Abstract
Background: Time series analyses on the relationship between nurse staffing and inpatient care quality are rare due to inconsistent frequencies of data between common observations of nurse-staffing (e.g., monthly) and inpatient care quality indicators (e.g., quarterly). Methods: In order to deal with the issue of mixed frequency data, this research adopted the MF-VAR model to explore causal relationships among nurse staffing, inpatient care quality, and hospital competition under the global budget payment scheme of Taiwan’s healthcare system. Results: Our results identified bi-directional causation between nurse staffing and patient outcomes and one-way Granger causality running between nurse staffing and reimbursement payments for inpatient care services. Impulse-response analyses found positive (negative) effects of the patient-to-nurse ratio on adverse patient outcomes (reimbursement payments) in all types of hospitals and detrimental effects of adverse patient outcomes on the patient-to-nurse ratio in medical centers and regional hospitals across a 12-month period. Conclusions: These findings suggest that nurse staffing is an essential determinant of both patient outcomes and reimbursement payments. Strategic policies such as direct subsidy and hospital accreditation for appropriate nurse staffing levels should be implemented for medical centers and regional hospitals to mitigate the harmful effects of adverse patient outcomes on nurse staffing.
1. Introduction
In their pioneering work on the relationship between hospital nurse staffing and patient outcomes and factors influencing nurse retention, Aiken and her colleagues identified the patient-to-nurse ratio (PNR, hereafter) as an essential determinant of patient outcomes and nurse retention [1]. A crucial conclusion of their study is that each additional patient per nurse is associated with higher patient mortality in the US. Continuing this line of research, one strand of studies provided evidence of the positive effect of hospital nurse staffing levels on patient mortality worldwide, such as in Australia [2,3], Belgium [4], Canada [5], Chile [6], England [7], Finland [8], Korea [9], Norway [10], Taiwan [11,12,13], and a group of European and OECD countries [14,15,16,17,18]. Another strand of the literature investigated the relationships between nurse staffing levels and various nursing-sensitive patient outcomes such as fall, pressure ulcer, medication error, various infections, physical restraint, missed observation, failure to respond to patients, length of stay, readmission to hospitals, emergency department attendance, etc. [2,19,20,21,22,23,24,25].
It is important to address that hospital competition under a publicly financed healthcare system may create a vicious cycle. In general, the cycle starts with quantity competition in inpatient care services leading to a high PNR and then further worsens patient outcomes or inpatient care quality (ICQ, hereafter). For example, Taiwan’s National Health Insurance (NHI, hereafter) system is a publicly financed healthcare system delivering universal coverage of healthcare services with moderate cost-sharing for all Taiwanese residents. The beneficiaries of Taiwan’s NHI pay 5.17% of the payroll income for the regular insurance premium rate and 2.11% of the non-payroll income (such as bonuses, part-time income, professional service income, dividend income, interest income, and rental income) for a supplementary premium rate [26]. Additionally, the covered benefits of Taiwan’s NHI system include outpatient care, inpatient care, emergence department (ED, hereafter) care, dental care, eye care, maternity delivery, physiotherapy and rehabilitation services, home health care, chronic mental illness, prescription drugs, and traditional Chinese medicine [26]. Nevertheless, the copayment for the outpatient care (ED care) per visit varies from USD 1.67 (USD 5.00) to USD 14.00 (USD 18.33), and the co-insurance rate for inpatient care per diem varied from 5% to 30% depending on various healthcare providers and the length of stay, respectively [26].
As with other publicly financed healthcare systems such as the National Health Services (NHS, hereafter) and Social Health Insurance systems (SHI, hereafter), it is expected that financial difficulty will be the most challenging issue under Taiwan’s NHI system [26,27,28,29]. In order to constrain the upward trend in healthcare expenditure, the Taiwan National Health Insurance Administration (NHIA, hereafter) applied the Global Budget Payment Scheme (GBPS, hereafter) to reimburse for healthcare services in the hospital sector since 2002 [26,30,31,32]. In general, the GBPS assigns a fixed total budget for inpatient care services with hospitals being reimbursed on a fee-for-service basis, and it follows that hospitals have strong incentives to compete with quantity rather than quality of inpatient care services in order to obtain target revenues under a fixed total budget of healthcare expenditure [26,30,31,32].
It is also important to point out that the hospital sector of Taiwan’s NHI system consists of three different types of hospitals, these being district hospitals (delivering secondary care), regional hospitals (providing tertiary care), and medical centers (handling the most complicated illnesses and supporting teaching and research in clinical practices) [29,30]. In order to prevent the negative effects of hospital (quantity) competition on patient outcomes under the GBPS of Taiwan’s NHI system, Taiwan’s NHIA imposed a PNR mandate such that the PNR of the day-shift should be below 7 for hospital wards in the three different types of hospitals. Nonetheless, the mean PNR of the three shifts (i.e., day, afternoon, and night shifts) within a daily cycle can legally vary from 9, 12, and 15 for hospital wards in medical centers, regional hospitals, and district hospitals, respectively [33]. This mandated PNR policy, in fact, is not restrictive, but flexible, for hospitals to adjust their nurse labor force to cope with severe quantity competition of inpatient care services in the hospital sector of Taiwan’s NHI system. Therefore, the most likely response of hospitals to market (quantity) competition under the GBPS of Taiwan’s NHI system is to shift their PNRs upward in order to maintain their own share of a fixed total budget [34]. It follows that a heavier workload imposed on incumbent nurses would not only increase the likelihood of nurses’ burnout but also worsen patient outcomes [1,35]. Therefore, a vicious cycle originating from hospital (quantity) competition under the GBPS should be anticipated which will deteriorate ICQ through inappropriate nurse staffing levels under Taiwan’s NHI system.
From the perspective of preventing the vicious cycle triggered by hospital (quantity) competition under the GBPS, the surveillance of PNR time series at hospital wards is an important managerial strategy for the healthcare administration to use to maintain high ICQ, better nursing work environments, and a reasonable inpatient care expenditure (ICE, hereafter) to reimburse hospitals for their inpatient care services. Nevertheless, time series analyses on the relationship between nurse staffing and patient outcomes are limited in the literature. Some studies relating to the nurse staffing and patient outcomes nexus focused on identifying potential structural changes in ICQ indicators due to initiating new nurse staffing regulations [19,36], and other research applied conventional time series methodologies (such as the trend and seasonality decomposition method and the latent growth model) to investigate the determinant of patient outcomes and trajectory of ICQ indicators [37,38]. Although these time series studies provide some justification for nurse staffing as an important determinant of patient outcomes, these studies were not grounded in a time series theoretical foundation with regards to three aspects: First, the causal linkage between nurse staffing and patient outcomes cannot be established in these studies, especially for the existence of bidirectional causality between these two variables. Second, these studies fail to provide precautionary information in terms of the propagation mechanism of a nurse staffing policy shock across a period of time. Third, a recent study proposed by Winter and his colleagues cautioned against a potential data aggregation effect on estimations of the nurse staffing and patient outcomes relationship [39]. Moreover, nurse staffing and patient outcomes can be reported in different time frequencies. For example, variables for nurse staffing and patient outcomes may be reported either monthly or quarterly. In order to perform time series analyses with all variables being single frequency, these studies aggregated high frequency data (e.g., monthly data) into low frequency data (e.g., quarterly data). Such temporal aggregation was proven to have some adverse impacts on statistical inferences of time series analyses [40,41].
In this study, we specifically investigate the interdependences between nurse staffing, patient outcomes, and hospital competition under the GBPS of Taiwan’s NHI system. The motivation of this study is three-fold: First, Taiwan has experienced a fast demographic transition from an aging society to an aged society within 25 years (from the period of 1993~2018), and it is projected to become a hyper-aged country in 2025 [42]. The growth of the aging population will burden Taiwan’s NHI system in terms of rising healthcare expenditures. It can be expected that more stringent cost-containment policies will be enforced to suppress an upward trend of healthcare expenditures, and it is predictable that such policies would create an even more competitive market for hospitals. Second, although Taiwan’s NHI system has been successful in providing comprehensive healthcare services for all Taiwanese residents, the quality of healthcare services has been challenged regarding various dimensions of the OECD Health Care Quality Indicator Project [43]. Third, the nurse labor participation rate (defined as the total number of incumbent nurses divided by the total number of licensed nurses) has been around 60% since 2005, meaning that approximately 40% of total licensed nurses are reluctant to engage in nursing works [44]. It was reported that 89.76% of local hospitals had difficulty recruiting nurses in Taiwan, and the shortage of nurses and the poor environment at nursing workplaces are overwhelming problems negatively influencing the appropriate deployment of nursing staffs in the hospital sector of Taiwan’s NHI system [34,45,46].
