Reducing Children’s Obesity in the Age of Telehealth and AI/IoT Technologies in Gulf Countries
Abstract
1. Introduction and Background
2. Related Work
2.1. Research Aspect
- a.
- Clinical Intervention
- b.
- Technology-Based Intervention
- Mobile (the system is supported with a mobile application).
- IoT (the system is supported with IoT sensors).
- Webpage (the system is supported with a webpage interface).
- Language (the supported language of the system proposed).
- Saudi Dietary (allow the user to know how many calories a Saudi dish has).
- Targeted User (what kind of obesity is the system designed for).
- Community (allow parents to communicate through the system platform).
- Connected Health Provider (allow the user to connect with a health care provider and allow the physician to keep track of the user progress).
- Recommender (support automatic recommendation that is not manually added).
- Interactive (support an interactive component to encourage and motivate the users to follow the given recommendations).
2.2. Commercial Aspect
2.2.1. Competitive Software
- a.
- Sleep Applications
- b.
- Weight Loss Apps
- c.
- Activity Apps
2.2.2. Comparison
- Monitoring sleep (allow users to track their sleeping habits).
- Monitoring activity (tracking user activity per day and showing statistics).
- Monitoring fitness (users can choose any schedule for sports to do).
- Heart rate (provide the users clear information about their heart rate).
- Language (the language supported by the system).
- Targeted user (what kind of obesity is the system designed for).
- Community (platform that allows users to share and communicate or contact with specialist).
2.3. Complementary Hardware
- Battery life (the number of hours in which the watch is working without charging).
- Activity (tracking daily activities).
- Fitness (tracking workout activity such as cardio or strength training).
