Blockchain Application in Healthcare Systems: A Review
Abstract
1. Introduction
2. Background Study of Blockchain
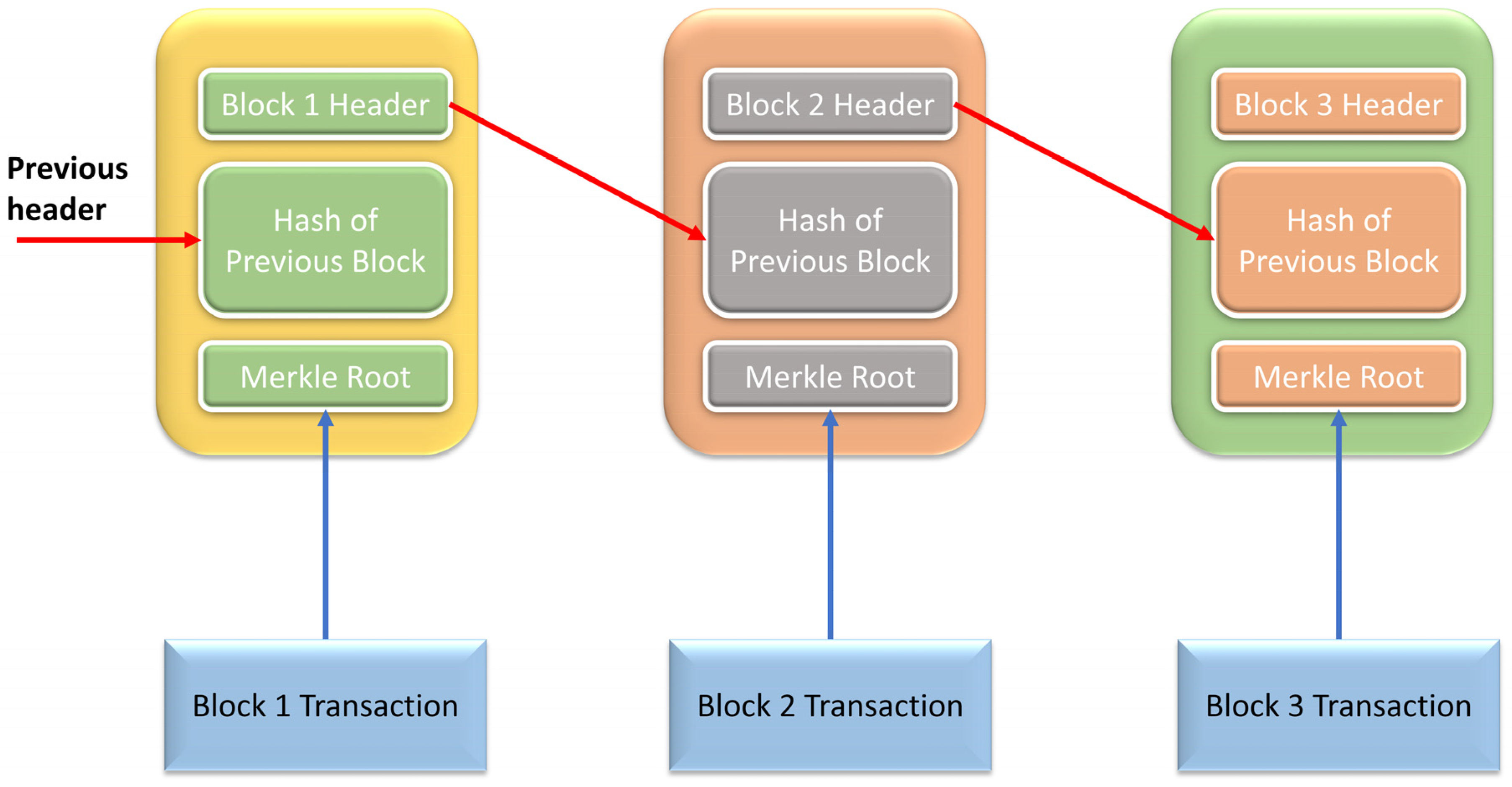
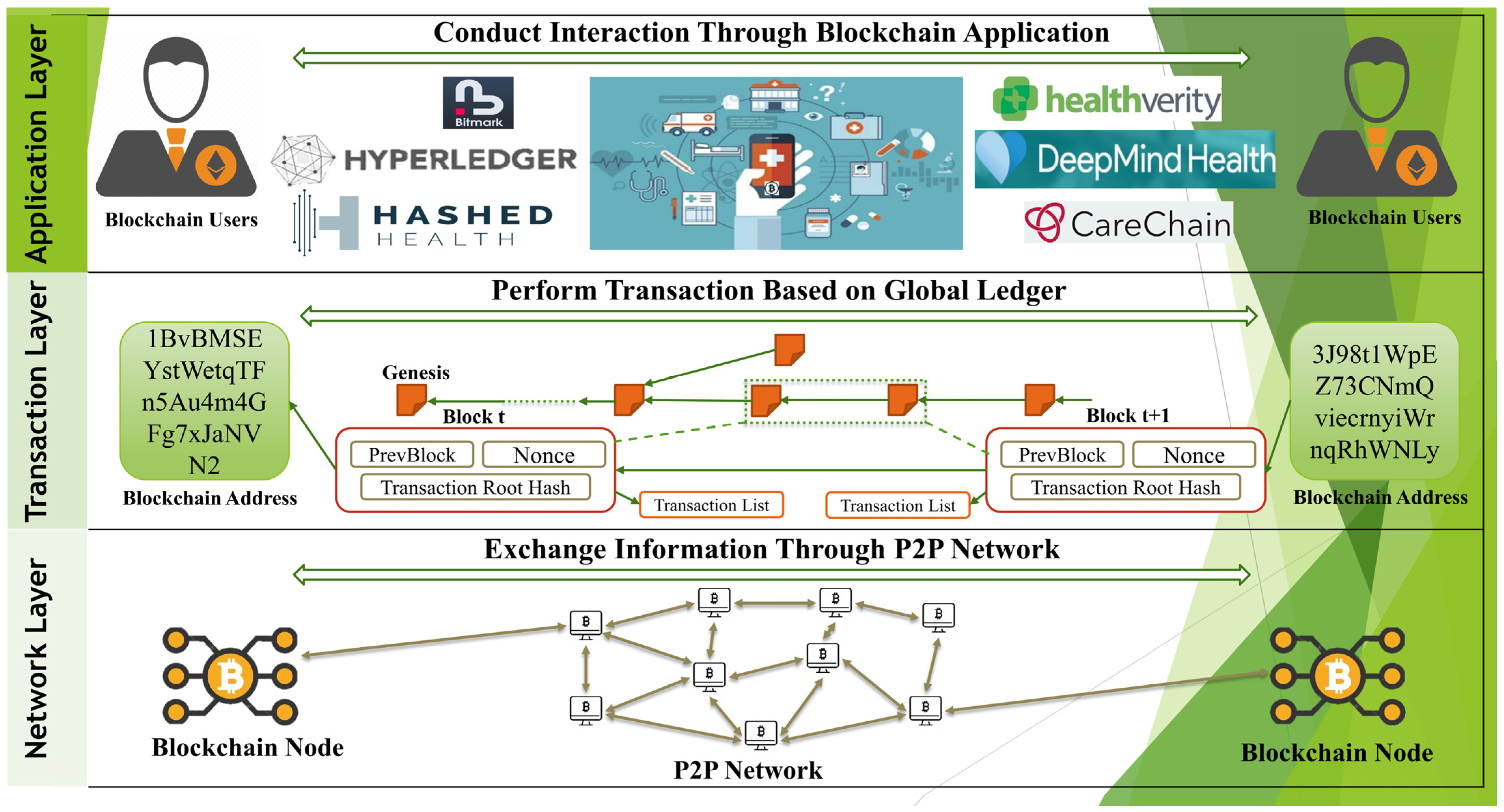
2.1. What Is BlockChain
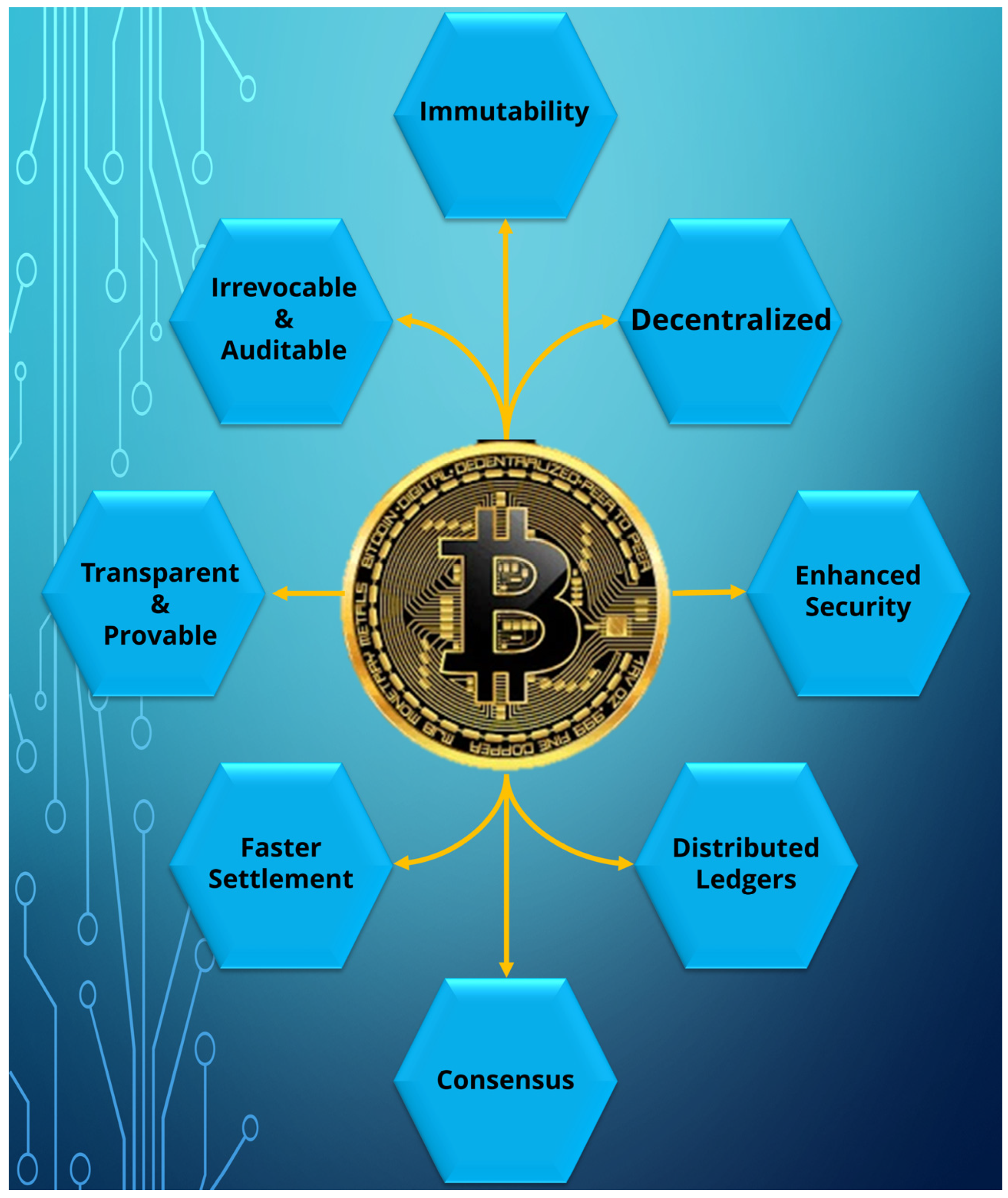
2.1.1. Key Features
2.1.2. Different Kinds of Blockchain
2.1.3. Difference between Blockchain in Healthcare and General Sectors
2.1.4. Existing Blockchains
2.1.5. Mechanisms for Consensus
| Possessions | PBFT | PoS | PoW |
|---|---|---|---|
| Management of nodes | Authorized | Accessible | Accessible |
| Adversarial tolerance | Faulty replicas less than 33.3% | Stake less than 51% | Computation power less than 25% |
| Expenditure of energy | Poor | Moderate | High |
| Instance | Hyperledger Fabric [29] | Peercoin [21] | Bitcoin [23] |
2.1.6. Smart Contracts
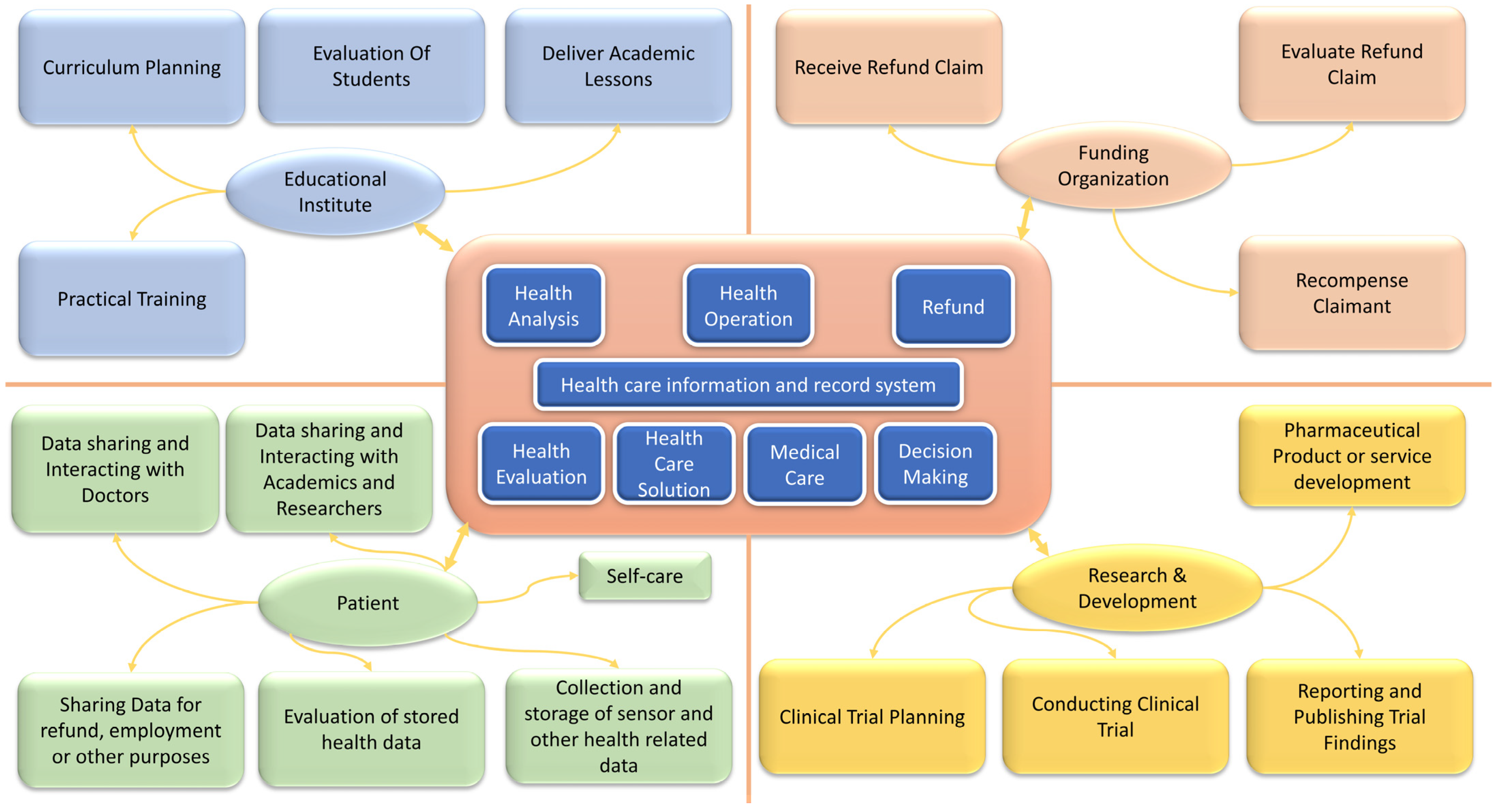
2.2. Blockchain Potential in Healthcare
2.3. Types of Blockchain in Healthcare System: Public, Private and Consortium
2.3.1. Public Blockchain
2.3.2. Private Blockchain
2.3.3. Consortium Blockchain
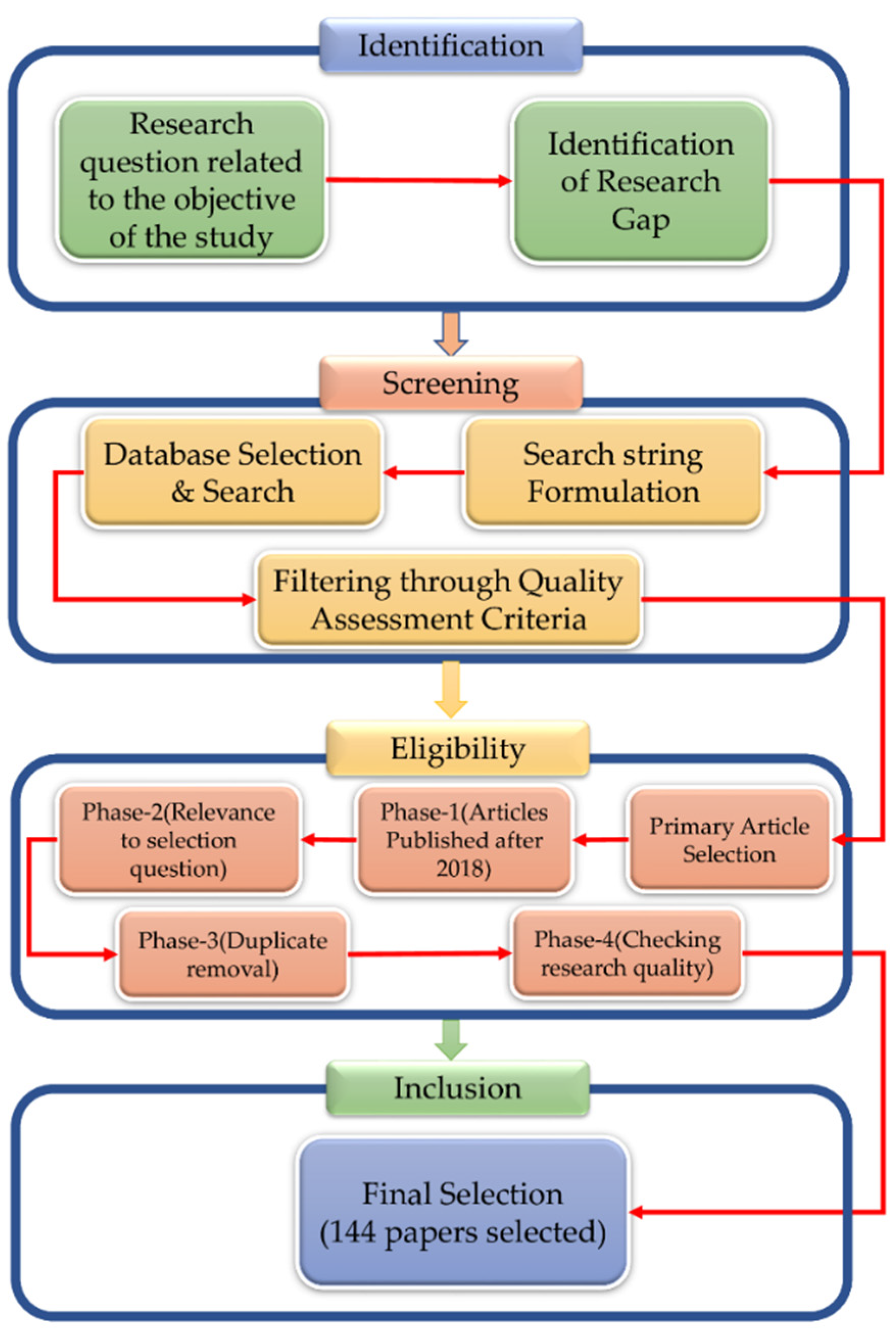
3. Review Methodology
3.1. Research Questions
- What is the latest study profile of applications used on the blockchain in the healthcare sector?
- In which sectors of healthcare is the blockchain being used?
- What are the constraints in this study area?
- What aspects of healthcare could benefit from the use of the blockchain in the future?
3.2. Search Strategy and Databases
- Identification of abstract and related words in the article that were identified during the first search.
- The use of Boolean characters such as OR and operators in the building of search strings.
- Identification of related words, abbreviations, and synonyms.