In order to incorporate mixed frequency data into the investigation of the causal relationship between nurse staffing and patient outcomes under the GBPS of Taiwan’s NHI system, we first adopted the Mixed Frequency Vector Auto-regressive (MF-VAR, hereafter) model proposed by Ghysel and his colleagues [47,48] to test the causal linkages among nurse staffing (measured by monthly PNR), patient outcomes (measured by two quarterly ICQ indicators defined in the next section), and hospital (quantity) competition (measured by quarterly real ICE per admission) based on three pairs of causal relationships: (1) PNR leading ICQ versus ICQ leading PNR, (2) PNR leading ICE versus ICE leading PNR, and (3) ICQ leading ICE versus ICE leading ICQ. The identification of these three pairs of causal relationships allows us to establish potential mechanisms triggering the vicious cycle of hospital competition under the GBPS of Taiwan’s NHI system.
In this study, the conventional VAR model based on the temporal aggregation of mixed frequency data into single frequency data is referred to as the Low Frequency Vector Auto-regressive (LF-VAR, hereafter) model. The MF-VAR model has several advantages against the LF-VAR model from four aspects. First, the MF-VAR model incorporates a high-frequency nurse staffing variable (i.e., monthly PNR used in this study) into the time series analyses. This allows us to demonstrate heterogeneous effects on low frequency variables reflecting patient outcomes (i.e., quarterly ICQ indicators) across the high frequency timescale (three months) within each low frequency time-span (say, one quarter timespan) [40,47,48,49]. Second, the impulse-response functions (IRFs, hereafter) for the mixed frequency data were estimated in order to capture the propagation mechanism of a nurse-staffing policy (or patient outcomes) shock across a period of time, which can then be used to evaluate the responses of ICQ indicators (PNR) on the change in PNR (ICQ indicators). Third, forecast error variance decomposition analyses for the mixed frequency data were conducted to show that an aggregation of monthly nurse staffing data into quarterly data is likely to underestimate the influence of nurse staffing on patient outcomes. Fourth, all statistical inferences from the MF-VAR model are based on the bootstrap method, which is capable of accommodating the small sample size of data used in this study [40,49]. Therefore, the results obtained from the MF-VAR model provide new insights into the linkages among nurse staffing, patient outcomes, and hospital competition under the GBPS of Taiwan’s NHI system.
2. Materials and Methods
2.1. Data and Variables
The main purpose of this study is to explore the interdependences between nurse staffing, patient outcomes, and hospital competition under the GBPS of Taiwan’s NHI system. The average PNR of the three shifts (i.e., day, afternoon, and night shifts) of the daily cycle at hospital wards was used to indicate the nurse staffing level. Taiwan’s NHIA reports PNR monthly for the three different types of hospitals (i.e., medical centers, regional hospitals, and district hospitals). The re-emergency-department-visit rate in the same hospital within 3 days after discharge (hereafter, 3-day EDV rate) and the unplanned readmission rate within 14 days after discharge (hereafter, 14-day readmission rate) were suggested by Taiwan’s NHIA to measure ICQ under the GBPS of Taiwan’s NHI system [50]. In order to avoid inconsistencies in monetary values across different periods of time, the real ICE per admission (adjusted by the medical price index based on the 2016 price level) was used to measure reimbursement payments for inpatient care services provided by the three different types of hospitals. Since the GBPS was applied to reimburse inpatient care services, the real ICE per admission also serves as a measure of hospital (quantity) competition in the hospital sector of Taiwan’s NHI system. Note that Taiwan’s NHIA reported the two ICQ indicators and reimbursed healthcare services quarterly for the three different types of hospitals. Hence, the quarterly data of ICQ indicators and the real ICE per admission and monthly data of PNR were used for our empirical analyses.
Since all data used in this study belong to time series data, we need to deal with the unit root property involved in time-series data in order to avoid spurious correlations among nurse staffing, patient outcomes, and hospital (quantity) competition [27,30]. Previous studies utilized cyclical components extracted from time series data to obtain the stationarity of time series [27]. Accordingly, we extracted the cyclic components of these time series data through the Hodrick and Prescott filter method to assure the stationarity of the time series [51]. Note that cyclic components of these time series data have two important features: First, the long-run trend of times series was removed, so cyclic components of these time series data have a zero mean without a time trend. Second, these cyclic components are interpreted as the percentage deviating from the long-run trend of the original time series. The aggregate cyclic component of PNR (used to estimate the LF-VAR model) was computed as an average of the three individual cyclic components of PNR across a 3-month cycle of a quarter timespan. All the data used in this study were obtained from the Open Database of National Health Insurance administrated by Taiwan’s NHIA. The data collection process was approved by the Research Ethics Committee of Taichung Tzu Chi Hospital with the Certificate of Exempt Review ID: REC REC110-23. The quarterly and monthly sample periods start from 2015: Q1 to 2021: Q4 and 2015: M1 to 2021: M12, resulting in a total of 28 and 84 quarterly and monthly observations, respectively.
2.2. VAR Models
The relationship between nurse staffing and patient outcomes can be represented by the hospital production function below:
where the ICQ indicator () is the output of a hospital production function. and represent labor and capital inputs of a hospital production function, respectively. measures the environmental factors such as hospital competition under the GBPS. The labor () and capital () inputs of a hospital production function were measured by PNR, and three different types of hospitals (such as district hospitals for secondary care, regional hospitals for tertiary care, and medical centers for the most complicated sicknesses and research and development for clinic practices) were used to control different levels of capital inputs in a hospital production function. Hospital competition is signified by the real ICE per admission under the GBPS of Taiwan’s NHI system. The same specification of hospital production was used in previous studies on the association between nurse staffing and patient outcomes [11,12,13]. Since the output and inputs of a hospital production function are all endogenous in clinical practices, Equation (1) could be established as the MF-VAR model as follows:
where, given a fixed capital input of hospital production (e.g., medical centers, regional hospitals, or district hospitals), (i = 1,2,3) represents the PNR in the ith month of a quarter timespan. and signify the ICQ indicator and real ICE per admission, respectively. denotes each quarter during our study period. The lag length () was selected based on the method proposed by Newey and West with the maximal lag set at 3 in order to capture the potential seasonal (or monthly) effect [52]. ( and ) are the elements of the parameter matrix in the VAR system.(i = 1,2,..,5) denote error terms. Since the cyclic components of these time series data were used for the estimation of the MF-VAR model, the estimated parameters of constant terms in the parameter matrix were skipped due to the zero mean property of the Hodrick and Prescott filter method. The way we established our model specification in Equation (2) is the same as for prior studies applying the MF-VAR model for time series analyses in the field of social sciences [40,49]. The technical details of the notations in the parsimonious specification of the MF-VAR model can be found in Ghysel’s study [47].
For the sake of model specification comparison between the MF-VAR and LF-VAR models, it should be noted that the individual monthly PNRs (, , and ) are stacked in a vector, and one of the possible relationships among PNR, ICQ, and real ICE per admission can be expressed as the 4th low of Equation (2) as follows:
As indicated in Equation (3), nurse staffing from each month (, i = 1,2,3) has heterogeneous effects (, j = 1,2,3) on ICQ. In contrast to the MF-VAR model, the model specification of the LF-VAR model is given by Equation (4):
where, Lt represents the quarterly PNR calculated as the average of monthly PNR (i.e., ). Other notations used in Equation (4) share the same definitions as those used in Equations (2) and (3). Analogous to Equations (2) and (3), one of the possible linkages among PNR, ICQ, and real ICE per admission can be written as the 2nd low of Equation (4) as follows:
The specification in Equation (5) implies that , , and have a homogeneous impact (/3) on ICQ (), and, in turn, the possibilities of monthly effects and lagged information transmission within each quarter are excluded from the LF-VAR model. Finally, the MF-VAR model can be estimated in the same way as the LF-VAR model because these two models share the same asymptotic theory. Nevertheless, the p values for testing the causal (lead-lag) relationships among PNR, ICQ, and real ICE per admission and confidence intervals of IRFs were generated by the bootstrap method due to a small size of samples used in this study.
2.3. Granger Causality Tests
Since all variables establishing a hospital production function are endogenous in clinical practices, the assumption of the interdependence of variables is fulfilled to specify our MF-VAR model and apply the mixed frequency Granger causality tests to investigate the lead-lag relationships among nurse staffing, patient outcomes, and hospital competition. In order to introduce mixed frequency Granger causality tests, we rewrote Equation (2) in the following matrix form:
where, , , and is the parameter matrix comprised of elements = ,, and . The joint zero hypothesis specified by = 0, postulates a non-causal linkage running from variable j to variable i. The Wald test statistic derived from Ghysel and his colleagues [48] was used to test for this hypothesis. Nonetheless, previous studies [48,49] indicated that the asymptotic distribution of the Wald statistic under the null hypothesis of non-causality from the MF-VAR model suffers from a severe size distortion with a small sample size. Therefore, the heteroscedasticity-robust parametric bootstrap method with 10,000 repetitions proposed by Gonçalves and Kilian [53] was used for calculating p values in order to accommodate size distortion and potential heteroscedasticity under the MF-VAR model, as suggested by Ghysel and his colleagues [48]. Six causal linkages among PNR, ICQ, and real ICE per admission (these being PNR leading ICQ, ICQ leading PNR, PNR leading ICE, ICE leading PNR, ICQ leading ICE, and ICE leading ICQ) were examined using the Granger causality tests. The investigation of these six causal relationships allows us to understand potential mechanisms activating the vicious cycle of hospital competition under the GBPS of Taiwan’s NHI system.