- Heart rate sensor (have sensors that listen to the user’s heart rate).
- Sleep (tracking how many hours the user sleeps).
- Price (the cost of the smart watch).
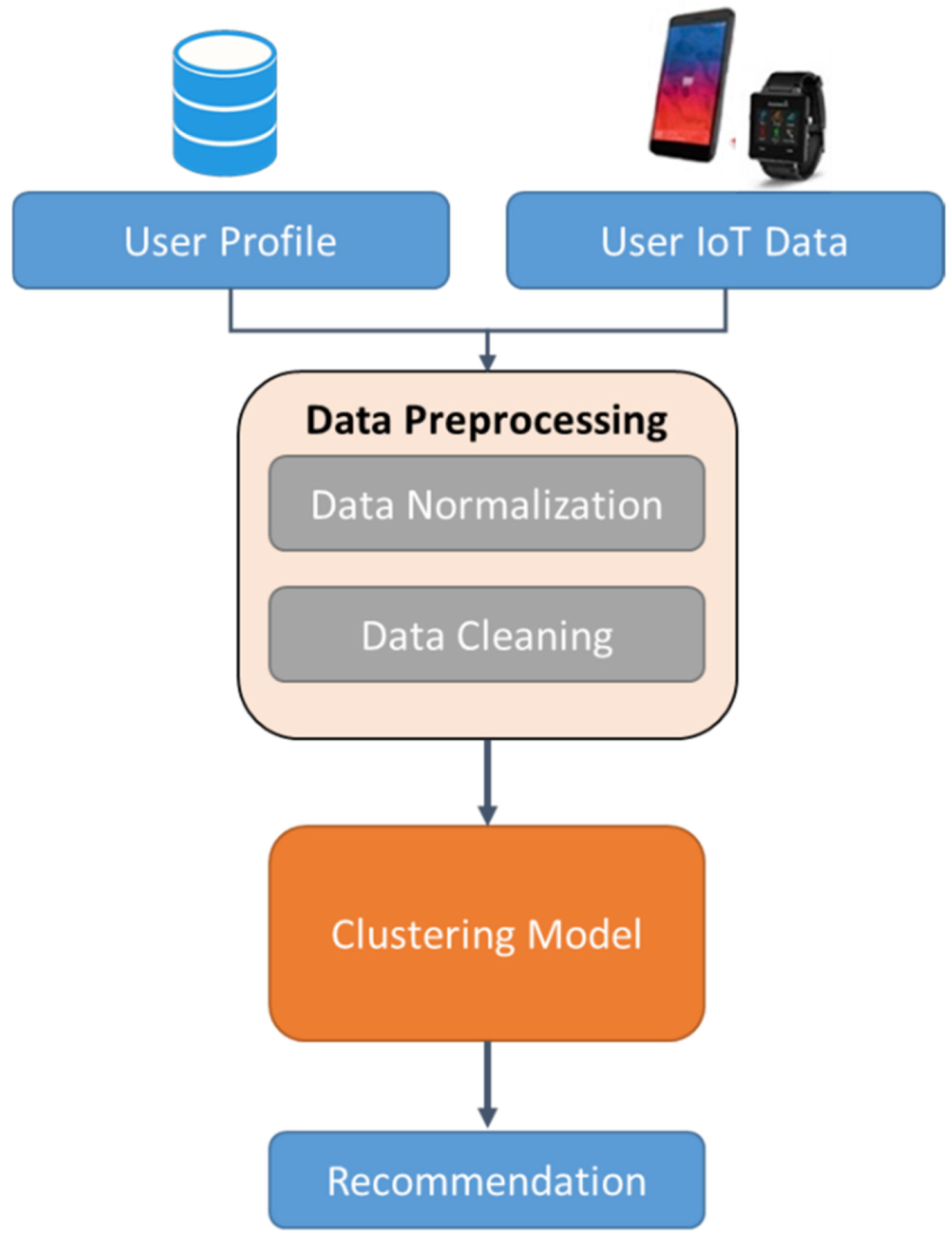
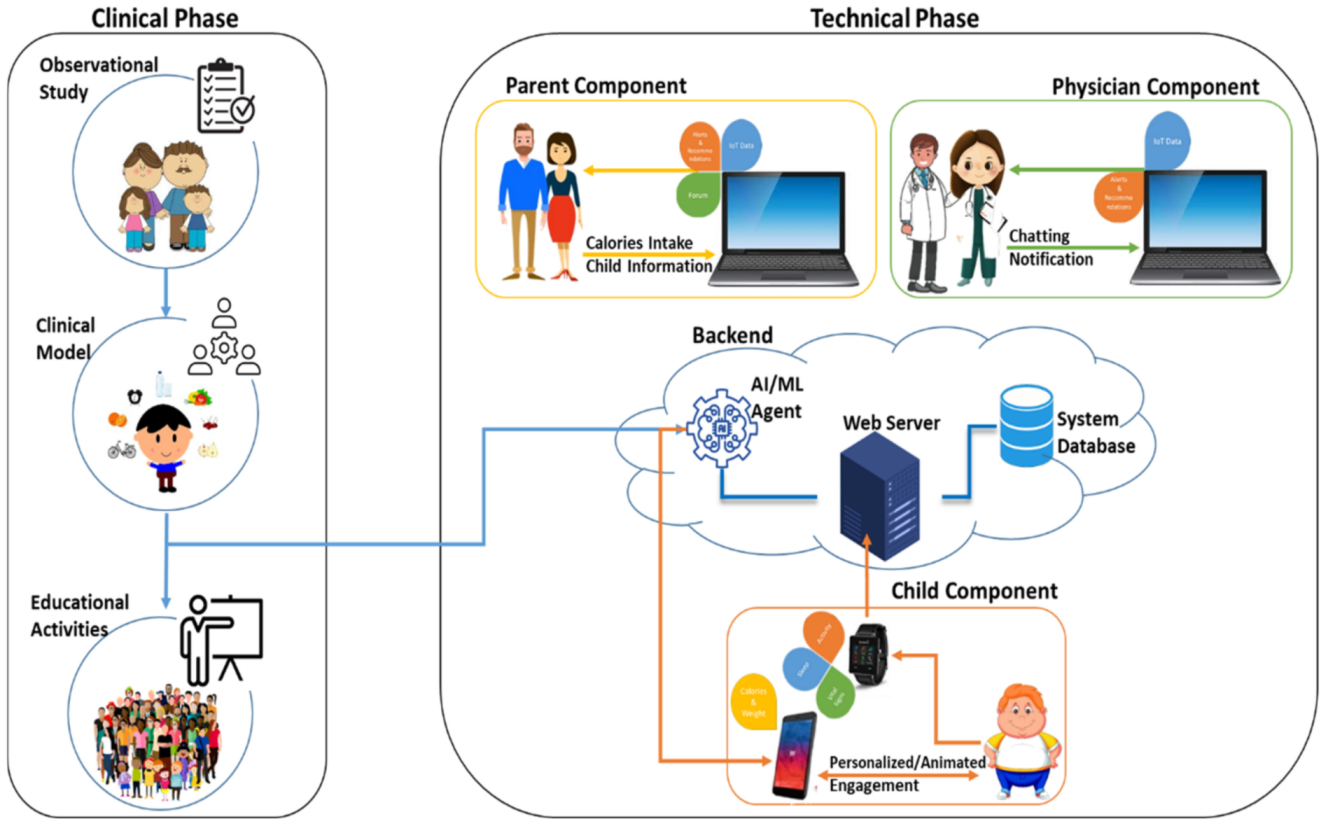
3. Proposed Framework
- Child Component: The child is monitored and interactively advised by the system and provided with different recommendations to improve their lifestyle. The AI component of the application will allow it to encourage children to sleep better and eat healthy food. The recommendation is presented using a user-friendly interface that encourages the child to accept it.
- Parent Component: Equip the parents with a web-page platform that allows them to monitor the child’s sleep and physical activities. The parents will be able to enter their child’s calorie intake and the system will prompt them on how many calories are consumed from different dishes including Saudi food. Moreover, the system will send notices to both parents and physicians if abnormalities are detected within the child’s sleep, diet, or physical activity. The platform also provides a social community forum where parents can share their thoughts with other parents.
- Physician Component: Equip the health care providers with a web-page platform that allows them to monitor the child’s lifestyle and connect with them if needed. Through the system, physicians can evaluate the child’s patterns, add notes, and send notifications to the child or their parents. They can also chat with the parent if they needed an answer to a quick inquiry.
- Backend Component: This part of the system contains the server that stores all the data and the AI agent that is developed to use ML methods and predict the best possible action to recommend the child with. Anomalies are also detected by this agent to alert the adults when things need to be taken more seriously.