3.3. Quality Assessment
- What is the study’s aim, and what does the article say about it?
- Is there any mention of literary reviews, histories, or contexts in the article?
- Is the article relevant to current work?
- Is there a research method presented in the article?
- Is there any analysis in the article?
- Is there a conclusion in the article?
3.4. Article Selection
4. Literature Review of Selected Articles
4.1. Bibliographic Overview
4.2. Bibliometric Distribution
5. Research Themes of Blockchain-Based Healthcare Systems
5.1. Research Themes
5.1.1. Evolution of Concept
5.1.2. Advances in Technology
5.1.3. Increase Efficiency
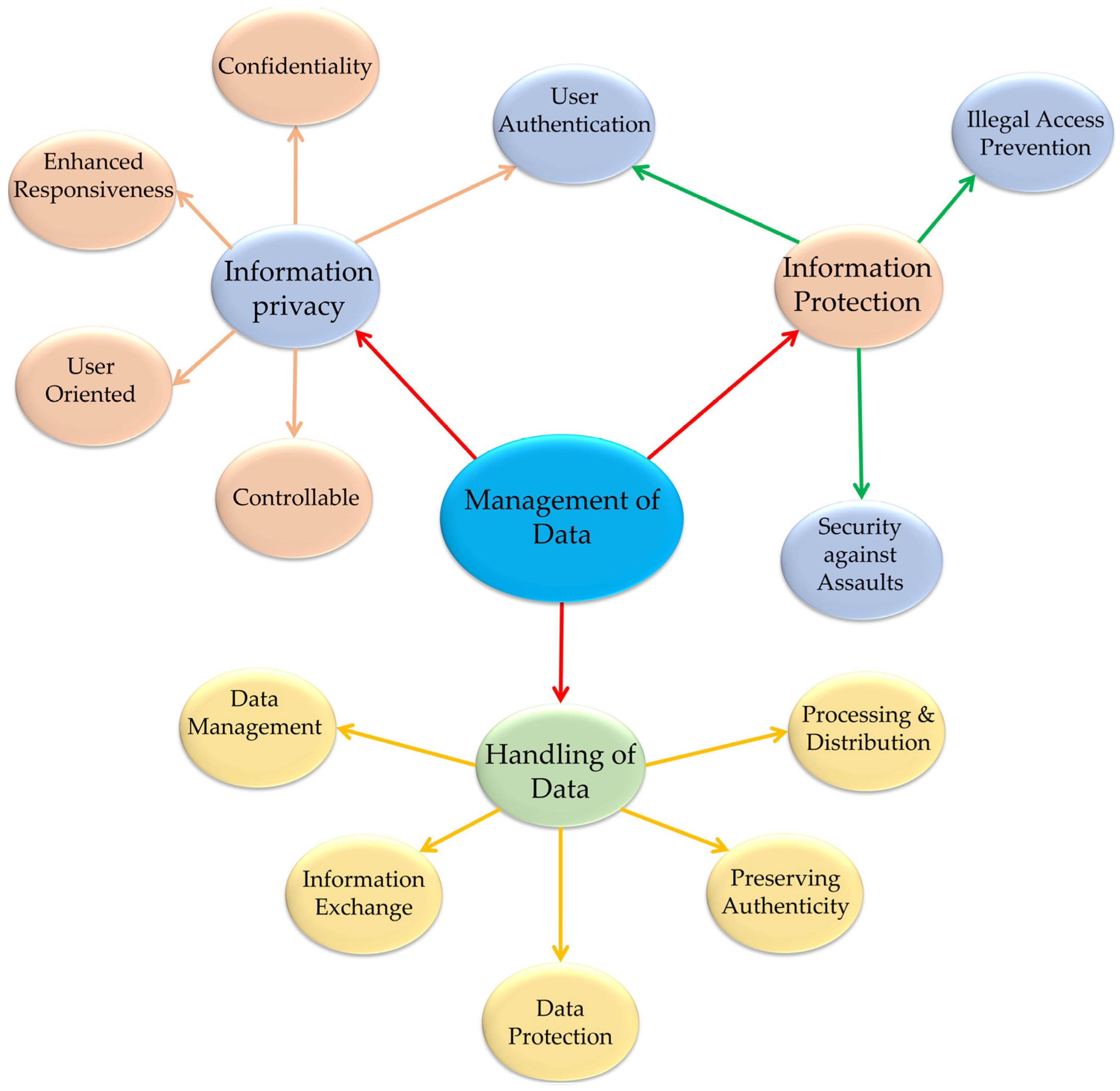
5.1.4. Management of Data
6. Major Application Areas of Blockchain in Healthcare Systems
6.1. Health Information Management
6.1.1. Healthcare Record Sharing
- (1)
- User layer: a graphical interface that will allow the user to access data.
- (2)
- Data query layer: a system architecture that manages and responds to query requests.
- (3)
- Database infrastructure: a layer constructed by a system database that only a few specialized organizations have access to.
- (4)
- Provenance and Data Structuring Layer: The adopted blockchain network structure, node authentication, smart contracts, and consensus protocol are all part of this layering process within the systems.
6.1.2. Healthcare Image Sharing
6.1.3. HealthCare System Log Management
6.1.4. Industry-Specific Approaches
- (1)
- MedCoin as an external token that can be used in exchange.
- (2)
- An internal token that would have the capability to generate a block hash to provide dispersed information located in any place in the system to the owner of the data.