2.4. Impulse-Response and Variance Decomposition
Once the causal relationships among nurse staffing, patient outcomes, and hospital competition were justified using the Granger causality tests, then the impulse response effect of a standard error shock in the jth element of at time t on could be expressed as follows:
where is the variance-covariance matrix in the MF-VAR system, and is the variance elements in the matrix. is an indicator vector where its jth element equals one. We plotted the impulse-response relationships among PNR, ICQ, and real ICE per admission based on the Granger causality tests, and the 90% confidence intervals of the IRFs were constructed using the Monte Carlo simulation method with 10,000 repetitions in order to investigate whether or not the estimated impulses are statistically significant at the 10% significance level. The forecast error variance decompositions for both LF-VAR and MF-VAR models were conducted following the estimation of the IRFs in Equation (6). Note that the estimation of Equation (7) involves a selection of the Cholesky order. The Cholesky orders for the LF-VAR and MF-VAR models were established as and , respectively. These settings comply with the process of reimbursement paid for inpatient care services in the hospital sector under the GPBS of Taiwan’s NHI system.
3. Results
3.1. Descriptive Statistics
Table 1 summarizes the descriptive statistics for the monthly PNR and quarterly real ICE per admission, 3-day EDV rate, and 14-day readmission rate for medical centers, regional hospitals, and district hospitals over the period of 2015:Q1–2021:Q4. As indicated in Table 1, means of the 3-day EDV rate (14-day readmission rate) for medical centers, regional hospitals, and district hospitals were 2.489% (6.428%), 2.814% (7.259%), and 2.599% (7.460%), respectively. The real ICE per admission on average varied from USD 2629.971, USD 1826.339, and USD 1679.079, corresponding to payments reimbursed for inpatient care services per admission for medical centers, regional hospitals, and district hospitals, respectively. In addition, the average PNR at hospital wards ranging from the lowest to highest were 7.436 at medical centers, 7.573 at district hospitals, and 9.261 at regional hospitals, and variations of average PNR at hospital wards were found within a quarter timescale. The highest (lowest) average PNR at hospital wards in the three different types of hospitals appeared in the first (second) month within a quarter timescale. In addition, the Jarque-Bera statistics were used to test the null hypothesis of normality of time series data, and some time series such as real ICE per admission at medical centers and district hospitals, and PNR at acute care wards of regional and district hospitals, were identified to be inconsistent with the normality assumption. These findings validated the application of bootstrap methods to estimate our empirical models. The trends of all variables used in this study can be found in Appendix A, and the median and interquartile range (IQR) are also reported in Table 1.

Table 1.
Descriptive Statistics 1.
3.2. Unit Root Tests
It is worth addressing that the PNR, ICQ, and real ICE per admission are time series data that are likely to have the unit root property. As shown in Table 2, the ADF tests with constant and with constant plus trend specifications identified non-stationary time series of real ICE per admission at the three different types of hospitals. In addition, the ADF tests with constant plus trend specification suggest that the time series of the two ICQ indicators were non-stationary except for the 14-day readmission rate at district hospitals. The presence of the unit roots of the 3-day EDV rate (14-day readmission rate) at regional hospitals (medical centers and regional hospitals) was found using the ADF tests with constant specification. Contrarily, the ADF tests with constant and with constant plus trend specifications identified stationary time series of PNR at the three different types of hospitals. These findings suggest that the order of time series data on PNR, the two ICQ indicators, and real ICE per admission is likely to be different at the three different types of hospitals. Since the cyclic components of these time series removed the long-run tendency of time series with zero means, the ADF tests without constant and trend specification were used to test for the unit root property of cyclic components of time series. As we expected, the stationarity of cyclic components of time series for the three different types of hospitals was confirmed. These findings eliminate spurious correlations among all variables used in this research from the unit root property of time series. Therefore, we were able to proceed with the Granger Causality tests with the cyclic components of these variables.

Table 2.
ADF Unit Root Tests 2.
3.3. Granger Causality Tests
Table 3 presents the results of the Granger causality tests under the MF-VAR model for the six causal relationships among ICQ, PNR, and real ICE per admission at the three different types of hospitals during our study period. Mixed frequency data were used for the Granger causality tests. As such, it is vital to understand that the causality running from the low frequency variable to the high frequency variable means causality running from a quarterly variable to a group of three individual monthly variables [40,48,49]. In addition, the asymptotic distribution of the Wald statistic under the null hypothesis of non-causality in the MF-VAR model has a severe size distortion due to a small sample size [40,48,49]. Because of this, p values were generated using the heteroscedasticity-robust parametric bootstrap method introduced by Gonçalves and Kilian [53] with 10,000 replications.

Table 3.
Granger Causality Tests 3.
Panel A of Table 3 displays the Granger causality tests for the six causal relationships among the 3-day EDV rate, PNR, and real ICE per admission at the three different types of hospitals. In contrast to little significance in the causal relationships identified by the LF-VAR model, the MF-VAR model identified bidirectional causation between PNR and the 3-day EDV rate at medical centers and regional hospitals, and one-way causality running from PNR to the 3-day EDV rate at district hospitals at the 10% (or stricter) significance level. In addition, a causal relationship running from PNR to real ICE per admission was identified for the three different types of hospitals, and another unidirectional causality running from the 3-day EDV rate to real ICE per admission was also detected for medical centers. In addition, Panel B of Table 3 reports results of the Granger causality tests for the six causal relationships among the 14-day readmission rate, PNR, and real ICE per admission at the three different types of hospitals. Although the LF-VAR model identified several causal relationships among the 14-day readmission rate, PNR, and real ICE per admission, previous studies addressed a potential aggregation bias in the statistical inferences of the LF-VAR model [40,47,48,49]. Therefore, we focused on the results of the Granger causality tests under the MF-VAR model. As indicated in Panel B of Table 3, the MF-VAR model identified one-way causal relationships running PNR to real ICE per admission at the three different types of hospitals. These findings are consistent with the causal linkage running from PNR to real ICE per admission as reported in Panel A of Table 3. Additionally, unidirectional Granger causality running from the 14-day readmission rate to PNR was also identified at district hospitals only.
3.4. Impulse-Response Analyses
Since the causal relationships among PNR, ICQ, and real ICE per admission were verified by the Granger causality tests under the MF-VAR model for Taiwan’s NHI system over the period of 2015:Q1–2021:Q4, we further plotted the mixed frequency IRFs to illustrate the propagation mechanism of interdependences between PNR, ICQ, and real ICE per admission across a 12-month period. As indicated in Figure 1, significantly positive (negative) responses of the 3-day EDV rate to a positive PNR shock in the first month of a quarter timespan were identified at the first and eighth (second) month horizons over a 12-month period for regional hospitals (see Figure 1(b1), and a significantly positive impulse-response relationship between the 3-day EDV rate and PNR in the first month of a quarter timespan was found at the first month horizon over a 12-month period for district hospitals (see Figure 1(c1)).
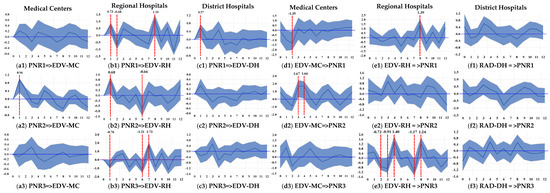
Figure 1.
Impulse Response Functions for Quality of Care Indicators and Nurse Staffing Level 4.
The significantly positive effect of PNR in the second month of a quarter timespan on the 3-day EDV rate was found at the first month horizon over a 12-month period for medical centers (see Figure 1(a2)). Nonetheless, the impulse-response relationship between the 3-day EDV rate and PNR in the second month of a quarter timespan was identified as significantly positive at the first month horizon but negative at the sixth month horizon over a 12-month period for regional hospitals (see Figure 1(b2)). Additionally, the responses of the 3-day EDV rate to a positive PNR shock in the third month within a quarter timespan were significantly negative (positive) at the first and sixth (seventh) month horizon over a 12-month period for district hospitals (see Figure 1(b3)). Despite asymmetric impulse-response effects of PNR on the 3-day EDV rate being found, the positive effects of PNR on the 3-day EDV rate dominated the negative effects across a 3-month cycle of a quarter timespan for all three types of hospitals.