4. Discussion
5. Conclusions
Author Contributions
Funding
Data Availability Statement
Conflicts of Interest
References
- Faienza, M.F.; Chiarito, M.; Molina-Molina, E.; Shanmugam, H.; Lammert, F.; Krawczyk, M.; D’Amato, G.; Portincasa, P. Childhood obesity, cardiovascular and liver health: A growing epidemic with age. World J. Pediatr. 2020, 16, 438–445. [Google Scholar] [CrossRef] [PubMed]
- ALNohair, S. Obesity in Gulf countries. Int. J. Health Sci. 2014, 8, 79. [Google Scholar] [CrossRef] [PubMed]
- Al Shaikh, A.; Aseri, K.; Farahat, F.; Abaalkhail, B.A.; Kaddam, I.; Salih, Y.; al Qarni, A.; al Shuaibi, A.; Tamimi, W. Prevalence of obesity and overweight among school-aged children in Saudi Arabia and its association with vitamin D status. Acta Bio. Med. Atenei Parm. 2020, 91, e2020133. [Google Scholar]
- Sneck, S.; Viholainen, H.; Syväoja, H.; Kankaapää, A.; Hakonen, H.; Poikkeus, A.-M.; Tammelin, T. Effects of school-based physical activity on mathematics performance in children: A systematic review. Int. J. Behav. Nutr. Phys. Act. 2019, 16, 109. [Google Scholar] [CrossRef] [PubMed]
- Pietrobelli, A.; Pecoraro, L.; Ferruzzi, A.; Heo, M.; Faith, M.; Zoller, T.; Antoniazzi, F.; Piacentini, G.; Fearnbach, S.N.; Heymsfield, S.B. Effects of COVID-19 lockdown on lifestyle behaviors in children with obesity living in Verona, Italy: A longitudinal study. Obesity 2020, 28, 1382–1385. [Google Scholar] [CrossRef]
- Marchitelli, S.; Mazza, C.; Lenzi, A.; Ricci, E.; Gnessi, L.; Roma, P. Weight gain in a sample of patients affected by overweight/obesity with and without a psychiatric diagnosis during the COVID-19 lockdown. Nutrients 2020, 12, 3525. [Google Scholar] [CrossRef]
- Freedman, D.S.; Kompaniyets, L.; Daymont, C.; Zhao, L.; Blanck, H.M. Weight gain among US adults during the COVID-19 pandemic through May 2021. Obesity 2022, 30, 2064–2070. [Google Scholar] [CrossRef]