6.1.5. Consensus Protocols Used on Healthcare Systems
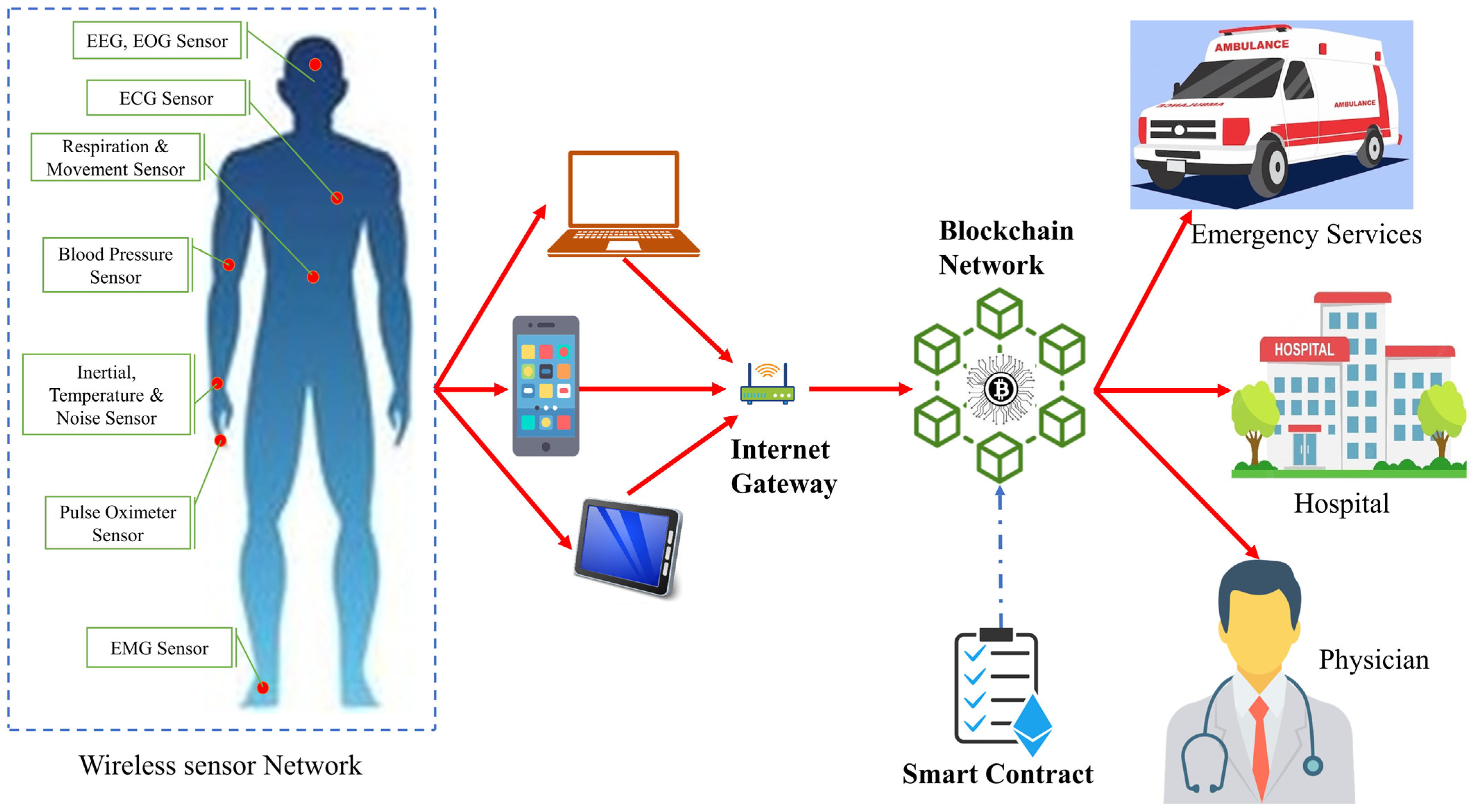
6.1.6. Patient Monitoring
6.1.7. Discussion
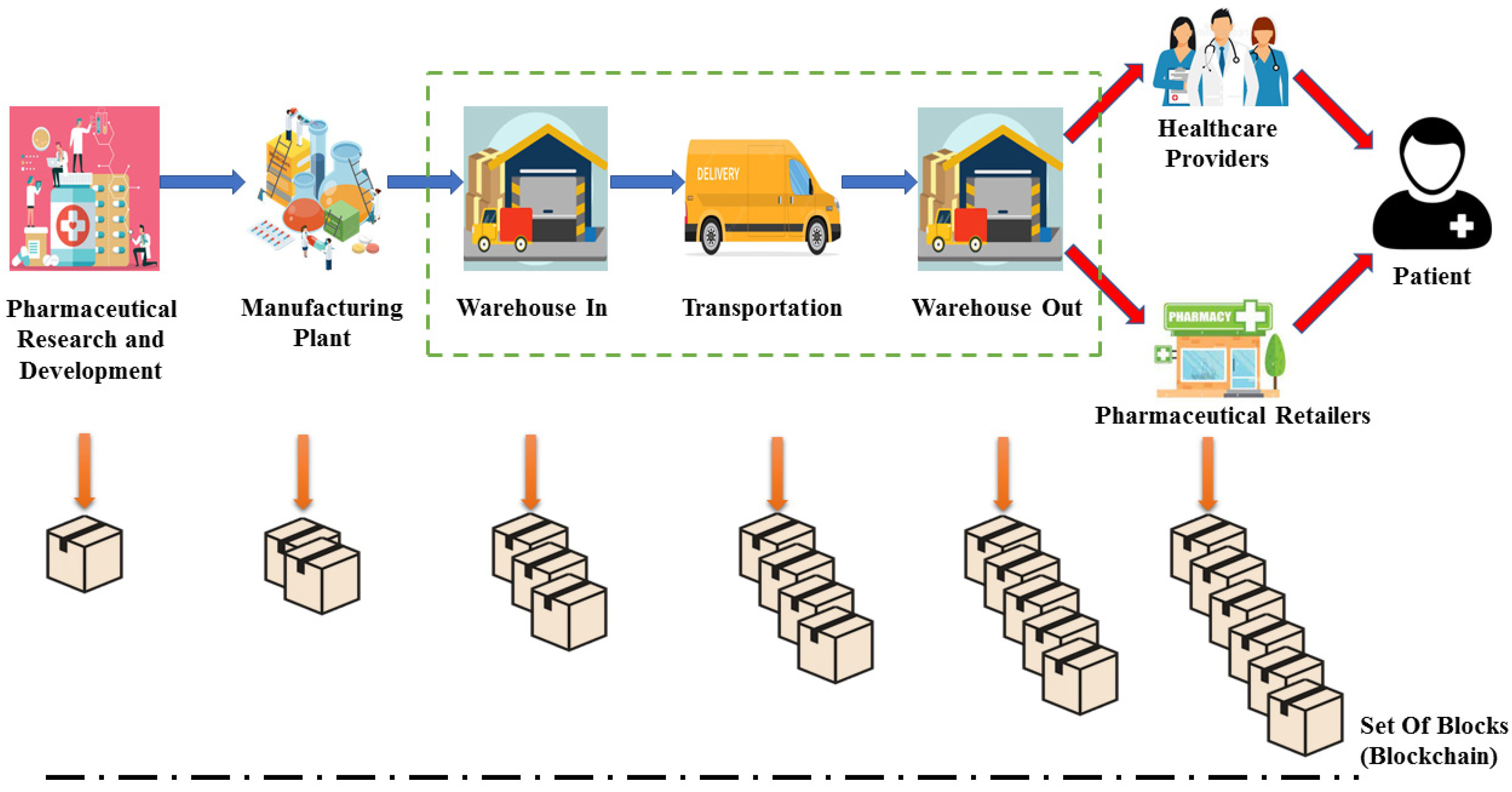
6.2. Supply Chain Management
6.3. Research and Education
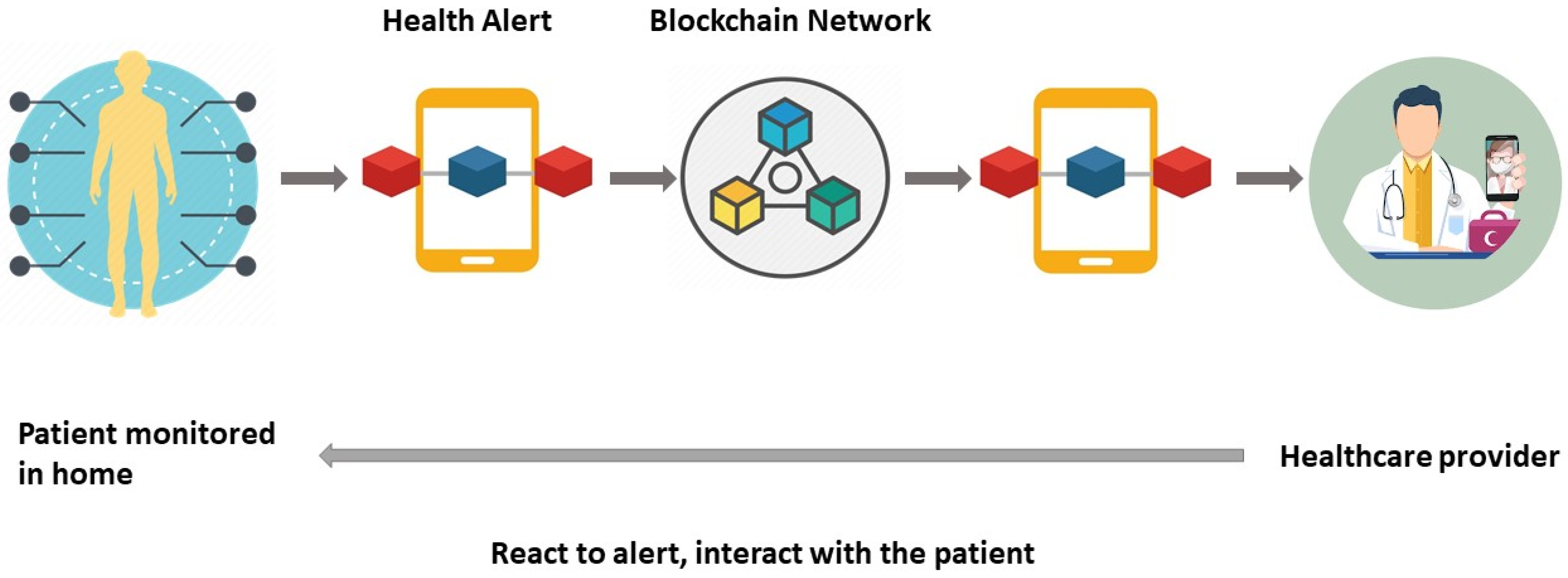
6.4. Remote Patient Monitoring
6.5. Health Insurance Claims
6.6. Health Data Analysis
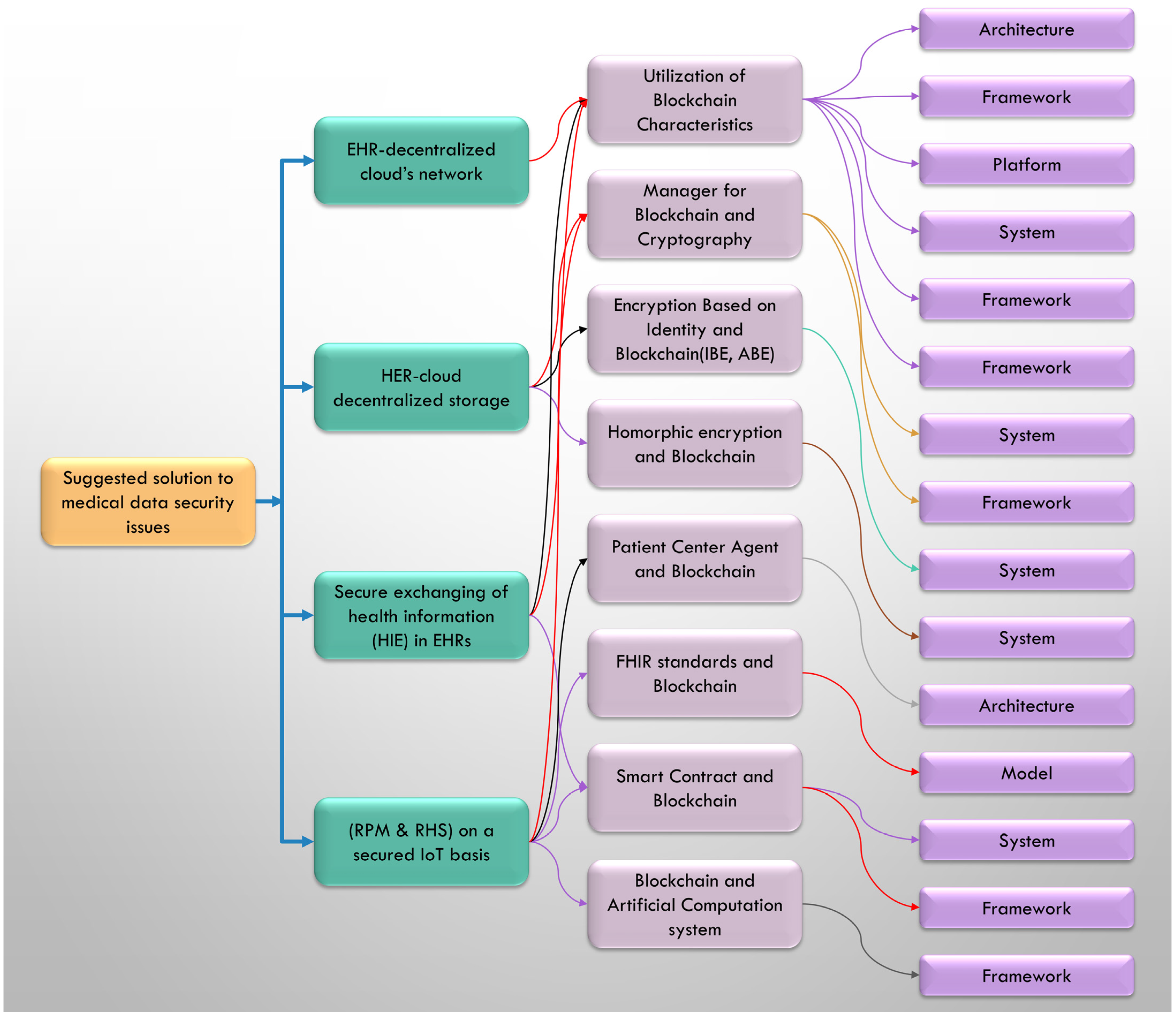
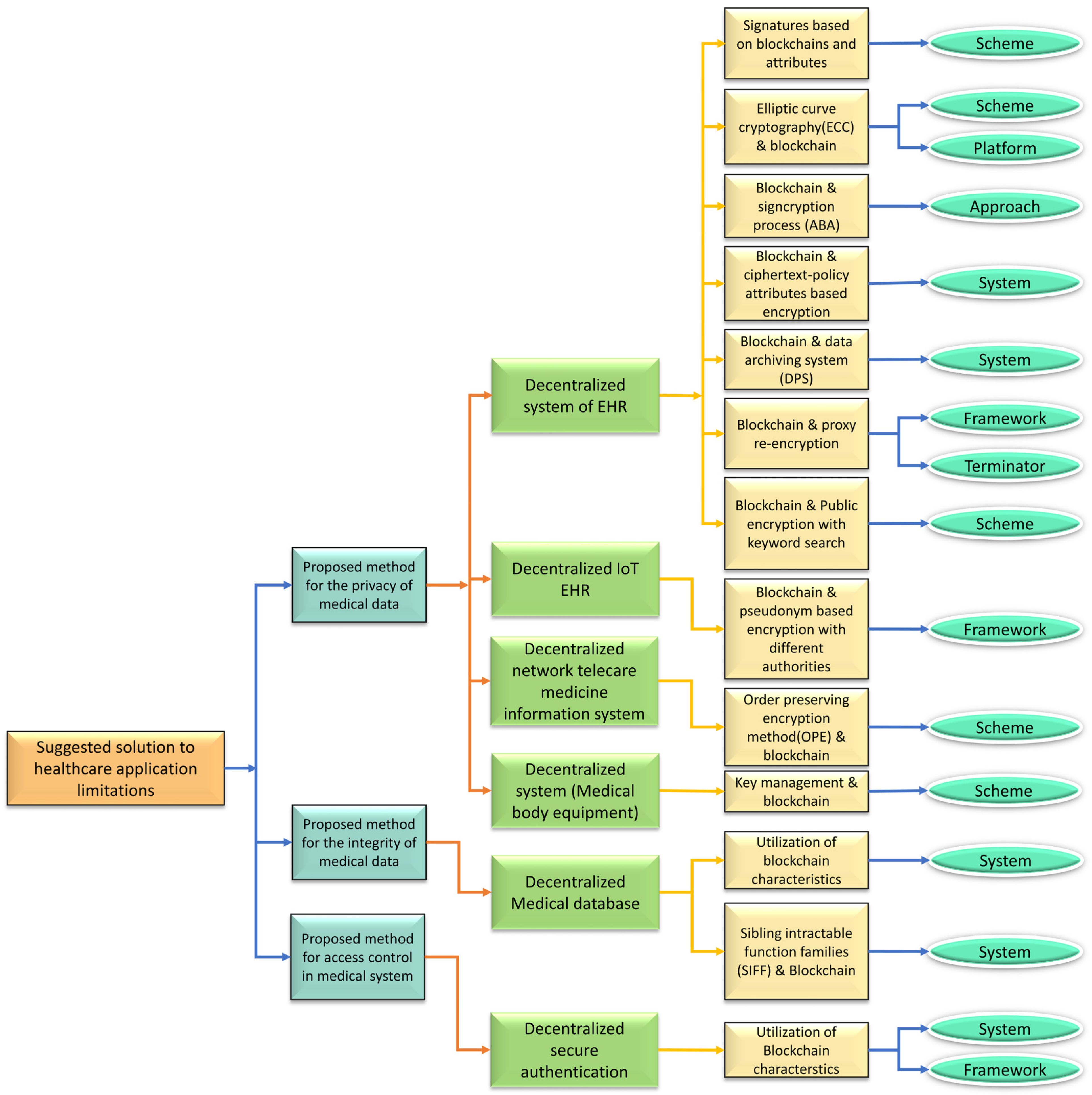
7. Blockchain-Based Solutions in Existing Healthcare Systems
7.1. Proposed Solutions for the Safety of Medical Data
7.2. Proposed Solutions for Resolving Privacy Issues with Medical Data
7.3. Proposed Solutions for Problems with Medical Data Integrity
7.4. Proposed Solutions to the Medical System’s Access Control Issues
7.5. Proposed Solutions to Interoperability Issues with Medical Data
7.6. Proposed Solutions to Issues Associated with Handling Large Amounts of Patient Data
8. Discussion
8.1. Limitations:
8.1.1. Performance
8.1.2. Assumptions
8.1.3. Constraints
- Costs: Other costs labeled as limitations in the current study involved linear protocol costs, which depended on the characteristics of the respective organization. For example, patients create operational overhead and assessments may be delayed because of applicants’ greater involvement in the apps [87,88]. The transaction and execution costs are created for the size of the string length and input size [90]. Searching time is also a cost-discussed issue as patients need to search for global smart contracts from storage data, so execution time should be short [57,76].
- Data and analysis: Much research has been conducted on data limitations, such as the lack of representation of specimen data. For data-driven simulations and tests, training data is not readily available [47]. Other studies have been limited by the inferiority of testing data [85]. Such limitations may fall on the completion or commencement of rule testing related to authentication within the organization [55]. It may also be affected by the performance testing of a development structure. For example, if the proposed structure presented in [49] is affected by a small amount of dataset, then it not only misuses the space, but also damages the recognition technique of multimedia images.
- Platform and framework elements: The blockchain platform on some elements of the advanced structure can act as an obligation for its improvement. Many previous reports have limitations, including the need for a gateway level for Tangle to receive a direct connection with the sensor [66]. This limited storage, however, is provided by a fog layer as well as compatibility with semantic inter-operative functionality and inheritance systems [65]. Failure to prioritize relevant entities can lead to complications, especially in emergencies, leading to conflicts in decision-making [48]. In addition, it is necessary to ensure that users will receive the full incentive when they share data [52]. Several studies have reported specific limitations for updated algorithms, such as the limitation of an advanced scheme of PSN-dependent blockchain for healthcare [56] and the limitation of another method such as the Optimized Masked Authenticated Messaging (MAM) module library [81].
- Societal environment: A very small amount of research has been conducted on the topic of the societal environment of blockchain healthcare system structure. For example, there would be a probability of creating collusion for information fraud [61] or it may be limited due to inability to monitor clinical abuses [65,79] acknowledged by their created architecture, which will depend on the user’s nationwide access to the internet connection. One more example is the exclusion of refugees from a country’s healthcare system [57,79].
8.1.4. Ethics and Security
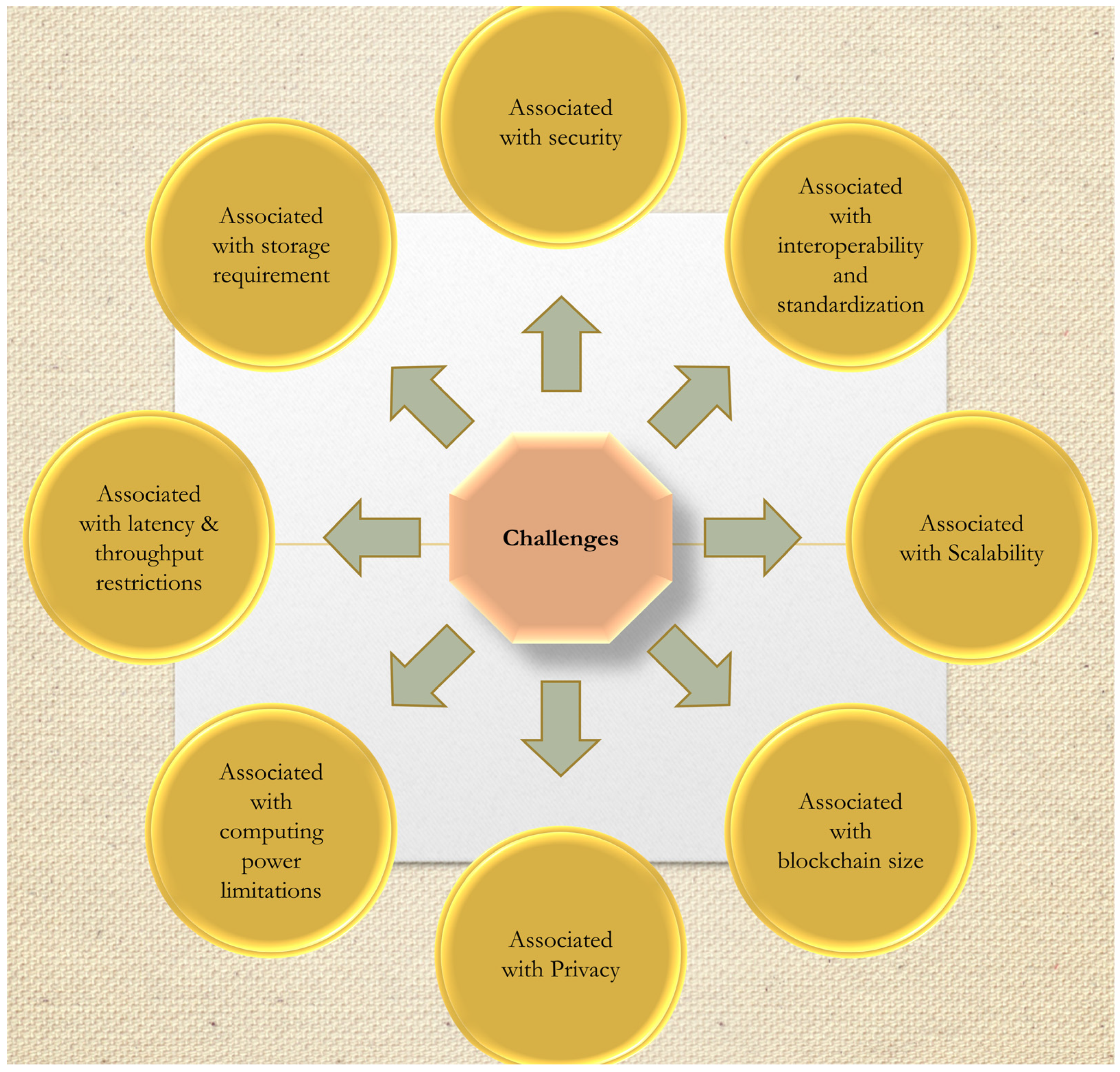
8.2. Challenges
8.2.1. Challenges Associated with Security
8.2.2. Challenges Associated with Interoperability and Standardization
8.2.3. Challenges Associated with Scalability
8.2.4. Challenges Associated with Storage Requirement
8.2.5. Challenges Associated with Computing Power Limitations
8.2.6. Challenges Associated with Blockchain Size
8.2.7. Challenges Associated with Latency and Throughput Restrictions
8.2.8. Challenges Associated with Privacy
8.3. Future Research Directions
8.3.1. Adoption of a Comprehensive Approach
8.3.2. Optimization of the Architecture
8.3.3. Data Security and Legal Compliance
8.3.4. Integration with Various Technologies
9. Conclusions
Author Contributions
Funding
Data Availability Statement
Conflicts of Interest
References
- McClean, S.; Gillespie, J.; Garg, L.; Barton, M.; Scotney, B.; Kullerton, K. Using phase-type models to cost stroke patient care across health, social and community services. Eur. J. Oper. Res. 2014, 236, 190–199. [Google Scholar] [CrossRef]
- Soltanisehat, L.; Alizadeh, R.; Hao, H.; Choo, K.K.R. Technical, Temporal, and Spatial Research Challenges and Opportunities in Blockchain-Based Healthcare: A Systematic Literature Review. IEEE Trans. Eng. Manag. 2023, 70, 353–368. [Google Scholar] [CrossRef]
- Xing, W.; Bei, Y. Medical Health Big Data Classification Based on KNN Classification Algorithm. IEEE Access 2020, 8, 28808–28819. [Google Scholar] [CrossRef]
- Khan, A.A.; Wagan, A.A.; Laghari, A.A.; Gilal, A.R.; Aziz, I.A.; Talpur, B.A. BIoMT: A State-of-the-Art Consortium Serverless Network Architecture for Healthcare System Using Blockchain Smart Contracts. IEEE Access 2022, 10, 78887–78898. [Google Scholar] [CrossRef]
- Quadery, S.E.U.; Hasan, M.; Khan, M.M. Consumer side economic perception of telemedicine during COVID-19 era: A survey on Bangladesh’s perspective. Inform. Med. Unlocked 2021, 27, 100797. [Google Scholar] [CrossRef] [PubMed]
- Tomlinson, M.; Rotheram-Borus, M.J.; Swartz, L.; Tsai, A.C. Scaling up mhealth: Where is the evidence. PLoS Med. 2013, 10, e1001382. [Google Scholar] [CrossRef]
- Chanda, J.N.; Chowdhury, I.A.; Peyaru, M.; Barua, S.; Islam, M.; Hasan, M. Healthcare Monitoring System for Dedicated COVID-19 Hospitals or Isolation Centers. In Proceedings of the 2021 IEEE Mysore Sub Section International Conference (MysuruCon), Hassan, India, 24–25 October 2021; pp. 405–410. [Google Scholar]
- Cagigas, D.; Clifton, J.; Diaz-Fuentes, D.; Fernández-Gutiérrez, M. Blockchain for Public Services: A Systematic Literature Review. IEEE Access 2021, 9, 13904–13921. [Google Scholar] [CrossRef]
- Jabeen, F.; Hamid, Z.; Akhunzada, A.; Abdul, W.; Ghouzali, S. Trust and Reputation Management in Healthcare Systems: Taxonomy, Requirements and Open Issues. IEEE Access 2018, 6, 17246–17263. [Google Scholar] [CrossRef]
- Ghayvat, H.; Pandya, S.; Bhattacharya, P.; Zuhair, M.; Rashid, M.; Hakak, S.; Dev, K. CP-BDHCA: Blockchain-Based Confidentiality-Privacy Preserving Big Data Scheme for Healthcare Clouds and Applications. IEEE J. Biomed. Health Inform. 2022, 26, 1937–1948. [Google Scholar] [CrossRef]
- Wang, S.; Ouyang, L.; Yuan, Y.; Ni, X.; Han, X.; Wang, F.Y. Blockchain-Enabled Smart Contracts: Architecture, Applications, and Future Trends. IEEE Trans. Syst. Man Cybern. Syst. 2019, 49, 2266–2277. [Google Scholar] [CrossRef]
- Khatri, S.; Alzahrani, F.A.; Ansari, M.T.J.; Agrawal, A.; Kumar, R.; Khan, R.A. A Systematic Analysis on Blockchain Integration with Healthcare Domain: Scope and Challenges. IEEE Access 2021, 9, 84666–84687. [Google Scholar] [CrossRef]
- Omar, I.A.; Jayaraman, R.; Debe, M.S.; Salah, K.; Yaqoob, I.; Omar, M. Automating Procurement Contracts in the Healthcare Supply Chain Using Blockchain Smart Contracts. IEEE Access 2021, 9, 37397–37409. [Google Scholar] [CrossRef]
- Shynu, P.G.; Menon, V.G.; Kumar, R.L.; Kadry, S.; Nam, Y. Blockchain-Based Secure Healthcare Application for Diabetic-Cardio Disease Prediction in Fog Computing. IEEE Access 2021, 9, 45706–45720. [Google Scholar] [CrossRef]
- Sun, Z.H.; Chen, Z.; Cao, S.; Ming, X. Potential Requirements and Opportunities of Blockchain-Based Industrial IoT in Supply Chain: A Survey. IEEE Trans. Comput. Soc. Syst. 2022, 9, 1469–1483. [Google Scholar] [CrossRef]
- Fernández-Caramés, T.M.; Fraga-Lamas, P. A Review on the Use of Blockchain for the Internet of Things. IEEE Access 2018, 6, 32979–33001. [Google Scholar] [CrossRef]