As shown in Figure 1(d1,e1), the responses of PNR in the first month of a quarter timespan to a positive shock in the 3-day EDV rate were significantly negative (positive) at the second (eighth) month horizon over a 12-month period for medical centers (regional hospitals). The significantly positive responses of PNR in the second month of a quarter timespan to a positive shock in the 3-day EDV rate were found at the third and fourth month horizons over a 12-month period for medical centers (see Figure 1(d2)). The impulse-response relationship between the 3-day EDV rate and PNR in the third month of a quarter timespan was negative at the second, third, and seventh month horizons, but it was identified to be positive at the fourth and eighth month horizons over a 12-month period for regional hospitals (see Figure 1(e3)). Although a changing impulse-response relationship between the 3-day EDV rate and PNR was identified, as shown in Figure 1(d1,d2,e1,e3), the negative effects of the 3-day EDV rate on PNR were dominated by the positive effect across a 3-month cycle of a quarter timespan for medical centers and regional hospitals. Nevertheless, the impulse-response relationship between 14-day readmission and PNR across a 3-month cycle of a quarter timespan did not generate any significant results for district hospitals.
The impulse-response relationships between PNR and real ICE per admission for the three different types of hospitals are illustrated in Figure 2 in Panels A and B, which, respectively, correspond to the 3-day EDV rate and 14-day readmission rate used to measure ICQ in the estimation of the MF-VAR model. No matter which ICQ indicator was selected, the responses of real ICE per admission to PNR in the second month of a quarter timespan were identified as significantly negative around the third, fourth, and fifth month horizons over a 12-month period for regional hospitals and district hospitals (see Figure 2(b2,c2,e2,f2)). The effects of PNR in the second month of a quarter timespan on real ICE per admission were determined to be significantly negative at the third month horizon and positive at the sixth month horizon over a 12-month period for medical centers (see Figure 2(d2)).
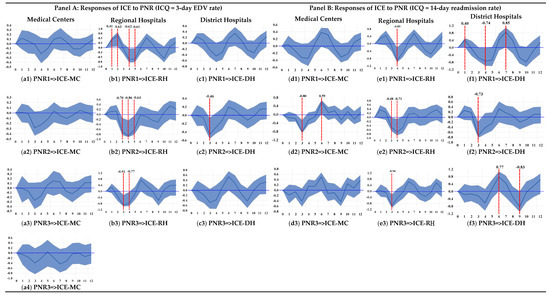
Figure 2.
Impulse Response Functions for Inpatient Care Expenditure, Nurse Staffing, and Quality of Care Indicator 5.
The impulse-response relationship between real ICE per admission and PNR in the first month of a quarter timespan was found to be significantly positive around the first and second month horizons and negative around the fourth and fifth month horizons over a 12-month period for regional hospitals (Figure 2(b1,e1)). Figure 2(b3,e3) illustrates a significantly negative impulse-response relationship between real ICE per admission and PNR in the third month of a quarter timespan around the third and fourth month horizons over a 12-month period for regional hospitals. The responses of real ICE per admission on PNR in the first (third) month of a quarter timespan were found to be significantly negative at the fourth (ninth) month horizon and positive at the first and seventh (sixth) month horizons over a 12-month period for district hospitals (Figure 2(f1,f3)). Despite an asymmetric relationship between real ICE per admission and PNR across a 3-month cycle of a quarter timespan being found, the negative effects of PNR on real ICE per admission across a 3-month cycle of a quarter timespan dominated the positive effects for all three types of hospitals.
3.5. Variance Decomposition
Table 4 presents two sets of the forecast error variance decompositions based on whether the 3-day EDV rate or 14-day readmission rate were used to serve as the ICQ indicator in the estimation of the LF-VAR and MF-VAR models. As indicated in Table 4, the proportions of forecast error variance of the ICQ indicator attributed to the PNR within a 3-month cycle of a quarter timespan (i.e., PNR = ΣPNRi) in the MF-VAR model for medical centers are 1.61~4.58 (=21.70/13.46~37.20/8.13), 1.55~3.81(=45.87/29.53~44.06/11.56), and 1.62~3.77 (=46.45/27.73~46.80/12.40) times higher than those attributed to an aggregation of PNR (i.e., PNRA) in the LF-VAR model in the short-run (h = 2), medium-run (h = 7), and long-run (h = 12), respectively, based on whether the 3-day EDV rate or 14-day readmission rate was chosen to measure ICQ. In addition, the proportions of forecast error variance of the real ICE per admission attributed to the PNR within a 3-month cycle of a quarter timespan (i.e., PNR = ΣPNRi) in the MF-VAR model for medical centers are 1.24~1.36 (=74.07/59.63~73.87/54.34), 1.50~1.65 (=70.93/47.18~71.88/43.48), and 1.60~1.69 (=73.91/46.16~74.71/44.12) times higher than those attributed to the aggregation of PNR (i.e., PNRA) in the LF-VAR model in the short-run (h = 2), medium-run (h = 7), and long-run (h = 12), respectively, based on whether the 3-day re-EDV rate or 14-day readmission rate was chosen to measure ICQ. Similar results, wherein the MF-VAR model generated a higher explanatory power than the LF-VAR model, could also be found for the relationships among PNR, ICQ, and real ICE per admission for regional hospitals and district hospitals. Therefore, the findings of the forecast error variance decompositions shown in Table 4 indicate that the MF-VAR model has a greater explanatory power than the LF-VAR model in the investigation of interdependences between PNR, ICQ, and real ICE per admission for the three different types of hospitals.

Table 4.
Forecast Error Variance Decomposition (%) 6.
4. Discussion
Two unidirectional causal propositions can be justified by looking at the causal relationships among PNR, the two ICQ indicators (i.e., 3-day EDV rate and 14-day readmission rate), and real ICE per admission identified by the Granger causality tests under the MF-VAR model. The PNR leading ICE proposition postulates that PNR leads real ICE per admission, and the EDV leading ICE proposition claims that the 3-day EDV rate leads real ICE per admission. The former proposition was substantiated by data from the three different types of hospitals, and the latter proposition was only verified by data from medical centers. In addition, the Granger causality tests also confirmed a feedback proposition for PNR and ICQ claiming bidirectional causation between PNR and the 3-day EDV rate in medical centers and regional hospitals. Additionally, the PNR leading 3-day EDV rate proposition (stating that PNR leads the 3-day EDV rate) and the 14-day readmission rate leading PNR proposition (asserting that the 14-day readmission rate leads PNR) were corroborated for district hospitals.
In general, four mechanisms activating the vicious cycle of hospital competition are implied by these propositions. First, the PNR origin mechanism suggests that a high PNR (i.e., a poor nurse staffing level) not only worsens the 3-day EDV rate but also reduces real ICE per admission (see Figure 3(a1)). Second, the EDV origin mechanism indicates that a higher 3-day EDV rate influences both real ICE per admission and PNR (see Figure 3(a2)). Third, the EDV rebound mechanism alludes that the 3-day EDV rate results in a higher PNR leading to decreased real ICE per admission (see Figure 3(a3)). Fourth, the readmission rebound mechanism points to the 14-day readmission rate causing a higher PNR which leads to a reduction in real ICE per admission (see Figure 3(a4)). The statistical significances of the signs and paths connecting PNR, the two ICQ indicators (i.e., 3-day EDV rate and 14-day readmission rate), and real ICE per admission (underpinning the four mechanisms described above) were determined based on the impulse-response analyses illustrated in Figure 1 and Figure 2. Several policy implications emerging from this work have merit and are worth being discussed as follows:
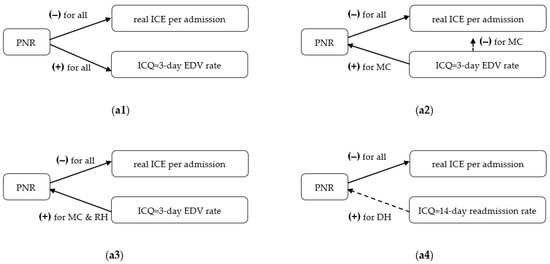
Figure 3.
Mechanisms for activating the vicious cycle of hospital competition. (a1) M1: the PNR origin mechanism for the three different levels of hospitals; (a2) M2: the EDV origin mechanism for medical centers only; (a3) M3: the EDV rebound mechanism for medical centers and regional hospitals; (a4) M4: the readmission rebound mechanism for district hospitals 7.