- Wu, A.J.; Aris, I.M.; Hivert, M.-F.; Rocchio, C.; Cocoros, N.M.; Klompas, M.; Taveras, E.M. Association of changes in obesity prevalence with the COVID-19 pandemic in youth in Massachusetts. JAMA Pediatr. 2022, 176, 198–201. [Google Scholar] [CrossRef]
- Woolford, S.J.; Sidell, M.; Li, X.; Else, V.; Young, D.R.; Resnicow, K.; Koebnick, C. Changes in body mass index among children and adolescents during the COVID-19 pandemic. JAMA 2021, 326, 1434–1436. [Google Scholar] [CrossRef]
- Lange, S.J.; Kompaniyets, L.; Freedman, D.S.; Kraus, E.M.; Porter, R.; Blanck, H.M.; Goodman, A.B. Longitudinal trends in body mass index before and during the COVID-19 pandemic among persons aged 2–19 years—United States, 2018–2020. Morb. Mortal. Wkl. Rep. 2021, 70, 1278. [Google Scholar] [CrossRef]
- Aker, M.; Altenmüller, K.; Arenz, M.; Babutzka, M.; Barrett, J.; Bauer, S.; Beck, M.; Beglarian, A.; Behrens, J.; Bergmann, T. Improved upper limit on the neutrino mass from a direct kinematic method by KATRIN. Phys. Rev. Lett. 2019, 123, 221802. [Google Scholar] [CrossRef]
- Hamm, J.N.; Erdmann, S.; Eloe-Fadrosh, E.A.; Angeloni, A.; Zhong, L.; Brownlee, C.; Williams, T.J.; Barton, K.; Carswell, S.; Smith, M.A. Unexpected host dependency of Antarctic Nanohaloarchaeota. Proc. Natl. Acad. Sci. USA 2019, 116, 14661–14670. [Google Scholar] [CrossRef]
- People, H. Physical Activity; Department of Health & Human Services: Washington, DC, USA, 2020. [Google Scholar]
- Matricciani, L.; Paquet, C.; Galland, B.; Short, M.; Olds, T. Children’s sleep and health: A meta-review. Sleep Med. Rev. 2019, 46, 136–150. [Google Scholar] [CrossRef]
- Kertesz, R. Sleep and the challenges of the COVID-19 pandemic. Available online: chrome-extension://efaidnbmnnnibpcajpcglclefindmkaj/https://community.hmhc.ca/sessions/files/2020-10-28-18-15-40-Talk_SleepInChildrenSlides.pdf/ (accessed on 28 June 2022).
