020072