First, as indicated in Figure 3(a1), the PNR origin mechanism was observed in all three different types of hospitals, but the EDV origin mechanism is suitable for medical centers only. The EDV (readmission) rebound mechanism was found in medical centers and regional hospitals (district hospitals). Therefore, the PNR not only qualifies as an important determinant of patient outcomes, but it also serves as both a key factor and mediator influencing real ICE per admission for the three different types of hospitals. In general, a positive impact on PNR increases the 3-day EDV rate but decreases real ICE per admission in all types of hospitals based on the impulse-response analyses over a 12-month period (see Figure 1, Figure 2, and Figure 3(a1)). These findings were consistent with results from previous studies on the relationship between nurse staffing and patient outcomes [1,2,3,4,5,6,7,8,9,10,11,12,13,14,15,16,17,18,19,20,21,22,23,24,25,35].
Second, it is important to note that the impulse-response relationship between the 3-day EDV rate and real ICE per admission was not significant based on the impulse-response analyses over a 12-month period. (see Figure 2(a4) and Figure 3(a2)). Therefore, we focus on the two rebound mechanisms for our discussion. As illustrated in Figure 3(a3,a4), we found that the rebound effects running from ICQ to PNR were essentially different between large hospitals (such as medical centers and regional hospitals) and small hospitals (i.e., district hospitals) in terms of the significance of the relationship between ICQ indicators and PNR. As shown in Figure 3(a3,a4), the 3-day EDV rate was found to be a trigger impacting PNR and then influencing real ICE per admission at medical centers and regional hospitals, but the readmission rebound mechanism was not significant in district hospitals based on the impulse-response analyses over a 12-month period (see Figure 1(f1,f3) and 3(a4)). These findings reflect the facts that district hospitals play a minor part in ED care services and that nighttime ED closures (or down-grading to the so-called urgent outpatient centers) are frequently observed in district hospitals due to a lack of sufficient nurses. Such shortages of nurses also lead to hospital bed closures in district hospitals where inpatient care resources are then shifted towards treating chronic rather than acute conditions. Hence, it was reported that the average length of stay ranged from 13~16 days in district hospitals, much higher than that for medical centers (7~9 days), but the mean PNR in district hospitals was very close to that in medical centers (7.572 versus 7.436; see Table 1) during our study period [54].
Third, although the EDV rebound effect was expected to be negative as hospital ad-ministration managerial actions were taken to influence ICQ for the sake of quality-of-care control, a positive rebound effect of the 3-day EDV rate on PNR was identified in medical centers and regional hospitals based on the impulse-response analyses over a 12-month period (see Figure 1 and Figure 3(a3)). According to annual statistics of the medical care institution and hospital utilization reported by Taiwan’s Ministry of Health and Welfare, the total number of hospitals decreased from 556 to 478 (of these, the number of medical centers remained stable at around 21~23, while the number of regional hospitals increased from 65 to 74, with a contrasting significant reduction in the number of district hospitals) during our study period of 2015:Q1–2021:Q4 [55]. Moreover, Taiwan’s NHIA reported that district hospitals represent over 80% of total hospitals, while approximately 76%~81% of total hospital admissions were contributed by medical centers and regional hospitals under the GBPS of Taiwan’s NHI system [55,56]. These statistics suggest that quantity competition for medical centers and regional hospitals is much higher than that for district hospitals, so managerial actions taken for the sake of quality-of-care control in medical centers and regional hospitals are highly likely to be offset by severe quantity competition in the hospital sector of Taiwan’s NHI system.
Fourth, the rebound effects of ICQ on PNR from medical centers and regional hospitals will mostly likely counter the adverse effect of hospital competition (see Figure 3(a1,a3)). Considering this along with substantial evidence identifying PNR as one of the crucial determinants of ICQ and real ICE per admission, as indicated in Figure 1, Figure 2, and Figure 3(a1), quality of care maintenance policies (such as directly subsidizing for a lower PNR and the inclusion of a reasonable PNR as a key standard for hospital accreditation) should be enforced in order to reduce adverse effects of higher nurse staffing levels on patient outcomes and quantity competition under the GBPS of Taiwan’s NHI system. Special attention should be concentrated on reducing the rebound effects of the 3-day EDV rate on PNR from medical centers and regional hospitals through imposing more substantial quality-of-care control plans and more stringent regulation of seasonal inpatient care volume for medical centers and regional hospitals.
This study makes contributions beyond those of the existing literature on the relationship between nurse staffing and patient outcomes in three respects: First, although the aggregation and omitted variable biases (due to aggregating different frequencies data into single frequency data) have attracted lots of attention regarding the estimation of the nurse staffing and patient outcomes relationship in the healthcare services research field [39], this study, for the first time, adopted the MF-VAR model proposed by Ghysel and his colleagues [47,48] to incorporate different frequencies data into the investigation of the relationships among PNR, ICQ, and real ICE per admission under the GBPS of Taiwan’s NHI system over the period of 2015:Q1–2021:Q4. We illustrated that the MF-VAR model is superior to the LF-VAR (i.e., conventional VAR) model in terms of higher explanatory power (See Table 4). Second, this study contrasts with the previous time series research exploring the association between nurse staffing and patient outcomes, in which the causal responses of patient outcomes (nurse staffing) to a nurse staffing (patient outcomes) shock across a period of time were not available. In this study, we not only tested for six causal relationships among PNR, ICQ, and real ICE per admission through the MF-VAR-Granger Causality tests proposed by Ghysel and his colleagues [47,48], but we also estimated the IRFs based on the MF-VAR model. In this way, we were able to capture the dynamic impact of nurse staffing on patient outcomes and on healthcare expenditure for inpatient care service reimbursement across a high frequency timescale (a 3-month cycle of a quarter timespan in this study) over a 12-month period, and four mechanisms potentially trigging the vicious cycle of hospital competition were discussed accordingly.
Third, it is essential to address that the healthcare systems worldwide have been toward public-private mixed (or more private-like) financing systems due to an aging population, diffusion of new technologies, and growth of income [28]. It follows that we observed a common privatization trend in healthcare provision, and, in turn, it created a severer market competition in many publicly financed healthcare systems such as the NHS (e.g., Australia, Belgium, Finland, Iceland, Ireland, Norway, Spain, and United Kingdom) and SHI systems (e.g., Austria, Canada, Korea, and Japan) [26,28]. Although the harmful effects of PNR on patient outcomes were confirmed from previous studies in the NHS [2,3,4,7,8,10,14,15,16,17,18] and SHI systems [5,9,14,15,16,17,18], most of these studies belonged to the cross-sectional or static-type studies. It follows that these studies failed to identify causality between nurse staffing and patient outcomes, evaluate the propagation mechanism of nurse staffing on patient outcomes, and avoid the potential aggregation biases [2,3,4,5,6,7,8,9,10,14,15,16,17,18]. Therefore, the methodologies (such as the MF-VAR model, Granger causality test, and impulse-response analyses) used in this study not only generated results echoing the evidence obtained from previous studies [2,3,4,5,6,7,8,9,10,14,15,16,17,18], but they also amended the disadvantages of the cross-sectional or static-type studies. The methodologies used in this study could be easily performed through inputting publicly reported time series data in cases when individual data are difficult to be collected (e.g., the COVID-19 outbreak period). The empirical results obtained through our empirical models could serve as important information for the surveillance of ICQ under the hospital competition in the publicly financed healthcare system.
This study, nonetheless, has several limitations. First, the potential size distortion due to a small sample size used in this study (i.e., a total of 28 and 84 quarterly and monthly observations) would create invalid inferences, so all results generated from the MF-VAR model were based on the bootstrap method in order to adjust for the size distortion. Second, the cyclical components of time series were used for our MF-VAR model, so inferences obtained from this study are limited regarding the short-run relationships among nurse staffing, patient outcomes, and hospital competition under the GBPS of Taiwan’s NHI system. Third, this study belongs to the ecological type of time series analyses. Thus, in order to prevent the ecological fallacy of study [57], our empirical results neither refer to individual patients’ decisions in seeking care (such as ED care or inpatient care) after discharge from a hospital nor the hospitals’ managerial actions (such as nurse deployment) in response to changes in patient outcomes. We recommend that future studies collect the individual data needed to explore the interactions among hospitals’ managerial actions impacting quality of care, the patients’ decisions in seeking care, and patient outcomes in response to hospital competition under the GBPS of Taiwan’s NHI system.
5. Conclusions
Hospital administrators and healthcare practitioners have long been concerned about the adverse effect of poor nurse staffing on patient outcomes [1,2,3,4,5,6,7,8,9,10,11,12,13,14,15,16,17,18,19,20,21,22,23,24,25,35]. The critical force driving inappropriate deployment of nursing staffs at hospitals is hospital (quantity) competition under the GBPS. In this study, we applied the MF-VAR model to investigate the interdependences between nurse staffing, patient outcomes, and hospital competition under the GBPS of Taiwan’s NHI system for the first time. Our empirical results from the forecast error variance decomposition yielded higher explanatory power from the MF-VAR model in contrast to the conventional VAR model with single frequency data. The mixed frequency Granger causality tests identified bi-directional causation between nurse staffing and patient outcomes and one-way Granger causality running from nurse staffing to reimbursement to inpatient care services. The impulse-response analyses found positive (negative) effects of PNR on adverse patient outcomes (reimbursement payments for inpatient care services) in all types of hospitals but detrimental effects of adverse patient outcomes on PNR in medical centers (regional and district hospitals) across a 12-month period.