- Senkov, O.N.; Miracle, D.B.; Chaput, K.J.; Couzinie, J.P. Development and exploration of refractory high entropy alloys—A review. J. Mater. Res. 2018, 33, 3092–3128. [Google Scholar] [CrossRef]
- Aliss, E.M.; Sutaih, R.H.; Kamfar, H.Z.; Alagha, A.E.; Marzouki, Z.M. Physical activity pattern and its relationship with overweight and obesity in Saudi children. Int. J. Pediatr. Adolesc. Med. 2020, 7, 181–185. [Google Scholar] [CrossRef]
- Cuda, S.E.; Censani, M. Pediatric obesity algorithm: A practical approach to obesity diagnosis and management. Front. Pediatr. 2019, 6, 431. [Google Scholar] [CrossRef]
- Turner-McGrievy, G.M.; Wilcox, S.; Boutté, A.; Hutto, B.E.; Singletary, C.; Muth, E.R.; Hoover, A.W. The dietary intervention to enhance tracking with mobile devices (DIET mobile) study: A 6-month randomized weight loss trial. Obesity 2017, 25, 1336–1342. [Google Scholar] [CrossRef]
- Stephens, J.; Allen, J. Mobile phone interventions to increase physical activity and reduce weight: A systematic review. J. Cardiovasc. Nurs. 2013, 28, 320. [Google Scholar] [CrossRef]
- Machorro-Cano, I.; Alor-Hernández, G.; Paredes-Valverde, M.A.; Ramos-Deonati, U.; Sánchez-Cervantes, J.L.; Rodríguez-Mazahua, L. PISIoT: A machine learning and IoT-based smart health platform for overweight and obesity control. Appl. Sci. 2019, 9, 3037. [Google Scholar] [CrossRef]
- Alotaibi, M. A social robotic obesity management and awareness system for children in Saudi Arabia. Int. J. Online Eng. 2018, 14, 159–169. [Google Scholar] [CrossRef]
- Hosseini, H.; Yilmaz, A. Using telehealth to address pediatric obesity in rural Pennsylvania. Hosp. Top. 2019, 97, 107–118. [Google Scholar] [CrossRef] [PubMed]
- Chau, S.; Oldman, S.; Smith, S.R.; Lin, C.A.; Ali, S.; Duffy, V.B. Online behavioral screener with tailored obesity prevention messages: Application to a pediatric clinical setting. Nutrients 2021, 13, 223. [Google Scholar] [CrossRef] [PubMed]
- Lee, J.; Jeongeun, K.; Ahjung, B.; Meiling, J.; Meihua, P.; Kyungryeon, K.; Hyeoiyun, L. Application design for child obesity management based on users’ preferences and needs. West. J. Nurs. Res. 2020, 42, 356–364. [Google Scholar] [CrossRef] [PubMed]
- Afif, N.A. Prevalence of common sleep problems in school-aged Saudi students. Int. J. Adv. Appl. Sci. 2020, 7, 100–104. [Google Scholar] [CrossRef]
- Silva, G.E.; Goodwin, J.L.; Parthasarathy, S.; Sherrill, D.L.; Vana, K.D.; Drescher, A.A.; Quan, S.F. Longitudinal association between short sleep, body weight, and emotional and learning problems in Hispanic and Caucasian children. Sleep 2011, 34, 1197–1205. [Google Scholar] [CrossRef] [PubMed]
- Rutters, F.; Gerver, W.; Nieuwenhuizen, A.; Verhoef, S.; Westerterp-Plantenga, M. Sleep duration and body-weight development during puberty in a Dutch children cohort. Int. J. Obes. 2010, 34, 1508–1514. [Google Scholar] [CrossRef]
- Martinez-Lopez, A.; Blasco-Morente, G.; Perez-Lopez, I.; Herrera-Garcia, J.; Luque-Valenzuela, M.; Sanchez-Cano, D.; Lopez-Gutierrez, J.; Ruiz-Villaverde, R.; Tercedor-Sanchez, J. CLOVES syndrome: Review of a PIK3CA-related overgrowth spectrum (PROS). Clin. Genet. 2017, 91, 14–21. [Google Scholar] [CrossRef]