- Liu, Q.; Liu, Y.; Luo, M.; He, D.; Wang, H.; Choo, K.-K.R.C. The Security of Blockchain-Based Medical Systems: Research Challenges and Opportunities. IEEE Syst. J. 2022, 16, 5741–5752. [Google Scholar] [CrossRef]
- Wu, G.; Wang, S.; Ning, Z.; Zhu, B. Privacy-Preserved Electronic Medical Record Exchanging and Sharing: A Blockchain-Based Smart Healthcare System. IEEE J. Biomed. Health Inform. 2022, 26, 1917–1927. [Google Scholar] [CrossRef]
- Ahmed, I.; Mousa, A. Security and Privacy Issues in Ehealthcare Systems: Towards Trusted Services. Int. J. Adv. Comput. Sci. Appl. 2016, 7, 229–236. [Google Scholar] [CrossRef]
- Ren, J.; Li, J.; Liu, H.; Qin, T. Task offloading strategy with emergency handling and blockchain security in SDN-empowered and fog-assisted healthcare IoT. Tsinghua Sci. Technol. 2022, 27, 760–776. [Google Scholar] [CrossRef]
- Chinaei, M.H.; Gharakheili, H.H.; Sivaraman, V. Optimal Witnessing of Healthcare IoT Data Using Blockchain Logging Contract. IEEE Internet Things J. 2021, 8, 10117–10130. [Google Scholar] [CrossRef]
- Egala, B.S.; Pradhan, A.K.; Badarla, V.; Mohanty, S.P. Fortified-Chain: A Blockchain-Based Framework for Security and Privacy-Assured Internet of Medical Things With Effective Access Control. IEEE Internet Things J. 2021, 8, 11717–11731. [Google Scholar] [CrossRef]
- Li, P.; Xu, C.; Jin, H.; Hu, C.; Luo, Y.; Cao, Y.; Mathew, J.; Ma, Y. ChainSDI: A Software-Defined Infrastructure for Regulation-Compliant Home-Based Healthcare Services Secured by Blockchains. IEEE Syst. J. 2020, 14, 2042–2053. [Google Scholar] [CrossRef]
- Qahtan, S.; Sharif, K.Y.; Zaidan, A.A.; Alsattar, H.A.; Albahri, O.S.; Zaidan, B.B.; Zulzalil, H.; Osman, M.H.; Alamoodi, A.H.; Mohammed, R.T. Novel Multi Security and Privacy Benchmarking Framework for Blockchain-Based IoT Healthcare Industry 4.0 Systems. IEEE Trans. Ind. Inform. 2022, 18, 6415–6423. [Google Scholar] [CrossRef]
- Kapadiya, K.; Patel, U.; Gupta, R.; Alshehri, M.D.; Tanwar, S.; Sharma, G.; Bokoro, P.N. Blockchain and AI-Empowered Healthcare Insurance Fraud Detection: An Analysis, Architecture, and Future Prospects. IEEE Access 2022, 10, 79606–79627. [Google Scholar] [CrossRef]
- Kumar, R.; Kumar, P.; Tripathi, R.; Gupta, G.P.; Islam, A.N.; Shorfuzzaman, M. Permissioned Blockchain and Deep Learning for Secure and Efficient Data Sharing in Industrial Healthcare Systems. IEEE Trans. Ind. Inform. 2022, 18, 8065–8073. [Google Scholar] [CrossRef]
- Saini, A.; Wijaya, D.; Kaur, N.; Xiang, Y.; Gao, L. LSP: Lightweight Smart-Contract-Based Transaction Prioritization Scheme for Smart Healthcare. IEEE Internet Things J. 2022, 9, 14005–14017. [Google Scholar] [CrossRef]
- Singh, A.P.; Pradhan, N.R.; Luhach, A.K.; Agnihotri, S.; Jhanjhi, N.Z.; Verma, S.; Ghosh, U.; Roy, D.S. A Novel Patient-Centric Architectural Framework for Blockchain-Enabled Healthcare Applications. IEEE Trans. Ind. Inform. 2021, 17, 5779–5789. [Google Scholar] [CrossRef]
- Hasselgren, A.; Kralevska, K.; Gligoroski, D.; Pedersen, S.A.; Faxvaag, A. Blockchain in healthcare and health sciences—A scoping review. Int. J. Med. Inform. 2020, 134, 104040. [Google Scholar] [CrossRef]
- Aujla, G.S.; Jindal, A. A Decoupled Blockchain Approach for Edge-Envisioned IoT-Based Healthcare Monitoring. IEEE J. Sel. Areas Commun. 2021, 39, 491–499. [Google Scholar] [CrossRef]
- Saini, A.; Zhu, Q.; Singh, N.; Xiang, Y.; Gao, L.; Zhang, Y. A Smart-Contract-Based Access Control Framework for Cloud Smart Healthcare System. IEEE Internet Things J. 2021, 8, 5914–5925. [Google Scholar] [CrossRef]
- Akash, S.S.; Ferdous, M.S. A Blockchain Based System for Healthcare Digital Twin. IEEE Access 2022, 10, 50523–50547. [Google Scholar] [CrossRef]
- Bansal, G.; Rajgopal, K.; Chamola, V.; Xiong, Z.; Niyato, D. Healthcare in Metaverse: A Survey on Current Metaverse Applications in Healthcare. IEEE Access 2022, 10, 119914–119946. [Google Scholar] [CrossRef]
- Yazdinejad, A.; Srivastava, G.; Parizi, R.M.; Dehghantanha, A.; Choo, K.K.R.; Aledhari, M. Decentralized Authentication of Distributed Patients in Hospital Networks Using Blockchain. IEEE J. Biomed. Health Inform. 2020, 24, 2146–2156. [Google Scholar] [CrossRef] [PubMed]
- Kumar, Y.; Nakamoto, S. Bitcoin 6.0: Military Grade e-Payment System. SSRN Electron. J. 2020. [Google Scholar] [CrossRef]
- Jolfaei, A.A.; Aghili, S.F.; Singelee, D. A Survey on Blockchain-Based IoMT Systems: Towards Scalability. IEEE Access 2021, 9, 148948–148975. [Google Scholar] [CrossRef]
- Dinh, T.T.A.; Liu, R.; Zhang, M.; Chen, G.; Ooi, B.C.; Wang, J. Untangling Blockchain: A Data Processing View of Blockchain Systems. IEEE Trans. Knowl. Data Eng. 2018, 30, 1366–1385. [Google Scholar] [CrossRef]
- Anoaica, A.; Levard, H. Quantitative Description of Internal Activity on the Ethereum Public Blockchain. In Proceedings of the 2018 9th IFIP international conference on New technologies, Mobility and security (NTMS), Paris, France, 26–28 February 2018; pp. 1–5. [Google Scholar]
- Feng, L.; Zhang, H.; Tsai, W.T.; Sun, S. System architecture for high-performance permissioned blockchains. Front. Comput. Sci. 2019, 13, 1151–1165. [Google Scholar] [CrossRef]
- Khan, C.; Lewis, A.; Rutland, E.; Wan, C.; Rutter, K.; Thompson, C. A Distributed-Ledger Consortium Model for Collaborative Innovation. Computer 2017, 50, 29–37. [Google Scholar] [CrossRef]
- King, S.; Nadal, S. PPCoin: Peer-to-Peer Crypto-Currency with Proof-of-Stake. In Proceedings of the 2016 ACM SIGSAC Conference on Computer and Communications Security—CCS’16, Vienna, Austria, 24–28 October 2016; Volume 1918, pp. 1–27. [Google Scholar]
- Feng, Q.; He, D.; Zeadally, S.; Khan, M.K.; Kumar, N. A survey on privacy protection in blockchain system. J. Netw. Comput. Appl. 2019, 126, 45–58. [Google Scholar] [CrossRef]
- Fahim, A.; Hasan, M.; Chowdhury, M.A. Smart parking systems: Comprehensive review based on various aspects. Heliyon 2021, 7, e07050. [Google Scholar] [CrossRef]
- Hasan, M.; Biswas, P.; Bilash, M.T.I.; Dipto, M.A.Z. Smart Home Systems: Overview and Comparative Analysis. In Proceedings of the 2018 Fourth International Conference on Research in Computational Intelligence and Communication Networks (ICRCICN), Kolkata, India, 22–23 November 2018; pp. 264–268. [Google Scholar]
- Järvelin, K.; Vakkari, P. LIS research across 50 years: Content analysis of journal articles. J. Doc. 2021, 78, 65–88. [Google Scholar] [CrossRef]
- Murthy, C.V.B.; Shri, M.L.; Kadry, S.; Lim, S. Blockchain based cloud computing: Architecture and research challenges. IEEE Access 2020, 8, 205190–205205. [Google Scholar] [CrossRef]
- Acquah, M.A.; Chen, N.; Pan, J.S.; Yang, H.M.; Yan, B. Securing fingerprint template using blockchain and distributed storage system. Symmetry 2020, 12, 951. [Google Scholar] [CrossRef]
- Yang, J.; Onik, M.M.H.; Lee, N.Y.; Ahmed, M.; Kim, C.S. Proof-of-familiarity: A privacy-preserved blockchain scheme for collaborative medical decision-making. Appl. Sci. 2019, 9, 1370. [Google Scholar] [CrossRef]
- Lee, T.F.; Li, H.Z.; Hsieh, Y.P. A blockchain-based medical data preservation scheme for telecare medical information systems. Int. J. Inf. Secur. 2021, 20, 589–601. [Google Scholar] [CrossRef]
- Sang, Z.; Yang, K.; Zhang, R. A security technology of power relay using edge computing. PLoS ONE 2021, 16, e0253428. [Google Scholar] [CrossRef] [PubMed]
- Zhou, L.; Wang, L.; Sun, Y. MIStore: A Blockchain-Based Medical Insurance Storage System. J. Med. Syst. 2018, 42, 149. [Google Scholar] [CrossRef]
- Ejaz, M.; Kumar, T.; Kovacevic, I.; Ylianttila, M.; Harjula, E. Health-blockedge: Blockchain-edge framework for reliable low-latency digital healthcare applications. Sensors 2021, 21, 2502. [Google Scholar] [CrossRef]
- Suma, B.; Murali, G. Blockchain usage in the electronic health record system using attribute-based signature. Int. J. Recent Technol. Eng. 2019, 8, 993–997. [Google Scholar]
- Natarajan, B.; Balaji, K. Medical Data Management Using Blockchain. J. ISMAC 2020, 2, 222–231. [Google Scholar]
- Magyar, G. Blockchain: Solving the privacy and research availability tradeoff for EHR data: A new disruptive technology in health data management. In Proceedings of the 2017 IEEE 30th Neumann Colloquium (NC), Budapest, Hungary, 24–25 November 2017; pp. 135–140. [Google Scholar]