These findings generated from the aforementioned models suggest that nurse staffing is an essential determinant of both patient outcomes and reimbursement payments under the GBPS of Taiwan’s NHI system. Therefore, the vicious cycle triggered by hospital (quantity) competition under the GBPS of Taiwan’s NHI system works differently in different types of hospitals. Strategic policies (such as directly subsidizing for appropriate nurse staffing levels and the inclusion of the nurse staffing level as a vital standard for hospital accreditation) should be implemented for all hospitals in order to preserve the quality of inpatient care services, and more comprehensive interventions aimed towards switching hospital competition from quantity to quality competition should focus on the harmful effect of adverse patient outcomes on nurse staffing in medical centers and regional hospitals.
Funding
This research was funded by the Ministry of Science and Technology in Taiwan for the research project entitled “Now-casting for the effect of nurse staffing on quality of inpatient care during the COVID-19 pandemic outbreak: Evidence from Taiwan” with Grant No. 110-2410-H-025-012. The APC was funded by the Ministry of Science and Technology and National Taichung University of Science and Technology, Taiwan.
Data Availability Statement
Data are available upon request to the author.
Acknowledgments
The final proof-reading of this study by Lisa Brutcher (at Washington State University, USA) is deeply acknowledged. All errors are mine.
Conflicts of Interest
The author declares no conflict of interest, and the funders had no role in the design of the study; in the collection, analyses, or interpretation of data; in the writing of the manuscript; or in the decision to publish the results.
Appendix A
In order to present these data better, we exhibit the trends of all variables used in this study in Figure A1. Note that Taiwan’s NHIA implemented the first stage of the post-acute care intervention program during the period of July 1st 2017~April 10th 2020 [58]. Attributable to this intervention program, we found significant structural changes in the two ICQ indicators and PNR at medical centers and district hospitals during the intervention period. In addition, we also found a sudden drop in PNRs in the three different types of hospitals during the periods of three COVID-19 strike waves (see grey shading area in Figure A1) in Taiwan, corresponding to a sharp fall in the two ICQ indicators and rise in real ICE per admission. These results reflect the fact that inpatient care utilization was largely reduced due to public fear of COVID-19 infection and the promotion of policies discouraging non-urgent healthcare services, and, in turn, a reduction in hospital (quantity) competition and lower PNRs were found. These findings have implications regarding the interdependences between PNR, ICQ, and real ICE per admission under the GBPS of Taiwan’s NHI system.
In order to obtain stationary time series of these variables, the cyclic components of these time series were extracted through the Hodrick and Prescott filter method [51]. The cyclic components of all variables with the logarithm transformation in level terms were both de-mean and de-trend time series, which enabled us to accommodate structural changes of those variables discussed in the aforementioned pargagaph. The plots of the cyclic components of all variables are displayed in Figure A2.
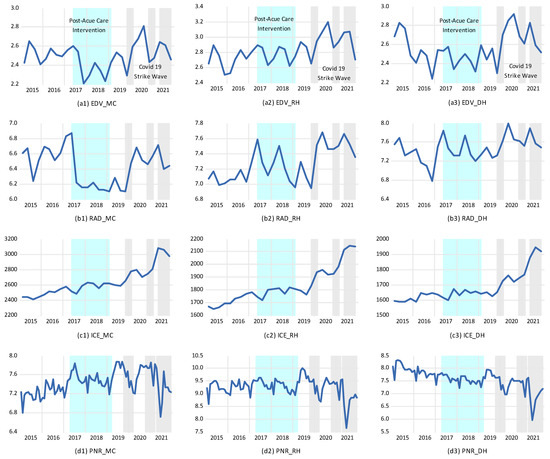
Figure A1.
Time plots for all variables used in this study 8.
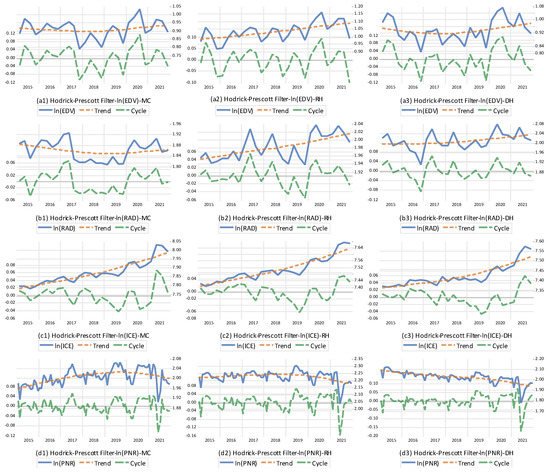
Figure A2.
Time plots for all variables transformed by the Hodrick-Prescott filter method 9.
Notes
| 1 | Inpatient care expenditure per admission was calculated using total inpatient care expenditure divided by total admissions in a specific type of hospital, and it was measured using the 2016 price level (constant 2016 USD). The patient-to-nurse ratio was defined as the mean of number of patients divided by the nurse staffing number within three shifts per day in a specific type of hospital. The quarterly and monthly sample periods start from 2015: Q1 to 2021: Q4 and 2015: M1 to 2021: M12, resulting in a total of 28 and 84 quarterly and monthly observations, respectively. The IQR and JB statistics represent the interquartile range and Jarque-Bera statistics, respectively. ”**”, ”*” denote 1% and 5% significance levels for the rejection of null hypothesis of the normality of time series, respectively. |
| 2 | All variables are defined in the same way as for Table 1. The lag length is selected based on Bayesian Information Criterion (BIC) with the maximal lag as eight. ”**” and “*” represent 1% and 5% significance levels, respectively. , k = MC, RH, and DH define cyclic components of aggregate monthly PNR. |
| 3 | Quarterly data on cyclical components of quality of care indicators (such as the 3-day EDV rate and 14-day readmission rate), inpatient care expenditure per admission, and monthly data on cyclical components of the patient-to-nurse ratio were used to estimate the MF-VAR model. The monthly data on cyclical components of the patient-to-nurse ratio were aggregated into quarterly data (PNRA) when the LF-VAR model was estimated. The lag length is selected based on Newey and West’s automatic lag selection with the maximal lag as 3 [52]. “PNRA EDV”, for example, represents the null hypothesis of non-causality from PNRA to RER. The bold font of PNR denotes the vector of cyclical components of PNR symbolized by [C_lnPNR1, C_lnPNR2, C_lnPNR3]’. “PNR EDV”, for example, represents the null hypothesis of joint non-causality from the vector of cyclical components of PNR to the cyclical component of EDV. The p values were calculated using the heteroscedasticity-robust parametric bootstrap of Gonçalves and Kilian [53] with 10,000 replications. “***”,”**”,”*” represent 1%, 5%, and 10% significance levels, respectively. |
| 4 | Figure 1 plots the impulse response functions (IRFs) for monthly horizons h = 0, 1, 2, …, 12 based on the MF-VAR model of quarterly data on cyclical components of quality of care indicators (such as the 3-day EDV rate and 14-day readmission rate), inpatient care expenditure per admission, and three individual monthly cyclical components of the patient-to-nurse ratio symbolized by C_lnPNR1, C_lnPNR2, and C_lnPNR3 in a quarter timespan. The Cholesky decomposition with order PNR1, PNR2, PNR3, EDV (or RAD), and ICE is selected. The sample period covers 2015:Q1–2021:Q4. The responses of variable Y (say, EDV) to 1σ shock in X (say, PNR1) at monthly horizon h is written as “PNR1=>RER”. MC, RH, and DH represent medical centers, regional hospitals, and district hospitals, respectively. Blue shaded areas denote 90% confidence intervals of IRFs based on the Monte Carlo simulation method with 10,000 replications. |
| 5 | Figure 2 plots the impulse response functions (IRFs) for monthly horizons h = 0, 1, 2, …, 12 based on the MF-VAR model of quarterly data on cyclical components of quality of care indicators (such as the 3-day EDV rate and 14-day readmission rate), inpatient care expenditure per admission, and three individual monthly cyclical components of the patient-to-nurse ratio symbolized by C_lnPNR1, C_lnPNR2, and C_lnPNR3 in a quarter timespan. The Cholesky decomposition with order PNR1, PNR2, PNR3, EDV (or RAD), and ICE is selected. The sample period covers 2015:Q1~2021:Q4. The responses of variable Y (say, EDV) to 1σ shock in X (say, ICE) at monthly horizon h is written as “ICE =>EDV”. Blue shaded areas denote 90% confidence intervals of IRFs based on the Monte Carlo simulation method with 10,000 replications. MC, RH, and DH denote medical centers, regional hospitals, and district hospitals, respectively. |
| 6 | Notations presented in this table are the same as those used in Table 3. The sum of variance decomposition may not equal 100 due to rounding. |