- Polet, J.; Hassandra, M.; Lintunen, T.; Laukkanen, A.; Hankonen, N.; Hirvensalo, M.; Tammelin, T.; Hagger, M.S. Using physical education to promote out-of school physical activity in lower secondary school students—A randomized controlled trial protocol. BMC Pub. Health 2019, 19, 157. [Google Scholar] [CrossRef]
- Dobbins, M.; Husson, H.; DeCorby, K.; LaRocca, R.L. School-based physical activity programs for promoting physical activity and fitness in children and adolescents aged 6 to 18. Cochrane Database Syst. Rev. 2013, 9. [Google Scholar] [CrossRef]
- Pozuelo-Carrascosa, D.; García-Hermoso, A.; Álvarez-Bueno, C.; Sánchez-López, M.; Martinez-Vizcaino, V. Effectiveness of school-based physical activity programmes on cardiorespiratory fitness in children: A meta-analysis of randomised controlled trials. Br. J. Sports Med. 2018, 52, 1234–1240. [Google Scholar] [CrossRef]
- Alahmed, Z.; Lobelo, F. Physical activity promotion in Saudi Arabia: A critical role for clinicians and the health care system. J. Epidemiol. Glob. Health 2018, 7, S7–S15. [Google Scholar] [CrossRef]
- Al-Hussaini, A.; Bashir, M.S.; Khormi, M.; AlTuraiki, M.; Alkhamis, W.; Alrajhi, M.; Halal, T. Overweight and obesity among Saudi children and adolescents: Where do we stand today? Saudi J. Gastroenterol. Off. J. Saudi Gastroenterol. Assoc. 2019, 25, 229. [Google Scholar] [CrossRef]
- Alzeidan, R.A.; Rabiee-Khan, F.; Mandil, A.A.; Hersi, A.S.; Ullah, A.A. Changes in dietary habits and physical activity and status of metabolic syndrome among expatriates in Saudi Arabia. East. Mediterr. Health J. 2017, 23, 836–844. [Google Scholar] [CrossRef]
- Soheilipour, F.; Salehiniya, H. Breakfast habits, nutritional status and their relationship with academic performance in elementary school students of Tehran, Iran. Med. Pharm. Rep. 2019, 92, 52. [Google Scholar] [CrossRef]
- Tambalis, K.D.; Panagiotakos, D.B.; Psarra, G.; Sidossis, L.S. Concomitant associations between lifestyle characteristics and physical activity status in children and adolescents. J. Res. Health Sci. 2019, 19, e00439. [Google Scholar]
- BaHammam, A.; AlFaris, E.; Shaikh, S.; Saeed, A.B. Prevalence of sleep problems and habits in a sample of Saudi primary school children. Ann. Saudi Med. 2006, 26, 7–13. [Google Scholar] [CrossRef]
- BaHammam, A.; Saeed, A.B.; Al-Faris, E.; Shaikh, S. Sleep duration and its correlates in a sample of Saudi elementary school children. Singap. Med. J. 2006, 47, 875. [Google Scholar]
- Bawazeer, N.M.; Al-Daghri, N.M.; Valsamakis, G.; Al-Rubeaan, K.A.; Sabico, S.L.B.; Huang, T.T.K.; Mastorakos, G.; Kumar, S. Sleep duration and quality associated with obesity among Arab children. Obesity 2009, 17, 2251–2253. [Google Scholar] [CrossRef]
- Al-Hazzaa, H.M.; Alhussain, M.H.; Alhowikan, A.M.; Obeid, O.A. Insufficient sleep duration and its association with breakfast intake, overweight/obesity, socio-demographics and selected lifestyle behaviors among Saudi school children. Nat. Sci. Sleep 2019, 11, 253. [Google Scholar] [CrossRef]
- Rodrigues, J.J.; Lopes, I.M.; Silva, B.M.; Torre, I.d.L. A new mobile ubiquitous computing application to control obesity: SapoFit. Inf. Health Soc. Care 2013, 38, 37–53. [Google Scholar] [CrossRef]