- Azaria, A.; Ekblaw, A.; Vieira, T.; Lippman, A. MedRec: Using Blockchain for Medical Data Access and Permission Management. In Proceedings of the 2016 2nd International Conference on Open and Big Data (OBD), Vienna, Austria, 22–24 August 2016; pp. 25–30. [Google Scholar]
- Islam, N.; Faheem, Y.; Din, I.U.; Talha, M.; Guizani, M.; Khalil, M. A blockchain-based fog computing framework for activity recognition as an application to e-Healthcare services. Future Gener. Comput. Syst. 2019, 100, 569–578. [Google Scholar] [CrossRef]
- Fan, K.; Wang, S.; Ren, Y.; Yang, K.; Yan, Z.; Li, H.; Yang, Y. Blockchain-Based Secure Time Protection Scheme in IoT. IEEE Internet Things J. 2019, 6, 4671–4679. [Google Scholar] [CrossRef]
- Jamil, F.; Ahmad, S.; Iqbal, N.; Kim, D.H. Towards a remote monitoring of patient vital signs based on iot-based blockchain integrity management platforms in smart hospitals. Sensors 2020, 20, 2195. [Google Scholar] [CrossRef] [PubMed]
- Mohammed, R.; Alubady, R.; Sherbaz, A. Utilizing blockchain technology for IoT-based healthcare systems. J. Phys. Conf. Ser. 2021, 1818, 012111. [Google Scholar] [CrossRef]
- Hirano, T.; Motohashi, T.; Okumura, K.; Takajo, K.; Kuroki, T.; Ichikawa, D.; Matsuoka, Y.; Ochi, E.; Ueno, T. Data validation and verification using blockchain in a clinical trial for breast cancer: Regulatory sandbox. J. Med. Internet Res. 2020, 22, e18938. [Google Scholar] [CrossRef]
- Lee, S.J.; Cho, G.Y.; Ikeno, F.; Lee, T.R. BAQALC: Blockchain applied lossless efficient transmission of DNA sequencing data for next generation medical informatics. Appl. Sci. 2018, 8, 1471. [Google Scholar] [CrossRef]
- Tagde, P.; Tagde, S.; Bhattacharya, T.; Tagde, P.; Chopra, H.; Akter, R.; Kaushik, D.; Rahman, M. Blockchain and artificial intelligence technology in e-Health. Environ. Sci. Pollut. Res. 2021, 28, 52810–52831. [Google Scholar] [CrossRef]
- Noh, S.W.; Park, Y.; Sur, C.; Shin, S.U.; Rhee, K.H. Blockchain-Based User-Centric Records Management System. Int. J. Control Autom. 2017, 10, 133–144. [Google Scholar] [CrossRef]
- Zhang, P.; White, J.; Schmidt, D.C.; Lenz, G.; Rosenbloom, S.T. FHIRChain: Applying Blockchain to Securely and Scalably Share Clinical Data. Comput. Struct. Biotechnol. J. 2018, 16, 267–278. [Google Scholar] [CrossRef]
- Farahani, B.; Firouzi, F.; Luecking, M. The convergence of IoT and distributed ledger technologies (DLT): Opportunities, challenges, and solutions. J. Netw. Comput. Appl. 2021, 177, 102936. [Google Scholar] [CrossRef]
- Chenthara, S.; Ahmed, K.; Wang, H.; Whittaker, F.; Chen, Z. Healthchain: A novel framework on privacy preservation of electronic health records using blockchain technology. PLoS ONE 2020, 15, e0243043. [Google Scholar] [CrossRef] [PubMed]
- Kuo, T.T.; Gabriel, R.A.; Ohno-Machado, L. Fair compute loads enabled by blockchain: Sharing models by alternating client and server roles. J. Am. Med. Inform. Assoc. 2019, 26, 392–403. [Google Scholar] [CrossRef] [PubMed]
- Hasselgren, A.; Rensaa, J.A.H.; Kralevska, K.; Gligoroski, D.; Faxvaag, A. Blockchain for increased trust in virtual health care: Proof-of-concept study. J. Med. Internet Res. 2021, 23, e28496. [Google Scholar] [CrossRef] [PubMed]
- Hemalatha, P. Monitoring and Securing the Healthcare Data Harnessing IOT and Blockchain Technology. Turk. J. Comput. Math. Educ. 2021, 12, 2554–2561. [Google Scholar]
- Cao, Y.; Sun, Y.; Min, J. Hybrid blockchain–based privacy-preserving electronic medical records sharing scheme across medical information control system. Meas. Control. 2020, 53, 1286–1299. [Google Scholar] [CrossRef]
- Casado-Vara, R.; Corchado, J. Distributed e-health wide-world accounting ledger via blockchain. J. Intell. Fuzzy Syst. 2019, 36, 2381–2386. [Google Scholar] [CrossRef]
- Hyla, T.; Pejaś, J. eHealth integrity model based on permissioned blockchain. Future Internet 2019, 11, 76. [Google Scholar] [CrossRef]
- Guo, Y.; Li, Y.; Wang, F.; Wei, Y.; Rong, Z. Processes controlling sea surface temperature variability of ningaloo niño. J. Clim. 2020, 33, 4369–4389. [Google Scholar] [CrossRef]
- Wang, S.; Wang, J.; Wang, X.; Qiu, T.; Yuan, Y.; Ouyang, L.; Guo, Y.; Wang, F. Blockchain-Powered Parallel Healthcare Systems Based on the ACP Approach. IEEE Trans. Comput. Soc. Syst. 2018, 5, 942–950. [Google Scholar] [CrossRef]
- Shrestha, A.K.; Vassileva, J.; Deters, R. A Blockchain Platform for User Data Sharing Ensuring User Control and Incentives. Front. Blockchain 2020, 3, 497985. [Google Scholar] [CrossRef]
- Bokefode, J.D.; Komarasamy, G. A remote patient monitoring system: Need, trends, challenges and opportunities. Int. J. Sci. Technol. Res. 2019, 8, 830–835. [Google Scholar]
- CSuwanposri, C.; Bhatiasevi, V.; Thanakijsombat, T. Drivers of Blockchain Adoption in Financial and Supply Chain Enterprises. Glob. Bus. Rev. 2021. [Google Scholar] [CrossRef]
- Haleem, A.; Javaid, M.; Singh, R.P.; Suman, R.; Rab, S. Blockchain technology applications in healthcare: An overview. Int. J. Intell. Netw. 2021, 2, 130–139. [Google Scholar] [CrossRef]
- Le Nguyen, B.; Lydia, E.L.; Elhoseny, M.; Pustokhina, I.; Pustokhin, D.A.; Selim, M.M.; Nguyen, G.N.; Shankar, K. Privacy preserving blockchain technique to achieve secure and reliable sharing of IoT data. Comput. Mater. Contin. 2020, 65, 87–107. [Google Scholar] [CrossRef]
- PPandey, P.; Litoriya, R. Securing and authenticating healthcare records through blockchain technology. Cryptologia 2020, 44, 341–356. [Google Scholar] [CrossRef]
- Nagasubramanian, G.; Sakthivel, R.K.; Patan, R.; Gandomi, A.H.; Sankayya, M.; Balusamy, B. Securing e-health records using keyless signature infrastructure blockchain technology in the cloud. Neural Comput. Appl. 2020, 32, 639–647. [Google Scholar] [CrossRef]
- Roehrs, A.; da Costa, C.A.; Righi, R.R.; Mayer, A.H.; da Silva, V.F.; Goldim, J.R.; Schmidt, D.C. Integrating multiple blockchains to support distributed personal health records. Health Inform. J. 2021, 27, 14604582211007546. [Google Scholar] [CrossRef]
- Ijaz, M.; Li, G.; Lin, L.; Cheikhrouhou, O.; Hamam, H.; Noor, A. Integration and applications of fog computing and cloud computing based on the internet of things for provision of healthcare services at home. Electronics 2021, 10, 1077. [Google Scholar] [CrossRef]
- Chukwu, E.; Garg, L. A systematic review of blockchain in healthcare: Frameworks, prototypes, and implementations. IEEE Access 2020, 8, 21196–21214. [Google Scholar] [CrossRef]
- Taralunga, D.D.; Florea, B.C. A blockchain-enabled framework for mhealth systems. Sensors 2021, 21, 2828. [Google Scholar] [CrossRef]
- Chen, Y.; Meng, L.; Zhou, H.; Xue, G. A Blockchain-Based Medical Data Sharing Mechanism with Attribute-Based Access Control and Privacy Protection. Wirel. Commun. Mob. Comput. 2021, 2021, 6685762. [Google Scholar] [CrossRef]
- Fang, W.; Chen, W.; Zhang, W.; Pei, J.; Gao, W.; Wang, G. Digital signature scheme for information non-repudiation in blockchain: A state of the art review. EURASIP J. Wirel. Commun. Netw. 2020, 2020, 56. [Google Scholar] [CrossRef]
- Ray, P.P.; Dash, D.; Salah, K.; Kumar, N. Blockchain for IoT-Based Healthcare: Background, Consensus, Platforms, and Use Cases. IEEE Syst. J. 2021, 15, 85–94. [Google Scholar] [CrossRef]
- Sivan, R.; Zukarnain, Z.A. Security and privacy in cloud-based e-health system. Symmetry 2021, 13, 742. [Google Scholar] [CrossRef]
- Hölbl, M.; Kompara, M.; Kamišalić, A.; Nemec Zlatolas, L. A systematic review of the use of blockchain in healthcare. Symmetry 2018, 10, 470. [Google Scholar] [CrossRef]
- Patane, R.; Nadar, A.; Dubey, V.; Nadar, C. Medical Data Access and Permission Management Using BlockChain. JETIR Res. J. 2019, 6, 655–658. [Google Scholar]
- Praveen, G. The Impact of Blockchain on the Healthcare Environment. J. Inform. Electr. Electron. Eng. 2021, 2, 1–11. [Google Scholar] [CrossRef]
- Xia, Q.I.; Sifah, E.B.; Asamoah, K.O.; Gao, J.; Du, X.; Guizani, M. MeDShare: Trust-Less Medical Data Sharing Among Cloud Service Providers via Blockchain. IEEE Access 2017, 5, 14757–14767. [Google Scholar] [CrossRef]
- Yehualashet, D.E.; Seboka, B.T.; Tesfa, G.A.; Demeke, A.D.; Amede, E.S. Barriers to the adoption of electronic medical record system in ethiopia: A systematic review. J. Multidiscip. Healthc. 2021, 14, 2597–2603. [Google Scholar] [CrossRef]