| 7 | The directions of arrows were drawn based on the Granger causality tests. The arrows with bold (dot) lines represent significant (insignificant) paths connecting two target variables based on 90% confidence intervals of the impulse-response effects accumulated across a 3-month cycle of a quarter timespan over a 12-month period. MC, RH, and DH denote medical centers, regional hospitals, and district hospitals, respectively. |
| 8 | EDV and RAD represent the 3-day EDV rate and 14-day readmission rate, respectively. ICE is real inpatient care expenditure per admission at the 2016 price level (USD). PNR symbolizes the patient-to-nurse ratio. MC, RH, and DH represent medical centers, regional hospitals, and district hospitals, respectively. Light blue and grey shaded areas show the post-acute care intervention period and COVID-19 strike waves, respectively. |
| 9 | All notations used in this figure are the same as for Figure 1. represents the natural logarithm transformation. |
References
- Aiken, L.H.; Clarke, S.P.; Sloane, D.M.; Sochalski, J.; Silber, J.H. Hospital nurse staffing and patient mortality, nurse burnout, and job dissatisfaction. JAMA 2002, 2288, 1987–1993. [Google Scholar] [CrossRef] [PubMed]
- McHugh, M.D.; Aiken, L.H.; Sloane, D.M.; Windsor, C.; Douglas, C.; Yates, P. Effects of nurse-to-patient ratio legislation on nurse staffing and patient mortality, readmissions, and length of stay: A prospective study in a panel of hospitals. Lancet 2021, 397, 1905–1913. [Google Scholar] [CrossRef]
- McHugh, M.D.; Aiken, L.H.; Windsor, C.; Douglas, C.; Yates, P. Case for hospital nurse-to-patient ratio legislation in Queensland, Australia, hospitals: An observational study. BMJ Open 2020, 10, e036264. [Google Scholar] [CrossRef]
- Haegdorens, F.; Van Bogaert, P.; De Meester, K.; Monsieurs, K.G. The impact of nurse staffing levels and nurse’s education on patient mortality in medical and surgical wards: An observational multicentre study. BMC Health Serv. Res. 2019, 19, 864. [Google Scholar] [CrossRef]
- Rochefort, C.M.; Beauchamp, M.E.; Audet, L.A.; Abrahamowicz, M.; Bourgault, P. Associations of 4 nurse staffing practices with hospital mortality. Med. Care 2020, 58, 912–918. [Google Scholar] [CrossRef] [PubMed]
- Aiken, L.H.; Simonetti, M.; Sloane, D.M.; Cerón, C.; Soto, P.; Bravo, D.; Galiano, A.; Behrman, J.R.; Smith, H.L.; McHugh, M.D.; et al. Hospital nurse staffing and patient outcomes in Chile: A multilevel cross-sectional study. Lancet Glob. Health 2021, 9, e1145–e1153. [Google Scholar] [CrossRef]
- Griffiths, P.; Maruotti, A.; Recio Saucedo, A.; Redfern, O.C.; Ball, J.E.; Briggs, J.; Dall’Ora, C.; Schmidt, P.E.; Smith, G.B.; Missed Care Study Group. Nurse staffing, nursing assistants and hospital mortality: Retrospective longitudinal cohort study. BMJ Qual. Saf. 2019, 28, 609–617. [Google Scholar] [CrossRef] [PubMed]
- Fagerström, L.; Kinnunen, M.; Saarela, J. Nursing workload, patient safety incidents and mortality: An observational study from Finland. BMJ Open 2018, 8, e016367. [Google Scholar] [CrossRef]
- Kim, Y.; Kim, H.Y.; Cho, E. Association between the bed-to-nurse ratio and 30-day post-discharge mortality in patients undergoing surgery: A cross-sectional analysis using Korean administrative data. BMC Nurs. 2020, 19, 17. [Google Scholar] [CrossRef] [PubMed]
- Tvedt, C.; Sjetne, I.S.; Helgeland, J.; Bukholm, G. An observational study: Associations between nurse-reported hospital characteristics and estimated 30-day survival probabilities. BMJ Qual. Saf. 2014, 23, 757–764. [Google Scholar] [CrossRef] [PubMed]
- Liang, Y.W.; Chen, W.Y.; Lin, Y.H. Estimating a hospital production function to evaluate the effect of nurse staffing on patient mortality in Taiwan: The longitudinal count data approach. Rom. J. Econ. Forecast. 2015, 18, 154–169. [Google Scholar]
- Liang, Y.W.; Chen, W.Y.; Lee, J.L.; Huang, L.C. Nurse staffing, direct nursing care hours and patient mortality in Taiwan: The longitudinal analysis of hospital nurse staffing and patient outcome study. BMC Health Serv. Res. 2012, 12, 44. [Google Scholar] [CrossRef] [PubMed]
- Liang, Y.W.; Tsai, S.F.; Chen, W.Y. A longitudinal study of the effects of nurse staffing on patient outcomes for Taiwan acute care hospital. J. Nurs. Res. 2012, 20, 1–8. [Google Scholar] [CrossRef] [PubMed]
- Amiri, A.; Vehviläinen-Julkunen, K.; Solankallio-Vahteri, T.; Tuomi, S. Impact of nursing staffing on reducing infants, neonatal, perinatal mortality rates: Evidence from 35 OECD countries. Int. J. Nurs. Sci. 2020, 7, 161–169. [Google Scholar]
- Amiri, A.; Solankallio-Vahteri, T. Nurse-staffing level and quality of acute care services: Evidence from cross-national panel data analysis in OECD countries. Int. J. Nurs. Sci. 2019, 6, 6–16. [Google Scholar] [CrossRef]
- Ball, J.E.; Bruyneel, L.; Aiken, L.H.; Sermeus, W.; Sloane, D.M.; Rafferty, A.M.; Lindqvist, R.; Tishelman, C.; Griffiths, P.; RN4Cast Consortium. Post-operative mortality, missed care and nurse staffing in nine countries: A cross-sectional study. Int. J. Nurs. Stud. 2018, 78, 10–15. [Google Scholar] [CrossRef]
- Aiken, L.H.; Sloane, D.; Griffiths, P.; Rafferty, A.M.; Bruyneel, L.; McHugh, M.; Maier, C.B.; Moreno-Casbas, T.; Ball, J.E.; Ausserhofer, D.; et al. Nursing skill mix in European hospitals: Cross-sectional study of the association with mortality, patient ratings, and quality of care. BMJ Qual. Saf. 2017, 26, 559–568. [Google Scholar] [CrossRef]
- Aiken, L.H.; Sloane, D.M.; Bruyneel, L.; Van den Heede, K.; Griffiths, P.; Busse, R.; Diomidous, M.; Kinnunen, J.; Kózka, M.; Lesaffre, E.; et al. Nurse staffing and education and hospital mortality in nine European countries: A retrospective observational study. Lancet 2014, 383, 1824–1830. [Google Scholar] [CrossRef]
- Van, T.; Annis, A.M.; Yosef, M.; Robinson, C.H.; Duffy, S.A.; Li, Y.F.; Taylor, B.A.; Krein, S.; Sullivan, S.C.; Sales, A. Nurse staffing and healthcare-associated infections in a national healthcare system that implemented a nurse staffing directive: Multi-level interrupted time series analyses. Int. J. Nurs. Stud. 2020, 104, 103531. [Google Scholar] [CrossRef]
- Wang, L.; Lu, H.; Dong, X.; Huang, X.; Li, B.; Wan, Q.; Shang, S. The effect of nurse staffing on patient-safety outcomes: A cross-sectional survey. J. Nurs. Manag. 2020, 28, 1758–1766. [Google Scholar] [CrossRef]
- Butler, M.; Schultz, T.J.; Halligan, P.; Sheridan, A.; Kinsman, L.; Rotter, T.; Beaumier, J.; Kelly, R.G.; Drennan, J. Hospital nurse-staffing models and patient- and staff-related outcomes. Cochrane Database Syst. Rev. 2019, 4, CD007019. [Google Scholar] [CrossRef] [PubMed]
- Redfern, O.C.; Griffiths, P.; Maruotti, A.; Recio Saucedo, A.; Smith, G.B.; Missed Care Study Group. The association between nurse staffing levels and the timeliness of vital signs monitoring: A retrospective observational study in the UK. BMJ Open 2019, 9, e032157. [Google Scholar] [CrossRef] [PubMed]
- Twigg, D.E.; Kutzer, Y.; Jacob, E.; Seaman, K. A quantitative systematic review of the association between nurse skill mix and nursing-sensitive patient outcomes in the acute care setting. J. Adv. Nurs. 2019, 75, 3404–3423. [Google Scholar] [CrossRef] [PubMed]
- Bobay, K.L.; Yakusheva, O.; Weiss, M.E. Outcomes and cost analysis of the impact of unit-level nursing staffing post-discharge utilization. Nurs. Econ. 2011, 29, 69–78. [Google Scholar] [PubMed]
- Weiss, M.E.; Yakusheva, O.; Bobay, K.L. Quality and cost analysis of nurse staffing, discharge preparation, and post discharge utilization. Health Serv. Res. 2011, 46, 1473–1494. [Google Scholar] [CrossRef]
- National Health Insurance Administration. National Health Insurance: 2021–2022 Annual Report. Executive Yuan, Taiwan. 2022. Available online: https://www.nhi.gov.tw/Content_List.aspx?n=9223A12B5B31CB37&topn=4864A82710DE35ED (accessed on 15 August 2022).