- Khaleel, F.L.; Khaleel, M.L.; Alsalam, Y.; Alsubhi, M.A.; Alfaqiri, A.S. Smart application criterion based on motivation of obese people. In Proceedings of the 2019 International Conference on Electrical Engineering and Informatics (ICEEI), Bandung, Indonesia, 9–10 July 2019; pp. 530–535. [Google Scholar]
- Taçyıldız, Ö.; Ertuğrul, D.Ç.; Bitirim, Y.; Akcan, N.; Elçi, A. Ontology-based obesity tracking system for children and adolescents. In Proceedings of the 2018 IEEE 42nd Annual Computer Software and Applications Conference (COMPSAC), Tokyo, Japan, 23–27 July 2018; pp. 329–334. [Google Scholar]
- Vazquez-Briseno, M.; Navarro-Cota, C.; Nieto-Hipolito, J.I.; Jimenez-Garcia, E.; Sanchez-Lopez, J. In Proceedings of the CONIELECOMP 2012, 22nd International Conference on Electrical Communications and Computers. Cholula, Mexico, 27–29 February 2012; pp. 168–172. [Google Scholar]
- Al-Humaimeedy, A.S.; Almozaini, R.; Almansour, L.; Alaqeely, K.; Almutairi, A.; Alolayan, A. So’rah: An Arabic mobile health application for Saudi dietary evaluation. eTELEMED 2018, 2018, 131–136. [Google Scholar]
- Alloghani, M.; Hussain, A.; Al-Jumeily, D.; Fergus; Abuelma’Atti, O.; Hamden, H. A mobile health monitoring application for obesity management and control using the internet-of-things. In Proceedings of the 2016 Sixth International Conference on Digital Information Processing and Communications (ICDIPC), Beirut, Lebanon, 21–23 April 2016; pp. 19–24. [Google Scholar]
- Wibisono, G.; Astawa, I.G.B. Designing machine-to-machine (M2M) prototype system for weight loss program for obesity and overweight patients. In Proceedings of the 2016 7th International Conference on Intelligent Systems, Modelling and Simulation (ISMS), Bangkok, Thailand, 25–27 January 2016; pp. 138–143. [Google Scholar]
- Chinchole, S.; Patel, S. Cloud and sensors based obesity monitoring system. In Proceedings of the 2017 International Conference on Intelligent Sustainable Systems (ICISS), Palladam, India, 7–8 December 2017; pp. 153–156. [Google Scholar]
- Hosseini, H.G.; Baig, M.M.; Lind, M. A smartphone-based obesity risk assessment application using wearable technology with personalized activity, calorie expenditure and health profile. Eur. J. Biomed. Inf. 2020, 16, 1–10. [Google Scholar]
- Goroso, D.G.; Watanabe, W.T.; Napoleone, F.; da Silva, D.; Salinet, J.L.; da Silva, R.R.; Puglisi, J.L. Remote monitoring of heart rate variability for obese children. Biomed. Signal Process. Control 2021, 66, 102453. [Google Scholar] [CrossRef]
- Sleep Cycle. Available online: https://www.sleepcycle.com/ (accessed on 26 June 2022).
- Lunden, J. Apps That Help You Monitor Your Sleep. Available online: https://www.joanlunden.com/category/14-sleep/item/1409-9-apps-that-help-you-monitor-your-sleep (accessed on 26 June 2021).
- MyFitnessPal. 2021. Available online: https://www.myfitnesspal.com/ (accessed on 28 June 2022).
- Fitbit. Available online: https://www.fitbit.com/global/us/home (accessed on 24 June 2022).
- Runkeeper. Available online: https://runkeeper.com/cms/ (accessed on 26 June 2022).
- Jefit App. Available online: https://www.jefit.com/ (accessed on 26 June 2022).