- Mayer, A.H.; da Costa, C.A.; Righi, R.D.R. Electronic health records in a Blockchain: A systematic review. Health Inform. J. 2020, 26, 1273–1288. [Google Scholar] [CrossRef]
- Blocki, J.; Harsha, B.; Kang, S.; Lee, S.; Xing, L.; Zhou, S. Data-Independent Memory Hard Functions: New Attacks and Stronger Constructions. In Lecture Notes in Computer Science; Springer: Cham, Switzerland, 2019; pp. 573–607. [Google Scholar]
- Abdellatif, A.A.; Samara, L.; Mohamed, A.; Erbad, A.; Chiasserini, C.F.; Guizani, M.; Dennis, M. MEdge-Chain: Leveraging Edge Computing and Blockchain for Efficient Medical Data Exchange. IEEE Internet Things J. 2021, 8, 15762–15775. [Google Scholar] [CrossRef]
- Yadav, S.; Rishi, R. A Systematic and Critical Analysis of the Developments in the Field of Intelligent Transportation System. Adv. Dyn. Syst. Appl. 2021, 16, 901–911. [Google Scholar] [CrossRef]
- Hasan, H.R.; Salah, K.; Jayaraman, R.; Omar, M.; Yaqoob, I.; Pesic, S.; Taylor, T.; Boscovic, D. A Blockchain-Based Approach for the Creation of Digital Twins. IEEE Access 2020, 8, 34113–34126. [Google Scholar] [CrossRef]
- Kumar, A.; Krishnamurthi, R.; Nayyar, A.; Sharma, K.; Grover, V.; Hossain, E. A Novel Smart Healthcare Design, Simulation, and Implementation Using Healthcare 4.0 Processes. IEEE Access 2020, 8, 118433–118471. [Google Scholar] [CrossRef]
- Patel, V. A framework for secure and decentralized sharing of medical imaging data via blockchain consensus. Health Inform. J. 2019, 25, 1398–1411. [Google Scholar] [CrossRef]
- Zhuang, Y.; Sheets, L.R.; Chen, Y.-W.; Shae, Z.-Y.; Tsai, J.J.P.; Shyu, C.-R. A Patient-Centric Health Information Exchange Framework Using Blockchain Technology. IEEE J. Biomed. Health Inform. 2020, 24, 2169–2176. [Google Scholar] [CrossRef]
- Tawalbeh, L.A.; Muheidat, F.; Tawalbeh, M.; Quwaider, M. IoT Privacy and Security: Challenges and Solutions. Appl. Sci. 2020, 10, 4102. [Google Scholar] [CrossRef]
- Shi, S.; He, D.; Li, L.; Kumar, N.; Khan, M.K.; Choo, K.K.R. Applications of blockchain in ensuring the security and privacy of electronic health record systems: A survey. Comput. Secur. 2020, 97, 101966. [Google Scholar] [CrossRef]
- da Fonseca Ribeiro, M.I.; Vasconcelos, A. MedBlock: Using blockchain in health healthcare application based on blockchain and smart contracts. In Proceedings of the 22nd International Conference on Enterprise Information Systems (ICEIS 2020), Online Streaming, 5–7 May 2020; Volume 1, pp. 156–164. [Google Scholar]
- De Aguiar, E.J.; Faiçal, B.S.; Krishnamachari, B.; Ueyama, J. A Survey of Blockchain-Based Strategies for Healthcare. ACM Comput. Surv. 2020, 53, 27. [Google Scholar] [CrossRef]
- Wang, Z.; Wang, L.; Chen, Q.; Lu, L.; Hong, J. A traditional Chinese medicine traceability system based on lightweight blockchain. J. Med. Internet Res. 2021, 23, e25946. [Google Scholar] [CrossRef]
- Velmovitsky, P.E.; Souza, P.A.D.S.E.; Vaillancourt, H.; Donovska, T.; Teague, J.; Morita, P.P. A blockchain-based consent platform for active assisted living: Modeling study and conceptual framework. J. Med. Internet Res. 2020, 22, e20832. [Google Scholar] [CrossRef]
- Tomlinson, B.; Boberg, J.; Cranefield, J.; Johnstone, D.; Luczak-Roesch, M.; Patterson, D.J.; Kapoor, S. Analyzing the sustainability of 28 ‘Blockchain for Good’ projects via affordances and constraints. Inf. Technol. Dev. 2021, 27, 439–469. [Google Scholar] [CrossRef]
- Wang, Y.C.; Ganzorig, B.; Wu, C.C.; Iqbal, U.; Khan, H.A.A.; Hsieh, W.S.; Jian, W.S.; Li, Y.C.J. Patient satisfaction with dermatology teleconsultation by using MedX. Comput. Methods Programs Biomed. 2018, 167, 37–42. [Google Scholar] [CrossRef]
- Salahuddin, M.A.; Al-Fuqaha, A.; Guizani, M.; Shuaib, K.; Sallabi, F. Softwarization of Internet of Things Infrastructure for Secure and Smart Healthcare. Computer 2017, 50, 74–79. [Google Scholar] [CrossRef]
- Oyinloye, D.P.; Teh, J.S.; Jamil, N.; Alawida, M. Blockchain consensus: An overview of alternative protocols. Symmetry 2021, 13, 1363. [Google Scholar] [CrossRef]
- Cachin, C.; Schubert, S.; Vukolić, M. Non-determinism in Byzantine fault-tolerant replication. Leibniz Int. Proc. Inform. LIPIcs 2017, 70, 24.1–24.16. [Google Scholar]
- Salimitari, M.; Chatterjee, M.; Fallah, Y.P. A survey on consensus methods in blockchain for resource-constrained IoT networks. Internet Things 2020, 11, 100212. [Google Scholar] [CrossRef]
- Wang, X.; Zha, X.; Ni, W.; Liu, R.P.; Guo, Y.J.; Niu, X.; Zheng, K. Survey on blockchain for Internet of Things. Comput. Commun. 2019, 136, 10–29. [Google Scholar] [CrossRef]
- Lee, Y.; Rathore, S.; Park, J.H.; Park, J.H. A blockchain-based smart home gateway architecture for preventing data forgery. Hum. Cent. Comput. Inf. Sci. 2020, 10, 9. [Google Scholar] [CrossRef]
- de Oliveira Fornasier, M. The applicability of the Internet of Things (IoT) between fundamental rights to health and to privacy. Rev. Investig. Const. 2019, 6, 297–321. [Google Scholar]
- Li, H.; Yu, L.; He, W. The Impact of GDPR on Global Technology Development. J. Glob. Inf. Technol. Manag. 2019, 22, 1–6. [Google Scholar] [CrossRef]
- Vanderpool, D. HIPAA COMPLIANCE: A Common Sense Approach. Innov. Clin. Neurosci. 2019, 16, 38–41. [Google Scholar] [PubMed]
- Hussain, S.Z.; Kumar, M. Secured Key Agreement Schemes in Wireless Body Area Network—A Review. Indian J. Sci. Technol. 2021, 14, 2005–2033. [Google Scholar] [CrossRef]
- Salem, O.; Alsubhi, K.; Mehaoua, A.; Boutaba, R. Markov Models for Anomaly Detection in Wireless Body Area Networks for Secure Health Monitoring. IEEE J. Sel. Areas Commun. 2021, 39, 526–540. [Google Scholar] [CrossRef]
- Taiwo, O.; Ezugwu, A.E. Smart healthcare support for remote patient monitoring during COVID-19 quarantine. Inform. Med. Unlocked 2020, 20, 100428. [Google Scholar] [CrossRef] [PubMed]
- Huang, G.; al Foysal, A. Blockchain in Healthcare. Technol. Invest. 2021, 12, 168–181. [Google Scholar] [CrossRef]
- Uddin, M.A.; Stranieri, A.; Gondal, I.; Balasubramanian, V. Continuous Patient Monitoring with a Patient Centric Agent: A Block Architecture. IEEE Access 2018, 6, 32700–32726. [Google Scholar] [CrossRef]
- Fatokun, T.; Nag, A.; Sharma, S. Towards a blockchain assisted patient owned system for electronic health records. Electronics 2021, 10, 580. [Google Scholar] [CrossRef]
- Chang, S.E.; Chen, Y.C. Blockchain in health care innovation: Literature review and case study from a business ecosystem perspective. J. Med. Internet Res. 2020, 22, e19480. [Google Scholar] [CrossRef] [PubMed]
- Gope, P.; Gheraibia, Y.; Kabir, S.; Sikdar, B. A Secure IoT-Based Modern Healthcare System with Fault-Tolerant Decision Making Process. IEEE J. Biomed. Health Inform. 2021, 25, 862–873. [Google Scholar] [CrossRef]
- Alamri, B.; Crowley, K.; Richardson, I. Blockchain-Based Identity Management Systems in Health IoT: A Systematic Review. IEEE Access 2022, 10, 59612–59629. [Google Scholar] [CrossRef]
- Saxena, S.; Bhushan, B.; Ahad, M.A. Blockchain based solutions to secure IoT: Background, integration trends and a way forward. J. Netw. Comput. Appl. 2021, 181, 103050. [Google Scholar] [CrossRef]
- Velmovitsky, P.E.; Bublitz, F.M.; Fadrique, L.X.; Morita, P.P. Blockchain applications in health care and public health: Increased transparency. JMIR Med. Inform. 2021, 9, e20713. [Google Scholar] [CrossRef]
- Mettler, M.; Hsg, M.A. Blockchain technology in healthcare: The revolution starts here. In Proceedings of the 2016 IEEE 18th International Conference on e-Health Networking, Applications and Services (Healthcom), Munich, Germany, 14–16 September 2016; pp. 16–18. [Google Scholar]
- Boulos, M.N.K.; Wilson, J.T.; Clauson, K.A. Geospatial blockchain: Promises, challenges, and scenarios in health and healthcare. Int. J. Health Geogr. 2018, 17, 25. [Google Scholar] [CrossRef] [PubMed]
- Johny, S.; Priyadharsini, C. Investigations on the Implementation of Blockchain Technology in Supplychain Network. In Proceedings of the 2021 7th International Conference on Advanced Computing and Communication Systems (ICACCS), Coimbatore, India, 19–20 March 2021; pp. 1–6. [Google Scholar] [CrossRef]
- Ahmad, R.W.; Salah, K.; Jayaraman, R.; Yaqoob, I.; Ellahham, S.; Omar, M. The role of blockchain technology in telehealth and telemedicine. Int. J. Med. Inform. 2021, 148, 104399. [Google Scholar] [CrossRef] [PubMed]