- Chen, W.Y. On the network transmission mechanisms of disease-specific healthcare expenditure spillovers: Evidence from the connectedness network analyses. Healthcare 2021, 9, 319. [Google Scholar] [CrossRef]
- Chen, W.Y. Does healthcare financing converge? Evidence from eight OECD Countries. Int. J. Health Care Financ. Econ. 2013, 13, 279–300. [Google Scholar] [CrossRef]
- Chen, W.Y.; Chi, C.H.; Lin, Y.H. The willingness-to-pay for the health care under Taiwan’s National Health Insurance system. Appl. Econ. 2011, 43, 1113–1123. [Google Scholar] [CrossRef]
- Chen, W.Y. The effect of interdependences of referral behaviors on the quality of ambulatory care: Evidence from Taiwan. Risk Manag. Healthc. Policy 2021, 14, 4709–4721. [Google Scholar] [CrossRef]
- Wong, L. A Guide to Taiwan’s Health Industries. Taipei: PricewaterhouseCoopers (PwC). 2020. Available online: https://www.pwc.tw/en/publications/taiwan-health-industries.html (accessed on 15 August 2022).
- Chen, W.Y.; Lin, Y.H. Hospital non-price competition under global budget payment and prospective payment system. Expert Rev. Pharm. Outcomes Res. 2008, 8, 301–308. [Google Scholar] [CrossRef]
- Lu, M.S.; Tseng, H.Y.; Liang, S.Y.; Lin, C.F. Concept for planning the nurse-patient ratio and nursing fee payment linkage system. Hu Li Za Zhi 2017, 64, 17–24. [Google Scholar] [CrossRef] [PubMed]
- Turton, M. Does Taiwan’s nursing problem have a cure? Taipei Times. 21 February 2022. Available online: https://www.taipeitimes.com/News/feat/archives/2022/02/21/2003773473 (accessed on 15 August 2022).
- Jun, J.; Ojemeni, M.M.; Kalamani, R.; Tong, J.; Crecelius, M.L. Relationship between nurse burnout, patient and organizational outcomes: Systematic review. Int. J. Nurs. Stud. 2021, 119, 103933. [Google Scholar] [CrossRef] [PubMed]
- de Cordova, P.B.; Rogowski, J.; Riman, K.A.; McHugh, M.D. Effects of public reporting legislation of nurse staffing: A trend analysis. Policy Politics Nurs. Pract. 2019, 20, 92–104. [Google Scholar] [CrossRef] [PubMed]
- He, J.; Staggs, V.S.; Bergquist-Beringer, S.; Dunton, N. Nurse staffing and patient outcomes: A longitudinal study on trend and seasonality. BMC Nurs. 2016, 15, 60. [Google Scholar] [CrossRef] [PubMed]
- Everhart, D.; Schumacher, J.R.; Duncan, R.P.; Hall, A.G.; Neff, D.F.; Shorr, R.I. Determinants of hospital fall rate trajectory groups: A longitudinal assessment of nurse staffing and organizational characteristics. Health Care Manag. Rev. 2014, 39, 352–360. [Google Scholar] [CrossRef]
- Winter, S.G.; Bartel, A.P.; de Cordova, P.B.; Needleman, J.; Schmitt, S.K.; Stone, P.W.; Phibbs, C.S. The effect of data aggregation on estimations of nurse staffing and patient outcomes. Health Serv. Res. 2021, 56, 1262–1270. [Google Scholar] [CrossRef]
- Liu, Y.H.; Chang, W.S.; Chen, W.Y. Health progress and economic growth in the United States: The Mixed Frequency VAR analyses. Qual. Quant. 2019, 53, 1895–1911. [Google Scholar] [CrossRef]
- Silvestrini, A.; Veredas, D. Temporal aggregation of univariate and multivariate time series models: A survey. J. Econ. Surv. 2008, 22, 458–497. [Google Scholar] [CrossRef]
- National Development Council. Population Projections for the R.O.C. (Taiwan): 2020~2070. Executive Yuan, Taiwan. 2022. Available online: https://www.ndc.gov.tw/en/cp.aspx?n=2E5DCB04C64512CC (accessed on 15 August 2022).
- Cheng, T.M. Taiwan’s Health Care System: The Next 20 Years. Brookings Op-Ed. 2015. Available online: https://www.brookings.edu/opinions/taiwans-health-care-system-the-next-20-years/ (accessed on 15 August 2022).
- Taiwan Union of Nurses Association. Taiwan Nursing Workforce Statistics. Available online: https://www.nurse.org.tw/publicUI/H/H10201.aspx?arg=8DA73DB09C6642F030 (accessed on 15 August 2022).
- Huang, C.C.; Lin, S.H.; Zheng, K.W. The relationship among emotional intelligence, social support, job involvement, and turnover intention—A study of nurses in Taiwan. J. Econ. Bus. 2019, 2, 652–659. [Google Scholar] [CrossRef]
- Chin, W.S.; Chen, Y.C.; Ho, J.J.; Cheng, N.Y.; Wu, H.C.; Shiao, J.S.C. Psychological work environment and suicidal ideation among nurses in Taiwan. J. Nurse Scholarsh. 2019, 51, 106–113. [Google Scholar] [CrossRef]
- Ghysels, E. Macroeconomics and the reality of mixed frequency data. J. Econom. 2016, 193, 294–314. [Google Scholar] [CrossRef]
- Ghysels, E.; Hill, J.B.; Motegi, K. Testing for Granger causality with mixed frequency data. J. Econom. 2016, 192, 207–230. [Google Scholar] [CrossRef]
- Motegia, K.; Sadahirob, A. Sluggish private investment in Japan’s Lost Decade: Mixed frequency vector autoregression approach. North Am. J. Econ. Financ. 2018, 43, 118–128. [Google Scholar] [CrossRef]
- National Health Insurance Administration. Web of Quality of Care in National Health Insurance. Executive Yuan, Taiwan. 2022. Available online: https://www.nhi.gov.tw/AmountInfoWeb/TargetItem.aspx?rtype=2 (accessed on 15 August 2022).
- Hodrick, R.J.; Prescott, E.C. Postwar U.S. business cycles: An empirical investigation. J. Money Credit Bank. 1997, 29, 1–16. [Google Scholar] [CrossRef]
- Newey, W.; West, K. Automatic lag selection in covariance matrix estimation. Rev. Econ. Stud. 1994, 61, 631–653. [Google Scholar] [CrossRef]
- Gonçalves, S.; Kilian, L. Bootstrapping autoregressions with conditional heteroscedasticity of unknown form. J. Econom. 2004, 123, 89–120. [Google Scholar] [CrossRef]
- National Health Insurance Administration. Statistics for the Daily Patient-to Nurse Ratio. Executive Yuan, Taiwan. 2022. Available online: https://www.nhi.gov.tw/Content_List.aspx?n=4037A32CDEF1DDCF&topn=CDA985A80C0DE710 (accessed on 15 August 2022).
- Ministry of Health and Welfare. Statistics of Medical Care Institution & Hospital Utilization. Executive Yuan, Taiwan. 2022. Available online: https://dep.mohw.gov.tw/dos/lp-5099-113.html (accessed on 15 August 2022).
- National Health Insurance Administration. Business Report for National Health Insurance. Executive Yuan, Taiwan. 2022. Available online: https://www.nhi.gov.tw/Content_List.aspx?n=6A330BB09FB0EA45&topn=23C660CAACAA159D (accessed on 15 August 2022).
- Robinson, W.S. Ecological correlations and the behavior of individuals. Am. Sociol. Rev. 1950, 15, 351–357. [Google Scholar] [CrossRef]
- Ministry of Health and Welfare. Post-Acute Care Integration Program. Executive Yuan, Taiwan. 2020. Available online: https://www.nhi.gov.tw/Content_List.aspx?n=5A0BB383D955741C&topn=5FE8C9FEAE863B46 (accessed on 15 August 2022).
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the author. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).