- Apple Watch Series 5. Available online: https://www.apple.com/apple-watch-series-5/ (accessed on 25 June 2022).
- Fitbit Versa 2. Available online: https://www.fitbit.com/us/products/smartwatches/versa (accessed on 26 June 2022).
- Galaxy Watch Active 2. Available online: https://www.samsung.com/us/mobile/wearables/galaxy-watch-active-2/ (accessed on 26 June 2022).
- Ignite. Polar Ignite. Available online: https://www.polar.com/en/ignite (accessed on 26 June 2022).

| Publication | [45] | [42] | [47] | [48] | [49] | [44] | [22] | [46] | [21] | [43] | [50] | [51] |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Date | 2012 | 2013 | 2016 | 2016 | 2017 | 2018 | 2018 | 2018 | 2019 | 2019 | 2020 | 2021 |
| Mobile | √ | √ | √ | √ | √ | √ | √ | √ | √ | √ | √ | √ |
| IoT | √ | √ | √ | √ | √ | √ | √ | |||||
| Webpage | √ | √ | √ | √ | √ | √ | √ | |||||
| Language | English | English | English | English | English | English | Arabic | Arabic | English | English | English | English |
| Saudi Dietary | √ | |||||||||||
| Targeted User | Child | Public | Child | Public | Public | Child | Child | Public | Public | Public | Public | Child |
| Community | ||||||||||||
| Health care Provider | √ | √ | √ | √ | √ | √ | ||||||
| Recommend | √ | √ | √ | √ | √ | |||||||
| Interactive | √ |
| App Name | Monitor Sleep | Monitor Activity | Monitor Fitness | Heart Rate | Language | Targeted Users | Community |
|---|---|---|---|---|---|---|---|
| Sleep Cycle | ✓ | ✓ | ✓ | English | Adult | ||
| Pillow | ✓ | ✓ | English | Adult | |||
| MyFitnessPal | ✓ | ✓ | ✓ | ✓ | English | Adult | |
| Fitbit | ✓ | ✓ | ✓ | ✓ | English | Adult | ✓ |
| RunKeeper | ✓ | ✓ | ✓ | English | Adult | ✓ | |
| JEFIT | ✓ | ✓ | English | Adult | ✓ |
| Device Name | Battery Life | Activity | Fitness | Sleep Tracker | Heart Sensor |
|---|---|---|---|---|---|
| Apple Watch | 18 h | ✓ | ✓ | ✓ | |
| Fitbit Versa 2 | 3 day | ✓ | ✓ | ✓ | ✓ |
| Galaxy Active 2 | 24 h | ✓ | ✓ | ✓ | ✓ |
| Polar Ignite | 17 h | ✓ | ✓ | ✓ | ✓ |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Faisal, M.; ElGibreen, H.; Alafif, N.; Joumaa, C. Reducing Children’s Obesity in the Age of Telehealth and AI/IoT Technologies in Gulf Countries. Systems 2022, 10, 241. https://doi.org/10.3390/systems10060241
Faisal M, ElGibreen H, Alafif N, Joumaa C. Reducing Children’s Obesity in the Age of Telehealth and AI/IoT Technologies in Gulf Countries. Systems. 2022; 10(6):241. https://doi.org/10.3390/systems10060241
Chicago/Turabian StyleFaisal, Mohammed, Hebah ElGibreen, Nora Alafif, and Chibli Joumaa. 2022. "Reducing Children’s Obesity in the Age of Telehealth and AI/IoT Technologies in Gulf Countries" Systems 10, no. 6: 241. https://doi.org/10.3390/systems10060241
APA StyleFaisal, M., ElGibreen, H., Alafif, N., & Joumaa, C. (2022). Reducing Children’s Obesity in the Age of Telehealth and AI/IoT Technologies in Gulf Countries. Systems, 10(6), 241. https://doi.org/10.3390/systems10060241