- Rejeb, A.; Treiblmaier, H.; Rejeb, K.; Zailani, S. Blockchain research in healthcare: A bibliometric review and current research trends. J. Data Inf. Manag. 2021, 3, 109–124. [Google Scholar] [CrossRef]
- Pajooh, H.H.; Rashid, M.; Alam, F.; Demidenko, S. Hyperledger Fabric Blockchain for Securing the Edge Internet of Things. Sensors 2021, 21, 359. [Google Scholar] [CrossRef]
- Hellani, H.; Sliman, L.; Samhat, A.; Exposito, E. On Blockchain Integration with Supply Chain: Overview on Data Transparency. Logistics 2021, 5, 46. [Google Scholar] [CrossRef]
- Mackey, T.K.; Nayyar, G. A review of existing and emerging digital technologies to combat the global trade in fake medicines. Expert Opin. Drug Saf. 2017, 16, 587–602. [Google Scholar] [CrossRef]
- Mann, S.P.; Savulescu, J.; Ravaud, P.; Benchoufi, M. Blockchain, consent and present for medical research. J. Med. Ethic 2020, 47, 244–250. [Google Scholar] [CrossRef]
- Lee, H.A.; Kung, H.H.; Udayasankaran, J.G.; Kijsanayotin, B.; Marcelo, A.B.; Chao, L.R.; Hsu, C.Y. An architecture and management platform for blockchain-based personal health record exchange: Development and usability study. J. Med. Internet Res. 2020, 22, e16748. [Google Scholar] [CrossRef] [PubMed]
- Hang, L.; Kim, B.; Kim, K.; Kim, D. A Permissioned Blockchain-Based Clinical Trial Service Platform to Improve Trial Data Transparency. BioMed Res. Int. 2021, 2021, 5554487. [Google Scholar] [CrossRef] [PubMed]
- Roman-Belmonte, J.M.; De La Corte-Rodriguez, H.; Rodriguez-Merchan, E.C. How blockchain technology can change medicine. Postgrad. Med. 2018, 130, 420–427. [Google Scholar] [CrossRef] [PubMed]
- Rensaa, J.A.H.; Gligoroski, D.; Kralevska, K.; Hasselgren, A.; Faxvaag, A. VerifyMed-A blockchain platform for transparent trust in virtualized healthcare: Proof-of-concept. In Proceedings of the 2nd International Electronics Communication Conference (IECC 20), Singapore, 8–10 July 2020; pp. 73–80. [Google Scholar]
- Omar, I.A.; Jayaraman, R.; Salah, K.; Simsekler, M.C.E.; Yaqoob, I.; Ellahham, S. Ensuring protocol compliance and data transparency in clinical trials using Blockchain smart contracts. BMC Med. Res. Methodol. 2020, 20, 224. [Google Scholar] [CrossRef]
- Khan, S.N.; Loukil, F.; Ghedira-Guegan, C.; Benkhelifa, E.; Bani-Hani, A. Blockchain smart contracts: Applications, challenges, and future trends. Peer Peer Netw. Appl. 2021, 14, 2901–2925. [Google Scholar] [CrossRef]
- Kleinaki, A.-S.; Mytis-Gkometh, P.; Drosatos, G.; Efraimidis, P.S.; Kaldoudi, E. A Blockchain-Based Notarization Service for Biomedical Knowledge Retrieval. Comput. Struct. Biotechnol. J. 2018, 16, 288–297. [Google Scholar] [CrossRef]
- Sharma, A.; Kaur, S.; Singh, M. A comprehensive review on blockchain and Internet of Things in healthcare. Trans. Emerg. Telecommun. Technol. 2021, 32, e4333. [Google Scholar] [CrossRef]
- Zhang, J.; Xue, N.; Huang, X. A Secure System For Pervasive Social Network-Based Healthcare. IEEE Access 2016, 4, 9239–9250. [Google Scholar] [CrossRef]
- Weiss, M.; Botha, A.; Herselman, M.; Loots, G. Blockchain as an enabler for public mHealth solutions in South Africa. In Proceedings of the 2017 IST-Africa Week Conference, Windhoek, Namibia, 31 May–2 June 2017; pp. 1–8. [Google Scholar] [CrossRef]
- Jabarulla, M.Y.; Lee, H.-N. Healthcare System for Combating the COVID-19 Pandemic: Opportunities and Applications. Healthcare 2021, 9, 1019. [Google Scholar] [CrossRef]
- Liang, X.; Zhao, J.; Shetty, S.; Liu, J.; Li, D. Integrating blockchain for data sharing and collaboration in mobile healthcare applications. In Proceedings of the 2017 IEEE 28th Annual International Symposium on Personal, Indoor, and Mobile Radio Communications (PIMRC), Montreal, QC, Canada, 8–13 October 2017; pp. 1–5. [Google Scholar] [CrossRef]
- Rodriguez-León, C.; Villalonga, C.; Munoz-Torres, M.; Ruiz, J.R.; Banos, O. Mobile and wearable technology for the monitoring of diabetes-related parameters: Systematic review. JMIR Mhealth Uhealth 2021, 9, e25138. [Google Scholar] [CrossRef]
- Ichikawa, D.; Kashiyama, M.; Ueno, T. Tamper-Resistant Mobile Health Using Blockchain Technology. JMIR mHealth uHealth 2017, 5, e111. [Google Scholar] [CrossRef] [PubMed]
- Paganelli, A.I.; Velmovitsky, P.E.; Miranda, P.; Branco, A.; Alencar, P.; Cowan, D.; Endler, M.; Morita, P.P. A conceptual IoT-based early-warning architecture for remote monitoring of COVID-19 patients in wards and at home. Internet Things 2021, 18, 100399. [Google Scholar] [CrossRef]
- Firdaus, A.; Anuar, N.B.; Ab Razak, M.F.; Hashem, I.A.T.; Bachok, S.; Sangaiah, A.K. Root Exploit Detection and Features Optimization: Mobile Device and Blockchain Based Medical Data Management. J. Med Syst. 2018, 42, 112. [Google Scholar] [CrossRef] [PubMed]
- Alkhateeb, Y.M. Blockchain Implications in the Management of Patient Complaints in Healthcare. J. Inf. Secur. 2021, 12, 212–223. [Google Scholar] [CrossRef]
- Kamenivskyy, Y.; Palisetti, A.; Hamze, L.; Saberi, S. A Blockchain-Based Solution for COVID-19 Vaccine Distribution. IEEE Eng. Manag. Rev. 2022, 50, 43–53. [Google Scholar] [CrossRef]
- Bhadoria, R.S.; Das, A.P.; Bashar, A.; Zikria, M. Implementing Blockchain-Based Traceable Certificates as Sustainable Technology in Democratic Elections. Electronics 2022, 11, 3359. [Google Scholar] [CrossRef]
- Kasyap, H.; Tripathy, S. Privacy-preserving Decentralized Learning Framework for Healthcare System. ACM Trans. Multimed. Comput. Commun. Appl. 2021, 17, 1–24. [Google Scholar] [CrossRef]
- Agbo, C.C.; Mahmoud, Q.H.; Eklund, J.M. Blockchain Technology in Healthcare: A Systematic Review. Healthcare 2019, 7, 56. [Google Scholar] [CrossRef]
- Ray, P.P.; Chowhan, B.; Kumar, N.; Almogren, A. BIoTHR: Electronic Health Record Servicing Scheme in IoT-Blockchain Ecosystem. IEEE Internet Things J. 2021, 8, 10857–10872. [Google Scholar] [CrossRef]
- Gadekallu, T.R.; Manoj, M.K.; Kumar, N.; Hakak, S.; Bhattacharya, S. Blockchain-Based Attack Detection on Machine Learning Algorithms for IoT-Based e-Health Applications. IEEE Internet Things Mag. 2021, 4, 30–33. [Google Scholar] [CrossRef]
- Khatoon, A. A Blockchain-Based Smart Contract System for Healthcare Management. Electronics 2020, 9, 94. [Google Scholar] [CrossRef]
- Kaur, H.; Alam, M.A.; Jameel, R.; Mourya, A.K.; Chang, V. A Proposed Solution and Future Direction for Blockchain-Based Heterogeneous Medicare Data in Cloud Environment. J. Med. Syst. 2018, 42, 156. [Google Scholar] [CrossRef] [PubMed]
- Li, F.; Liu, K.; Zhang, L.; Huang, S.; Wu, Q. EHRChain: A Blockchain-Based EHR System Using Attribute-Based and Homomorphic Cryptosystem. IEEE Trans. Serv. Comput. 2021, 15, 2755–2765. [Google Scholar] [CrossRef]
- Jiang, S.; Jakobsen, K.; Bueie, J.; Li, J.; Haro, P.H. A Tertiary Review on Blockchain and Sustainability With Focus on Sus-tainable Development Goals. IEEE Access 2022, 10, 114975–115006. [Google Scholar] [CrossRef]
- Sun, J.; Ren, L.; Wang, S.; Yao, X. A blockchain-based framework for electronic medical records sharing with fine-grained access control. PLoS ONE 2020, 15, e0239946. [Google Scholar] [CrossRef]
- Kaur, J.; Rani, R.; Kalra, N. Blockchain-based framework for secured storage, sharing, and querying of electronic healthcare records. Concurr. Comput. Pract. Exp. 2021, 33, e6369. [Google Scholar] [CrossRef]
- Alabdulkarim, Y.; Alameer, A.; Almukaynizi, M.; Almaslukh, A. SPIN: A Blockchain-Based Framework for Sharing COVID-19 Pandemic Information across Nations. Appl. Sci. 2021, 11, 8767. [Google Scholar] [CrossRef]
- Touloupou, M.; Themistocleous, M.; Iosif, E.; Christodoulou, K. A Systematic Literature Review Toward a Blockchain Benchmarking Framework. IEEE Access 2022, 10, 70630–70644. [Google Scholar] [CrossRef]
- Wang, Q.; Xia, T.; Ren, Y.; Yuan, L.; Miao, G. A New Blockchain-Based Multi-Level Location Secure Sharing Scheme. Appl. Sci. 2021, 11, 2260. [Google Scholar] [CrossRef]
- Huang, A.W.; Kandula, A.; Wang, X. A Differential-Privacy-Based Blockchain Architecture to Secure and Store Electronic Health Records. In Proceedings of the 3rd International Conference on Blockchain Technology, Shanghai, China, 26–28 March 2021; pp. 189–194. [Google Scholar]
- Dauda, I.; Nuhu, B.; Abubakar, J.; Abdullahi, I.; Maliki, D. Blockchain Technology in Healthcare Systems: Applications, Methodology, Problems, and Current Trends. J. Sci. Technol. Educ. 2021, 9, 431–443. [Google Scholar]
- Angeletti, F.; Chatzigiannakis, I.; Vitaletti, A. The role of blockchain and IoT in recruiting participants for digital clinical trials. In Proceedings of the 2017 25th International Conference on Software, Telecommunications and Computer Networks (SoftCOM), Split, Croatia, 21–23 September 2017; pp. 1–5. [Google Scholar] [CrossRef]
- Ali, M.S.; Vecchio, M.; Putra, G.D.; Kanhere, S.S.; Antonelli, F. A Decentralized Peer-to-Peer Remote Health Monitoring System. Sensors 2020, 20, 1656. [Google Scholar] [CrossRef] [PubMed]
- Ali, A.; Rahim, H.A.; Pasha, M.F.; Dowsley, R.; Masud, M.; Ali, J.; Baz, M. Security, Privacy, and Reliability in Digital Healthcare Systems Using Blockchain. Electronics 2021, 10, 2034. [Google Scholar] [CrossRef]
- Hussien, H.; Yasin, S.; Udzir, N.; Ninggal, M. Blockchain-Based Access Control Scheme for Secure Shared Personal Health Records over Decentralised Storage. Sensors 2021, 21, 2462. [Google Scholar] [CrossRef] [PubMed]
- Hasan, M.; Anik, M.H.; Islam, S. Microcontroller Based Smart Home System with Enhanced Appliance Switching Capacity. In Proceedings of the 2018 Fifth HCT Information Technology Trends (ITT), Dubai, United Arab Emirates, 28–29 November 2018; pp. 364–367. [Google Scholar]
- Sharma, Y. A survey on privacy preserving methods of electronic medical record using blockchain. J. Mech. Contin. Math. Sci. 2020, 15, 32–47. [Google Scholar] [CrossRef]
- Eltayieb, N.; Elhabob, R.; Hassan, A.; Li, F. A blockchain-based attribute-based signcryption scheme to secure data sharing in the cloud. J. Syst. Arch. 2019, 102, 101653. [Google Scholar] [CrossRef]
- Rajput, A.; Li, Q.; Ahvanooey, M. A Blockchain-Based Secret-Data Sharing Framework for Personal Health Records in Emergency Condition. Healthcare 2021, 9, 206. [Google Scholar] [CrossRef]
- Panda, S.S.; Jena, D.; Mohanta, B.K.; Ramasubbareddy, S.; Daneshmand, M.; Gandomi, A.H. Authentication and Key Management in Distributed IoT Using Blockchain Technology. IEEE Internet Things J. 2021, 8, 12947–12954. [Google Scholar] [CrossRef]
- Pawar, P.; Parolia, N.; Shinde, S.; Edoh, T.O.; Singh, M. eHealthChain—a blockchain-based personal health information management system. Ann. Telecommun. 2021, 77, 33–45. [Google Scholar] [CrossRef]
- Javed, I.; Alharbi, F.; Bellaj, B.; Margaria, T.; Crespi, N.; Qureshi, K. Health-ID: A Blockchain-Based Decentralized Identity Management for Remote Healthcare. Healthcare 2021, 9, 712. [Google Scholar] [CrossRef]
- Shinde, R.; Patil, S.; Kotecha, K.; Ruikar, K. Blockchain for Securing AI Applications and Open Innovations. J. Open Innov. Technol. Mark. Complex. 2021, 7, 189. [Google Scholar] [CrossRef]
- Faisal, F.; Hasan, M.; Sabrin, S.; Hasan, Z.; Siddique, A.H. Voice Activated Portable Braille with Audio Feedback. In Proceedings of the 2021 2nd International Conference on Robotics, Electrical and Signal Processing Techniques (ICREST), Dhaka, Bangladesh, 5–7 January 2021; pp. 418–423. [Google Scholar] [CrossRef]
- Khezr, S.; Moniruzzaman, M.; Yassine, A.; Benlamri, R. Blockchain Technology in Healthcare: A Comprehensive Review and Directions for Future Research. Appl. Sci. 2019, 9, 1736. [Google Scholar] [CrossRef]
- Yli-Huumo, J.; Ko, D.; Choi, S.; Park, S.; Smolander, K. Where Is Current Research on Blockchain Technology?—A Systematic Review. PLoS ONE 2016, 11, e0163477. [Google Scholar] [CrossRef] [PubMed]
- Li, X.; Jiang, P.; Chen, T.; Luo, X.; Wen, Q. A survey on the security of blockchain systems. Future Gener. Comput. Syst. 2017, 107, 841–853. [Google Scholar] [CrossRef]
- LeHoty, D.L. The greater scope of the economic security program. Kyoto Daigaku Kokukagaku Kiyo Bull. Stomatol. Kyoto Univ. 1965, 30, 28–30. [Google Scholar]
- McGhin, T.; Choo, K.-K.R.; Liu, C.Z.; He, D. Blockchain in healthcare applications: Research challenges and opportunities. J. Netw. Comput. Appl. 2019, 135, 62–75. [Google Scholar] [CrossRef]
- Hasan, M.; Hossein, J.; Hossain, M.; Zaman, H.U.; Islam, S. Design of a Scalable Low-Power 1-Bit Hybrid Full Adder for Fast Computation. IEEE Trans. Circuits Syst. II Express Briefs 2019, 67, 1464–1468. [Google Scholar] [CrossRef]
- Chowdhury, S.; Hasan, M. Design of an automatic gain control loop for high speed communication. Int. J. Circuit Theory Appl. 2022, 51, 47–66. [Google Scholar] [CrossRef]
- Alla, S.; Soltanisehat, L.; Tatar, U.; Keskin, O. Blockchain technology in electronic healthcare systems. In Proceedings of the IISE Annual Conference and Expo 2018, Orlando, FL, USA, 19–22 May 2018; pp. 754–759. [Google Scholar]
- Sultana, J.; Saha, B.; Khan, S.; Sanjida, T.M.; Hasan, M.; Khan, M.M. Identification and Classification of Melanoma Using Deep Learning Algorithm. In Proceedings of the 2022 IEEE International Conference on Distributed Computing and Electrical Circuits and Elec-tronics (ICDCECE), Ballari, India, 23–24 April 2022; pp. 1–6. [Google Scholar]
- Abou Jaoude, J.; Saade, R.G. Blockchain Applications—Usage in Different Domains. IEEE Access 2019, 7, 45360–45381. [Google Scholar] [CrossRef]


| Blockchain Type\Properties | Private Blockchain | Consortium Blockchain | Public Blockchain |
|---|---|---|---|
| Efficiency | High | High | Low |
| Determination of consensus | An organization | Chosen node set | All miners |
| Constancy | Could be tampered | Could be tampered | Almost impossible |
| Centralized | Yes | Partial | No |
| Reading authorization | Public or restricted | Public or restricted | Public |
| Process of Consensus | Approved | Approved | Permissionless |
| Research Theme | Objective | Challenges | Year | Type | Ref |
|---|---|---|---|---|---|
| Medical Data Management and Sharing System | Creation of a blockchain-based decentralized data management system | Data security, accessibility, data transfer and privacy | 2018–2021 | Journal, Conference | [53,54,55,56,64,65,66,67,68,75,76,80,87,92,94,98,102,141,142,144,157,169,170,171,172,179,181] |
| Telemedicine and remote patient monitoring (RPM) | Blockchain-based secure telemedicine and RPM system | Patient monitoring, data collection, data safety and privacy | 2017–2021 | Journal, Conference | [49,57,59,60,61,69,70,72,73,77,108,109,122,123,125,128,149,150,151,152,154,155,156,176,177,185,187] |
| Electronic Health Record (EHR) System | Using blockchain to develop secure and accessible EHR system | Data security, decentralization, data accessibility and integrity | 2018–2021 | Journal, Conference | [71,81,82,83,89,126,160,162,165,166,167,168,178,182,184] |
| Data storage and Security | Developing secure data transmission and storage systems | Data security, data authorization, data integrity, safe transfer | 2018–2021 | Journal, Conference | [47,51,58,62,74,80,86,97,100,104,106,117,145,147,159,163,173,175,183,186] |
| Edge and Cloud computing, data analysis | Integrating blockchain with data processing systems such as cloud and edge computing for better decision making | Data security, management, reliability, data manipulation, late communication, difficult resource allocation | 2018–2021 | Journal, Conference | [46,48,50,52,56,108,137] |
| Literature Review and Case study | Review of the recent development in blockchain-based healthcare systems | Data collection, analysis, arranging and representation | 2018–2021 | Journal | [45,63,66,78,79,84,85,88,90,91,93,95,96,99,101,103,105,107,110,111,112,113,114,115,116,118,119,120,121,127,129,130,131,132,133,134,135,136,138,139,140,143,146,148,153,158,161,164,174,180,188] |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Ghosh, P.K.; Chakraborty, A.; Hasan, M.; Rashid, K.; Siddique, A.H. Blockchain Application in Healthcare Systems: A Review. Systems 2023, 11, 38. https://doi.org/10.3390/systems11010038
Ghosh PK, Chakraborty A, Hasan M, Rashid K, Siddique AH. Blockchain Application in Healthcare Systems: A Review. Systems. 2023; 11(1):38. https://doi.org/10.3390/systems11010038
Chicago/Turabian StyleGhosh, Pranto Kumar, Arindom Chakraborty, Mehedi Hasan, Khalid Rashid, and Abdul Hasib Siddique. 2023. "Blockchain Application in Healthcare Systems: A Review" Systems 11, no. 1: 38. https://doi.org/10.3390/systems11010038
APA StyleGhosh, P. K., Chakraborty, A., Hasan, M., Rashid, K., & Siddique, A. H. (2023). Blockchain Application in Healthcare Systems: A Review. Systems, 11(1), 38. https://doi.org/10.3390/systems11010038







